Abstract
The human skeleton undergoes constant remodeling throughout the lifetime. Bone remodeling, the fundamental process for bone renewal, is targeted by treatments of osteoporosis to correct the imbalance between bone resorption and bone formation and reduce the risk of fractures with its associated clinical consequences. Currently available osteoporosis therapies affect bone resorption and bone formation in the same direction and either decrease (inhibitors of bone resorption) or increase (parathyroid hormone [PTH] peptides) bone remodeling. However, stopping bone resorption alone approach cannot replace already lost bone, which is required for better fracture protection in women with severe disease. This raised the hypothesis that for optimal therapeutic outcome, bone formation and bone resorption should be modulated in different directions. This chapter will discuss the concept of dynamic skeleton, coupling of bone remodeling, as well as principles of bone modulation. It will then discuss implications from research studies and clinical practice on bone modulation, as well as new aspects of the bone-protecting effects of vitamin D. It will conclude by elaborating some nontraditional molecules with anti-osteoporotic potential.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bone remodeling
- Osteoclasts
- Osteoblasts
- Osteocytes
- Bone formation
- Bone resorption
- Wnt signaling
- Calcium-sensing receptor
- RANK ligand
Introduction
In spite of its inert appearance, the bone is an extremely dynamic tissue that is continuously being remodeled to adapt to changing mechanical demands. Such remodeling, which is carried out on a microscopic scale, consists in the removal of low-performing bone and its replacement by new, fully functional bone. The first symptom and considered the major characteristic of osteoporosis is a decrease in the bone mass and quality [1], rendering people prone to sustaining osteoporotic fracture (fragility fracture) caused by low-energy trauma [2]. Osteoporosis is more prevalent in older adults, with nearly 200 million patients are diagnosed to have osteoporosis annually, and an estimated nine million new osteoporotic fractures occur in a given year [3,4,5]. Surgery is the primary treatment approach for osteoporotic fractures; however, poor prognoses have been reported and attributed to a combination of biological and surgical factors [6]. Fractured osteoporotic bones are usually compromised and comminuted, which makes it hard to achieve an optimum reduction and stable fixation [5, 7]. Osteoporotic fractures mostly occur in elderly patients, who usually live with other comorbidities or unfavorable systemic conditions and most likely take medications that make them prone to complications [8]. Furthermore, the abnormal remodeling status of the bone with osteoporosis would deteriorate after getting bed bound while admitted to the hospital and very limited mobility after discharge, which poses a disadvantage with respect to fracture healing and bone callus strength; consequently, the refracture risk following surgery increases significantly [9]. Therefore, it is not surprising, bearing in mind the complexity of treatment, length of hospital admission, and poor prognosis, that the annual facility-related hospital cost of osteoporotic fractures is the highest (up to $5.1 billion), followed by that of myocardial infarction and stroke [10].
In the course of the past three decades, several drugs have been developed that can prevent fractures; however, although the effect of these treatments on vertebral fractures is impressive, the effect on non-vertebral fractures is less than satisfactory [11, 12]. Moreover, significant reduction of vertebral fractures occurs early in the course of therapy, typically within 6 months, whereas reduction of non-vertebral fractures and hip fractures specifically has not been observed before at least 1 year of therapy [13]. Furthermore, although the results of the clinical studies remain controversial, the majority have reported decrease in the callus area (20–40%) and bone mineral density (BMD) at the fracture sites in elderly osteoporotic patients. Studies have indicated that the delayed or nonunion of osteoporotic fractures is implicated in the scarce capacity of bone regeneration with aging [14, 15]. Additionally, the bone properties of such patients are quite different from those of normal individuals and are manifested in the decrease of bone mechanics and mechanosensation, as well as the abnormal bone metabolism caused by immune disorders [16].
Pharmacological interventions aim to decrease this risk and the associated clinical consequences by correcting the imbalance between bone resorption and bone formation that constitutes the pathophysiological basis of the disease. Most currently available agents inhibit bone resorption and formation to varying degrees and decrease the risk of fractures but cannot replace already lost bone, and they only modestly decrease the risk of non-vertebral fractures, the most frequent osteoporotic fractures. Parathyroid hormone (PTH) peptides, the only approved bone-forming agents, stimulate bone formation but also bone resorption and have not been shown to reduce the risk of hip fractures, the most devastating clinical consequence of osteoporosis. These unmet needs have led to efforts for the development of new therapeutics for osteoporosis based on improved knowledge of the local regulation of bone remodeling arising mainly from the study of rare bone diseases and genetically modified animal models [17]. This chapter will discuss the concept of dynamic skeleton, coupling of bone remodeling, as well as principles of bone modulation. It will then discuss implications from research studies and clinical practice on bone modulation, as well as new aspects of the bone-protecting effects of vitamin D. It will conclude by elaborating some nontraditional molecules with anti-osteoporotic potential.
The Dynamic Skeleton
The unique character of the bone tissue is attributed to its mix of elasticity and strength that permits deformation under a certain level of loading stress before failing [18]. The strength of bone depends mainly on both the density and distribution of the inorganic matrix mineralization [19]. Cortical bone, which consists of dense and well-organized lamellae, has higher strength but a lower capacity to withstand a load that exceeds the elastic deformation range compared to that of trabecular bone, which is composed of unparallel lamellar units with variable porosity (50–90%) [20]. The mechanical competence of trabecular bone is based largely on the BMD, while the stiffness of cortical bone is highly dependent on its porosity [5, 21]. In contrast to calcified matrix mineralization, the organic matrix (e.g., collagen and non-collagenous proteins) is considered the main factor responsible for controlling bone ductility and its capacity to withstand an impact without cracking [22]. A large proportion (90%) of the organic matrix is composed of type I collagen, which undergoes numerous posttranslational modifications [23]. Among them, enzymatic modifications positively affect the biomechanical stability of the bone, while nonenzymatic cross-linking is associated with a deterioration in these properties [22]. Non-collagenous proteins, including osteopontin (OPN) and osteocalcin (OCN), account for 10% of the organic matrix and limit crack energy through the control of hydroxyapatite size and orientation [24]. Whereas bone material properties provide only a static snapshot of bone quality, the abilities of self-regeneration and remodeling provide a dynamic profile of bone health [25].
As the bones are not completely developed at birth, they continue to be formed slowly out of cartilage or connective tissue, which are converted into the hard, lamellar components of the bone. Growth of the bones (modeling) comes to an end at puberty with ossification of the “growth plates.” Modeling is of particular interest as the bone is much more capable of reacting to external loads during growth than at any other time. About 90% of adult bone is formed by the end of adolescence, and subsequent gains during adulthood are very small. Later, in the adult life, the adult skeleton is renewed by remodeling. Bone remodeling is a process where osteoclasts and osteoblasts work sequentially in the same bone remodeling unit. The basics of both bone modeling and remodeling will be reviewed in the coming section.
