Abstract
The classical myeloproliferative neoplasms (MPN) are characterized by clonal expansion of one or more hematopoietic cell lineages and are driven by mutations that activate constitutive signaling via JAK2 pathway. The criteria for diagnosis have now been defined by the World Health Organization (WHO) and the term MPN as is currently used encompasses the entities of primary myelofibrosis, polycythemia vera, and essential thrombocytosis. There is imperfect correlation between the genotype and disease phenotype in MPN and the latter is determined by a variety of patient factors that are independent of the driver mutation. The disease course in MPN can span decades and accurate risk assessment is critical in the choice of therapy and treatment is largely geared toward prevention of complications and providing symptomatic relief. Although new agents have been approved in recent years, no therapy has been convincingly shown to alter disease progression and allogeneic hematopoietic stem cell transplantation (HCT) remains the only curative therapy known to date.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
9.1 Introduction
William Dameshek first developed the concept of “myeloproliferative disorders” in 1951 to describe a group of bone marrow disorders including chronic myeloid leukemia (CML), polycythemia vera (PV), myelofibrosis (MF), and erythroleukemia [1]. He described them as clonal stem cell disorders in which individual blood cell lineage grew “en masse.” CML is the most common among these and is discussed elsewhere in this volume. The current WHO classification of hematological malignancies includes CML, primary myelofibrosis (PMF), essential thrombocythemia (ET), polycythemia vera (PV) chronic neutrophilic leukemia, chronic eosinophilic leukemia, and Myeloproliferative neoplasm (MPN), unclassifiable under the umbrella of MPN [2]. For the purpose of this chapter, we will focus on the more common entities of PMF, ET, and PV. The phenotype of these entities can overlap to a large degree and they share some common clinical features including hepatosplenomegaly, as well as constitutional symptoms due to aberrant cytokine production, including weight loss, night sweats, fatigue, early satiety, and bone pain. They also share pathophysiological features characterized by elevated peripheral blood counts, hypercellular bone marrow, development of bone marrow fibrosis, and extramedullary hematopoiesis. Over last 2 decades, our understanding of pathophysiology has significantly advanced with the discovery of driver mutations. Initially, in 2005, the seminal discovery of a mutation V617F in JAK (Janus kinase)-2 leading to gain of function was described in PV, ET, and PMF [3]. Subsequently, two more driver mutations in MPL and CALR were discovered [4,5,6] and one of these three mutations is detected in over 90% of these MPNs. These mutations constitutively activate signaling pathways for hematopoiesis. The basis for the association of the same genotype with different phenotypes among the MPNs remains enigmatic to date.
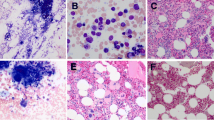
9.2 Diagnosis
The WHO classification of hematologic malignancies has defined diagnostic criteria for PV, ET, and PMF [2]. A bone marrow biopsy is required at the time of diagnosis which can help differentiate these three types of MPN. BCR-ABL1 rearrangement has to be excluded as some forms of CML may look similar morphologically and phenotypically. Criteria for diagnosis of the individual disorders are listed in Tables 9.1 and 9.2.
9.3 Biology and Genetics of MPN
9.3.1 Driver Mutations
The majority of cases of MPN carry one of three mutually exclusive MPN-restricted mutations (JAK2, MPL, or CALR) that drive myeloproliferation. Each of these three different gene mutations ultimately results in constitutive activation of JAK2-dependent cytokine receptor signaling pathways [7]. CALR and MPL mutations are only found in ET or MF, whereas JAK2 mutation can be present in any of the three MPNs. The distribution of these three mutations among MPN is shown in Fig. 9.1.
A somatic mutation in JAK2 was the first driver mutation discovered in BCR-ABL-negative classical MPN and is the most common [3]. The most common mutation in JAK2 is V617F and results from G to T transition at nucleotide 1849 on exon 14 of JAK2 gene on chromosome 9p24.1 resulting in substitution of valine to phenylalanine in the pseudokinase domain. This leads to constitutive ligand-independent activation of JAK2 which is the cognate tyrosine kinase for multiple cytokine receptors including receptors for erythropoietin, thrombopoietin, and granulocyte colony stimulating factor.
