Abstract
While, risk assessment tools help identify individuals who need treatment, their usefulness relies on the clinician’s ability to correctly translate their results into clinical practice congruent with evidence-based guidelines. Although osteoporosis is a highly treatable condition and despite the fact that clinical guidelines have been widely available to help those patients, many individuals who are at substantial risk of fracture still go untreated. Therefore, promoting early diagnosis and developing management guidelines applicable to standard clinical practice are essential to tackle such challenge. However, this alone is unlikely to solve this problem. The fact being that only 11% of patients suffering from a fragility hip fracture have been started on bone protective therapy as a secondary prevention and the well-known finding of patients’ nonadherence to treatment raise the red flags highlighting deficiencies in the current practice. Consequently, there are unmet needs in the diagnosis and management of osteoporosis, and, successively, there is, obviously, a room for improvement in the approach toward stratification and management of people at risk of osteoporosis or sustaining a fragility fracture. Closing this treatment gap is a priority that involves improving selection of patients at risk of fracture for DXA scanning, securing optimal treatment when indicated, and providing follow-up that encourages patient adherence to treatment. This chapter will discuss the unmet needs and challenges of the diagnosing and management of osteoporosis and the limitations of currently available tools.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Osteoporosis is always a hot topic that is discussed on yearly basis at all the international conferences dealing with the topic of bone health, reflecting the importance of the disease. In fact osteoporosis is a major health issue, affecting around 200 million women worldwide. Moreover, although osteoporosis is typically linked to women, it is also diagnosed in men, however, to less extent. While one in three women over age 50 will experience osteoporotic fractures, one in five men aged over 50 will sustain the disease [1, 2]. Worldwide, osteoporosis accounts for a greater disability burden than cancer, with the exception of lung cancer [3]. This is supported by the reports showing that the incidence of osteoporosis is increasing [2]. In contrast, osteoporosis treatment remains a challenge, with 50–70% of the patients discontinuing their osteoporosis medications within the first year of initiation [4]. Therefore, there is an urgent need for improved management of osteoporosis and its consequences.
Over the past decade, several guidelines have been published for the pharmacological management of osteoporosis in postmenopausal women, which highlight the need for earlier, more widespread screening, and treatment are published [5]. However, a US observational study of women experiencing a first hip fracture between 2008 and 2013 showed that only 17% and 23% had evidence of osteoporosis assessment and/or treatment within 6 or 12 months of their fractures, respectively [6]. Furthermore, the Healthcare Effectiveness Data and Information Set (HEDIS), which is a tool used by more than 90% of America’s health plans to measure performance on important dimensions of care and service for a number of disease areas [7], assessed the number of women aged 65–85 years who suffered a fracture and who had either a bone mineral density (BMD) test or prescription for a drug to treat osteoporosis in the 6 months after their fracture with the intent to reduce the risk of fractures resulting from osteoporosis in older women. Testing/treatment rate in women who sustained a fracture in the USA reached 49.6% in 2018 [8]. Results from a recently published survey of untreated postmenopausal women with osteoporosis and their physicians reported that patients themselves decided against pharmacological treatment in at least half of the cases of nontreatment. The most frequent reasons for this patient decision were concerns regarding side effects, alternative nonprescription options (including behavioral modification), and questioning medication benefits [6, 9].
Such inconsistency in management, together with underdiagnosis and undertreatment of people who are at high risk for fracture, represents the unmet need in the diagnosis and management of osteoporosis. It is, therefore, vital to identify and address these factors which may contribute to such challenge. Table 15.1 summarizes the unmet needs and challenges in the field of osteoporosis. This chapter will discuss the unmet needs and challenges of diagnosing and management of osteoporosis and the limitations of currently available tools.
Challenge 1: Fracture Risk Score and Absolute Risk of Fracture
The National Institutes of Health Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy defines osteoporosis as a skeletal disorder characterized by low bone strength and increased risk of fracture [10]. This definition of osteoporosis reflects the changing perspective on this disease, i.e., osteoporosis is no longer considered a disorder of low bone mineral density alone. Epidemiologic studies have been performed to examine the risk factors that are associated with low bone mineral density and fragility fractures [11, 12]. Consequently, assessments of clinical risk factors that are independent of BMD have been identified as important prognosticators for fracture prediction. Namely, in addition to BMD, advancing age, prior history of fragility fracture, chronic glucocorticoid use, low body mass index (BMI), parental history of hip fracture, cigarette smoking, and excess alcohol intake are the risk factors that have been demonstrated to be most predictive of fracture.
Expression of fracture risk: Absolute risk (AR) is the probability of fracture, usually expressed as a percentage, over a specified period of time. Relative risk (RR) is the ratio of absolute risks of two populations [13]. RR tends to overestimate fracture risk in some populations and underestimate it in others [14]. As an example, a 50-year-old and an 80-year-old woman with a hip T-score of −2.5 each have the same RR for hip fracture compared with an age-matched population with normal BMD [13], while the 10-year probability of hip fracture is much higher in the 80-year-old woman. Both are measures of risk, but estimation of an individual’s fracture risk requires knowledge of absolute risk when relative risk estimates are used. Therefore, absolute risk is a measure easily explainable to both the physician [15] and the patient.
Several fracture risk assessment tool have been developed; however, the most popular and commonly used out of them is the developed, in 2008, by the University of Sheffield (FRAX) that estimates the 10-year probability of hip fracture and major osteoporotic fracture (hip, clinical spine, proximal humerus, or forearm) for untreated patients between ages 40 and 90 years using easily obtainable clinical risk factors for fracture and femoral neck BMD (g/cm2, using dual-energy X-ray absorptiometry [DXA]), when available [16, 17]. As well as the FRAX tool, other fracture risk calculators are available online which include the Garvan fracture risk calculator (www.garvan.org.au) and QFracture (www.qfracture.org) .
There are several important limitations that need to be considered when FRAX is used as a calculation tool. The relationships between risk factors and fracture risk incorporated within the FRAX model have been constructed from the primary data of nine population-based cohorts around the world [18,19,20]. Databases from most of the countries incorporated into FRAX provided accurate rates of hip fractures because all patients with a hip fracture are admitted to a hospital. However, patients with a wrist or proximal humeral fracture are usually treated as outpatients, leading to an underestimation of the incidence of these types of fractures [21]. Assessing the rate of clinical vertebral fracture is also challenging since it is difficult to distinguish between patients with a clinical vertebral fracture and patients who have back pain with an incidental vertebral compression fracture. Therefore, the reported rates of major osteoporotic fractures at sites other than the hip may not be accurate. Kanis et al. [19] studied the use of clinical risk factors to predict osteoporotic fractures on the basis of baseline and follow-up data from nine population-based cohorts. They found that models for predicting hip fractures were substantially better than those for predicting osteoporotic fractures at other sites, regardless of whether the models included bone mineral density alone, clinical risk factors alone, or a combination of both [22]. For these reasons, the prediction of the risks of three other major osteoporotic fractures (proximal humeral, wrist, and clinical vertebral fractures) may not be as accurate as the prediction of the risk of hip fracture.
There is also a question of the generalizability of data obtained from the population-based cohorts. For example, the US FRAX model was formulated from data from the Rochester cohort, which was recruited from two random population samples in Olmsted County, Minnesota. This community is predominantly White and is better educated than the White population of the USA as a whole [23]. In addition, recent data have shown that the incidence of hip fracture among Olmsted County residents is declining [24]. Therefore, the incidence and mortality data in the US FRAX model may not reflect current incidence and mortality rates.
The use of FRAX sometimes results in 10-year fracture probabilities that lead to treatment recommendations that contradict those of the National Osteoporosis Foundation. For example, a 50-year-old postmenopausal woman with a body mass index of 24.1 kg/m2, no clinical risk factors, and a T-score of −2.5 meets the threshold for pharmacological therapy on the basis of the T-score; however, the fracture probabilities calculated with the FRAX tool (8.7% for a major osteoporotic fracture and 2.5% for a hip fracture) are below the treatment threshold. Conversely, an 80-year-old postmenopausal woman with the same body mass index, a parental history of hip fracture, and a T-score of −1.0 has 10-year risks of 26% and 9.9%, respectively, for a major osteoporotic fracture and for a hip fracture—a level of risk at which treatment should be considered [25]. Yet, there is no strong evidence to support treatment of patients with this level of bone mineral density. In addition, FRAX may not accurately predict fracture risk across all age groups [22]. Furthermore, fracture risk probabilities calculated with FRAX are not valid for patients who have already received pharmacological treatment for osteoporosis such as bisphosphonates.
