Abstract
In the past few years, we have seen major breakthroughs in the treatment of lung cancer, especially non-small-cell lung cancer (NSCLC). Targeted therapy for late-stage adenocarcinoma has greatly expanded the clinical utility of molecular testing. Immunotherapy with immune checkpoint inhibitors further extended the benefit of novel therapeutics to other lung cancer types. In this chapter, the molecular basis and mutation landscape of lung cancer are reviewed; the clinically significant mutations are discussed in detail. Every aspect of the molecular genetic testing for lung cancer, from current standard of care recommended in the practice guidelines to recent developments including tumor mutation burden (TMB) measurement and liquid biopsy, are elaborated from indications, test methodologies, and result analyses to clinical reporting. At the end, six cases are presented for readers to learn the pathologic features and molecular genetic tests of NSCLC in different clinical scenarios.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Lung cancer
- Molecular testing
- Targeted therapy
- Mutation
- Chromosome rearrangement
- Next-generation sequencing (NGS)
- Immuno-oncology
- Tumor mutation burden (TMB)
- Liquid biopsy
List of Frequently Asked Questions
-
1.
What are the major types of lung cancer and how are they different in the molecular mechanisms of tumorigenesis?
-
2.
What are the clinically significant genetic abnormalities seen in lung adenocarcinoma?
-
3.
What is the mutation landscape of squamous cell carcinoma of the lung?
-
4.
When is mutation testing for squamous cell carcinoma indicated?
-
5.
What is the mutation landscape of small cell lung cancer?
-
6.
Are there any clinically significant genetic alterations associated with other relatively uncommon lung cancer types?
-
7.
What is the purpose of molecular genetic testing for lung cancer?
-
8.
What genes/mutations should be tested for non-small-cell lung cancer?
-
9.
When should a lung cancer sample be tested for mutation profile?
-
10.
When multiple lung cancer lesions and/or multiple metastatic tumors are identified and excised/biopsied in one patient, should each of them be tested for mutation profile separately?
-
11.
How are different types of genetic aberrations of lung cancer tested in the clinical diagnostic laboratories?
-
12.
What are the benefits and challenges of using next generation sequencing-based tests for non-small-cell lung cancer?
-
13.
What are the specimen types acceptable for mutation profiling of lung cancer?
-
14.
What is the role of cell-free DNA testing (liquid biopsy) for lung cancer?
-
15.
What is the clinical significance of tumor mutation burden (TMB) in lung cancer and how is it tested?
-
16.
What other tests can be considered to provide guidance for immunotherapy of lung cancer?
Frequently Asked Questions
-
1.
What are the major types of lung cancers and how are they different in the molecular mechanisms of tumorigenesis?
-
Lung cancer is a common cancer and the leading cause of cancer deaths in the Western world. Although the incidence and death rate have been declining since 1990 per statistics published by the American Cancer Society in 2020 [1], lung cancer is still ranked #2 of all new cancer cases (excluding basal cell and squamous cell skin cancers and in situ carcinoma except urinary bladder) in both males and females (estimated over 110,000 cases in each sex in 2020) and #1 in all cancer deaths (72,500 males and 63,220 females, both >20% of all cancer deaths) in the United States.
-
In clinical practice, the major lung cancer types are non-small-cell lung cancer (NSCLC), including adenocarcinoma, squamous cell carcinoma, and other relatively less common types and small cell lung cancer (SCLC) [2]. Adenocarcinoma and squamous cell carcinoma comprise approximately 70%, SCLC 15–20% of all lung cancers [3].
-
Tobacco smoking has been recognized as the major cause of lung cancer, responsible for over 85% of all lung cancer cases [4]. The percentage of cigarette-smoking-caused lung cancers has declined thanks to the mass media campaigns and tobacco control policies [5, 6]. There are significant differences in the molecular tumorigenesis between cigarette-smoking-related and unrelated lung cancers. The tobacco smoke carcinogen-induced mutations are frequently G to T transversions, such as RAS codon 12 GGT (glycine) mutated to TGT (cysteine) or GTT (valine), and loss of function mutations of the tumor suppressor gene TP53.
-
Overall, activating mutations of oncogenes are frequently seen in adenocarcinoma not related to cigarette smoking, resulting in self-sufficiency in growth signals, insensitivity to antigrowth signals, and evasion of apoptosis. The clinically significant alterations in this category include activating mutations in genes encoding the epidermal growth factor receptor (ERBB receptor tyrosine kinases) and related elements in the cell proliferation and survival signal pathways, and rearrangement involving ALK1 or ROS1. Loss of function mutations of tumor suppressor genes are more common in tobacco-related SCLC and SCC. These mutations also occur in adenocarcinoma of nonsmokers but are usually not the driver mutations [3].
-
It is much more difficult to target a loss of function (tumor suppressor genes) than an activating alteration. Currently available targeted therapies, therefore, mostly apply to adenocarcinoma in non-smokers, whose tumors show so-called oncogene addiction. Small molecules inhibiting the protein kinases overactive due to genetic alterations represent the major breakthrough in the treatment of NSCLC. On the other hand, loss of tumor suppressor functions frequently results in accumulation of secondary mutations and higher mutation load in the tumor. These tumors are more likely to have neoantigens and, therefore, may respond better to immunotherapies, which is the second breakthrough of lung cancer treatment, clinically effective for the non-oncogene-addicted tumors.
-
-
2.
What are the clinically significant genetic abnormalities seen in lung adenocarcinoma?
-
Multiple genetic abnormalities are associated with lung adenocarcinoma. According to the data archived at cBioportal.com, the most commonly mutated genes in lung adenocarcinoma are (in the order of highest to lowest) TP53 (52.4%), KRAS (30.5%), EGFR (24.2%), STK11 (16.8%), and KEAP1 (15.8%); the genes most commonly involved in translocation/fusion are ALK (2.2%), EML4 (2.0%), ROS1 (1.5%), CD74 (1.0%), and RET (1.0%). They can either be grouped into driver mutations versus non-driver mutations based on their roles in tumorigenesis, or into actionable mutations versus non-actionable mutations based on whether there are drugs targeting the specific mutation.
-
Currently, the actionable mutations/alterations in adenocarcinoma with approved drugs include [7, 8]:
-
EGFR mutations: Mutations occur throughout the EGFR (ERBB1) gene, resulting in abnormal activation of the EGFR kinase activity. Majority of the mutations occur in exon 18–21, encoding the protein kinase domain [9].
-
ALK rearrangements: ELM4-ALK1 is the most common ALK fusion gene [10].
-
ROS1 rearrangements: ROS1 has various partner genes with CD74 being the most common one [11].
-
MET abnormalities include exon 14 skipping and MET amplification, both leading to increased MET protein level and kinase activity [12].
-
BRAF mutations: BRAF mutations in lung adenocarcinoma have a different spectrum from that seen in melanoma; BRAF c.1799T > A; p.V600E only comprises approximately 50% of all BRAF mutations [13].
-
RET rearrangements are rare, present in only 1–2% of lung adenocarcinoma [14].
-
Neurotrophic tyrosine receptor kinase ( NTRK ) fusions: NTRK1 fusion proteins are relatively common in lung adenocarcinoma; NTRK2 and NTRK3 fusions are present at low frequencies [15].
-
HER2 : Mutations in the kinase domain of ERBB2 (HER2/neu), one of the epidermal growth factor receptor or ErbB family tyrosine kinases, are found in approximately 1–4% of lung adenocarcinomas [16,17,18]. They are seen in tumors with a similar phenotype to those harboring EGFR mutations.
-
-
EGFR mutations are the most common targetable mutations in lung adenocarcinoma and have a high prevalence in younger, female, Asian non-smoker patients. The inframe deletion in exon 19 (see case 1 as an example) and c.2573T > G; p.Leu858Arg (L858R) mutation in exon 21 together comprise approximately 90% of all EGFR mutations, with the prevalence of exon 19 deletion slightly higher than that of L858R [9]. These two mutations are sensitive to the tyrosine kinase inhibitors (TKIs). The responsiveness to TKIs varies for the other less commonly seen mutations, such as EGFR c.2155G > A; p.G719S, c.2582T > A; p.L861Q, and c.2303G > T; p.S768I, etc.
-
In addition to the targetable EGFR mutations, there are also mutations associated with drug resistance. Identifying them helps to predict the responsiveness to targeted therapy. Two well-defined EGFR mutations are associated with resistance to first- and second-generation EGFR TKIs. Patients carrying these two mutations usually respond to therapy with a third generation TKI.
-
The EGFR c.2369C > T; p.Thr790Met (T790M) mutation is the most common mutation in EGFR that is responsible for acquired resistance to the first- and second-generation TKIs. The incidence of T790M in treatment-naïve patients is less than 1%, whereas in first- and second-generation TKI-treated patients, it can be as high as ~50% [19, 20] (see case 2 as an example).
