Abstract
The amino acid PET tracer L3,4-dihydroxy-6-[18F]fluoro-L-phenylalanine (FDOPA), a radiolabeled analog of L-DOPA, is indicated for the molecular imaging of metabolic abnormalities of presynaptic dopamine transporters and L-type amino acid transporters. In clinical neurology, FDOPA-PET assesses the brain’s dopaminergic function for diagnosing Parkinson’s disease (PD) and differentiation between essential tremor and parkinsonian syndromes. In neuro-oncology, FDOPA-PET uptake measures the rate of L-type amino acid transport activity, given that malignant brain tumors are linked to increased protein synthesis and amino acid transport, resulting in higher uptake than normal tissue. FDOPA-PET is increasingly being used to complement MRI in diagnosing and managing patients with brain tumors, especially gliomas.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FDOPA Imaging for Neuro-oncology
Introduction
MRI is currently the modality of choice for diagnosing and monitoring brain tumors given its high resolution and excellent soft-tissue contrast. MRI is widely available and remains the mainstay for the initial clinical diagnosis, treatment planning, and posttreatment follow-up of brain tumors. A key feature of many high-grade gliomas is the compromise of the blood-brain barrier (BBB), which allows molecules, including intervenous CT and MR contrast, to enter the tumor but not enter a normal brain with an intact BBB. This compromise of the BBB can be detected as tumor enhancement on MRI through gadolinium-based contrast agent administration. However, many low-grade gliomas and some high-grade gliomas, mainly grade III, do not show contrast enhancement. Additionally, many high-grade gliomas that do show contrast enhancement also have substantial non-enhancing regions. Lack of contrast enhancement on MRI makes delineating tumor volumes and surgical margins much more challenging for surgical treatment planning and post-treatment follow-up of brain tumors. In addition, the ability of MRI to differentiate between treatment-induced changes and residual or recurrent tumor is also limited as the imaging features have substantial overlap [1].
Brain PET imaging with amino acid tracers has great potential to provide more accurate and informative imaging in neuro-oncology. MRI alone has limited accuracy for delineating tumor margins and poorly predicts the biological aggressiveness of gliomas, especially when tumors do not enhance with conventional gadolinium-based contrast agents. Several PET tracers have been used to study aspects of brain tumor metabolism [2,3,4,5,6], one of the first was 2-deoxy-2-18F-fluoro-D-glucose (FDG), used to image glucose uptake and glycolytic metabolism. While there is some utility for brain tumor imaging using FDG-PET, there are limitations [7, 8] due to the high physiological glucose metabolism of normal gray matter, which results in modest FDG uptake of low-grade and some recurrent high-grade tumors making detection difficult [9]. Even in brain tumors visible on FDG-PET images, the high uptake of FDG in normal brain makes this tracer unsuitable for establishing tumor margins. Additionally, the specificity of FDG in tumor detection is often limited by uptake in non-tumor regions of inflammation [8, 10, 11].
Amino Acid Tracers in Neuro-oncology: FDOPA-PET
The PET tracer 3′-deoxy-3′-18F-fluorothymidine (FLT) is used to image cellular proliferation and is more sensitive than FDG for detecting recurrent high-grade brain tumors due to the low background uptake of FLT in normal brain tissue. It has also been shown to correlate with the ex vivo Ki-67 proliferation marker and is an overall better prognostic marker of tumor progression and survival than FDG-PET [12]. However, FLT does not readily cross the intact BBB, limiting the evaluation of regions of tumors that do not enhance with contrast [13, 14]. Therefore, FLT is not well-suited to visualize the entire gross tumor volume or tumor margins when non-enhancing tumors are present.
Several amino acid PET tracers have established utility for imaging brain tumors, 11C-methyl-L-methionine (MET), O-(2-[18F]fluoroethyl)-L-tyrosine (FET), and FDOPA [15,16,17,18]. These tracers target the system L substrates that are upregulated in tumors and do not depend on the BBB compromise [19, 20]. LAT1 expression has been shown to positively correlate with FDOPA uptake in resected glioma samples [20]. Unlike contrast-enhanced MRI, radiolabeled amino acid substrates transported by system L can visualize both contrast-enhancing and non-enhancing brain tumors [21, 22]. The two most widely used PET tracers for brain tumor imaging are MET and FET [23, 24]. MET is an essential amino acid-labeled carbon-11, and despite its efficacy, the short half-life of 20 minutes limits its use to sites with an in-house cyclotron facility. FET was developed in the late 1990s to provide an 18F-labeled amino acid PET tracer with a longer half-life (110 minutes) suitable for batch production and remote distribution. Studies directly comparing FET to MET for the characterization of brain tumors and differentiation of residual or recurrent tumor from treatment-related changes have shown these tracers to be very similar [24, 25].
FDOPA has been shown to have very similar brain tumor imaging properties to MET as expected from their shared transport mechanism. In a study directly comparing MET and FDOPA uptake in the same patients, mean tumor to contralateral SUV ratios were almost identical (2.05 for MET and 2.04 for FDOPA) [26]. In studies directly comparing FDOPA and FET, equivalent sensitivity was observed for high-grade and low-grade gliomas with no substantial difference in tumor uptake pattern seen [27, 28].