The magnitude by which FRAX may over- or underestimate fracture risk has been studied using large population databases, and procedures for adjusting FRAX probability have been proposed [26, 27]. As an example, an analysis of the Canadian Manitoba BMD database shows that when there is discordance between lumbar spine and femoral neck BMD, the FRAX estimate for major osteoporotic fracture may be increased or decreased by one-tenth for each rounded T-score difference or offset between lumbar spine and femoral neck (e.g., when the lumbar spine T-score is 1.0 less than the femoral neck T-score, the 10-year probability of major osteoporotic fracture can be increased by one-tenth) [26]. Another analysis using the UK General Practice Research Database showed that for patients exposed to high-dose glucocorticoids (prednisolone >7.5 mg/day or equivalent), the 10-year probability of major osteoporotic fracture may be increased by 15 percent and the 10-year probability of hip increased by 20 percent [27]. The increase in fracture risk associated with type II diabetes mellitus may be captured by entering “yes” for rheumatoid arthritis in the FRAX algorithm [28]. With modifications such as these, the FRAX probability of fracture can be refined [29]. However, these correction factors have not been computed for the majority of countries represented by FRAX, including the USA. Thus, they should be applied to US populations with caution.
Other important risk factors for fractures are not included in this calculation tool. These include the serum level of 25-hydroxyvitamin D, physical activity, risk of falls, and biochemical bone markers. Therefore, the calculated risk may be less than the actual risk. In addition, FRAX does not take into account bone mineral density at the spine or the substantially higher risk of spine fracture among those with a history of vertebral compression fractures. A cohort study of 6459 women 55 years of age or older with low bone mineral density, of whom 31% (2027) had a radiographically detected vertebral fracture at baseline, demonstrated that a combination of a vertebral fracture on a baseline radiograph, femoral neck bone mineral density, and age predicted incident radiographically evident vertebral fractures significantly better than did use of FRAX and bone mineral density at the femoral neck (p = 0.0017) [30]. Nevertheless, FRAX remains an important tool that represents an advance in the care of osteoporosis. The current FRAX model provides an aid to enhance patient assessment by the integration of clinical risk factors alone and/or in combination with bone mineral density. It is anticipated that the limitations described above will be addressed in future FRAX versions.
Challenge 2: Implementation of Health Economics into Clinical Guidelines
The use of health economic thresholds incorporating QALYs (quality-adjusted life year) led to some difficulties with some of the initial guidelines developed [31, 32], as the costs of treatments meant that patients with osteoporosis confirmed by dual-energy X-ray absorptiometry (DXA) would not have access to drugs, since estimated health costs exceeded £20,000/QALY [7]. In response, the National Osteoporosis Guideline Group (NOGG) in the UK developed evidence-based guidelines with alternative treatment thresholds, which were not set using health economic considerations but the clinical fracture risk after a first low-trauma fracture [33]. On the other hand, the National Osteoporosis Foundation osteoporosis treatment recommendations were based on the 10-year fracture probability model, whereas, in Scotland, “SIGN” (Scottish Intercollegiate Guideline Network) guidelines took an alternative approach, interpreting clinical trial-based evidence to support drug treatment for those who have had a vertebral fracture and hip fracture or with a bone mineral density (BMD) T-score less than −2.5 [34]. The most recent recommendations from NICE [35] are a radical change, with no health economic argument against oral or parenteral therapy down to a 10-year fracture risk of 1%. However, it recently has been suggested that “Unthinking assimilation of the NICE multiple technology appraisal risks a generation of older individuals taking a bisphosphonate regardless of the individual benefit-to-risk ratio” [36]. There are now a number of guidelines on osteoporosis across Europe and North America, with country- and comorbidity-specific recommendations. Each takes a slightly different approach, resulting in inconsistent recommendations (Table 15.1). Consequently, clinicians are faced with an overwhelming amount of guidance on the management of osteoporosis and bone health from international, national, and local governing bodies. No wonder, such global inconsistency would reflect on the patients’ management particularly at the primary care level.
In addition, there is a low reimbursement for DXA investigations in the USA. It is possible that pharmaceutical industries also play a role, as during the first years after introduction of osteoporotic drugs, an increase of bisphosphonate use was observed (in 2007 ~ 15% of postmenopausal women used bisphosphonates) [37]. Currently, there is a growing market share of generics drugs and increased withdrawal of large pharmaceutical industries, which might be related to a decrease in bisphosphonate use. This emphasizes the certain unmet need for new drugs with an even better efficacy/safety profile.
Challenge 3: Treatment Thresholds
After the advent of absolute fracture risk calculators, guidelines for the management of osteoporosis have been published. These have been updated several times over the past decade. However, there were disparity between different guidelines and the treatment thresholds advised which represent a challenge to osteoporosis specialists trying to manage their patients, according to these guidelines. Best examples are the guidelines released by the US-based National Osteoporosis Foundation (NOF) and the UK-based National Osteoporosis Guidelines Group (NOGG) which differ markedly in their approaches to treatment recommendations.
The National Osteoporosis Foundation recommendations for pharmacological treatment of osteoporosis [38] are based in part on the US adaptations of the World Health Organization 10-year fracture probability model and algorithms for determining treatment thresholds [39]. These recommendations are based on cost-effectiveness in populations of patients and should be used together with other considerations when making treatment decisions for individual patients. According to the National Osteoporosis Foundation recommendations, treatment of osteoporosis should be considered for (1) patients with a history of hip or vertebral fracture, (2) patients with a T-score of −2.5 or lower at the femoral neck or spine, and (3) patients who have a T-score of between −1.0 and − 2.5 at the femoral neck or spine and a 10-year hip fracture risk of ≥3% or a 10-year risk of a major osteoporosis-related fracture of ≥20% as assessed with the FRAX. The advantages of this new recommendation as compared with the earlier published National Osteoporosis Foundation recommendations include better allocation of limited healthcare resources to patients who are at higher risk for fracture and most likely to benefit from therapy. In addition, these new guidelines take into consideration different ethnicities in the USA and include the male population.
Similar to the National Osteoporosis Foundation, the UK developed by the National Osteoporosis Guidelines Group (NOGG) [39] incorporated FRAX-derived risk calculations. However, the approaches taken to recommendations for intervention by these guidelines differ markedly, as summarized in Fig. 15.1. The NOF intervention thresholds are based upon economic cost-effectiveness analyses [40,41,42,43,44], whereas the NOGG guidelines recommend intervention if the probability of fracture exceeds that of a person of the same age who has suffered a previous osteoporotic fracture [45]. Thus, the NOGG intervention and assessment thresholds vary by age and gender, such that reassurance is recommended for older individuals at high risk of fracture, whereas intervention is recommended for younger individuals at lower risk of fracture.
Summaries of the NOGG and NOF guidelines for management of osteoporosis (left), with their application to a cohort of 1471 healthy older women (right). a, Nineteen women in the cohort were younger than 65 yr. at baseline. The NOF guidelines recommend BMD measurement in women younger than 65 yr. if there are concerns based on the risk factor profile. For the purposes of this analysis, we assumed that all these 19 women had a measurement of BMD for this reason. (Unless provided in the caption above, the following copyright applies to the content of this slide: Copyright © 2010 by The Endocrine Society)
Potentially, the differing approaches between guidelines might lead to different treatment recommendations and fracture outcomes. In the study done by Mark and Grey [46], two illustrative clinical cases were presented to symbolize the difference between the two treatment recommendations. Patient (1) is a female, aged 80 years old, in good health, with BMI of 23.8 kg/m2, no personal or parental history of fracture, and a femoral neck BMD T-score of −3. Her estimated 10-year risk of major osteoporotic fracture using FRAX with BMD is 21% and of hip fracture is 9%. Applying the NOGG guidelines leads to a recommendation to reassure, whereas the NOF guidelines recommend treatment. Patient (2) is a female, aged 65 years old, in good health, and also has a BMI of 23.8 kg/m2, no personal or parental history of fracture, and a femoral neck BMD T-score of −3. Her estimated 10-year risk of major osteoporotic fracture is 16% and of hip fracture is 5%. Both the NOGG and NOF guidelines recommend treatment. This paved the way for the most recent osteoporosis treatment recommendations published by NOGG in 2017, in which NOGG has released its update in which the intervention thresholds have been based on FRAX probability and so cannot be used with fracture risk derived from QFracture or other calculators [4]. NOGG recommended also that diagnostic assessment should include not only the assessment of BMD where indicated but also the exclusion of diseases that mimic osteoporosis, elucidation of the cause of the osteoporosis, and the management of any associated morbidity. In addition, recommendations for the routine investigation of patients with osteoporosis have been advised and are summarized in Tables 15.2 and 15.3.
Challenge 4: DXA
Appropriate and accurate use of densitometric techniques is of great importance: bone mineral measurements provide not only diagnostic criteria but also prognostic information on fracture risk probability, and they are also used to monitor treated or untreated patient [47]. For this reason, several guidelines have been developed in the last years with a number of recommendations that include indications for BMD testing, which skeletal site to measure and how to interpret and report BMD results, and proper timing for follow-up [48,49,50,51]. These guidelines, typically issued by relevant medical societies or specialized working groups, play an important role in clinical practice: they provide valuable suggestions based on the highest level of evidence, which is usually achieved through a critical evaluation of systematically searched primary studies [52, 53].
