Abstract
Perinatal depression can have deleterious effects on the formation of the relationship between mother and infant: evidence shows that it threatens not only the mental but also the physical health of the mother and the physical and psychological development of the baby; and it can have a profound impact on the care that the baby receives and on the future relationships that the baby will form. As babies learn from the outside in, through the mind of another person, they learn how to behave from the responses of their environment. In the context of perinatal depression, which often combines elevated stress levels with low emotional arousal, it can be difficult for a mother to recognize and perceive her own and her infant’s emotions, needs, and desires in order to appropriately interact with their infant. The purpose of this paper is to present an overview on previous literature reviewing research on perinatal depression and its impact on the mother-infant interaction, with a particular focus on current dyadic interventions for the enhancement of their relationship. Given the prevalence of perinatal depression and the adverse effects this disorder has on women and their children, the identification of effective treatments, which include both the mother and baby, has important implications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Perinatal depression is a mood disorder that can affect women during pregnancy and after childbirth. The word ‘perinatal’ refers to the time before and after the birth of a child: depression that occurs during pregnancy is referred to as antenatal (AND), and depression occurring after childbirth is described as postpartum depression (PND). This mood disorder is one of the most common complications of the antenatal and postpartum periods [1]: AND affects approximately 7–12% of women, and PND affects 10–15% of women, with even higher rates among low-income populations [2,3,4] and ethnic minority groups [5]. Furthermore, women who experience perinatal depressive episodes are at increased risk for subsequent episodes of both postpartum and non-postpartum depression [6]. In terms of major risk factors for perinatal depression, they include a history of depression and/or anxiety, bipolar disorder, unintended pregnancy, life stress, history of sexual abuse, domestic violence, low social support, and poor relationship quality [7,8,9].
Perinatal depression not only has implications for maternal mental health and wellbeing [10], which includes depressed mood, anxiety, compulsive thoughts, loss of control, feelings of inadequacy, inability to cope, irrational fears, fatigue, and despair [11], but also for decreased quality of interactions between mothers and their children [12], higher levels of psychiatric disturbances among children [13], and greater child insecurity in attachment relationships [14]. Some studies have underlined that poor perinatal attachment until 15 months postpartum, reduced medical check-ups, low foetal development, preterm deliveries, and low care of the infant are often associated with prenatal depressive symptoms [15,16,17]. Moreover, a child’s behavioural, cognitive, linguistic, and emotional problems can persist into school age as a long-term effect of a mother’s perinatal depression [18, 19]. Evidence shows that problems can recur also into adulthood. In a study conducted with the aim to study whether the adult offspring of antenatally depressed mothers were at an elevated risk of developing a mental health disorder (i.e. psychoses, depression, bipolar disorder, antisocial and borderline personality disorder, and schizotypal and affective traits), results showed that adult offspring of antenatally depressed mothers had an increased risk of depression, and the male offspring for antisocial personality disorder, compared to cohort members without antenatally depressed mothers [20].
2 Mother-Infant Interaction
During mother-infant interactions, depressed mothers usually interact less with their infant and are more withdrawn [21, 22] and less responsive to infant cues, leading to greater incidences of insensitive caregiving [23, 24]. Maternal sensitivity is highly predictive of infant secure attachment [25], which has long been linked to optimal developmental outcomes including offspring mental health [26]. Depressive mothers also develop a less-intense relationship with their children, experience more stress, perceive their children in a more negative way, and may assess them as less securely attached than non-depressive mothers [27]. Some mothers experience lowered maternal instinct, as well as greater hostility and aggressive impulses, and a feeling of rejection towards their own children [28]. Moreover, depressed mothers are less likely to mentalize appropriately with their infants [29]. As babies learn from the outside in, through the mind of another person, they learn how to regulate their behaviours from the responses of their mothers. In the context of depression, which often combines elevated stress levels with low emotional arousal, it can be difficult for a mother to recognize and perceive her own and her child’s needs and emotions: this can have consequences on the ability to feel what they are thinking and to think about what they are feeling in order to appropriately interact with their infant. Consequently, children may tend to mirror this behaviour by disengaging and adopting a passive behavioural style [21].
2.1 Attachment
The infant’s extreme dependency on their caregiver, their sensitivity to interpersonal contacts [30], and the fact that, in the great majority of cases, the mother constitutes the infant’s primary environment in the first postnatal months make the question of the impact of depression one of particular importance. According to John Bowlby [31], humans are born with a predisposition to become attached to caregivers, and attachment is one specific and circumscribed aspect of the relationship between a child and caregiver that involves with making the child feel safe, secure, and protected. In addition, attachment is a mechanism where the child uses the primary caregiver as a secure base from which to explore and, when necessary, as a haven of safety and a source of comfort [32], and it is a powerful predictor of a child’s later social and emotional outcome [33]. Many studies have suggested that the influence of a mother’s depressive disorder on the way the mother and child interact can be linked to the subsequent emotional disturbance of the child [34] and to the insecure infant attachment [35,36,37].
