Abstract
There have been marked changes in the management of metastatic renal cell carcinoma (mRCC). Prognosis in the era of interleukin-2 was poor, with a median survival estimated at approximately 1 year. Now, with multiple targeted therapies and checkpoint inhibitors approved, median survival has more than tripled for patients with this disease. One issue that has arisen is how to optimally sequence therapies. At present, it is largely clinical judgment that guides application. In this chapter, we outline the emerging role of biomarkers in renal cell carcinoma, ranging from exploratory markers such as the microbiome to more well-established tissue-based predictors such as programmed death-ligand 1 (PD-L1) expression. Through this approach, we attempt to offer further context around how biomarkers may ultimately be applied in clinical practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
In 2020, an estimated 73,750 number of patients will be diagnosed with renal cell carcinoma (RCC), and of these, 14,830 may die of the disease [1]. Of those diagnosed, the vast majority (~90%) will present with localized disease. For patients with localized disease, the cornerstone of therapy is surgery – depending on a number of factors including size and extent, partial nephrectomy or radical nephrectomy may be attempted. For individuals who have significant comorbidity and for those with smaller lesions, local approaches such as cryoablation or radiofrequency ablation may be feasible. One challenge is that, despite the use of these definitive interventions, patients may still recur with metastatic disease. While improvements in systemic therapy have occurred, the unfortunate reality is that most patients with metastatic disease are incurable.
For this reason, aggressive efforts have been made to develop adjuvant therapies for RCC. The US FDA approved adjuvant therapy with sunitinib in 2017; this was based on the phase III S-TRAC clinical trial [2]. However, this study was quite controversial given the demonstration of only a modest benefit in disease-free survival (DFS) with sunitinib over placebo in patients with high-risk localized RCC. Furthermore, the study demonstrated no benefit in overall survival (OS). Flanking this dataset were several other publications that cited no benefit with adjuvant targeted therapy. For example, the ASSURE trial compared sunitinib and sorafenib to placebo and showed no benefit in DFS or OS, and the PROTECT trial comparing pazopanib to placebo had similar results [3]. With this in mind, attention has turned to the development of adjuvant immunotherapy approaches for localized RCC. Several completed and ongoing studies compare checkpoint inhibitor (CPI) monotherapy or combination therapy for varying durations. These are the subject of other chapters in this textbook.
In the current chapter, we will focus our attention on the role of biomarkers in identifying benefit with immunotherapy for RCC. It is well recognized that not all patients benefit from immunotherapy, and in the adjuvant setting, where a high therapeutic index is essential, biomarkers may allow for optimized application of immunotherapy.
Predictive Markers of Immunotherapy
PD-L1 Expression
In current clinical practice, CPIs abrogate signaling through three primary targets: (1) cytotoxic T-lymphocyte-associated protein 4 (CTLA4), (2) programmed cell death protein 1 (PD-1), and (3) programmed cell death ligand 1 (PD-L1). PD-1 and CTLA4 are on the T-cell surface, while PD-L1 is expressed on the antigen-presenting cell (APC). Trials in adjuvant therapy for RCC utilize agents directed at each of these targets. The first adjuvant immunotherapy trial to be initiated was IMmotion010, a trial comparing atezolizumab (a PD-L1 inhibitor) to placebo. KEYNOTE-564 was initiated shortly thereafter, comparing pembrolizumab to placebo. Other perioperative trials have since emerged evaluating nivolumab, durvalumab with tremelimumab, and nivolumab with ipilimumab. Each of these agents has data in the context of metastatic RCC (mRCC), and in most, there is detailed information regarding the prognostic and predictive potential of PD-L1 status.
PD-L1 status is complex – there are a variety of antibodies used to characterize PD-L1, and each has a different sensitivity as well as specificity for tumor and/or immune cells. The phase III CheckMate 214 trial comparing nivolumab with ipilimumab to sunitinib is perhaps the best opportunity to evaluate the role of PD-L1, as the study juxtaposes a targeted therapy regimen against an immunotherapy regimen. A recent update at the 2020 American Society of Clinical Oncology (ASCO) Annual Meeting offered a detailed assessment of PD-L1 status in this trial, using a separate assessment of PD-L1 in tumor cells and a combined positive score (CPS) evaluating PD-L1 expression in both tumor cells and immune cells. For this assessment, the Dako PD-L1 IHC 28-8 antibody was used. In the tumor cell PD-L1 assessment, 754 patients were noted to have <1% expression, while 236 patients had 1% or greater expression. Although the magnitude of survival benefit was greater in those individuals with 1% or greater expression, an OS advantage was seen in both subsets with nivolumab and ipilimumab as compared to sunitinib. Using the PD-L1 CPS yielded a similar observation. Notably, using this method, a total of 384 patients had a score of <1, while 596 had a score of 1 or greater – a more even distribution of patients.
