Abstract
Telehealth refers to the use of electronic media to support a broad range of remote services such as patient care, education, and monitoring. Drawing upon the “design thinking” framework, a holistic approach to telehealth service design would be one that takes into consideration the multiple, interdependent dimensions of telehealth services, including processes, user-experience, and sustainability. The information technology infrastructure library (ITIL) is a well-known framework of best practices in IT service management. However, as a stand-alone resource, it is limited in being able to provide a meaningful set of strategies for telehealth service design and implementation for clinicians and healthcare leaders. The ITIL framework emanated from an industry-based approach to developing best practices for IT service management. This paper takes an organizational theory-based approach to identifying strategies for telehealth service design and implementation. These strategies are then integrated with practices put forth by the ITIL framework, to develop a “holistic framework” of strategies and best practices for telehealth service design and implementation, intended to be meaningful to clinicians, healthcare leaders, and IT service managers alike. The primary purpose of this paper is to integrate theory-based “design thinking” and “consolidated framework for implementation research (CFIR)” frameworks, with the existing industry-based ITIL framework, to develop a holistic framework of strategies and best practices for telehealth service design and implementation. A supplemental purpose is to apply the holistic framework to cases of success and failure in telehealth services, to discuss implications for practice and future research.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
16.1 Introduction
Telehealth refers to the use of electronic media to support a broad range of remote services such as patient care, education, and monitoring (Schwamm, 2014). It helps to overcome two barriers that patients face when seeking health care: distance and time. Telehealth has been found to deliver a range of benefits, including improved access to healthcare, more timely interactions between providers and patients, leading to improved continuity of care, and more efficient use of providers’ time, to name a few. Proponents of telehealth have argued that it has the potential to transform healthcare delivery by reducing costs and increasing quality of care and patient satisfaction (Schwamm, 2014; Taylor, 2013).
In the United States, although telehealth was a “hot topic” before the COVID-19 pandemic, its use was far from widespread and was limited to certain medical specialties (Adler-Milstein et al., 2014; Andrus, 2017; Kane & Gillis, 2018; Lin et al., 2018; Schwamm, 2014). With the arrival of the pandemic, however, there has been a massive acceleration in the use of telehealth, not only because of physical (social) distancing requirements, but also due to the temporary removal of regulatory barriers to telehealth use. Nevertheless, the questions that do not yet have definitive answers are: Is telehealth here to stay? Will providers find it to be an effective method for providing care? Will patients prefer it over traditional in-person visits? Will policy and regulatory barriers to telehealth use be permanently lifted? (Perry, 2020; Shachar et al., 2020). Although there is much uncertainty about the future of telehealth in the post-pandemic era, one point of consensus is that the elimination of policy-level barriers to telehealth use by itself, would not suffice to enable widespread, sustainable use of telehealth services. Instead, the literature has emphasized the need for healthcare organizations and providers to make concerted efforts to design and implement telehealth services for successful and sustainable use (Failed, 2014; Hebert, 2001; Kho et al., 2020; Moehr et al., 2006; Schwamm, 2014).
Purpose of this Chapter
Drawing upon the “design thinking” or “systems thinking” framework, a holistic approach to telehealth service design would be one that takes into consideration the multiple, interdependent dimensions of telehealth services, including processes, user-experience, and sustainability (Dovigi et al., 2020; Taylor, 2013). Likewise, drawing upon the “consolidated framework for implementation research (CFIR)” a holistic approach to telehealth service implementation would be one that involves extensive planning and stakeholder engagement BEFORE service design, and substantial investment in execution, reflection, and evaluation, AFTER service design (Bobinet & Petito, 2020).
The information technology infrastructure library (ITIL) is a well-known framework of best practices in IT service management (Damschroder et al., 2009; Greene, 2020; White & Greiner, 2019). However, as a stand-alone resource, it is limited in being able to provide a meaningful set of strategies for telehealth service design and implementation for clinicians and healthcare leaders (as discussed in the next section). In other words, there is a gap in the literature with respect to a “holistic framework” of strategies and best practices for the design and implementation of telehealth services, which could be meaningful to clinicians, healthcare leaders, and IT service managers alike. This paper seeks to address this gap.
As discussed in the next section, the ITIL framework emanated from an industry-based approach to identifying best practices for IT service management (Damschroder et al., 2009; White & Greiner, 2019). This paper takes an organizational theory-based approach to developing strategies for telehealth service design and implementation. These strategies are then integrated with practices put forth by the existing ITIL framework, to develop a holistic framework of strategies and best practices for telehealth service design and implementation.
In summary, the primary purpose of this paper is to integrate theory-based “design thinking” and “CFIR” frameworks, with the existing industry-based ITIL framework, to develop a holistic framework of strategies and best practices for telehealth service design and implementation. A supplemental purpose is to apply the holistic framework to cases of success and failure in telehealth services and discuss implications for future research and practice in telehealth service design and implementation.
16.2 Limitations of the ITIL Framework in Informing Telehealth Service Design and Implementation
In the 1980s, the U.K. Government’s Central Computer and Telecommunication Agency developed the information technology infrastructure library (ITIL) in an effort to improve standards for IT service quality (Damschroder et al., 2009; Greene (n. d.), 2020; White & Greiner, 2019). Since then, the ITIL has not only gained international popularity but has also evolved into a widely-used framework of best practices for IT service management. Version 3 of ITIL (released in 2007) included a detailed description of practices arranged along the service lifecycle: service strategy, service design, service transition, service operation, and continual service improvement. Version 3 also described itself as a three-dimension model of (1) people, (2) process, and (3) technology, while version 4 (released in 2019) included a fourth dimension of (4) partners and supplies in an effort to market itself as a comprehensive framework of best practices for IT service management (Greene, 2020).
On the face of it therefore, ITIL may come across as the “ultimate solution” for designing and implementing any IT-enabled service including telehealth services. However, despite its popularity in the IT industry, the ITIL by itself is not designed to be meaningful to clinicians and healthcare managers looking to get started with a new telehealth service and establish a successful and sustainable telehealth infrastructure. Having originated in the IT industry, the ITIL utilizes considerable industry-level jargon and terminology to describe practices in each service lifecycle stage (Greene, 2009). For example, the stage of service design includes jargon-based practices like service catalog management, service continuity management, etc., which may be meaningful to an IT service manager but not necessarily to a clinician or healthcare leader (Wiki, 2020). On the other hand, applying “design thinking” theory to telehealth service design suggests that the first step to designing an effective telehealth service is to view the service in the context of the clinician-patient interaction, i.e., the social system in which it is embedded, which in turn is a broad strategy that would be meaningful to clinicians and healthcare leaders (Taylor, 2013; Wiki 2020).
