Abstract
Neurodegenerative cognitive disorders have a huge impact on our societies, especially as the general population continues to grow older. These disorders include various dementias including Alzheimer’s dementia as the most common one. To date no effective treatments have been identified. Transcranial direct current stimulation (tDCS) has been tested for its effects in patients with neurodegenerative disorders, especially patients with Alzheimer’s dementia and mild cognitive impairment. Recent studies have also tested tDCS in frontotemporal dementia, Lewy body dementia, Parkinson’s disease, primary progressive aphasia, and vascular dementia. In general, studies show a positive effect on cognition and good tolerability when the disease is still in a mild clinical stage. Promising results are emerging when tDCS is combined with cognitive enhancement interventions. However, studies to date are limited by small sample sizes, large variability in parameters of stimulation, multiple exploratory outcomes, and lack of long-term interventions and assessments. Future studies need to address these limitations and the challenge of personalizing stimulation using, for example, modeling approaches. Future studies could also focus on prevention of cognitive decline and not only acute cognitive enhancement but also non-cognitive symptoms of these disorders. Finally, future research should add multidomain biological assessments to trials using tDCS alone or combined with cognitive enhancing interventions to better understand moderators and mechanism of action.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Alzheimer’s dementia
- Cognition
- Frontotemporal dementia
- Lewy body dementia
- Mild cognitive impairment
- Neurodegeneration
- Parkinson’s disease
- Prevention
- Primary progressive aphasia
- tDCS
Neurodegenerative cognitive disorders, also referred to as dementias, affect more than 46 million people worldwide [1]. By 2050, this number is estimated to be more than 131 million. The current costs associated with dementia are estimated to be US $818 billion . To date, there are no interventions to prevent, cure, or even slow down the underlying disease even though some pharmacological treatments could slow down the symptoms or for some of these disorders the underlying risk factors could be modified. Alzheimer’s dementia (AD) is the most common form of dementia. Other forms of dementia include vascular dementia, Lewy body dementia, frontotemporal dementia, Parkinson’s disease dementia, and others.
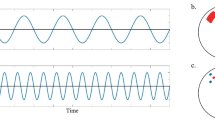
Transcranial direct current stimulation (tDCS) is a non-invasive brain stimulation method that can be safely administered to conscious outpatients (i.e., it does not require general anesthesia or surgical implantation of a device). It utilizes low intensity electrical current either to typically increase cortical excitability with an anodal electrode or suppress cortical excitability with a cathodal electrode [2]. Given its ease of use, portability, and high potential of scalability, several studies have tested the effect of tDCS in patients with dementia. Most studies have focused on patients with AD, and more recently studies have focused on mild cognitive impairment (MCI) or other forms of dementia and cognitive impairments. In this chapter, these studies are reviewed and classified based on the clinical condition they targeted. Specific details and summaries of the clinical and cognitive findings are also presented in Table 20.1.
1 Alzheimer’s Dementia
In Ferruci et al. [3], 10 participants with Alzheimer’s dementia (AD) received 3, 15-min tDCS sessions in a random order and 1 week apart: anodal transcranial direct current stimulation (tDCS), cathodal tDCS, and sham tDCS. Two stimulators were used. For each stimulator, one electrode was placed over the temporoparietal area (left or right) and the other over the right deltoid muscle. Current was 1.5 mA. Cognition was assessed before and 30 min after each session. Anodal tDCS improved word recognition and discrimination by 17% while cathodal tDCS impaired both.
In Boggio et al. [4], 10 participants with AD received 2, 30-min sessions of unilateral anodal tDCS – 1 session to the left dorsolateral prefrontal cortex (DLPFC), another to the left temporal cortex – and a third session of sham tDCS. Cathodal electrode was placed over the right supra-orbital area. Current was 2 mA. Cognition was assessed during stimulation. Anodal tDCS at both sites improved performance on a visual recognition memory task by 18% for the DLPFC and 14% for the temporal cortex [4].
The above two studies were followed by others that assessed the impact of a course of tDCS on cognition. In Boggio et al. [5], 15 participants with mild-to-moderate AD received daily consecutively for 5 days, 30-min sessions of bilateral anodal or sham tDCS in a random order. Anodes were placed over the temporal lobes. Cathodal electrode was placed over the right deltoid muscle. Current was 2 mA. Cognition was assessed before the first tDCS session, at the end of treatment on day 5, 1 week later, and then 4 weeks later. Anodal tDCS resulted in improvements in visual recognition memory, and these improvements persisted for 4 weeks following the course of tDCS. The percent change from baseline was about 11%. tDCS was well tolerated by all participants.
In Khedr et al. [6], 34 participants with mild-to-moderate AD were randomized to receive anodal tDCS, cathodal tDCS, or sham tDCS. tDCS was applied to the left DLPFC for 25 min daily for 10 days. The reference electrode was placed over the contralateral supra-orbital region. Current was 2 mA. Follow-up assessments were conducted immediately, and 1 and 2 months following the tDCS course. Other than for a couple of participants experiencing transient itching, headache, and dizziness, tDCS was well tolerated. Both anodal and cathodal tDCS resulted in improvement on Mini-Mental State Examination (MMSE) [7] compared with sham tDCS. The two forms of active tDCS did not differ in efficacy. Improvement on MMSE was by about four points with an initial improvement immediately following tDCS, an additional improvement 1 month later, and persistence of this improvement one additional month later. Such is a change is considered clinically significant.
In Bystad et al. [8], 25 participants with mild-to-moderate AD were randomized to receive anodal tDCS applied to the let temporal cortex with the cathodal electrode over the right frontal cortex or sham tDCS. tDCS was applied for 30 min daily for 5 days. Current was 2 mA. Follow-up assessments were conducted immediately. Other than for itching, transient headaches, and skin irritation, tDCS was well tolerated. Unlike, previous studies to date, active tDCS did not result in better verbal memory (primary outcome), global cognition, executive function, or processing speed compared to sham tDCS.