In the past several years, multiple studies have explored the use of FDOPA for imaging of newly diagnosed and previously treated brain tumors, including the comparison of FDOPA to MRI, FDG-PET, and MET-PET. In newly diagnosed patients, the sensitivity and specificity of FDOPA-PET in differentiating low-grade from high-grade tumors are similar to MET, varying from 70–96% and 86–100%, respectively, with FDOPA uptake correlating to the grade of the newly diagnosed glioma [21, 29,30,31,32]. The distinction of tumor recurrence or progression from radiation injury has been shown to be possible with the use of FDOPA with a sensitivity of 81.3% and specificity of 84.3% [33]. In a single study, FDOPA tracer uptake (SUVmax) correlated with tumor grade and proliferative activity only in untreated gliomas and not in previously treated gliomas [30]. In a head-to-head comparison, FDOPA is more accurate than FDG for imaging low-grade tumors, evaluating recurrent tumors, and distinguishing tumor recurrence from radiation necrosis [21, 34,35,36]. Compared to contrast-enhanced MRI, the accuracy of FDOPA-PET/CT was higher (97% vs. 80%, respectively) [17]. In a large comparative study with MRI, precise anatomic localization of FDOPA was facilitated by image fusion, with FDOPA-PET detecting both enhancing and non-enhancing tumors [37]. FDOPA has also been shown to be able to predict response in recurring malignant gliomas treated with bevacizumab [38]. A study of FDOPA-PET findings in gliomas correlated with histopathology-validated PET imaging showed that gliomas are underestimated by contrast-enhanced MRI and FDOPA more accurately delineate non-enhancing tumors [39]. This study also demonstrated the clinical utility of FDOPA-PET for guiding stereotactic biopsy by distinguishing areas of higher FDOPA uptake values. Better delineation of tumor margins is of considerable importance, given that gross total resection of gliomas is a primary goal of surgery and is associated with increased survival [40, 41].
The growing body of literature on amino acid PET tracers provides strong evidence of their significant clinical value in neuro-oncology by providing insights into the diagnosis and management of brain tumors and overcoming MRI limitations. Systemic reviews of the use of FDOPA-PET in diagnosing and managing primary brain tumors summarized the value of FDOPA as providing high diagnostic accuracy in the delineation of tumor extent, diagnosis of treatment-related changes, and assessment of treatment response [42, 43].
Image Interpretation
The diagnostic importance of amino acid PET is increasingly recognized and reflected in the response assessment in neuro-oncology (RANO) guidelines, which strongly recommended their use in brain tumor management [44], and by the joint practice guidelines collaboratively developed by the European Association of Nuclear Medicine (EANM), the Society of Nuclear Medicine and Molecular Imaging (SNMMI), the European Association of Neuro-Oncology (EANO), and the working group for Response Assessment in Neuro-oncology with PET (PET-RANO) [45].
The visual assessment of FDOPA-PET images is to identify and locate areas of tracer uptake above the normal brain background using an appropriate color scale, set to the background counts in the lower third of the visual scale range. Standard summation (static) images are used for clinical reading and should be co-registered and fused with a recent high-resolution brain MRI if PET/MRI is not available. A positive FDOPA-PET scan is when the tracer uptake exceeds the background activity in the contralateral cortex. A negative scan is when no increased uptake above background is identified.
The recommended approach for a semi-quantification analysis to measure tracer uptake is performed by calculating the tumor to striatum ratio (TSR) using mean SUV (TSRmean) and maximum SUV (TSRmax) values, respectively. The guidelines note that FDOPA TSR cutoff thresholds for the definition of biological tumor volume have not been validated for all clinical questions.
Currently, there are no established guidelines for processing and determining clinical values using dynamic FDOPA-PET acquisitions.
Clinical Application in Neuro-oncology and PET/MRI
In clinical practice , one of the key utilizations of the hybrid modality PET/MR is in neuro-oncology, given that MRI is the modality of choice for diagnosing and monitoring brain tumors, and PET provides complementary functional information. One of the most successful PET/MRI applications has been in pediatric oncology, providing multiple benefits to these patients by offering a reduction in the total number of imaging studies and necessary sedations, decreasing radiation exposure, and the potential adverse long-term effects from sedation and radiation due to serial imaging. Taken together, the advantages of simultaneous brain PET/MR imaging and a growing list of PET tracers have great potential to significantly improve and simplify patient management in neuro-oncology.
Pediatric and adult brain tumor treatment commonly includes antiangiogenic drugs such as bevacizumab, a humanized anti-VEGF monoclonal antibody. Bevacizumab treatment results in an early decrease in contrast enhancement, which creates problems for imaging evaluation since this apparent decreased vascular permeability and enhancement does not correlate with decreased tumor viability in this setting. Recently, simultaneous FDOPA-PET/MRI was used to monitor the effects of antiangiogenic therapy with bevacizumab in pediatric patients with recurrent gliomas and suggested that FDOPA may better predict response at 3 months after initiating therapy than MRI alone [46].
In this study, tumors were readily visualized with FDOPA-PET/MRI on the baseline study prior to therapy with bevacizumab. The metabolic tumor volume (MTV), defined by a 1.5-fold threshold based on the normal contralateral side uptake, decreased in all patients by varying amounts. After 4 weeks of bevacizumab therapy, the largest MTV decrease was 2% of the baseline MTV (Fig. 13.1) and the smallest decrease was 77% of baseline (Fig. 13.2). Patients with a smaller baseline decrease in MTV had worst clinical outcomes. One patient had two distinct lesions with variable response to therapy; the optic chiasm tumor baseline decrease in MTV was 33%, while that of the optic nerve glioma was 56% (Figs. 13.3 and 13.4).