Most of the assessments of the quality of infant attachment have been made using the Ainsworth’s Strange Situation procedure [38]: in a study conducted with children aged two to three, it was found that insecure attachment was more frequent in children whose mothers had a history of major depression than in those whose mothers had no such history, and the evidence for insecure attachment was the child’s avoidance of and resistance to the mother when reunited with her after a brief separation [39]. Another study conducted by Lyons-Ruth and colleagues using the Strange Situation found an association between insecure attachment at 12 months and high levels of maternal depression [35]. Similarly, Lynne Murray [36] found a significant association between the occurrence of depression in the postnatal period and insecurity of attachment at 18 months postpartum, with avoidance being the prominent insecure attachment profile. In addition, the author found insecure attachment, behaviour problems, and poorer cognitive outcome associated with the occurrence of postnatal depression to obtain in infants of 18 months even though, in the great majority of cases, the mother’s depression had remitted by around 6–8 months postpartum.
2.2 Mentalization
Mentalization has been defined as the mental ability to recognize and interpret one’s own and others’ behaviour in the context of underlying mental processes such as needs, feelings, thoughts, beliefs, and desires, and it is central for the affect regulation, interpersonal relationships, and social functioning [40]. As Peter Fonagy [41] underlines, mentalizing is something we do interactively: while interacting, each person remains attentive to mental states, holding the other person’s mind in mind as well as their own. Additionally, we aspire to understand each other as autonomous persons and to influence each other on the basis of our understanding.
It is well known that mentalization is a developmental achievement that emerges in the attachment context of the early infant-caregiver interaction: during the first years of life, the primary caregiver’s appropriate mirroring of the infant’s needs and emotions—and the infant’s exposure to it—is essential to the development of an adequate intersubjectivity [42] and mentalizing models [43]. An adequate interaction context then, where the caregiver shows interest in the infant’s mental state, can be expected to facilitate secure attachment and advance the development of mentalization [44, 45]. Furthermore, mentalizing is proposed as one of the mechanisms that utilize its influence on child’s attachment security and socio-cognitive development [46].
Mentalizing is not only something mothers do but also something they can fail to do. Although just few studies have investigated maternal mentalization in the context of perinatal depression during mother-infant interaction, depressed mood is hypothesized to lead to increased arousal and stress levels, resulting in impairments and distortions in mentalization, which in turn may cause a loss of resilience in the face of stress, adding to a vicious cycle of increasingly depressed mood [47]. Murray et al. [48] have reported that depressed mothers are less likely to acknowledge infant intentions and agency, compared with non-depressed mothers. Similarly, Herrera et al. [49] found that mothers with depression made fewer references to their infants’ emotional and cognitive experience in their speech, and, finally, another study of in-patients found that depressed mothers, compared with healthy controls, were marginally less likely to comment on their infants’ mental state [29].
In women who experience mental problems shortly after birth, impaired mentalization may have negative consequences for the mother’s ability to provide sensitive caregiving for her child [50]. A study conducted with depressed fathers and their 3-month-old infants showed that not only depressed fathers were more negative about themselves and their infants compared with non-depressed fathers but depression was also associated with speech that was more focused on the paternal experience and less on the infant’s experience [51]. Levy and Truman [52] suggested that when caregivers are not able to reflect on their own mental states, their ability to be sensitive and emotionally responsive to their children is restricted. In fact, it has been underlined that the ability to mentalize is a key aspect of maternal sensitivity [45], which is one of the most important predictors of child socioemotional development [53].
2.3 Maternal Sensitivity
Maternal sensitivity includes a variety of interrelated affective and behavioural caregiving attributes. It is defined as the quality of a mother’s behaviours that are based on her abilities to perceive and interpret her infant’s cues and respond to them appropriately, and it is a dynamic process which accompanies the adaptation and changeability [54]. Maternal sensitivity is an important aspect and a key indicator of the quality of early mother-infant interactions. As caregivers are critical to the development of the offspring, maternal sensitivity can affect an infant’s behaviour and development [55]. Particularly, during the first year of life, sensitive mothering is considered to be the most important precursor of the secure attachment relationship that influences an infant’s physical, psychological, and cognitive development [56, 57]. Indeed, decreased maternal sensitivity is associated with poor mother-child interaction quality and, ultimately, insecure infant attachment.
It is largely demonstrated that maternal depression, both during and after pregnancy, is associated with decreased maternal sensitivity and less responsiveness to infants [58,59,60]. Mothers who suffer from depression are more susceptible to cognitive deficits and appear biased when processing emotional events [61]. Distorted maternal cognitions, driven by depressive symptoms, may lead to a mother-centred, rather than infant-centred, approach to caregiving, such as attending to their own needs before attending to infant signals, and this may result in less sensitive caregiving, particularly when infants are in distress [62, 63]. Moreover, they are more likely to have a negative view about themselves and the world and therefore may tend to have a negative view about their infants. Some studies have shown that the effects of depression during the perinatal period on early childhood outcomes can also have an impact on child language development, cognitive functioning, and increased risk of socioemotional difficulties [64,65,66], and these effects are thought to be, in part, related to decreased maternal sensitivity towards the infant and young child.
3 Mother-Infant Interventions
Although the perinatal period is considered a very delicate and sensitive phase for both mothers and infants, there are still many critical obstacles in the way of treatment for maternal perinatal depression. Since having a baby is generally considered to be a joyous event, perinatal depressive symptoms may be particularly susceptible to stigma, and women may be especially reluctant to talk about depression during the prenatal and postpartum period [67]. New mothers may tend to avoid, and not to communicate and elaborate, negative effects and thoughts related to childbirth, which could lead them to express and value openly only the positive aspects of childbirth. Negative or upsetting events that are kept secret or silent are more likely to result in health problems than those that could be spoken about more openly or, better, expressed in a written language that demands more integration and structure than spoken language [68]. Expressive writing could represent a low-cost early intervention to prevent or reduce the development of postpartum distress in new mothers [69].