The distribution of bone density across a population is dependent on race, age, and gender. For example, African-Americans have lower rates of fracture compared to US Caucasians and Asians, and this parallels the population distribution differences among races [54]. In one study, the age-adjusted mean for femoral neck BMD was 0.686 g/cm2 in US Caucasians and 0.841 g/cm2 in African Americans [55]. Because of such racial and ethnic differences, the significance of T-scores must be considered based on the fracture risk of ethnic and racially matched persons. A similar rationale can be applied to men who have larger skeletal structures compared to women. To control for racial differences, DXA calculates T-scores using normative databases based on NHANES III data that include non-Hispanic White, Black, Hispanic, and Asian individuals [56]. A pediatric normative base is also available. However, while bone size is directly related to strength, DXA does not account for bone size in assessing fracture risk. Attempts to correct bone size for height and weight have been reported [57]. Some DXA manufacturers allow for weight correction in the calculation of Z-scores to adjust for an expected decrease in fracture risk as weight increases. Height correction is especially important in assessing fracture risk in children affected by short stature or growth delay [58].
DXA images are a two-dimensional (vertical and horizontal) condensation of a three-dimensional structure. As such, bone thickness is not measured in this scan. The BMC measured reflects the amount of cortical and trabecular tissue present within a structure that acts to attenuate the X-ray signal; bones with more tissue attenuate the signal to a greater degree resulting in a higher gray value and BMC measure. Bone area is a measure of the size of the region of interest “ROI.” For the hip, the ROI width is fixed, and thus variation in bone area reflects differences in external bone size. The ratio of these two variables provides a measure of the mass density but not a measure of morphology or material properties. Further, BMD does not differentiate whether the variation in BMD arises from differences in cortical mass, trabecular mass, or external bone size [59].
Conventional wisdom is that women uniformly lose endosteal and trabecular bone in a similar pattern. Recent data however suggest that the pattern of bone loss with aging in women is not uniform [60]. Bone shape and size at the menopause transition may in fact have a critical role in determining long-term bone loss with aging. Women with narrower femoral necks experienced modest decreases in BMC compared to those with wider femoral necks (Fig. 15.3). But, women with narrow femoral necks also had larger increases in femoral neck area compared to women with wider femoral necks. BMD is the quotient of the BMC divided by the area. Because the larger increase in the denominator (area) in women with narrow femoral necks is similarly matched by the larger decrease in the numerator (BMC) in women with wide femoral necks, the result is that both groups have similar losses in BMD over time but for very different reasons. The impact of these structural and mass changes on strength is currently under investigation. In addition to the previous discussion regarding how most fragility fractures occur in persons with T-scores > − 2.5, this example illustrates another limitation of DXA scanning to accurately predict bone strength and fracture risk.
Diagnosis of Osteoporosis: More Than Dual-Energy X-Ray Absorptiometry Alone
It could be argued that performing a VFA (vertebral fracture assessment) in all patients for whom a DXA is indicated and performed would be beneficial [61]. With this technique, (asymptomatic) vertebral deformities can be detected. For example, it was recently documented in a cross-sectional study that vertebral fractures were found in 13% of rheumatoid arthritis (RA) patients [62]. Vertebral fractures are clinically relevant: although only one-third of the vertebral deformities are associated with clinical signs and symptoms of an acute vertebral fracture, they are a good predictor of subsequent vertebral and hip fractures and may have impact on quality of life [63]. Moreover, assessment of vertebral fractures in addition to BMD enhances fracture risk prediction [64]. Thus, the finding of one or more moderate or severe vertebral deformities in patients with osteopenia may make the difference between starting treatment with anti-osteoporotic medication or not.
The European League Against Rheumatism (EULAR)/ European Federation of National Associations of Orthopaedics and Traumatology (EFORT) recommendations advocate that in all patients 50 years and over with a recent fracture in addition to DXA/VFA, fall risk evaluation and screening for secondary causes of osteoporosis need to be performed [65]. In patients with an elevated fall risk, it is clinically relevant to establish whether modifiable risk factors can be identified; the same is true for potentially treatable causes of secondary osteoporosis and other metabolic bone disorders. Obviously, both high fall rate and untreated secondary osteoporosis may limit the effect of both nonmedical and drug treatment. There are hardly any data on the implementation of these four crucial diagnostic steps in daily practice. However, considering the access to DXA which is suboptimal and the poor implementation of the other four steps (VFA incorporation in DXA, fall risk assessment, fracture risk assessment, and active screening for secondary causes of osteoporosis), this emphasizes that there is an urgent need for better diagnostic procedures in patients at risk for fractures [66].
Challenge 5: Measuring Bone Strength
Although the DXA device is an easy-to-use tool for diagnosing osteoporosis, a limitation is that the DXA device measures only one aspect of bone strength, that is, bone density, which can be considered as the amount of hydroxyapatite (Ca10(PO4)6(OH)2) per bone area. Therefore, the BMD value measured by DXA is influenced by degenerative changes, atherosclerosis (aortic calcifications), and fractured lumbar vertebrae, as these conditions are characterized by calcifications potentially increasing BMD values [67, 68].
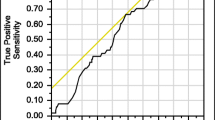
Another limitation of DXA is that it creates a two-dimensional image of bone structures, and therefore details cannot be identified. A large proportion of fractures occur in individuals not identified by a low augmented BMD (aBMD) (Fig. 15.2). For these reasons, new and more advanced techniques such as trabecular bone score (TBS), high-resolution peripheral quantitative computed tomography (HR-pQCT), ultrasound, finite element analysis (FEA), and magnetic resonance imaging (MRI) are under development.
Structural changes in bone with osteoporosis medications. The antiresorptive medications (bisphosphonates and denosumab) and anabolic medications (teriparatide and likely abaloparatide) produce very different structural changes in bone. Although both classes increase trabecular bone, their effects on cortical bone are different. Bisphosphonates and denosumab do not expand periosteal bone but do decrease the endosteal diameter by an increase in endosteal bone volume. Antiresorptives also reduce cortical porosity. Anabolic agents lead to an increase in periosteal bone with a simultaneous increase in endosteal bone resorption resulting in a bone without a large change in cortical thickness. At the same time, anabolic agents increase cortical porosity. Despite the increase in cortical porosity, the larger bone has increased strength. NC no change. (Adapted from: Choksi et al. [59] (under open access scheme)
TBS is a surrogate marker for bone microarchitecture and has been associated with prevalent and incident fractures [69]. Although TBS changes during treatment, TBS is less sensitive to change than aBMD. Although TBS may have a role in predicting future fracture risk in specific disorders like hyperparathyroidism and diabetes, its precise role in osteoporotic care remains to be elucidated.
HR-pQCT is probably a more promising technique: one of the biggest advantages of HR-pQCT is that it constructs a three-dimensional image of the bone and it has the additional value of measuring the microarchitecture of bone, that is, both cortical and trabecular aspects of bone. Previous studies showed that several HR-pQCT-derived bone parameters, with or without FEA, are associated with previous fractures [70,71,72]. More recently, it was shown that cortical area and cortical bone mass by HR-pQCT analysis was independently of aBMD associated with fracture risk, suggesting that HR-pQCT may have additional value on fracture risk calculation [73]. Moreover, it was demonstrated that in individuals with identical BMD at distal radius area, differences in bone microarchitecture were observed by HR-pQCT due to differences in morphological and biomechanical differences, especially at the cortical level of bone [74, 75].
Although promising, an important point is that some clinical questions remain: up to now, we do not know what is the most clinically relevant and prognostically optimal region of interest to report in clinical practice. Furthermore, standardization of repetitive measurements of the same region of interest needs to be improved. Therefore, incorporation of this modern diagnostic tool is promising but remains challenging. In addition, HR-pQCT may have clinical relevance for certain rheumatic diseases like ankylosing spondylitis (AS) characterized by bone formation. In AS patients, suboptimal bone microarchitecture in both axial and peripheral skeleton (distal radius) was demonstrated [76] which is an important finding, as lumbar spine bone density measurement by DXA in AS patients may give an overestimation of BMD due to syndesmophytes or bamboo spine development. Recently, HR-pQCT imaging made it possible to monitor the healing process of fractures by a noninvasive manner, as this technique identified differences in cortices and trabeculae during a follow-up period of 2 years in the fractured and nonfractured site, whereas BMD was similar at both sites [77]. Moreover, a recent collaboration between different bone specialists showed that HR-pQCT imaging is a promising tool to define erosions in RA patients instead of using plane X-rays [78]. Another interesting observation is that HR-pQCT can measure changes in microarchitecture during treatment for a disease. This was illustrated in coeliac disease patients who underwent treatment with gluten-free diet, where it was observed that both BMD as microarchitectural parameters at the trabecular and cortical level improved during intervention [79]. Very recently, data were presented of an observational study in 589 French postmenopausal women with 135 incident fractures, who were followed over 9.4 years. The authors compared the structure fragility score (SFS) combining trabecular and cortical indices by HR-pQCT at the distal radius, with the BMD of the femoral neck and the FRAX® score: the predictive value seems to be comparable for all methods, with no additional value of the SFS on top of the BMD or the FRAX® [80].