Bone Modeling
Bones, mostly, are composed of an outer shell of protective and supportive cortical (compact) bone, inside of which is a network of trabeculae (plates) that comprise the cancellous, or spongy, part of the bone. Bones are formed during embryonic development by the process of endochondral ossification, in which they are first modeled in a mold or anlagen of cartilage [26]. Blood vessels invade the cartilage, which is resorbed by chondroclasts, to form a medullary cavity. The precise origin of these chondroclasts is still uncertain, but they may be in the hematopoietic cell lineage. They are not required to be osteoclasts because endochondral ossification is normal or only slightly impaired in mammals that do not form osteoclasts. The cartilage is replaced by cortical bone formed by periosteal apposition and by trabecular bone, which is laid down within the medullary space at the epiphyseal growth plate. Hematopoietic, stromal, and adipocytic bone marrow cells fill the remaining space within the bones. A network of endothelium-lined sinusoids and feeding blood vessels nutritionally supports these cells and the trabecular bone. Up to approximately 30% of the volume of the space inside the bones of the axial skeleton is composed of trabecular bone, which contributes significantly to the supportive role of bones in the maintenance of normal posture. In contrast, trabecular bone is confined largely to the ends of most long bones, their diaphyseal cavities filled mostly with fatty marrow in adult humans [27].
Bone Remodeling
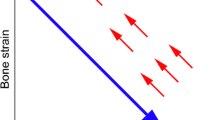
Following bone modeling (growth), the integrity of bones is maintained by the process of bone remodeling, in which worn-out sections of bones are removed by osteoclasts and replaced with new bone laid down by osteoblasts (Fig. 17.1). Osteoclasts are multinucleated cells derived from mononuclear precursors in the mononuclear-phagocyte lineage that fuse with one another by cytoplasmic, but not nuclear, fusion [29]. Their formation and activity are regulated predominantly by osteoblasts and stromal cells. The stromal cells are derived from precursors in the mesenchymal cell lineage that also gives rise to chondroblasts, adipocytes, fibroblasts, and muscle cells.
A sketch of BMU operation after a group of osteocytes has undergone apoptosis near bone surface. Bone resorption (red arrows) and bone formation (blue arrows) are performed in this order. Bone remodeling is initiated when osteoclast precursor cells are recruited to the altered bone surface (black stellate cells) and fuse to form mature, bone-resorbing osteoclasts (red cells) that attach to the surface. Mature osteoclasts degrade the mineralized matrix (light yellow) and produce resorption pits also called resorption bays or Howship’s lacunae. Once osteoclasts have degraded the target area, they undergo apoptosis, and osteoblasts (dark blue cells) situated behind them first secrete osteoid matrix (dark yellow) and subsequently differentiate into mature osteocytes (light blue stellate cells). (Quoted from: Arias et al. [28] under open access scheme)
Osteoclasts remove packets (trenches) of the bone (approximately 60 μm deep) from the surfaces of bone trabeculae at remodeling sites, and osteoblasts fill in these defects by laying down and mineralizing the new bone in a process similar to that used to replace sections of damaged roadways. Thus, osteoclasts typically do not resorb through the full thickness of trabecular elements during normal bone resorption and, consequently, leave a base of bone matrix to which osteoblasts are attracted and upon which they can lay down new bone matrix. The resorption phase lasts up to approximately 30–40 days; the formation phase takes about 120–170 days [30]. Recent studies have indicated that bone-lining cells in the osteoblast/stromal cell lineage clean up the resorbed surfaces and prepare them for new matrix deposition by removing projecting collagen fibers and laying down a thin layer of matrix to form the cement line that can be seen marking sites of resorption. The collagen fibers are degraded by matrix metalloproteinases secreted by these bone-lining cells, which do not appear to differentiate into the osteoblasts that subsequently fill in the resorption cavity [27].
Coupling of Bone Remodeling
Bone remodeling occurs in an orderly fashion by the basic multicellular units (BMUs) and temporary anatomical structures comprising a team of osteoclasts in the front and a team of osteoblasts in the back, supported by blood vessels, nerves, and connective tissue. Osteoclasts resorb the bone by removing bone mineral and degrading the organic matrix, while osteoblasts move to the resorbed area and lay down new bone matrix that subsequently mineralizes, a process known as coupling. The mechanisms regulating this coupling are not entirely clear, but it is thought that growth factors mobilized from the bone matrix during resorption might contribute to intercellular signaling and subsequent stimulation of bone formation (Fig. 17.2). Alternatively, or in addition, the osteoclasts produce factors that might contribute to generation and differentiation of osteoblast precursors [32, 33]. It is now generally accepted that osteocytes are the main regulators of bone remodeling due to their location in the bone allowing them to sense mechanical signals and to respond to chemical signals regulating bone and mineral metabolism by secreting factors that can modulate the number and function of osteoblasts and osteoclasts [34].
Schematic representations of the normal coupling process of bone resorption and formation during the remodeling process. (a) RANKL promotes differentiation and activation of osteoclasts at remodeling sites. Coupling factors derived from the resorbed bone matrix or directly from the activated osteoclasts stimulate the recruitment and maturation of osteoblasts to initiate bone formation on the existing resorption surface. (b) Denosumab blocks osteoclastogenesis, and bisphosphonate induces the loss of ruffled border and eventual osteoclast apoptosis. These therapies lead to little-to-no resorption surface and fewer numbers of osteoclasts on bone. (c) Treatment with a cathepsin K (CatK) inhibitor reduces osteoclastic resorption efficiency and retards transcytotic trafficking of matrix removal. This does not prevent other osteoclast functions, such as the generation of a shallow resorption surface and the release of osteogenic factors; together, these functions initiate osteoblast bone formation (BP bisphosphonate, CatKi cathepsin K inhibitor, Ob osteoblast, OC osteoclast, pOb osteoblast progenitor, pOC osteoclast progenitor, RANK receptor activator of nuclear factor kappa-B, RANKL RANK ligand. (Reproduced with permission from (le Duong [31]). Still awaiting the permission (email resent on first of August 2020))
An increased number and life span of osteoclasts and a decrease in the formation and life span of osteoblasts induce an imbalance between bone resorption and bone formation, the cellular basis of osteoporosis. This imbalance, in favor of resorption, results in bone loss and deterioration of bone architecture. The decline in the ability of osteoblasts to refill the resorption cavity leads to reduction of the thickness of the bone packets and thinning of the trabeculae. In addition, the enhanced osteoclastic resorption per unit time that occurs at the menopause results in perforation and removal of trabeculae and loss of their connectivity [35]. Cortical bone becomes wider in diameter and thinner, due to the move of the endosteal surface outward at a greater pace than the bone placed in the periosteum but also more porotic due to enhanced intracortical remodeling [36].