FDOPA-PET/MRI in a pediatric patient with two distinct tumors with variable response to therapy. Images of the optic nerve glioma obtained prior to therapy (a, red arrows) and after 4 weeks of bevacizumab therapy (b, white arrows). There is a moderate decrease of the metabolic tumor volume (MTV), with 56% remaining
FDOPA-PET/MRI in a pediatric patient with two distinct tumors with variable response to therapy. Images of the optic chiasm glioma obtained prior to therapy (a, red arrows) and after 4 weeks of bevacizumab therapy (b, white arrows). There is a significant decrease of the metabolic tumor volume (MTV), with 33% remaining
Studies using simultaneous FDOPA-PET/MRI images have shown more accurate tumor visualization and delineation in gliomas, and the FDOPA-PET tumor region extended beyond the area defined by T1-weighted contrast enhancement and was variable in size to the area of T2/FLAIR hyperintensity (Figs. 13.5 and 13.6) [47, 48]. One study also integrated imaging findings with biopsy locations, histopathology, and established molecular markers in gliomas and noted that it impacted patient management [47], shown in Figs. 13.7, 13.8, and 13.9.
FDOPA-PET/MRI in an adult patient with anaplastic oligodendroglioma grade III, Ki-67 of 80–90%. (a) FDOPA contour representing the region of tumor uptake based on the tumor to normal brain ratio (TBR) > 1.5 (yellow outline). (b) FLAIR contour delineating the region of hyperintensity (magenta outline). (c) TBR contour superimposed on T2/FLAIR illustrates that tumor uptake extends beyond the T2/FLAIR abnormalities (red arrow). (d and e) TBR contour superimposed on T1-weighted MR with contrast. FDOPA-PET demonstrates higher sensitivity than MR T1-weighted with contrast and T2/FLAIR signal intensity abnormalities to delineate the non-enhancing tumor. (Courtesy of Dr. Jonathan McConathy, Director, Division of Molecular Imaging and Therapeutics, The University of Alabama at Birmingham, Birmingham, Alabama, United States)
FDOPA-PET/MRI in an adult patient with anaplastic oligodendroglioma, WHO grade III, Ki-67 of 80–90%. (a and c) FDOPA contour represents the region of tumor uptake based on the tumor to normal brain ratio (TBR) > 1.5 (magenta outline). (b–d) TBR contour superimposed on T1-weighted MR with contrast. Contralateral normal brain used as the reference region (yellow outline). MRI T1-contrast does not reliably reflect areas of viable brain tumor. The FDOPA-PET impacted the selection of biopsy sites and resection. (a–d) Red arrows indicate the stereotactic biopsy sites
FDOPA-PET/MRI in an adult patient was recurrent anaplastic astrocytoma, WHO grade III, Ki-67 of 10.5%. (a and b) Left frontal non-enhancing and T2/FLAIR hyperintensity that was initially reported as stable post-treatment changes (red arrows). (c and d) Marked focal increased FDOPA avidity (white arrows) in the follow-up of previously treated astrocytoma, consistent with tumor recurrence. FDOPA-PET/MRI was more accurate than MRI alone in distinguishing between tumor recurrence and radiation necrosis
FDOPA Imaging for Dopaminergic System
Introduction
The dopaminergic system is associated with numerous neurological disorders (Parkinson’s disease, Huntington’s disease, tardive dyskinesia) and psychiatric disorders (depression, addiction, and schizophrenia), given the significant role it plays in several functions, including motor, memory, cognition, and emotions. Parkinson’s disease (PD) is a chronic neurodegenerative disorder clinically characterized by asymmetric parkinsonism (bradykinesia, tremor, rigidity, and postural instability) and progressive loss of dopamine neurons in the midbrain with resulting dopaminergic deafferentation of the basal ganglia [49]. The pathological hallmarks of PD are degeneration of the nigrostriatal dopaminergic system and the presence of Lewy bodies and neurites, intracellular inclusions of aggregated α-synuclein, and other proteins such as ubiquitin [50]. Parkinsonian syndromes are a group of disorders that shared the clinical signs of PD but are considered separate conditions based on their different pathologies. Atypical parkinsonism syndromes are other neurodegenerative diseases associated with parkinsonism, and the most common being multiple system atrophy, corticobasal degeneration, progressive supranuclear palsy, and dementia with Lewy bodies (DLB). These conditions are linked with nigrostriatal degeneration, a type of multiple system atrophy. Clinical manifestations of parkinsonism may also be seen by syndromes not associated with nigrostriatal degeneration, such as essential tremor, drug-induced parkinsonism, and vascular parkinsonism [51]. Moreover, difficulties are associated with the clinical differentiation of patients with parkinsonism with dementia from Alzheimer’s disease, given the overlapping features [52].
Dopamine PET-Ligands
Functional imaging with dopamine PET-ligands is used to assess dopamine synthesis, transport, and receptor densities and is performed using single-photon emission computed tomography (SPECT) or PET [53]. These imaging agents can target either presynaptic dopamine transporter and synthesis or postsynaptic D2 dopamine receptors [54]. As an example, we focus here on the PET tracer, FDOPA, which is widely used for presynaptic dopaminergic imaging to distinguish between the different causes of parkinsonism and neurodegenerative versus non-dopamine deficiency etiologies [55, 56]. FDOPA is approved by the European Medicines Agency (EMA) for assessing dopaminergic neuronal integrity in suspected parkinsonian syndromes, and in October 2019, a US academic medical center received US Food and Drug Administration (FDA) approval to manufacture FDOPA for clinical use [57]. Studies have demonstrated that FDOPA-PET scans are able to diagnose presynaptic dopaminergic deficits in early phases of PD with excellent sensitivity and specificity [58].