Although these studies do not demonstrate that HR-pQCT is superior to DXA for fracture risk assessment, it clearly illustrates that new modern techniques may have additional value and may be promising in the future to have a better fracture risk assessment, especially in certain high-risk patient groups.
These concerns illustrate that the prevention of subsequent fractures after an initial fracture care needs to be improved. An important step forward may be intensification of collaboration between different medical specialists and general practitioners. The recommendations published by EULAR, in collaboration with the European Federation of National Associations of Orthopaedics and Traumatology (EFORT), for patients with fractures is a good example; in which ten recommendations are advocated for optimal fracture care of patients older than 50 years with a fragility fracture, to prevent subsequent fractures [81].
Challenge 6: Osteoporosis Treatment
The current treatments have one important feature in common; bone resorption and formation remain coupled [82]. This is both from a pharmacological and clinical point of view not optimal and results in unmet needs. First, antiresorptive treatments can only increase bone mineral density (BMD) to a certain extent as the decrease in osteoclast number and release of substances from the bone matrix subsequently impairs the recruitment of osteoblasts and de novo synthesis of new bone by the osteoblasts. Therefore, if the patient initially had very low bone mass, antiresorptive treatments will not be able to improve BMD enough to optimally prevent future fractures. In addition, if the patient also had deteriorated bone architecture, this will be improved, but not restored. Second, teriparatide stimulates osteoblasts and subsequently osteoclasts which limits the effect, and some patients with very low bone mass or suboptimal response to teriparatide are left with very low BMD after treatment. Third, only few studies have examined if the coupling of bone resorption and formation can be overcome by combining the therapies, and the unmet needs thereby may be improved.
Furthermore, while all antiresorptive and anabolic therapies increase spine and hip BMD, with the highest increases in the spine (Fig. 15.3), there is a discrepancy in how these therapeutic agents affect the skeleton (Table 15.4). As newer agents are studied, a trend in more efficacious BMD improvement with each new agent is apparent. Although many osteoporosis treatments have not been directly compared in head-to-head trials, the mechanisms of actions of these newer treatments often predict a superior efficacy in increasing BMD [83].
Areal BMD as determined by DXA declines with aging for different reasons. With aging, women with smaller femoral necks tend to increase bone area through an increase in cortical thickness by an increase in periosteal and endosteal bone formation. Since BMD may only decrease slightly but bone area increases more, the result is lower areal BMD as measured by DXA despite likely having little change in bone strength. In the case of women with larger femoral necks, the endosteal cortex undergoes excessive resorption without periosteal expansion resulting in a thinner cortex. The result is a lower BMC without significant change in bone area. The DXA areal BMD decreases and may result in a bone with less strength. (Quoted from: Choksi et al. [59] (under open access scheme))
All approved osteoporosis medications produce significant increases in spine and hip BMD as measured by DXA. The degree of BMD increase in the spine is likely a consequence of the greater surface area of trabecular-rich vertebral bodies on which the agents act. Twelve months of treatment with bisphosphonates increased BMD by approximately 4% in the spine and 2% in the hip as reported in the landmark FIT, VERT, BONE, and Horizon trials [84, 85, 96, 97]. The efficacy of daily, weekly, and monthly oral and yearly IV bisphosphonate medications are similar [98,99,100,101,102]. Compliance with oral bisphosphonates is a common factor in those patients who fail to respond to treatment [103,104,105]. Denosumab has even greater effects likely owing to its enhanced ability to suppress bone resorption [89]. Teriparatide, an anabolic agent, increases spine and hip BMD [59]. Abaloparatide, another recently available anabolic agent, also markedly increases spine and hip BMD [93].
Romosozumab, recently approved for treatment, is a humanized monoclonal antibody that targets sclerostin and has been reported to increase spine BMD approximately 13.5% and hip BMD approximately 6.5% after 12 months of treatment [94, 95].
Numerous published studies have reported the architectural changes in the skeleton with such agents using a variety of techniques that include HR-pQCT and QCT of in situ hip and spine as well as similar techniques of iliac crest bone biopsy samples. What has become clear is that they do not uniformly produce similar results (Table). Bisphosphonates increase cortical thickness primarily by decreasing the endosteal perimeter, partially through the filling in of previously excavated resorption pits at the endosteal surfaces. In addition, bisphosphonates also reduce cortical porosity and increase the amount of trabecular bone. Denosumab has similar effects and presumably to a higher degree owing to its improved fracture reduction compared to bisphosphonates [59].
Challenge 6: Patient Education
A plunge of around 50% from 2008 to 2012 in postmenopausal women using bisphosphonates was documented in the USA, the so-called crisis in osteoporosis [106, 107], (Fig. 15.4). The reason for the crisis is probably multifactorial: a common public awareness about devastating side effects as atypical femur fractures and osteonecrosis of the jaw is probably the most important. Suboptimal communication by physicians that are not capable of achieving a large fracture reduction by bisphosphonates (30–70% vertebral fracture reduction) versus the very small risk of severe side effects, around 1 in 100,000 bisphosphonate users, may exacerbate this issue. It is important to realize that effective drugs reduce fracture rates, but do not fully prevent the occurrence of fractures. Other explanations are lack of education to and engagement with osteoporosis by physicians, who may regard osteoporosis as a low medical priority, poor coordination of healthcare systems, inadequate access to diagnostic tools such as DXA and VFA, low adherence and compliance to anti-osteoporotic drugs, and the treatment gap [108]. Patient education can be stratified into phases subject to the patients’ age.
Crisis in osteoporosis treatment: prevalence of bisphosphonate use among females and males aged 55 years and older from 1996 to 2012. Data source: Medical Expenditure Panel Survey (MEPS). (Jha et al. [37]. To get permission: the author publishing with an STM Signatory Publisher. How can we proceed?)
How to Improve Peak Bone Mass?
In general, it can be stated that peak bone mass can be influenced not only negatively but also positively during young adult age. Therefore, it is important to realize that due to welfare, there is a change in lifestyle not only due to changes in nutrition and diet, but adolescents also seem to have a more sedentary lifestyle. Nowadays, youth has changed activities during leisure to a more sedentary relaxation with game consoles and other video games. This may be a difficult but necessary challenge as several studies showed that sedentary behavior in young children is associated with a lower bone density and ultimately lower peak bone mass [109, 110]. Recently, it could be demonstrated that more hours of watching television per day was associated with a lower BMD [111].
On the other hand, there is a chance to initiate intervention programs to increase peak bone mass for young adults, as it was observed that physical activity was associated with increased BMD levels [44]. In this study, it was shown that moderate activity, e.g., walking, cycling or exercises, for at least 4 h a week, and participation in recreational sports for at least 4 h a week or participation in hard training or sports competitions several times each week may increase BMD up to 11% and 13%, respectively in girls and boys aged 15–19 years [112]. Moreover, a retrospective cross-sectional study in prepubertal girls that observed global physical activity and not only activities related to sports was associated with a greater peak bone mass [113]. Nevertheless, although physical exercise may have a positive effect on BMD and peak bone mass, there are remaining questions about the optimal intensity and duration of therapy. Promising results were shown in a recent study by Mitchell and colleagues, as this study observed an improvement of bone after physical activity in children genetically predisposed to lower bone density [114]. Another point is how to change behavior from a sedentary type to a lifestyle with more physical exercise in large groups of young adults. Therefore, there is an urgent need for not only limiting the negative modifiable factors (low calcium, low vitamin D, smoking, and alcohol) but also investing in positive modifiable factors (mainly exercise) to aid in achieving optimal peak bone mass values in many individuals.
Proactive Non-pharmacological Measures to Prevent Fractures
Non-pharmacological supplements (including adequate calcium intake and vitamin D levels and exercise) have an important role to play in maintaining a healthy lifestyle, which is crucial for patients at high risk of sustaining a fracture, particularly, on the other hand, a nonhealthy lifestyle may have negative impact on BMD, bone quality as well as risk of falling [115].