Similarly, although ITIL discusses steps to be followed BEFORE and AFTER the service design stage to ensure successful service implementation, it utilizes considerable IT jargon to describe the implementation steps. For example, terms like service portfolio management and business relationship management are used to describe practices in the lifecycle stage of service strategy (which comes BEFORE service design) (Taylor, 2013; Wiki 2020). On the other hand, applying the “CFIR” framework to telehealth service implementation suggests that service design must be preceded by a planning and engagement phase that takes into consideration characteristics of the intervention (e.g., telehealth technology), the inner and outer settings of the healthcare organization, and characteristics of individuals being impacted, to effectively engage a multidisciplinary and inter-sectoral set of stakeholders (e.g., providers, patients, IT vendors, economists, and policymakers) in telehealth service implementation (Bobinet & Petito, 2020). This in turn is a broad strategy that clinicians and healthcare leaders would be able to relate to. In other words, integrating theory-based frameworks like “design thinking” and “CFIR” with the industry-based ITIL framework has the potential to generate a holistic framework of strategies and best practices for the design and implementation of telehealth services, that is, relevant and meaningful to clinicians, healthcare leaders, and IT service managers alike.
16.3 Dimensions of Telehealth Services
The first step toward developing a holistic framework of strategies and best practices for telehealth service design and implementation would be to understand the multiple, interdependent dimensions of telehealth services: (1) processes; (2) user-experience; and (3) sustainability (Dovigi et al., 2020; Kho et al., 2020; Taylor, 2013; Wiki 2020).
-
1.
Processes: When telehealth is used to artificially eliminate distance between the provider and patient, it changes the processes associated with provider-patient interactions. However, the design of telehealth services cannot simply be a linear sum of processes changes. Instead, many process changes are interdependent one change may impact other parts of the solution. For example, process changes may necessitate risk assessments to ensure that they do not compromise quality of care (Tang et al., 2006; Taylor, 2013). Process changes may also create additional requirements for clinician, staff, and patient training to support the transition to a new model of care. In some instances, such requirements may add significantly to the costs, which may have the potential to compromise the proposed process and erode the value of telehealth services. Importantly, process changes would need to be supported by integral mechanisms to collect data to demonstrate improvements to care and outcomes. This would be essential for making a case for sustainability of process changes (Wiki 2020; Tang et al., 2006). In summary, process changes resulting from introduction of telehealth, demand a more holistic approach to service design.
-
2.
User-experience: Telehealth service design needs to be directly responsive to the needs, expectations, and experience of its users, including providers and patients (Dovigi et al., 2020; Wiki (n. d. e) 2020). A telehealth encounter must be accessible, reliable, convenient, efficient, and must accommodate sudden modifications. It should integrate with the patient’s preferred electronic media, such as messaging or e-mail, with formal records and updates that could be saved and retrieved. It should push or pull appropriate information at the right times in the care pathway and provide information at the most appropriate point in the encounter (e.g., preregistration). Concurrently, the needs and expectations of providers must be taken into consideration, e.g., their guidelines for which symptoms and conditions can and cannot be managed virtually, their need for real-time access to patient data, their checklist of considerations for safety and quality, support for the regulatory restrictions they face in clinical practice, etc. Patients in turn would expect to have clear instructions how to prepare for the telehealth encounter and how they could provide feedback, e.g., through a post-visit survey. These types of “usability” considerations are typically identified when developing a prototype of the telehealth service design (Dovigi et al., 2020; Taylor, 2013).
-
3.
Sustainability: Since telehealth changes the provider-patient interaction, it has been argued that success and sustainability of a new telehealth service ultimately depends on how the new telehealth offering changes the distinct value proposition for each key stakeholder (e.g., clinicians, patients, and administrators). In other words, it has been argued that success and sustainability of telehealth services depends far more on managing the provider and patient’s expectations and behavior than on technology (Taylor, 2013; Wiki 2020; Tang et al., 2006). However, technology considerations in telehealth service design become most relevant when planning for the sustainability of the telehealth service. New telehealth services become self-sustaining when they effectively transition their demands for resources from project funding to “business as usual” operations. This transition needs to be an integral part of the scope of telehealth service design. Early attention to design considerations such as interoperability has potential to increase sustainability in the face of inevitable change. Similarly, integration with upstream and downstream systems such as scheduling systems, billing and administration, record keeping, and planned clinic sessions also has potential to boost sustainability. Importantly, integrating performance indicators into telehealth projects from the outset will ensure that each project is designed to meet specific measurable objectives (Brown, 2008; Senge, 1992; Tang et al., 2006). This in turn can help to provide a quantifiable basis for defining the effectiveness of telehealth services for future funding and investment, to satisfy key stakeholders.
16.4 Identifying Effective Strategies and Practices for Telehealth Service Design
The above discussion related to the dimensions of telehealth services helps to understand that telehealth service design requires a comprehensive approach to working with participants (e.g., providers and patients), to identify the key forces and factors at play, and address them through a holistic design solution. Some telehealth projects may effectively design “parts” of a new service, however, such design may not sufficiently account for the role of other critical forces in the problem context (Brown, 2008; Senge, 1992; Tang et al., 2006; Taylor, 2013). A holistic design solution for telehealth services, would seek to resolve all of the significant forces in the problem’s context to create a new balance, requiring designers of telehealth services to take a “systems” view of the context for provider-patient interaction (Wiki, 2020; Tang et al., 2006). The need for a holistic design solution in turn provides the rationale for a “systems thinking” or “design thinking” approach to developing strategies for the design of telehealth services.
“Design thinking” has been described as “a discipline that seeks to match people’s needs with what is technologically feasible and what a viable business strategy can convert into customer value and market opportunity.” (Tang et al., 2006; Taylor, 2013). It is similar to “systems thinking” in that, it recognizes the role of the target for design (i.e., service) within a larger socio-technical system. The approach involves extensive in-situ observation and end user participation to identify potential interventions, and often employs prototyping and mock-ups to rapidly evaluate these in context. Such an iterative approach in turn has potential to highlight implications of the proposed intervention to all stakeholders and deliver a solution that is co-designed and has broad buy-in through end user participation. The backbone of this process, therefore, is the understanding of end user behavior, including the needs and motivations of end users. Service designers could obtain this information through a variety of fact-finding techniques, including ethnography, end user interviews, or shadowing of end users. In summary, such an approach to designing telehealth service focuses design effort on the actual service offered by the clinician/provider to the patient, and provides a key perspective on user experience (Tang et al., 2006; Taylor, 2013).