Principles of Bone Modulation
Bone construction is achieved mainly by bone modeling, which lead to a change in both the external as well as the internal shape and dimensions of the bone. Commonly, bone modeling is considered as being formative; however, in fact, it can be either formative or resorptive. Formative bone modeling takes place on the periosteal surface and usually occur during growth. Formative bone modeling is carried out by osteoblasts, which are able to synthesize and deposit a volume of bone upon a bone surface that has not undergone prior bone resorption [36, 37]. On the other hand, resorptive bone modeling takes place on the endocortical surface which consequently excavates the medullary canal of long bones during growth and is not followed by bone formation. Resorptive modeling occurs also on the periosteal surface during growth to enable integration of the metaphysis with the diaphysis of long bones [37]. The resorptive bone modeling is carried out by osteoclasts, which are able to resorb a volume of the bone upon a bone surface. Modeling helps to give the bone its strength for loading, resistance to deformation, and lightness of weight to facilitate mobility [36].
On another front, renewal or reconstruction of the bone is achieved by bone remodeling. Bone remodeling is carried out by bone multicellular units, which is composed of teams of osteoclasts and osteoblasts which resorb, respectively, a volume of older or damaged bone and then replace it with a newly synthesized bone [37]. Remodeling is a bone surface-dependent process. Primarily this includes the intracortical surface of the Haversian canals, the endocortical surface of the medullary canal, and the opposing trabeculae surfaces [36].
Remodeling balance is always achievable during young adulthood when nearly equal volumes of the bone are removed then replaced upon these three components of the endosteal surface so that no permanent bone loss or microstructural deterioration occurs (Fig. 17.3) [38].
(a) Reversible deficit in bone volume: at any time BMUs at different sites are at different stages of their remodeling cycle. Deficit is the result of cavities which are completely refilled with osteoid but still incompletely mineralized. So the reversible deficit is a deficit of mineral not matrix. (b) Age-related (early menopause): rapid increase in the rate of bone remodeling. The reduction in the volume of the bone resorbed by each BMU but even greater reduction in the volume of bone deposited at the same location resulting in BMU imbalance and morphological basis of irreversible bone loss. (c) Postmenopause: Rapid remodeling continues, but BMD declines more slowly than during early menopause. This is explained by the finding that bone loss is driven mainly by the speed of remodeling and the degree of the negative BMU balance, not by the greater difference in the number of cavities being excavated and not concurrently being incompletely refilled as occurs during early menopause
The net outcome of the imbalance between bone resorption and formation, which occurs at the menopause, is increased bone fragility. This provides the rationale for the development of pharmacological agents for the management of osteoporosis. It is clear from the described changes that reduction of bone resorption must be an essential component of any therapeutic approach for the maintenance or improvement of bone strength. However, this approach cannot replace already lost bone, which is required for better fracture protection in women with severe disease. For this, specific stimulation of bone formation is essential. Thus, in theory, optimal pharmacological management of osteoporosis should aim at decreasing bone resorption (endosteal and intracortical) and stimulating bone formation at all skeletal envelopes, including the periosteum. Such approach will not only prevent the structural decay of bone tissue but will also increase bone mass and may lead to improved reduction of the risk of non-vertebral fractures, which occur predominantly at cortical bone sites [39].
Concurrent treatment of women with osteoporosis with teriparatide and the inhibitor of bone resorption, denosumab, increased BMD at all skeletal sites considerably more than either monotherapy alone after 2 years [39, 40]. The difference in response between teriparatide and teriparatide/denosumab treatment is probably due to inhibition of teriparatide-stimulated RANKL (receptor activator of nuclear factor kappa-B ligand) production by denosumab that reduced bone resorption and allowed teriparatide to exert a stimulatory effect only on bone formation. These results reinforce the hypothesis that for optimal therapeutic outcome, bone formation and bone resorption should be modulated in different directions. The results of the studies of cathepsin K inhibitors illustrated that this may be feasible. Cathepsin K inhibitors, however, may preserve bone formation but are not anabolic agents, an important unmet need in the management of osteoporosis [38].
The design of a genuine anabolic treatment for osteoporosis must address the possibility of stimulating bone formation without concomitant stimulation of bone resorption and ensuring that formation is stimulated at quiescent bone surfaces. Human and animal genetics indicated that this may be feasible. In particular, the recognition of the pivotal role of the Wnt signaling pathway in bone formation provided a number of potential targets for the development of new pharmaceuticals. For clinical use, however, treatments should not only modify the expression of target molecules but need also to have bone specificity to avoid potential off-target effects [41, 42]. One such target is sclerostin, a negative regulator of bone formation produced exclusively in the skeleton by osteocytes [43]. The restricted expression of sclerostin in the skeleton and the lack of abnormalities in organs other than the skeleton in patients and animals with sclerostin deficiency made this protein an attractive target for the development of a new bone-forming therapy for the management of osteoporosis. This approach was further supported by studies of heterozygous carriers of sclerosteosis who have increased serum levels of P1NP and high, normal, or increased BMD but no clinical symptoms, signs, or complications of sclerosteosis [44, 45]. This will be discussed in further details in another chapter in this book.
The concept of bone modulation in osteoporosis management was further supported by the findings of recent studies documenting that the effectivity on fracture healing has been strengthened when teriparatide is combined with other anti-osteoporotics. Casanova et al. [46], using micro-CT and quantitative histomorphometry, showed that a 3-week administration of teriparatide together with zoledronic acid significantly increased bone volume and reduced trabecular spacing in mice with operatively induced fractures. Leder et al. [47] in a randomized control trial described more significant increases in BMD at the hip and at the lumbar spine in postmenopausal women treated for 2 years with teriparatide and denosumab, when compared with women on single administration of these medicaments. Furthermore, better fracture repair could be obtained using a combination of teriparatide and anti-sclerostin and/or anti-cathepsin K antibodies [48].
Implications from Research Studies and Clinical Practice
Inhibitors of Bone Resorption
Inhibitors of osteoclastic bone resorption, such as bisphosphonates, denosumab, and selective estrogen receptor modulators (SERMs), reduce the rate of bone resorption to varying degrees by different mechanisms of action. The reduction of the rate of bone resorption is invariably followed by reduction of the rate of bone formation due to the coupling of the two processes. The final result is an overall decrease of the rate of bone turnover to a level that depends on the potency of the individual agent used and is maintained during the whole period of treatment. The introduction of the most potent inhibitor of bone resorption, denosumab, into clinical practice made any further development of this class of agents obsolete. However, studies of humans and animals with osteopetrosis indicated that reduction of bone resorption may not necessarily be coupled with reduced bone formation if the osteoclasts remain intact [49].
Loss of function of a number of molecules regulating removal of bone mineral or degradation of bone matrix was shown to be associated with a decrease of bone resorption without, however, affecting or even stimulating bone formation [50, 51]. Cathepsin K (CatK), a protease abundantly expressed in osteoclasts responsible for the degradation of the organic matrix of the bone, is the most extensively studied molecule in preclinical and clinical studies.