The vast majority of PV patients (over 95%) have JAK2 V617F mutation. Among the remainder, about 3% of patients with PV carry JAK2 exon 12 mutations that cause mostly isolated erythrocytosis at the time of diagnosis. JAK2 mutations are present in about ~50% of patients with PV and PMF [8].
Mutations in the thombopoietin receptor gene (MPL) mostly occur in exon 10 of the gene located on chromosome 1p34.2. Among these the most common are W515L and W515K occurring in the juxtamembrane domain of the receptor. Other mutations have been described but are less common [6, 8]. MPL mutations are present in about 8% of PMF and 4% of ET patients [8]. Similar to JAK2 mutations, MPL mutations cause constitutive activation of MPL receptor in the absence of TPO and activate downstream signaling [9].
Mutations in calreticulin gene (CALR) were discovered with ET and PMF patients who were JAK2 and MPL mutation negative, occurring in 67% and 88%, respectively [4]. CALR gene is located on chromosome 19p13.13. CALR works normally as a chaperone that binds to MPL in endoplasmic reticulum. However, mutant CALR binds to the extracellular domain of MPL receptor and activates signaling. Frameshift mutations in CALR are located on exon 9 and are of two types. Deletions are termed Type 1 (most commonly a 52 base pair deletion) and insertions are classified as Type 2 (most commonly a 5 base pair insertion). Type 1 and Type 2 mutations are equally distributed in ET whereas in PMF Type 1 is more common. They are absent in patients with PV and mutually exclusive with JAK2 and MPL mutations. CALR Type 1 mutation is associated with better survival compared to Type 2 [8].
Only a driver mutation is identified in 50–60% of cases of MPN. In others, in addition to one of the three abovementioned driver mutations, coexisting other mutations may be present at varying frequency. These are not restricted to MPN and may be found in other myeloid neoplasms including acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) [10, 11]. These include RNA splicing mutations, e.g., SRSF2, SF3B1, U2AF1, and mutations that result in chromatin modifications, e.g., ASXL1, DNMT3A, IDH1/2, EZH2, and TET2, alter signal transduction, e.g., CBL, as well as mutations in the tumor suppressor gene TP53.
There are a some mutations that are considered high risk including ASXL1, IDH1/2, EZH2, SRSF2, and U2AF1, due to shorter overall and leukemia-free survival in MF population [12, 13]. These new discoveries are being utilized in newer prognostic scoring systems to help determine prognosis more accurately.Cytogenetic abnormalities may occur in MPN. Common abnormalities include gains of chromosomes 8 and 9, del 9(p), del 20(q), and del 13(q) among others. Abnormalities like complex karyotype and deletion of 17p are associated with disease progression [2].
A unique feature of MPN is the variability in genotype-phenotype correlation whereby the same driver mutation can be associated with different phenotypes. This is determined by a variety of host factors including age and most importantly patient sex, with PV and ET being more common in women. The incidence of MPN rises with age, being most common after age 60, possibly related to acquisition of mutations that result in clonal hematopoiesis. The precise basis of this variability, however, remains unclear [8].
In most cases, MPN results from sporadic acquisition of somatic driver mutations. In about 7% of cases, there is a familial predisposition to MPN with multiple family members developing the same or another MPN. The genetic basis of such predisposition includes inheritance of single nucleotide variants that predispose to driver mutations, SNPs in TERT gene as well as germline mutations in JAK2 and MPL [8, 14,15,16,17].
9.4 CASE 1: Primary Myelofibrosis
A 66-year-old man with no significant prior illness was diagnosed with PMF when he presented in June 2017 with weakness, dyspnea on exertion and night sweats. He was found to have hemoglobin of 6.6 g/dL, WBC count of 3600/µL, and platelet count was 279,000/µL. He became red cell transfusion dependent and required about 1 unit per month. Bone marrow aspirate from June 2018 was hemodilute and showed left-shifted myelopoiesis and trephine biopsy showed a markedly hypocellular marrow with moderate collagen fibrosis and osteosclerosis. There were 1% circulating blasts in peripheral blood but bone marrow did not show increased blasts. Cytogenetics was normal. JAK2 V617F was detected and additionally there were U2AF1 and S34F mutations. Comparison with previous marrow from August 2017 showed increased collagen fibrosis and new U2AF1 mutation suggesting disease progression. Splenomegaly was mild on imaging. He was started on ruxolitinib at 20 mg twice daily with some improvement in constitutional symptoms. He had tried erythropoietin for some time but did not improve anemia. He did not have any history of venous or arterial thrombosis.