A study that explored pregnant women’s barriers to mental health care found that although women with severe depression were generally willing to seek mental health care, they identified multiple barriers such as cost, lack of insurance, lack of transportation, long waits for treatment, previous bad experience with mental health care, and not knowing where to go for treatment [70]. Increasing the options for effective treatment of perinatal depression with the aim of improving mother-infant relationship remains a critical public health goal. The first year of the infant’s life is considered a crucial moment for the development of their self-regulatory skills [71, 72]: mother’s perinatal depression may have implications for the development of those important skills, making the infant more vulnerable to later psychopathology. In reviewing mediating factors between postnatal depression and adverse child outcomes, Murray and Cooper [73] stress early maternal interactional style, secondary to exposure to depression/social adversity, as critical in contributing to adverse outcomes. Thus, early interventions to improve mother-infant interaction are highly recommended in order to protect offspring future development.
There is growing evidence demonstrating that perinatal depression impacts a mother’s ability to properly interact with her baby. But treating maternal mood alone is not sufficient for improving mother-infant relationship difficulties [74]. Evidence-based individual psychotherapies, such as interpersonal psychotherapy and cognitive behavioural therapy, have demonstrated efficacy in reducing mothers’ depressive symptoms during the perinatal period [75], with overall depression remission rates similar to that of anti-depressants [76]. Evidence indicates that treating postpartum depression alone may not be sufficient in protecting children against long-term poor outcomes [27, 77]. In addition to reducing depressive symptoms, optimal perinatal depression interventions should address impaired caregiving to improve interaction quality and, in turn, enhance infants’ developmental outcomes [78, 79].
Mother-infant interventions may be an important complement to individual approaches, optimizing both maternal, infant, and relationship outcomes [80]. Evidence suggests that dyadically based postpartum interventions are more efficacious than individual psychotherapy for enhancing parenting and improving outcomes for infants of depressed mothers. These relationship-based treatments may be short or long term, and many of them are rooted in psychodynamic and attachment theories [81, 82]. Finally, some reviews [83, 84] have emphasized that interventions, mainly focused on the mother-infant relationship, have the best chance of improving outcomes for the children of depressed mothers, as well as reducing maternal depression.
3.1 Dyadic Psychotherapy
Child-parent psychotherapy (CPP) is an attachment theory-informed intervention intended to enhance the quality of the parent-child relationship and foster secure attachment, in which the primary focus is on the relationship between parent and child, rather than on each as individuals. Mothers and their children are seen in conjoint therapy sessions: through the use of observation and empathic comments, the therapist works towards assisting the mother in recognizing how she experiences and perceives her infant and herself, thereby allowing for correction of distorted perceptions and alterations in how the infant and the self are experienced. The therapist also attends to the nature of the interactions that occur between the mother and her child [85].
CPP has also been specifically examined within the context of maternal depression. CPP can protect cognitive development, and it increases rates of secure attachment among children of mothers with depression [86]. A recent study has shown that children of mothers with depression who received CPP attained significantly higher rates of secure attachment post-intervention than children of mothers with depression who received no intervention [87]. The follow-up study with the same sample reported evidence of the long-term effect of CPP: participation in CPP is associated with increased maternal warmth and decreased child anger/behavioural problems when children are 9 years old through its effect on attachment security at 36 months [87]. These results indicate that CPP continues to have positive indirect effects on both caregivers and children as far as 6 or more years post-intervention. The longitudinal findings from the study suggest that participation in CPP may have fostered positive maternal behaviour (i.e., maternal warmth) that improved attachment security and that this change in maternal behaviour is stable over time.
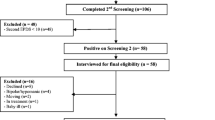
However, a pilot study conducted in 2014 did not confirm the same positive efficacy of mother-infant psychotherapy in the improvement of mother-infant interaction in the context of perinatal depression [88]. The study tested the perinatal dyadic psychotherapy (PDP), a dual-focused mother-infant intervention to prevent/decrease maternal postpartum depression and improve aspects of the mother-infant relationship related to child development. Forty-two depressed first-time mothers and their 6-week-old infants were enrolled and randomized to receive the PDP intervention or usual care. The intervention consisted of eight home-based, nurse-delivered mother-infant sessions consisting of a supportive, relationship-based, mother-infant psychotherapy and a developmentally based infant-oriented component focused on promoting positive mother-infant interactions. Results showed that depression and anxiety symptoms and diagnoses decreased significantly, and maternal self-esteem increased significantly across the study time frame. However, there were no significant differences between groups on parenting stress or mother-infant interaction at post-intervention and follow-up. Further research is needed to explore using low-intensity interventions as a first step in a stepped care approach.