An accurate diagnosis of PD is a prerequisite for patient management, given that only PD patients clinically respond to antiparkinson drug therapy. Neuroimaging has played an increasingly important role in the differential diagnosis, and various imaging modalities have been used to confirm PD or rule out other parkinsonian syndromes. For example, FDOPA-PET may be used to differentiate LB-type dementias (PD and DLB) from non-LB dementias, such as AD, based on the determination of nigrostriatal degeneration, in which the midbrain striatal uptake becomes more visible due to global reduction of striatal FDOPA uptake [59]. The accurate diagnosis among parkinsonism variants remains challenging using neuroimaging, particularly in the early or mild stages of the disease. Multiple investigators have reported minimal differences in the reduction of FDOPA uptake between PD and parkinsonian syndromes associated with nigrostriatal degeneration, given the overlap between these populations [60, 61]. FDOPA-PET is normal in essential tremor, drug-induced parkinsonism, and psychogenic parkinsonism since these disorders are not associated with pathologic dopaminergic loss [62,63,64].
Neuroimaging with FDOPA-PET has been applied to psychiatric disorders evaluating presynaptic dopaminergic integrity. In a study on depression, FDOPA uptake in the left caudate was significantly lower in depressed patients with psychomotor retardation than in normals, providing direct evidence of a link between dopamine hypofunction and psychomotor retardation in depression [65]. Increased striatal FDOPA accumulation has been reported in patients with psychosis, suggesting an increased synthesis and dopamine turnover in these patients [66]. Increased FDOPA uptake was also noted in patients who responded to classic antipsychotics, but not in patients with treatment-resistant schizophrenia, suggesting that dopamine synthesis capacity may be a useful biomarker to predict treatment responsiveness [67]. Several studies have used FDOPA-PET to evaluate dopamine’s role in the human reward system [68] and to assess aging effects and cognitive functions [69], given that reward processing is particularly vulnerable to aging.
Image Interpretation
The EANM and the SNMMI have developed practice guidelines that address dopaminergic imaging’s clinical and technical aspects in parkinsonian syndromes [70]. The diagnostic importance of presynaptic dopaminergic imaging using FDOPA-PET is for detecting loss of nigrostriatal dopaminergic neuron terminals in patients with parkinsonian syndromes. The visual assessment goal is to identify and locate areas of striatal uptake (putamen and caudate nucleus) using an appropriate color scale by setting the maximum color scale value to the maximal tracer value within the striatum. A semi-quantification approach of tracer uptake is performed by calculating the striato-occipital ratio (SOR) [71], which has been shown to detect subtle asymmetric putamen FDOPA reductions and correlate SOR with ratings of disability. Analysis of dynamic FDOPA-PET time-activity curves (TACs) has been used to quantify and model multiple aspects of FDOPA influx constants (Ki maps) [58].
Visual Assessment
In a negative dopaminergic imaging PET scan, the normal striata show a comma-shaped with symmetric well-delineated borders on axial images with the maximum uptake corresponding to the putamen. Mild asymmetry may occur in normal subjects.
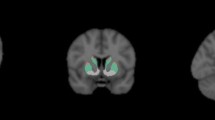
In a positive dopaminergic imaging PET scan, there is a decreased tracer uptake on one or both striata, with an oval or circular shape. An asymmetric pattern of reduced putamen and preserved caudate uptake showing a caudate to putamen posterior-anterior gradient or dot shape is most consistent with parkinsonism syndromes (Fig. 13.10). The locus coeruleus and substantial nigra nuclei may become more visible in nigrostriatal degeneration cases (Figs. 13.11 and 13.12).
FDOPA-PET/MRI demonstrates a positive dopaminergic imaging PET scan. The (a) axial images and (b) coronal images show asymmetric reduced tracer uptake in the putamen, more pronounced in the posterior part creating a posterior-anterior gradient (read arrows) with preserved bilateral tracer uptake in the caudate (white arrows) and right putamen (black arrows). (Courtesy of Dr. Juan M. Chomont, Chief of Radiology at INTECNUS, S.C. de Bariloche, Argentina)
FDOPA-PET/MRI demonstrates locus coeruleus and substantia nigra tracer uptake in a patient with severe nigrostriatal degeneration (a and b: red arrows). Marked bilateral putaminal reduction in tracer binding (c, blue arrows) and normal caudate uptake (c, white arrows). (Courtesy of Dr. Juan M. Chomont, Chief of Radiology at INTECNUS, S.C. de Bariloche, Argentina)
Role of PET/MRI Dopaminergic System Imaging
The introduction of simultaneous PET/MRI in the field of movement disorders is still in the early stages. Recent studies [72,73,74] have focused on better characterization of parkinsonism using PET/MRI. Structural findings on MRI, namely lacunar infarcts or enlarged perivascular spaces found in the basal ganglia and midbrain, may aid in improving PET assessment. These lesions, best identified on MRI, cause decreased striatal uptake depending on their location, mimicking PET features of PD and provide alternative etiologies for the patient’s symptoms.
References
Schwarzenberg J, Czernin J, Cloughesy TF, Ellingson BM, Pope WB, Geist C, et al. 3′-deoxy-3'-18F-fluorothymidine PET and MRI for early survival predictions in patients with recurrent malignant glioma treated with bevacizumab. J Nucl Med. 2012;53(1):29–36. https://doi.org/10.2967/jnumed.111.092387.
Shields AF, Grierson JR, Dohmen BM, Machulla HJ, Stayanoff JC, Lawhorn-Crews JM, et al. Imaging proliferation in vivo with [F-18]FLT and positron emission tomography. Nat Med. 1998;4(11):1334–6. https://doi.org/10.1038/3337.