He was found to have a histocompatible sibling and underwent allogeneic HCT using fludarabine and melphalan conditioning in January 2019. His HCT course was uneventful and he remains free of disease 1 year and 10 months after HCT.
9.5 Discussion
-
1.
Initial Diagnosis and prognostication:
Onset of PMF can be insidious and early stages can be asymptomatic and diagnosed when splenomegaly or elevated WBC count or platelet count is detected on routine clinical examination and laboratory testing. Early prefibrotic phase of PMF may only have leukocytosis or thrombocytosis and bone marrow biopsy is required for differentiation from ET. PMF can cause profound constitutional symptoms and these may be present in up to 50% of cases. In a patient with prior PV or ET progressing to secondary myelofibrosis, features of evolution to myelofibrosis are slowly progressive anemia, leucoerythroblastosis, increasing organomegaly, and constitutional symptoms. Bone marrow biopsy is performed to document transformation and also helps to better prognosticate disease by determining chromosomal abnormalities and percentage of myeloblasts. Often there will be a dry tap and in that case cytogenetics and mutations panel can be done on peripheral blood. There are many prognostic scoring systems used to guide treatment and commonly used ones include Dynamic International Prognostic Scoring System (DIPSS) [18]. Accurate determination of spleen and liver size at diagnosis is important as improvement in size on treatment is a good indication of response which has been used in most of the clinical trials. This patient would be scored “high risk” per DIPSS criteria (age >65, constitutional symptoms, peripheral blood blasts ≥1%, and anemia with Hb <10g/dL [5 points]) with a median survival of 1.5 years. By DIPSS Plus which takes into account additional factors like karyotype, transfusion dependency, and platelet count, he would again be classified as “high risk” with a median survival of 16 months [19]. More recently, new prognostic scoring systems have been developed incorporating mutation profile in addition to clinical and pathologic features. MIPSS 70+ v2.0 is one such prognostic scoring system that was devised [20]. Given the fact that he has a high-risk mutation U2AF1 his score would be high risk (8 points) with estimated median survival of 3.5 years. All of these factors as well as the impact of constitutional symptoms and transfusion dependency on his quality of life factored into the decision to proceed to allogeneic HCT.
Both PV and ET can evolve over time to myelofibrosis and this entity is termed secondary myelofibrosis (SMF). Since the prognostic scoring systems discussed above are developed for PMF, a specific prognostic scoring model (MYSEC-PM) has been developed specifically to predict survival in SMF [21].
-
2.
What is the Initial treatment of symptomatic myelofibrosis?
Myelofibrosis can cause profound constitutional symptoms due to elevation of various inflammatory cytokines, i.e., interleukin (IL)-8, IL-2R, IL-12 and IL-15, TNF a, G-CSF, and VEGF [22]. These constitutional symptoms include night sweats, weight loss (>10% of body weight), non-infectious fevers, fatigue, and bone pain all of which severely affects quality of life for patients, in addition to splenomegaly which causes abdominal discomfort and early satiety that contributes to weight loss. A tool called Myelofibrosis Symptoms Assessment Form (MFSAF) has been developed to objectively assess these symptoms and their response to treatment [23]. This assessment is used in various clinical trials that assess treatments for MF. As our patient was symptomatic with constitutional symptoms, treatment with the JAK2 inhibitor ruxolitinib was indicated to relieve these. Ruxolitinib was the first JAK inhibitor approved for the treatment of myelofibrosis based on two randomized phase III trials COMFORT 1 and 2, where it showed significant improvement in splenomegaly and constitutional symptoms. In COMFORT 1 trial, 67% of patients had spleen volume response (defined as reduction in spleen volume of 35% or more on MRI) that was maintained for 48 weeks or more and 46% in ruxolitinib arm had improvement in symptom score by 50% or more at 24 weeks. In COMFORT II that compared ruxolitinib to best available therapy, 29% of patients in ruxolitinib arm achieved spleen volume reduction at 48 weeks [24, 25]. Ruxolitinib is generally well tolerated with anemia and thrombocytopenia being the major side effects and initial dosing of ruxolitinib depends on the platelet count. It is important to mention that approval of ruxolitinib is regardless of patient’s JAK2 mutation status. Fedratinib is another JAK inhibitor now approved for intermediate-2 or high-risk primary or secondary MF and its response rate and side effect profile are similar to ruxolitinib except for the side effect of encephalopathy which require monitoring of thiamine level and supplementation if needed [26].