In a case report by the same group [9], a single participant with mild AD underwent an accelerated tDCS course of 12 sessions, twice a day, over 6 consecutive days. Each session consisted of anodal tDCS applied to the let temporal cortex with the cathodal electrode over the right frontal cortex and lasted for 30 min. Current was 2 mA. This report indicated that the participant experienced a clinically significant improvement in verbal memory recall and tDCS was well tolerated.
In another case report by the same group [10]), another single participant with mild AD received anodal tDCS daily for 8 months. The anode was placed over the left temporal cortex and the cathode over the right frontal cortex. Current was also 2 mA. tDCS was well tolerated. The participant experienced at the 8-month assessment 39% improvement in verbal immediate recall, 23% improvement in verbal delayed recall, 16% improvement in vocabulary, 10% decline in visuospatial ability, and general stability in other domains.
In Roncero et al. [11], 10 participants with AD (N = 3) or frontotemporal dementia (N = 7) were randomized in a cross-over design to active followed by sham tDCS (2 months later or vice versa) for 10 daily sessions. Anode was placed over the left inferior parietal cortex and the cathode over the right fronto-orbital region. Current was 2 mA. Each session was for 30 min. The primary outcome was picture naming. Active tDCS significantly improved picture naming ability by 40% vs. an improvement of 19% following sham tDCS.
In Cespon et al. [12], 12 participants with AD and 14 healthy older participants were randomized to receive anodal, cathodal or sham tDCS for 1 session delivered to the left DLPFC and then crossed over to receive all three types of stimulation with a 5-day interval between 2 consecutive sessions. The reference electrode was placed over the right shoulder. Current was 1.5 mA. Duration of stimulation was 13 min. Before and after each stimulation session, participants underwent a working memory task while undergoing an electroencephalogram (EEG). All participants were analyzed together. There were no differences detected in working memory performance among the three types of stimulation. However, anodal tDCS was associated with increased P200 and P300 amplitudes in healthy participants while cathodal tDCS was associated with increased P200 amplitude and frontal theta activity in AD participants. Further, only in healthy participants improvements in working memory after anodal tDCS were correlated with increased P300.
In Liu et al. [13], 17 participants with mild AD or mild cognitive impairment (MCI; mean age: 77, SD: 5) were randomized in a cross-over design to receive 1 session of bifrontal or bitemporal or sham tDCS, all separated by 1 week. During bifrontal stimulation, two anodes were placed over the left and right DLPFC and the cathode over the inion. During bitemporal stimulation, two anodes were placed over the left and right temporal cortices and the cathode over the inion. Current was 2 mA. Duration of stimulation was 20 min. On the day before each stimulation and immediately after, participants were assessed cognitively including an assessment of working memory which was the primary domain. The authors report that only following bitemporal stimulation the improvement in working memory was significantly higher than the improvement following sham.
A few studies reported on the impact of tDCS on maintaining cognitive stability among patients with AD rather than cognitive improvement.
In Im et al. [14], 20 participants with mild AD were randomized to receive anodal tDCS to the left DLPFC with the cathode over the right DLPFC, or sham tDCS, daily for 6 months, 30 min per day. The first 3 sessions were delivered by a nurse in a hospital setting and the remaining sessions were delivered at home by a caregiver. Current was 2 mA. Active tDCS resulted in better global cognition as measured using the MMSE and better naming compared to sham tDCS at 6 months. Those randomized to active tDCS also experienced a trend toward improvement in executive function while those randomized to sham tDCS experienced a trend toward a decline. Further, those randomized to active tDCS experienced stability on 18F-fluoro-2-deoxyglucose positron emission tomography (FDG-PET) over the left middle/inferior temporal gyrus compared to a significant decline among those randomized to sham tDCS.
In Gangemi et al. [15], two randomized trials were reported. In the first one, 26 participants with mild AD were randomized to active or sham tDCS, for 10 daily consecutive sessions. Each session lasted for 20 min. Current was 2 mA. Anode was placed over the left frontotemporal cortex and the cathode over the right frontal lobe. Global cognition and a composite measure of cognitive and function were assessed before and immediately after the 10-day course of tDCS. Active stimulation was associated with stability in cognition/function compared to a decline in cognition among those randomized to sham stimulation. In the second one, 18 participants with mild AD were randomized to a similar protocol except that they received the 10 sessions every month for 8 months. At the end of the 8 months, active stimulation was also associated with stability in cognition/function compared to a decline that was associated with sham intervention. The two studies support the beneficial impact of tDCS on maintaining cognition/function among patients with mild AD although it was not clear why there was a significant decline over 10 days among those who were randomized to sham tDCS. In both studies, resting EEG were collected before and after the interventions and there were changes reported within certain frequencies although it was not clear what the specific EEG analyzed variables were.
Patients with AD not only experience cognitive dysfunction, but also significant behavioral and psychological symptoms. One study focused on the effects of tDCS on apathy. In Suemoto et al. [16], 40 participants with moderate AD were randomized to receive anodal or sham tDCS delivered to the left DLPFC for 20 min, every other day for 6 sessions over 2 weeks. Cathodal electrode was placed over the right orbit. Current was 2 mA. Assessments were conducted at baseline, 1 week into the tDCS course, at the end of the 2-week course, and then 1 week after completing the course. The primary outcome measure was the score on the Apathy Scale [17]. tDCS was well tolerated with minor side effects, mainly scalp burning sensation and tingling. The two groups did not differ on Apathy Scale at any of the time points of assessments, nor did they differ on other secondary measure, including cognitive, mood, and caregiver burden measures.