Heiss WD, Wienhard K, Wagner R, Lanfermann H, Thiel A, Herholz K, et al. F-Dopa as an amino acid tracer to detect brain tumors. J Nucl Med. 1996;37(7):1180–2.
Herholz K, Langen KJ, Schiepers C, Mountz JM. Brain tumors. Semin Nucl Med. 2012;42(6):356–70. https://doi.org/10.1053/j.semnuclmed.2012.06.001.
Heiss WD, Raab P, Lanfermann H. Multimodality assessment of brain tumors and tumor recurrence. J Nucl Med. 2011;52(10):1585–600. https://doi.org/10.2967/jnumed.110.084210.
Gulyas B, Halldin C. New PET radiopharmaceuticals beyond FDG for brain tumor imaging. Q J Nucl Med Mol Imaging. 2012;56(2):173–90.
Olivero WC, Dulebohn SC, Lister JR. The use of PET in evaluating patients with primary brain tumours: is it useful? J Neurol Neurosurg Psychiatry. 1995;58(2):250–2.
Ricci PE, Karis JP, Heiserman JE, Fram EK, Bice AN, Drayer BP. Differentiating recurrent tumor from radiation necrosis: time for re-evaluation of positron emission tomography? AJNR Am J Neuroradiol. 1998;19(3):407–13.
Chen W. Clinical applications of PET in brain tumors. J Nucl Med. 2007;48(9):1468–81.
Bading JR, Shields AF. Imaging of cell proliferation: status and prospects. J Nucl Med. 2008;49(Suppl 2):64S–80S.
Chao ST, Suh JH, Raja S, Lee SY, Barnett G. The sensitivity and specificity of FDG PET in distinguishing recurrent brain tumor from radionecrosis in patients treated with stereotactic radiosurgery. Int J Cancer. 2001;96(3):191–7.
Chen W, Cloughesy T, Kamdar N, Satyamurthy N, Bergsneider M, Liau L, et al. Imaging proliferation in brain tumors with 18F-FLT PET: comparison with 18F-FDG. J Nucl Med. 2005;46(6):945–52.
Tripathi M, Sharma R, D'Souza M, Jaimini A, Panwar P, Varshney R, et al. Comparative evaluation of F-18 FDOPA, F-18 FDG, and F-18 FLT-PET/CT for metabolic imaging of low grade gliomas. Clin Nucl Med. 2009;34(12):878–83.
Shinomiya A, Miyake K, Okada M, Nakamura T, Kawai N, Kushida Y, et al. 3'-Deoxy-3′-[(18)F]-fluorothymidine ([(18)F]-FLT) transport in newly diagnosed glioma: correlation with nucleoside transporter expression, vascularization, and blood-brain barrier permeability. Brain Tumor Pathol. 2013;30(4):215–23. https://doi.org/10.1007/s10014-013-0136-2.
Neuner I, Kaffanke JB, Langen KJ, Kops ER, Tellmann L, Stoffels G, et al. Multimodal imaging utilising integrated MR-PET for human brain tumour assessment. Eur Radiol. 2012;22(12):2568–80. https://doi.org/10.1007/s00330-012-2543-x.
Glaudemans AW, Enting RH, Heesters MA, Dierckx RA, van Rheenen RW, Walenkamp AM, et al. Value of 11C-methionine PET in imaging brain tumours and metastases. Eur J Nucl Med Mol Imaging. 2013;40(4):615–35. https://doi.org/10.1007/s00259-012-2295-5.
Karunanithi S, Sharma P, Kumar A, Khangembam BC, Bandopadhyaya GP, Kumar R, et al. Comparative diagnostic accuracy of contrast-enhanced MRI and (18)F-FDOPA PET-CT in recurrent glioma. Eur Radiol. 2013;23(9):2628–35. https://doi.org/10.1007/s00330-013-2838-6.
Dunet V, Pomoni A, Hottinger A, Nicod-Lalonde M, Prior JO. Performance of 18F-FET versus 18F-FDG-PET for the diagnosis and grading of brain tumors: systematic review and meta-analysis. Neuro-Oncology. 2016;18(3):426–34. https://doi.org/10.1093/neuonc/nov148.
del Amo EM, Urtti A, Yliperttula M. Pharmacokinetic role of L-type amino acid transporters LAT1 and LAT2. Eur J Pharm Sci. 2008;35(3):161–74. https://doi.org/10.1016/j.ejps.2008.06.015.
Youland RS, Kitange GJ, Peterson TE, Pafundi DH, Ramiscal JA, Pokorny JL, et al. The role of LAT1 in (18)F-DOPA uptake in malignant gliomas. J Neuro-Oncol. 2013;111(1):11–8. https://doi.org/10.1007/s11060-012-0986-1.
Chen W, Silverman DH, Delaloye S, Czernin J, Kamdar N, Pope W, et al. 18F-FDOPA PET imaging of brain tumors: comparison study with 18F-FDG PET and evaluation of diagnostic accuracy. J Nucl Med. 2006;47(6):904–11.
Walter F, Cloughesy T, Walter MA, Lai A, Nghiemphu P, Wagle N, et al. Impact of 3,4-dihydroxy-6-18F-fluoro-L-phenylalanine PET/CT on managing patients with brain tumors: the referring physician's perspective. J Nucl Med. 2012;53(3):393–8. https://doi.org/10.2967/jnumed.111.095711.