-
3.
When to perform Allogeneic Hematopoietic Cell Transplant (HCT) for myelofibrosis.
Allogeneic HCT is currently the only curative option for patient with myelofibrosis either primary or evolving from another MPN. This is offered to patients with advanced symptomatic disease if they are otherwise suitable candidates and have a suitable donor. It may be associated with significant morbidity and mortality related to treatment and thus this decision requires careful consideration and discussion between clinician and patient, particularly with regard to timing of HCT. Various studies have shown it can effectively eliminate malignant clone, resolve marrow fibrosis, and organomegaly over time [27, 28]. It is currently indicated for adverse risk disease patient including intermediate-2 and higher per DIPSS/DIPSS plus, and high risk or higher for patients with MIPSS70+ v2.0 risk disease. Recently, our group published long-term outcome results of a cohort of primary as well as secondary MF patients who underwent reduced intensity allogeneic HCT and showed OS of 65% at 5 years and 59% progression-free survival. Cumulative incidence of relapse at 5 years and non-relapse mortality were only 17% each [27]. These are encouraging results considering the fact that this was a rather high-risk population many of whom having comorbidities that are often observed in MF patients. These results also demonstrate the curative potential of allogeneic HCT for MPN-associated MF.
As our patient in Case 1 remained transfusion dependent on the ruxolitinib treatment and his disease was high risk by DIPSS and DIPSS plus as well as MIPSS70+ v2.0, allogeneic HCT was contemplated due to its curative potential. His brother was identified as a histocompatible donor. Given the propensity of MPNs to be present in multiple members of some families, it is important to evaluate sibling donors carefully for early signs of MPN. He underwent reduced intensity allogeneic HCT using fludarabine and melphalan reduced intensity conditioning regimen. He had no acute and chronic GVHD and remains well almost 2 years after HCT. As expected, there was residual reticulin and collagen fibrosis in his bone marrow biopsy done 3 months after HCT, but JAK2 mutation as well as the previously detected mutations were not detected and donor chimerism was 99%. His peripheral blood counts continue to improve and have almost normalized.
9.6 CASE 2. Polycythemia Vera
A 26-year-old male first developed right lower extremity DVT following a long airplane ride. He subsequently developed a recurrence off anticoagulation 9 months later and at that time was diagnosed with JAK2-mutated PV. His laboratory studies showed hemoglobin of 17g/dL, WBC of 12,000/µ, and platelet count of 545,000/µL. He had no blasts in the peripheral blood. Patient underwent bone marrow biopsy which showed hypercellular marrow with 80% cellularity, with erythroid, myeloid hyperplasia, and megakaryocytic hyperplasia with myeloblasts <5%. Reticulin stain showed MF-1 fibrosis. Cytogenetics showed 46XY. Molecular studies revealed JAK2 V617F and in addition ASXL1 and EZH2 mutations.
-
1.
Prognostication and goals of therapy
Similar to the case with other MPNs, patients with PV have a shortened life expectancy compared to age and sex matched general population [29]. The most common life-threatening complications of PV are thrombosis, both arterial and venous followed by fibrotic progression and leukemic transformation. Initial prognostication and risk assessment are important since that determines the choice of initial treatment and follow-up.
Thrombosis accounted for 41% of deaths in a large prospective study of 1638 patients [30]. At onset of study, 3% of patients had thrombotic history (29% arterial, 14% venous) and after a median follow-up of 2.8 years, 14% of patients in this study had experienced cardiovascular events. In a more recent study of WHO-defined PV patients, thrombosis history was present in 23% at study entry and occurred in 21% (16% arterial, 9% venous) at a median follow-up of 7 years [30, 31].