Since the understanding of end user behavior is integral to the “design thinking” approach, the literature has discussed the importance of integrating design thinking with behavioral economics, the science of individual decision-making in a variety of everyday settings (Dyk, 2014; Singh et al., 2010; Thaler & Sunstein, 2009). Studies in this field have indicated that people make more decisions reactively (in-the-moment) than analytically, drawing on arbitrary factors such as product packaging, convenience of access, simplicity, or brand familiarity, and as the primary basis of decisions or choices (Thaler & Sunstein, 2009). The literature in turn, has discussed how service designers could leverage these insights about end user behavior to create opportunities for “nudging” or selecting defaults to achieve desired behaviors, i.e., to influence choices for both individual and common good. Examples of “nudging” include setting savings plan enrollment and risk profile defaults to “on” and placing healthy food options at eye level. From the perspective of telehealth service design therefore, behavioral economics or “nudging” can offer useful insights into low-friction design of services, particularly in situations where complexity is not avoidable at the user interface (Singh et al., 2010).
The above discussion provides insights into strategies for telehealth service design that could be highly relevant to clinicians and healthcare leaders (Taylor, 2013). A holistic approach to designing telehealth services would incorporate the following elements based on principles of “design thinking:”
-
(1)
It would begin with in-situ observation, to capture the nuances of clinical practice, clinician-patient interaction, and patient preferences.
-
(2)
It would be based on the principle of co-design in which clinicians and patients (end users) work together with service designers to determine the objectives and develop the service design; a co-design approach in turn would enable clinicians to contribute expert insights and patients to offer practical suggestions, while designers facilitate the process but do not dictate the results.
-
(3)
It would be highly iterative, recognizing that insight must be vigorously tested and refined and that a viable telehealth service must resolve complex forces in many dimensions at once.
-
(4)
It would recognize the socio-technical system in which the clinician-patient interaction occurs and would pursue the boundaries of the service design until the new service could be justified in the context of a complete and balanced system.
-
(5)
It would seek to stabilize patient behaviors rather than enforce process compliance. It would incorporate an awareness of the different techniques in telehealth services for influencing productive choices through defaults that act in the interest of both parties, and the provision of “just enough” information to efficiently support the clinician-patient interaction at each step.
Each of the aforementioned strategies in turn, represents a rich source of techniques for telehealth service design. To come full circle with the design process, it is essential to discover which techniques are most relevant and how they could be structured into a methodology, that is, practical and accessible to clinicians and patients (Taylor, 2013). The strategies for telehealth service design (discussed above) in turn could be synergized with existing ITIL “best practices” for service design, to develop a comprehensive set of strategies and best practices for telehealth service design, for use by clinicians, healthcare leaders, and IT service managers alike. The ITIL framework includes the following 11 best practices for service design: (1) Design coordination, (2) service catalog management (SCM), (3) service level management (SLM), (4) risk management, (5) capacity management, (6) availability management, (7) IT service continuity management (ITSCM), (8) information security management, (9) compliance management, (10) architecture management, and (11) supplier management (11). Each of these IT service design best practices could integrated into the overall strategy for telehealth service design informed by principles of “design thinking” and behavioral economics.
16.5 Identifying Effective Strategies and Practices for Telehealth service Implementation
The service lifecycle stages put forth by ITIL help to understand that the service implementation cycle begins well BEFORE service design (with service strategy) and extends to well AFTER service design, to service transition, service execution, and continuous service improvement. The existing telehealth literature has consistently emphasized the importance of recognizing the complexity in implementing telehealth services (Taylor, 2013; Yellowlees, 2005). In addition to the need to consider multiple interdependent dimensions (of processes, user-experience, and sustainability), by definition, telehealth services are delivered over a distance and often span multiple organizational entities with varying cultures, practices, and business models. Correspondingly, the design and implementation of telehealth services often involves the engagement of stakeholders from a variety of disciplines from both inner and outer settings of the organization. In view of this complexity, a considerable portion of the telehealth literature has paid attention to determinants of failure or success of telehealth implementation initiatives (Almathami et al., 2020; Attewell, 1992; Batsis et al., 2020; Broens et al., 2014; Buchachi & Pakenham-Walsh, 2007; Christie et al., 2018; Cilliers & Flowerday, 2013; Damschroder et al., 2009; Dyk, 2014; Finch et al., 2006; Foster & Sethares, 2014; Garavand et al., 2019; Hadjistavropoulos et al., 2017; Khoja et al., 2007a, 2007b, 2013; Koivunen & Saranto, 2018; Pelletier-Fleury et al., 1997; Tanriverdi & Iacono August, 1998; Warner et al., 2018).
Within the last decade, van Dyk (2014) conducted a comprehensive review to identify and compare existing frameworks on telehealth service implementation to identify common themes and areas for future development (Yellowlees, 2005). A total of nine frameworks related to telehealth use and implementation were reviewed, including: (1) barriers to the diffusion of telemedicine, which emphasizes technical, behavioral, economic, and organizational barriers (Khoja et al., 2007a); (2) telehealth readiness assessment tools, which emphasize core (planning), technological, learning, societal, and policy readiness (Cilliers & Flowerday, 2013; Khoja et al., 2007b); (3) telehealth applications of the unified theory of acceptance and use of technology (UTAUT), which describes the interaction among several variables influencing technology acceptance, including perceived importance of standardization (Finch et al., 2006; Garavand et al., 2019); (4) seven core principles for the successful implementation of telemedicine (discussed earlier) (Broens et al., 2020); (5) lessons in telemedicine service innovation, which identifies factors contributing to telehealth success, including the policy context, evidence gathering, outcomes monitoring, perceived benefit, reconfiguring services, professional roles, and willingness to cross boundaries (Buchachi & Pakenham-Walsh, 2007); (6) framework for assessing health system challenges to scaling up for telehealth, which includes consideration for policy, organizational, technological, and financial challenges (Buchachi & Pakenham-Walsh, 2007; Cilliers & Flowerday, 2013); (7) comprehensive model for the evaluation of telemedicine, which considers several issues related to telehealth implementation, including cost of education, quality of clinical services, community access to services, among others (Pelletier-Fleury et al., 1997); (8) layered telemedicine implementation model, which identifies determinants of success associated with each lifecycle phase of telemedicine (Khoja et al., 2007b); and (9) the Khoja-Durrani-Scott (KDS) evaluation framework, which also considers telehealth lifecycle stages and incorporates various themes of evaluation, including readiness and change, policy, technological, behavioral, economic, and ethical (Damschroder et al., 2009). Overall, the review by van Dyk (2014) concluded that a holistic approach is needed to telehealth implementation, which includes consideration for organizational structures, change management, technology, economic feasibility, societal impacts, perceptions, user-friendliness, evidence and evaluation, and policy and legislation (Attewell, 1992).