-
EGFR exon 20 insertion is considered the major mechanism of refractoriness to the first- and second-generation TKIs in treatment-naïve patients [21].
-
-
ALK1 or ROS1 rearrangement creates a fusion protein with constitutive tyrosine kinase activity. They occur in lung adenocarcinoma at low frequency, with ALK1 rearrangements in 1–3% and ROS1 rearrangements in 0.7–3.4% of Caucasian patients [22] [23]. In NSCLC, ELM4 is the most common fusion partner of ALK1; other partner genes, such as TGF, KLC1, and KIKF5B, are rare [24]. The partner gene provides the dimerization domain required for the constitutive activation of ALK1 kinase [24, 25]. More than 20 variants of ELM4-ALK1 fusion proteins have been identified, all containing the intracellular kinase domain of ALK1, but variable length of ELM4 due to different breakpoints. The trimerization domain (TD) of ELM4 is required for the constitutive activity of ELM4-ALK1 fusion protein. The presence and the length of the tandem atypical propeller (TAPE) domain of ELM4 affect protein localization and sensitivity to ALK1 inhibitors [10, 25, 26]. CD74, SDC4, EZR, and SLC34A2 are well-documented ROS1 fusion partners, among which CD74 is the most common one, comprising approximately 38% of all ROS1 fusions [11]. ROS1 can also be rearranged to partner with TPM3, MYH9, CCDC6, FIG, LRIG3, KDELR2, MSN, TMEM106B, TPD52L1, CLTC, and LIMA1 [27]. Unlike ALK1 and ROS1 rearrangements that have multiple breakpoints, ROS1 fusions with CD74 and EZR often occur at intron 33, whereas breakpoints at intron 31 are more frequently seen in fusions with SDC4 and SLC34A2 [11]. The underlying mechanisms of how the fusions lead to ROS1 kinase activation is currently unknown. The presence of ALK1 or ROS1 rearrangement predicts sensitivity to ALK1 or ROS1 kinase inhibitors. Due to a high degree of homology between the kinase domains of ALK1 and ROS1 [28], most of the currently available ALK inhibitors including crizotinib, ceritinib, lorlatinib, etc., also show cross inhibitory effect on ROS1 fusion proteins [29].
-
MET exon 14 skipping refers to the loss of exon 14 due to mutations at the splice site or nearby introns. Exon 14 skipping and mutation of codon Y1003 prevent Casitas B-lineage lymphoma proto-oncogene (c-CBL) E3 ligase binding, resulting in decreased protein degradation and increased MET protein level, enhanced MET phosphorylation, and prolonged MET activation [12]. MET amplification is frequently seen in acquired resistance to EGFR inhibitors but also occurs in treatment-naïve patients. The increased MET activity due to exon 14 skipping and MET amplification are both sensitive to MET inhibitors [12, 30].
-
RET rearrangement is rare in NSCLC with a frequency of 1–2% [14]. The RET fusion genes consist of the RET kinase domain and a dimerization domain provided by its partner gene. The dimerization confers constitutive RET kinase activity of the fusion protein [31]. Patients carrying RET fusion genes respond to multi-target tyrosine kinase inhibition; however, their clinical outcome is inferior to those with other oncogene-addicted NSCLC receiving selective TKIs [32].
-
BRAF mutations in lung adenocarcinoma include c.1799T > A; p.Val600Glu (V600E), and non-V600E mutations, with an approximate ratio of 1:1. V600E mutation occurs in 1.5–3.5% of lung adenocarcinoma; non-V600E mutations can either be activating or inactivating [13]. BRAF rearrangements in lung adenocarcinoma are rare [33]. A novel fusion SND1-BRAF has been reported in lung adenocarcinoma in non-smokers with increased phosphorylation levels of MEK/ERK and cell proliferation by in vitro study [34].
-
NTRK fusions in lung adenocarcinoma involve all three isoforms of NTRKs. NTRK1 rearrangements are present in approximately 3%; NTRK2 and NTRK3 rearrangements in less than 1% of lung adenocarcinomas [15, 35]. There is a great diversity of NTRK gene partners, which render constitutive kinase activity to the fusion proteins and sensitivity to TKIs [36]. MPRIP-NTRK1, CD74-NTRK1, and TMP53-NTRK2 are the relatively frequent fusions in lung adenocarcinoma [37].
-
HER2 mutations occur in exon 20 (insertion), the kinase, transmembrane, and extracellular domains; some of them may have concurrent HER2 amplification [18]. HER2-mutated lung cancers are sensitive to kinase inhibitors like dacomitinib [38] and afatinib [17], HER2 monoclonal antibody trastuzumab [16] and ado-trastuzumab emtansine, a HER2-targeted antibody-drug conjugate [18].
-
-
3.
What is the mutation landscape of squamous cell carcinoma of the lung?
-
Squamous cell carcinoma (SCC) has a strong association with tobacco smoking. Despite the relatively higher mutation burden, the typical tyrosine kinase gene mutations/aberrations seen in adenocarcinoma are rare in squamous cell carcinoma [39,40,41]. Mutations/aberrations detected in squamous cell lung carcinoma are similar to the squamous cell carcinoma from other organs, referred to as “squamousness” gene signatures [42, 43].
-
The most common genetic alterations in lung SCC occur in the cell cycle regulator genes, including deletion and loss of function mutations in TP53 (>75%) and CDKN2A/B (~70%) [39, 41]. TP53 mutation-associated signature is a significant prognostic biomarker and potentially predictive of response to immunotherapies [44].
-
Receptor tyrosine kinase (RTK) gene amplifications are present in >30% of lung SCC, with EGFR and FGFR1 being most common; however, mutations/fusions are rare [40, 45]. FGFR1 amplification is associated with better prognosis [46]. ERBB family mutations are seen in >20% of lung SCC; however, clinical responses to TKIs were not promising in the patients harboring these mutations, suggesting they are unlikely driver mutations [43].
-
RAS, MAPK, and PI3K signaling pathway dysregulation is another feature of SCC, most commonly loss of NF1, amplification or mutation of PIK3CA, and loss of PTEN. The potential value for targeted therapy of these alterations is under investigation [40].
-
Squamous cell carcinoma has been shown to have a higher tumor mutation burden (TMB) than adenocarcinoma [47]. In recent years, TMB has evolved as a novel biomarker to predict the sensitivity to immune-checkpoint inhibitors (see answers to question 15).
-
-
4.
When is mutation testing for squamous cell carcinoma indicated?
-
Given that there is no effective targeted therapy for lung SCC in routine clinical practice, mutation profiling is not recommended for well-defined squamous cell carcinoma by the current practice guidelines [48].
-
Approximately 0.4–4% of all lung carcinomas contain both adeno and squamous components under the light microscope, and the frequency is even higher based on the ultrastructural appearance [49, 50]. These tumors may be sensitive to targeted therapies if related mutations are present [48]. Therefore, if the specimens from lung cancer, such as a small biopsy or needle aspiration, are not representative of the whole tumor, or the morphologic and immunophenotypic features are not entirely characteristic of SCC and a definitive classification is challenging, pathologists should consider mutation testing of the sample (see example case 4).
-
The current expert consensus opinion is that oncologists or pathologists may consider molecular testing in tumors other than adenocarcinoma when the probability of a targetable oncogenic driver is high based on the clinical features of the patient, including young age (<50 years) and absence of tobacco exposure history [28, 48, 51].
-
Although routine clinical testing of TMB has not been standardized, TMB assessment together with mutation profiling with targeted panel next generation sequencing (NGS) is a hot topic for molecular testing of NSCLC, including SCC [52,53,54].
-
-
5.
What is the mutation landscape of small cell lung cancer?
-
Small cell carcinoma of the lung (SCLC) is a high-grade neuroendocrine tumor, possessing the worst prognosis among all lung carcinomas. There has not been any targeted therapy for SCLC so far. Recent genomic studies of SCLC reveal a complex genomic profile [55].
-
Both copy number gains and losses involving multiple chromosomes have been identified using array-based genomic analysis. Recurrent loss of 3p (FHIT and RASSF1), 17p (TP53), 13q (RB1), and 10q (PTEN) have been reported in multiple studies. The other commonly seen copy number gains/amplifications include 1p, 2p, and 8q harboring the MYC family genes [56,57,58,59,60,61,62,63].
-
SCLC has a high mutation rate partly attributed to exposure to tobacco carcinogens. Several pathways are involved in the mutations associated with SCLC. Deletion and/or loss of function mutations in RB1 and TP53 occur in >90% of the SCLC [63].
-
Alteration of telomere length is frequently detected in neuroendocrine carcinomas of the lung, greater in high grade forms (large cell neuroendocrine carcinoma and SCLC) [64]. TERT copy gain, together with RB1 deletion, was an independent predictor of poor prognosis in a study by Simbolo et al. [65].