The role of PD-L1 has also been assessed in the context of two other recent pivotal trials in the front-line setting of mRCC, namely, KEYNOTE-426 and JAVELIN Renal 101. The KEYNOTE-426 study compared axitinib with pembrolizumab to sunitinib, while the JAVELIN Renal 101 study compared axitinib with avelumab to sunitinib. Both studies met their primary endpoint of demonstrating a progression-free survival benefit with the combination of axitinib with CPI. Only KEYNOTE-426 has yielded a survival advantage to date, however [4]. Both studies included an assessment of PD-L1 status, with the benefit of combination therapy occurring in both PD-L1-positive and PD-L1-negative groups. Currently, there are no adjuvant trials evaluating a combined strategy of targeted therapy with immunotherapy, but these data may be informative in smaller neoadjuvant trials exploring this concept (e.g., an ongoing study of axitinib with avelumab).
Gene Signatures
One of the most informative biomarker studies to date in mRCC is the randomized, phase II IMmotion150 trial. This study assessed the combination of bevacizumab with atezolizumab compared to atezolizumab monotherapy, with sunitinib representing the control arm. With over 100 patients per arm and robust correlatives, this was a sizeable experience. RNA sequencing allowed for determination of three unique subtypes of patients – (1) an angiogenic profile; (2) T effector high, myeloid inflammation low profile; and (3) T effector high, myeloid inflammation high profile. As the profile name implies, patients with an angiogenic profile fared better with VEGF-directed therapy. Patients with a T effector high, myeloid inflammation low profile did similarly well with atezolizumab monotherapy and the combination with bevacizumab. Interestingly, patients with a T effector high, myeloid inflammation high profile “required” the combination of bevacizumab with atezolizumab [5].
This gene signature from IMmotion150 has been assessed in the context of several recent studies. In the JAVELIN Renal 101 study, several signatures were assessed. Notably, a 26-gene score was derived within the JAVELIN study that included a diverse array of immune response genes – a high score using this metric was able to discern superior outcome with the combination of axitinib with avelumab as compared to sunitinib. When the IMmotion150 score was applied in the JAVELIN Renal 101 study, it was interesting to note that the angiogenesis-high group fared better with sunitinib – no other significant differences were noted [6].
RNA sequencing data was also recently presented from the CheckMate 214 study. In this undertaking, 109 specimens were available from patients receiving nivolumab with ipilimumab, and 104 samples were available from patients receiving sunitinib. Within this limited subset, various gene signatures (including the IMmotion150 and JAVELIN Renal 101 signatures) were explored. Interestingly, the only notable differences were in the angiogenic score once again. Consistent with the previous experience, patients with a high angiogenic score appear to fare better with sunitinib as compared to nivolumab with ipilimumab with respect to progression-free survival. However, there is no significant difference in OS [7].
Genomic Predictors of Outcome
There is emerging evidence that, beyond genomic signatures, single genes may be effective predictors of clinical outcome. PBRM1 is a chromatin remodeling gene that may be associated with immunotherapy response. In a study combining patients from a prospective assessment of nivolumab in mRCC with several institutional registries, response to immunotherapy appeared to be enriched in those patients with PBRM1 mutation. This high-profile publication was followed by several efforts to validate PBRM1 in recent phase III clinical trials. In the JAVELIN Renal 101 study, no association between PBRM1 and outcome was reported [6]. Furthermore, in a recent assessment of patients in CheckMate 214, there was also no significant difference in PFS or OS based on PBRM1 status [7].
As the quest for novel biomarkers continues, our group has recently reported an assessment of 91 patients with mRCC. In our study, we identified 58 patients who had received VEGF-TKI and/or immunotherapy [8]. TERT promoter mutations were associated with lack of clinical benefit with immunotherapy in this cohort. Given the limited sample size, prospective validation of these findings is warranted.
Microbiome
A fascinating but admittedly early foray in biomarker research in mRCC is evaluation of the microbiome. Our group was the first to characterize the microbiome in mRCC. In a small cohort of 20 patients with mRCC, we collected stool and performed 16S ribosomal RNA profiling at varying timepoints during VEGF-TKI therapy [9]. Our findings indicated that higher levels of Bacteroides spp. were found in patients with treatment-induced diarrhea; lower levels of Prevotella spp. were found in the same patients.
More sophisticated metagenomic sequencing has since evolved to characterize gut bacterial composition. This was applied in a large series of patients with both mRCC and metastatic non-small cell lung cancer treated at the Institut Gustave Roussy. In 40 patients with mRCC, it was suggested that higher levels of Akkermansia spp. were associated with treatment response [10]. In separately published studies, the same group has also identified that antibiotic use may potentially influence clinical outcome, perhaps by reducing populations of “immunotherapy-sensitizing bacteria” [11].
Our group has recently performed a detailed study of 31 patients with mRCC initiating therapy with checkpoint inhibitors. Stool was collected at baseline and at varying timepoints during therapy. In contrast to the French group, our study pointed most strongly to Prevotella copri as a predictor of immunotherapy response. As we were able to temporally characterize changes in stool profile, our findings did suggest an increase in Akkermansia spp. in those patients who responded to immunotherapy. Finally, our results also suggested that stool bacterial diversity correlated with treatment response.