Cathepsin K Inhibitors
Cathepsin K (CatK) is a member of a family of cysteine proteases that is synthesized as a proenzyme before being transported to lysosomes where it is cleaved to produce the active enzyme that degrades collagen type I and other bone matrix proteins within the acidic environment of resorption lacunae [52]. Congenital absence of CatK in patients with pycnodysostosis, a rare, autosomal, recessive osteochondrodysplasia, is characterized by increased bone density, bone deformities, and increased bone fragility, complications that are not present in heterozygotes [53]. CatK-deficient mice develop a high bone mass phenotype in the presence of fully differentiated osteoclasts, while mice overexpressing CatK had increased bone turnover and decreased trabecular bone volume [54, 55]. The discovery that loss of function of CatK decreases bone resorption with increased number of viable osteoclasts and the surprising finding of preservation or even increase in bone formation provided the rationale for the development of a new class of antiresorptive agents that target this enzyme (Fig. 17.2) [31, 56, 57]. The mechanism responsible for the maintenance or increase in bone formation in the presence of reduced bone resorption by CatK inhibition may be due to stimulation of osteoblasts by osteoclast-derived factors (clastokines, such as sphingosine-1-phosphate) or matrix-derived growth factors (such as IGF-1) that are not degraded [58, 59]. Initial studies of CatK inhibitors showed off-target inhibition of other cathepsins due either to their lack of specificity for CatK or to their accumulation in lysosomes of cells other than osteoclasts and led to the design of new agents potentially devoid of such effects. Two CatK inhibitors have been studied for the treatment of osteoporosis, namely, odanacatib (Merck & Co) and ONO-5334 (Ono Pharmaceutical Company).
Odanacatib is a selective, orally administered CatK inhibitor [60]. Unlike basic CatK inhibitors, odanacatib is neutral and does not accumulate in the acidic environment of lysosomes which could lead to off-target inhibition of other cathepsins [56, 61]. Odanacatib is metabolized by CYP3A4 and its absorption is not impaired by food intake [31, 62]. In animal models, odanacatib reduced bone resorption while preserving bone formation in trabecular and endocortical surfaces. In addition, odanacatib reduced cortical remodeling and increased modeling-based bone formation and improved the cortical area of the femur and its strength [63, 64]. Odanacatib was further superior to alendronate in increasing cortical thickness, possibly through increased periosteal bone formation, an action that was also observed during treatment with another CatK inhibitor [65, 66]. However, in 2016, Merk has published that it has decided to discontinue development after an independent adjudication and analysis of major adverse cardiovascular events confirmed an increased risk of stroke. Phase III results showed that while the drug could reduce fractures, it also increased the risk of atrial fibrillation and stroke.
Stimulators of Bone Formation
The only currently available bone-forming agent, PTH, stimulates bone formation but also bone resorption. PTH binds to the PTH/PTHrP type I receptor and activates several signaling pathways, including the canonical Wnt signaling pathway, having both anabolic and catabolic effects on the bone that are probably exerted via signaling in osteocytes [67]. Teriparatide, given by daily subcutaneous injections, increases cancellous and endocortical bone formation, mainly at sites undergoing active bone remodeling, but has limited effect on periosteal bone formation and increases cortical porosity [68]. PTHrP 1–36 and their analogue abaloparatide, which bind to the PTH/PTHrP 1 receptor, also increase bone formation and bone resorption markers, but to a lesser extent than teriparatide, and improve hip BMD significantly more than teriparatide [69, 70].
New Aspects of the Bone-Protecting Effects of Vitamin D
Vitamin D positively influences not only the mineralization of the bone matrix but via genomic and non-genomic effects modulates the function of some nonskeletal systems, including muscles. D-hormone metabolites have been shown to influence bone homeostasis directly. Bioactive 25(OH) D3, 1,25 (OH)2D3, as well as 24R,25 (OH)2D3 stimulated osteoblast growth and differentiation in vitro [71]. 1,25(OH)2 D3 administered in vivo for 28 consecutive days significantly increased bone formation, reduced bone resorption, and increased trabecular bone volume in mice [72].
Long-term treatment with 1α,25[OH](2)-2β-(3-hydroxypropyloxy) vitamin D3 metabolite (eldecalcitol) suppressed bone turnover, decreased the risk of bone microstructure deterioration, and increased bone biomechanical strength in ovariectomized rats [73]. Yamasaki et al. [74] found that eldecalcitol increased bone formation at the endocortical surface in female rats.
In clinical studies, significant increases in BMD in the spine of osteopenic women were found at the end of the first, second, and third years of treatment with 1,25(OH)2D3, while no positive effects in cholecalciferol-treated women were observed [75]. Thus, it can be said that D-hormone metabolites have unambiguously positive effects on bone mass and microstructure.
Further Nontraditional Molecules with Anti-osteoporotic Potential
Osteoclast formation is increased after the activation of T cells through NF-κB, NFATc1, or c-Fos signaling. In bone tissue culture, this process was inhibited by β-carboline alkaloid harmine. Additionally, the alkaloid increased osteoblast differentiation via Runx2, osterix, and bone morphogenetic peptide (BMP) [76]. Thus, harmine inhibits bone resorption and simultaneously activates bone formation. According to our knowledge, no study analyzing anti-osteoporotic effectivity of the alkaloid in vivo has been published yet.
Certain anti-osteoporotic activity was recorded in neoflavonoids, isolated chromatographically from Dalbergia sissoo heartwood. The flavonoids significantly stimulated calvarial osteoblast proliferation and mineralization [77]. Similarly, caviunin-based isoflavonoid stimulates bone formation via BMP2 and Wnt/β-catenin pathways, effectively inhibits osteoclastogenesis, and repairs cortical bone. In ovariectomized mice caviunin increased the mechanical strength of the vertebra and femur [78]. Similar anabolic effects on the skeleton mediated by Wnt/β-catenin signaling have been registered experimentally in aglycone of icariin. Micro-CT analysis showed that icariin after 12 weeks of treatment increased BMD, trabecular bone number, trabecular thickness, reduced trabecular separation, and increased biomechanical strength in oophorectomized rats [79]. Some flavonoids could be positioned as potential pharmaceuticals or food supplements for fracture repair in postmenopausal osteoporosis.
Strong bioactivity in the culture of osteoblast-like cells has been shown in the three-dimensional calcium-bearing structure CaP1 (which has three molecules of water). In vivo, the substance increased bone mineralization without any toxicity [80]. Bone regenerative effects were also found in synthetic diether molecules inhibiting RANKL-induced osteoclast formation [81], as well as in octacalcium phosphate, which increased bone mineralization via an irreversible transition into hydroxyapatite [82].
