Abstract
In this chapter we examine environmental sociology’s engagement with environmental health as a research topic and as a growing form of activism. We begin by providing a brief history of environmental illness and examine the ways in which government and industrial science have failed to protect human and environmental health. We then discuss the ways in which impacted community members and environmental health advocates have brought these issues to the attention of academics and the broader public. Next, we turn our attention to academic studies of contaminated communities, which formed the basis of early environmental sociology; scholarship on health social movements and other challenges to the dominant epidemiological paradigm; and more recent developments in exposure experience and contested illness. Finally, we discuss new research methods that involve researchers from multiple academic disciplines working with impacted communities. Putting all the above elements of research methods and sensibilities together, we arrive at a public sociology for environmental health, which represents a highly engaged approach to environmental concerns in which the needs of affected people and communities are placed in the primary position of importance. In the tradition of “public sociology” (Burawoy, Social Forces, 82(4):1603–1618; 2004), this type of research also seeks to inform debates and discussions outside of academia. We end the chapter with some concluding thoughts on environmental health and justice activism in the current era.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Health outcomes are shaped by a complex interaction of individual and societal-level factors, including: where we live and work, our ability to access health care, genetics, race and ethnicity, income and educational background, lifestyle choices, social support, and cumulative exposure to hazards. The World Health Organization (2016) estimates that environmental factors contribute to nearly a quarter of all deaths worldwide. Yet discussions of the causes of illness and disease are often limited to genetics and individual lifestyle factors, while past and current environmental exposures remain invisible (Brown, 2007). Think about the kinds of questions that you were asked the last time you needed to see a doctor. You were probably asked about your family history of disease and how often you smoke, drink alcohol, and exercise. You were probably not asked about your daily and cumulative exposure to air pollution, how close you live to hazardous waste sites or polluting industries, whether your water pipes have been tested for lead, or what kinds of chemicals are used in your home, school and workplace. Yet these factors are at least as important as genetics and lifestyle in determining your overall level of health and wellness.
In this chapter we examine environmental sociology’s engagement with environmental health as a research topic and as a growing form of activism, as well as with environmental health scientists and community advocates. We rely heavily on the work of environmental health advocates and scientists, environmental historians, and public health scholars, whose pioneering work in this area has provided a foundation for environmental sociologists concerned with health. Throughout the chapter we show that a commitment to public sociology, advocacy, and activism are often intertwined with the environmental health research carried out by environmental sociologists. This highly engaged approach to environmental concerns places the needs of affected people and communities in the primary position of importance and contributes to the creation of alternative epistemologies and practices.
Environmental health is still a relatively understudied topic within environmental sociology, even though many of the topics that are central to environmental sociology have very clear environmental health implications. The study of climate change and climate justice has become a foundational part of the subdiscipline—though few sociologists address or engage with the health conditions and hazards that are exacerbated by climate change, including heat stress, morbidity and mortality from climate-induced disasters, spread of infectious disease like the Zika virus, discovery of contaminated sites after disasters, increases in air pollution, and the ramifications of dietary changes necessitated by the changing climate. For example, in a recent edited volume summarizing existing sociological perspectives on climate change and society (Dunlap & Brulle, 2015), there is no chapter dedicated to the health impacts of climate change—although health issues are sometimes included in environmental sociologists’ examination of climate-related inequities (c.f. Harlan et al., 2015). Similarly, environmental sociologists who study the power of the petrochemical sector and its closely allied private vehicle sector should logically consider the environmental health implications of that sector, but often do not. Natural resource scholars concerned about the impact of mining on resource-dependent communities and Native American tribes should logically examine the health effects of copper smelters, uranium tailings, and mercury from coal-fueled power plants, but often do not. Some notable exceptions can be found in the work of environmental sociologists who examine the health-related impacts of pesticides and other industrial chemicals (Harrison, 2011; Little, 2014; Saxton, 2015), coal (Bell, 2016), uranium (Malin, 2015), and unconventional oil and gas production (Wylie, 2018; Ladd, 2018).
While this chapter will not explicitly engage with these aspects of “undone environmental health sociology,” we hope our work stimulates others to think of the health aspects of their environmental sociology research and practice. Indeed, one of the major points we wish to make is that environmental sociology should view health as central to most, if not all, of its work—much as environmental sociology asks sociology overall to consider the centrality of environmental concerns.
One of the most notable aspects of the field of environmental health is researchers’ engagement with communities impacted by environmental contamination. Since laypeople have often been the primary source of hazard recognition and action, environmental health researchers typically build ongoing relationships with affected communities, either by providing research and advocacy services for them or by working with them in joint research/practice partnerships. Increasingly, work in these areas is taking the form of transdisciplinary social science-environmental health collaborations, which typically involve researchers from multiple disciplines in addition to the community partner.
As we cannot cover all of the sources and consequences of the environmental health hazards discussed above in this chapter, we focus mainly on a subset of environmental health considerations related to chemical exposures. This is primarily because chemical exposures are often less visible to the general public than the health hazards associated with environmental pollution generated by the transportation, agricultural, and extractive sectors. Exposure to toxics affects both individuals and collectivities. Individual-level experience includes personal health concerns, psychological awareness of toxic trespass, assigning of responsibility, and decisions about personal levels of change such as avoiding harmful products. Community-level experience includes collective action in the form of public protest, litigation, pressure on government, and pressure on those parties held responsible for contamination. Not only do people experiencing toxic exposures have to discover the existence of contaminated sites and deal with the effects of their exposure, they frequently also must struggle to prove that diseases or conditions they are suffering from are related to that contamination (Brown, 2007; Brown & Mikkelsen, 1997; Edelstein, 1988; Hoover, 2017).
We begin by providing a brief history of environmental illness and its political-economic context. We then turn to the matter of regulatory neglect in order to better understand how government and industrial science have failed to protect human and environmental health, relying primarily on the work done by impacted community members and environmental health advocates in bringing these issues to the attention of academics and the public. Next, we consider studies of contaminated communities, which formed the basis of early environmental sociology, followed by health social movements and other challenges to the dominant epidemiological paradigm, as well as more recent developments in exposure experience and contested illness. Finally, we discuss new research methods and sensibilities and end with some concluding thoughts on environmental health and justice activism in the current era.
A Brief History of Environmental Illness
It is clear why we should all pay more attention to environmental health. In 2015, pollution was responsible for more deaths worldwide than tobacco smoke, nearly three times as many as AIDS, malaria, and tuberculosis combined, and more than 20 times as many as war and murder (Landrigan et al., 2017). Air pollution alone was responsible for 4.2 million early deaths that year, with the majority occurring in rapidly industrializing areas of the developing world (WHO, 2016). Cancer is a leading cause of mortality, with one in five people—one in three in industrialized nations—expected to develop the disease in their lifetimes (WHO, 2016). Around 20% of cancers are directly attributable to environmental factors (WHO, 2016). In the United States, asthma rates have been steadily increasing for decades, from 3.1% of the population in 1980 to 8.4% in 2010 (CDC, 2012). From 2001 through 2009, asthma rates rose the most among black children, who experienced a 50% increase in the disease (CDC, 2011). From 2014 to 2016, asthma rates among black children rose from 13.4% to 15.7% (CDC, 2018a). Communities of color remain disproportionately impacted by pollution, toxicity, and environmental hazards (as reviewed in Chap. 3).
Meanwhile, of the 80,000 chemicals currently registered for use in the United States, it is estimated that fewer than 2% have been assessed for toxicity, and only five have ever been banned (Steingraber, 2010:103). Other chemical removals have stemmed from voluntary agreements between EPA and chemical companies, such as in the examples perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate (PFOS), though replacement chemicals have many structural and toxicological similarities. State bans have been a more productive mechanism, as seen with bisphenol-A (BPA), flame retardants, and some polyfluoroaskyl chemicals (PFAS). Many of these chemicals have been linked to cancer, high blood pressure and heart disease, diabetes, obesity, asthma, neurological, and reproductive problems. Yet these chemicals are ubiquitous in our environment—they are in the air that we breathe, the foods that we eat, the materials found in our homes, workplaces, schools and hospitals, and the products we put on our bodies.
Chemicals have not only become part of our lives—they have quite literally become part of us. Centers for Disease Control and Prevention (CDC) biomonitoring studies routinely show that that nearly all Americans have detectable levels of harmful substances such as perchlorate, mercury, BPA, perfluorinated chemicals, and flame-retardants in their blood (CDC, 2018b). While the CDC study focused on adults, an Environmental Working Group study found more 232 industrial compounds and pollutants in the cord blood of American infants (EWG, 2009). Activists have termed this kind of chemical contamination toxic trespass—because without our consent and often without our knowledge, the chemicals in consumer and personal care products, home and office furnishings, and building materials have now passed into our bodies.
The Chemical Revolution
Along with modern conveniences like electricity and locomotives, the Industrial Revolution also brought new environmental and health hazards to the American public. Coal miners were routinely killed when mines collapsed or exploded; others developed respiratory ailments like silicosis and pneumoconiosis—also known as black lung disease (Bell, 2013, 2016; Bell & York, 2012). Clouds of smoke and soot hung over cities like toxic clouds and lingered in ill-ventilated homes near the manufacturing districts. Burning coal discharged harmful pollutants into the air including mercury, lead, cadmium, carbon monoxide, and arsenic. The consequences of these exposures included severe asthma, chronic respiratory infections, and premature death. Meanwhile, the chemical industry was being born, as chemists learned that the distillates of coal tar could be used to create synthetic dyes (Travis, 1993).
The hazardous health effects of synthetic chemicals used in the manufacturing process have long been known to industrial science, although this knowledge was rarely shared with workers or the general public. By 1895, it was clear that German dye factory workers were experiencing convulsions, bloody urine, and skin discolorations (Fagin, 2013). By 1906, thirty-eight workers at a dye factory in Frankfurt had been diagnosed with bladder cancer; yet this knowledge did little to slow the growth of the industry (Fagin, 2013). After World War I, new factories were opened in the U.S., where workers were not told about the known dangers of the chemicals they were handling. In 1932, twenty-three bladder cancer cases were discovered at a DuPont dye factory. Despite being told about the other instances of bladder cancer among workers in similar factories, the company claimed that it could not spare any money to research the health impacts of the chemicals used in dye manufacture (Fagin, 2013). In 1958, when yet another cancer cluster was discovered at Cincinnati Chemical Works and confirmed by the Ohio State Health Department, the plant was closed and production simply moved to New Jersey, where new employees began work with no knowledge of what had happened in the Cincinnati plant (Fagin, 2013).