In more recent years, the consolidated framework for implementation research (CFIR) (Bobinet & Petito, 2020). has been leveraged to guide telehealth service implementation initiatives (Bardosh et al., 2017; Batsis et al., 2020; Hadjistavropoulos et al., 2017; Warner et al., 2018; Weinstein et al., 2014). Since its introduction in 2009, the CFIR has gained considerable popularity and recognition as an influential theoretical framework to inform both “implementation science” and “implementation strategy.” (Bobinet & Petito, 2020). The CFIR comprises five major domains (characteristics of the intervention, the outer setting, the inner setting, characteristics of the individuals involved, and the process by which implementation is accomplished). Each domain in turn is mapped to an array of constructs informed by existing implementation theories and conceptual models. The five domains (and constructs) in the CFIR in turn interact in rich and complex ways to influence implementation effectiveness.
To elaborate, the CFIR domain of intervention characteristics has been mapped to the following constructs: (1) intervention source, (2) evidence strength and quality, (3) relative advantage, (4) adaptability, (5) trialabilty, (6) complexity, (7) design and packaging, and (8) cost. The domain of outer setting has been mapped to the following constructs: (1) patients’ needs and resources; (2) cosmopolitanism (or degree of networking with external organizations); (3) peer pressure; and (4) external policies and incentives. The domain of inner setting has been mapped to the following constructs: (1) structural characteristics, (2) networks and communication, (3) culture, including norms and values of an organization, and (4) implementation climate or the absorptive capacity for change. Six sub-constructs contribute to a positive implementation climate for an intervention: readiness for implementation, compatibility, relative priority, organizational incentives and rewards, goals and feedback, and learning climate. Readiness for implementation in turn includes three sub-constructs, leadership engagement, available resources, and access to information and knowledge. The domain of individual characteristics has been mapped to the following constructs: (1) knowledge and beliefs about the intervention, (2) individual self-efficacy; (3) individual stage of change, (4) individual identification with organization, and 5) other personal attributes. Lastly, within the domain of implementation process, the CFIR describes four essential activities of that are common across organizational change models: planning, engaging, executing, and reflecting and evaluating (Bobinet & Petito, 2020).
Each of the core activities associated with the CFIR implementation process in turn could be mapped to the PRE-service design and POST-service design stages of the ITIL service lifecycle. For example, the activities of “planning” and “engaging” in the CFIR domain of implementation process could be mapped to the service strategy phase of the ITIL service lifecycle (PRE-service design). Likewise, the CFIR activity of “executing” could be mapped to the service transition and service operation phases of the ITIL service lifecycle (POST-service design), while the CFIR activity of “reflecting and evaluating” in the domain of implementation process could be mapped to the continual service improvement phase of the ITIL service lifecycle. Overall, the CFIR is a pragmatic meta-theoretical framework with a comprehensive taxonomy of domains and constructs that could be used to guide formative evaluation of implementation efforts over three phases of evaluation (Bobinet & Petito, 2020), including:
-
(1)
Implementation capacity/needs assessment (prior to implementation, in the planning and engaging phases of the CFIR implementation process or the service strategy phase of the ITIL lifecycle).
-
(2)
Implementation/process evaluation (during implementation, in the executing phase of the CFIR implementation process or the service transition and service operation phases of the ITIL lifecycle).
-
(3)
Implementation outcome/impact evaluation (post implementation, in the reflecting and evaluating phase of CFIR or the continuous service improvement phase of the ITIL lifecycle).
Prior to implementation (i.e., in the planning and engaging phases of implementation), the CFIR can be leveraged for capacity/needs assessment to identify potential barriers and facilitators to implementation from the perspective of the individuals and organizations involved in the implementation. For example, in a recent study (Warner et al., 2018), the CFIR was used to assess barriers and facilitators to implementing a telemedicine-delivered healthy lifestyle program for obesity management in a rural obesity clinic. Elements of consolidated framework for implementation research (CFIR) provided a basis for assessing intervention characteristics, inner and outer settings, and individual characteristics using surveys and semi-structured interviews. In this study, the reach, effectiveness, adoption, implementation, and maintenance (RE-AIM) framework was used in concert with the CFIR to assess staff barriers to success for future scalability. While CFIR can be used to explain why implementation succeeded or failed, the RE-AIM provides a practical framework for planning and evaluating practice change interventions to assure their external validity. Using CFIR, the intervention was found to be valuable from both patient and staff perspectives. A significant barrier limiting sustainability was physical space for intervention delivery and privacy and dedicated resources for staff. The study concluded that it was crucial to engage staff, enhance organizational culture and increase reach, for rural health obesity clinics to be able to enhance sustainability of using telemedicine for the management of obesity.
In a similar vein, the CFIR could be leveraged during implementation (i.e., in the executing phase) for monitoring progress for unanticipated influences and progress toward implementation goals. For example, in a recent study, the CFIR was used to conduct a process evaluation of the implementation of Internet-delivered cognitive behavior therapy (ICBT) within community mental health clinics (Bardosh et al., 2017). The process evaluation was designed to understand facilitators and barriers impacting the uptake and implementation of ICBT. The study found that ICBT implementation was perceived to be most prominently facilitated by intervention characteristics (namely the relative advantages of ICBT compared to face-to-face therapy) and implementation processes (namely the use of an external facilitation unit that aided with engaging patients, therapists, and managers and ICBT implementation). The inner setting was identified as the most significant barrier to implementation as a result of limited resources for ICBT combined with greater priority given to face-to-face care.
Finally yet importantly, the CFIR could be leveraged in the post-implementation (reflecting and evaluating) phase, for impact evaluation, to guide exploration into the question of what factors influenced implementation of the intervention. For example, a recent study examined contextual factors influencing implementation effectiveness and potential for scale-up of an evidence-based mHealth intervention (Weinstein et al., 2014). A comparative qualitative case study design was used, which drew on multiple key informant interviews with stakeholders involved in six projects (utilizing the same health intervention). The CFIR was used to compare findings (implementation effectiveness) across projects.
A two-fold approach to ensuring sustainability of telehealth services.
It would be relevant to note that although sustainability of telehealth services can be provided for as part of service design, the true test for telehealth service sustainability would arise in the service transition and service operation phases (i.e., in the executing phase of CFIR) (Bobinet & Petito, 2020). In regard to the “sustainability” dimension in telehealth services, it would be important to distinguish between:
-
(1)
Sustainability issues associated with people, processes, and technology and
-
(2)
Sustainability issues associated with funding support beyond the pilot period.
Although the first could be addressed through application of theory-informed strategies and best practices for telehealth service design and implementation (e.g., the holistic framework) developed in this paper, the second would need to be addressed separately by the providers and organizations involved in the telehealth implementation depending on the nature of services and specialties involved. In this regard, it would be relevant to note that the likelihood of longer term funding sustainability of a telemedicine program is known to increase when it offers: (1) gap service coverage, e.g., teleradiology; (2) urgent service coverage, e.g., telestroke, teleburn, teletrauma, etc.; (3) mandated services, e.g., correctional telemedicine; or (4) Video-enabled multi-site group chart rounds (Hailey & Crowe, 2003). The extension for community healthcare outcomes (ECHO®) program developed group chart clinical rounds that are managed over telemedicine networks. The underlying concept is that specialists in the management of specific chronic diseases can maximize their effectiveness by mentoring a group of primary care physicians on how to manage these diseases (Hailey & Crowe, 2003).