Calcium and vitamin D and exercise: there is ample evidence showing a positive effect of healthy lifestyle elements (calcium, vitamin D, exercise) on the bone. In addition, the balance, though not yet fully proven, between a positive effect of a healthy lifestyle on bone, in combination with the absence of side effects, is attractive. An adequate calcium balance is an important factor in bone strength. Obviously, an extremely low dietary calcium intake, particularly in patients with malabsorption, for example, after bariatric surgery, may induce a strong tendency to serum hypocalcemia and a subsequent elevated bone resorption. This can be counteracted by oral calcium supplementation. On the other hand, earlier data have suggested that calcium supplementation might be associated with increased cardiovascular risk [116]. However, several other studies have not confirmed such assumed relationship between high dietary calcium intake and cardiovascular events [117, 118], leading to a continuing debate about whether calcium supplementation may lead to an elevated myocardial infarction risk. This is even more critical, as a study which included rheumatoid arthritis patients revealed that the risk of a cardiovascular event was elevated after a fragility fracture with a hazard ratio of 1.8 (95% confidence interval: 0.85–1.63) [119]. Another point is that when calcium is prescribed for osteoporotic patients with a low dietary calcium intake, it is difficult to estimate the dietary calcium intake with a simple questionnaire [120], and it is also difficult to assess the percentage of the calcium that has been absorbed in the intestine and which part of that is finally taken up and laid in the bone.
Another important modifiable risk factor is Vitamin D. Lower serum 25-hydroxy(OH) vitamin D levels have been reported to exert a negative impact on bone mineralization, consequently, on bone strength, and may also lead to muscular weakness and an increased risk of falling [121, 122]. Furthermore, low levels of serum 25(OH) vitamin D have been reported in patients who sustained a hip fracture [121]. Other studies have shown an association between low vitamin D levels and an increased risk of all-cause mortality, which could reflect a causal effect but could also result from less exposure to sunshine in elderly individuals with severe underlying diseases and comorbidities [123, 124].
In a large meta-analysis, it was shown that vitamin D supplementation (800 IU/day), in patients who received calcium supplementation, is associated with a 20% reduction in non-vertebral fractures and also with a 20% reduction in falls [125, 126]. In a randomized controlled trial observing different dosages of vitamin D, in >95% of patients, a serum level of 50 nmol/l was found after 6 months of treatment. However, it is not clear to which patients vitamin D supplementation should be prescribed: to all osteoporotic patients or only to those with a vitamin D level deficiency or insufficiency? Strikingly, very high-peak dosages of vitamin D (annually 500,000 IU/year) seem to be associated with increased fall risk and fracture risk [127, 128], while a dosage of 2000 IU per day was associated with a higher fall risk than with a dosage of 800 IU per day [129].
Smoking is another important non-pharmacological factor that has a negative effect on bone strength, mediated by direct negative impact on osteoblasts, upregulation of receptor activator of nuclear factor-kB ligand (RANKL), alterations in calciotropic hormones and decreased intestinal calcium absorption [130]. In addition, heavy smokers are often physically inactive and have a low body weight, which are also important risk factors for fractures. Thus, there is much evidence that stopping smoking and starting with a healthier lifestyle are crucial in those individuals regarded as heavy smokers; unfortunately it is not easy to stop smoking, particularly for those who are addicted to nicotine.
With regard to alcohol, more than four alcoholic beverages per day show deleterious impact on bone tissue, particularly a negative effect on bone formation [120]. However, even more than two units of alcohol per day increases the risk of osteoporotic and hip fractures, not only because of the negative effect on bone but also because of a negative effect on neuromuscular coordination and fall risk [131].
Other dietary-modifiable factors that influence bone mass and future fracture risk include other nutritional factors like protein intake and fruit. Previous studies have shown an incremental increase in bone mass with protein intake in young adults, and, recently, different diets have been identified to decrease fracture risk by improving bone strength [132]. Moreover, better milk intake improves bone mineral acquisition in adolescent girls [133]. On the other hand, ketogenic diets may cause a steady rate of bone loss, as measured in the spine, presumed to be because ketones are acidic; and so, keto diets can put people in what’s called a “chronic acidotic state.” These observations may implicate clinical relevance, although the main question is how much intake of proteins, fruit, or dairy is necessary in general; and the next question is whether these amounts can be applied to the individual patient in standard clinical practice.
Physical exercise, especially weight-bearing activity, has been reported to have beneficial effects on the skeleton in both adolescents [134,135,136] and the elderly. Many studies have shown that weight-bearing exercise can increase bone mineral density (BMD), particularly at a young age. Many previous studies have demonstrated an osteogenic effect of high impact and weight-bearing exercise on BMD using DXA [137,138,139]. In humans, the main stresses applied at the level of the calcaneus are ground reaction forces (GRF) as the heel strikes during locomotion [140]. Based on the GRF, swimming (GRF < 1 × body weight), dancing (GRF between 1 and 4 × body weight), and soccer (GRF > 4 × body weight) can be classified as low, moderate, and high impact exercise, respectively [141,142,143]. The relationship between loading magnitude and bone can be explained by the bone mechanostat theory proposed by Frost [144], who stated that exercise has a combined effect on bone modeling and remodeling, in that bone mass is increased by modeling and the added bone is retained by remodelling. Mechanical loading is also beneficial to bone structure. If a load is imposed, the bone will accommodate and undergo an alteration in mass, external geometry, and internal microarchitecture [108, 145].
Multifaceted Osteoporosis Group Education
In today’s healthcare system, patients are expected to play an active role and take responsibility for their own health [146, 147]. In light of this development, disease-specific group education (GE ) has become an integral and continuing part of healthcare provision [148] and a recommended way to encourage patients to become active participants in their own care [149,150,151]. Active participation includes making decisions about medical treatment and learning how to make lifestyle changes. The constant need to make health decisions is evident for patients with the chronic disease such as osteoporosis [152]. These patients face numerous self-care decisions, for example, whether to take medicine and to start doing weight-bearing exercises. Usually patients with osteoporosis consult their physician or general practitioner to discuss and evaluate the treatment within the first year after starting treatment. Afterward, treatment is evaluated every 2–3 years; hence, making decisions on how to manage osteoporosis in daily life relies heavily on the patient.
In the encounter between patients and physicians, decision-making is described as an iterative process including three steps: (1) information exchange, (2) deliberation about options, and (3) deciding on treatment to implement [153,154,155]. Research on patients with osteoporosis and decision support has shown that decision aids increase patients’ knowledge of options for managing osteoporosis and help them clarify their own preferences [156, 157]. A systematic review found that tools, especially those including reminders and education support, may reduce fracture risk by increased use of osteoporosis medicine leading to increase in bone mineral density (BMD) [158]. A study of patients with osteoporosis fractures and their decisions about taking prescribed osteoporosis medication revealed that regardless of whether the decision was easy or difficult to make, patients stated that the decision was not permanent as a number of circumstances could cause them to change it again [152]. Another study explored decision-making in the context of multifaceted group education for patients with osteoporosis. During group education, patients changed their understanding of lifestyle conducive to bone health, which had an impact on their decision-making. Patients sought clear recommendations on how to manage a life with osteoporosis and were offered information regarding a variety of ways to follow the recommendations. Teachers supported the patients by providing medical information and listening to patients’ experiences. Group education led to many healthy decisions on the part of the patients and to advice and directions on how the patients could implement decisions in the future to ensure bone health [159].
In conclusion, osteoporosis is a silent disease with increasing prevalence due to the global aging population. Decreased bone strength and bone quality is the hallmark of osteoporosis which leads to an increased risk of fragility fractures in elderly. This must be considered as a major health concern, as it has previously been established that fragility fracture has been associated with decreased quality of life due to increased disability and more frequent hospital admission, and, most importantly, osteoporotic fractures have been related to an augmented mortality risk. Although multiple national and international osteoporosis governing bodies have developed and updated several guidelines to aid clinical practice, there remain multiple unmet needs in the field of osteoporosis and fracture care. Tackling such challenges would definitely reflect on the patients’ management and fracture prevention.
References
Burge R, Dawson-Hughes B, Solomon DH. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22:465–75.
Bone health and osteoporosis: a report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Office of the Surgeon General, 2004; [cited January 3rd, 2020]. Available from: https://www.surgeongeneral.gov/library/.
US Department of Commerce, Economics and Statistics Administration, US Census Bureau The next four decades. The older population in the United States: 2010 to 2050. Population estimates and projections. Washington (DC): US Department of Commerce; [cited 3rd January 2020]. Available from: https://www.census.gov/prod/2010pubs/p25-1138.pdf.
Amin S, Achenbach SJ, Atkinson EJ, et al. Trends in fracture incidence: a population-based study over 20 years. J Bone Miner Res. 2014;29:581–9.
Leader D, Williams SA, Curtis JR, et al. Osteoporosis-related fracture events in 2015 in the US. Poster session presented at: AMCP Nexus; 2017. Oct 16–19; Dallas.
Gillespie CW, Morin PE. Osteoporosis-related health services utilization following first hip fracture among a cohort of privately-insured women in the United States, 2008–2014: an observational study. J Bone Miner Res. 2017;32:1052–61.