Early Struggles for Recognition
The rapid growth of petrochemical-based industries meant that the public was being exposed to increasing volumes and concentrations of pollution and toxicity with little regulatory oversight. By the end of the nineteenth century, activists in the settlement house movement were already leading struggles for worker protection and public health in rapidly industrializing urban spaces. Chicago’s Hull House, founded by Jane Addams in 1888, quickly became a center for social justice and progressive reform that often centered on growing pollution and toxicity being produced by industry (Dowie, 1996; Gottlieb, 1993). Resident activists made the connection between issues of degradation of the urban environment, disease, and workplace hazards. For example, Alice Hamilton, a professor of pathology at the Women’s Medical School of Northwestern University, pioneered systematic analyses of workplace hazards and foreshadowed later environmental health concerns associated with heavy metals and petroleum-based chemicals. Florence Kelly, another leader of Hull House, made the connection between community and workplace hazards in her research, noting that the working and living conditions were “ruinous to the health of [industrial] employees” and their families (Gottlieb, 1993: 63).
In 1962, Rachel Carson’s Silent Spring called public attention to the environmental and health effects of DDT and other toxic chemicals, asserting that “[f]or the first time in the history of the world, every human being is now subjected to contact with dangerous chemicals, from the moment of conception until death. In the less than two decades of their use, the synthetic pesticides have been so thoroughly distributed throughout the animate and inanimate world that they occur virtually everywhere” (Carson, 1962: 15). A marine biologist by training, Carson synthesized and presented an enormous amount of data to demonstrate the harm that chemical pesticides pose to ecosystems and human communities. She described how DDT accumulates in the fatty tissues of animals that eat pesticide-laden vegetation—an effect that is magnified at each successive level of the food chain, so that the species at the top of the food chain carry the highest concentrations of DDT in their bodies. For Carson, the danger for most people was not a single large scale or catastrophic exposure, but the “innumerable small-scale exposures to which we are subjected day by day, year after year” (1962: 173). She was among the first to link synthetic chemicals like DDT to breast cancer, and to foreshadow the role of endocrine disrupting compounds (EDCs) on human health. Carson was subjected to a relentless campaign of personal and professional attacks led by the pesticide industry, which questioned her scientific credentials and even her sanity. President Kennedy tasked the President’s Science Advisory Committee with reviewing Carson’s evidence, which was fully substantiated by the Committee’s report (PSAC, 1963). Public outcry led to the creation of the Environmental Protection Agency (EPA) in 1970, and one of its first acts was to ban DDT.
Community-Based Campaigns for Environmental Health and Justice
During the late 1970s and early 1980s, grassroots movements for environmental health and justice arose in response to toxic chemical contamination in poor communities and communities of color. Love Canal, for example, was a working-class residential neighborhood of Niagara Falls that was built above a toxic waste site without residents’ knowledge. Residents had complained of odors and substances surfacing in their yards for decades, and in 1976 the city finally hired a consulting firm to investigate. The investigation revealed toxic chemical residues in the air, buried drums of toxic waste, and high levels of PCBs in the storm sewer system (CHEJ, 2018). The city did not follow the recommended mitigation strategies, having conducted a cost-benefit analysis of cleaning up the contamination and deciding that the $20 million that it would cost exceeded the monetary value of the working-class residents’ lives (Gibbs & Livesey, 2003). Community residents, led by Lois Gibbs, conducted a community health survey documenting an unusually high number of miscarriages and children with born with birth defects and various intellectual disabilities. When their data was dismissed by the New York State Department of Health, the community took their fight to the EPA. After two-year battle that included taking EPA representatives hostage (Gibbs & Levine, 1982), the community was finally bought out and relocated. The Love Canal episode ultimately led to the creation of EPA’s Superfund program in 1980—a federal program designed to finance cleanup of toxic waste sites. Lois Gibbs would go on to found the Citizens Clearinghouse for Hazardous Waste, now the Center for Health, Environment and Justice (CHEJ), a national organization that has assisted thousands of grassroots groups fighting toxic contamination in their communities.
Although communities of color had been protesting the siting of hazardous waste for decades, in 1982 a proposal to build a landfill for PCB-contaminated soil in a small, predominantly African American community in Warren County, North Carolina led to a massive protest staged by the NAACP (Bullard, 1990). The protest received mainstream media coverage as well as the attention of the Congressional Black Caucus. The Warren County protests inspired other groups in poor minority communities to fight the discriminatory decision-making processes that resulted in a disproportionate share of environmental burdens and hazards being located within them (Bullard, 1990)—and sparked a sub-field of related scholarship among environmental sociologists and others (reviewed in Chap. 3).
Robert Bullard’s (1990) Dumping in Dixie: Race, Class, and Environmental Quality was the first major academic work in the rapidly growing field of environmental justice, emphasizing how systematic and institutionalized environmental racism leads to higher levels of environmental exposure, health inequalities, and exclusion from environmental decision-making for people of color in the United States. Many key community organizing efforts that formed the basis for the environmental health and justice movement began in rural, largely African-American areas of Louisiana’s industrial chemical corridor between New Orleans and Baton Rouge, often referred to as Cancer Alley (Lerner, 2006; Roberts & Toffolon-Weiss, 2001). Later on, Cancer Alley activists would be among the first to employ lay community monitoring (now called civic science) via the Louisiana Bucket Brigade, whose inexpensive community monitoring devices demonstrated widespread petroleum-based contamination that was otherwise not being monitored or reported on by official sources (Allen, 2003).
The community organizing that employed popular epidemiology and civic science (Brown & Mikkelsen, 1997; Ottinger, 2010; Wylie, 2018) has led some environmental sociologists to focus on the intersection of toxic contamination, community response, and the failure of environmental governance (Dillon et al., 2018). At the same time, it has made environmental sociology a major contributor to public sociology, in particular by combining support of environmental organizing, frequent participation in that organizing, and critiques of existing government and scientific policy and practice.
Regulatory Neglect
The Toxic Substances Control Act (TSCA) of 1976 gave EPA the authority to require industry reporting of chemicals as well as health and safety testing, and to enforce restrictions on chemicals deemed to present an “unreasonable risk of injury to health or the environment.” However, it exempted the 62,000 chemicals already in production from many testing and reporting requirements. New chemicals could enter the market unless the EPA could prove that they posed an “unreasonable risk.” Yet the agency had only 90 days to make that determination and rarely had the time, staff or funding to test new chemicals thoroughly. As a result, nearly all new chemicals have been allowed to go on the market with little to no health or toxicity data.
In 2010, Senator Frank Lautenberg (D-NJ) and Representatives Henry Waxman (D-CA) and Bobby Rush (D-IL) introduced Congressional bills intended to address some of the shortcomings of TSCA. The chemical industry spent more than $125 million on lobbying Congress during the debate over TSCA reform (Cordner, 2016). The revised law, referred to as the Frank R. Lautenberg Chemical Safety for the twenty-first Century Act (LCSA), was passed in 2016 and represents a significant but still partial victory for human and environmental health. While the new law requires EPA to prioritize and evaluate chemicals based on the risks they pose to human and environmental health rather than on the costs and benefits of regulating them, only a handful of chemicals are scheduled to be evaluated each year. The final version of LSCA also prevents states from enacting their own restrictions on the chemicals under EPA review, even though these reviews are likely to take years, and bars future regulatory action on any chemicals that have undergone an EPA review. Finally, the single-chemical approach to assessment (i.e. in contrast to evaluating together chemicals belonging to the same class, like BPA and BPS) leaves the door open for regrettable substitutions. The result is that in the United States, chemicals are still “innocent until proven guilty.” Once chemicals are in use, the burden is on consumers, community residents, and the victims of chemical contamination to prove harm.
Yet consumers and community members have no affordable, systematic way to monitor or document their exposure to toxic chemicals (Wylie, 2018). Moreover, conclusively proving harm is almost an impossible task (Langston, 2010; Murphy, 2006; Nash, 2006; Oreskes & Conway, 2010). Contaminated communities’ personal experiences have historically not been seen as sufficient or “legitimate” evidence of contamination (Gibbs, 2002), but “scientific” proof of chemical-induced illness in humans is nearly impossible to come by because the type of controlled experiments on human populations required to generate conclusive evidence of harm would be impractical and unethical. Furthermore, the effects of chemical exposure may not become evident for many years (Colborn et al., 1997; Murphy, 2006) and waiting decades for epidemiological studies to demonstrate harm is not a feasible solution for contaminated communities. Finally, even when epidemiological studies document unusually high rates of illness, this does not necessarily prompt government or regulatory action because these studies cannot “prove” that the sufferings of community members were caused by the hazard in their community (Gibbs, 2002). Contaminated communities thus often find themselves in an impossible bind, with their concerns remaining unacknowledged and unaddressed by regulatory agencies.
Community Concerns Ignored by Regulatory Agencies
The pattern of community health concerns being ignored by regulatory agencies is, unfortunately, a longstanding one. In 1979, mothers in Woburn, Massachusetts discovered a cluster of leukemia cases among neighborhood children whose drinking water had all come from the same well. They demanded an investigation. However:
health authorities from the state and federal agencies concluded that there was no connection between the drinking water and the clustering of disease. The Woburn parents persevered, making maps that showed the clustering of leukemia cases along pipelines from a particular contaminated drinking-water well. Local parents took these maps to health officials, politicians, and journalists who they thought would help them. It was not until years later that the Massachusetts Department of Health confirmed the connection of disease to the water supply and closed the drinking-water well. (Gibbs, 2002: 103).
Other cases in San Jose, CA, Brownsville, TX, Tucson, AZ, and Elmira, NY, illustrate instances in which parents brought environmental health issues to the attention of the proper authorities only to be dismissed. In each case, the parents’ suspicions about environmental contamination were later confirmed (Gibbs, 2002). Various sociological studies documenting this pattern of community discovery of contamination and the difficulty of proving adverse health outcomes (e.g., Brown & Mikkelsen, 1997; Edelstein, 1988; Erikson, 1994; Levine, 1982) soon followed. These scholars found widespread distrust of government and industry among community members for failing to prevent the original contamination and then failing to take responsibility and remediate the problem once community groups detected it. That problem has led contaminated communities to do their own fact-finding and research that residents either lead or collaborate on.