For example, in cardiology (one of the higher telehealth using specialties), telehealth has been leveraged extensively for urgent service coverage, e.g., for percutaneous coronary intervention (Hailey & Crowe, 2003). To boost the potential for sustainability of telehealth offerings, lower telehealth using specialties like allergy immunology could learn from the cardiology experience by utilizing telehealth for mandated services, e.g., telehealth for asthma management in the correctional health setting. Also, given the anticipated shortage of allergists nationwide, the field could benefit by aligning with project ECHO®, i.e., enabling medical education to be integrated with clinical practice to facilitate the connection between allergy specialists and primary physicians in rural areas. Additionally, allergy providers could be proactive in attracting sustained funding support for telehealth from hospitals and payers through initiatives aligned with the triple aim of healthcare: (1) improve patient experience, (2) lower costs, and (3) promote population health. For example, allergy providers could undertake initiatives to utilize remote monitoring for asthma management to prevent unnecessary emergency and inpatient visits for asthma, reduce costs, and promote population health. Such efforts would be highly relevant to hospitals and payers seeking to expand the provision of telehealth services, in an era of value-based reimbursement.
16.6 A Holistic Framework of Strategies and Practices for Telehealth Service Design/Implementation
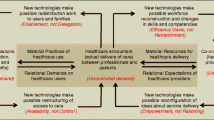
Following from the discussion in the last two sections, i.e., (1) effective strategies and practices for telehealth service design and (2) effective strategies and practices for telehealth service implementation, Fig. 16.1 summarizes a holistic framework of strategies and practices for telehealth service design and implementation. As indicated, the framework integrates theory-informed strategies, i.e., “design thinking” or “CFIR” theory-based strategies with industry-based ITIL best practices across each of the five stages the telehealth service lifecycle. In the next section, the “holistic framework” is applied to cases of success and failure in telehealth to discuss implications for future research and practice.
16.7 Discussion
Applying the “holistic framework” to cases of success and failure in telehealth.
The international conference on successes and failures in telehealth (SFT) which has been held annually for nearly 20 years, attracts a diverse group of stakeholders. The unique focus of the SFT is to provide an engaging forum to share both positive (successes) and the more challenging (failures) experiences in telehealth, to help promote the increasing uptake of telehealth and digital healthcare on a national and international scale. Over the years, papers presented at the SFTs have made a helpful contribution to understanding and overcoming the practical challenges of using implementing telehealth. Presentations at the conferences have covered a variety of health systems and telehealth applications. To address the question of what the papers presented tell us about the successes and failures in telehealth, a review was carried out of the papers from selected SFT conferences, the proceedings of which were published as supplements to the journal of telemedicine and telecare (Gilman & Stensland, 2013). This review helped to identify some common themes on challenges or determinants of success and failure of telehealth, including the involvement of stakeholders in planning, health professionals’ attitudes toward training, changes in responsibility, autonomy, perceived need for telehealth, the stability of management structures, the turnover of personnel and cooperation between organizations, the reliability of equipment, adequacy of technical support, the reliability of vendors, and policy and budgetary issues (Gilman & Stensland, 2013).
Each of the challenges identified in review of papers from the SFT conferences could be addressed through application of the “holistic framework” developed in this paper. For example, the challenge of stakeholder involvement, health professional attitudes, perceived need for the telehealth intervention, and reliability of vendor could be addressed at the service strategy or planning and engaging (pre-implementation) stage of the telehealth lifecycle. At this stage, the CFIR could be used to assess barriers and facilitators to telehealth implementation from the perspective of individuals involved. Likewise, during the service design phase, these challenges could be addressed through a “design thinking” approach to telehealth service design, based on in-situ observation, principles of co-design, and thorough understanding of the socio-technical context within which clinician patient interaction occurs. Likewise, in the service transition and service execution phases, the CFIR could be leveraged to monitor progress from the perspective of individuals involved. Also, in the post-implementation phase, the CFIR could be leveraged to conduct and impact and process evaluation to understand why the implementation failed from the perspective of individuals involved.
In a similar vein, challenges associated with stability of management structures, turnover of personnel, and cooperation between organizations, could be addressed by leveraging CFIR to assess barriers and facilitators associated with the inner setting, through constructs of (1) structural characteristics, (2) networks and communication, (3) culture, and (4) implementation climate or the absorptive capacity for change. As discussed earlier, a positive implementation climate requires readiness for implementation, which in turn includes three sub-constructs, leadership engagement, available resources, and access to information and knowledge. This assessment of barriers and facilitators associated with inner setting in turn could be conducted pre-implementation, during pre-implementation and post-implementation. Likewise, challenges associated with reliability of equipment and adequacy of technical support could be addressed by leveraging the CFIR to assess barriers to implementation from the perspective of intervention characteristics in the service strategy phase. Moreover, in the service design phase, systems thinking principles could be used to identify and address all training needs from the perspectives of telehealth service users.
Lastly, policy and budgetary challenges could be addressed by assessing barriers to implementation on CFIR domain of outer setting which in turn could be accomplished pre, during, and post implementation. During the service design phase, consideration for the policy and budgetary issues could be incorporated into the socio-technical context used to inform the design of telehealth services. As discussed earlier, although sustainability issues associated with people, process, technology, and partners/suppliers could be addressed using the holistic framework, sustainability issues associated with funding would need to be addressed separately by providers and organizations involved in implementation, to ensure that funding constraints do not adversely affect service transition and service execution phases. In the continuous service improvement phase, the CFIR could be combined with the RE-AIM framework, to assess potential for scalability and sustainability of the intervention. In summary, appropriate utilization of the “holistic framework” can provide clinicians, healthcare leaders, and IT service managers alike with a comprehensive approach to addressing barriers to the effective design and implementation of telehealth services.
16.8 Implications for Practice and Future Research
As discussed in the Introduction, a key concern in the current telehealth literature is the widespread sustainability of telehealth use across multiple specialties in the post-pandemic environment. Considering the example of the United States (US), recent (pre-pandemic) studies in the US have reported wide variation in telehealth use across medical specialties. This is intriguing, because the US lacks a nationwide standardized set of telehealth reimbursement policies, which in turn, has historically posed a barrier to telehealth adoption in all specialties (Brown, 2006; Spivak et al., 2020). Despite these macro (policy-level) constraints experienced by all medical specialties, some specialties have been able to normalize telehealth to mainstream practice (e.g., psychiatry, cardiology); while others are just getting started during the COVID-19 pandemic (e.g., allergy-immunology) (Brown, 2006; Spivak et al., 2020).