These cumulative results have led to the design of a randomized, phase I study exploring the probiotic CBM-588 in combination with immunotherapy. CBM-588 represents spores of Clostridium butyricum. Spores of C. butyricum theoretically generate and release butyrate in the lower intestinal tract. By doing so, they may enhance proliferation of Bifidobacteria and other species that have been associated with treatment response.
Conclusions and Future Directions
The biomarkers discussed herein are the most well established we have to predict outcome with immunotherapy in patients with RCC. Of course, these have all been validated in the metastatic setting. Definitive data for these biomarkers in the non-metastatic setting will only emerge once there are preliminary data available from the phase III trials evaluating adjuvant immunotherapy. Smaller studies of neoadjuvant therapy may provide some insight but will unlikely be practice changing.
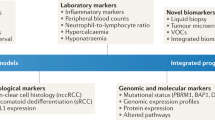
It is of critical importance that this research progresses in the adjuvant setting. Immunotherapy, although well tolerated by many patients, does come with potentially severe consequences. Reports of rapid and fatal myocarditis have recently emerged in the literature, and truthfully, any immune-related toxicity can have dire consequences if not managed aggressively and in a timely fashion. Using biomarkers to identify those individuals who are most prone to benefit from immunotherapy will ultimately limit unnecessary exposure to these agents. Although a considerable investment in time, money, and effort, this line of research is bound to save lives (Fig. 17.1 and Table 17.1).
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30. https://doi.org/10.3322/caac.21590.
Ravaud A, Motzer RJ, Pandha HS, George DJ, Pantuck AJ, Patel A, et al. Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N Engl J Med. 2016;375:2246–54. https://doi.org/10.1056/NEJMoa1611406.
Pal SK, Haas NB. Adjuvant therapy for renal cell carcinoma: past, present, and future. Oncologist. 2014;19:851–9. https://doi.org/10.1634/theoncologist.2014-0105.
Rini BI, Plimack ER, Stus V, Gafanov R, Hawkins R, Nosov D, et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380:1116–27. https://doi.org/10.1056/NEJMoa1816714.
McDermott DF, Huseni MA, Atkins MB, Motzer RJ, Rini BI, Escudier B, et al. Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat Med. 2018;24:749–57. https://doi.org/10.1038/s41591-018-0053-3.
Choueiri TK, Albiges L, Haanen JBAG, Larkin JMG, Uemura M, Pal SK, et al. Biomarker analyses from JAVELIN renal 101: Avelumab + axitinib (A + Ax) versus sunitinib (S) in advanced renal cell carcinoma (aRCC). J Clinic Oncol. 2019;37:101. https://doi.org/10.1200/JCO.2019.37.15_suppl.101.
Motzer RJ, Choueiri TK, McDermott DF, Powles T, Yao J, Ammar R, et al. Biomarker analyses from the phase III CheckMate 214 trial of nivolumab plus ipilimumab (N+I) or sunitinib (S) in advanced renal cell carcinoma (aRCC). J Clinic Oncol. 2020;38:5009. https://doi.org/10.1200/JCO.2020.38.15_suppl.5009.
Dizman N, Lyou Y, Salgia N, Bergerot PG, Hsu J, Enriquez D, et al. Correlates of clinical benefit from immunotherapy and targeted therapy in metastatic renal cell carcinoma: comprehensive genomic and transcriptomic analysis. J Immunother Cancer. 2020;8:e000953. https://doi.org/10.1136/jitc-2020-000953.
Pal SK, Li SM, Wu X, Qin H, Kortylewski M, Hsu J, et al. Stool bacteriomic profiling in patients with metastatic renal cell carcinoma receiving vascular endothelial growth factor-tyrosine kinase inhibitors. Clin Cancer Res. 2015;21:5286–93. https://doi.org/10.1158/1078-0432.CCR-15-0724.
Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillère R, et al. Gut microbiome influences efficacy of PD-1–based immunotherapy against epithelial tumors. Science. 2018;359(91) https://doi.org/10.1126/science.aan3706.
Derosa L, Hellmann MD, Spaziano M, Halpenny D, Fidelle M, Rizvi H, et al. Negative association of antibiotics on clinical activity of immune checkpoint inhibitors in patients with advanced renal cell and non-small-cell lung cancer. Ann Oncol. 2018;29:1437–44. https://doi.org/10.1093/annonc/mdy103.
Disclosures
SKP reports previous consulting roles for Genentech, Aveo, Eisai, Roche, Pfizer, Novartis, Exelixis, Ipsen, BMS, and Astellas.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Malhotra, J., Meza, L., Salgia, N., Pal, S.K. (2022). Predictive Biomarkers of Immunotherapy Efficacy in RCC and Their Role in Non-metastatic Stages. In: Necchi, A., Spiess, P.E. (eds) Neoadjuvant Immunotherapy Treatment of Localized Genitourinary Cancers. Springer, Cham. https://doi.org/10.1007/978-3-030-80546-3_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-80546-3_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-80545-6
Online ISBN: 978-3-030-80546-3
eBook Packages: MedicineMedicine (R0)