3.2 Video Feedback Intervention
Video feedback is an effective technique used in early interventions which include video recording sessions of the mother and the baby playing together for 15–20 min [89]. Afterwards, the recorded scenes are analysed, and certain sequences are selected to work on with the mother. Video feedback technique can reveal important details of the mother-baby interaction: analysing the video recorded makes it possible to focus on specific aspects, which provides an opportunity to process and reflect on successful and difficult moments of the interaction [90]. Moreover, this allows mothers to identify emotions and reorganize their mental representations of themselves and the baby [91]. Then, with the therapist’s help, these images are shown to the mother in order to foster her reflection on her baby’s physical and verbal cues, as well as on her own representational models and bonding experiences [89]. According to Beebe [92], video feedback allows parents to learn about their babies’ non-verbal language, thus promoting new forms of interaction. The objective is to provide parents with a new perspective on the child’s non-verbal language and his/her skills and behaviours [93].
In the specific case of perinatal depression, evidence indicates that after a video feedback intervention, mothers discover a more positive image of themselves and increase their enjoyment of the time they spend with their children, which has a positive impact on their interaction [94]. A study conducted in 2015 [95] assessed a brief intervention for mother-infant dyads with mothers suffering from depressive symptomatology using the video feedback technique. The results of the intervention confirmed the effectiveness of early video feedback interventions in dyads with maternal depressive symptomatology and relationship difficulties. Results showed a significant increase in maternal sensitivity and child cooperativeness in the intervened dyads: the mothers in the experimental group display an increased ability to read children’s signals, interpret them adequately, and respond suitably and in accordance with their needs, alongside a decrease in their hostile behaviour, in terms of overt or concealed anger, which can be manifested through incongruity in maternal behaviour or direct intrusions.
In concordance to these findings, another pilot study conducted in 2020 [96] has confirmed the efficacy of video feedback technique intervention in the context of perinatal depression. The pilot study was designed to improve maternal-infant interaction, depressive symptoms, and cortisol patterns of depressed mothers and their infants. The results showed that there were significant differences favouring the group who received the intervention compared with the control group regarding the quality of maternal-infant interaction, particularly with maternal sensitivity and cognitive growth fostering activities and reduced infant diurnal cortisol. Thus, video feedback intervention appears to support improvements in interactions between depressed mothers and their infants and optimize infants’ diurnal cortisol patterns.
3.3 Group-Based Interventions
Mother-child group therapy interventions refer to a format of the dyads taking part in a psychological intervention aimed at helping them change or deal with problems they are encountering, guided by a therapist or counsellor. The advantages of group over individual interventions include learning by observing others (i.e. vicarious learning), knowing and being comforted by the fact that others share one’s difficulties, and practising in a safe environment constructive solution for interpersonal problems [97]. A recent pilot study showed the efficacy of a group-based perinatal depression intervention on depressive symptomatology, maternal-foetal attachment, and maternal sensitivity delivered with pregnant women with moderate to severe depressive symptoms. The pilot study findings provided preliminary support for the benefits of a perinatal depression intervention, delivered in a group setting, on reducing depressive symptomatology and improving maternal-foetal attachment and maternal sensitivity. Results also suggested that a group-based intervention, targeting depressive symptoms, delivered during pregnancy may have enduring effects on maternal sensitivity.
Ponteri [98] conducted a mixed-method study to investigate the effectiveness of group art therapy for depressed mothers and their children. Four mother-child pairs attended 8 weeks of 90-min group art therapy sessions. A video of 20 min of a play session was recorded to assess mother–child interaction. The findings revealed that mothers who participated in the group art therapy reported higher levels of self-esteem and a more positive self-image following treatment. Participants mentioned in their post-interview that the group art therapy helped them to recognize their strengths as a person. Group art therapy with mothers and their babies provided a safe, therapeutic forum for women to explore issues such as self-esteem, competency, and a new identity as a mother and fostered a positive social and learning environment for the child. Thus, art therapy showed the potential for dual benefits: improving mother’s self-image and decreasing of depressive symptoms and improving the quality of interactions between her and her baby.
Many mothers engage in community group activities with their babies, as they are found to be effective at relaxing mothers, providing good sources of social interaction, decreasing the monotony of each day, and a sense of personal fulfilment for mothers [99]. Specifically, there is a growing body of evidence demonstrating the effects of community group singing on both maternal and children’s mental health [83, 100]. Research has demonstrated valuable benefits of singing to new-borns, such as improving mother-infant interaction and reducing infant distress [101, 102]. Listening to music during pregnancy is also associated with greater maternal wellbeing and reduced depressive symptoms in the first 3 months post-birth, while daily singing to babies is associated with fewer symptoms of depression and increased maternal wellbeing, self-esteem, and perceived mother-infant bond [103]. A study conducted in 2018 showed that new mothers involved in 10-week programme of singing group had a significantly faster decrease in their depressive symptoms compared with mothers that participated to play groups [104]. Overall, the study suggested that a programme of group singing workshops could help speed the recovery from symptoms of PND among new mothers. Based on these results with a group of 134 women, a new randomized clinical trial (SHAPER-PNDFootnote 1) aims to establish effectiveness of a 10-week singing intervention in a larger sample of 400 participants [105]. Mothers and their babies will be assigned to either a 10-week singing intervention or a 10-week active waiting-list control group, where they will be encouraged to attend community mother-baby activities. Early remission from PND has been associated with reduced effects on both mother and baby [106]. Thus, evidence that singing interventions can speed the rate of recovery in women affected by symptoms of PND could have clinical relevance.