In recent years, environmental health concerns associated with unconventional oil and gas extraction have grown as hydraulic fracturing (also known as “fracking”) operations have expanded dramatically across the United States (Willow & Wylie, 2014). Environmental sociologists have begun to study the impacts of fracking on ecosystems and human communities as well as the regulatory failures that are associated with it. The health risks posed by the chemicals and volatile organic compounds used in fracking are well-documented (Colborn et al., 2011). Moreover, oil and gas extraction “emits pollutants that are associated with cardiovascular disease, the leading cause of mortality in the United States” (McKenzie et al., 2019). Threats to the health and safety of oil and gas workers abound—and these threats are extended and amplified for families who have had wells drilled on or near their property are exposed toxic emissions twenty-four hours per day. Yet even when air samples for hazardous pollutants are found to be many hundreds of times above regulatory thresholds, regulatory agencies often fail to issue any violations (Global Community Monitor, 2011; Opsal & O’Connor, 2014; Wylie, 2018).
The reason for this can be traced back to the early 2000s, when the Bush administration exempted oil and gas operations from numerous federal environmental protection statutes, leaving the responsibility for environmental health and safety monitoring primarily up to the states (Colborn et al., 2011). As Colborn et al. note, although some states have oil and gas commissions that are ostensibly responsible for monitoring natural gas production activity, the “primary mission of these agencies has been to facilitate natural gas extraction and increase revenues for the states” (2011: 1040). In addition, even if they wanted to monitor, state agencies are chronically under-resourced and under-funded (Malin et al., 2017; Sumi, 2012).
Some environmental sociologists have chosen to collaborate with environmental health scientists, since affected communities often require scientific evidence of contamination and its health effects, and sociologists are increasingly able to work together with like-minded environmental health scientists to do so (Adams et al., 2011; Altman et al., 2008; Hoover et al., 2015). This has broadened environmental sociology’s contributions to public sociology, since much of the research of this type is used to advance public policy, legislation, and regulation.
The Politics of Measurement
The way in which risk is defined, assessed, and measured further shapes the response that communities will receive from regulators. For many hazardous chemicals, regulatory agencies rely on threshold limit values (TLVs) that are established by moving from high doses of a specific chemical to progressively lower levels in order to find the threshold at which there is no discernible effect. These values then determine the level at which a particular chemical is deemed to be safe or dangerous, and allowable limits are set below that level (Murphy, 2004, 2006). However, TLVs are designed to prevent acute harms such as knock-down and death, not to control the effects of aggregate lower dose exposures over longer periods of time. Furthermore, toxicologists find that they cannot “fingerprint” the contribution of specific sources when exposure to chemicals is ubiquitous (Altman et al., 2008). Chemical exposure studies test for causation of illness via single exposure routes and consider in isolation experiences that are actually composite and interactive (Nash, 2004; Wylie, 2011). A lack of evidence of significant exposure via the single route tested for is then used to “used to dismiss the possibility of harm even when harms are readily apparent” (Wylie, 2011: 354).
An ironic illustration of this is described by Michelle Murphy. When new carpets were installed in their Washington building, EPA scientists began to complain of “tearing eyes, irritated throats, burning lungs, shortness of breath, crippling headaches, and dizziness” (Murphy, 2004: 277). Yet toxicological tests were unable to detect an acute dose of any specific chemical, and the official determination was that there was no threat to human health (Murphy, 2004). These EPA scientists, even with their resources, prestige, and scientific training, struggled unsuccessfully to have their health concerns acknowledged and were unable to ‘prove’ harmful exposure. When toxicological tools failed to detect “significant” contamination, and so EPA staff was told that their contamination was not meaningful.
As environmental epidemiologist Devra Davis summarizes: “when we can’t marshal definitive statistical proof of a toxin’s specific harmful effect … it has become standard to say that we simply don’t know whether the toxin is harmful or not. The absence of evidence of harm—even when no effort has been made to gather such evidence—becomes grounds for inaction” (2002: xviii). Environmental sociologist Alissa Cordner (2015) (and author of Chap. 9 on Risk) describes environmental hazards and risks as “contested topics” whose definitions often vary across institutional contexts and disciplines. This is important, she suggests, because the way in which risk is defined will influence the ways in which regulatory and other types of institutions assess and manage risk. When TLVs become the way of ‘knowing’ whether a chemical is harmful or not, embodied knowledge about what makes humans sick is ignored. In other words, the privileging of remote, lab-based science over the embodied experiences of people on the ground means that if a person is experiencing symptoms associated with chemical exposure, but the levels they have been exposed to have been determined to be “safe,” it is the human experience rather than the number generated in the lab that is dismissed.
Although a majority of social scientific studies on fracking employ quantitative analysis (Willow & Wylie, 2014), an emerging body of qualitative ethnographic research has begun to examine the embodied experiences of people living in communities impacted by fracking (c.f. Hudgins & Poole, 2014; Simonelli, 2014; Willow, 2014; Wylie & Albright, 2014). This is critically important given the fact that local residents’ embodied experience is often very different from “official evaluations of risk” (Checker, 2007: 113). In addition, as Willow and Wylie note, since residents of fracking zones “are often discredited as irrational within the wider public discourse” it is not sufficient to only “collect samples and compile statistics; we need to tell real stories that speak to real people’s experiences, to give voice to views that may otherwise remain unheard” (2014: 226).
Personal Care and Consumer Products
Though many of us think of outdoor sources (e.g., factories, refineries, power plants, landfills, contaminated disposal areas) as the primary source of toxicity and pollution, our indoor environments also contain hundreds of chemicals that are known to be toxic. From the chemicals in cleaning and personal care products to pesticide residue on food to non-stick coatings on cookware to flame retardants in our furniture, clothing, and electronics, consumer products are a central component of our environment—and an area in which poor regulations and lack of information can have negative implications for our health.
The average American uses anywhere from 4 to 25 products each day, with women using an average of 12 and men using an average of 6 (EWG, 2018a). One in five of the 29,000 personal care products in the Environmental Working Group’s public database have been found to contain chemicals linked to cancer (EWG, 2018b). Synthetic estrogens and other endocrine disrupting compounds (EDCs) are now common in modern industrial and consumer environments. These compounds mimic natural estrogen or interfere with the production of other hormones, which is a particular concern for women’s health and reproductive systems. Bisphenol-A (BPA) is one well-known example; other EDCs include certain flame retardants (used in furniture, clothing, and electronics), polychlorinated biphenyls or PCBs (banned by the EPA in 1979 but still found in insulation, electrical equipment, caulking, and oil-based paint), phthalates and phenols (used in cosmetics, food and beverage containers and plastic wraps), and pesticides and herbicides that are widely sold and used in the United States. Over 900 synthetic compounds in industrial and commercial products have been identified as EDCs, including many that have been shown to make human breast cancer cells grow in a laboratory (Silent Spring Institute, 2018). Breast cancer rates have increased by more than 40 percent since 1973, with the result that one out of every eight women in the United States today is diagnosed with the disease (Gray et al., 2017).
Building on the work of environmental health nonprofits and advocacy organizations like Environmental Working Group and Breast Cancer Prevention Partners (formerly Breast Cancer Fund), a few environmental sociologists have recognized the consequences of these exposures for women’s health. Lubitow and Davis examine the corporate response to rising breast cancer incidence, which has included the practice of pinkwashing, which they define as the “co-optation of breast cancer symbolism by corporate actors who stand to profit from the use of breast cancer awareness imagery, including pink ribbons” (2011: 139). They suggest that pinkwashing allows corporations which may be producers of toxic products to profit from growing sales of these products (now adorned with pink ribbons) and simultaneously control the public narrative and women’s experience of the disease in a way that obscures the contributions of environmental exposures to rising cancer rates (Lubitow & Davis, 2011).
Alternative Approaches to Regulation and Research
In 2006, the European Union (EU) passed a far more comprehensive and precautionary approach to chemical manufacture and use than the U.S. The EU’s Registration, Evaluation, Authorisation and Restriction of Chemicals (REACH) legislation employs a “no data, no market” rule that requires manufacturers to provide health and safety data for both new and existing chemicals that are manufactured in or sold within Europe. This is an application of the precautionary principle—the idea that in the absence of evidence, we should err on the side of caution and not take any chances with human health.
The U.S. federal government has shown little inclination to follow the EU’s example or to challenge the chemical industry’s preferences for the regulatory status quo. While the EU has banned over 1000 chemicals from use in cosmetic and body care products under REACH, the U.S. Food and Drug Administration (FDA) restricts just nine. As a result, personal care products that are sold in the U.S. and in Europe can have different formulations: one with toxic chemicals, and one without. For example, in 2011 the Campaign for Safe Cosmetics reported that two chemicals linked to cancer (formaldehyde and 1,4 dioxane) had been found in dozens of baby shampoos and bath products being sold in the U.S., even though Johnson & Johnson was selling formaldehyde-free versions of these products in Europe (Malkan 2016). This is because, in contrast to European law, U.S. cosmetic makers may use almost any material in their products with little regulatory oversight or restriction. In a recent and historic case, Johnson & Johnson was ordered to pay nearly $5 billion in damages to women who had developed ovarian cancer as a result of using the company’s baby powder and other talc products (Hsu, 2018). Investigations by The New York Times and Reuters revealed that Johnson & Johnson knew about the risk that asbestos in its talc products posed for decades but concealed the information from consumers and the general public (Hsu, 2018). Finally, in response to growing public awareness and concern over BPA in the U.S., a number of manufacturers chose to remove BPA from their products and adopted a “BPA-free” label. However, in the absence of regulatory standards, many manufacturers quietly replace BPA with BPS, which is nearly chemically identical and has similar estrogenic properties. Variations on this story—lengthy EPA assessments, resistance to regulatory action from industry and government, and regrettable substitutions that do nothing to address the underlying concerns about toxicity, as previously discussed—have been repeated again and again for other major contaminants.