HEDIS® & performance management, 2018. Washington (DC): National Committee for Quality Assurance; [cited 3rd January 2020]. Available from: http://www.ncqa.org/HEDISQualityMeasurement/WhatisHEDIS.aspx.
Osteoporosis testing and management in older women. Washington (DC): National Committee for Quality Assurance; [cited 3rd January 2020]. Available from http://www.ncqa.org/report-cards/health-plans/state-of-health-care-quality/2017-table-of-contents/osteoporosis.
Weaver JP, Olsson K, Sadasivan R, et al. Reasons for not treating women with postmenopausal osteoporosis with prescription medications: physicians’ and patients’ perspectives. J Women's Health. 2017;26:1302–131.
NIH Consensus Development Panel on Osteoporosis Prevention. Diagnosis, and therapy osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785–95.
Greenspan SL, Myers ER, Maitland LA, Resnick NM, Hayes WC. Fall severity and bone mineral density as risk factors for hip fracture in ambulatory elderly. JAMA. 1994;271:128–33.
Garnero P, Hausherr E, Chapuy MC, Marcelli C, Grandjean H, Muller C, Cormier C, Breart G, Meunier PJ, Delmas PD. Markers of bone resorption predict hip fracture in elderly women: the EPIDOS prospective study. J Bone Miner Res. 1996;11:1531–8.
Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312(7041):1254.
Kanis JA, Johnell O, Oden A, Jonsson B, De Laet C, Dawson A. Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone. 2000;27(5):585.
Henry MJ, Pasco JA, Merriman EN, Yu Z, Sanders KM, Kotowicz MA, Nicholson GC. Fracture risk score and absolute risk of fracture. Radiology. 2011;259(2):495–501.
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19(4):385.
WHO Fracture Risk Assessment Tool (FRAX). http://www.shef.ac.uk/FRAX (Accessed on January 3rd, 2020).
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–82.
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, Eisman JA, Fujiwara S, Gluer C, Goltzman D, Hans D, Krieg MA, La Croix A, McCloskey E, Mellstrom D, Melton LJ 3rd, Pols H, Reeve J, Sanders K, Schott AM, Silman A, Torgerson D, van Staa T, Watts NB, Yoshimura N. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–46.
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK. International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res. 2002;17:1237–44.
Watts NB, Ettinger B, LeBoff MS. FRAX facts. J Bone Miner Res. 2009;24:975–9.
Browner WS. Predicting fracture risk: tougher than it looks. BoneKEy. 2007;4:226–30.
Melton LJ 3rd. History of the Rochester epidemiology project. Mayo Clin Proc. 1996;71:266–74.
Melton LJ 3rd, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM, Therneau TM, Leibson CL. Secular trends in hip fracture incidence and recurrence. Osteoporos Int. 2009;20:687–94.
Unnanuntana A, Gladnick BP, Donnelly E, Lane JM. The assessment of fracture risk. J Bone Joint Surg Am. 2010;92(3):743–53.
Leslie WD, Lix LM, Johansson H, et al. Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int. 2011;22:839.
Kanis JA, Johansson H, Oden A, McCloskey EV. Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int. 2011;22:809.
Schacter GI, Leslie WD. DXA-based measurements in diabetes: can they predict fracture risk? Calcif Tissue Int. 2017;100:150.
McCloskey EV, Harvey NC, Johansson H, Kanis JA. FRAX updates 2016. Curr Opin Rheumatol. 2016;28:433.
Donaldson MG, Palermo L, Schousboe JT, Ensrud KE, Hochberg MC, Cummings SR. FRAX and risk of vertebral fractures: the fracture intervention trial (FIT). J Bone Miner Res. 2009;24:1793–9.
Sample I. Patients denied osteoporosis drug. The Guardian 2009. https://www.theguardian.com/science/2009/sep/08/brittle-bone-osteoporosis-drug-treatment.
Tuck S. Elizabeth a little, Terry J Aspray, implications of guidelines for osteoporosis and its treatment. Age Ageing. 2018;47(3):334–9.
Compston J. NOGG and NICE: new guidelines and quality standards for osteoporosis. Maturitas. 2017;106:97–8. https://doi.org/10.1016/j.maturitas.2017.08.002.
Scottish Intercollegiate Guidelines Network (SIGN). SIGN 142: Management of Osteoporosis and the Prevention of Fragility Fractures. Edinburgh: Scottish Intercollegiate Guidelines Network, 2015 March 2015.
National Institute for Health and Care Excellence. Developing NICE Guidelines: The Manual [PMG20]. London: National Institute for, Health Clinical Excellence, 2017.
Harvey NC, McCloskey EV, Kanis JA, Compston J, Cooper C. Bisphosphonates in osteoporosis: NICE and easy? Lancet. 2017;390:2243–4.
Jha S, Wang Z, Laucis N. Trends in media reports, oral bisphosphonate prescriptions, and hip fractures 1996–2012: an ecological analysis. J Bone Miner Res. 2015;30:2179–87.
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359–81.
NOGG 2017. Clinical guideline for the prevention and treatment of osteoporosis. https://www.sheffield.ac.uk/NOGG/NOGG%20Guideline%202017.pdf (accessed on January 3rd, 2020).
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23–57.
Camacho PM, Petak SM, Binkley N, Clarke BL, Harris ST, Hurley DL, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Clinical Practice Guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2016. Endocr Pract. 2016;22(Suppl. 4):1–42.
Papaioannou A, Morin S, Cheung AM, et al. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182:1864–73.
Dawson-Hughes B, Tosteson AN, Melton LJ 3rd, Baim S, Favus MJ, Khosla S, Lindsay RL. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int. 2008;19:449–58.
Tosteson AN, Melton LJ 3rd, Dawson-Hughes B, Baim S, Favus MJ, Khosla S, Lindsay RL. Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int. 2008;19:437–47.
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A. Case finding for the management of osteoporosis with FRAX—assessment and intervention thresholds for the UK. Osteoporos Int. 2008;19:1395–408.
Bolland MJ, Grey A. Disparate outcomes from applying U.K. and U.S. Osteoporosis Treatment Guidelines. The Journal of Clinical Endocrinology & Metabolism. 2010;95(4):1856–60.
Donaldson LJ, Cook A, Thomson RG. Incidence of fractures in a geographically defined population. J Epidemiol Community Health. 1990;44:241–5.
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–82.
Trombetti A, Herrmann F, Hoffmeyer P, Schurch MA, Bonjour JP, Rizzoli R. Survival and potential years of life lost after hip fracture in men and age-matched women. Osteoporos Int. 2002;13:731–7.
Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD. Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res. 2005;20:1813–9.
Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman E, Hofman A, Uitterlinden AG, van Leeuwen JP, Pols HA. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone. 2004;34:195–202.
Ralston SH, Uitterlinden AG. Genetics of osteoporosis. Endocr Rev. 2010;31:629–62.
Almeida M, Laurent MR, Dubois V, Claessens F, O'Brien CA, Bouillon R, Vanderschueren D, Manolagas SC. Estrogens and androgens in skeletal physiology and pathophysiology. Physiol Rev. 2017;97:135–87.
Cauley JA. Defining ethnic and racial differences in osteoporosis and fragility fractures. Clin Orthop Relat Res. 2011;469:1891–9.
Nam HS, Kweon SS, Choi JS, Zmuda JM, Leung PC, Lui LY, Hill DD, Patrick AL, Cauley JA. Racial/ethnic differences in bone mineral density among older women. J Bone Miner Metab. 2013;31:190–8.
Third National Health and Nutrition Examination Survery (NHANES III), Bone Densitometry Manual. Arlington: National Osteoporosis Foundation. https://wwwn.cdc.gov/nchs/data/nhanes3/manuals/bone.pdf.
Carey JJ, Delaney MF. T-scores and Z-scores. Clin Rev Bone Miner Metab. 2010;8:113–21.
Zemel BS, Leonard MB, Kelly A, Lappe JM, Gilsanz V, Oberfield S, Mahboubi S, Shepherd JA, Hangartner TN, Frederick MM, et al. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J Clin Endocrinol Metab. 2010;95:1265–73.
Choksi P, Jepsen KJ, Clines GA. The challenges of diagnosing osteoporosis and the limitations of currently available tools. Clin Diabetes Endocrinol. 2018;4:12. https://doi.org/10.1186/s40842-018-0062-7.
Jepsen KJ, Kozminski A, Bigelow EM, Schlecht SH, Goulet RW, Harlow SD, Cauley JA, Karvonen-Gutierrez C. Femoral neck external size but not aBMD predicts structural and mass changes for women transitioning through menopause. J Bone Miner Res. 2017;32:1218–28.
Bultink IE, Lems WF. Performance of vertebral fracture assessment in addition to dual energy X-ray absorptiometry in patients with rheumatoid arthritis. Rheumatology (Oxford). 2014;53:775–6.