4 Conclusion
It is well known that perinatal depression not only has implications for maternal mental health and wellbeing but also for decreased quality of interactions between mothers and their children, which has long been linked to negative developmental outcomes including offspring mental health. A systematic review from 2017 aimed to examine which among AND and PND treatment interventions are most efficacious in improving parenting and/or child development and underlined that, although promising findings exist for interpersonal psychotherapy, cognitive behavioural therapy, maternal child interaction guidance, and other interventions including massage and psychotherapeutic group support, it is difficult to draw any definitive conclusions regarding any one treatment that shows the most potential to influence maternal and infant outcomes [79]. Currently, there is not sufficient evidence available to make practice recommendations for a universal intervention, and further research in this area is recommended. On another note, given the evidence that perinatal depression impacts a mother’s ability to properly interact with her baby, and treating maternal mood alone is not sufficient for improving mother-infant relationship difficulties, there is growing evidence demonstrating interventions that focus on addressing mother-infant interaction appear to be benefit to both mothers and their children.
Notes
- 1.
Scaling-up Health-Arts Programmes: the largest study in the world bringing arts-based mental health interventions into a national health service.
References
Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Part 1):1071–83.
Campbell SB, Cohn JF. The timing and chronicity of postpartum depression: implications for infant development. In: Murray L, Cooper PJ, editors. Postpartum depression and child development. Guilford Press; 1997. p. 165–97.
Muñoz RF, Le H-N, Ippen CG, Diaz MA, Urizar GG Jr, Soto J, Mendelson T, Delucchi K, Lieberman AF. Prevention of postpartum depression in low-income women: development of the Mamás y Bebés/mothers and babies course. Cogn Behav Pract. 2007;14(1):70–83.
Murray L, Cooper P. Intergenerational transmission of affective and cognitive processes associated with depression: infancy and the preschool years. In: Goodyer IM, editor. Unipolar depression: a lifespan perspective. Oxford University Press; 2003.
Robinson AM, Benzies KM, Cairns SL, Fung T, Tough SC. Who is distressed? A comparison of psychosocial stress in pregnancy across seven ethnicities. BMC Pregnancy Childbirth. 2016;16(1):1–11.
Cooper PJ, Murray L. Course and recurrence of postnatal depression: evidence for the specificity of the diagnostic concept. Br J Psychiatry. 1995;166(2):191–5.
Howard LM, Molyneaux E, Dennis C-L, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384(9956):1775–88.
Norhayati MN, Hazlina NHN, Asrenee AR, Emilin WMAW. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. 2015;175:34–52.
Verreault N, Da Costa D, Marchand A, Ireland K, Dritsa M, Khalifé S. Rates and risk factors associated with depressive symptoms during pregnancy and with postpartum onset. J Psychosom Obstet Gynecol. 2014;35(3):84–91.
Murray L, Fearon P, Cooper P. Postnatal depression, mother-infant interactions, and child development: prospects for screening and treatment. In: Identifying perinatal depression and anxiety: evidence-based practice in screening, psychosocial assessment, and management. Wiley-Blackwell; 2015. p. 139–64.
Sichel D. Postpartum psychiatric disorders. In: Dunitz M, editor. Mood disorders in women; 2000. p. 313–28.
Stein A, Gath DH, Bucher J, Bond A, Day A, Cooper PJ. The relationship between post-natal depression and mother–child interaction. Br J Psychiatry. 1991;158(1):46–52.
Murray L, Stein A. 13 The effects of postnatal depression on the infant. Baillieres Clin Obstet Gynaecol. 1989;3(4):921–33.
Marmorstein NR, Malone SM, Iacono WG. Psychiatric disorders among offspring of depressed mothers: associations with paternal psychopathology. Am J Psychiatr. 2004;161(9):1588–94.
Cataudella S, Lampis J, Busonera A, Marino L, Zavattini GC (2016) From parental-fetal attachment to a parent-infant relationship: a systematic review about prenatal protective and risk factors.
Hazell Raine K, Nath S, Howard LM, Cockshaw W, Boyce P, Sawyer E, Thorpe K. Associations between prenatal maternal mental health indices and mother–infant relationship quality 6 to 18 months’ postpartum: a systematic review. Infant Ment Health J. 2020;41(1):24–39.
Smorti M, Ponti L, Tani F. Maternal depressive symptomatology during pregnancy is a risk factor affecting newborn’s health: a longitudinal study. J Reprod Infant Psychol. 2019;37(4):444–52.
Goodman JH. Perinatal depression and infant mental health. Arch Psychiatr Nurs. 2019;33(3):217–24.
Waters CS, Hay DF, Simmonds JR, van Goozen SHM. Antenatal depression and children’s developmental outcomes: potential mechanisms and treatment options. Eur Child Adolesc Psychiatry. 2014;23(10):957–71.
Taka-Eilola T, Veijola J, Murray GK, Koskela J, Mäki P. Severe mood disorders and schizophrenia in the adult offspring of antenatally depressed mothers in the Northern Finland 1966 Birth Cohort: relationship to parental severe mental disorder. J Affect Disord. 2019;249:63–72.
Field T. Maternal depression effects on infants and early interventions. Prev Med. 1998;27(2):200–3.
Field T, Healy BT, Goldstein S, Guthertz M. Behavior-state matching and synchrony in mother-infant interactions of nondepressed versus depressed dyads. Dev Psychol. 1990;26(1):7.