-
Large cell neuroendocrine carcinoma (LCNEC) is another form of high-grade carcinoma of neuroendocrine origin. There are similarities in the gene expression profiles suggesting a common origin of LCNEC and SCLC [66], and their molecular profiles are significantly different from that of low grade neuroendocrine tumors [67]. Molecular genetic distinction between LCNEC and SCLC has also been reported [68, 69]. However, the inconsistency of these findings and the clinical significance of the differences warrant further study.
-
-
6.
Are there any clinically significant genetic alterations associated with other relatively uncommon lung cancer types?
-
Some of the other relatively uncommon lung cancer types included in the fourth edition of WHO Classification [2] are carcinosarcoma, pulmonary blastoma, NUT carcinoma, primary pulmonary lymphoepithelioma-like carcinoma (PLELC), and salivary-gland-type lung carcinomas.
-
Carcinosarcoma is an aggressive NSCLC that frequently contains a variety of components, with phenotypes ranging from adenocarcinoma, SCC, to different sarcomas. The mutation profiles corresponding to different components may be present in one tumor. Multiple studies have reported that TP53 mutations are frequently present, followed by KRAS mutation. Targetable mutations associated with adenocarcinoma, such as EGFR mutations and ALK rearrangement, are rarely detected, but ALK and EGFR amplification and overexpression are not uncommon [70,71,72,73,74,75,76,77]. One study found a high frequency of actionable MET mutations (8 of 36 cases tested) [78].
-
Pulmonary blastomas are frequently associated with missense mutations of CTNNB1 [79, 80], resulting in aberrant nuclear/cytoplasmic localization of beta-catenin protein and activation of the Wnt signaling pathway [81].
-
No clinically significant mutation profile has been discovered in PLELC so far. One study found low TMB in PLELC despite relatively high frequency of TP53 mutations [82].
-
Salivary-gland-type lung carcinomas arise from the submucosal glands of the airway, accounting for <1% of all lung tumors [83]. Histologically, they resemble their salivary gland counterpart, and most of them also share the same genetic alterations. Table 7.1 lists the major types of pulmonary salivary gland tumors and their associated genetic signatures.
-
NUT carcinomas carry the characteristic NUT rearrangement. The fusion partners are most commonly (70%) BRD4 resulting from t(15;19) [84, 85]. BRD3, BRD4, and NSD3 are other common gene partners of NUT [86]. The fusion protein causes epigenetic deregulation, resulting in loss of cell differentiation [87]. Detection of the NUT rearrangement in challenging cases provides evidence for a definitive diagnosis.
-
-
7.
What is the purpose of molecular genetic testing for lung cancer?
-
As a standard of care, the purpose of performing mutation profiling for lung cancer in routine clinical practice is to select patients for mutation-based targeted therapy. In patients who developed resistance to a targeted therapy, mutation profiling is an important approach to search for resistance mechanisms.
-
When multiple lesions are present, mutation profiling may provide useful information to evaluate the origin of the different lesions, the clonal diversity, and clonal evolution (see questions 10 and 11 below).
-
Detecting characteristic genetic alterations provide definitive or additional supporting evidence for the diagnosis and classification of some special types of carcinomas (see answers to question 6 above).
-
Beyond the standard of care recommended by the practice guidelines, molecular tests should also be considered when there is compelling evidence from clinical trial results that investigational targeted therapies are effective. TMB is considered a promising biomarker independent of PD-L1 immunostaining to select lung cancer patients for immunotherapies.
-
-
8.
What genes/mutations should be tested for non-small-cell lung cancer?
-
Genes with targetable mutations associated with non-squamous NSCLC are recommended by several published guidelines to be tested as the current standard of care [8, 48, 88]:
-
EGFR mutations, and ALK1 and ROS1 rearrangements must be tested as a separate single gene or panel test, for all lung adenocarcinoma patients. BRAF, MET, RET, KRAS, and HER2 testing should be included in a larger panel whenever appropriate, if there is sufficient sample available [48].
-
KRAS mutation single gene test can be performed separately because of the high prevalence and the mutual exclusivity of KRAS mutation with EGFR mutations and ALK fusions in NSCLC. If KRAS mutation is detected, larger panel testing for other mutations is not necessary. Currently, there is no compelling evidence to support single gene tests for BRAF, MET, RET, and HER2 [48].
-
The first-generation NTRK inhibitors, larotrectinib and entrectinib, were approved by the US Food and Drug Administration (US FDA) in 2017 for the treatment of any NTRK-fusion-positive cancers, including NSCLC [89]. When clinically indicated, testing for NTRK fusions in the absence of other driver alterations is recommended in the newer guidelines [8].
-
TMB testing to help selecting patients for immunotherapy [90], although not included in the guideline published in 2018 [48], may be considered for some patients with metastatic NSCLC [91].
-
Given the high prevalence of EGFR T790M mutation in acquired resistance to first- and second-generation EGFR TKIs, EGFR T790M must be tested in the setting of disease progression while on targeted therapy to select patients for third-generation TKIs [48].
-
Although mutations in the ALK1 gene may be associated with drug resistance, current evidence is not sufficient to support routine testing for ALK1 mutations.
-
TP53 is altered in >40% of NSCLC and >80% of lung SCC [92]. Most clinical studies suggest that NSCLC with TP53 alterations carry a worse prognosis and may be relatively more resistant to chemo- and radiation therapies [93]. Recently, TP53 co-mutations in EGFR- mutated NSCLC have also been associated with poor outcome of TKI therapy [94]. TP53 is usually included in the NGS panel for lung cancer mutation profiling to provide prognostic and predictive information.
-
-
There are many genes/mutations associated with NSCLC for which targeted or specific therapies are in development. Testing these genes/mutations may be considered in specific patient groups to provide information for clinical trial recruitment.
-
-
9.
When should a lung cancer sample be tested for mutation profile?
-
Lung cancer mutation testing/profiling is only required in patients presenting with advanced-stage (stage IV) or metastatic disease who are suitable for therapy, either at initial diagnosis or recurrent disease with progression, if not previously tested [8, 48, 88].
-
Molecular testing is encouraged for early-stage lung cancer [48]. Testing lung cancer samples from early-stage patients allows for obtaining molecular profiling results from high-quality resection specimen when it is readily available. These results are saved for the future in case the lung cancer progresses and it becomes necessary to have mutation profile results but it is difficult or unnecessary to obtain more sample. However, with the improvement of clinical management, a subset of early stage patients will be cured by surgical resection and/or chemoradiation therapy, thus, never needing the mutation profile. Each institution should set its own policy on testing patients with early-stage diseases.
-
Repeat testing on recurrent tumor or a blood sample (for circulating cell free tumor DNA) can be considered for patients who developed resistant or refractory disease to investigate the molecular basis of resistance and search for potential mutation targets to enroll the patients in clinical trials.
-
When a diagnosis is established and it is determined that molecular testing is necessary, tissue samples should be prioritized for molecular testing before exhaustion for other studies, especially when only cytology or limited biopsy samples are available. When the specimen size is small and additional studies are anticipated, it could be very helpful to cut multiple additional unstained sections upfront to avoid later refacing the tissue block for additional sections, which could result in significant loss of the limited tissue.
-
-
10.
When multiple lung cancer lesions and/or multiple metastatic tumors are identified and excised/biopsied in one patient, should each of them be tested for mutation profile separately?
-
There is no significant clonal diversity in a tumor that would cause sampling bias in the molecular testing of NSCLC [95, 96]. Furthermore, the mutation patterns remain quite stable in metastatic and recurrent tumors [95]. Therefore, primary or metastatic tumors are equally suitable for molecular testing [97]. It is not necessary to test different regions of one tumor for mutation profiles, and routine testing of metastatic or recurrent lesions of a known primary NSCLC is not recommended.
-
In patients with synchronous multifocal lung cancers, these lesions can be metastatic from one primary or concurrent multiple primary lung cancers [98, 99]. Distinguishing multiple synchronous primary from metastatic malignant masses is important for lung cancer staging and has significant treatment implications because the treatment protocols for metastatic late-stage lung cancer is substantially different from early-stage disease (see case 3 as an example).
-
Comparing the histomorphologic features of multiple tumors can be a powerful tool to determine whether they are metastatic late-stage cancer or multiple primaries. However, histologic features are not always reliable [100]. Furthermore, when a metastatic cancer is identified in a patient with a history of more than one cancer of the same histologic type (i.e., adenocarcinoma of different organ origin), it could be more challenging to determine the origin of the metastatic cancer based on histologic and even immunophenotypic features.
-
Molecular profile as definitive clonal evidence for a tumor sample has been used to study clonal diversity, clonal evolution, and intra-tumor heterogeneity [95,96,97, 101]. Combining histomorphologic and genotypic assessments is the ultimate approach to the accurate staging of lung cancer and defining the origin and evolution of a metastatic cancer [102, 103].