Singhal T, Narayanan TK, Jain V, Mukherjee J, Mantil J. [11C]-L-methionine positron emission tomography in the clinical management of cerebral gliomas. Mol Imaging Biol. 2008;10(1):1–18.
Grosu AL, Astner ST, Riedel E, Nieder C, Wiedenmann N, Heinemann F, et al. An interindividual comparison of O-(2-[18F]fluoroethyl)-L-tyrosine (FET)- and L-[methyl-11C]methionine (MET)-PET in patients with brain gliomas and metastases. Int J Radiat Oncol Biol Phys. 2011;81(4):1049–58. https://doi.org/10.1016/j.ijrobp.2010.07.002.
Weber WA, Wester HJ, Grosu AL, Herz M, Dzewas B, Feldmann HJ, et al. O-(2-[18F]fluoroethyl)-L-tyrosine and L-[methyl-11C]methionine uptake in brain tumours: initial results of a comparative study. Eur J Nucl Med. 2000;27(5):542–9.
Becherer A, Karanikas G, Szabo M, Zettinig G, Asenbaum S, Marosi C, et al. Brain tumour imaging with PET: a comparison between [18F]fluorodopa and [11C]methionine. Eur J Nucl Med Mol Imaging. 2003;30(11):1561–7.
Kratochwil C, Combs SE, Leotta K, Afshar-Oromieh A, Rieken S, Debus J, et al. Intra-individual comparison of (1)(8)F-FET and (1)(8)F-DOPA in PET imaging of recurrent brain tumors. Neuro-Oncology. 2014;16(3):434–40. https://doi.org/10.1093/neuonc/not199.
Lapa C, Linsenmann T, Monoranu CM, Samnick S, Buck AK, Bluemel C, et al. Comparison of the amino acid tracers 18F-FET and 18F-DOPA in high-grade glioma patients. J Nucl Med. 2014;55(10):1611–6. https://doi.org/10.2967/jnumed.114.140608.
Tsuyuguchi N, Sunada I, Iwai Y, Yamanaka K, Tanaka K, Takami T, et al. Methionine positron emission tomography of recurrent metastatic brain tumor and radiation necrosis after stereotactic radiosurgery: is a differential diagnosis possible? J Neurosurg. 2003;98(5):1056–64. https://doi.org/10.3171/jns.2003.98.5.1056.
Fueger BJ, Czernin J, Cloughesy T, Silverman DH, Geist CL, Walter MA, et al. Correlation of 6-18F-fluoro-L-dopa PET uptake with proliferation and tumor grade in newly diagnosed and recurrent gliomas. J Nucl Med. 2010;51(10):1532–8. https://doi.org/10.2967/jnumed.110.078592.
Nioche C, Soret M, Gontier E, Lahutte M, Dutertre G, Dulou R, et al. Evaluation of quantitative criteria for glioma grading with static and dynamic 18F-FDopa PET/CT. Clin Nucl Med. 2013;38(2):81–7. https://doi.org/10.1097/RLU.0b013e318279fd5a.
Terakawa Y, Tsuyuguchi N, Iwai Y, Yamanaka K, Higashiyama S, Takami T, et al. Diagnostic accuracy of 11C-methionine PET for differentiation of recurrent brain tumors from radiation necrosis after radiotherapy. J Nucl Med. 2008;49(5):694–9. https://doi.org/10.2967/jnumed.107.048082.
Lizarraga KJ, Allen-Auerbach M, Czernin J, DeSalles AA, Yong WH, Phelps ME, et al. (18)F-FDOPA PET for differentiating recurrent or progressive brain metastatic tumors from late or delayed radiation injury after radiation treatment. J Nucl Med. 2014;55(1):30–6. https://doi.org/10.2967/jnumed.113.121418.
Jacob MJ, Pandit AG, Jora C, Mudalsha R, Sharma A, Pathak HC. Comparative study of (18)F-DOPA, (13)N-Ammonia and F18-FDG PET/CT in primary brain tumors. Indian J Nucl Med. 2011;26(3):139–43. https://doi.org/10.4103/0972-3919.103996.
Jora C, Mattakarottu JJ, Aniruddha PG, Mudalsha R, Singh DK, Pathak HC, et al. Comparative evaluation of 18F-FDOPA, 13N-AMMONIA, 18F-FDG PET/CT and MRI in primary brain tumors - a pilot study. Indian J Nucl Med. 2011;26(2):78–81. https://doi.org/10.4103/0972-3919.90256.
Karunanithi S, Sharma P, Kumar A, Khangembam BC, Bandopadhyaya GP, Kumar R, et al. 18F-FDOPA PET/CT for detection of recurrence in patients with glioma: prospective comparison with 18F-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2013;40(7):1025–35. https://doi.org/10.1007/s00259-013-2384-0.
Ledezma CJ, Chen W, Sai V, Freitas B, Cloughesy T, Czernin J, et al. 18F-FDOPA PET/MRI fusion in patients with primary/recurrent gliomas: initial experience. Eur J Radiol. 2009;71(2):242–8. https://doi.org/10.1016/j.ejrad.2008.04.018.
Harris RJ, Cloughesy TF, Pope WB, Nghiemphu PL, Lai A, Zaw T, et al. 18F-FDOPA and 18F-FLT positron emission tomography parametric response maps predict response in recurrent malignant gliomas treated with bevacizumab. Neuro-Oncology. 2012;14(8):1079–89. https://doi.org/10.1093/neuonc/nos141.