Jones NA, Field T, Hart S, Lundy B, Davalos M. Maternal self-perceptions and reactions to infant crying among intrusive and withdrawn depressed mothers. Infant Mental Health J. 2001;22(5):576–86.
Murray L, Fiori-Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev. 1996;67(5):2512–26.
Campbell SB, Brownell CA, Hungerford A, Spieker SJ, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Dev Psychopathol. 2004;16(2):231–52.
DeKlyen M, Greenberg MT. Attachment and psychopathology in childhood. In: Handbook of attachment: theory, research, and clinical applications. The Guilford Press; 2008. p. 637–65.
Forman DR, O’hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother–child relationship. Dev Psychopathol. 2007;19(2):585–602.
Klier CM. Mother–infant bonding disorders in patients with postnatal depression: the postpartum bonding questionnaire in clinical practice. Arch Womens Ment Health. 2006;9(5):289–91.
Pawlby S, Fernyhough C, Meins E, Pariante CM, Seneviratne G, Bentall RP. Mind-mindedness and maternal responsiveness in infant–mother interactions in mothers with severe mental illness. Psychol Med. 2010;40(11):1861–9.
Murray L. Effects of postnatal depression on infant development: direct studies of early mother-infant interactions. In: Kumar R, Brockington I, editors. Motherhood and mental illness, vol. 2. Butterworths; 1988. p. 159–90.
Bowlby J. Attachment and loss: retrospect and prospect. Am J Orthopsychiatry. 1982;52(4):664.
Waters E, Cummings EM. A secure base from which to explore close relationships. Child Dev. 2000;71(1):164–72.
Benoit D. Infant-parent attachment: definition, types, antecedents, measurement and outcome. Paediatr Child Health. 2004;9(8):541–5.
Rutter M, Quinton D. Parental psychiatric disorder: effects on children. Psychol Med. 1984;14(4):853–80.
Lyons-Ruth K, Zoll D, Connell D, Grunebaum HU. The depressed mother and her one-year-old infant: environment, interaction, attachment, and infant development. In: Tronick EZ, editor. Maternal depression and infant disturbance. New directions for child development: Jossey-Bass; 1986.
Murray L. The impact of postnatal depression on infant development. Child Psychol Psychiatry Allied Discipl. 1992;
Teti DM, Gelfand DM, Messinger DS, Isabella R. Maternal depression and the quality of early attachment: an examination of infants, preschoolers, and their mothers. Dev Psychol. 1995;31(3):364.
Ainsworth MD, Wittig BA. Attachment and exploratory behaviour in one-year-olds in a strange situation. In: Floss BM, editor. Determinants of infant behaviour. London: Methuen; 1969.
Radke-Yarrow M, Cummings EM, Kuczynski L, Chapman M. Patterns of attachment in two-and three-year-olds in normal families and families with parental depression. Child Dev. 1985:884–93.
Fonagy P, Gergely G, Jurist EL. Affect regulation, mentalization and the development of the self. Routledge; 2018.
Fonagy P. Mentalizing in practice. In: Allen JG, Fonagy P, editors. Handbook of mentalization-based treatment. John Wiley & Sons; 2006. p. 3–30.
Fischer-Kern M, Tmej A. Mentalization and depression: theoretical concepts, treatment approaches and empirical studies—an overview. Z Psychosom Med Psychother. 2019;65(2):162–77.
Bateman AW, Fonagy PE. Mentalizing and borderline personality disorder. In: Allen G, Fonagy P, editors. Handbook of mentalizing in mental health practice. John Wiley & Sons; 2006. p. 185–200.
Sharp C, Fonagy P, Goodyer IM. Imagining your child’s mind: psychosocial adjustment and mothers’ ability to predict their children’s attributional response styles. Br J Dev Psychol. 2006;24(1):197–214.
Slade A. Parental reflective functioning: an introduction. Attach Hum Dev. 2005;7(3):269–81.
Sharp C, Fonagy P. The parent’s capacity to treat the child as a psychological agent: Constructs, measures and implications for developmental psychopathology. Soc Dev. 2008;17(3):737–54.
Bateman A, Fonagy P. Mentalizing in mental health practice. In: Bateman P, Fonagy A, editors. Handbook of mentalizing in mental health practice. Arlington, VA: American Psychiatric Publishing Inc.; 2012. p. 3–42.
Murray L, Kempton C, Woolgar M, Hooper R. Depressed mothers’ speech to their infants and its relation to infant gender and cognitive development. J Child Psychol Psychiatry. 1993;34(7):1083–101.
Herrera E, Reissland N, Shepherd J. Maternal touch and maternal child-directed speech: effects of depressed mood in the postnatal period. J Affect Disord. 2004;81(1):29–39.
Vliegen N, Casalin S, Luyten P. The course of postpartum depression: a review of longitudinal studies. Harv Rev Psychiatry. 2014;22(1):1–22.
Sethna V, Murray L, Ramchandani PG. Depressed fathers’ speech to their 3-month-old infants: a study of cognitive and mentalizing features in paternal speech. Psychol Med. 2012;42(11):2361–71.
Levy DW, Truman S. Reflective functioning as mediator between drug use, parenting stress and child behavior. College on Problems of Drug Dependence Annual Meeting, Quebec, 2002.
De Wolff MS, Van Ijzendoorn MH. Sensitivity and attachment: a meta-analysis on parental antecedents of infant attachment. Child Dev. 1997;68(4):571–91.