-
The decision of whether to test each of the tumors should be based on the clinical context of the patients, and the communications between pathologists and clinicians [88]. Recurrent tumors are recommended to be re-tested only when there are clinical indications, such as progression under targeted therapy suggesting acquired resistance, pathologic evidences suggesting clonal evolution, or a different tissue/organ origin.
-
-
11.
How are different types of genetic aberrations of lung cancer tested in the clinical diagnostic laboratories?
-
Many different molecular methods can be used to detect mutations and/or other genetic alterations in NSCLC. Because only a few genes/alterations (EGFR mutations, ALK1 and ROS1 translocations) are mandatory to be tested, single-gene or small panel tests are still widely performed in clinical diagnostic laboratories. After the first practice guideline published in 2013, some manufacturers have made commercial test kits focused on NSCLC mutations. The characteristics, advantages, and disadvantages of different methods used in molecular tests of NSCLC are summarized in Table 7.2.
-
Point mutations, either as single- or multi-nucleotide variants, frequently occur in EGFR, KRAS, BRAF, HER2, and many other genes and are detectable by almost any molecular testing methods, if designed appropriately. Mutant-allele-specific polymerase chain reaction (PCR) needs special primer design to detect multinucleotide variants (MNVs); the commercially available allele-specific primers or probes are usually not designed for the multinucleotide changes. For example, allele-specific PCR designed for BRAF c.1799T > A; p.V600E would not accurately detect less commonly seen c.1798_1799delinsAA; p.V600K or c.1798_1799delinsAG; p.V600R mutations. Droplet digital PCR method is a variant form of PCR that markedly increases the analytic sensitivity and quantitation accuracy. It is particularly useful when the sample contains a low percentage of tumor or mutant DNA, such as circulating cell-free DNA (cfDNA) extracted from blood (liquid biopsy).
-
Small insertions and deletions (indels) frequently occur in mutant EGFR (exon 19 deletion, exon 20 insertion) and HER2 (exon 20 insertion). Although a well-designed PCR method may detect most of the indels, relatively uncommon ones that have the same pathologic effect are usually not covered. A fragment size analysis or sequencing based method is preferred; the latter could provide detailed information of the nucleotide changes.
-
Fusions genes resulting from chromosome rearrangements (ALK1, ROS1, RET, NTRK, rarely BRAF and FGFR) are detectable by fluorescence in situ hybridization (FISH) with excellent sensitivity and specificity, if the probes are designed appropriately (see case 5 as an example). Because these fusion genes are all transcribed to mRNA with fusion protein expression, mRNA-based reverse transcription (RT) PCR is also an excellent detection method, providing better analytic sensitivity than FISH. However, RT-PCR may not cover all the translocation variants because rare or novel variants are usually not included in the primer design.
-
Targetable gene amplifications in lung cancer occur in MET, HER2, and FGFR. The detection of gene amplification is challenging by PCR or sequencing methods. FISH with a chromosome enumeration probe (CEP) as internal control is a sensitive and specific method to detect gene amplification. For example, MET amplification is defined as a MET/CEP7 (chromosome 7 enumeration probe) ratio >2.2. The probe design for specific genes is required, and a standardized cutoff threshold is critical to define an amplification. A copy number array analysis can sensitively detect gene amplification at the whole-genome level, but it is too costly to be routinely performed; only selected patients may be indicated.
-
More frequent than amplification, targetable alterations of MET include mutations at the RNA splice site or intronic region resulting in exon 14 skipping. Although many mutations have been confirmed resulting in exon 14 skipping, testing at the DNA level is challenging to recognize all the mutations to that effect [104]. Only an mRNA-based test (RT-PCR or RNA sequencing) could provide definitive evidence by amplifying the abnormally spliced mRNA with shorter length [105] (see case 6).
-
Although it is easier to implement FDA-approved in vitro diagnostic (IVD) tests [106], the laboratory directors need to have a full understanding of the detection range of the PCR-based tests to know whether additional testing would be required if the results from the IVD tests are negative.
-
Given the complexity and variable prevalence of the targetable genetic changes associated with NSCLC, there are different ways to approach the molecular testing in a clinical diagnostic laboratory [107]. It might be worthwhile for molecular diagnostic laboratories to establish a cost-effective test triaging an algorithm based on local resources and clinical requirements. Potentially practical algorithms include (1) test KRAS first, if any mutation identified, no other tests are indicated; (2) test EGFR first, if no mutation detected, reflex to ALK1, ROS1 translocation, and/or KRAS mutation test, or a panel test to include more alterations. (3) start with a small panel to cover the most relevant genes, such as EGFR mutation and ALK1 and ROS1 translocations; if the results are all negative, then consider testing uncommon and investigational mutations with an expanded panel in a subgroup of patients as clinically indicated. In the future, most clinical laboratories will likely implement extensive large-panel NGS to cover all the mutations associated with NSCLC.
-
Laboratories performing mutation tests for NSCLC should have a plan for reflex testing in case any sample fails the first test or the quality/quantity not sufficient to complete the routine tests. In our institution, we perform a small panel (26 genes) NGS for SNVs/MNVs and small indels, together with a FISH panel including ALK1, ROS1, RET translocations, and MET amplification. If a sample fails to qualify for the NGS test, it is reflexed to a SNaPshot panel for the hotspot mutations of 10 genes including EGFR, KRAS, and BRAF, together with a fragment size analysis for EGFR exon 19 deletion, exon 20 insertion, as well as HER2 exon 20 insertion. This approach allows us to obtain the mutation profile of all the clinically significant alterations from almost any sample, small or large.
-
In addition to molecular tests, immunohistochemical staining (IHC) for ALK1 is considered as equivalent to FISH for ALK fusions; however, only the D5F3 antibody from Ventana has been approved by the FDA for patient selection for crizotinib treatment [106]. IHC can be used as a screening test for ROS1 translocation; positive results must be confirmed by FISH [48]. BRAF V600E mutation can be screened by IHC with VE1 antibody; however, the performance characteristics need to be determined by the individual laboratory; and this antibody cannot detect BRAF non-V600E mutations. Due to the low prevalence of HER2 amplification, the immunohistochemical stain of HER2 is not useful in predicting the treatment response of inhibitors or antibodies. IHC has no value in detecting EGFR mutations.
-
-
12.
What are the benefits and challenges of using next-generation sequencing (NGS)-based tests for non-small-cell lung cancer?
-
If designed appropriately, one NGS test can cover multiple genes, various types of mutations/aberrations, including point mutations, deletions, insertions, and copy number variants. Sequencing libraries built from tumor RNA can be loaded together with that from DNA to identify fusion genes and assess gene expression levels. TMB, a potential biomarker for immunotherapy, can also be calculated based on the data from a large-panel NGS (see question 15).
-
Other advantages of NGS include low input of genetic materials, high sensitivity, and low cost per gene. When multiple gene targets are tested for lung cancer, an NGS panel is more cost effective over multiple single-gene tests [107]. The high analytic sensitivity of deep sequencing coupled with molecular barcoding (unique molecular identifier, UMI) provides an ideal method to detect low-frequency mutant alleles, making it suitable for circulating tumor DNA (ctDNA) testing using blood samples (see answers to question 14 below).
-
Because detecting ALK1 and ROS1 fusions are clinically required, designing a cost effective small NGS panel to cover all the clinically significant NSCLC alterations is challenging. The targeted panel NGS test can also be challenging in detecting large indels and copy number changes due to problematic alignment algorithms of bioinformatic pipelines for large indels, and the limited, sometimes biased, data available to calculate a normalized diploid level.
-
NGS panels, especially the large ones, generate a large amount of data. The post-sequencing analysis, variant interpretation, and data storage are current challenges for NGS tests. Furthermore, reporting many variants of uncertain significance (VUS) from a large panel may dilute the significance of clinically relevant mutations. Therefore, for the clinical mutation profiling of lung cancer, despite the increasing demand for larger panels from oncologists and patients, each molecular diagnostic laboratory needs to balance the panel size with the cost, turnaround time, and clinical relevance.
-
-
13.
What are the specimen types acceptable for mutation profiling of lung cancer?
-
Formalin-fixed, paraffin-embedded (FFPE) tissues or cell blocks are widely validated for FISH and molecular testing of NSCLC. The unstained FFPE sections for molecular tests should be unbaked. The routine 5- to 10-μm thick sections are used, and the number of sections depends on the size of the tumor and the test to be performed. In general, five 5-μm thick sections should be enough for non-sequencing assays, and ten 5-μm sections may be preferable for NGS.
-
Fresh, frozen, or alcohol-fixed specimens are all acceptable for molecular tests; fresh or frozen specimens producing high-quality RNA are particularly good for RNA-based tests. However, each tissue type needs to be validated separately. Tissue samples treated with other methods such as acidic or heavy metal fixatives, or decalcifying solutions, should be avoided due to high false-negative rate [108,109,110].