Calling upon the “macro-meso-micro” three-layer framework, three levels of factors, including macro (societal or policy level), meso (group or organizational level), and micro (individual-level) factors can help to explain behavior (e.g., telehealth use in a medical specialty). Since macro (policy-level) factors (barriers) by themselves do not help to explain the wide variation in telehealth use across specialties, it would be important to examine the meso (organizational level) and micro (individual-level) factors (barriers or facilitators) influencing telehealth use in medical specialties, to better understand reasons for the variation across specialties, and identify implications for widespread sustainability of telehealth use in the post pandemic era.
The “holistic framework” developed in this paper can provide healthcare organizations at the meso level and individual providers at the micro level, with a foundation for getting started with designing and implementing a successful and sustainable telehealth service. Future research on other meso (group or organizational-level) factors and micro (individual provider and patient-level) factors could help to supplement the strategies and insights gained from this paper for effective telehealth design and implementation, to provide additional implications for ensuring widespread sustainability of telehealth services. For example, if research shows that specialty society organizations at the meso level could have substantive role to play a role in promoting telehealth use within their respective specialties (for example, by educating providers on how to get started with telehealth, providing opportunities for telehealth training, or advocating for telehealth training in medicine residency curriculum), then the “holistic framework” developed in this paper could provide a strong foundation for specialty societies to develop organized provider-training (within the specialty), on designing and implementing a successful and sustainable telehealth service infrastructure.
Future research may also reveal that specialty societies in the US are in a unique positon to influence macro (policy-level) factors influencing telehealth use (e.g., reimbursement and coverage), through advocacy for consistent payment policies from public and private payers. In other words, specialty societies may be in a unique position to influence both meso-level factors (e.g., provider tech-training and culture within a specialty) and macro-level factors (telehealth reimbursement policies). Correspondingly, specialty societies could play a substantive role in alleviating sustainability issues associated with people, process, and technology (e.g., by leveraging the holistic framework to develop organized training for telehealth design and implementation) and sustainability issues associated with funding support for telehealth (by influencing macro-level factors like payment policies). In regard to the latter, specialty societies could play a significant role in supplementing independent provider efforts to ensure funding sustainability (e.g., by facilitating provider alignment with the triple aim framework).
Following from the above discussion, two lines of future research could help further enrich the strategies, practices, and insights gained from the “holistic framework” for telehealth design and implementation: (1) research on improving telehealth implementation effectiveness (e.g., systematic evidence on the relationships among the key domains and constructs of CFIR to influence implementation effectiveness) and (2) research on promoting telehealth implementation sustainability, e.g., future research on strategies for reducing variation in telehealth use across medical specialties to enable widespread sustainability in telehealth use in a post-pandemic era.
16.9 Conclusion
Telehealth changes the established patient-clinician interaction. As such, the success of a new telehealth service is known to depend more on changing the expectations and behavior (and the resultant clinician-patient relationship) than on technology. Success in telehealth projects is highly dependent on understanding how the new telehealth offering changes the distinct value proposition to each of the parties—clinicians, patients, and administrators. Successful and sustainable telehealth services will not be created by addressing the needs of one party or by focusing on one part of the problem.
Although existing theories and frameworks for telehealth design and implementation do echo these realities at a broad level, the practical strategies emanating from these theories remain fragmented and divorced from industry-level best practice frameworks for telehealth design and implementation. The latter in turn have limited relevance to key telehealth implementation stakeholders like clinicians and healthcare leaders. This paper synthesizes strategies for telehealth service design and implementation emanating from the existing theoretical literature and integrates them with industry-based (ITIL) best practices, to develop a “holistic framework” of strategies and best practices for telehealth service design and implementation. In doing so, the paper addresses a key gap in the telehealth literature. Additionally, the framework is applied to cases of success and failure in telehealth to discuss implications for future research and practice. Overall, the strategies, best practices, and insights for sustainability gained from the “holistic framework,” could be used to shape a contemporary method for design and implementation of telehealth services that has potential to improve the outcomes of telehealth implementation projects. They can also enable telehealth project champions to avoid misconceptions that might lead to unintended and expensive consequences.
References
Adler-Milstein, J., Kvedar, J., & Bates, D. W. (2014). Telehealth among US hospitals: Several factors, including state reimbursement and licensure policies, influence adoption. Health Aff (millwood)., 33(2), 207–215. https://doi.org/10.1377/hlthaff.2013.1054 PMID: 24493762.
Almathami, H. K. Y., Win, K. T. & Vlahu-Gjorgievska, E. (2020) Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients’ Homes: Systematic Literature Review. J Med Internet Res., 22(2):e16407
Andrus B. (2017) 5 Healthcare Specialties Leading the Way In Telemedicine, E-visit (Ed.), Accessed December 1, 2020, from https://blog.evisit.com/virtual-care-blog/top-specialties-for-telemedicine
Attewell, P. (1992) Technology diffusion and organizational learning: The case of business computing. Organ. Sci., 3(1), 1–19. from https://doi.org/10.1287/orsc.3.1.1
Bardosh, K. L., Murray, M., Khaemba, A. M., Smillie, K., & Lester, R. (2017). Operationalizing mHealth to improve patient care: A qualitative implementation science evaluation of the WelTel texting intervention in Canada and Kenya. Global Health., 13(1), 87. https://doi.org/10.1186/s12992-017-0311-z.PMID:29208026;PMCID:PMC5717811
Batsis, J. A., McClure, A. C., Weintraub, A. B., Sette, D., Rotenberg, S., Stevens, C. J., Gilbert-Diamond, D., Kotz, D. F., Bartels, S. J., Cook, S. B., & Rothstein, R. I. (2020). Barriers and facilitators in implementing a pilot, pragmatic, telemedicine-delivered healthy lifestyle program for obesity management in a rural, academic obesity clinic. Implement Sci Commun., 1(83), 1–9. https://doi.org/10.1186/s43058-020-00075-9.PMID:33015640;PMCID:PMC7526351
Bobinet, K. & Petito, J. (2020) Designing The Consumer-Centered Telehealth & eVisit Experience. The Office of National Coordinator for Health Information Technology U.S. Department of Health & Human Services, Accessed November 10, 2020, from https://www.healthit.gov/sites/default/files/DesigningConsumerCenteredTelehealtheVisit-ONC-WHITEPAPER-2015V2edits.pdf
Broens, T. H., Vollenbroek-Hutten, M. M., Hermens, H. J., van Halteren, A. T. & Nieuwenhuis, L. J. () Determinants of successful telemedicine implementations: A literature study. J. Telemed. Telecare, 13(6), 303–309. doi: https://doi.org/10.1258/135763307781644951.