Thus, studies in AD have had mixed results when assessing for an acute improvement following a short course of tDCS effect. However, and notwithstanding that the number of studies is small, those that assessed for a cognitive stabilization effect seems to have been more positive. A parallel line of research is to investigate whether the pro-cognitive effects of tDCS can optimize performance in response to other cognitive enhancing interventions, or whether they can be augmented through these other interventions.
In Cotelli et al. [18], 36 participants with mild-to-moderate AD were randomized to receive anodal tDCS combined with memory training, sham tDCS combined with memory training, or anodal tDCS combined with motor training. tDCS was applied to left DLPFC for 25 min, 5 days a week, for 2 weeks. The reference electrode was placed on the right deltoid muscle. Current was 2 mA. tDCS was initiated at the beginning of each training session that occurred 5 days a week for 2 weeks. Memory training consisted of training on face-name association task. Assessments were conducted at baseline, after the 2 weeks of tDCS course, and then 3 and 6 months from the start of the tDCS course. Both groups who received memory training experienced improvement in face-name association talk compared with the group who received motor training. The improvement persisted at 3 month follow-up. However, there was no significant generalization to other cognitive tasks beyond what the participants trained on. More importantly, groups who received anodal or sham tDCS, combined with memory training, did not differ in performance.
In Penolazzi et al. [19], one patient with mild AD received one course of anodal tDCS, daily for 20 min for 10 days, over the left DLPFC. Reference electrode was placed over the right supra-orbital area. Current was 2 mA. Each tDCS was followed by 45 min of cognitive training. Two months later, the patient received the same course of cognitive training but with sham tDCS. Following the first course, the patient experienced improvement in global cognitive function and it persisted for 1 month. There was no such improvement following the second course.
In Inagawa et al. [20], 20 participants with AD or MCI except for 2 with Lewy body disease were randomized to receive active or sham tDCS delivered during cognitive training and over 20 min, twice a day, for 5 consecutive days. Current was 2 mA. Anode was placed over the left DLPFC and the cathode over the right supra-orbital region. While active tDCS was well tolerated, it did not improve cognition as measured using the MMSE or the Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) [21] over sham tDCS.
2 Mild Cognitive Impairment
Given the early preliminary positive evidence supporting a pro-cognitive effect of tDCS in patients with AD, it was logical to assess its effects in pre-AD stages of the illness for potentially more impact on the course of illness.
In Meinzer et al. [22], 18 participants with MCI due to AD (11 amnestic MCI and 7 multiple domain MCI) received, in a cross-over design, 1 session of anodal or sham tDCS to the left inferior frontal gyrus for 20 min. The sessions were separated by 1 week . The cathode was placed over the right supra-orbital region. Current was 1 mA. Participants received tDCS while performing a semantic word-retrieval task and undergoing functional magnetic resonance imaging (fMRI). tDCS was well tolerated. During sham tDCS, participants performed worse than healthy control participants. In contrast, during anodal tDCS, their performance normalized to become comparable to that of the healthy control participants. This normalization was accompanied by normalization of task-related and resting-state brain activity as measured with fMRI.
In Yun et al. [23], 16 participants with MCI were randomized to receive active or sham tDCS for 3 sessions per week for 3 weeks. Anode was placed over the right DLPFC and the cathode over the left DLPFC. Current was 2 mA. Objective and subjective measures of cognition were completed before and after the tDCS course, as well as FDG-PET. tDCS was well tolerated. While there was no impact of active tDCS on objective measures of cognition, it was associated with better subjective measures and with increased cerebral metabolism in several brain regions, including dorsolateral, ventrolateral, and medial prefrontal cortices, the dorsal anterior cingulate, the anterior and posterior insular regions, and the hippocampal and parahippocampal regions.
In Fileccia et al. [24], 34 participants with MCI were randomized to receive active or sham tDCS, 1 session per day, 5 days per week for up to 20 sessions. Each session was 20 min. Current was 2 mA. Cognitive assessment was completed before and after the 20 sessions. The anode was placed over the left DLPFC and the cathode over the right deltoid. Active stimulation and not sham stimulation was associated with improved episodic memory, figure naming, and general cognition.
In Gomes et al. [25], 58 participants with MCI were randomized to active or sham tDCS, 2 sessions per week, each for 30 min, for 5 weeks with cognitive assessments completed before, and immediately and 90 days after the intervention. The anode was placed over the left DLPFC with the cathode over the right supra-orbital area. Current was 2 mA. Active stimulation was associated with better executive function, verbal fluency, and memory recall, but with worse visuospatial construction, when compared to sham stimulation immediately after the 10-session course. No results were reported on 90-day performances.
In Manenti et al. [26], 18 participants with amnestic MCI were randomized to receive 1 session of active or sham tDCS during the reactivation phase of an episodic memory task. The participants were administered the task on the day before. Then, they were tested on free recall and recognition on the day after and 30 days later. Each session was for 15 min. Current was 1.5 mA. The anode was placed over the left lateral prefrontal cortex and the cathode over the right supra-orbital region. Anodal tDCS was found to be associated with better recognition than sham tDCS after the day of stimulation, though it was not clear whether this was on the day after stimulation or 30 days later.
Similar to studies in AD, a few studies in MCI assessed the impact of adding tDCS to another cognitive enhancement intervention.
In Gonzalez et al. [27], 5 participants with MCI were assigned to receive cognitive stimulation for 3 daily sessions, followed by sham tDCS during cognitive stimulation for 1–5 daily sessions, followed by active tDCS during cognitive stimulation also for 1–5 daily sessions, followed by cognitive stimulation alone again. Each session was for 30 min. The anode was placed over the left DLPFC and the cathode over the right deltoid. Current was 2 mA. Each phase of this study was separated from the previous one by 1 week. Compared to cognitive stimulation alone, active tDCS with cognitive stimulation was associated with faster processing speed, attention, and planning.