-
Cytologic specimens including liquid-based cytology and fresh cell suspension, direct smear, and stained cytology slides can also be used for FISH and molecular tests. For cytology slides, Quick-diff is preferred than the Papanicolaou stain because DNA in the latter degrades faster [111].
-
Cellular fluids sampled from body cavities involved by metastatic tumors are usually sufficient for diagnostic evaluation, including molecular genetic testing. Peripheral blood, spinal fluid, and urine may be used to extract cfDNA for the assessment of therapy response and drug resistance in certain clinical circumstances.
-
Regardless which tissue/sample type is used for FISH or molecular tests, the tumor content (the percentage of malignant cell nuclei) should be determined by a pathologist examining the corresponding cytology smear or H&E slides. A training and feedback program for pathologists evaluating the tumor cell content can significantly improve the skill and accuracy of estimation [112]. The analytic sensitivity (lower limit of detection, LLOD) of each test is method dependent. The current guidelines strongly encourage laboratories to implement tests that can detect mutations in specimens with as low as 10% cancer cells (5% mutant allele frequency) [48]. Circling the tumor-rich area on an H&E slide for macrodissection should be routinely performed to increase the tumor cell percentage and improve test accuracy, especially when the overall tumor cell percentage is low [113].
-
-
14.
What is the role of cell-free DNA testing (liquid biopsy) for lung cancer?
-
Detecting cancer-related mutations from the circulating tumor DNA (ctDNA) shed into blood by apoptotic or necrotic tumor cells is referred to as “liquid biopsy. ” Testing cfDNA from other body fluids can also be performed with the same methods [114]. As a minimally invasive procedure, liquid biopsy has quickly gained popularity among oncologists for NSCLC and other solid tumors.
-
Given the low concentration of cfDNA and variable fraction of ctDNA, a method with high analytic sensitivity is required for cfDNA-based cancer mutation detection. Currently most laboratories use droplet digital PCR or deep sequencing (NGS with high read depth) for cfDNA tests. The test protocols are challenging to validate and costly for each sample.
-
Studies have found excellent concordance and specificity (83.3–99.0%) of the mutation profiles detected from plasma compared with that from tissue samples. The clinical sensitivity of liquid biopsy ranges from 50% to 80% for guideline-recommended NSCLC biomarkers [48, 115,116,117,118].
-
It is assumed that mutations detected in ctDNA better reflect the heterogeneity of the tumors; therefore, mutation profiling with liquid biopsy could provide a more complete picture than testing tissue sampled from a single tumor region. On the other hand, the heterogeneous origin of ctDNA can complicate the result interpretation. A patient with lung cancer may have concurrent primary cancers in another organs; assigning a cfDNA mutation profile to lung cancer requires a complete evaluation of the patient to rule out other potential primary lesions.
-
Currently, there is not enough evidence to support the use of cfDNA molecular tests for the screening and diagnosis of primary lung adenocarcinoma. When there is already a diagnosis of NSCLC but the tissue sample is insufficient for molecular testing, cfDNA assay is an option to identify targetable mutations [48].
-
When there is a need to identify the acquired resistant mutations, especially when it is clinically unfeasible to perform invasive procedures for tissue sampling due to comorbidities and/or other contraindications, a rebiopsy can be avoided if the cfDNA test is positive. Otherwise tumor sample testing should still be pursued due to the lower clinical sensitivity of cfDNA testing [48].
-
Serial sampling to monitor the mutation evolution using cfDNA, which is much easier than repeat tissue biopsies, could reveal critical information to recognize the heterogeneous molecular basis of EGFR TKI [119, 120] or ALK inhibitor resistance [121, 122], especially when acquired EGFR T790M mutation decreases with the expanded use of third-generation EGFR TKIs [123].
-
-
15.
What is the clinical significance of tumor mutation burden (TMB) in lung cancer and how is it tested?
-
Tumor mutational burden (TMB) is a measurement of the total number of somatic mutations in the genome of tumor cells. It was originally defined as the number of nonsynonymous mutations per genome or per million base pairs (mut/Mb) calculated from the whole-genome (WGS) or whole-exon sequencing (WES) data [124]. The level of TMB is significantly variable across tumor types. NSCLC (both adenocarcinoma and squamous cell carcinoma) and SCLC have high average mutation burdens following melanoma [125, 126]. It is reasonably assumed that TMB can be a proxy for the number of neoantigens that is associated with the strength of immune response triggered by tumor cells.
-
Multiple studies have shown that high TMB is associated with better responses to immune checkpoint inhibitors (ICIs) in NSCLC, independent of the expression levels of PD-L1 [47, 90, 127, 128]. TMB is, thereby, recognized as a powerful biomarker to select patients for ICI therapy although there are still some controversial results by other studies [129, 130].
-
The gold standard for TMB was established from the data analysis of simultaneous WES of tumor and matched blood or normal tissue, in which only somatic nonsynonymous variants were included in the calculation. Recent studies demonstrated that data from NGS of a targeted panel with >300 genes could generate TMB results comparable to those calculated from WES [131,132,133].
-
Multiple factors can affect the accurate assessment and interpretation of TMB [134]:
Preanalytical factors:
-
FFPE tissue is most frequently used for NGS testing. Tissue quality and processing can significantly affect the level of artifacts, especially false-positive variants from nucleotide modifications.
-
Tumor cell content and background tumor environment also affect the test results. Because a targeted panel sequencing can achieve higher sequencing depth than a WES, it is presumably more suitable for samples with lower tumor content that cannot be enriched (e.g., cytology cell block with relatively scattered tumor cells/clusters). However, this assumption has yet to be confirmed in clinical studies.
-
Multiple studies have confirmed that TMB from plasma ctDNA correlates well with that from tissue samples (bTMB vs. tTMB [115, 135, 136]). If the value of bTMB is confirmed by correlating with clinical outcomes of immunotherapy, the utility of liquid biopsy could be largely expanded (see more discussion in question 14).
Analytical factors:
-
The methods to calculate TMB and the cutoff value of high TMB need to be adjusted and validated based on the sequencing data from different platforms.
-
To increase the accuracy of TMB measurement from targeted panel sequencing that generates less nonsynonymous variants, it is proposed to include synonymous variants and indels, which may render a better correlation with the TMB calculated from WES results.
-
When a tumor sample is sequenced without paired normal tissue or blood sample, the germline variants can only be filtered through bioinformatic analysis using germline variant databases. Not all germline variants can be recognized this way; therefore, the TMB is likely overestimated.
Postanalytical factors:
-
The procedure of interpreting and reporting TMB results have not been standardized, especially when the data from a targeted panel NGS is used.
-
Currently there is no consensus cutoff value to define a high TMB. Although 10 mut/Mb is used as the threshold in the FDA approval of pembrolizumab for adults and children with TMB-H solid tumors [137], many WES-based studies reported TMB as total mutations per tumor. It is yet to be determined whether lung adenocarcinoma, SCC, and SCLC need different TMB cutoff values to guide immunotherapy decisions.
-
Before a consensus guideline is available for TMB reporting, the TMB Harmonization Consortium recommended that TMB be reported as mut/Mb [138]. The types of mutations included in the TMB calculation, the cutoff value, and the rationale to establish the cutoff should also be included in the report [139].
-
-
-
16.
What other tests can be considered to provide guidance for immunotherapy of lung cancer?
-
Assessment of PD-L1 expression by IHC is widely accepted as a useful marker to select NSCLC patients for immunotherapy with ICIs [140], although there are no standardized method and interpretation guideline, and the predictive value is questioned in some studies [141]. In addition to the TMB test discussed above, a combination of multiple biomarkers may provide a better prediction of ICI response in NSCLC patients.
-
The mutation profiling routinely performed in most clinical laboratories for lung cancer has predictive value for ICI therapy. EGFR mutation, ALK1, or ROS1 translocation-positive NSCLC usually responds poorly to ICIs even when the tumor expresses a high level of PD-L1 [142]. TP53-mutated, but STK11 and EGFR wild-type NSCLCs are associated with longer disease-free survival (DFS) in ICI-treated patients [143].
-
The evolution of ctDNA level in plasma defined by changes of the mutant allele frequency, regardless of specific mutations, may predict ICI response. Low ctDNA at the first evaluation after nivolumab treatment was associated with better clinical response, progression-free survival (PFS), and overall survival in a recent study [144]. The ctDNA level may become an early predictor of a durable good response to nivolumab [145].
-
While most studies on the efficacy of immunotherapy focus on the potential neoantigens created from genetic alterations of the malignant cells (the target), investigating the T-cells (the effector) mediating the killing of tumor cells have also provided information potentially valuable to independently predict responses to immunotherapy [146,147,148]. More clinical studies are required to confirm the validity of these results.