Environmental sociologists have been active in promoting a perspective that links together concerns about environmental health effects, legislation, regulation, requisite scientific evidence, and community engagement. Environmental sociologists examine such concerns through the lens of corporate secrecy combined with regulatory capture of agencies such as EPA (Dillon et al., 2018; Frickel et al., 2010). In this perspective, the seemingly simple action of replacing one chemical with another is viewed as a complex process involving corporate, government, and scientific actors who insist on a single-chemical approach that serves to obscure the larger social context (Cordner et al., 2016).
Research in the field of science and technology studies (STS) has shown that regulatory decisions in the U.S. are based not on purely on scientific calculations, but are instead shaped by a myriad of social, political, and economic factors (Cordner et al., 2016, 2019; Frickel & Moore, 2006; Krimsky, 2003). This includes the strategic production and dissemination of industry-friendly research that is often intended to plant seeds of doubt regarding the state of the science (Michaels, 2008; Oreskes & Conway, 2010). These strategies have been highly effective. However, social scientists have also examined the ways in which scientific data has been used to advance social movement efforts that are more protective of human health (Brown, 2007; Brown et al., 2011; Frickel, 2004; Lubitow, 2013; McCormick, 2007). For example, Lubitow (2013) shows how collaborative efforts between activists and scientists working on bisphenol-A (BPA) resulted in a set of frames that resonated with the public and established the need for action on BPA.
Contaminated Communities and Environmental Sociology
There are two general forms of environmental contamination. Episodic cases have a specific geographical location with a human-caused or human-exacerbated disaster like oil or chemical spills, pesticide drift, large-scale toxic emissions, nuclear meltdowns, or the discovery of a disease cluster. In the early years of environmental sociology, these were typical research subjects. Ongoing exposure to contamination may be low-level and chronic rather than acute and dramatic. This does not mean that episodic contamination is not part of a pattern of ongoing contamination, but rather that this second form is not discovered as a result of a visible crisis. This second form, for instance, includes the persistent presence of contaminants such as BPA, parabens, phthalates, or flame retardants in personal and consumer goods, and is the subject of the later section on “exposure experience.”
In all of the above situations, disease sufferers and exposed populations face many obstacles. In addition to ethnographic studies that analyze community-wide and individual responses to contamination, and policy analyses that examine state and federal failures at detection, remediation, and regulation, as we noted earlier, environmental sociologists have also engaged in collaborative work with environmental health scientists on biomonitoring and household exposure studies.
Contested Environmental Illness
Government oversight of industrial activities and disasters is often very poor, and moreover, government response often serves to minimize the problem. Corporations that are responsible for contamination fight hard to disprove claims of illegal or immoral activities, buy off complainants, and fund researchers who will side with the companies. Scientists are often unavailable to provide the research that would document the contamination since affected people and communities lack resources to hire them—and scientists may have a disincentive to perform this type of research since it is often not well-received in academic settings. Even affected people may oppose investigation because of ideological identification with the company or industry, personal connections with the polluters, fear that their area will be stigmatized and/or that companies will leave, and that property values will decrease and the tax base will erode once the contamination is revealed. This has been shown in nuclear war production (Kaplan, 2000), industrial toxics dumping (Fagin, 2013; Judge et al., 2016), and natural resource extraction (Cable, 1993).
The totality of these obstacles makes for a “dominant epidemiological paradigm” in which many institutions and professions do not recognize environmental causation of disease. Players in the dominant epidemiological paradigm include established institutions entrusted with the diagnosis, treatment, and care of disease sufferers, as well as academic professional associations, journals, media, universities, medical philanthropies, and government officials. Overturning this paradigm requires not just scientific innovation and progress, but often social movement activity by affected people and groups (Brown, 1992). As a result, we are faced with “contested environmental illnesses,” i.e. diseases and conditions that engender major scientific disputes and extensive public debates over environmental causes. These include well-established diseases like breast cancer, where the debate focuses on the role of environmental factors, as well as less-established diseases like Gulf War Illness, where there is debate about its very existence (Brown, 2007).
The earliest environmental ethnographies were rooted in narrative tales of the experiences of residents moving from discovery to action, as noted in the earlier section on “Regulatory Neglect.” This tradition began with Erikson’s analysis of the 1972 flood at Buffalo Creek, Kentucky, where a poorly constructed and inadequately maintained dam broke, causing a massive amount of coal mining slurry to sweep down the hollow, where it destroyed hundreds of homes, killed 125 people, wounded many others, and left enduring psychological scars on surviving community members. Attorneys for the survivors asked sociologist Kai Erikson to study the situation, and his report became the first book-length community study of a human-caused environmental disaster (Erikson, 1976). Erikson placed human-made disaster into the cultural, social, and historical context of the community; addressed the individual mental health and physical health outcomes of affected individuals within the cumulative community-level effects; and demonstrated that social science can work to help affected people. Like Erikson, psychologist Michael Edelstein (1988) emphasized the joint physical and mental health effects of environmental disaster, and developed the widely used term “contaminated communities.” His notion of the “inversion of home” showed how, in these communities, the safe haven of one’s home is transformed into a constant source of danger and fear.
Many contamination episodes are “chronic technological disasters” that unfold over a long period of time—for example, hazardous waste dumping or other forms of ongoing pollution—as opposed to singular, often more dramatic occurrences such as a chemical factory explosion or a refinery fire (Kroll-Smith & Couch, 1990). On top of that, contaminated sites usually take a very long time to deal with, from the process of contamination discovery, public agency investigations, scientific research into the contamination and possible remediation, corporate delay tactics and attempts to contest responsibility, and, frequently, litigation. Combined, the contamination discovery and its resolution can take many decades (e.g., Brown & Mikkelsen, 1997; Fagin, 2013).
Discoveries of toxic contamination alone are not enough to compel action or remediation. Polluting facilities and industries often seek to create obstacles for contaminated communities, while local and state governments may fail to act appropriately because they fear revenue loss and may also have political and personal ties to polluting companies. At the federal level, regulatory action is often weak because of anti-regulatory norms—and, as victims of chemical exposure have learned— the supposedly neutral science of risk is very politically involved, usually unlikely to confirm public health hazards, and often not beneficial to affected communities. This was illustrated by Clarke’s (1989) examination of the Binghamton, New York state office building fire that released high levels of PCBs. In this case, although the county health commissioner pressed for comprehensive biomonitoring of potentially exposed people, the state health department refused, having determined that the likely PCB exposures were an “acceptable risk.”
Sadly, people suffering from environmental illness often cannot get adequate help from health professionals either, mainly due to health professionals’ lack of education around issues of environmental hazards. Environmental health has been inadequately studied both by epidemiology and by medicine (Clapp & Ozonoff, 2004). Significantly, the work of environmental sociologists in collaboration with environmental health scientists has both called out this problem and offered practical solutions to dealing with it through litigation, corporate and governmental provision of alternative water sources, health surveys, health effects studies, and regulation. In their studies of activist responses to contaminated sites, sociologists have reported how hard it is for epidemiologists to gain federal and private grant support for environmental research (Clapp & Ozonoff, 2004). The National Institute of Environmental Health Sciences is one of the smallest institutes within NIH, and other institutes fund very little research on environmental factors. In medical training, occupational and environmental medicine have been relegated to a minor position, and the environmental dimension typically gets less attention than the occupational (Castorina & Rosenstock, 1990). Extensive evidence from clinician surveys and case reports of environmental health trainings show that health professionals are not sufficiently literate in environmental health (Brown et al., 2018; Trasande et al., 2010). These shortcomings are not surprising, since the larger society is generally unaware of environmental factors in disease causation. The “environmental health literacy” approach seeks to educate all sectors of society to not only understand environmental factors in disease, but to act on them (Finn and O’Fallon 2018).
Ultimately, health social movements are necessary to press the case for environmental causation of illness. These movements operate in various manifestations and combinations of demands for recognition of environmental health causation, better health access, more equity in health care, support for lay epistemologies of disease, and lay involvement in scientific research and medical practice. Health social movements arose in many non-environmental areas, such as health care access, women’s health, occupational health, AIDS, mental patients’ rights, and disability rights (Brown et al., 2004). These movements can be seen as falling into the following categories: health access movements, which seek equitable access to healthcare and improved provision of healthcare services; constituency-based health movements, such as the women’s health movement and gay and lesbian health movement, which focus on health inequalities rooted in race, ethnicity, gender, class and/or sexuality; and embodied health movements, which address disease, disability, or the experience of illness by challenging accepted scientific and medical perspectives on etiology, diagnosis, treatment, and prevention. Embodied health movements often mobilize around “contested illnesses” that are unexplained or unacknowledged by current medical science or whose purported environmental cause is disputed (Brown, 2007), and it is clear that much of what we have written above centers on this embodied experience. The contested illnesses that we wrote about above are especially in need of such a manifold health social movement approach because of their struggles against the many components of the dominant epidemiological paradigm.
Exposure Experience
Exposure experience is the process by which people identify, understand, and respond to chemical embodiment (Altman et al., 2008). It stems from the medical sociology concept of “illness experience,” which examines how people understand and live with disease, how it impacts their work and home lives, how it may lead them to challenge diagnostic definitions and treatment approaches, and how all the above are impacted by race, class, gender, and other elements of social structure (Bell, 2008; Lawton, 2003). Exposure experience developed as a concept later than the earlier experiences of social discovery and mobilization in contaminated communities. The earliest sociological research on contamination response involves people seeing visible contamination in forms such as chemical spills, explosions, soot deposition, seeping materials, and clouds of pesticide spray. The presence of such external contamination does not, however, show if it entered people’s homes and bodies. Household exposure offers the possibility of seeing what toxicants entered living and working spaces, and biomonitoring show how contaminants enter the internal human environment (Brody et al., 2007). Since contamination does not rely on proximity to a polluting facility, bodily exposure to contaminants makes people more aware of the ubiquity of those substances in the world around them and of the near-impossibility of avoiding exposure by moving elsewhere.
People’s experiences of household exposure and biomonitoring are shaped by place-based awareness of external contamination, as well as by the embodied experience resulting from testing of their homes and bodies. For example, low-income and largely people of color residents bordering a refinery in Richmond, CA were unsurprised at high levels of contaminants coming from the nearby facility, but were surprised to learn about contaminants coming from consumer products. Residents of a wealthier comparison area, Bolinas, who assumed their environments were very pristine and had tried to shop for healthy products, were even more surprised to learn about endocrine disruptors in their household air and dust (Adams et al., 2011). Participants in a household exposure report-back study in Cape Cod, MA interpreted their individual results through a shared history of living in an area that is considered to be a contaminated place, and had to rethink conceptions of pollution as they learned about contaminants in their homes coming from consumer products rather than a nearby military base (Altman et al., 2008).