In Das et al. [28], 22 participants with MCI were randomized to receive active or sham tDCS for 20 min while watching Planet Earth videos and right before starting a cognitive training session for a total of 8 sessions over 4 weeks. The anode was placed over the left inferior frontal gyrus and the cathode over the right shoulder. Current was 2 mA. In this study, sham tDCS was associated with better executive function, inhibition, innovation, and episodic memory even though active tDCS was associated with improved resting state cerebral blood flow in the right middle frontal cortex. These findings suggested that anodal tDCS inhibited any potential gains from the cognitive training program. The authors speculated that tDCS could have activated inhibitory homeostatic response that “blocked” benefit from cognitive training. Alternatively, the repeated stimulation could have increased “firing” of neuronal networks and, in turn, prevented consolidation of top-down learning strategies acquired during cognitive training. A third speculation the authors provided, suggested by the increase in cerebral blood flow on the right side, that is, the side opposite of stimulation, is that tDCS could have disrupted the allocation of cerebral blood flow, and, in turn, compromised the neuronal processes that support the learning strategies. Of note, tDCS was delivered before and not during the cognitive enhancement intervention, and while being cognitively engaged in watching a stimulating video, which also could have contributed to the “blocking” effect.
In Martin et al. [29], 68 participants with amnestic MCI were randomized to active or sham tDCS that was combined with cognitive training for 15 sessions administered 3 days per week over 5 weeks. Each cognitive training session lasted 45 to 60 min. During the first 30 min of each session, active tDCS at 2 mA was delivered followed by tDCS at 0.016 mA for the remaining of the session, or sham tDCS at 0.016 mA was delivered for the whole session, after ramping up and down for 1.5 min. The anode was placed over the left DLPFC and the cathode over the right frontal cortex. Cognitive assessments with verbal memory being the primary outcome domain were administered at baseline, end of treatment, and 30 days later. While there was no interaction between time and group, the study showed that only those who received active tDCS experienced improvement in verbal memory from baseline at the first follow-up and both groups experienced an improvement at the 30-day follow-up. Concerns regarding the potential active role of low intensity current was raised given the persistent improvement in verbal memory among those who received the sham intervention.
In de Sousa et al. [30], 18 participants with MCI and 32 healthy older control participants were randomized to receive first active or sham tDCS combined with a training session on a visuospatial task for 3 days followed by 3 months later, by the alternate stimulation combined with the 3-day training on the same task. Current was 1 mA. The anode was placed over the right temporoparietal cortex and the cathode over the left supra-orbital area. Stimulation was for 20 min. Cognitive assessment was completed immediately after the 3-day training and 1 month later. At the first follow-up, only the MCI participants experienced an enhanced training under active tDCS compared to sham tDCS. They also experienced a gain under active tDCS that is similar to what the healthy control participants gained from the training. However, these benefits did not persist at the 1-month follow-up.
Taken together, and notwithstanding that the studies to date need to be replicated in larger samples, there seems to be an advantage of using tDCS during the earlier stages of cognitive impairment including when it is being combined with a cognitive enhancement intervention.
3 Frontotemporal Dementia, Lewy Body Dementia, Parkinson’s Disease, Primary Progressive Aphasia, and Vascular Dementia
3.1 Frontotemporal Dementia
Frontotemporal dementia represents a group of neurodegenerative cognitive disorders that are typically characterized by early impairments in behavior, executive function, and language. Frontotemporal dementia is considered the third most common form of dementia following AD and Lewy body dementia [31]. Patients with frontotemporal dementia are divided into two subtypes depending on their predominant symptoms: behavioral or language subtype. The onset of frontotemporal dementia tends to be at a younger age than AD or Lewy body dementia. In addition to having no current treatments for the cognitive symptoms of frontotemporal dementia, and, in contrast to AD, there is minimal evidence to support treatments for the behavioral and emotional symptoms of this disorder.
In Benussi et al. [32], 55 participants with frontotemporal dementia were randomized to receive active or sham tDCS, 5 days per week for 2 weeks. Each session was for 20 min. Current was 2 mA. The anode was placed over the left DLPFC and the cathode over the right deltoid. Cognitive and neurophysiological assessments using transcranial magnetic stimulation (TMS) were completed at baseline, and then immediately and 3 and 6 months after the 2-week course of tDCS. TMS measures were also conducted at 1 month after the 2-week course. tDCS was well tolerated. Active stimulation was associated with better global cognition, verbal fluency, processing speed, executive function, emotions’ recognition, and behavioral symptoms compared to sham stimulation. Active stimulation was also associated with enhanced intracortical facilitation and enhanced inhibition as indexed using TMS. There was also a correlation between change in intracortical facilitation and change in processing speed and executive function.
3.2 Lewy Body Dementia
Lewy body dementia accounts for 3–15% of all dementias [33, 34]. It is typically characterized by fluctuating cognitive impairments, visual hallucinations, and Parkinsonian motor symptoms. It is also considered an umbrella that includes dementia of Lewy body and Parkinson’s disease dementia. The diagnosis of dementia with Lewy body is made when the motor symptoms develop within 1 year before or after the onset of cognitive deficits. In contrast, a Parkinson’s disease dementia diagnosis is made when the motor symptoms had been present for more than 1 year prior to the cognitive deficits [35]. Cholinesterase inhibitors are recommended for the treatment of Lewy body dementia, though their clinical impact is modest [36, 37].
In contrast to patients with AD, patients with Lewy body disease experience significant impairments in attention, executive function, and visuospatial abilities early on during the illness. These impairments may even precede deficits in learning and memory [38,39,40].
tDCS has been tested for its effects on Lewy body dementia-associated cognitive deficits. It has also been tested for its effects on cognitive impairment associated with Parkinson’s disease per se, that is, without a full manifestation of dementia.