Mohammad A, Lohan D, Bergin D. The prevalence of vertebral fracture on vertebral fracture assessment imaging in a large cohort of patients with rheumatoid arthritis. Rheumatology (Oxford). 2014;53:821–7.
Lems WF. Clinical relevance of vertebral fractures. Ann Rheum Dis. 2007;66:2–4.
Siris ES, Genant HK, Laster AJ. Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int. 2007;18:761–70.
Lems WF, Dreinhofer KE, Bischoff-Ferrari H. EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis. 2017;76:802–10.
Van der Velde, RY, Bours, SPG, Wyers, CE. Effect of implementation of guidelines on assessment and diagnosis of vertebral fractures in patients older than 50 years with a recent non-vertebral fracture. Osteoporos Int. Epub ahead of print 26 July 2017. https://doi.org/10.1007/s00198-017-4147-4.
Rand T, Seidl G, Kainberger F. Impact of spinal degenerative changes on the evaluation of bone mineral density with dual energy X-ray absorptiometry (DXA). Calcif Tissue Int. 1997;60:430–3.
Frohn J, Wilken T, Falk S. Effect of aortic sclerosis on bone mineral measurements by dual-photon absorptiometry. J Nucl Med. 1991;32:259–62.
Harvey NC, Gluer CC, Binkley N. Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone. 2015;78:216–24.
Keyak JH, Sigurdsson S, Karlsdottir G. Male-female differences in the association between incident hip fracture and proximal femoral strength: a finite element analysis study. Bone. 2011;48:1239–45.
Kopperdahl DL, Aspelund T, Hoffmann PF. Assessment of incident spine and hip fractures in women and men using finite element analysis of CT scans. J Bone Miner Res. 2014;29:570–80.
Wang X, Sanyal A, Cawthon PM. Prediction of new clinical vertebral fractures in elderly men using finite element analysis of CT scans. J Bone Miner Res. 2012;27:808–16.
Ohlsson C, Sundh D, Wallerek A. Cortical bone area predicts incident fractures independently of areal bone mineral density in older men. J Clin Endocrinol Metab. 2017;102:516–24.
Kazakia GJ, Burghardt AJ, Link TM. Variations in morphological and biomechanical indices at the distal radius in subjects with identical BMD. J Biomech. 2011;44:257–66.
Nicks KM, Amin S, Atkinson EJ. Relationship of age to bone microstructure independent of areal bone mineral density. J Bone Miner Res. 2012;27:637–44.
Klingberg E, Lorentzon M, Gothlin J. Bone microarchitecture in ankylosing spondylitis and the association with bone mineral density, fractures, and syndesmophytes. Arthritis Res Ther. 2013;15:R179.
De Jong JJ, Heyer FL, Arts JJ. Fracture repair in the distal radius in postmenopausal women: a follow-up 2 years postfracture using HRpQCT. J Bone Miner Res. 2016;31:1114–22.
Barnabe C, Toepfer D, Marotte H. Definition for rheumatoid arthritis erosions imaged with high resolution peripheral quantitative computed tomography and inter-reader reliability for detection and measurement. J Rheumatol. 2016;43:1935–40.
Zanchetta MB, Longobardi V, Costa F. Impaired bone microarchitecture improves after one year on gluten-free diet: a prospective longitudinal HRpQCT study in women with celiac disease. J Bone Miner Res. 2017;32:135–42.
Boutroy S. Measurement of cortical and trabecular deterioration identifies postmenopausal women at imminent risk for fracture: the OFELY study. ASBMR. 2016;2016:Abstract 1076.
Lems WF, Raterman HG. Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther Adv Musculoskelet Dis. 2017:299–316.
Langdahl B, Ferrari S, Dempster DW. Bone modeling and remodeling: potential as therapeutic targets for the treatment of osteoporosis. Ther Adv Musculoskelet Dis. 2016;8:225–35.
Langdahl BL, Andersen JD. Treatment of osteoporosis: unmet needs and emerging solutions. J Bone Metab. 2018;25(3):133–40.
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture intervention trial research group. Lancet. 1996;348:1535–41.
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. vertebral efficacy with Risedronate therapy (VERT) study group. JAMA. 1999;282:1344–52.
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the fracture intervention trial. JAMA. 1998;280:2077–82.
Chesnut CH, Ettinger MP, Miller PD, Baylink DJ, Emkey R, Harris ST, Wasnich RD, Watts NB, Schimmer RC, Recker RR. Ibandronate produces significant, similar antifracture efficacy in north American and European women: new clinical findings from BONE. Curr Med Res Opin. 2005;21:391–401.
Park S. Choi KAB0854 The bmd change after ibandronate (BONVIVA®) treatment in osteopenic postmenopausal women. Ann Rheum Dis. 2017;76:1355.
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–65.
Fujiwara S, Hamaya E, Sato M, Graham-Clarke P, Flynn JA, Burge R. Systematic review of raloxifene in postmenopausal Japanese women with osteoporosis or low bone mass (osteopenia). Clin Interv Aging. 2014;9:1879–93.
Wells G, Tugwell P, Shea B, et al. Meta-analyses of therapies for postmenopausal osteoporosis. V. Meta-analysis of the efficacy of hormone replacement therapy in treating and preventing osteoporosis in postmenopausal women. Endocr Rev. 2002;23:529–39.
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–41.
Miller PD, Hattersley G, Riis BJ, Williams GC, Lau E, Russo LA, Alexandersen P, Zerbini CA, Hu MY, Harris AG, et al. Effect of Abaloparatide vs placebo on new vertebral fractures in postmenopausal women with osteoporosis: a randomized clinical trial. JAMA. 2016;316:722–33.
Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375:1532–43.
Saag KG, Petersen J, Brandi ML, Karaplis AC, Lorentzon M, Thomas T, Maddox J, Fan M, Meisner PD, Grauer A. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377:1417–27.
Chesnut CH 3rd, Skag A, Christiansen C, Recker R, Stakkestad JA, Hoiseth A, Felsenberg D, Huss H, Gilbride J, Schimmer RC, et al. Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res. 2004;19:1241–9.
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–22.
Rizzoli R, Greenspan SL, Bone G 3rd, Schnitzer TJ, Watts NB, Adami S, Foldes AJ, Roux C, Levine MA, Uebelhart B, et al. Two-year results of once-weekly administration of alendronate 70 mg for the treatment of postmenopausal osteoporosis. J Bone Miner Res. 2002;17:1988–96.
Brown JP, Kendler DL, McClung MR, Emkey RD, Adachi JD, Bolognese MA, Li Z, Balske A, Lindsay R. The efficacy and tolerability of risedronate once a week for the treatment of postmenopausal osteoporosis. Calcif Tissue Int. 2002;71:103–11.
Delmas PD, McClung MR, Zanchetta JR, Racewicz A, Roux C, Benhamou CL, Man Z, Eusebio RA, Beary JF, Burgio DE, et al. Efficacy and safety of risedronate 150 mg once a month in the treatment of postmenopausal osteoporosis. Bone. 2008;42:36–42.
Reginster JY, Adami S, Lakatos P, Greenwald M, Stepan JJ, Silverman SL, Christiansen C, Rowell L, Mairon N, Bonvoisin B, et al. Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study. Ann Rheum Dis. 2006;65:654.
Craig SJ, Youssef PP, Vaile JH, Sullivan L, Bleasel JF. Intravenous zoledronic acid and oral alendronate in patients with a low trauma fracture: experience from an osteoporosis clinic. Intern Med J. 2011;41:186–90.
Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, Silverman S. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc. 2006;81:1013–22.
Brookhart MA, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, Patrick AR, Mogun H, Solmon DH. Gaps in treatment among users of osteoporosis medications: the dynamics of noncompliance. Am J Med. 2007;120:251–6.
Patrick AR, Brookhart MA, Losina E, Schousboe JT, Cadarette SM, Mogun H, Solomon DH. The complex relation between bisphosphonate adherence and fracture reduction. J Clin Endocrinol Metab. 2010;95:3251–9.
Hospital Authority Dietetic Information Center. http://www.ha.org.hk/dic (accessed 21 May 2005).Google Scholar.
Ng YFG, Maitland ME. Relationship of kinetic demands of athletic training and knee joint laxity. Phys Ther Sport. 2001;2:66–70.
Yung PS, Lai YM, Tung PY, et al. Effects of weight bearing and non-weight bearing exercises on bone properties using calcaneal quantitative ultrasound. Br J Sports Med. 2005;39:547–51.
Sioen I, Michels N, Polfliet C. The influence of dairy consumption, sedentary behaviour and physical activity on bone mass in Flemish children: a cross-sectional study. BMC Public Health. 2015;15:717.
Herrmann D, Buck C, Sioen I. Impact of physical activity, sedentary behaviour and muscle strength on bone stiffness in 2–10-year-old children—cross-sectional results from the IDEFICS study. Int J Behav Nutr Phys Act. 2015;12:112.
