Abstract
The chapter analyses possible contributions offered by medical devices technology in order to tackle the troubles affecting healthcare services worldwide. These issues affect the efficacy and efficiency of all healthcare systems, finally undermining their very sustainability. The most evident problems, at least in the affluent part of the world, are rising cost, mainly due to demographic changes and the increase of non-transmissible chronic diseases. In addition, the lack of adequate healthcare for the lower-income part of the society is evident and unacceptable.
The chapter will focus on the creation of value for the patients and other stakeholders starting from the care delivery value chain and will underline the contribution of the technology to improve the different healing steps.
A special consideration will be given to the need of a consistent and multidisciplinary approach including all the different components of the healthcare system from technology to infrastructure to human resources and the involved stakeholders.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
The global healthcare systemFootnote 1 suffers from many issues that undermine its effectiveness and long-term sustainability.
The most evident concerns are rising costs mainly due to the increase of the elderly population, its higher morbidity and the increase of non-transmissible chronic diseases. These causes are more evident in the most affluent societies, but are now extending also to lower-income countries, as underlined by a WHO report [1].
As will be detailed in the following, healthcare systems are not always able to provide the adequate level of care to the vast majority of people worldwide due to increased expenditure in labour and medication. Moreover, we often observe the lack of minimal level of care in low-income countries and for lower-income people even in affluent societies.
Many authors identify the key point to solve these systems’ weaknesses. They propose the healthcare systems to become more focused on the delivery of value for the patients and the community they serve.
This chapter will deal with first observations that a consistent and multidisciplinary use of medical devices can be instrumental to find solutions for the problems of healthcare systems.
1 The Medical Devices Technology: A Preliminary Definition
According to the Medical Device Regulation 2017/745 of the European Union (EU MDR), a medical device can be defined as any instrument, apparatus, appliance, software, implant, reagent, material or other article intended by the manufacturer to be used, alone or in combination, for human beings for diagnosis, prevention, monitoring, prediction, prognosis, treatment or alleviation of diseaseFootnote 2 [2]).
According to this definition, the term medical device covers a wide range of products, spanning from a simple wooden-made tongue depressor to a hospital bed to a complex MRI or X-ray equipment.
With the present development of the technology, the expression medical device includes also the group of contrivances that, even if not originally designed for medical application, are now used for healthcare purposes, perhaps with auxiliary functions. In fact, the dedicated (and possibly wearable) sensors, supplemented by software and functions embedded in smartphone and smartwatch, are a further promising source of innovation and diagnostic support. Devices based on artificial intelligence (AI) and big data analyses systems should also be considered in this group.
It must be ensured that the collected data have a real medical meaning and can be used for diagnosis, prevention and therapy. For this reason, it is mandatory to apply here all the regulations as done for the “traditional” medical devices.
2 The Main Challenge
It seems that the destiny of every complex system, such as a society or an organization, is to be challenged by considerations on effectiveness, efficiency and sustainability (see Chap. 11 for more details) [3,4,5]. The solution to this problem usually requires a committed change in perspective by all stakeholders. This also holds true for the healthcare systems today.
With respect to the recent past, we experience the availability of an incredible amount of new and encouraging powerful tools and technologies for diagnosis and for successful therapies. We are also confronted with a complex and difficult scenario, characterized by:
-
Ageing of the population, at least in the wealthier countries, that increases the need to treat chronic illnesses with the consequent upsurge of related cost.
-
Explosion of the cost, especially in the affluent part of the world. This might also be provoked by the increased expectations stimulated by the successful progress of healthcare technology [4].
-
Need to ensure the adequate health assistance to a wider part of the population in lower-income countries and to the less wealthy group of the population in affluent societies.
-
Reduced marginal returns of healthcare expenditure, e.g. in terms of acquired healthy life years versus the total expenditure. This seems to be a “law” for all the complex organizations. This is especially perceived in the countries where the total expenditure is high [3,4,5].
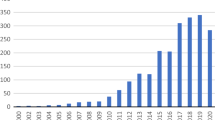
The reduction of the marginal return for healthcare expenditure is illustrated by the diagram in Fig. 1.1 [6].
The increasing expenditure in healthcare does not result in a proportional increase in life expectancy. This suggests a reducing return in the healthcare investments. (Modified from [6])
This trend dramatically shows that in all countries belonging to the Organization for Economic Co-operation and Development (OECD), the increase of expenditure in healthcare does not yield a linear improvement in the healthy life expectancy at birth.