In Boggio et al. [41], 18 participants with Parkinson’s disease received 1 session of anodal tDCS delivered to the left DLPFC for 20 min. Reference electrode was placed over the right orbit. They also underwent a session of motor cortex stimulation and sham tDCS to the left DLPFC. Current was 1 mA in one set of experiments and 2 mA in another set. Before and during the last 5 min of each tDCS session, participants were administered a working memory task. All experiments were well tolerated. tDCS at 1 mA did not result in any working memory change, In contrast, at 2 mA, left DLPFC stimulation resulted in more correct responses than motor cortex or sham tDCS. No change in speed of response was found.
In Pereira et al. [42], 16 participants with Parkinson’s disease were randomized to receive 1 session of anodal tDCS to the left DLPFC or left temporoparietal cortex in a counterbalanced order, for 20 min. The cathode was placed over the right supra-orbital area. Current was 2 mA. Anodal tDCS to the DLPFC resulted in improved phonemic but not semantic fluency. It also resulted in enhanced functional connectivity and task-related deactivation as measured with fMRI.
In Doruk et al. [43], 18 participants with Parkinson’s disease were randomized to receive anodal tDCS delivered to the left or right DLPFC, or sham tDCS for 20 min, daily, 5 days a week, for 2 weeks. The cathode was placed over the contralateral supra-orbital region. Current was 2 mA. Assessments were conducted at baseline, at the end of tDCS course, and 1 month following baseline. Overall, tDCS was well tolerated with reports of tingling, sleepiness, mild headache, neck pain, skin redness, and trouble concentrating. Anodal tDCS, irrespective of laterality, resulted in improved performance on executive function at the end of the tDCS course and that persisted at 1 month of follow-up. Sham tDCS resulted in improvement at the end of tDCS course, but the improvement did not persist. No significant effects were observed on other cognitive functions.
In Elder et al. [44], 13 participants with Lewy body dementia, including 8 with Parkinson’s disease dementia and 5 with dementia with Lewy bodies, received a single session of anodal tDCS delivered to the left DLPFC for 20 min. The cathode was placed over the right deltoid muscle. Current was 2.8 mA. Before and 10 min after the stimulation, attentional and visuospatial cognitive tasks that have been shown to detect Lewy body dementia-specific deficits were administered. Participants experienced improvements on some of the attentional but on none of the visuospatial tasks following tDCS. tDCS was well tolerated.
In Manenti et al. [45], 20 participants with MCI due to Parkinson’s disease were randomized to receive active or sham tDCS combined with physical therapy for 25 min per day, 5 days a week for 2 weeks. The anode was placed over the right or left DLPFC, contralaterally to the side of the body with more motor symptoms, for each individual. Current was 2 mA. Motor, mood, and cognitive symptoms were assessed at baseline and immediately and 3 months following the intervention. Despite no improvement over placebo with respect to motor or mood symptoms, participants randomized to active tDCS experienced better improvement in cognition immediately following the intervention and this enhanced improvement was stable at the 3-month assessment.
In Elder et al. [46], 38 participants with Parkinson’s disease dementia were randomized to receive a single session of active or sham tDCS for 20 min and then crossed over to receive the alternate stimulation after 24 hours. Current was 2.8 mA. The anode was placed over the left DLPFC and the cathode over the right deltoid. Cognitive assessment was completed following each session. The study did not demonstrate any significant difference in cognition between active and sham tDCS.
In Lau et al. (2019), 10 participants with Parkinson’s disease were randomized to 1 session of active or sham tDCS during the performance of a visual working memory and an emotional inhibition task. They were then crossed over to receive the alternate stimulation 2 weeks later. Current was 2 mA. The anode was placed on the left DLPFC and the cathode over the right supra-orbital area. No differences in performance on the two cognitive tasks were detected between active and sham stimulation.
Overall, the literature on Lewy body dementia is consistent with the literature in AD and MCI. While there is a mixture of positive and negative findings, the less severe the cognitive impairment, the more beneficial tDCS seems, especially when combined with a cognitive enhancement intervention.
3.3 Primary Progressive Aphasia
Primary progressive aphasia is a diagnosis used to identify a heterogeneous group of patients who experience localized degeneration of the language-related brain regions. Patients with primary progressive aphasia are typically classified into one of three variants: the no-fluent/agrammatic variant, when the early clinical presentation consists of slow, effortful, and distorted speech; the semantic variant, when the early clinical presentation consists of well-structured sentences but with poor content and significant loss of the vocabulary; and the logopenic variant, when the early clinical presentation consists of word-finding difficulty and lapses during conversations, as well as sound and spelling errors [47, 48]. Primary progressive aphasia is gradually progressive and during the later stages of the illness, the distinction between the different types of language deficits becomes blurred and cognitive domains other than language become affected. No treatments are available to date.
In de Aguiar et al. [49], 30 participants with primary progressive aphasia were randomized to receive active of sham tDCS for 20 min during the first part of 45-min therapy sessions that were delivered for 10–15 sessions in total. Two months later, participants were crossed over to receive another course of therapy with the alternate type of stimulation. Current was 2 mA. Anode was placed over the left inferior frontal gyrus and the cathode over the right cheek. Assessments were conducted at baseline and then immediately, 2 weeks, and 2 months after the end of therapy. Active stimulation was associated with better performance on trained words at the 2-month and not the previous follow-ups, compared to sham stimulation.
3.4 Vascular Dementia
While often in late life, dementias are associated with mixed pathologies, including pathologies of AD, Lewy body disease, and cerebrovascular disease, vascular dementia is diagnosed when the core clinical features are ascertained to be best attributed to vascular changes identified by brain imaging and cerebrovascular risk factors. The brain parenchymal changes can be ischemic or hemorrhagic in origin. Cerebral amyloid angiopathy can also lead to vascular dementia [50].