-
Case Presentations
The clinical histories of these cases are slightly modified to simplify the presentation and avoid the potential association of any protected patient information.
Case 1
Learning Objectives
-
To understand the NGS test result of EGFR exon 19 deletion
-
To discuss the nomenclature of complex variants detected by NGS
Case History
A 60-year-old female with a smoking history 30 years ago has a right upper lobe lung mass found at a routine clinic visit. A computerized tomography (CT) scan confirms a 3.7 × 2.4 cm single lesion. A core biopsy is performed and reveals lung adenocarcinoma. The mass is excised by a robotic right upper lobectomy with additional lymphadenectomy. Figure 7.1a, b show the histomorphologic findings are characteristic of invasive adenocarcinoma, acinar predominant; there is also in situ nonmucinous adenocarcinoma with a lepidic component shown in (b). Metastasis tumor is found in one ipsilateral lymph node.
Adenocarcinoma with EGFR exon 19 deletion. (a) and (b) Representative histomorphology images of the lobectomy specimen (H&E stain, A. 100X, B. 200X). (c) Screenshot of the NGS result displayed in the Integrative Genomics Viewer (IGV, Broad Institute) showing the EGFR exon 19 region. The NGS protocol leverages two separate libraries built from either strand of a DNA fragment (displayed on the upper and lower panel of image C, Library 1 and 2). The horizontal bars represent the sequencing reads, with purple and pink colors indicating read directions. The chromosome coordinates indicated in the image are based on the reference assembly hg19, GRCh37. The reference DNA sequence and corresponding amino acids are displayed on the bottom. A 15-base-pair deletion and a C > T single nucleotide variant (SNV) are seen on the same sequencing reads in both libraries and both read directions. As displayed on the yellow box, the total variant frequency is 9% in this result with a total read depth of 53,135
Pathological Diagnosis
Adenocarcinoma, acinar predominant (acinar 55%, micropapillary 40%, papillary 5%), moderately to poorly differentiated
Maximum tumor diameter: 3.6 cm. The adenocarcinoma is staged IIB (T2a N1 M0)
Molecular Genetic Study
A 26-gene NGS test is performed on the lobectomy specimen. Tumor content is enriched by macrodissection. The only clinically significant alteration detected is shown in Fig. 7.1c. This is a complex sequence variant in exon 19 of EGFR, with a 15-base-pair deletion (codon 746 glutamic acid to 750 alanine) and a C to T variant at codon 751 Threonine. Based on the original data displayed in the image, the inframe deletion is on the same allele with the single nucleotide variant (cis mutations). It would not be entirely wrong to report the two variants separately as “EGFR E746_A750del (c.2236_2250del)” and “EGFR T751I (c.2252C > T)”; in fact, if the original alignment reveals the two variants are on different alleles (trans mutations), they must be reported separately. However, it is more appropriate to combine them as one mutation in the nomenclature to reflect that the complex variants are on the same allele:
-
EGFR (NM_005228.3) c.2236_2252delinsAT (p.E746_T751delinsI) in approximately 9% of alleles
Chromosome coordinates: chr7:55242466-55242482: GAATTAAGAGAAGCAAC > AT
Clinical Follow-Up
The patient receives adjuvant chemotherapy after surgery. No new or enlarging suspicious pulmonary nodules detected by follow-up CT scan 9 months later.
Discussion
Approximately half of the EGFR mutations in NSCLC are inframe exon 19 deletions, such as the mutation detected in this patient. These deletions result in increased kinase activity of EGFR, lead to hyperactivation of downstream proliferation and pro-survival signaling pathways, and conferred increased sensitivity to EGFR tyrosine kinase inhibitor treatment.
As discussed above, the EGFR exon 19 inframe deletion in this case is complicated by an additional single-nucleotide variant. This specific variant is a known oncogenic variant described in TKI-responsive lung adenocarcinomas [149] and appears to be very similar to the well-characterized EGFR p.E746_A750del variant that confers TKI sensitivity in NSCLC.
The NGS result of this case signifies the importance for the molecular pathologists to review the original alignment data to generate an accurate mutation report.
Case 2
Learning Objective
The EGFR T790M mutation is the most common mechanism of acquired resistance after EGRF TKI-targeted therapy.
Case History
A 69-year-old male was diagnosed with bilateral metastatic adenocarcinoma of the lung with activating EGFR L858R mutation. He received targeted therapy using the first-generation TKI, erlotinib. Although he has no symptoms, based on imaging study results, the disease has slowly progressed in 2 years. A blood cfDNA test (liquid biopsy, performed by Guardant360® CDx) reported negative results; the original EGFR L858R mutation was not detected either. A biopsy of the right upper lobe lung lesion is performed.
Pathological Diagnosis
Before treatment (right lung transbronchial biopsy):
-
Adenocarcinoma, non-mucinous with predominantly a lepidic growth pattern, intermediate nuclear grade
After 2 years of erlotinib treatment (right upper lobe, transbronchial biopsy):
-
Adenocarcinoma, acinar-type growth pattern
Representative histomorphologic images of the two biopsies are shown in Fig. 7.2.
Molecular Genetic Studies
A 26-gene NGS test is performed on both biopsies.
Before treatment, two mutations detected:
-
EGFR (NM_005228.3) c.2573T > G (p.Leu858Arg), 15% of alleles
-
TP53 (NM_000546.5) c.742C > T (p.Arg248Trp), 22% of alleles
After treatment, two new mutations detected:
-
CTNNB1 (NM_001098210.1) c.95A > C (p.Asp32Ala) 10% of alleles
-
EGFR (NM_005228.3) c.2369C > T (p.Thr790Met), 9% of alleles; and c.2573T > G (p.Leu858Arg), 26% of alleles
-
TP53 (NM_000546.5) c.742C > T (p.Arg248Trp) 19% of alleles
Clinical Follow-Up
Erlotinib is discontinued after the second biopsy reported T790M mutation; treatment with third-generation EGFR inhibitor, osimertinib starts. Eight-weeks later, restaging CT scan shows about 50% size reduction in right upper lobe tumor and size reduction in scattered lung nodules. However, follow-up imaging scans 3 years later show the disease is still slowly progressing.
Discussion
Resistance to first- and second-generation EGFR TKIs can be either on-target that includes acquired EGFR resistance mutations or EGFR amplification or off-target that includes activation of non-EGFR pathways, lineage transformation, etc. EGFR T790M mutation is the most common on-target mechanism for the resistance of first- and second-generation EGFR TKIs. Molecular testing of T790M mutation is recommended for patients with disease progression while on EGFR TKI therapy, like in this case. Although liquid biopsy provides a minimally invasive way to detect additional mutations in these patients, the clinical sensitivity is relatively low. When a liquid biopsy result is negative, lesional tissue biopsy should be attempted. In this case, because the EGFR L858R mutation reported in the original biopsy sample was not detected by liquid biopsy, the negative result is problematic, and additional mutations are confirmed by follow-up tissue biopsy.
An additional CTNNB1 p.Asp32Ala mutation is detected at the same allele frequency as EGFR T790M, further confirming the clonal evolution. It is not clear whether the CTNNB1 and TP53 mutations are associated with the patient’s unsatisfactory response to the third-generation TKI therapy.
Case 3
Learning Objectives
-
Synchronous multifocal lung cancers can be metastatic from one primary, or concurrent multiple primary lung cancers.
-
Molecular profiling provides definitive clonal information for tumor samples. Combining histomorphologic and genotypic assessment is the ultimate approach to an accurate staging of lung cancer with multiple masses.
Case History
A 73-year-old female had a history of left breast cancer 20 years ago. A CT scan shows bilateral lung nodules. Three nodules located in the right lower lobe, middle lobe, and upper lobe are resected.
Pathologic Diagnosis
Right lower lobe (A):
-
Adenocarcinoma, acinar type with lepidic pattern, maximum diameter 1.7 cm
-
A separate nodule is consistent with metastatic carcinoma from breast (positively for GATA3 and mammaglobin; negative for TTF-1 and napsin)
Right middle lobe (B): Metastatic carcinoma from breast (based on morphology and IHC stains)
Right upper lobe (C):
-
Adenocarcinoma, lepidic type (tumor size: 3.2 cm based on a CT scan report)
The histomorphologic features of the lung adenocarcinoma from block A2 and C1 are displayed in Fig. 7.3.