When there is a direct economic connection to the polluter, exposure experience may combine criticism and litigation with support of the company’s importance to the region, and political mobilization may manifest later than in other cases. This was the situation in the Mid-Ohio Valley area affected by massive PFOA contamination from a DuPont Chemical factory which played a major role in the local economy (Judge et al., 2016). In Appalachia, Cable (1993) argues while individual forms of resistance are common, they may not always coalesce into collective resistance because people feel too constrained by the economic, and social power of companies that are often the major—if not sole—employer, and who exert a great deal of control over local politics. Cable’s study of chemical contamination of Yellow Creek, Kentucky found that people made complaints and attempted to work through institutional channels for many years, only mobilizing when the growth of the environmental movement made collective action seem more possible. But the economic and political power of local industry does not always lead to quiescence or to minimal levels of resistance. Indeed, the environmental justice movement had an especially firm origin in Louisiana towns and unincorporated areas that were overwhelmingly dominated by petrochemical firms (Allen, 2003).
Given the ongoing challenges in obtaining an adequate response from government and regulatory science, it has become increasingly clear that consumers, communities, and sympathetic scientists will need to develop and deploy alternate research approaches. We have touched on these earlier in discussion the importance of lay knowledge and research involvement and the growing trend of collaboration between environmental sociologists and environmental health scientists. In the next section, we discuss community-based approaches to studying and documenting toxic contamination in our environments and in our bodies.
New Research Methods and Sensibilities
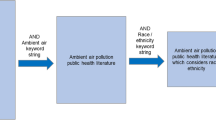
Community-Based Participatory Research
Because mainstream science and government were often unable or unwilling to conduct the research needed to show contamination and its effects, victims of toxic contamination were among the first laypeople to develop research collaborations with scientists. Such partnerships offer the potential for both individual and community empowerment in terms of achieving recognition of the problem, obtaining remediation, taking legal action, conducting research, and advocating for chemical regulation (Brown & Mikkelsen, 1997). There has been a long trajectory of community-based participatory research (CBPR) approaches (Wallerstein et al., 2017), coupled with resident-identified contamination through “popular epidemiology” (Brown & Mikkelsen, 1997) and “street science” (Corburn, 2005), yielding various ways to deal with community contamination. Due to advances in exposure sampling and analytical chemistry and the rise of CBPR models that employ household exposure and biomonitoring, more communities are able to access these techniques in order to study chemical body burdens (Morello-Frosch et al., 2009). Community-based exposure and biomonitoring projects help level information disparities between polluting industries and surrounding communities, creating access to otherwise inaccessible exposure data. Such research allows communities greater agency as they develop understandings, assert meanings, and respond to their exposure (Brody et al., 2007, 2014; MacKendrick, 2010; Washburn, 2014).
Community-based participatory research (CBPR) involves close, collaborative planning, conduct, and translation of research between participants and researchers. Research participants—often residents of impacted communities or community groups–are involved in the research at every step. This public involvement ensures that research questions are relevant and useful; increases the quality, quantity, and utility of collected data; and increases the potential for dissemination of research findings and their translation into policy interventions (Israel et al., 1998; O’Fallon and Dearry 2002; Wallerstein et al., 2017). We extend CBPR to include a deliberative, reflexive process to explore our engagement in such projects. This framework of reflexive research ethics involves self-conscious, interactive, and iterative reflection upon researchers’ commitment to serving activist needs, examining relationships with research participants and communities, and engaging with principles of professional and scientific conduct (Cordner et al., 2012; Panikkar et al., 2012). One demonstration of this concept is found in the practice of advocacy biomonitoring.
Advocacy Biomonitoring
Prompted by the development of the Center for Disease Control and Prevention’s National Health and Nutrition Examination Survey (NHANES) biomonitoring project, environmental activists quickly understood the value of showing people what contaminants were in their bodies. Advocacy biomonitoring involves laypeople, working through activist organizations to produce important environmental health science. These projects are often initiated by non-scientists, usually NGOs, who contract outside laboratories to conduct the chemical analyses. Some NGOs have scientists on staff, but they are not typically academic scientists who would have the ability to conduct the biomonitoring research on their own. Sample sizes are small, typically ranging from three to 30 people, so results are not intended to be analyzed statistically but rather to illustrate the number and type of chemicals in ordinary people. Many of these projects involve individuals publicly sharing their exposure data, along with photographs and biographies. These studies thereby become contamination narratives and calls for social change, as well as personal approaches to exposure reduction. Projects typically target chemicals that are less-studied and poorly regulated, and for which health implications and exposure sources often uncertain. These studies emphasize the importance of going beyond individual solutions to press for regulatory and corporate reform in order to reduce exposures (MacKendrick, 2018; Morello-Frosch and Brown 2014; Washburn, 2014). A new variant, conducted by Silent Spring Institute, uses crowd-sourced biomonitoring using the DetoxMe Action Kit, in which people pay to participate in urine biomonitoring for 10 emerging contaminants, as part of a national collaborative of participants.
CBPR Approaches to Biomonitoring and Household Exposure
The integration of social science in biomonitoring and household exposure studies has facilitated the development of new theories such as the “research right-to-know” (Morello-Frosch et al., 2009), “exposure experience” (Altman et al., 2008), and “politicized collective illness identity” (Brown, 2007) that have redefined and restructured exposure studies as a whole, while also increasing public understanding, environmental health literacy, community empowerment, and mutual trust and respect between researchers and study communities. Transdisciplinary environmental health research has increased public awareness of the effects of exposure, but has also moved beyond the physical and health consequences of environmental disaster and contamination to include community empowerment, ethical practices of sharing data, and policy implications (Brown, 2007; Brown et al., 2011). An example is the Household Exposure Study (HES), a CBPR project to evaluate exposures to pollutants from legacy contaminants, consumer products, and local emissions (Brody et al., 2009). Silent Spring Institute, an independent research center started through the efforts of the Massachusetts Breast Cancer Coalition, collaborated with academics in examining environmental exposures on Cape Cod. Later, in partnership with the environmental justice organization Communities for a Better Environment, Silent Spring expanded the HES to collect data in two Northern California communities. Community members were engaged at every level, as participants rather than subjects, in shaping their report-backs and the type of information that they would provide, as well as in pressing for governmental policy action (Adams et al., 2011; Brown et al., 2010).
Civic Science
Civic science (also called citizen science) has been a growing mechanism for affected communities to gather badly needed data about the chemicals and hazards they are being exposed to in their daily lives. While civic participation in scientific data collection has a long history (e.g., public ornithology), civic partnerships in scientific knowledge production (beyond residents merely serving as an instrument of data collection) are more recent—and have been key contributions of social science in this area. One significant example of such work can be seen in the efforts of the Louisiana Bucket Brigade to collect air quality samples in fenceline communities (Ottinger, 2010). Another community used a drift catcher to track drift from pesticide applications (Harrison, 2011). The Public Lab for Open Technology and Science pioneered developing tools for public monitoring of environmental quality, with a range of techniques such as using helium balloons equipped with digital cameras to detect oil spill effects from the BP oil spill, hydrogen sulfide detectors using photographic paper to visualize the toxic hazards associated with oil and gas development, and thermal bobs to detect water temperature increases from thermal pollution. These tools and other similar approaches enable communities to report toxic releases that are often unknown to or overlooked by regulatory agencies (Wylie, 2018). In this manner, they are providing broad social context for seemingly isolated instances of contamination, mobilizing affected residents, aiding social movements, challenging the dominant epidemiological paradigm, and developing alternative research approaches. That combination is indeed a deeply sociological approach to environmental health.
Developing a Transdisciplinary Approach
Transdisciplinary collaborations, such as the ones discussed here, replace the solo researcher or lab team with actively engaged community-based participant research teams though a series of negotiations and recursive interactions between disciplinary practices that bring together social scientists, environmental health scientists, and community groups and residents. This reflexive and iterative research process moves beyond multidisciplinarity, in which researchers maintain their respective disciplinary methods and perspectives, to a truly interdisciplinary form that fully integrates and engages with the overlaps and intersections between disciplines to ensure all facets are investigated (Russell et al., 2008). Furthermore, these projects give communities data to fully comprehend their exposure experience, to pressure the government to respond and remediate environmental harm, and to bring about policy change that is proactive and precautionary to prevent other communities from experiencing similar problems.
Public Sociology for Environmental Health
Putting all the above elements of research methods and sensibilities together, we arrive at a public sociology for environmental health. In the tradition of “public sociology” (Burawoy, 2004), this type of research seeks to inform debates and discussions outside of academia. In one example, the Contested Illnesses Research Group at Brown University worked with students in an undergraduate class and a community group, ENACT (Environmental Neighborhood Awareness Committee of Tiverton) to press the polluter and the state agencies for a cleanup agreement. They also succeeded in securing a major increase in polluter fines for companies failing to obey the state environmental agency’s orders, and in crafting a home equity loan program, the Environmentally Compromised Home Ownership (ECHO) Loan Program, that would provide loans from the state for residents living on or near contaminated sites (Senier et al., 2008).
In another example, researchers first at Brown University’s Contested Illnesses Research Group and later Northeastern University’s Social Science Environmental Health Research Institute undertook a strong public policy approach in studying the political, economic, scientific, and public discovery and action on emerging contaminants. For one class of those contaminants, flame retardants, researchers were part of a national coalition that contributed to the reduction in use and thus population exposure to flame retardants, as well as impacting regulatory reform in California that spread to other states and cities. The researchers contributed to the efforts of community groups working on local bans of flame retardants, and worked directly with manufacturers, fire marshals, firefighters, and scientists to reduce flame retardant use and to adopt safer flammability standards. For another class of chemicals—per- and polyfluorinated compounds (PFAS), researchers assisted affected communities in gaining scientific expertise, pressing state and federal agencies for cleanup and research, and mobilizing themselves into a national coalition of community-based organizations (Cordner et al., 2018). The range of methods and sensibilities we discuss here show the path for a highly engaged approach to environmental concerns, one in which the needs of affected people and communities are placed in the primary position of importance.