A similar behaviour can be found when considering the expected improvement of the QALY over the expenditure.
QALY (Quality Adjusted Life Years) is a measure of the burden of disease. The concept is to weight the years of life lived with a defined quality of the life. One QALY is equal to 1 year in perfect health. The presence of any sort of disability assigns a weight less than one. The basis for the assessment of QALY is a generally accepted questionnaire.
A more detailed discussion of this aspect can be found in Chap. 11.
3 A Possible Answer
The majority of authors, including the group of experts at World Economic Forum (WEF) 2020, agree that the change of the present paradigm of healthcare systems seem to be the only real solution to afford the above-mentioned challenges [5]. This approach promises to be the most powerful and sustainable one in the long term, especially if compared with the plain cost-cutting exercise, which is often much appreciated by the policymakers.
Basic research, best practices dissemination and a value-based reimbursement are among the most powerful tools to achieve this paradigm change together with a patient-centric approach. This can bring value in the system and increase the return of spent resources. The creation of a patient-centred healthcare system requires to move from a quantity-based delivery of services to a value-based approach and evaluation [7,8,9,10].
We assume that a major contribution to these concepts can be provided by medical devices.
This approach suggests that the therapies, or the medical acts in general, should be chosen (and possibly reimbursed) not (only) on the basis of their quantity, but (mostly) on the value they can create for the health and well-being of the patients (see also Chap. 10 of this book).
According to Kaplan and Porter [9], the value in healthcare should be measured in terms of the patient achieved outcomes according to the money spent.
This can be summarized as:
The starting point is to correctly define the health outcome of patients. Too often this is intended just as the plain delivery of services, with the assumption, that more (delivered) services is equal to more (delivered) value. A model developed by M. Porter et al. [8,9,10,11,12] suggests instead to focus on the real health and life quality improvements achieved by the patient. This includes a possible patient discomfort experienced during the treatment and the sustainability of the reached health status.
These authors underline the need to concentrate on the overall value created for the patient, rather than on parameters that are only giving a partial view of the caring activity. The proposed model indicates three tiers for the assessment of what has a real value for the patient. This hierarchy of achievements includes:
-
Patient’s achieved health status or maintained in case of degenerative/chronic illness.
-
Process of healing including the possible discomfort created by or connected to the therapy.
-
Process of recovery (time for achieving the best possible health status and possible suffered discomfort).
-
Sustainability of the achieved health status including the resulting quality of life (QoL) and need for possible re-interventions.
Each of the above tiers may be subdivided in additional subcategories, according to the specific pathology and treatment strategy.
The complexity of medical treatment should also consider a set of many competing outcomes, e.g. near-term versus long-term functionality. These must be weighted to achieve the best compromise, also in light of the patient’s individual preference. For the purpose of the present discussion, we can avoid to go into further detail.
The creation of value for the patient is accomplished through different steps that can be summarized, according to the above authors, with the Care Delivery Value Chain (CDVC). This chain shows the different activities undertaken at the different stages of an illness, from prevention, to diagnosis, treatment and rehabilitation. The detailed steps should be further specified depending on the pathology under consideration.
Table 1.1 shows the main steps to be undertaken for the creation of value in healthcare. This generic chart should be enriched with more details according to the pathology, illness status and healthcare insurance.
The relevant activities can be categorized in two main areas:
-
Supporting activities such as informing, measuring and accessing.
-
Primary activities directly devoted to the delivery of care.
Again, making reference to a non-specific treatment model, the contribution of the medical devices to each of these activities can be summarized in Table 1.2.
The achievement of the value for the patient should be observed and monitored at each step of the value chain.
As shown by WEF in 2020 [5] and by E. Topol in 2012 [13], the transition to a new type of healthcare is controlled by the intense application of new technologies. In addition, many techniques inherited from other fields of engineering can provide an important support.
This is the case of the application of highly sophisticated prosthetic devices and artificial body parts and organs, robotic tools, advanced imaging techniques, dedicated non-invasive and invasive sensors for physiological parameters, algorithms and computing power.
Table 1.3 and map in Fig. 1.2 give another, perhaps more comprehensive, view of the possible contribution of the medical devices to the change of the healthcare paradigms.
The super convergenceFootnote 3 [13] of all these instruments paves the way towards the new medicine, but also helps to improve the present praxis and allows for an important cost saving.
One possible example is the continuous collection of important parameters obtained with non-invasive and invasive sensors or with devices autonomously operated by the patient.