McVeigh JA, Zhu K, Mountain J. Longitudinal trajectories of television watching across childhood and adolescence predict bone mass at age 20 years in the Raine study. J Bone Miner Res. 2016;31:2032–40.
Winther A, Dennison E, Ahmed LA. The Tromso Study: fit futures: a study of Norwegian adolescents’ lifestyle and bone health. Arch Osteoporos. 2014;9:185.
Pasqualini L, Leli C, Ministrini S. Relationships between global physical activity and bone mineral density in a group of male and female students. J Sports Med Phys Fitness. 2017;57:238–43.
Mitchell JA, Chesi A, Elci O. Physical activity benefits the skeleton of children genetically predisposed to lower bone density in adulthood. J Bone Miner Res. 2016;31:1504–12.
Body JJ, Bergmann P, Boonen S. Non-pharmacological management of osteoporosis: a consensus of the Belgian Bone Club. Osteoporos Int. 2011;22:2769–88.
Bolland MJ, Avenell A, Baron JA. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341 https://doi.org/10.1136/bmj.c3691.
Lewis JR, Calver J, Zhu K. Calcium supplementation and the risks of atherosclerotic vascular disease in older women: results of a 5-year RCT and a 4.5-year follow-up. J Bone Miner Res. 2011;26:35–41.
Bauer DC. The calcium supplement controversy: now what? J Bone Miner Res. 2014;29:531–3.
Ni MO, Crowson CS, Gabriel SE. Fragility fractures are associated with an increased risk for cardiovascular events in women and men with rheumatoid arthritis: a population-based study. J Rheumatol. 2017;44:558–64.
Rasch LA, de van der Schueren MA, van Tuyl LH. Content validity of a short calcium intake list to estimate daily dietary calcium intake of patients with osteoporosis. Calcif Tissue Int. 2017;100:271–7.
Rizzoli R, Boonen S, Brandi ML. Vitamin D supplementation in elderly or postmenopausal women: a 2013 update of the 2008 recommendations from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Curr Med Res Opin. 2013;29:305–13.
Bruyere O, Cavalier E, Souberbielle JC. Effects of vitamin D in the elderly population: current status and perspectives. Arch Public Health. 2014;72:32.
Gaksch M, Jorde R, Grimnes G. Vitamin D and mortality: individual participant data meta-analysis of standardized 25-hydroxyvitamin D in 26916 individuals from a European consortium. PLoS One. 2017;12:e0170791.
Abrahamsen B. The calcium and vitamin D controversy. Ther Adv Musculoskelet Dis. 2017;9:107–14.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339 https://doi.org/10.1136/bmj.b3692.
Bischoff-Ferrari HA, Willett WC, Orav EJ. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;367:40–9.
Gallagher JC, Sai A, Templin T. Dose response to vitamin D supplementation in postmenopausal women: a randomized trial. Ann Intern Med. 2012;156:425–37.
Sanders KM, Stuart AL, Williamson EJ. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303:1815–22.
Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ. Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med. 2016;176:175–83.
Yoon V, Maalouf NM, Sakhaee K. The effects of smoking on bone metabolism. Osteoporos Int. 2012;23:2081–92.
Berg KM, Kunins HV, Jackson JL. Association between alcohol consumption and both osteoporotic fracture and bone density. Am J Med. 2008;121:406–18.
De Jonge EA, Kiefte-de Jong JC, Hofman A. Dietary patterns explaining differences in bone mineral density and hip structure in the elderly: the Rotterdam Study. Am J Clin Nutr. 2017;105:203–11.
Cadogan J, Eastell R, Jones N. Milk intake and bone mineral acquisition in adolescent girls: randomised, controlled intervention trial. BMJ. 1997;315:1255–60.
Snow-Harter C, Bousxein MS, Lewis BT, et al. Effects of resistance and endurance exercise on bone mineral status of young women: a randomized exercise intervention trial. J Bone Miner Res. 1992;7:761–9.
Scerpella TA, Davenport M, Morganti CM, et al. Dose related association of impact activity and bone mineral density in pre-pubertal girls. Calcif Tissue Int. 2003;72(1):24–31.
Hara S, Yanagi H, Amagai H, et al. Effect of physical activity during teenage years, based on type of sport and duration of exercise, on bone mineral density of young, premenopausal Japanese women. Calcif Tissue Int. 2001;68(1):23–30.
Duncan CS, Blimike CJR, Cowell CT, et al. Bone mineral density in adolescent female athletes: relationship to exercise type and muscle strength. Med Sci Sports Exerc. 2002;343:286–94.
Etherington J, Harris PA, Nandra D, et al. The effect of weight-bearing exercise on bone mineral density: a study of female ex-elite athletes and the general population. J Bone Miner Res. 1996;11(9):1333–8.
Alfredson H, Nordstrom P, Lorentzon R. Total and regional bone mass in female soccer players. Calcif Tissue Int. 1996;59:439–42.
Mayoux-Benhamou MA, Roux C, Rabourdin JP, et al. Plantar flexion force is related to calcaneus bone ultrasonic parameters in postmenopausal women. Calcif Tissue Int. 1998;62:462–4. CrossRefPubMedWeb of ScienceGoogle Scholar.
Bakker I, Twisk JW, Mechelen WV, et al. Ten-year longitudinal relationship between physical activity and lumbar bone mass in (young) adults. J Bone Miner Res. 2003;18:325–32. CrossRefPubMedWeb of ScienceGoogle Scholar.
Rubin CT, Lanyon LE. Regulation of bone mass by mechanical strain magnitude. Calcif Tissue Int 1985;37:411–417 . CrossRefPubMedWeb of ScienceGoogle Scholar.
Messenger N, Scott S, McNaught-Davis P. Can the effects of exercise on bone quality be detected using the CUBA clinical ultrasound system? Br J Sports Med. 1998;32:162–6.
Frost HM. Why do bone strength and “mass” of aging adults become unresponsive to vigorous exercise? Insights of the Utah paradigm. J Bone Miner Metab. 1999;17:90–7. CrossRefPubMedWeb of ScienceGoogle Scholar.
Marcus R. Mechanisms of exercise effects on bone. In: Bilezikian JP, editor. Principles of bone biology. San Diego: Academic Press; 1996. p. 1135–43.
Coulter A. Engaging patients in healthcare. Milton Keynes: Open University Press; 2011.
Nettleton S. The sociology of health and illness. 3rd ed. Cambridge, UK: Polity; 2013.
WHO, Therapeutic Patient Education. Continuing education Programmes for health care providers in the field of prevention of chronic diseases, 1998.
Coulter A, Ellins J. Patient-focused interventions—a review of the evidence, vol. 1, Health foundation. 2006. The Health Foundation. https://www.health.org.uk/sites/default/files/PatientFocusedInterventions_ReviewOfTheEvidence.pdf.
Coster S, Norman I. Cochrane reviews of educational and self-management interventions to guide nursing practice: a review. Int J Nurs Stud. 2009;46(4):508–28. View at Publisher.
Schöpf AC, Ullrich A, Nagl M, Farin E. Group health education in inpatient rehabilitation: patients' role perceptions. Health Educ J. 2016;75(3):289–305.
Sale JEM, Gignac MA, Hawker G, et al. Decision to take osteoporosis medication in patients who have had a fracture and are ‘high’ risk for future fracture: a qualitative study. BMC Musculoskelet Disord. 2011;12:92.
Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49(5):651–61.
Murray E, Charles C, Gafni A. Shared decision-making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient Educ Couns. 2006;62(2):205–11.
Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7.
Montori VM, Shah ND, Pencille LJ, et al. Use of a decision aid to improve treatment decisions in osteoporosis: the osteoporosis choice randomized trial. Am J Med. 2011;124(6):549–56.
Cranney A, O'Connor AM, Jacobsen MJ, et al. Development and pilot testing of a decision aid for postmenopausal women with osteoporosis. Patient Educ Couns. 2002;47(3):245–55.
Kastner M, Straus SE. Clinical decision support tools for osteoporosis disease management: a systematic review of randomized controlled trials. J Gen Intern Med. 2008;23(12):2095–105.
Jensen AL, Wind G, Langdahl BL, Lomborg K. The impact of multifaceted osteoporosis group education on patients’ decision-making regarding treatment options and lifestyle changes. J Osteoporosis. 2018, 2018. 9703602:10. https://doi.org/10.1155/2018/9703602.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
El Miedany, Y. (2022). Unmet Needs and Challenges in Osteoporosis. In: El Miedany, Y. (eds) New Horizons in Osteoporosis Management. Springer, Cham. https://doi.org/10.1007/978-3-030-87950-1_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-87950-1_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87949-5
Online ISBN: 978-3-030-87950-1
eBook Packages: MedicineMedicine (R0)