Toward Environmental Health and Justice for all
The Importance of Federal Funding
The political climate in the 1990s paved the way for rising support for government funding of environmental issues, especially after the first national People of Color Environmental Leadership Summit and the development of the Principles of Environmental Justice (Bullard, 1993). Additionally, National Institute of Environmental Health Sciences (NIEHS) director Kenneth Olden, a supporter of environmental justice and of community involvement in research, was appointed in 1991. By 1995, NIEHS had become the first of the National Institutes of Health (NIH) to create a CBPR grant initiative. New programs focused on environmental justice and the ethical, legal, and social implications of scientific research offered the infrastructure needed for social scientists and community groups to enter the NIEHS sphere. Annual meetings brought together grantees, creating a network in which environmental health and social science researchers learned from one another and developed additional collaborations. Eventually, social science research became a requirement for some NIEHS programs and projects, an essential step for promoting interdisciplinary environmental health research (Baron et al., 2009).
However, NIEHS represents only around 1.98 percent of the NIH budget (HHS, 2019), and there is relatively little environmental health research taking place throughout the rest of NIH. The EPA had some CBPR and environmental justice programs at one time, including the very successful Community Action for a Renewed Environment (CARE) program that provided grants that enabled communities to conduct environmental health assessments (Phase 1) and then proceed to amelioration and intervention approaches (Phase 2). But this successful program was always underfunded; in 2009, only 9 grants out of 235 proposals were awarded, representing less than a 4% funding rate (NEJAC, 2010). CARE was abruptly ended during President Obama’s administration in 2012. There are now relatively few opportunities for communities to access this type of funding through EPA. Similarly, the very successful Science to Achieve Results (STAR) program, which supported graduate students in various fields working on environmental problems and solutions was ended in 2015 without explanation.
The Regulatory Climate
The present regulatory climate is particularly unfriendly to the principles of environmental health and justice. The EPA has placed restrictions on oil and gas research throughout its portfolio, largely due to Congressional pressure. The Trump administration’s initial pick to head the EPA, Scott Pruitt, spent much of his previous career as Oklahoma attorney general suing the EPA over environmental regulations, and made it clear that his intention was to dismantle the agency (Davenport & Lipton, 2017). The EPA under Scott Pruitt reversed many progressive gains in environmental policy and regulation, and has removed many restrictions on industrial production, mining, and fossil fuel development. Andrew Wheeler, the head of EPA from 2018 to 2021, is a former coal industry lobbyist. Opposition to EPA’s recent actions has come from not only existing environmental and environmental health groups, but also from general science organizations like the Union of Concerned Scientists. New groups have sprung up specifically to deal with the Trump-era EPA’s anti-environmental approach. One such group, the Rapid Response Network, mobilizes people to comment on EPA rule changes during open comment sessions, and publicizes criticism of EPA actions. Another, the Environmental Data and Governance Initiative (EDGI), archives federal environmental data, monitors federal environmental websites for changes and deletions, and interviews past and present EPA staff to learn the history and current situation of EPA actions (Dillon et al., 2017, 2018). EDGI has been extensively cited in major media outlets and on the floor of the U.S. Congress, and represents a form of “data resistance” (Vera et al., 2018).
EPA policy and practice in the Trump era resembled that of the Reagan era, but even under Democratic leadership, the EPA has often been a revolving door with industry (Carpenter & Moss, 2014). The initial limitations on TSCA mentioned earlier were the result of direct corporate influence that has extended since the 1976 passage of that act (Richter et al., 2018). Environmental health and justice activists have a long history of struggles with EPA going back to Love Canal (Gibbs, 2002).
Manufacturers and Consumers
Although federal action on hazardous chemicals seems unlikely in the immediate future, industrial and consumer product manufacturers don’t need to wait for government mandates—they could choose to phase-out harmful chemicals and switch to safer alternatives, require chemical safety screenings, and make product ingredients and safety information publicly available. In practice, this usually requires significant pressure from activists and consumer groups. Activist and consumer-initiated pressure has already led many corporations to remove flame retardants and some PFAS from their products (Brown et al., 2020). Safer Chemicals Healthy Families—a coalition of 450 organizations and businesses representing more than 11 million individuals—successfully pressured leading home improvement retailers to remove the toxic chemicals methylene chloride and N-methylpyrrolidone (NMP) chemicals from their products by the end of 2018, after EPA’s proposed ban was shelved following Scott Pruitt’s confirmation as EPA Administrator.
Consumers are also using databases like Environmental Working Group’s Skin Deep database to search for nontoxic alternatives to conventional household and personal care products as well as Silent Spring Institute’s Detox Me Action Kit to better understand and reduce their exposure to common household chemicals. However, it is important to note that even if some of us are able to reduce our exposure to toxics within our own homes by investing the time and money required to research and purchase nontoxic products and foods, there is a limit to how much we can accomplish as individual consumers. We cannot, for example, control the chemicals used by our neighbors, let alone those by factories, power plants, or incinerators in our regions. Biomonitoring studies have found pollutants such as pesticides, lead, mercury and PCBs in the blood of people who were making deliberate efforts to reduce their exposure; some of the most careful shoppers, those who regularly purchase organic or natural products, had some of the highest levels of industrial chemicals in their bodies (Commonweal, 2007). People living in remote regions of the Arctic, thousands of miles from factories, also have chemicals flame retardants and PFASs in their blood, because they are found in the water, air, and animals that migrate north. Moreover, MacKendrick (2010) shows that as mainstream media outlets have increasingly focused on green consumption and individual acts of self-protection (rather than state action to prevent toxic exposures), the responsibility for this costly and time intensive “precautionary consumption” falls disproportionately on women and mothers—and does little to actually mitigate the risk of exposure to toxic hazards (MacKendrick, 2018). As sociologist Andrew Szasz (2007) concludes, we cannot, as individuals, “shop our way to safety.” Instead, the scale of the problem requires a collective political response. History tells us that no significant change is likely without broad-based social movements demanding that human and environmental health be prioritized over corporate profits.
Back to the Grassroots
Grassroots groups have been fighting for progressive change at the local level for decades, and that has helped shape the impressive new national focus on climate activism and mobilization around the Green New Deal. More recently, regional and national coalitions like the Alliance for a Healthy Tomorrow and Coming Clean have become important sites for collaboration, networking, and coordination between grassroots groups and other organizations. Increasingly these coalitions recognize that for genuine large-scale transformation, movements for environmental health and justice must ultimately be linked with larger struggles for social, economic, and racial justice. In February 2019, progressive Congressional representatives led by Rep. Alexandria Ocasio-Cortez (D-NY) and Senator Edward Markey (D-MA) introduced legislation to enact a Green New Deal— a policy approach that would transition the U.S. economy away from fossil fuels and address historical inequities in job access, housing, and transportation. Alternative frameworks for chemical regulation could conceivably fall within a Green New Deal umbrella.
Yet even in a future administration and with an EPA more in line with its original mission to protect human health and the environment, the effects of industry power, regulatory capture, and scientific conservatism on the policymaking apparatus will remain. Thus, the work of the many organizations that have made environmental health and justice their mission since the days of Alice Hamilton, Jane Addams, and Florence Kelly will continue. It is our hope that an ever-growing number of people will join the movement in demanding safer products, regulatory oversight based on the Precautionary Principle, an end to toxic exposures, remediation of existing hazardous sites, and restorative justice for communities that have suffered disproportionate harm. It is also our hope that environmental sociologists will continue to expand their practical work to further environmental justice, to engage in academic-community research partnerships to serve the needs of contaminated communities, to advance transdisciplinary work with environmental health scientists, and carry out advocacy along with their research. Together, we can create a world that is healthier, safer, and more just for us all.
References
Adams, C., Brown, P., Morello-Frosch, R., Brody, J., Rudel, R., Zota, A., et al. (2011). Disentangling the exposure experience: The roles of community context and report-back of environmental exposure data. Journal of Health and Social Behavior, 52(2), 180–196.
Allen, B. (2003). Uneasy alchemy: Citizens and experts in Louisiana’s chemical corridor disputes. Cambridge, MA: Mit Press.
Altman, R., Morello-Frosch, R., Brody, J., Rudel, R., Brown, P., & Averick, M. (2008). Pollution comes home and gets personal: Women’s experience of household chemical exposure. Journal of Health and Social Behavior, 49(4), 417–435.
Baron, S., Sinclair, R., Payne-Sturges, D., Phelps, J., Zenick, H., Collman, G. W., et al. (2009). Partnerships for environmental and occupational justice: Contributions to research, capacity and public health. American Journal of Public Health, 99, S517–S525.
Bell, S. (2008). Experience of illness and narrative understandings. In In Perspectives in Medical Sociology, edited by Phil Brown. Long Grove, IL: Waveland Press.
Bell, S. E. (2013). Our roots run deep as ironweed: Appalachian women and the fight for environmental justice. Chicago and Urbana: University of Illinois Press.
Bell, S. E. (2016). Fighting king coal: The challenges to micromobilization in central Appalachia. Cambridge, MA: MIT Press.
Bell, S. E., & York, R. (2012). Coal, injustice, and environmental destruction: Introduction to the special issue on coal and the environment. Organization & Environment, 25(4), 359–367.
Brody, J., Morello-Frosch, R., Brown, P., Rudel, R., Altman, R., Frye, M., et al. (2007). ‘Is it safe?’: New ethics for reporting personal exposures to environmental chemicals. American Journal of Public Health, 97(9), 1547–1554.
Brody, J., Morello-Frosch, R., Zota, A., Brown, P., Perez, C., & Rudel, R. (2009). Linking exposure assessment science with policy objectives for environmental justice and breast cancer advocacy: The northern California household exposure study. American Journal of Public Health, 99(S3), S600–S609.
Brody, J., Dunagan, S., Morello-Frosch, R., Brown, P., Patton, S., & Rudel, R. (2014). Reporting individual results for biomonitoring and environmental exposures: Lessons learned from environmental communication case studies. Environmental Health, 13(1), 40.
Brown, P. (1992). Popular epidemiology and toxic waste contamination: Lay and professional ways of knowing. Journal of Health and Social Behavior, 33, 267–281.
Brown, P. (2007). Toxic exposures: Contested illnesses and the environmental health movement. New York: Columbia University Press.
Brown, P., & Mikkelsen, E. (1997). No safe place: Toxic waste, leukemia, and community action. Berkeley: University of California Press.