Pafundi DH, Laack NN, Youland RS, Parney IF, Lowe VJ, Giannini C, et al. Biopsy validation of 18F-DOPA PET and biodistribution in gliomas for neurosurgical planning and radiotherapy target delineation: results of a prospective pilot study. Neuro-Oncology. 2013;15(8):1058–67. https://doi.org/10.1093/neuonc/not002.
Schomas DA, Laack NN, Brown PD. Low-grade gliomas in older patients: long-term follow-up from Mayo Clinic. Cancer. 2009;115(17):3969–78. https://doi.org/10.1002/cncr.24444.
Kreth FW, Thon N, Simon M, Westphal M, Schackert G, Nikkhah G, et al. Gross total but not incomplete resection of glioblastoma prolongs survival in the era of radiochemotherapy. Ann Oncol. 2013;24(12):3117–23. https://doi.org/10.1093/annonc/mdt388.
Somme F, Bender L, Namer IJ, Noel G, Bund C. Usefulness of (18)F-FDOPA PET for the management of primary brain tumors: a systematic review of the literature. Cancer Imaging. 2020;20(1):70. https://doi.org/10.1186/s40644-020-00348-5.
Xiao J, Jin Y, Nie J, Chen F, Ma X. Diagnostic and grading accuracy of (18)F-FDOPA PET and PET/CT in patients with gliomas: a systematic review and meta-analysis. BMC Cancer. 2019;19(1):767. https://doi.org/10.1186/s12885-019-5938-0.
Albert NL, Weller M, Suchorska B, Galldiks N, Soffietti R, Kim MM, et al. Response Assessment in Neuro-Oncology working group and European Association for Neuro-Oncology recommendations for the clinical use of PET imaging in gliomas. Neuro-Oncology. 2016;18(9):1199–208. https://doi.org/10.1093/neuonc/now058.
Law I, Albert NL, Arbizu J, Boellaard R, Drzezga A, Galldiks N, et al. Joint EANM/EANO/RANO practice guidelines/SNMMI procedure standards for imaging of gliomas using PET with radiolabelled amino acids and [(18)F]FDG: version 1.0. Eur J Nucl Med Mol Imaging. 2019;46(3):540–57. https://doi.org/10.1007/s00259-018-4207-9.
Gauvain K, Ponisio MR, Barone A, Grimaldi M, Parent E, Leeds H, et al. (18)F-FDOPA PET/MRI for monitoring early response to bevacizumab in children with recurrent brain tumors. Neurooncol Pract. 2018;5(1):28–36. https://doi.org/10.1093/nop/npx008.
Ponisio MR, McConathy JE, Dahiya SM, Miller-Thomas MM, Rich KM, Salter A, et al. Dynamic (18)F-FDOPA-PET/MRI for the preoperative evaluation of gliomas: correlation with stereotactic histopathology. Neurooncol Pract. 2020;7(6):656–67. https://doi.org/10.1093/nop/npaa044.
Blanchet EM, Millo C, Martucci V, Maass-Moreno R, Bluemke DA, Pacak K. Integrated whole-body PET/MRI with 18F-FDG, 18F-FDOPA, and 18F-FDA in paragangliomas in comparison with PET/CT: NIH first clinical experience with a single-injection, dual-modality imaging protocol. Clin Nucl Med. 2014;39(3):243–50. https://doi.org/10.1097/RLU.0000000000000289.
Lees AJ, Hardy J, Revesz T. Parkinson's disease. Lancet. 2009;373(9680):2055–66. https://doi.org/10.1016/S0140-6736(09)60492-X.
Berardelli A, Wenning GK, Antonini A, Berg D, Bloem BR, Bonifati V, et al. EFNS/MDS-ES/ENS [corrected] recommendations for the diagnosis of Parkinson's disease. Eur J Neurol. 2013;20(1):16–34. https://doi.org/10.1111/ene.12022.
Brooks DJ. Parkinson's disease: diagnosis. Parkinsonism Relat Disord. 2012;18(Suppl 1):S31–3. https://doi.org/10.1016/S1353-8020(11)70012-8.
Rizzo G, Copetti M, Arcuti S, Martino D, Fontana A, Logroscino G. Accuracy of clinical diagnosis of Parkinson disease: a systematic review and meta-analysis. Neurology. 2016;86(6):566–76. https://doi.org/10.1212/WNL.0000000000002350.
Thobois S, Jahanshahi M, Pinto S, Frackowiak R, Limousin-Dowsey P. PET and SPECT functional imaging studies in parkinsonian syndromes: from the lesion to its consequences. NeuroImage. 2004;23(1):1–16. https://doi.org/10.1016/j.neuroimage.2004.04.039.
Elsinga PH, Hatano K, Ishiwata K. PET tracers for imaging of the dopaminergic system. Curr Med Chem. 2006;13(18):2139–53. https://doi.org/10.2174/092986706777935258.
Kumakura Y, Cumming P. PET studies of cerebral levodopa metabolism: a review of clinical findings and modeling approaches. Neuroscientist. 2009;15(6):635–50. https://doi.org/10.1177/1073858409338217.
Sarikaya I. PET imaging in neurology: Alzheimer's and Parkinson's diseases. Nucl Med Commun. 2015;36(8):775–81. https://doi.org/10.1097/MNM.0000000000000320.
U.S. FDA. Highlights of prescribing information fluorodopa F 18. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/200655s000lbl.pdf. Accessed 10/2019.
Sossi V, de La Fuente-Fernandez R, Holden JE, Doudet DJ, McKenzie J, Stoessl AJ, et al. Increase in dopamine turnover occurs early in Parkinson's disease: evidence from a new modeling approach to PET 18 F-fluorodopa data. J Cereb Blood Flow Metab. 2002;22(2):232–9. https://doi.org/10.1097/00004647-200202000-00011.