Furthermore, the food-derived compound sulforaphane and natural isothiocyanate promote osteoblast activity via epigenetic mechanisms. The molecule activates DNA demethylation increasing matrix mineralization. In mice it stimulates the expression of osteoblastic markers, such as Runx2 and collagen I A1 or ALP1, while inhibiting the nuclear factor-κB (RANKL) in osteocytes with subsequent increases in the trabecular number [83]. New strategies in therapy for osteolytic diseases consist of targeting noncoding microRNAs (miRNAs), which control gene expression in osteoclasts. Thus, miRNAs appear to be the key molecules in the regulation of bone resorption [84]. Bone homemostasis is determined by the osteogenesis/adipogenesis ratio in mesenchymal cells. Prevailing adipogenesis over osteogenesis is a principle pathological factor in accelerated bone loss. A strong modulator of osteogenic differentiation is the glutamate exchanger xCT (SLC7A11) sulfasalazine, which enhances the osteogenic potential via an increase in BMP2/4 expression. Sulfasalazine administered in vivo inhibited bone loss in hypoestrogenic mice [85]. Thus, sulfasalazine is a further candidate useful in the treatment of postmenopausal osteoporosis.
Potential bone-protecting candidates are also growth factors, such as BMP, fibroblast growth factor (FGF), and vascular endothelial growth factor (VEGF) [86]. Some of these mediate the action of other molecules [85]. The beneficial effects of erythropoetin or statins on fracture healing are under investigation; however, sufficient evidence of their anti-osteoporotic action in vivo is still lacking [87].
Implications of Remodeling and Modeling on the Long-Term Effects of Osteoporosis Drugs on Bone Mass and Strength
Bone mass, as evaluated by aBMD, remains the most important determinant of bone strength, explaining up to 80% of the failure load [88]. Hence greater gains in aBMD, and thereby higher aBMD values, have been associated with lesser fracture risk, both in the presence and absence of osteoporosis therapy [89, 90]. However, large differences in BMD gain, particularly at sites of predominantly cortical bone such as the hip, have been noted between osteoporosis drugs, and even among antiresorptives. Hence relatively weak antiresorptives such as selective estrogen receptor modulators induce a small (1–2%) initial gain of hip BMD, pertaining to the partial refilling of the remodeling space, but later do not prevent the loss of hip aBMD [91], because new bone resorption units continue to be activated and remodeling-based bone loss continues, particularly intracortically, which is not fully compensated for by the amount of modeling-based bone formation (Fig. 17.3). With more potent bisphosphonates, greater inhibition of bone remodeling allows greater gains in aBMD initially, but long-term clinical trials have consistently shown a plateauing effect after 2–3 years at the hip [92, 93]. This phenomenon could be explained by a new equilibrium reached between the amount of bone removed by the residual bone remodeling and the amount of new bone deposited by modeling-based bone formation, even though the latter may be somewhat negatively affected by bisphosphonates [94] (Fig. 17.4). However, with a complete suppression of bone remodeling, as achieved with denosumab, and provided bone modeling is sustained, as suggested by the studies on monkeys [95], then a positive bone accrual could be maintained long term, thereby potentially explaining the continuous BMD increase observed with this drug for up to 10 years [96]. Eventually, with new compounds such as odanacatib and particularly romosozumab, that both inhibit bone remodeling while promoting bone modeling, even if transiently, an even greater gain of aBMD could be observed.
The theoretical contribution of bone remodeling and modeling to the change in hip bone mineral density (BMD) in postmenopausal women with or without existing osteoporosis treatment.
Bisphosphonates [93, 97]; denosumab [98]; romosozumab [99, 100]; SERMs, selective estrogen receptor modulators [91]; parathyroid hormone [101]
In conclusion, the two components of bone remodeling, resorption, and formation constitute the primary target of pharmacological interventions for the management of the disease. It is now clear that bone resorption and formation can be differently modulated by new classes of anti-osteoporotic medications that provide a novel, personalized perspective for the management of patients in clinical practice.
References
Brown C. Osteoporosis: staying strong. Nature. 2017;550:S15–s17.
Sozen T, Ozisik L, Basaran NC. An overview and management of osteoporosis. Eur J Rheumatol. 2017;4:46–56.
Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–9.
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33.
Yaacobi E, Sanchez D, Maniar H, Horwitz DS. Surgical treatment of osteoporotic fractures: an update on the principles of management. Injury. 2017;48(Suppl. 7):S34–s40.
Feron JM, Mauprivez R. Fracture repair: general aspects and influence of osteoporosis and anti-osteoporosis treatment. Injury. 2016;47(Suppl. 1):S10–4.
von Ruden C, Augat P. Failure of fracture fixation in osteoporotic bone. Injury. 2016;47(Suppl. 2):S3–S10.
Smith DM, Khairi MR, Johnston CC Jr. The loss of bone mineral with aging and its relationship to risk of fracture. J Clin Investig. 1975;56:311–8.
Bernatz JT, et al. Osteoporosis is common and undertreated prior to total joint arthroplasty. J Arthroplast. 2019;34:1347–53.
Singer A, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90:53–62.
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR, HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356(18):1809–22.
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C, FREEDOM Trial. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–65.
Langdahl B, Ferrari S, Dempster DW. Bone modeling and remodeling: potential as therapeutic targets for the treatment of osteoporosis. Ther Adv Musculoskelet Dis. 2016;8(6):225–35. https://doi.org/10.1177/1759720X16670154.
Clark D, Nakamura M, Miclau T, Marcucio R. Effects of aging on fracture healing. Curr Osteoporos Rep. 2017;15:601–8.
Baxter MA, et al. Study of telomere length reveals rapid aging of human marrow stromal cells following in vitro expansion. Stem Cells. 2004;22:675–82.
Foulke BA, Kendal AR, Murray DW, Pandit H. Fracture healing in the elderly: a review. Maturitas. 2016;92:49–55.
Appelman-Dijkstra NM, Papapoulos SE. Novel approaches to the treatment of osteoporosis. Best Pract Res Clin Endocrinol Metab. 2014;28(6):843–57.
Turner CH. Biomechanics of bone: determinants of skeletal fragility and bone quality. Osteoporos Int. 2002;13:97–104.
Florencio-Silva R, Sasso GR, Sasso-Cerri E, Simoes MJ, Cerri PS. Biology of bone tissue: structure, function, and factors that influence bone cells. Biomed Res Int. 2015:421746.
Iwaniec UT, Turner RT. Influence of body weight on bone mass, architecture and turnover. J Endocrinol. 2016;230:R115–30.
van der Linden JC, Weinans H. Effects of microarchitecture on bone strength. Curr Osteoporos Rep. 2007;5:56–61.
Stock SR. The mineral–collagen interface in bone. Calcif Tissue Int. 2015;97:262–80.