Based on data from large studies, the two main risk factors for thrombosis are history of prior thrombotic events and age over 60 years. Therefore, patients with either of these risk factors can be considered as having “high-risk” disease, while patients who do not have these two risk factors are at low risk for thrombosis. Other thrombosis risk factors identified include leukocytosis (WBC >15000/µL) and cardiovascular risk factors including hypertension.
Besides thrombosis, leukemic transformation is a major life-threatening complication of PV. Its incidence ranges from 5.5 to 18.7% at 15 years [31]. The presence of cytogenetic abnormalities or certain gene mutations detected on next-generation sequencing including mutations in ASXL1, SRSF2, and IDH2 appears to increase risk of transformation [32, 33]. Eventually almost all patients with PV will evolve into secondary MF. Clues to fibrotic progression include worsening leucoerythroblastosis in peripheral blood, increasing hepatosplenomegaly and peripheral blood cytopenia.
The goals of therapy in PV, therefore, can be broadly summarized as prevention of arterial and venous thrombosis; detection of progression and avoiding leukemic transformation; and providing symptomatic relief from symptoms related to hyperviscosity, splenomegaly, and pruritus, the latter being a dominant symptom in some patients.
-
2.
Choice of therapy
The mainstays of initial therapy in PV regardless of risk status are phlebotomy and low-dose aspirin. The goal of phlebotomy is to maintain hematocrit <45% and this is achieved over time by induction of iron deficiency by repeated phlebotomies. This benefit of phlebotomy was established in CYTO-PV study which showed patients with HCT <45% resulted in significantly lower rate of cardiovascular deaths and major thrombotic episodes [34]. The role of low-dose aspirin was established in a large multicenter European study (ECLAP) in which 518 patients were randomized in a double blinded placebo-controlled trial to 100mg of daily aspirin [35]. This study showed that low-dose aspirin significantly lowered risk of thrombotic episodes in these patients.
Cytoreductive therapy is indicated in high-risk patients and hydroxyurea remains the first-line therapy in most patients based on available data from multiple studies [31]. Interferon-alpha including its pegylated form is a first-line option for some patients and unlike hydroxyurea, it can induce molecular responses in a subset of patients. Whether these molecular responses alter the natural history of disease remains unclear and interferon has significantly more toxicity than hydroxyurea. Other options for hydroxyurea-intolerant/refractory patients include oral busulfan and the JAK inhibitor ruxolitinib. Compared to best available therapy, ruxolitinib was more effective in controlling blood counts, reducing spleen size, and providing symptom relief in hydroxyurea-resistant/intolerant PV patients [36]. Its impact on prevention of thrombosis or prolonging leukemia-free survival remains unclear. For patients who experience venous thromboembolism limited data suggest use of systemic anticoagulation in addition to low-dose aspirin. Patients who progress to symptomatic secondary MF should be referred for HCT evaluation if they are suitable candidates given the curative potential of allogeneic HCT.
Our patient in Case 2 can be classified as high-risk PV due to history of thrombosis, and thus he started on treatment to lower cardiovascular risk. He initially started on aspirin, and phlebotomy. His hematocrit normalized after 6 months and he no longer needed phlebotomy. Since he was young and wanted to start a family, he started on treatment of pegylated interferon alpha as it has the possibility of inducing cytogenetic remission and does not have risk of teratogenicity as with hydroxyurea. He tolerated interferon well, although interferon dose had to be adjusted due to development of liver function test abnormalities. His main symptom was aquagenic pruritus. This was controlled with antihistamines, aspirin, and interferon. He also remains on rivaroxaban given the two episodes of venous thrombosis.
9.7 CASE 3: Essential Thrombocythemia
A 45-year-old female presented with mild left upper quadrant abdominal discomfort that prompted a visit to her primary care physician. Laboratory studies showed WBC of 15,500/µL, hemoglobin of 14g/dL, and platelet count of 588,000/µL. No cause of reactive thrombocytosis was evident. She was further evaluated and underwent bone marrow biopsy that showed hypercellular marrow, megakaryocytic hyperplasia, and atypia with MF-1 reticulin fibrosis. Cytogenetics were normal. JAK2 V617F mutation was positive and BCR-ABL1 was negative. Spleen was palpable 6 cm below left costal margin. She denied any constitutional symptoms or erythromelalgia and had no history of thrombotic events.