In Andre et al. [51], 21 participants with mild vascular dementia (mean age ~74) were randomized to receive active or sham tDCS, at home, for 1 session per day consecutively for 4 days. Current was 2 mA. Anode was placed over the left DLPFC and the cathode over the right supra-orbital region. A comprehensive cognitive battery was completed at baseline, immediately after the tDCS course and 2 weeks later. Compared to sham tDCS, active tDCS was associated with faster reaction times on a working memory task and an inhibition task. It was associated with better performance on a naming task. However, these measures were few among many other cognitive measures on which there were no differences were detected between active and sham tDCS.
4 Conclusions and Future Directions
Overall, the current literature suggests that tDCS is potentially a useful non-surgical neurostimulation modality to improve cognition in patients with neurodegenerative cognitive disorders, especially during the early clinical stages of these disorders and when combined with another intervention that enhances cognition synergistically. However, it is important to note all studies to date are limited by generally small sample sizes and multiple outcome measures that the studies are exploring. In turn, many of the positive studies have not found differences between active and sham stimulation but positive signal of improvement within the group receiving the active stimulation and not within the group receiving sham. Hence, confirmatory and adequately powered studies are urgently needed and some are underway in older healthy adults (e.g., Woods et al. [52]) and older adults with a neurocognitive disorder (e.g., Rajji et al. [53]).
The literature suggests that if tDCS is to be effective with a persistent impact, it needs to be delivered repetitively, similar to most other interventions for brain disorders. It also suggests that long-term delivery of tDCS, close to a daily frequency, could prevent cognitive decline among older adults with a neurodegenerative cognitive disorder. Studies assessing different durations of tDCS along with different frequencies per week will help characterize the dosing of tDCS. This is especially critical for patients with neurodegenerative disorders who may either need to commute to a center where tDCS is to be delivered or may depend on caregivers and their availabilities to administer it. There is a high need to study the feasibility, tolerability, and acceptability of different remotely delivered tDCS regimens, whether delivered alone or in combination with other cognitive enhancement interventions for patients across the severity spectrum of neurodegenerative disorders [54].
Electrodes placement and current intensity are two other variables that need further studying in various disorders. The current literature supports the use of anodal tDCS in general and 2 mA currents. Further personalization could be supported by modeling studies. Modeling studies predict the flow of current during tDCS [55] and help minimize the impact of morphological variation on tDCS effects. Again, this is highly salient to patients with neurodegenerative disorders who are likely to have experienced cortical shrinkage and tissue loss and using individualized tDCS dosing based on patient’s specific morphological characteristics may be necessary in future trials [56].
Combining tDCS with other interventions will add also another level of complexity to be systematically investigated. tDCS interferes with neuroplasticity mechanisms [57, 58] as do other interventions such as cognitive training [59]. Timing of tDCS in relationship with another intervention will need to consider the potential interference of one intervention with another at the level of neuroplasticity mechanisms.
Finally, multidomain studies that combine different biological assessments, for example, genetics structural and functional imaging, neurophysiology, within the context of well-powered clinical trials are needed to better understand moderators of tDCS impact on cognition or other symptoms of neurodegenerative disorders, as well as its mechanisms of action in vivo.
References
Alzheimer's-Association. Alzheimer’s disease facts and figures. Alzheimer Dement. 2015;11(3)
Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, Merabet L, et al. Clinical research with transcranial direct current stimulation (tDCS): challenges and future directions. Brain Stimul. 2012;5(3):175–95.
Ferrucci R, Mameli F, Guidi I, Mrakic-Sposta S, Vergari M, Marceglia S, et al. Transcranial direct current stimulation improves recognition memory in Alzheimer disease. Neurology. 2008;71(7):493–8.
Boggio PS, Khoury LP, Martins DCS, Martins O, de Macedo EC, Fregni F. Temporal cortex direct current stimulation enhances performance on a visual recognition memory task in Alzheimer disease. J Neurol Neurosurg Psychiatry. 2009;80(4):444–7.
Boggio PS, Ferrucci R, Mameli F, Martins D, Martins O, Vergari M, et al. Prolonged visual memory enhancement after direct current stimulation in Alzheimer's disease. Brain Stimul. 2012;5(3):223–30.
Khedr EM, El Gamal NF, El-Fetoh NA, Khalifa H, Ahmed EM, Ali AM, et al. A double-bling randomized clinical trial on the efficacy of cortical direct current stimulation for the treatment of Alzheimer's disease. Front Aging Neurosci. 2014;6
Folstein MF, Folstein SE, McHugh PR. Mini-mental state - practical method for grading cognitive state of patients for clinician. J Psychiatr Res. 1975;12(3):189–98.
Bystad M, Gronli O, Rasmussen ID, Gundersen N, Nordvang L, Wang-Iversen H, et al. Transcranial direct current stimulation as a memory enhancer in patients with Alzheimer's disease: a randomized, placebo-controlled trial. Alzheimers Res Ther. 2016;8
Bystad M, Rasmussen ID, Abeler K, Aslaksen PM. Accelerated Transcranial direct current stimulation in Alzheimer's disease: a case study. Brain Stimul. 2016;9(4):634–5.
Bystad M, Rasmussen ID, Gronli O, Aslaksen PM. Can 8 months of daily tDCS application slow the cognitive decline in Alzheimer's disease? A case study. Neurocase. 2017;23(2):146–8.
Roncero C, Kniefel H, Serivce E, Thiel A, Probst S, Chertkow H. Inferior parietal transcranial direct current stimulation with training improves cognition in anomic Alzheimer’s disease and frontotemporal dementia. Alzheimers Dement. 2017;3:247–53.
Cespon J, Rodella C, Miniussi C, Pellicciari MC. Behavioural and electrophysiological modulations induced by Transcranial direct current stimulation in healthy elderly and Alzheimer's disease patients: a pilot study. Clin Neurophysiol. 2019;130(11):2038–52.