Histomorphology of the adenocarcinomas from two different locations. (a) Photo taken directly on the glass slide of A2 (right lower lobe) and C1 (right upper lobe). These nodules have all been confirmed to be lung origin, not metastatic breast cancer, by IHC stains. Although three nodules are seen on slide A2, they partially merge with each other under microscopic observation. These nodules were not separated when preparing for the NGS test. (b–e) Microscopic images, H&E stain, 40X. (b) Lesion from C1; (c, d, e) Three nodules from A2. These lesions show similar histomorphologic features of adenocarcinoma. It is unable to determine whether they are independent primary adenocarcinomas or metastasis from one primary
Molecular Genetic Studies
Only the lung cancer components (A2 and C1) are submitted for the 26-gene NGS test. The sequence variants detected are:
Right lower lobe (A2):
-
KRAS (NM_033360) c.34G > T (p.G12C), 28% of alleles
-
APC (NM_000038) c.3386T > C (p.L1129S), 46% of alleles
Right upper lobe (C1):
-
MET (NM_001127500) c.3081_3082 + 2delAGGT (p.E1027fs), 14% of alleles; this deletion spans both exons and introns, most likely resulting in exon 14 skipping
-
APC c.3386T > C (p.L1129S), 49% of alleles.
The two lesions are staged as separate primary tumors based on the molecular profiling results:
-
Lower lobe stage: pT1b (1–2 cm)
-
Upper lobe stage: pT2a: (3–4 cm)
Discussion
Multiple synchronous lung nodules are present in approximately 20% of the lung cancer cases [98, 99]. Determining whether they are independent primary tumors or intrapulmonary metastasis is crucial for the correct pathological staging and prognosis evaluation. Historically, the determination solely relied on histomorphologic features. Genetic studies can provide definitive evidence to determine the clonal relationship of different nodules. This patient presents with two separate lung adenocarcinomas at different lobes of the right lung, and the two tumor nodules share similar morphology. If one is primary and the other is metastasis, the stage will be pT4. In this case, the different driver mutations indicate they are two independent primary tumors; thus they are staged separately as pT1b and pT2a. Of note, the patient also has metastatic breast cancer nodules in the lung that are easily recognized by the different immunostaining patterns. If a metastatic cancer shows similar morphologic and immunostaining features with the primary lung cancer, it will be even more challenging to determine their origin without clonal evidence. A same APC sequence variant is detected in different primary lesions with an allele frequency close to 50%, suggesting this is most likely a germline variant. The APC p.L1129S is found in 0.10–0.24% of the general population (rs143638171). As a germline variant, it is considered benign or likely benign by contributors to NCBI’s ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/RCV000077988/). However, this variant is usually not filtered out as a benign germline variant due to its low prevalence in the general population. This kind of variant of uncertain clinical significance (VUS) is frequently encountered in cancer mutation profiling.
Case 4
Learning Objectives
-
A small subset of lung carcinomas contains both adeno and squamous components. Not all the different components can be sampled in a small biopsy.
-
Even if only squamous cell carcinoma is present in a core biopsy, it may be considered for molecular testing when there is a possibility of unsampled adenocarcinoma based on the clinical history or clues from histomorphologic features.
Case History
A 55-year-old female has a left femoral pathologic fracture . She was diagnosed with lung adenocarcinoma 2 years ago and treated with osimertinib based on the molecular test findings. A total hip arthroplasty is performed, and the bone specimen is received for pathology examination.
Pathological Diagnosis
Right lower lobe lung biopsy (from 2 years ago):
-
Adenocarcinoma, lung primary
Left femoral neck resection:
-
Metastatic keratinizing squamous cell carcinoma
The histomorphology images of both the lung and bone lesions are shown in Fig. 7.4.
Molecular Genetic Studies
A 26-gene panel NGS test performed on both specimens identifies the same mutation profiles (displayed in Figs. 7.5 and 7.6).
Screenshots of the NGS results displayed in IGV. The screenshots demonstrate that the same sequence variants are present in both (a) primary lung cancer and (b) metastatic bone lesion. The NGS protocol is the same as described in Fig. 7.1. Figure 7.5 EGFR exon 19 deletion; Fig. 7.6 APC c.3479 C > A (p.T1160K). More detailed information about the variant reads is displayed in the yellow box
Lung mass:
-
EGFR (NM_005228.3) c.2235_2249del (p.E746_A750del), 53% of alleles
-
APC (NM_000038.5) c.3479C > A (p.T1160K), 58% of alleles
Bone (left femoral neck):
-
EGFR (NM_005228.3) c.2235_2249del (p.E746_A750del), 48% of alleles
-
APC (NM_000038.5) c.3479C > A (p.T1160K), 63% of alleles
Discussion
The histologic feature of the metastatic bone lesion is diagnostic of keratinizing squamous cell carcinoma, making it difficult to determine its primary origin. Mutation profiling with NGS identifies the lung and bone lesions share the same mutations, including the driver mutation EGFR exon 19 deletion, indicating the bone lesion is a metastasis of the NSCLC. In that regard, the results of molecular testing are useful in determining the origin of the metastatic tumor, especially when the morphologic features are different.
More importantly, this case demonstrates that various components may be present or derived from an NSCLC. We can reasonably hypothesize that a squamous cell carcinoma component was present in the primary lung cancer but not sampled in the biopsy.
Re-biopsy sampling for molecular test is indicated in patients whose lung cancer progresses or metastasizes to other locations while on targeted therapy to identify possible loss of actionable EGFR mutations or acquisition of resistant mutations, such as EGFR C797S, L718Q, G724S, and S768I. In this case, no other EGFR mutations were detected in the metastatic carcinoma in the bone.
Case 5
Learning Objectives
-
To understand the FISH method detecting chromosome rearrangements that result in fusion genes
-
To recognize the variant signal pattern of ALK1 break apart FISH result
Case History
A 69-year-old male, non-smoker, is referred to ophthalmology for two right choroidal lesions. He is treated with steroids, but the lesions grew. Metastatic cancer is suspected, and a positron emission tomography (PET) scan shows a non-FDG avid nodule in the right lower lung lobe measuring 2.6 × 2.4 cm and a subcarinal lymph node measuring 1.9 × 2.0 cm with FDG 3.8. Fine needle aspiration of the subcarinal lymph node is performed.
Pathologic Diagnosis
The cytology smear and cell block show malignant cells (Fig. 7.7); immunostains performed on the cell block sections reveal the malignant cells are positive for TTF1 and napsin, consistent with metastatic adenocarcinoma from lung primary.
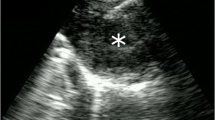
FISH Analysis
-
POSITIVE for variant ALK1 gene rearrangement with loss of 5′ ALK in 81% of the 200 cells scored (Fig. 7.8)
Fluorescence in situ hybridization (FISH) of ALK1 rearrangement. Dual-color break-apart probes show 1 fusion (red + green/yellow, the red part is smaller in many cells) and 1–2 red signals, indicating loss of 5′ (green) signal. Although rearrangement typically shows split of green and red signals, loss of 5′ green signal is a variant pattern indicating rearranged ALK1 gene
Discussion
Although ALK1 rearrangements are present only infrequently in NSCLC, they are targetable alterations required to be tested per current practice guidelines. FISH is a sensitive and specific method to detect ALK rearrangements (and other rearrangements such as ROS1 and RET). To cover variable partners of ALK1 fusion, a break apart-probe design is preferred in the clinical FISH laboratory because the specific partner does not affect the therapy response. In the fusion protein, only the ALK kinase portion is functionally relevant; therefore a variant rearrangement with loss of 5′ signal and retention of the 3′ kinase portion, like in this case, is considered positive for ALK1 fusion.
EML4 is the most common gene partner of ALK1; both genes are located in the short (p) arm of chromosome 2. Segment inversion of chromosome 2p results in the constitutively active ALK-EML4 fusion protein. AlK1 can also fuse with other genes, such as TFG, KIF5B, KLC1, etc. In this case, an ALK-EML4 fusion gene has been confirmed in a later liquid biopsy test.
Case 6
Learning Objective
-
Splice site mutation caused MET exon 14 skipping can be recognized at the DNA level in many cases.
-
Definitive diagnosis of MET exon 14 skipping may require confirmatory tests at the RNA level.
Case History
A 70-year-old male is found to have a right upper lobe lung nodule (1.1 × 1.0 cm) and a subpleural left lung nodule (0.7 × 0.7 cm) in the CT scan during the work-up for his bladder cancer. A right upper lobe wedge resection is performed.
Pathologic Diagnosis
-
Pulmonary adeno-squamous carcinoma (1.1 × 1.0 × 1.0 cm)
The histomorphology of this case and a control case is shown in Fig. 7.9a, d.
Molecular Genetic Studies
The 26-gene panel NGS test is performed on the sample after enrichment of tumor cells by macrodissection. A right upper lobe nodule biopsied from an 88-year-old female is used as a control for this case; the same molecular test is also performed on the control case.