Shin H, Park Y, Ryu H, Seomun G. Maternal sensitivity: a concept analysis. J Adv Nurs. 2008;64(3):304–14.
Crittenden PM, Bonvillian JD. The relationship between maternal risk status and maternal sensitivity. Am J Orthopsychiatry. 1984;54(2):250.
Drake EE, Humenick SS, Amankwaa L, Younger J, Roux G. Predictors of maternal responsiveness. J Nurs Scholarsh. 2007;39(2):119–25.
Meins E, Fernyhough C, Fradley E, Tuckey M. Rethinking maternal sensitivity: mothers’ comments on infants’ mental processes predict security of attachment at 12 months. J Child Psychol Psychiatry. 2001;42(5):637–48.
Bind RH, Biaggi A, Bairead A, Du Preez A, Hazelgrove K, Waites F, Conroy S, Dazzan P, Osborne S, Pawlby S, Sethna V, Pariante C. Mother-infant interaction in women depressed in pregnancy and in women with a history of depression in the Psychiatry Research and Motherhood – Depression (PRAM-D) study. BJPsych Open; 2021. In Press
Lefkovics E, Baji I, Rigó J. Impact of maternal depression on pregnancies and on early attachment. Infant Ment Health J. 2014;35(4):354–65.
Parsons CE, Young KS, Rochat TJ, Kringelbach ML, Stein A. Postnatal depression and its effects on child development: a review of evidence from low-and middle-income countries. Br Med Bull. 2012;101(1):57–79.
Girgus JS, Nolen-Hoeksema S. Cognition and depression. In: Keys CLM, Goodman SH, editors. Women and depression: a handbook for the social, behavioral, and biomedical sciences. Cambridge University Press; 2006.
Cicchetti D. Developmental psychology. In: Lamb RMME, Freund AM, Lerner M, editors. The handbook of life-span development, Social and emotional development, vol. 2. Hoboken, NJ: John Wiley & Sons Inc.; 2010. p. 511–89.
Dix T, Moed A, Anderson ER. Mothers’ depressive symptoms predict both increased and reduced negative reactivity: aversion sensitivity and the regulation of emotion. Psychol Sci. 2014;25(7):1353–61.
Giallo R, Cooklin A, Wade C, D’Esposito F, Nicholson JM. Maternal postnatal mental health and later emotional–behavioural development of children: the mediating role of parenting behaviour. Child Care Health Dev. 2014;40(3):327–36.
Jensen SKG, Dumontheil I, Barker ED. Developmental inter-relations between early maternal depression, contextual risks, and interpersonal stress, and their effect on later child cognitive functioning. Depress Anxiety. 2014;31(7):599–607.
Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, O’Connor TG, Stein A. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. 2013;70(12):1312–9.
Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36(1):60–9.
Pennebaker JW, Susman JR. Disclosure of traumas and psychosomatic processes. Soc Sci Med. 1988;26(3):327–32.
Rebecchini, L. (2019). Using expressive writing to cope with childbirth. https://www.inspirethemind.org/blog/2019/06/26/using-expressive-writing-to-cope-with-the-childbirth?rq=lavinia.
Kopelman RC, Moel J, Mertens C, Stuart S, Arndt S, O’Hara MW. Barriers to care for antenatal depression. Psychiatr Serv. 2008;59(4):429–32.
Tronick E, Reck C. Infants of depressed mothers. Harv Rev Psychiatry. 2009;17(2):147–56.
Tronick EZ, Weinberg MK. Depressed mothers and infants: failure to form dyadic states of consciousness. In: Murray CP, editor. Postpartum depression and child development. Guilford Press; 1997. p. 54–81.
Murray L, Cooper PJ. Postpartum depression and child development. Psychol Med. 1997;27(2):253–60.
Milgrom J, McCloud P. Parenting stress and postnatal depression. Stress Med. 1996;12(3):177–86.
Kopelman R, Stuart S. Psychological treatments for postpartum depression. NJ: SLACK Incorporated Thorofare; 2005.
DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, O’Reardon JP, Lovett ML, Gladis MM, Brown LL. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):409–16.
Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short-and long-term effect of psychological treatment of post-partum depression: I. Impact on maternal mood. Br J Psychiatry. 2003;182(5):412–9.
Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. 2010;33(1):1–6.
Letourneau NL, Dennis C, Cosic N, Linder J. The effect of perinatal depression treatment for mothers on parenting and child development: a systematic review. Depress Anxiety. 2017;34(10):928–66.
Muzik M, Marcus SM, Flynn HA. Psychotherapeutic treatment options for perinatal depression: emphasis on maternal-infant dyadic outcomes. J Clin Psychiatry. 2009;70(9):1318–9.
Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, Brown M. Watch, wait, and wonder: testing the effectiveness of a new approach to mother–infant psychotherapy. Infant Mental Health J. 1999;20(4):429–51.
Fraiberg S, Adelson E, S. V. A psychoanalytic approach to the problems of impaired infant-mother relationships. In: Fraiberg L, editor. Selected writings of Selma Fraiberg. Ohio State University Press; 1987. p. 100–36.
Nylen KJ, Moran TE, Franklin CL, O’hara, M. W. Maternal depression: a review of relevant treatment approaches for mothers and infants. Infant Ment Health J. 2006;27(4):327–43.