-
1.
Initial Diagnosis and Prognostication:
Our patient in Case 3 was diagnosed with JAK2 mutation-positive ET as her platelet count was >450,000/µL and bone marrow findings of megakaryocyte hyperplasia and atypia in addition to JAK2 mutation met WHO criteria for ET. The major differential diagnosis is prefibrotic phase of PMF (Tables 9.1 and 9.2). Various prognostic models have been developed to predict outcome and guide treatment. Age has a major impact on survival with patients over 70 years of age having a median survival of 8.1 years compared to a median survival of 35 years for patients under 40 years [37]. Recently, a validated prognostic scoring system has been developed (International Prognostic Score for Essential Thrombocytosis, IPSET) that identifies age >60, history of thrombosis, and WBC count over 11,000/µL as determinants of worse survival [38]. Further refinements have been suggested to this model that incorporates the genetic mutation profile. For example, it is known that patients with CALR-mutated ET have higher platelet counts but less risk of thrombosis compared to ET patients with JAK2 mutations [39] Additional mutations besides the driver mutation can be detected in around 15% of ET patients and some of these including SRSF2, U2AF1, and TP53 may be associated with lower overall survival [37].
A major goal in treatment of ET is prevention of vascular events and thrombotic risk assessment is critical for choice of therapy. Models have also been developed to assess thrombotic risk including IPSET-thrombosis model that takes into account conventional risk factors in addition to JAK2 mutation status [40]. Low-dose aspirin is indicated in most patients unless thrombocytosis is mild and patient is asymptomatic. An algorithm for therapy based on thrombotic risk is shown in Table 9.3. Bleeding, often gastrointestinal, may occur in around 5% of patients with ET and is in some cases associated with acquired von Willebrand disease (due to binding of large vWF multimers by platelets) especially when platelet count is over 1 million.
It is important to note that cytoreductive therapy is indicated in only high-risk patients and should not be used solely for controlling or normalizing platelet count. When such therapy is indicated hydroxyurea is usually the first-line therapy based on a controlled study that showed significantly less thrombotic events in hydroxyurea-treated high-risk patients [41]. Pegylated interferon alfa-2a can be used as front-line therapy, particularly for younger patients given its potential to induce molecular response and slow disease progression as in PV, although it is associated with more side effects which make it a less attractive first choice agent. Anagrelide is another approved agent but again its use is limited by its poor adverse event profile, particularly fluid retention and cardiovascular toxicity. In patients who are intolerant or refractory to hydroxyurea, ruxolitinib can be used regardless of JAK2 mutation status [42] but it is important to emphasize that ruxolitinib has not demonstrated disease-modifying potential in MPN.
Erythromelalgia, characterized by erythema, congestion, and burning of distal extremities can be a troubling symptom in some patients. It can precede diagnosis of ET or PV by years. This is usually very responsive to aspirin therapy.
The main goals of treatment in ET are to prevent thrombotic events as well as provide symptom relief. It is important to emphasize that normalization of platelet count is not a goal of therapy. Patients who evolve to post ET MF should be referred for allogeneic HCT if suitable candidates. Our patient in case 3 would be classified as low-risk disease and was therefore treated only with low-dose aspirin (81 mg daily) which she tolerated well.