Tzaphlidou M. Bone architecture: collagen structure and calcium/phosphorus maps. J Biol Phys. 2008;34:39–49.
Guerado E, et al. Bone mineral density aspects in the femoral neck of hip fracture patients. Injury. 2016;47(Suppl. 1):S21–4.
Karsenty G, Wagner EF. Reaching a genetic and molecular understanding of skeletal development. Dev Cell. 2002;2:389–406.
Suda T, Takahashi N, Udagawa N, et al. Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocr Rev. 1999;20:345–57.
Boyce BF, Xing L, Shakespeare W, Wang Y, Dalgarno D, Iuliucci J, Sawyer T. Regulation of bone remodeling and emerging breakthrough drugs for osteoporosis and osteolytic bone metastases. Kidney Int. 2003;63(Supplement 85):S2–5.
Arias CF, Herrero MA, Echeverri LF, Oleaga GE, LoÂpez JM. Bone remodeling: a tissue-level process emerging from cell-level molecular algorithms. PLoS ONE. 2018;13(9):e0204171. https://doi.org/10.1371/journal.pone.0204171.
Eriksen EF. Normal and pathological remodeling of human trabecular bone: three-dimensional reconstruction of the remodeling sequence in normal and in metabolic bone disease. Endocr Rev. 1986;7:379–408.
Everts V, Delaisee JM, Korper W, et al. The bone lining cell: its role in cleaning Howship's lacunae and initiating bone formation. J Bone Miner Res. 2002;17:77–90.
le Duong T. Therapeutic inhibition of cathepsin K-reducing bone resorption while maintaining bone formation. Bonekey Rep. 2012;1:67.
Karsdal MA, Martin TJ, Bollerslev J, Christiansen C, Henriksen K. Are nonresorbing osteoclasts sources of bone anabolic activity? J Bone Miner Res. 2007;22(4):487–94.
Martin TJ, Sims NA. Osteoclast-derived activity in the coupling of bone formation to resorption. Trends Mol Med. 2005;11(2):76–81.
Schaffler MB, Cheung WY, Majeska R, Kennedy O. Osteocytes: master orchestrators of bone. Calcif Tissue Int. 2014;94(1):5–24.
Parfitt A. Age related structural changes in trabecular and cortical bone: cellular mechanisms and biomechanical consequences. Calcif Tissue Int. 1984;36(Suppl I):S123–8.
Seeman E, Delmas PD. Bone quality-the material and structural basis of bone strength and fragility. N Engl J Med. 2006;354(21):2250–61.
Seeman E, Martin T. Antiresorptive and anabolic agents in the prevention and reversal of bone fragility. Nat Rev Rheumatol. 2019;15:225–36.
Appelman-Dijkstra N, Papapoulos S. Modulating bone resorption and bone formation in opposite directions in the treatment of postmenopausal osteoporosis. Drugs. 2015;75:1049–58.
Tsai JN, Uihlein AV, Lee H, Kumbhani R, Siwila-Sackman E, McKay EA, Burnett-Bowie SA, Neer RM, Leder BZ. Teriparatide and denosumab, alone or combined, in women with postmenopausal osteoporosis: the DATA study randomised trial. Lancet. 2013;382(9886):50–6.
Leder BZ, Tsai JN, Uihlein AV, Burnett-Bowie SA, Zhu Y, Foley K, Lee H, Neer RM. Two years of Denosumab and teriparatide administration in postmenopausal women with osteoporosis (The DATA Extension Study): a randomized controlled trial. J Clin Endocrinol Metab. 2014;99(5):1694–700.
Papapoulos SE. Targeting sclerostin as potential treatment of osteoporosis. Ann Rheum Dis. 2011;70(Suppl 1):i119–22.
Papapoulos SE. Anabolic bone therapies in 2014: new bone forming treatments for osteoporosis. Nat Rev Endocrinol. 2015;11:69–70.
van Bezooijen RL, Roelen BA, Visser A, van der Wee-Pals L, de Wilt E, Karperien M, Hamersma H, Papapoulos SE, ten Dijke P, Lo¨wik CW. Sclerostin is an osteocyte-expressed negative regulator of bone formation, but not a classical BMP antagonist. J Exp Med. 2004;199(6):805–14.
van Lierop AH, Hamdy NA, Hamersma H, van Bezooijen RL, Power J, Loveridge N, Papapoulos SE. Patients with sclerosteosis and disease carriers: human models of the effect of sclerostin on bone turnover. J Bone Miner Res. 2011;26(12):2804–11.
Gardner JC, van Bezooijen RL, Mervis B, Hamdy NA, Lowik CW, Hamersma H, Beighton P, Papapoulos SE. Bone mineral density in sclerosteosis; affected individuals and gene carriers. J Clin Endocrinol Metab. 2005;90(12):6392–5.
Casanova M, Herelle J, Thomas M, Softley R, Schindeler A, Little D, Schneider P, Müller R. Effect of combined treatment with zoledronic acid and parathyroid hormone on mouse bone callus structure and composition. Bone. 2016;92:70–8.
Leder BZ, Tsai JN, Neer RM, Uihlein AV, Wallace PM, Burnett-Bowie SA. Response to therapy with teriparatide, denosumab, or both in postmenopausal women in the DATA (Denosumab and Teriparatide Administration) study randomized controlled trial. J Clin Densitom. 2016;19:346–51.
Tella SH, Gallagher JC. Biological agents in management of osteoporosis. Eur J Clin Pharmacol. 2014;70:1291–301.
Segovia-Silvestre T, Neutzsky-Wulff AV, Sorensen MG, Christiansen C, Bollerslev J, Karsdal MA, Henriksen K. Advances in osteoclast biology resulting from the study of osteopetrotic mutations. Hum Genet. 2009;124(6):561–77.
Henriksen K, Karsdal MA, Martin TJ. Osteoclast-derived coupling factors in bone remodeling. Calcif Tissue Int. 2014;94(1):88–97.
Thudium CS, Moscatelli I, Flores C, Thomsen JS, Brüel A, Gudmann NS, Hauge E-M, Karsdal MA, Richter J, Henriksen K. A comparison of osteoclast-rich and osteoclast-poor osteopetrosis in adult mice sheds light on the role of the osteoclast in coupling bone resorption and bone formation. Calcif Tissue Int. 2014;95(1):83–93.
Garnero P, Borel O, Byrjalsen I, Ferreras M, Drake FH, McQueney MS, Foged NT, Delmas PD, Delaisse´ JM. The collagenolytic activity of cathepsin K is unique among mammalian proteinases. J Biol Chem. 1998;273(48):32347–52.
Gelb BD, Shi GP, Chapman HA, Desnick RJ. Pycnodysostosis, a lysosomal disease caused by cathepsin K deficiency. Science. 1996;273(5279):1236–8.