Brown, P., Zavestoski, S., McCormick, S., Mayer, B., Morello-Frosch, R., & Altman, R. G. (2004). Embodied health movements: New approaches to social movements in health. Sociology of Health and Illness, 26, 50–80.
Brown, P., Morello-Frosch, R., Brody, J., Altman, R., Rudel, R., Senier, L., et al. (2010). Institutional review board challenges related to community-based participatory research on human exposure to environmental toxins: A case study. Environmental Health, 9(1), 39.
Brown, P., Morello-Frosch, R., Zavestoski, S., & the Contested Illnesses Research Group. (2011). Contested illnesses: Citizens, science, and health social movements. Berkeley: University of California.
Brown, P., Clark, S., Zimmerman, E., Miller, M., & Valenti, M. (2018). Health professionals’ environmental health literacy. In S. Finn & L. O’Fallon (Eds.), Environmental health literacy. New York: Springer.
Brown, P., De La Rosa, V., & Cordner, A. (2020). Toxic trespass and emerging contaminants: Science, activism, and policy for chemicals in our bodies. In A. Mah (Ed.), Environmental justice and citizen science in a post truth age. Manchester University Press.
Bullard, R. (1990). Dumping in Dixie: Race, class, and environmental quality. Boulder: Westview Press.
Bullard, R. (Ed.). (1993). Confronting environmental racism: Voices from the grassroots. Boston: South End Press.
Burawoy, M. (2004). Public sociologies: Contradictions, dilemmas, and possibilities. Social Forces, 82(4), 1603–1618.
Cable, S. (1993). From fussin’ to organizing: Individual and collective resistance at Yellow Creek. In S. L. Fisher (Ed.), Fighting back in Appalachia: Traditions of resistance and change. Temple University Press.
Carpenter, D., & Moss, D. (Eds.). (2014). Preventing regulatory capture: Special interest influence and how to limit it. New York, NY: Cambridge University Press.
Carson, R. (1962). Silent spring. Cambridge: The Riverside Press.
Castorina, J., & Rosenstock, L. (1990). Physician shortage in occupational and environmental medicine. Annals of Internal Medicine, 113, 983–986.
CDC (Center for Disease Control and Prevention). (2011, May). Asthma in the US growing every year. Vital Signs. https://www.cdc.gov/vitalsigns/asthma/index.html.
CDC. (2012). National surveillance of asthma: United States, 2001–2010. Vital and Health Statistics 3(35): November 2012. https://www.cdc.gov/nchs/data/series/sr_03/sr03_035.pdf.
CDC. (2018a). Most recent asthma data. https://www.cdc.gov/asthma/most_recent_data.htm.
CDC. (2018b). Fourth national report on human exposure to environmental chemicals. https://www.cdc.gov/exposurereport/index.html.
Checker, M. (2007). ‘But I know it’s true’: Environmental risk assessment, justice, and anthropology. Human Organization, 66(2), 112–124.
CHEJ (Center for Health, Environment and Justice). (2018). Love canal. http://chej.org/about-us/story/love-canal/.
Clapp, R. W., & Ozonoff, D. (2004). Environment and health: Vital intersection or contested territory? American Journal of Law & Medicine, 189–215.
Clarke, L. (1989). Acceptable risk?: Making decisions in a toxic environment. Berkeley: University of California Press.
Colborn, T., Dumanoski, D., & Myers, J. (1997). Our stolen future. New York: Penguin Group.
Colborn, T., Kwiatkowski, C., Schultz, K., & Bachran, M. (2011). Natural gas operations from a public health perspective. Human and Ecological Risk Assessment: An International Journal, 17(5), 1039–1056.
Commonweal. (2007). Is it in us? Chemical contamination in our bodies. https://www.commonweal.org/wp-content/uploads/2012/11/Is-It-In-Us-Report.pdf.
Corburn, J. (2005). Street science: Community knowledge and environmental health justice. Cambridge, MA: MIT Press.
Cordner, A. (2015). Defining and defending risk: Conceptual risk formulas in environmental controversies. Journal of Environmental Studies and Sciences, 5(3), 241–250.
Cordner, A. (2016, July 18). Why chemicals in the U.S. are still ‘innocent until proven guilty.’ Smithsonian Magazine. https://www.smithsonianmag.com/science-nature/why-chemicals-us-are-still-innocent-until-proven-guilty-180959818/#GmsWgJS5Y3QGmmUE.99.
Cordner, A., Ciplet, D., Morello-Frosch, R., & Brown, P. (2012). Research ethics for environmental health and justice: Academics and movement-building. Social Movement Studies, 11, 161–176.
Cordner, A., Richter, L., & Brown, P. (2016). Can chemical class approaches replace chemical-by-chemical strategies? Lessons from recent U.S. FDA regulatory action on per- and polyfluoroalkyl substances. Environmental Science & Technology, 50(23), 12584–12591.
Cordner, A., Brown, P., Richte, L. (2018). Environmental chemicals and public sociology: Engaged scholarship on highly fluorinated compounds. Paper presented at Annual Meeting of the American Sociological Association, 2018.
Cordner, A., De La Rosa, V. Y., Schaider, L. A., Rudel, R. A., Richter, L., & Brown, P. (2019). Guideline levels for PFOA and PFOS in drinking water: The role of scientific uncertainty, risk assessment decisions, and social factors. Journal of Exposure Science & Environmental Epidemiology: Official Journal of the International Society of Exposure Science, 29(2), 157–171.
Davenport, C., & Lipton, E. (2017, August 11). Scott Pruitt is carrying out his E.P.A. agenda in secret, critics say. New York Times. https://www.nytimes.com/2017/08/11/us/politics/scott-pruitt-epa.html.
Davis, D. (2002). When smoke ran like water: Tales of environmental deception and the battle against pollution. New York: Basic Books.
Dillon, L., Walker, D., Wylie, S., Shapiro, N., Lave, R., Martenyi, M., et al. (2017). Environmental data justice and the trump administration: Reflections on forming EDGI. Environmental Justice. Published Online December, 1, 2017.
Dillon, L. V. U., Shapiro, N., Sellers, C., Ohayon, J. L., Sullivan, M., Amoss, C., et al. (2018). The Environmental Protection Agency in the early trump administration: Prelude to regulatory capture. American Journal of Public Health, 108(S2), S89–S94.
Dowie, M. (1996). Losing ground: American environmentalism at the close of the twentieth century. Cambridge, MA: MIT Press.
Dunlap, R. E., & Brulle, R. J. (2015). Climate change and society: Sociological perspectives. New York, NY: Oxford University Press.
Edelstein, M. (1988). Contaminated communities: Coping with residential toxic exposure. Boulder, CO: Westview Press.
Erikson, K. (1976). Everything in its path: The destruction of community in the Buffalo Creek flood. New York: Simon & Schuster.
Erikson, K. T. (1994). A new species of trouble: The human experience of modern disasters. New York: Norton.
EWG (Environmental Working Group). (2009). Pollution in people: Cord blood contaminants in minority newborns. https://static.ewg.org/reports/2009/minority_cord_blood/2009-Minority-Cord-Blood-Report.pdf.
EWG. (2018a). Exposures add up–survey results. http://www.ewg.org/skindeep/2004/06/15/exposures-add-up-survey-results/#.WuY0u4gbPIU.
EWG. (2018b). Why this matters–cosmetics and your health. https://www.ewg.org/skindeep/why-this-matters-cosmetics-and-your-health/#.WuY5UogbPIU.
Fagin, D. (2013). Toms River: A story of science and salvation. New York: Bantam.
Finn, S., & O'Fallon, L. R. (Eds.). (2018). Environmental health literacy (Vol. 2019, 1st ed.). Cham: Springer.
Frickel, S. (2004). Just science? Organizing scientist activism in the US environmental justice movement. Science as Culture, 13(4), 449–780.
Frickel, S., & Moore, K. (2006). The new political sociology of science: Institutions, networks, and power. Madison, WI: University of Wisconsin Press.
Frickel, S., Gibbon, S., Howard, J., Kempner, J., Ottinger, G., & Hess, D. (2010). Undone science: Charting social movement and civil society challenges to research agenda setting. Science, Technology & Human Values, 35(4), 444–473.
Gibbs, L. (2002). Citizen activism for environmental health: The growth of a powerful new grassroots health movement. Annals of the American Academy of Political and Social Science, 584, 97–109.
Gibbs, L. M., & Levine, M. (1982). Love Canal: My story. Albany: State University of New York Press.
Gibbs, L., & Livesey, S. M. (2003). Organizing and leading the grassroots: An interview with Lois Gibbs, Love Canal homeowners' association activist, founder of citizens clearinghouse for hazardous waste, and executive director of the Center for Health, environment and justice. Organization & Environment, 16(4), 488–503.
Global Community Monitor. (2011, July 21). GASSED! Citizen investigation of toxic air pollution from natural gas development. http://gcmonitor.org/downloads/gassedreport.pdf.
Gottlieb, R. (1993). Forcing the spring: The transformation of the American environmental movement. Washington, DC: Island Press.
Gray, J. M., Rasanayagam, S., Engel, C., & Rizzo, J. (2017). State of the evidence 2017: An update on the connection between breast cancer and the environment. Environmental Health, 16, 94.
Harlan, S., Pellow, D. N., Roberts, J. T., Bell, S. E., Holt, W. G., & Nagel, J. (2015). Climate justice and inequality. In R. E. Dunlap & R. J. Brulle (Eds.), Climate change and society: Sociological perspectives. New York, NY: Oxford University Press.
Harrison, J. (2011). Pesticide drift and the pursuit of environmental justice. Cambridge MA: MIT.
Health and Human Services. (2019). US Department of. HHS FY 2018 budget in brief–NIH. Accessed Feb 9, 2019, from https://www.hhs.gov/about/budget/fy2018/budget-in-brief/nih/index.html
Hoover, E. (2017). The river is in us; fighting toxics in a Mohawk community. Minneapolis: University of Minnesota Press.
Hoover, E., Renauld, M., Edelstein, M., & Brown, P. (2015). Social science contributions to transdisciplinary environmental health. Environmental Health Perspectives, 123, 1100–1106.
Hudgins, A., & Poole, A. (2014). Framing fracking: Private property, common resources, and regimes of governance. Journal of Political Ecology, 21, 303–319.