References
Dameshek W (1951) Some speculations on the myeloproliferative syndromes. Blood 6(4):372–375
Arber DA, Orazi A, Hasserjian R et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. J Blood 127(20):2391–2405. https://doi.org/10.1182/blood-2016-03-643544
Kralovics R, Passamonti F, Buser AS et al (2005) A gain-of-function mutation of JAK2 in myeloproliferative disorders 352(17):1779–1790. https://doi.org/10.1056/NEJMoa051113
Klampfl T, Gisslinger H, Harutyunyan AS et al (2013) Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med 369(25):2379–2390. https://doi.org/10.1056/NEJMoa1311347
Nangalia J, Massie CE, Baxter EJ et al (2013) Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. N Engl J Med 369(25):2391–2405. https://doi.org/10.1056/NEJMoa1312542
Pikman Y, Lee BH, Mercher T et al (2006) MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLOS Med 3(7):e270. https://doi.org/10.1371/journal.pmed.0030270
Szuber N, Tefferi A (2018) Driver mutations in primary myelofibrosis and their implications. Curr Opin Hematol 25(2):129–135. https://doi.org/10.1097/moh.0000000000000406
Spivak JL (2017) Myeloproliferative neoplasms. N Engl J Med 376:2168–2181
Defour JP, Chachoua I, Pecquet C, Constantinescu SN (2015) Oncogenic activation of MPL/thrombopoietin receptor by 17 mutations at W515: implications for myeloproliferative neoplasms. Leukemia 30:1214. https://doi.org/10.1038/leu.2015.271
Rampal R, Ahn J, Abdel-Wahab O et al (2014) Genomic and functional analysis of leukemic transformation of myeloproliferative neoplasms. Proc Natl Acad Sci 111(50):E5401–E10. https://doi.org/10.1073/pnas.1407792111
Stegelmann F, Bullinger L, Griesshammer M et al (2010) High-resolution single-nucleotide polymorphism array-profiling in myeloproliferative neoplasms identifies novel genomic aberrations. Haematologica 95(4):666–669. https://doi.org/10.3324/haematol.2009.013623
Guglielmelli P, Lasho TL, Rotunno G et al (2014) The number of prognostically detrimental mutations and prognosis in primary myelofibrosis: an international study of 797 patients. Leukemia 28:1804. https://doi.org/10.1038/leu.2014.76
Tefferi A, Finke CM, Lasho TL et al (2018) U2AF1 mutation types in primary myelofibrosis: phenotypic and prognostic distinctions. Leukemia 32(10):2274–2278. https://doi.org/10.1038/s41375-018-0078-0
Jones AV, Chase A, Silver RT et al (2009) JAK2 haplotype is a major risk factor for the development of myeloproliferative neoplasms. Nat Genet 41:446–449
Hinds DA, Barnholt KE, Mesa RA et al (2016) Germline variants predispose to both JAK2V617F clonal hematopoiesis and myeloproliferative neoplasms. Blood 128:1121–1128
Oddsson A, Kristinsson SY, Helgason H et al (2014) The germline sequence variant rs2736100_C in TERT associates with myeloproliferative neoplasms. Leukemia 28:1371–1374
Ding J, Komatsu H, Wakita A et al (2004) Familial essential thrombocythemia associated with a dominant positive activating mutation of the c-MPL gene, which encodes for the receptor for thrombopoietin. Blood 103:4198–4200
Passamonti F, Cervantes F, Vannucchi AM et al (2010) A dynamic prognostic model to predict survival in primary myelofibrosis: a study by the IWG-MRT (International Working Group for Myeloproliferative Neoplsams Research and Treatment) Blood 115:1703–1708
Gangat N, Caramazza D, Vaidya R et al (2011) DIPSS plus: a refined dynamic international prognostic scoring system for primary myelofibrosis that incorporates prognostic information from karyotype, platelet count and transfusion status. J Clin Oncol 29:392–397
Tefferi A, Guglielmelli P, Lasho TL et al (2018) MIPSS70+ Version 2.0: mutation and karyotype-enhanced international prognostic scoring system for primary myelofibrosis. J Clin Oncol 36(17):1769–1770. https://doi.org/10.1200/jco.2018.78.9867
Passamonti F, Giorgino T, Mora B et al (2017) A clinical-molecular prognostic model to predict survival in patients with post polycythemia vera and post essential thrombocythemia myelofibrosis. Leukemia 31:2726–2731
Tefferi A, Vaidya R, Caramazza D, Finke C, Lasho T, Pardanani A (2011) Circulating interleukin (IL)-8, IL-2R, IL-12, and IL-15 levels are independently prognostic in primary myelofibrosis: a comprehensive cytokine profiling study. J Clin Oncol: Official J Am Soc Clin Oncol 29(10):1356–1363. https://doi.org/10.1200/jco.2010.32.9490