Brown, N. A. (2006). State Medicaid and private payer reimbursement for telemedicine: An overview. Journal of Telemedicine and Telecare, 12(2), S32–S39. https://doi.org/10.1258/135763306778393108 PMID: 16989672.
Brown, T. (2008) Design Thinking. Harvard Business Review, Brighton, MA, USA.
Buchachi, F., & Pakenham-Walsh, N. (2007). Information technology of health in developing countries. Chest, 132(5), 1624–1630. https://doi.org/10.1378/chest.07-1760
Christie, H. L., Bartels, S. L., Boots, L. M. M., Tange, H. J., Verhey, F. J. J., & de Vugt, M. E. (2018). A systematic review on the implementation of eHealth interventions for informal caregivers of people with dementia. Internet Interventions, 13(2018), 51–59. https://doi.org/10.1016/j.invent.2018.07.002.PMID:30206519;PMCID:PMC6112102
Cilliers, L. & Flowerday, S. V. (2013) Health information systems to improve health care: A telemedicine case study. SA J. Inf. Manag., 15(1):1–5, Art. #541, doi:https://doi.org/10.4102/sajim.v15i1.541.
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4(50), 1–15. https://doi.org/10.1186/1748-5908-4-50.PMID:19664226;PMCID:PMC2736161
Dovigi, E., Kwok, E. Y. L. & English, J.C. 3rd. (2020) A Framework-Driven Systematic Review of the Barriers and Facilitators to Teledermatology Implementation. Curr Dermatol Rep. 1–9. doi: https://doi.org/10.1007/s13671-020-00323-0. Epub ahead of print. PMID: 33200042; PMCID: PMC7658914.
Dovigi, E., Kwok, E. Y. L. & English, J.C. 3rd. (2020b) A Framework-Driven Systematic Review of the Barriers and Facilitators to Teledermatology Implementation. Curr Dermatol Rep. 1–9. doi: https://doi.org/10.1007/s13671-020-00323-0. Epub ahead of print. PMID: 33200042; PMCID: PMC7658914.
Finch, T., Mair, F., & May, C. (2006). Teledermatology in the UK: Lessons in service innovation. British Journal of Dermatology, 156(3), 521–527. https://doi.org/10.1111/j.1365-2133.2006.07608.x
Foster, M. V. & Sethares, K. A. (2014) Facilitators and barriers to the adoption of telehealth in older adults: an integrative review. Comput Inform Nurs. 32(11):523–533; quiz 534–535. doi: https://doi.org/10.1097/CIN.0000000000000105. PMID: 25251862.
Garavand, A., Samadbeik, M., Nadri, H., Rahimi, B., & Asadi, H. (2019). Effective Factors in Adoption of Mobile Health Applications between Medical Sciences Students Using the UTAUT Model. Methods of Information in Medicine, 58(4–05), 131–139. https://doi.org/10.1055/s-0040-1701607 PMID: 32170717.
Gilman, M., & Stensland, J. (2013). Telehealth and Medicare: Payment policy, current use, and prospects for growth. Medicare & Medicaid Research Review, 3(4), E1–E14. https://doi.org/10.5600/mmrr.003.04.a04.PMID:24834368;PMCID:PMC4011650
Greene J. (n. d.) The Essential Guide to ITIL Framework and Processes; Accessed November 5, 2020, from https://www.cherwell.com/it-service-management/library/essential-guides/essential-guide-to-itil-framework-and-processes/
Hadjistavropoulos, H. D., Nugent, M. M., Dirkse, D., & Pugh, N. (2017). Implementation of internet-delivered cognitive behavior therapy within community mental health clinics: A process evaluation using the consolidated framework for implementation research. BMC Psychiatry, 17(1), 331. https://doi.org/10.1186/s12888-017-1496-7.PMID:28899365;PMCID:PMC5596488
Hailey, D., & Crowe, B. A. (2003). profile of success and failure in telehealth–evidence and opinion from the Success and Failures in Telehealth conferences. Journal of Telemedicine and Telecare, 9(2), S22–S24. https://doi.org/10.1258/135763303322596165 PMID: 14748344.
Mended Hearts (n. d.) Telemedicine’s expanded role in cardiac care, Mended Hearts (Ed.), Accessed September 2, 2020, from https://mendedhearts.org/story/telemedicines-expanding-role-in-cardiac-care/
Hebert, M. (2001). Telehealth success: Evaluation framework development. Stud Health Technol Inform., 84(Pt 2), 1145–1149. PMID: 11604908.
Kane, C. K., & Gillis, K. (2018). The Use Of Telemedicine By Physicians: Still The Exception Rather Than The Rule. Health Aff (millwood)., 37(12), 1923–1930. https://doi.org/10.1377/hlthaff.2018.05077 PMID: 30633670.
Kho, J., Gillespie, N., & Martin-Khan, M. (2020). A systematic scoping review of change management practices used for telemedicine service implementations. BMC Health Services Research, 20(1), 815. https://doi.org/10.1186/s12913-020-05657-w PMID: 32873295.
Khoja, S., Scott, R. E., Casebeer, A. L., Mohsin, M., Ishaq, A. F., & Gilani, S. (2007a). e-Health readiness assessment tools for healthcare institutions in developing countries. Telemedicine Journal and E-Health, 13(4), 425–431. https://doi.org/10.1089/tmj.2006.0064 PMID: 17848110.
Khoja, S., Scott, R., Casebeer, A., Mohsin, M., Ishaq, A., & Gilani, S. (2007b). E-health readiness assessment tools for healthcare institutions in developing countries. Telemed. e-Health, 13(4), 425–432. https://doi.org/10.1089/tmj.2006.0064
Khoja, S., Durrani, H., Scott, R., Sajwani, A., & Piryani, U. (2013). Conceptual framework for development of comprehensive e-Health evaluation tool. Telemed. e-Health, 19(1), 48–53. https://doi.org/10.1089/tmj.2012.0073 Epub 2012 Sep 7.
Koivunen, M., & Saranto, K. (2018). Nursing professionals’ experiences of the facilitators and barriers to the use of telehealth applications: A systematic review of qualitative studies. Scandinavian Journal of Caring Sciences, 32(1), 24–44. https://doi.org/10.1111/scs.12445 Epub 2017 Aug 3 PMID: 28771752.
Lin, C. C., Dievler, A., Robbins, C., Sripipatana, A., Quinn, M., & Nair, S. (2018). Telehealth In Health Centers: Key Adoption Factors, Barriers. And Opportunities. Health Aff (millwood), 37(12), 1967–1974. https://doi.org/10.1377/hlthaff.2018.05125 PMID: 30633683.