Hsu, T. (2018, December 19). Johnson & Johnson loses bid to overturn a $4.7 billion baby powder verdict. The New York Times. https://www.nytimes.com/2018/12/19/business/johnson-johnson-baby-powder-verdict.html.
Israel, B. A., Schulz, A. J., Parker, E. A., & Becker, A. B. (1998). Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health, 19, 173–202.
Judge, M., Brown, P., Brody, J., Rudel, R., & Ryan, S. (2016). The exposure experience: Participant responses to a biomonitoring study of perfluorooctanoic acid (PFOA). Journal of Health and Social Behavior, 57, 333–350.
Krimsky, S. (2003). Science in the private interest: Has the lure of profits corrupted biomedical research? Lanham: Rowman & Littlefield.
Kaplan, L. (2000). Public participation in nuclear facility decisions: Lessons from Hanford. In D. L. Kleinman (Ed.), Science, technology, and democracy (pp. 67–86). Albany: SUNY Press.
Kroll-Smith, S., & Couch, S. (1990). The real disaster is above ground: A mine fire and social conflict. Lexington: University of Kentucky Press.
Ladd, A. E. (2018). Fractured communities: Risk, impacts, and protest against hydraulic fracking in U.S. shale regions. New Brunswick, New Jersey: Rutgers University Press.
Landrigan, P. J., Fuller, R., Acosta, N. J. R., Adeyi, O., Arnold, R., Basu, N., et al. (2017). The lancet commission on pollution and health. The Lancet, 391(10119), 462–512.
Langston, N. (2010). Toxic bodies: Hormone disruptors and the legacy of DES. New Haven and London: Yale University Press.
Lawton, J. (2003). Lay experiences of health and illness: Past research and future agendas. Sociology of Health & Illness, 25(3), 23–40.
Lerner, S. (2006). Diamond: A struggle for environmental justice in Louisiana’s chemical corridor. Cambridge, MA: MIT Press.
Levine, A. (1982). Love Canal: Science, politics, and people. Lexington, MA: Lexington Books.
Little, P. C. (2014). Toxic town: IBM, pollution, and industrial risks. New York, NY: New York University Press.
Lubitow, A. (2013). Collaborative frame construction in social movement campaigns: Bisphenol-a (BPA) and scientist-activist mobilization. Social Movement Studies, 12(4), 429–447.
Lubitow, A., & Davis, M. (2011). Pastel injustice: The corporate use of pinkwashing for profit. Environmental Justice, 4(2), 139–144.
MacKendrick, N. (2010). Media framing of body burdens: Precautionary consumption and the individualization of risk. Sociological Inquiry, 80(1), 126–149.
MacKendrick, N. (2018). Better safe than sorry: How consumers navigate exposure to everyday toxics. Berkeley, CA: University of California Press.
Malin, S. (2015). The price of nuclear power: Uranium communities and environmental justice. New Brunswick, New Jersey: Rutgers University Press.
Malin, S. A., Mayer, A., Shreeve, K., Olson-Hazboun, S. K., & Adgate, J. (2017). Free market ideology and deregulation in Colorado’s oil fields: Evidence for triple movement activism? Environmental Politics, 26(3), 521–545.
Malkan, S. (2016). “Johnson & Johnson is just the tip of the toxic iceberg.” Time Magazine. https://time.com/4239561/johnson-and-johnson-toxic-ingredients/
McCormick, S. (2007). Democratizing science movements. Social Studies of Science, 37(4), 609–623.
McKenzie, L. M., Crooks, J., Peel, J. L., Blair, B. D., Brindley, S., Allshouse, W. B., et al. (2019). Relationships between indicators of cardiovascular disease and intensity of oil and natural gas activity in northeastern Colorado. Environmental Research, 170, 56–64.
Michaels, D. (2008). Doubt is their product: How industry's assault on science threatens your health. Oxford: Oxford University Press.
Morello-Frosch, R., Brody, J., Brown, P., Altman, R., Rudel, R., & Perez, C. (2009). Toxic ignorance and right-to-know in biomonitoring results communication. Environmental Health, 8(1), 6.
Morello-Frosch, R., & Brown, P. (2014). Science, social justice, and post-belmont research ethics: Implications for regulation and environmental health science. In D. Kleinman & K. Moore (Eds.), Handbook of science, technology, and society. London: Routledge.
Murphy, M. (2004). Uncertain exposures and the privilege of imperception: Activist scientists and race at the U.S. Environmental Protection Agency. Osiris, 2nd Series, 19, 266–282.
Murphy, M. (2006). Sick building syndrome and the politics of uncertainty: Environmental politics, technoscience and women workers. Durham, NC: Duke University Press.
Nash, L. (2004). The fruits of ill-health: Pesticides and workers’ bodies in post-World War II California Osiris, 2nd Series, 19, 203–219.
Nash, L. (2006). Inescapable ecologies: A history of environment, disease and knowledge. Berkeley: University of California.
NEJAC (National Environmental Justice Advisory Council). (2010, April 6). Letter to EPA Administrator Lisa Jackson. https://www.epa.gov/environmentaljustice/letter-administrator-regarding-epas-care-program.
O'Fallon, L. R., & Dearry, A. (2002). Community-based participatory research as a tool to advance environmental health sciences. Environmental Health Perspectives, 110, 155–159.
Opsal, T., & O'Connor, S. T. (2014). Energy crime, harm, and problematic state response in Colorado: A case of the fox guarding the hen house? Critical Criminology, 22(4), 561–577.
Oreskes, N., & Conway, E. M. (2010). Merchants of doubt: How a handful of scientists obscured the truth on issues from tobacco smoke to global warming. New York: Bloomsbury Press.
Ottinger, G. (2010). Buckets of resistance: Standards and the effectiveness of citizen science. Science, Technology, and Human Values, 35, 244–270.
Panikkar, B., Smith, N., & Brown, P. (2012). Reflexive research ethics in fetal tissue xenotransplantation research. Accountability in Research: Policies and Quality Assurance, 19(6), 344–369.
President’s Science Advisory Committee (PSAC). (1963). Use of pesticides. Papers of John F. Kennedy. Presidential Papers. President's Office Files. Departments and Agencies.
Richter, L., Cordner, A., & Brown, P. (2018). Constructing ignorance: Environmental health data under the toxic substances control act. American Sociological Association Annual Meeting August, 11, 2018.
Roberts, T., & Toffolon-Weiss, M. (2001). Chronicles from the environmental justice frontlines. Cambridge, UK: Cambridge University Press.
Russell, A. W., Wickson, F., & Carew, A. L. (2008). Transdisciplinarity: Context, contradictions and capacity. Futures, 40, 460–472.
Saxton, D. I. (2015). Strawberry fields as extreme environments: The ecobiopolitics of farmworker health. Medical Anthropology, 34(2), 166–183.
Senier, L., Brown, P., Hudson, B., Fort, S., Hoover, E., & Tillson, R. (2008). The Brown superfund basic research program (SBRP): A multistakeholder partnership addresses real-world problems in a contaminated community. Environmental Science and Technology, 42(13), 4655–4662.
Silent Spring Institute. (2018). Risk factors for breast cancer. https://silentspring.org/risk-factors-breast-cancer-faq.
Simonelli, J. (2014). Home rule and natural gas development in New York: Civil fracking rights. Journal of Political Ecology, 14, 258–278.
Steingraber, S. (2010). Living downstream: An ecologist’s personal investigation of cancer and the environment (2nd ed.). Cambridge, MA: DaCapo Books.
Sumi, L. (2012). Enforcement report-COGCC: Inadequate enforcement means current Colorado oil and gas development is irresponsible. Earth, March 20.
Szasz, A. (2007). Shopping our way to safety: How we changed from protecting the environment to protecting ourselves. Minneapolis and London: University of Minnesota Press.
Trasande, L., Newman, N., Long, L., Howe, G., Kerwin, B. J., Martin, R. J., et al. (2010). Translating knowledge about environmental health to practitioners: Are we doing enough? Mt Sinai Journal of Medicine, 77, 114–123.
Travis, A. S. (1993). The rainbow makers: The origins of the synthetic dyestuffs industry in Western Europe. Bethlehem: Lehigh University Press.
Vera, L., Dillon, L., Brown, P., Sellers, C., Lemelin, A., Ohayon, J., et al. (2018). Data resistance: The work of the environmental data and governance initiative. Mobilization, 23, 511–529.
Wallerstein, N., Duran, B., Oetzel, J., & Minkler, M. (Eds.). (2017). Community-based participatory research for health: Advancing social and health equity (3rd ed.). New York: Wiley.
Washburn, R. (2014). Measuring personal chemical exposures through biomonitoring: The experiences of research participants. Qualitative Health Research, 24, 329–344.
WHO (World Health Organization). (2016). Preventing disease through healthy environments: A global assessment of the burden of disease from environmental risks. http://apps.who.int/iris/bitstream/handle/10665/204585/9789241565196_eng.pdf;jsessionid=857C9293CD473473D83126BA8F14DEDC?sequence=1.
Willow, A. (2014). The new politics of environmental degradation: Un/expected landscapes of disempowerment and vulnerability. Journal of Political Ecology, 21, 237–257.
Willow, A., & Wylie, S. (2014). Politics, ecology, and the new anthropology of energy: Exploring the emerging frontiers of hydraulic fracking. Journal of Political Ecology, 21(1), 222–236.
Wylie, S. (2011). Corporate bodies and chemical bonds: An STS analysis of natural gas development in the U.S. Dissertation, MIT History, Anthropology, and Science, Technology and Society Program.
Wylie, S. (2018). Fractivism: Corporate bodies and chemical bonds. Durham: Duke University Press.
Wylie, S., & Albright, L. (2014). Well watch: Reflections on designing digital media for multi-sited paraethnography. Journal of Political Ecology, 21, 320–348.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wilder, E., Brown, P. (2021). Environmental Factors in Health. In: Schaefer Caniglia, B., Jorgenson, A., Malin, S.A., Peek, L., Pellow, D.N., Huang, X. (eds) Handbook of Environmental Sociology. Handbooks of Sociology and Social Research. Springer, Cham. https://doi.org/10.1007/978-3-030-77712-8_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-77712-8_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-77711-1
Online ISBN: 978-3-030-77712-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)