Gowen M, Lazner F, Dodds R, Kapadia R, Feild J, Tavaria M, Bertoncello I, Drake F, Zavarselk S, Tellis I, Hertzog P, Debouck C, Kola I. Cathepsin K knockout mice develop osteopetrosis due to a deficit in matrix degradation but not demineralization. J Bone Miner Res. 1999;14(10):1654–63.
Kiviranta R, Morko J, Uusitalo H, Aro HT, Vuorio E, Rantakokko J. Accelerated turnover of metaphyseal trabecular bone in mice overexpressing cathepsin K. J Bone Miner Res. 2001;16(8):1444–52.
Boonen S, Rosenberg E, Claessens F, Vanderschueren D, Papapoulos S. Inhibition of cathepsin K for treatment of osteoporosis. Curr Osteoporos Rep. 2012;10(1):73–9.
Yasuda Y, Kaleta J, Bro¨mme D. The role of cathepsins in osteoporosis and arthritis: rationale for the design of new therapeutics. Adv Drug Deliv Rev. 2005;57(7):973–93.
Fuller K, Lawrence KM, Ross JL, Grabowska UB, Shiroo M, Samuelsson B, Chambers TJ. Cathepsin K inhibitors prevent matrix-derived growth factor degradation by human osteoclasts. Bone. 2008;42(1):200–11.
Lotinun S, Kiviranta R, Matsubara T, Alzate JA, Neff L, Luth A, Koskivirta I, Kleuser B, Vacher J, Vuorio E, Horne WC, Baron R. Osteoclast-specific cathepsin K deletion stimulates S1P-dependent bone formation. J Clin Invest. 2013;123(2):666–81.
Gauthier JY, Chauret N, Cromlish W, Desmarais S, Duong LT, Falgueyret J-P, Kimmel DB, Lamontagne S, Léger S, LeRiche T, Li CS, Massé F, McKay DJ, Nicoll-Griffith DA, Oballa RM, Palmer JT, Percival MD, Riendeau D, Robichaud J, Rodan GA, Rodan SB, Seto C, Thérien M, Truong V-L, Venuti MC, Wesolowski G, Young RN, Zamboni R, Black WC. The discovery of odanacatib (MK-0822), a selective inhibitor of cathepsin K. Bioorg Med Chem Lett. 2008;18(3):923–8.
Pennypacker BL, le Duong T, Cusick TE, Masarachia PJ, Gentile MA, Gauthier JY, Black WC, Scott BB, Samadfam R, Smith SY, Kimmel DB. Cathepsin K inhibitors prevent bone loss in estrogen-deficient rabbits. J Bone Miner Res. 2011;26(2):252–62.
Pennypacker BL, Oballa RM, Levesque S, Kimmel DB, le Duong T. Cathepsin K inhibitors increase distal femoral bone mineral density in rapidly growing rabbits. BMC Musculoskelet Disord. 2013;14:344.
Cusick T, Chen CM, Pennypacker BL, Pickarski M, Kimmel DB, Scott BB, le Duong T. Odanacatib treatment increases hip bone mass and cortical thickness by preserving endocortical bone formation and stimulating periosteal bone formation in the ovariectomized adult rhesus monkey. J Bone Miner Res. 2012;27(3):524–37.
Pennypacker BL, Chen CM, Zheng H, Shih MS, Belfast M, Samadfam R, le Duong T. Inhibition of cathepsin K increases modeling-based bone formation, and improves cortical dimension and strength in adult ovariectomized monkeys. J Bone Miner Res. 2014;29(8):1847–58.
Cabal A, Jayakar RY, Sardesai S, Phillips EA, Szumiloski J, Posavec DJ, Mathers PD, Savitz AT, Scott BB, Winkelmann CT, Motzel S, Cook L, Hargreaves R, Evelhoch JL, Dardzinski BJ, Hangartner TN, McCracken PJ, le Duong T, Williams DS. High resolution peripheral quantitative computed tomography and finite element analysis of bone strength at the distal radius in ovariectomized adult rhesus monkey demonstrate efficacy of odanacatib and differentiation from alendronate. Bone. 2013;56(2):497–505.
Jerome C, Missbach M, Gamse R. Balicatib, a cathepsin K inhibitor, stimulates periosteal bone formation in monkeys. Osteoporos Int. 2012;23(1):339–49.
Saini V, Marengi DA, Barry KJ, Fulzele KS, Heiden E, Liu X, Dedic C, Maeda A, Lotinun S, Baron R, Pajevic PD. Parathyroid hormone (PTH)/PTH-related peptide type 1 receptor (PPR) signalling in osteocytes regulates anabolic and catabolic skeletal responses to PTH. J Biol Chem. 2013;288(28):20122–34.
Compston JE. Skeletal actions of intermittent parathyroid hormone: effects on bone remodelling and structure. Bone. 2007;40(6):1447–52.
Horwitz MJ, Augustine M, Kahn L, Martin E, Oakley CC, et al. A comparison of parathyroid hormone-related protein (1-36) and parathyroid hormone (1-34) on markers of bone turnover and bone density in postmenopausal women: the PrOP study. J Bone Miner Res. 2013;28:2266–76.
Leder BZ, O’Dea LSL, Zanchetta JR, Kumar P, Banks K, McKay K, Lyttle CR, Hattersley G. Effects of abaloparatide, a human parathyroid hormone-related peptide analog, on bone mineral density in postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 2015;100(2):697–706.
Van Der Meijden K, Lips P, Van Driel M, Heijboer AC, Schulten EA, Den Heijer M, Bravenboer N. Primary human osteoblasts in response to 25-hydroxyvitamn D3, 1,25-dihydroxyvitamin D3 and 24R,25-dihyroxyvitamin D3. PLoS One. 2014;9:e110283.
Oelzner P, Petrow PK, Wolf G, Bräuer R. 1,25-dihydroxyvitamin D3 prevents bone loss of the secondary spongiosa in arthritic rats by an increase of bone formation and mineralization and inhibition of bone resorption. BMC Musculoskelet Disord. 2014;15:345.
Takeda S, Smith SY, Tamura T, Saito H, Takahashi F, Samadfam R, Haile S, Doyle N, Endo K. Long-term treatment with eldecalcitol (1α, 25-dihydroxy-2β-(3-hydroxypropyloxy) vitamin D3) suppresses bone turnover and leads to prevention of bone loss and bone fragility in ovariectomized rats. Calcif Tissue Int. 2015;96:45–55.
Yamasaki Y, Nagira K, Osaki M, Nagashima H, Hagino H. Effects of eldecalcitol on cortical bone response to mechanical loading in rats. BMC Musculoskelet Disord. 2015;16:158.
Zofkova I, Hill M. Long-term 1,25(OH)2 vitamin D therapy increases bone mineral density in osteopenic women. Comparison with the effect of plain vitamin D. Aging Clin Exp Res. 2007;19:472–7.