Pavese N, Rivero-Bosch M, Lewis SJ, Whone AL, Brooks DJ. Progression of monoaminergic dysfunction in Parkinson's disease: a longitudinal 18F-dopa PET study. NeuroImage. 2011;56(3):1463–8. https://doi.org/10.1016/j.neuroimage.2011.03.012.
Burn DJ, Sawle GV, Brooks DJ. Differential diagnosis of Parkinson's disease, multiple system atrophy, and Steele-Richardson-Olszewski syndrome: discriminant analysis of striatal 18F-dopa PET data. J Neurol Neurosurg Psychiatry. 1994;57(3):278–84. https://doi.org/10.1136/jnnp.57.3.278.
Eidelberg D, Dhawan V, Moeller JR, Sidtis JJ, Ginos JZ, Strother SC, et al. The metabolic landscape of cortico-basal ganglionic degeneration: regional asymmetries studied with positron emission tomography. J Neurol Neurosurg Psychiatry. 1991;54(10):856–62. https://doi.org/10.1136/jnnp.54.10.856.
Niccoli Asabella A, Gigante AF, Ferrari C, Di Palo A, Rubini D, Mossa EP, et al. Role of dopaminergic neurotransmission in pathophysiology of action tremor in Parkinson's disease. Hell J Nucl Med. 2015;18(Suppl 1):11–6.
Burn DJ, Brooks DJ. Nigral dysfunction in drug-induced parkinsonism: an 18F-dopa PET study. Neurology. 1993;43(3 Pt 1):552–6. https://doi.org/10.1212/wnl.43.3_part_1.552.
Tolosa E, Coelho M, Gallardo M. DAT imaging in drug-induced and psychogenic parkinsonism. Mov Disord. 2003;18(Suppl 7):S28–33. https://doi.org/10.1002/mds.10575.
Martinot M, Bragulat V, Artiges E, Dolle F, Hinnen F, Jouvent R, et al. Decreased presynaptic dopamine function in the left caudate of depressed patients with affective flattening and psychomotor retardation. Am J Psychiatry. 2001;158(2):314–6. https://doi.org/10.1176/appi.ajp.158.2.314.
McCutcheon R, Beck K, Jauhar S, Howes OD. Defining the locus of dopaminergic dysfunction in schizophrenia: a meta-analysis and test of the mesolimbic hypothesis. Schizophr Bull. 2018;44(6):1301–11. https://doi.org/10.1093/schbul/sbx180.
Kim E, Howes OD, Veronese M, Beck K, Seo S, Park JW, et al. Presynaptic dopamine capacity in patients with treatment-resistant schizophrenia taking clozapine: an [(18)F]DOPA PET study. Neuropsychopharmacology. 2017;42(4):941–50. https://doi.org/10.1038/npp.2016.258.
Smith CT, Wallace DL, Dang LC, Aarts E, Jagust WJ, D'Esposito M, et al. Modulation of impulsivity and reward sensitivity in intertemporal choice by striatal and midbrain dopamine synthesis in healthy adults. J Neurophysiol. 2016;115(3):1146–56. https://doi.org/10.1152/jn.00261.2015.
Kumakura Y, Vernaleken I, Buchholz HG, Borghammer P, Danielsen E, Grunder G, et al. Age-dependent decline of steady state dopamine storage capacity of human brain: an FDOPA PET study. Neurobiol Aging. 2010;31(3):447–63. https://doi.org/10.1016/j.neurobiolaging.2008.05.005.
Morbelli S, Esposito G, Arbizu J, Barthel H, Boellaard R, Bohnen NI, et al. EANM practice guideline/SNMMI procedure standard for dopaminergic imaging in Parkinsonian syndromes 1.0. Eur J Nucl Med Mol Imaging. 2020;47(8):1885–912. https://doi.org/10.1007/s00259-020-04817-8.
Takikawa S, Dhawan V, Chaly T, Robeson W, Dahl R, Zanzi I, et al. Input functions for 6-[fluorine-18]fluorodopa quantitation in parkinsonism: comparative studies and clinical correlations. J Nucl Med. 1994;35(6):955–63.
Zhao P, Zhang B, Gao S, Li X. Clinical features, MRI, and 18F-FDG-PET in differential diagnosis of Parkinson disease from multiple system atrophy. Brain Behav. 2020;10(11):e01827. https://doi.org/10.1002/brb3.1827.
Struck AF, Hall LT, Kusmirek JE, Gallagher CL, Floberg JM, Jaskowiak CJ, et al. (18)F-DOPA PET with and without MRI fusion, a receiver operator characteristics comparison. Am J Nucl Med Mol Imaging. 2012;2(4):475–82.
Teune LK, Renken RJ, de Jong BM, Willemsen AT, van Osch MJ, Roerdink JB, et al. Parkinson's disease-related perfusion and glucose metabolic brain patterns identified with PCASL-MRI and FDG-PET imaging. Neuroimage Clin. 2014;5:240–4. https://doi.org/10.1016/j.nicl.2014.06.007.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ponisio, M.R., Iranpour, P., Benzinger, T.L.S. (2022). FDOPA in Movement Disorders and Neuro-Oncology . In: Franceschi, A.M., Franceschi, D. (eds) Hybrid PET/MR Neuroimaging. Springer, Cham. https://doi.org/10.1007/978-3-030-82367-2_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-82367-2_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-82366-5
Online ISBN: 978-3-030-82367-2
eBook Packages: MedicineMedicine (R0)