Liu CS, Herrmann N, Gallagher D, Rajji TK, Kiss A, Vieira D, et al. A pilot study comparing effects of bifrontal versus bitemporal transcranial direct current stimulation in mild cognitive impairment and mild Alzheimer disease. J ECT. 2020;36(3):211–5.
Im JJ, Jeong H, Bikson M, Woods AJ, Unal G, Oh JK, et al. Effects of 6-month at-home transcranial direct current stimulation on cognition and cerebral glucose metabolism in Alzheimer's disease. Brain Stimul. 2019;12(5):1222–8.
Gangemi A, Colombo B, Fabio RA. Effects of short- and long-term neurostimulation (tDCS) on Alzheimer's disease patients: two randomized studies. Aging Clin Exp Res. 2021;33(2):383–90.
Suemoto CK, Apolinario D, Nakamura-Palacios EM, Lopes L, Paraizo Leite RE, Sales MC, et al. Effects of a non-focal plasticity protocol on apathy in moderate Alzheimer's disease: a randomized, double-blind, Sham-controlled Trial. Brain Stimul. 2014;7(2):308–13.
Starkstein SE, Mayberg HS, Preziosi TJ, Andrezejewski P, Leiguarda R, Robinson RG. Reliability, validity, and clinical correlates of apathy in Parkinson's disease. J Neuropsychiatry Clin Neurosci. 1992;4(2):134–9.
Cotelli M, Manenti R, Brambilla M, Petesi M, Rosini S, Ferrari C, et al. Anodal tDCS during face-name associations memory training in Alzheimer's patients. Front Aging Neurosci. 2014;6
Penolazzi B, Bergamaschi S, Pastore M, Villani D, Sartori G, Mondini S. Transcranial direct current stimulation and cognitive training in the rehabilitation of Alzheimer disease: a case study. Neuropsychol Rehabil. 2015;25(6):799–817.
Inagawa T, Yokoi Y, Narita Z, Maruo K, Okazaki M, Nakagome K. Safety and feasibility of transcranial direct current stimulation for cognitive rehabilitation in patients with mild or major neurocognitive disorders: a randomized sham-controlled pilot study. Front Hum Neurosci. 2019;13
Connor DJ, Sabbagh MN. Administration and scoring variance on the ADAS-Cog. J Alzheimers Dis. 2008;15(3):461–4.
Meinzer M, Lindenberg R, Mai Thy P, Ulm L, Volk C, Floeel A. Transcranial direct current stimulation in mild cognitive impairment: behavioral effects and neural mechanisms. Alzheimers Dement. 2015;11(9):1032–40.
Yun K, Song IU, Chung YA. Changes in cerebral glucose metabolism after 3 weeks of noninvasive electrical stimulation of mild cognitive impairment patients. Alzheimers Res Ther. 2016;8
Fileccia E, Di Stasi V, Poda R, Rizzo G, Stanzani-Maserati M, Oppi F, et al. Effects on cognition of 20-day anodal transcranial direct current stimulation over the left dorsolateral prefrontal cortex in patients affected by mild cognitive impairment: a case-control study. Neurol Sci. 2019;40(9):1865–72.
Gomes MA, Akiba HT, Gomes JS, Trevizol AP, Tavaes de Lacerda AL, Dias AM. Transcranial direct current stimulation (tDCS) in elderly with mild cognitive impairment: a pilot study. Dement Neuropsychol. 2019;13(2):187–95.
Manenti R, Sandrini M, Gobbi E, Binetti G, Cotelli M. Effects of Transcranial direct current stimulation on episodic memory in amnestic mild cognitive impairment: a pilot study. J Gerontol B Psychol Sci Soc Sci. 2020;75(7):1403–13.
Gonzalez PC, Fong KNK, Brown T. The effects of transcranial direct current stimulation on the cognitive functions in older adults with mild cognitive impairment: a pilot study. Behav Neurol. 2018;2018
Das N, Spence JS, Aslan S, Vanneste S, Mudar R, Rackley A, et al. Cognitive training and transcranial direct current stimulation in mild cognitive impairment: a randomized pilot trial. Front Neurosci. 2019;13
Martin DM, Mohan A, Alonzo A, Gates N, Gbadeyan O, Meinzer M, et al. A pilot double-blind randomized controlled trial of cognitive training combined with transcranial direct current stimulation for amnestic mild cognitive impairment. J Alzheimers Dis. 2019;71(2):503–12.
de Sousa AVC, Grittner U, Rujescu D, Külzow N, Flöel A. Impact of 3-day combined anodal transcranial direct current stimulation-visuospatial training on object-location memory in healthy older adults and patients with mild cognitive impairment. J Alzheimers Dis. 2020;75(1):223–44.
Bang J, Spina S, Miller BL. Frontotemporal dementia. Lancet. 2015;386(10004):1672–82.
Benussi A, Dell'Era V, Cosseddu M, Cantoni V, Cotelli MS, Cotelli M, et al. Transcranial stimulation in frontotemporal dementia: a randomized, double-blind, Sham-Controlled Trial. Alzheimers Dement. 6(1):e12033.
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology. 1996;47(5):1113–24.
Kosaka K, Yoshimura M, Ikeda K, Budka H. Diffuse type of Lewy body disease – progressive dementia with abundant cortical Lewy bodies and senile changes of varying degree – a new disease. Clin Neuropathol. 1984;3(5):185–92.
Hansen L, Salmon D, Galasko D, Masliah E, Katzman R, Deteresa R, et al. The Lewy body variant of Alzheimers-disease – a clinical and pathological entity. Neurology. 1990;40(1):1–8.
McKeith I, Del Ser T, Spano P, Emre M, Wesnes K, Anand R, et al. Efficacy of rivastigmine in dementia with Lewy bodies: a randomised, double-blind, placebo-controlled international study. Lancet. 2000;356(9247):2031–6.