Yonezawa T, Lee JW, Hibino A, Asai M, Hojo H, Cha BY, Teruya T, Nagai K, Chung UI, Yagasaki K, Woo JT. Harmine promotes osteoblast differentiation through bone morphogenetic protein signaling. Biochem Biophys Res Commun. 2011;409:260–5.
Kumar P, Kushwaha P, Khedgikar V, Gautam J, Choudhary D, Singh D, Trivedi R, Maurya R. Neoflavonoids as potential osteogenic agents from Dalbergia sissoo heartwood. Bioorg Med Chem Lett. 2014;24:2664–8.
Kushwaha P, Khedgikar V, Gautam J, Dixit P, Chillara R, Verma A, Thakur R, Mishra DP, Singh D, Maurya R, Chattopadhyay N, Mishra PR, Trivedi R. A novel therapeutic approach with Caviunin-based isoflavonoid that en routes bone marrow cells to bone formation via BMP2/Wnt-βcatenin signaling. Cell Death Dis. 2014;5:e1422.
Chen G, Wang C, Wang J, Yin S, Gao H, Xiang LU, Liu H, Xiong Y, Wang P, Zhu X, Yang LI, Zhang R. Antiosteoporotic effect of icariin in ovariectomized rats is mediated via Wnt/β-catenin pathway. Exp Ther Med. 2016;12:279–87.
Shi FN, Almeida JC, Helguero LA, Fernandes MH, Knowles JC, Rocha J. Calcium phosphonate frameworks for treating bone tissue disorders. Inorg Chem. 2015;54:9929–35.
DOH KE, KANG JH, Ting Z, Yim M, Choo HY. Novel diether compounds inhibiting differentiation of osteoclasts. Arch Pharm Res. 2016;39:178–90.
Suzuki O, Imaizumi H, Kamakura S, Katagiri T. Bone regeneration by synthetic octacalcium phosphate and its role in biological mineralization. Curr Med Chem. 2008;15:305–13.
Thaler R, Maurizi A, Roschger P, Sturmlechner I, Khani F, Spitzer S, Rumpler M, Zwerina J, Karlic H, Dudakovic A, Klaushofer K, Teti A, Rucci N, Varga F, Van Wijnen AJ. Anabolic and antiresorptive modulation of bone homeostasis by the epigenetic modulator sulforaphane, a naturally occurring isothiocyanate. J Biol Chem. 2016;291:6754–71.
Li H, Zhai Z, Qu X, Xu J, Qin A, Dai K. MicroRNAs as potential targets for treatment of osteoclast-related diseases. Curr Drug Targets. 2018;19(5):422–31.
Jin C, Zhang P, Zhang M, Zhang X, Lv L, Liu H, Liu Y, Zhou Y. Inhibition of SLC7A11 by sulfasalazine enhances osteogenic differentiation of mesenchymal stem cells by modulating BMP2/4 expression and suppresses bone loss in ovariectomized mice. J Bone Miner Res. 2016;32:508–21.
Lee ZH, Kim HJ, Ryoo HM. A novel oesteogenic activity of suberoylanilide hydroxamic acid is synergized by BMP-2. J Bone Metab. 2015;22:51–6.
Klontzas ME, Kenanidiz EI, Macfarlane RJ, Michail T, Potoupnis ME, Heliotis M, Mantalaris A, Tsiridis E. Investigational drugs for fracture healing: preclinical and clinical data. Expert Opin Investig Drugs. 2016;25:585–96.
Zysset P, Dall’ara E, Varga P, Pahr D. Finite element analysis for prediction of bone strength. Bonekey Rep. 2013;2:386.
Cosman F, Cauley J, Eastell R, Boonen S, Palermo L, Reid I, et al. Reassessment of fracture risk in women after 3 years of treatment with zoledronic acid: when is it reasonable to discontinue treatment? J Clin Endocrinol Metab. 2014;99:4546–54.
Schwartz A, Bauer D, Cummings S, Cauley J, Ensrud K, Palermo L, et al. Efficacy of continued alendronate for fractures in women with and without prevalent vertebral fracture: the FLEX trial. J Bone Miner Res. 2010;25:976–82.
Silverman S, Chines A, Kendler D, Kung A, Teglbjaerg C, Felsenberg D, et al. Sustained efficacy and safety of bazedoxifene in preventing fractures in postmenopausal women with osteoporosis: results of a 5-year, randomized, placebo-controlled study. Osteoporos Int. 2012;23:351–63.
Black D, Schwartz A, Ensrud K, Cauley J, Levis S, Quandt S, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006;296:2927–38.
Miller P, Recker R, Reginster J, Riis B, Czerwinski E, Masanauskaite D, et al. Efficacy of monthly oral ibandronate is sustained over 5 years: the MOBILE long-term extension study. Osteoporos Int. 2012;23:1747–56.
Gasser J, Kneissel M, Thomsen J, Mosekilde L. PTH and interactions with bisphosphonates. J Musculoskelet Neuronal Interact. 2000;1:53–6.
Ominsky M, Libanati C, Niu Q, Boyce R, Kostenuik P, Wagman R, et al. Sustained modeling-based bone formation during adulthood in cynomolgus monkeys may contribute to continuous BMD gains with denosumab. J Bone Miner Res. 2015;30:1280–9.
Papapoulos S, Lippuner K, Roux C, Lin C, Kendler D, Lewiecki E, et al. The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM extension study. Osteoporos Int. 2015;26:2773–83.
Black D, Reid I, Cauley J, Cosman F, Leung P, Lakatos P, et al. The effect of 6 versus 9 years of zoledronic acid treatment in osteoporosis: a randomized second extension to the HORIZON Pivotal Fracture Trial (PFT). J Bone Miner Res. 2015;30:934–44.
Bone H, Chapurlat R, Brandi M, Brown J, Czerwinski E, Krieg M, et al. The effect of three or six years of denosumab exposure in women with postmenopausal osteoporosis: results from the FREEDOM extension. J Clin Endocrinol Metab. 2013;98:4483–92.
McClung M, Chines A, Brown J, Diez-Perez A, Resch H, Caminis J, et al. Effects of 2 years of treatment with Romosozumab followed by 1 year of Denosumab or placebo in postmenopausal women with low bone mineral density. J Bone Miner Res. 2014;Suppl. 1:1152.
McClung M, Grauer A, Boonen S, Bolognese M, Brown J, Diez-Perez A, et al. Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med. 2014;370:412–20.
Neer R, Arnaud C, Zanchetta J, Prince R, Gaich G, Reginster J, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–41.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
El Miedany, Y. (2022). Bone Modulation. In: El Miedany, Y. (eds) New Horizons in Osteoporosis Management. Springer, Cham. https://doi.org/10.1007/978-3-030-87950-1_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-87950-1_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87949-5
Online ISBN: 978-3-030-87950-1
eBook Packages: MedicineMedicine (R0)