This procedure supports all phases of the care delivery chain, especially if the collected data can be shared among all the different caregivers at various stages of the caring process, possibly through a well-designed IT-infrastructure.
The power of internet in improving the literacy of the patients and the availability of “consumer” devices should not be underestimated. It allows a sort of “informative self-monitoring” of the patient. Such tools can support the decision-making of the people for an early referral to caregivers in case of possible pathologies. In this way it is possible to achieve a healthier way of life at an earlier stage or a better compliance with the prescribed therapy.
An important caveat at this point is to ensure the correctness and precision of the information made available to the patients (usually via internet) and the reliability of consumer devices.
Misleading communication can give rise of the generation of wrong expectations for applicable therapies among sick people. This is an area to be strictly monitored and controlled by medical authorities, regulatory institutions and policymakers.
In addition to the items listed in Fig. 1.2, it is important to remember the need for the availability of low-cost and hi-quality “simple devices”, like syringes, personal protective equipment (PPE), disinfection devices, face masks or simple medication disposables. The availability of these medical devices with acceptable quality and reliability also in remote areas or in low-income countries might not always be granted. These are important means to improve the overall health status of the population by e.g. avoiding the spread of infections, allowing for effective vaccination campaigns and reducing mortality [14, 15].
The medical device technology as shown in Fig. 1.2 also influences the social aspects of healthcare mainly through:
-
Moving the patients towards “self-care” and more autonomous implementation of therapies.
-
Influencing positively the communication between patients and professional caregivers implementing a deeper and more precise flow of information about pathologies and possible therapies [4].
4 The System Thinking
The successful clinical application of any medical device, especially in the case of complex equipment, needs to consider several dimensions and a fully multidisciplinary approach. This holds also true for the subsequent successful outcome of the medical act.
As reminded by WHO [16], system thinking is an essential approach for success in designing and operating the healthcare systems and healthcare provider institutions.
Figure 1.3 summarizes the different aspects and actions involved in the successful application of the medical technology, of which the medical devices represent a larger part.
All medical acts suffer from the ambiguity between a remedy and a potential creation of damage [17]. For this reason, we must operate the trade-off between benefits and risks, even in the clinical application of medical devices. This aspect is becoming more and more significant in light of the increasing complexity of devices and systems which are currently available on the market. The topic is involving all stakeholders, i.e. engineers, notified bodies (for normative and regulation requirements) as well as caregivers. The compliance to these prerequisites ensures that the devices put on the market are fit for purpose, meaning that they deliver the claimed benefits and are, at the same time, safe for the patients and operators.
The delivered benefits and the sustained cost are also important area of trade-off. The cost issue, even if perhaps not considered in the historical medical literature, is of utmost importance. This is due to the present complexity of many devices themselves and to the increasing healthcare demand.
The costs evaluation includes many aspects, basically the capital and operational costs. They must be subject to careful consideration by decision makers, such as in politics and in healthcare institutions (see also Chap. 6).
Another important area of interest is relevant to the different stakeholders involved in the selection and use of the devices. This group acts like a business chain and spans from manufacturers, vendors, decision makers and operators and finally patients.
The healthcare is a very specific branch of human activities, dealing with human beings and with their physical and mental health with the final goal to improve quality of life. The healthcare technology involves not only the healthcare professionals and the patient under treatment but also the relatives and people in contact with her/him. This group includes a potential lay user of medical devices and spreads up to the whole community.
Political decisions are also deeply affected, especially concerning the economic affordability and sustainability of the technological choices. Political decisions and market dynamics also influence and promote the development and the adoption of innovative solutions (see also Chap. 3). In addition, it is important to consider the implications of new and complex technologies on the consolidated healthcare system. The successful outcome of the healthcare act is influenced by many actors and resources as summarized in Fig. 1.4 [4, 16].
All the aspects illustrated in Fig. 1.4 influence the correct use of the medical devices and are affecting the successful implementation of the therapy.
A general but not exhaustive list includes:
-
The devices should be reliable, safe, effective and implemented according to standards and directives.
-
The caregivers (either professional or not) should be trained and open to use the technology.
-
The community should be willing to accept the use of these device and ready to allocate the required resources for their availability and full accessibility.
-
The management (also at political level) should operate for the accessibility and affordability of the devices and provide resources and required work organization.
-
The healthcare institutions (inside or outside the traditional hospitals) should prepare their physical infrastructures for the effective use of these devices.