Mesa RA, Schwager S, Radia D et al (2009) The Myelofibrosis Symptom Assessment Form (MFSAF): an evidence-based brief inventory to measure quality of life and symptomatic response to treatment in myelofibrosis. Leuk Res 33(9):1199–1203. https://doi.org/10.1016/j.leukres.2009.01.035
Harrison C, Kiladjian J-J, Al-Ali HK et al (2012) JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis 366(9):787–798. https://doi.org/10.1056/NEJMoa1110556
Verstovsek S, Mesa RA, Gotlib J et al (2012) A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis 366(9):799–807. https://doi.org/10.1056/NEJMoa1110557
Talpaz M, Kiladjian J-J (2020) Fedratinib, a newly approved treatmentfor patients with myeloproliferative neoplasm-associated myelofibrosis. Leukemia. https://doi.org/10.1038/s41375-020-0954-2
Ali H, Aldoss I, Yang D et al (2019) MIPSS70+ v2.0 predicts long-term survival in myelofibrosis after allogeneic HCT with the Flu/Mel conditioning regimen J Blood Adv 3(1):83–95. https://doi.org/10.1182/bloodadvances.2018026658
Gupta V, Malone AK, Hari PN et al (2014) Reduced-intensity hematopoietic cell transplantation for patients with primary myelofibrosis: a cohort analysis from the center for international blood and marrow transplant research. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant 20(1):89–97. https://doi.org/10.1016/j.bbmt.2013.10.018
Hultcrantz M et al (2012) Patterns of survival among patients with myeloproliferative neoplasms diagnosed in Sweden from 1973–2008: a population based study. J Clin Oncol 30:2995–3001
Marchioli R, Finazzi G, Landolfi R et al (2005) Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol 23(10):2224–2232. https://doi.org/10.1200/jco.2005.07.062
Tefferi A, Vannucchi AM, Barbui T (2018) Polycythemia vera treatment algorithm 2018. Blood Cancer J 8:3
Tang G et al (2017) Characteristics and clinical significance of cytogenetic abnormalities in polycythemia vera. Haematologica 102:1511–1518
Tefferi A et al (2016) Targeted deep sequencing in polycythemia vera and essential thrombocythemia. Blood Adv 1:21–30
Marchioli R, Finazzi G, Specchia G et al (2012) Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med 368(1):22–33. https://doi.org/10.1056/NEJMoa1208500
Landolfi R, Marchioli R, Kutti J et al (2004) Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med 350(2):114–124. https://doi.org/10.1056/NEJMoa035572
Vannucchi AM et al (2015) Ruxolitinib versus standard therapy for treatment of polycythemia vera. N Engl J Med 372:426–435
Teferri A, Pardanani A (2019) Essential thrombocythemia. N Engl J Med 381:2135–2144
Passamonti F, Thiele J, Girodon F et al (2012) A prognostic model to predict survival in 867 World Health Organization-defined essential thrombocythemia at diagnosis: a study by the International Working Group on myelofibrosis research and treatment. Blood 120:1197–1201
Rumi E, Pietra D, Ferretti V et al (2014) JAK2 or CALR mutation status defines subtypes of essential thrombocythemia with substantially different clinical course and outcomes. Blood 123:1544–1551
Barbui T, Finazzi G, Carobbio A et al (2012) Development and validation of an international prognostic score of thrombpsis in world health organization-essential thrombocythemia (IPSET-thrombosis). Blood 120:5128–5133
Cortelazzo S, Finazzi G, Ruggeri M et al (1995) Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N Engl J Med 332:1132–1136
Harrison CN, Mead AJ, Panchal A et al (2017) Ruxolitinib versus best available therapy for ET intolerant or resistant to hydroxycarbamide. Blood 130:1889–1897
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ali, H., Pullarkat, V., Snyder, D. (2021). Biology and Current Treatment of Myeloproliferative Neoplasms. In: Pullarkat, V., Marcucci, G. (eds) Biology and Treatment of Leukemia and Bone Marrow Neoplasms . Cancer Treatment and Research, vol 181. Springer, Cham. https://doi.org/10.1007/978-3-030-78311-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-78311-2_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-78310-5
Online ISBN: 978-3-030-78311-2
eBook Packages: MedicineMedicine (R0)