Stinton C, McKeith I, Taylor J-P, Lafortune L, Mioshi E, Mak E, et al. Pharmacological management of Lewy body dementia: a systematic review and meta-analysis. Am J Psychiat. 2015;172(8):731–42.
Collerton D, Burn D, McKeith I, O'Brien J. Systematic review and meta-analysis show that dementia with Lewy bodies is a visual-perceptual and attentional-executive dementia. Dement Geriatr Cogn Disord. 2003;16(4):229–37.
Tiraboschi P, Salmon DP, Hansen LA, Hofstetter RC, Thal LJ, Corey-Bloom J. What best differentiates Lewy body from Alzheimer's disease in early-stage dementia? Brain. 2006;129:729–35.
Meireles J, Massano J. Cognitive impairment and dementia in Parkinson's disease: clinical features, diagnosis, and management. Front Neurol. 2012;3:88.
Boggio PS, Ferrucci R, Rigonatti SP, Covre P, Nitsche M, Pascual-Leone A, et al. Effects of transcranial direct current stimulation on working memory in patients with Parkinson's disease. J Neurol Sci. 2006;249(1):31–8.
Pereira JB, Junque C, Bartres-Faz D, Marti MJ, Sala-Llonch R, Compta Y, et al. Modulation of verbal fluency networks by transcranial direct current stimulation (tDCS) in Parkinson's disease. Brain Stimul. 2013;6(1):16–24.
Doruk D, Gray Z, Bravo GL, Pascual-Leone A, Fregni F. Effects of tDCS on executive function in Parkinson's disease. Neurosci Lett. 2014;582:27–31.
Elder GJ, Firbank MJ, Kumar H, Chatterjee P, Chakraborty T, Dutt A, et al. Effects of transcranial direct current stimulation upon attention and visuoperceptual function in Lewy body dementia: a preliminary study. Int Psychogeriatr. 2015:1–7.
Manenti R, Brambilla M, Benussi A, Rosini S, Cobelli C, Ferrari C, et al. Mild cognitive impairment in Parkinson's disease is improved by transcranial direct current stimulation combined with physical therapy. Mov Disord. 2016;31(5):715–24.
Elder GJ, Ashcroft J, Morgan KD, Kulsum MU, Banerjee R, Chatterjee P, et al. Transcranial direct current stimulation in Parkinson's disease dementia: a randomised double-blind crossover trial. Brain Stimul. 2017;10(6):1150–1.
Marshall CR, Hardy CJD, Volkmer A, Russell LL, Bond RL, Fletcher PD, et al. Primary progressive aphasia: a clinical approach. J Neurol. 2018;265(6):1474–90.
Montembeault M, Brambati SM, Gorno-Tempini ML, Migliaccio R. Clinical, anatomical, and pathological features in the three variants of primary progressive aphasia: a review. Front Neurol. 2018;9
de Aguiar V, Zhao Y, Faria A, Ficek B, Webster KT, Wendt H, et al. Brain volumes as predictors of tDCS effects in primary progressive aphasia. Nrain Lang. 2020;200:104707.
Vinters HV, Zarow C, Borys E, Whitman JD, Tung S, Ellis WG, et al. Review: vascular dementia: clinicopathologic and genetic considerations. Neuropathol Appl Neurobiol. 2018;44(3):247–66.
Andre S, Heinrich S, Kayser F, Menzler K, Kesselring J, Khader PH, et al. At-home tDCS of the left dorsolateral prefrontal cortex improves visual short-term memory in mild vascular dementia. J Neurol Sci. 2016;369:185–90.
Woods AJ, Cohen R, Marsiske M, Alexander GE, Czaja SJ, Wu S. Augmenting cognitive training in older adults (the ACT study): design and methods of a phase III tDCS and cognitive training trial. Contemp Clin Trials. 2018;65:19–32.
Rajji TK, Bowie CR, Herrmann N, Pollock PB, Bikson M, Blumberger DM, et al. Design and rationale of the PACt-MD randomized clinical trial: prevention of Alzheimer's dementia with cognitive remediation plus Transcranial direct current stimulation in mild cognitive impairment and depression. J Alzheimers Dis. 2020;76(2):733–51.
Gough N, Brkan L, Subramaniam P, Chiuccariello L, De Petrillo A, Mulsant BH, et al. Feasibility of remotely supervised transcranial direct current stimulation and cognitive remediation: a systematic review. PLoS One. 2020;15(2)
Bikson M, Rahman A, Datta A, Fregni F, Merabet L. High-resolution modeling assisted design of customized and individualized transcranial direct current stimulation protocols. Neuromodulation. 2012;15(4):306–15.
Mahdavi S, Yavari F, Gharibzadeh S, Towhidkhah F. Modeling studies for designing transcranial direct current stimulation protocol in Alzheimer's disease. Front Comput Neurosci. 2014;8
Ranieri F, Podda MV, Riccardi E, Frisullo G, Dileone M, Profice P, et al. Modulation of LTP at rat hippocampal CA3-CA1 synapses by direct current stimulation. J Neurophysiol. 2012;107(7):1868–80.
Fritsch B, Reis J, Martinowich K, Schambra HM, Ji YY, Cohen LG, et al. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron. 2010;66(2):198–204.
Vinogradov S, Fisher M, de Villers-Sidani E. Cognitive training for impaired neural systems in neuropsychiatric illness. Neuropsychopharmacology. 2012;37(1):43–76.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rajji, T.K. (2021). Neurodegenerative Cognitive Disorders. In: Brunoni, A.R., Nitsche, M.A., Loo, C.K. (eds) Transcranial Direct Current Stimulation in Neuropsychiatric Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-76136-3_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-76136-3_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-76135-6
Online ISBN: 978-3-030-76136-3
eBook Packages: MedicineMedicine (R0)