Moehr, J. R., Schaafsma, J., Anglin, C., Pantazi, S. V., Grimm, N. A., & Anglin, S. (2006). Success factors for telehealth–a case study. International Journal of Medical Informatics, 75(10–11), 755–763. https://doi.org/10.1016/j.ijmedinf.2005.11.001 Epub 2006 Jan 4 PMID: 16388982.
Nguyen, M., Waller, M., Pandya, A., & Portnoy, J. (2020). A Review of Patient and Provider Satisfaction with Telemedicine. Current Allergy and Asthma Reports, 20(11), 72. https://doi.org/10.1007/s11882-020-00969-7.PMID:32959158;PMCID:PMC7505720
Pelletier-Fleury, N., Fargeon, V., & Lano´e, J. & Fardeau, M. (1997). Transaction costs economics as a conceptual framework for the analysis of barriers to the diffusion of telemedicine. Health Policy, 42(1), 1–14. https://doi.org/10.1016/s0168-8510(97)00038-9 PMID: 10173489.
Perry A. (2020) Institute for Healthcare Improvement. Recommendations for designing high quality telehealth, Institute for Healthcare Improvement (ihi, Ed.), Accessed August 15, 2020, from http://www.ihi.org/communities/blogs/recommendations-for-designing-high-quality-telehealth
Schwamm, L. H. (2014). Telehealth: Seven strategies to successfully implement disruptive technology and transform health care. Health Aff (millwood)., 33(2), 200–206. https://doi.org/10.1377/hlthaff.2013.1021 PMID: 24493761.
Senge, P. M. (1992). The Fifth Discipline: The Art and Science of the Learning Organization. Random House Business Books.
Shachar, C., Engel, J., & Elwyn, G. (2020). Implications for Telehealth in a Postpandemic Future: Regulatory and Privacy Issues. JAMA, 323(23), 2375–2376. https://doi.org/10.1001/jama.2020.7943 PMID: 32421170.
Singh, J., Lutteroth, C., & Wünsche B. C. (2010) Taxonomy of usability requirements for home telehealth systems. in Proceedings of the 11th International Conference of the NZ Chapter of the ACM Special Interest Group on Human-Computer Interaction. CHINZ, Association for Computing Machinery (ACM, Ed.), Auckland, New Zealand, July 8–9, pp. 29–32.
Spivak, S., Spivak, A., Cullen, B., Meuchel, J., Johnston, D., Chernow, R., Green, C. & Mojtabai, R. (2020) Telepsychiatry Use in U.S. Mental Health Facilities, 2010–2017. Psychiatr Serv., 71(2):121–127. doi: https://doi.org/10.1176/appi.ps.201900261. Epub 2019 Oct 16. PMID: 31615370.
Tang, Z., Johnson, T. R., Tindall, R. D., & Zhang, J. (2006). Applying heuristic evaluation to improve the usability of a telemedicine system. Telemedicine Journal and E-Health, 12(1), 24–34. https://doi.org/10.1089/tmj.2006.12.24 PMID: 16478410.
Tanriverdi, H., & Iacono, C. S. (August 1998). (1998) Knowledge Barriers to Diffusion of Telemedicine. In Proceedings of the International Conference of the Association for Information Systems, Helsinki, Finland, 14–16, 39–50.
Taylor, P. R. (2013) An approach to designing viable and sustainable telehealth services. Stud Health Technol Inform. 188(XXX):108–113. PMID: 23823297.
Thaler, R. & Sunstein, C. (2009). NUDGE: Improving Decisions about Health, Wealth, and Happiness. Penguin, London, UK. ISBN: 9780141040011 29.Briggs L. (2007) Changing Behaviour: A Public Policy Perspective, from https://legacy.apsc.gov.au/changing-behaviour-public-policy-perspective Australian Public Service Commission, Australian Government, Accessed February 5, 2021
Van Dyk L. (2014) A Review of Telehealth Service Implementation Frameworks. Int. J. Environ. Res. Public Health, 11(2), 1279–1298. PMID: 24464237 PMCID: PMC3945538.
Warner, G., Lawson, B., Sampalli, T., Burge, F., Gibson, R., & Wood, S. (2018). Applying the consolidated framework for implementation research to identify barriers affecting implementation of an online frailty tool into primary health care: A qualitative study. BMC Health Services Research, 18(1), 395. https://doi.org/10.1186/s12913-018-3163-1.PMID:29855306;PMCID:PMC5984376
Weinstein, R. S., Lopez, A. M., Joseph, B. A., Erps, K. A., Holcomb, M., Barker, G. P., & Krupinski, E. A. (2014). Telemedicine, telehealth, and mobile health applications that work: Opportunities and barriers. American Journal of Medicine, 127(3), 183–187. https://doi.org/10.1016/j.amjmed.2013.09.032 Epub 2013 Oct 29 PMID: 24384059.
White, S. K., & Greiner, L. (2019) What is ITIL? Your guide to the IT Infrastructure Library, Accessed November 10, 2020, from https://www.cio.com/article/2439501/infrastructure-it-infrastructure-library-itil-definition-and-solutions.html#:~:text=ITIL%20is%20a%20framework%20of,for%20growth%2C%20scale%20and%20change
Wiki (n. d. a) ITIL Service Strategy. Accessed November 5, 2020, from https://wiki.en.it-processmaps.com/index.php/ITIL_Service_Strategy
Wiki (n. d. b) ITIL Service Design. Accessed November 5, 2020, from https://wiki.en.it-processmaps.com/index.php/ITIL_Service_Design
Wiki (n. d. c) ITIL Service Transition. Accessed November 5, 2020, from https://wiki.en.it-processmaps.com/index.php/ITIL_Service_Transition
Wiki (n. d. d) ITIL Service Operation. Accessed November 5, 2020, from https://wiki.en.it-processmaps.com/index.php/ITIL_Service_Operation;.
Wiki (n. d. e) ITIL Continual Service Improvement. Accessed November 5, 2020, from https://wiki.en.it-processmaps.com/index.php/ITIL_CSI_-_Continual_Service_Improvement
Wikipedia (n. d.) ITIL; Accessed November 5, 2020, from https://en.wikipedia.org/wiki/ITIL
Yellowlees, P. (2005). Successfully developing a telemedicine system. Journal of Telemedicine and Telecare, 11(7), 331–336. https://doi.org/10.1258/135763305774472024
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rangachari, P. (2022). A Holistic Framework of Strategies and Best Practices for Telehealth Service Design and Implementation. In: Pfannstiel, M.A., Brehmer, N., Rasche, C. (eds) Service Design Practices for Healthcare Innovation. Springer, Cham. https://doi.org/10.1007/978-3-030-87273-1_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-87273-1_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87272-4
Online ISBN: 978-3-030-87273-1
eBook Packages: Business and ManagementBusiness and Management (R0)