-
The patients and lay caregivers must have the adequate literacy for the use of the devices. This is part of the education on the compliance with therapies.
The main message behind the above considerations is that the benefits coming from the use of medical devices necessarily require a genuine multidisciplinary approach. This involves the people’s mindset and culture, the infrastructure design and management as well as the political choices.
Conclusion
From the above discussion, it is possible to summarize the contribution of medical devices to problems presently affecting the healthcare system:
-
Availability of monitoring tools since the early inception of the illness to allow prevention and early referral. This allows a better health status for the patients and avoid/reduce the cost for the treatment of a heavier illness status.
-
Availability of devices that may help the (potential) patient either in the prevention phase or in the recovery phase (post treatment, e.g. surgery). This holds true for monitoring or self-monitoring tools as well as for devices that can support the patients/caregivers in maintaining the required compliance to the prescribed therapies.
-
Availability of devices supporting the patients in acquiring the best possible level of autonomy.
All these can help the healthcare environment to increase the value for the patients, seen as a better outcome with a containment of the cost in a socially acceptable way.
Take Home Message
-
The ageing of the population, the spread of chronic diseases and the reduction of the investment return in healthcare are undermining the long-term sustainability of the healthcare systems worldwide. In addition, the lower-income part of the population may still lack the adequate level of care.
-
The solution to the above issues requires a change in the present healthcare paradigm.
-
The use of medical devices, characterized by different level of complexity, can have a positive impact on the improvement of each step of the care delivery value chain and in the needed change of healthcare paradigm.
-
A system approach, to consider all the involved aspects, from technical knowledge, to personnel management to economics and innovation is a key factor to ensure the full exploitation of the medical devices potential.
Notes
- 1.
Following the definition of the World Health Organization, a health system “consists of all organizations, people and actions whose primary intent is to promote, restore or maintain health”. Its goals are “improving health and health equity in ways that are responsive, financially fair, and make the best, or most efficient, use of available resources” [15].
- 2.
The quoted definition from EU MDR has been shortened to improve the readability. A substantially similar definition is given by WHO. More precise and detailed designation, together with the relevant implications, can be found in Chap. 4 of the present book.
- 3.
The term has been used by E. Topol [13] to make reference to the contemporary availability and ubiquity of the digital technologies (including smartphones) that may support, e.g. the self-monitoring of vital parameters, the social networking, the pervasive connectivity, the imaging capability and the powerful data processing tools.
References
https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. Accessed 28 June 2021
Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC
Tainter J (1988) The collapse of complex societies. Cambridge University Press, Cambridge
Webster A (2007) Health, technology and society. Palgrave Macmillan, Basingstoke and New York
World Economic Forum (2020) The new health paradigm. https://www.weforum.org/videos/the-new-health-paradigm
World Bank (2019) Life expectancy vs. health expenditure 1970 to 2015. https://ourworldindata.org/grapher/life-expectancy-vs-health-expenditure
Porter ME, Lee TH (2013) The strategy that will fix health care. Harv Bus Rev 91(10):50–70
Porter ME (2010) What is value in health care? N Engl J Med 363:26
Kaplan RS, Porter ME (2011) How to solve the cost crisis in health care. Harv Bus Rev 89(9):47–64
Porter ME, Lee TH (2015) Why strategy matters now. N Engl J Med 372:18
Porter ME, Teisberg EO (2006) Redefining health care. Harvard Business School Publishing, Boston
Porter ME (1985) Competitive advantage creating and sustaining superior performance. The Free Press A Division of Macmillan, Inc., New York
Topol E (2012) The creative destruction of medicine. Basic Books, New York
WHO list of priority and medical devices. https://www.who.int/medicaldevices/priority/en
World Health Organization (2007) Everybody's business: Strengthening Health systems to improve health outcomes: Framework for action. WHO, Geneva
De Savigny D, Adam T (eds) (2009) Systems thinking for health systems strengthening. World Health Organization, Geneva
Curi U (2017) Le parole della cura - Medicina e filosofia. Raffaello Cortina Milano (text in Italian)
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Boccato, C., Cerutti, S., Vienken, J. (2022). The Medical Devices Promise to the Healthcare System. In: Boccato, C., Cerutti, S., Vienken, J. (eds) Medical Devices. Research for Development. Springer, Cham. https://doi.org/10.1007/978-3-030-85653-3_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-85653-3_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-85652-6
Online ISBN: 978-3-030-85653-3
eBook Packages: EngineeringEngineering (R0)