Poobalan AS, Aucott LS, Ross L, Smith WCS, Helms PJ, Williams JHG. Effects of treating postnatal depression on mother-infant interaction and child development: systematic review. Br J Psychiatry. 2007;191(5):378–86.
Guild DJ, Alto ME, Handley ED, Rogosch F, Cicchetti D, Toth SL. Attachment and affect between mothers with depression and their children: longitudinal outcomes of child parent psychotherapy. Res Child Adolesc Psychopathol. 2021:1–15.
Cicchetti D, Rogosch FA, Toth SL. The efficacy of toddler-parent psychotherapy for fostering cognitive development in offspring of depressed mothers. J Abnorm Child Psychol. 2000;28(2):135–48.
Toth SL, Rogosch FA, Manly JT, Cicchetti D. The efficacy of toddler-parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: a randomized preventive trial. J Consult Clin Psychol. 2006;74(6):1006.
Goodman JH, Prager J, Goldstein R, Freeman M. Perinatal dyadic psychotherapy for postpartum depression: a randomized controlled pilot trial. Arch Womens Ment Health. 2015;18(3):493–506.
Rusconi-Serpa S, Rossignol AS, McDonough SC. Video feedback in parent-infant treatments. Child Adolesc Psychiatric Clin. 2009;18(3):735–51.
Fonagy P. Affect regulation, mentalization, and the development of the self, vol. 2002. New York (Other Press); 2002.
Beebe B. Brief mother–infant treatment: psychoanalytically informed video feedback. Infant Mental Health J. 2003;24(1):24–52.
Beebe B. My journey in infant research and psychoanalysis: microanalysis, a social microscope. Psychoanal Psychol. 2014;31(1):4.
Beebe B. Mother–infant research informs mother–infant treatment. Clin Soc Work J. 2010;38(1):17–36.
Vik K, Braten S. Video interaction guidance inviting transcendence of postpartum depressed mothers’ self-centered state and holding behavior. Infant Ment Health J. 2009;30(3):287–300.
Olhaberry M, León MJ, Seguel M, Mena C. Video-feedback intervention in mother-baby dyads with depressive symptomatology and relationship difficulties. Res Psychother: Psychopathol Process Outcome. 2015;
Tryphonopoulos PD, Letourneau N. Promising results from a video-feedback interaction guidance intervention for improving maternal–infant interaction quality of depressed mothers: a feasibility pilot study. Can J Nurs Res. 2020;52(2):74–87.
Gidron Y. Group therapy/intervention. In: Gellman MD, Turner JR, editors. Encyclopedia of behavioral medicine. Springer; 2013.
Ponteri AK. The effect of group art therapy on depressed mothers and their children. Art Ther. 2001;18(3):148–57.
Gelfand DM, Teti DM, Seiner SA, Jameson PB. Helping mothers fight depression: evaluation of a home-based intervention program for depressed mothers and their infants. J Clin Child Psychol. 1996;25(4):406–22.
Clift S, Morrison I. Group singing fosters mental health and wellbeing: findings from the East Kent “singing for health” network project. Ment Health Soc Incl. 2011;
Coulton S, Clift S, Skingley A, Rodriguez J. Effectiveness and cost-effectiveness of community singing on mental health-related quality of life of older people: randomised controlled trial. Br J Psychiatry. 2015;207(3):250–5.
Nakata T, Trehub SE. Infants’ responsiveness to maternal speech and singing. Infant Behav Dev. 2004;27(4):455–64.
Vlismas W, Malloch S, Burnham D. The effects of music and movement on mother–infant interactions. Early Child Dev Care. 2013;183(11):1669–88.
Fancourt D, Perkins R. Effect of singing interventions on symptoms of postnatal depression: three-arm randomised controlled trial. Br J Psychiatry. 2018;212(2):119–21.
Estevao C, Fancourt D, Dazzan P, Chaudhuri KR, Sevdalis N, Woods A, Crane N, Bind R, Sawyer K, Rebecchini L, Hazelgrove K, Manoharan M, Burton A, Dye H, Osborn T, Jarrett L, Ward N, Jones F, Podlewska A, et al. Scaling-up Health-Arts Programmes: the largest study in the world bringing arts-based mental health interventions into a national health service. BJ Psych Bull. 2021;45(1):32–9. https://doi.org/10.1192/bjb.2020.122.
Harris B, Huckle P, Thomas R, Johns S, Fung H. The use of rating scales to identify post-natal depression. Br J Psychiatry. 1989;154(6):813–7.
Acknowledgements
Dr. Rebecchini is supported by a kind gift from Michael Samuel through King’s College London and King’s Health Partners; Dr. Bind and Professor Pariante are supported by the UK National Institute for Health Research (NIHR) through a Senior Investigator Award and the Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King’s College London.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rebecchini, L., Bind, R.H., Pariante, C. (2022). Perinatal Depression and Mother-Infant Interventions: A Literature Review. In: Percudani, M., Bramante, A., Brenna, V., Pariante, C. (eds) Key Topics in Perinatal Mental Health. Springer, Cham. https://doi.org/10.1007/978-3-030-91832-3_24
Download citation
DOI: https://doi.org/10.1007/978-3-030-91832-3_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-91831-6
Online ISBN: 978-3-030-91832-3
eBook Packages: MedicineMedicine (R0)