The following mutation is detected in the patient sample:
-
MET (NM_001127500) c.3082 + 1G > C, 16% of alleles, at chromosome 7: 116412044
The splice site mutation is likely to cause exon 14 skipping. A different single-nucleotide mutation is detected in the control case: MET c.3061T > C (p.Y1021H), 28.39% at Chromosome 7: 116412022. This variant should not affect RNA splicing, and the mRNA length should be the same as wild-type mRNA.
The NGS results are displayed in Fig. 7.9b, e.
Adenocarcinoma with MET exon 14 skipping mutation. This case (d–f) is illustrated in comparison to an adenocarcinoma with MET missense mutation (a–c). (a) and (d) Representative microscopic images, H&E stain, 100X. (b) and (e) IGV screenshots of NGS result. The NGS protocol is the same as described in Fig. 7.1. Displayed are the 3′ region of MET exon 14 and the 5′-region of intron 14–15. Of note, the MET c.3061 T > C (p.Y1021H) in the control case has only one read direction due to the limited read length, but both libraries 1 and 2 reveal the same variant (b). The MET exon 14 skipping is confirmed by a reverse transcription polymerase chain reaction (RT-PCR); ABL gene is used as the internal control for RT-PCR amplification. (c and f) PCR amplicons revealed by Qiaxcel® (Qiagen) capillary gel electrophoresis. A shorter amplicon is detected in the exon 14 skipping sample (166 bp in f vs. 281 bp in c). The expected ABL control amplicons (111/116 bp) are present in both cases
RT-PCR amplification of the MET region flanking exon 14 is performed. ABL1 Transcript serves as the amplification internal control. The results are deployed in Fig. 7.9c, f. The amplicon size from this patient (166 bp) is shorter than that from the control patient (281 bp, expected normal mRNA length).
Discussion
MET exon 14 skipping is a driver mutation in NSCLCs, and the absence of exon 14 leads to decreased MET protein degradation and increased kinase activity. RNA splicing requires a donor site (5′ end of the intron), a branch site (near the 3′ end of the intron), and an acceptor site (3′ end of the intron). Mutations in these regions result in splicing error, leading to loss of exons or retraining of intron sequence. In this case, a G > C mutated splice donor site causes exon 14 skipping.
Although most mutations affecting RNA splicing can be identified by DNA sequencing and many have been confirmed by testing the mRNA, not all mutations causing MET exon 14 skipping are recognizable at the DNA level. A confirmatory RNA testing may be required if targeting MET active mutation is clinically indicated.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30.
Travis WD, et al. World Health Organization classification of tumours. In: Bosman FT, et al., editors. WHO classification of tumours of the lung, pleura, thymus and heart. 4th ed. Lyon: International Agency for Research on Cancer (IARC); 2015. p. 412.
Fong KM, et al. Molecular basis of lung carcinogenesis. In: Coleman WB, Tsongalis GJ, editors. The molecular basis of human cancer. New York: Springer; 2017. p. 447–96.
Gazdar AF, Minna JD. Cigarettes, sex, and lung adenocarcinoma. J Natl Cancer Inst. 1997;89(21):1563–5.
American Cancer Society®. Cancer Facts & Figures 2020. 2020 [cited October 28, 2020]; Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf
Wakefield MA, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98(8):1443–50.
Reckamp KL. Targeted therapy for patients with metastatic non-small cell lung cancer. J Natl Compr Cancer Netw. 2018;16(5s):601–4.
Ettinger DS, et al. NCCN guidelines insights: non-small cell lung cancer, version 1.2020. J Natl Compr Cancer Netw. 2019;17(12):1464–72.
da Cunha Santos G, Shepherd FA, Tsao MS. EGFR mutations and lung cancer. Annu Rev Pathol. 2011;6:49–69.
Sabir SR, et al. EML4-ALK variants: biological and molecular properties, and the implications for patients. Cancers (Basel). 2017;9(9):118.
Cui M, et al. Molecular and clinicopathological characteristics of ROS1-rearranged non-small-cell lung cancers identified by next-generation sequencing. Mol Oncol. 2020;14(11):2787–95.
Reungwetwattana T, et al. The race to target MET exon 14 skipping alterations in non-small cell lung cancer: the why, the how, the who, the unknown, and the inevitable. Lung Cancer. 2017;103:27–37.
Leonetti A, et al. BRAF in non-small cell lung cancer (NSCLC): pickaxing another brick in the wall. Cancer Treat Rev. 2018;66:82–94.
Cancer Genome Atlas Research N. Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511(7511):543–50.
Vaishnavi A, et al. Oncogenic and drug-sensitive NTRK1 rearrangements in lung cancer. Nat Med. 2013;19(11):1469–72.
Cappuzzo F, Bemis L, Varella-Garcia M. HER2 mutation and response to trastuzumab therapy in non-small-cell lung cancer. N Engl J Med. 2006;354(24):2619–21.
De Grève J, et al. Clinical activity of afatinib (BIBW 2992) in patients with lung adenocarcinoma with mutations in the kinase domain of HER2/neu. Lung Cancer. 2012;76(1):123–7.
Li BT, et al. Ado-trastuzumab emtansine for patients with HER2-mutant lung cancers: results from a phase II basket trial. J Clin Oncol. 2018;36(24):2532–7.
Li W, et al. Primary and acquired EGFR T790M-mutant NSCLC patients identified by routine mutation testing show different characteristics but may both respond to osimertinib treatment. Cancer Lett. 2018;423:9–15.
Assi H, et al. Prevalence of T790M mutation among TKI-therapy resistant Lebanese lung cancer patients based on liquid biopsy analysis: a first report from a major tertiary care center. Mol Biol Rep. 2019;46(4):3671–6.
Fang W, et al. EGFR exon 20 insertion mutations and response to osimertinib in non-small-cell lung cancer. BMC Cancer. 2019;19(1):595.
Cress WD, et al. Lung cancer mutations and use of targeted agents in Hispanics. Rev Recent Clin Trials. 2014;9(4):225–32.
Bubendorf L, et al. Testing for ROS1 in non-small cell lung cancer: a review with recommendations. Virchows Arch. 2016;469(5):489–503.
Shackelford RE, et al. ALK-rearrangements and testing methods in non-small cell lung cancer: a review. Genes Cancer. 2014;5(1–2):1–14.
Choi YL, et al. Identification of novel isoforms of the EML4-ALK transforming gene in non-small cell lung cancer. Cancer Res. 2008;68(13):4971–6.
Soda M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448(7153):561–6.
Lin JJ, Shaw AT. Recent advances in targeting ROS1 in lung cancer. J Thorac Oncol. 2017;12(11):1611–25.
Bergethon K, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012;30(8):863–70.
Le T, Gerber DE. ALK alterations and inhibition in lung cancer. Semin Cancer Biol. 2017;42:81–8.
Kawakami H, et al. Targeting MET amplification as a new oncogenic driver. Cancers (Basel). 2014;6(3):1540–52.
Bronte G, et al. Targeting RET-rearranged non-small-cell lung cancer: future prospects. Lung Cancer (Auckl). 2019;10:27–36.
Ackermann CJ, et al. Targeted therapy for RET-rearranged non-small cell lung cancer: clinical development and future directions. Onco Targets and Therapy. 2019;12:7857–64.
Reddy VP, Laurie MG, Elvin JA, Vergilio J-A, Suh J, Ramkissoon S, et al. BRAF fusions in clinically advanced non-small cell lung cancer: an emerging target for anti-BRAF therapies. J Clin Oncol. 2017;35:9072.
Jang JS, et al. Common oncogene mutations and novel SND1-BRAF transcript fusion in lung adenocarcinoma from never smokers. Sci Rep. 2015;5:9755.
Vaishnavi A, Le AT, Doebele RC. TRKing down an old oncogene in a new era of targeted therapy. Cancer Discov. 2015;5(1):25–34.
Russell JP, et al. The TRK-T1 fusion protein induces neoplastic transformation of thyroid epithelium. Oncogene. 2000;19(50):5729–35.
Ricciuti B, et al. Targeting NTRK fusion in non-small cell lung cancer: rationale and clinical evidence. Med Oncol. 2017;34(6):105.
Kris MG, et al. Targeting HER2 aberrations as actionable drivers in lung cancers: phase II trial of the pan-HER tyrosine kinase inhibitor dacomitinib in patients with HER2-mutant or amplified tumors. Ann Oncol. 2015;26(7):1421–7.
Okamoto T, et al. Clinical and genetic implications of mutation burden in squamous cell carcinoma of the lung. Ann Surg Oncol. 2018;25(6):1564–71.
Gandara DR, et al. Squamous cell lung cancer: from tumor genomics to cancer therapeutics. Clin Cancer Res. 2015;21(10):2236–43.
TCGA. Comprehensive genomic characterization of squamous cell lung cancers. Nature. 2012;489(7417):519–25.
Schwaederle M, et al. Squamousness: next-generation sequencing reveals shared molecular features across squamous tumor types. Cell Cycle. 2015;14(14):2355–61.
Friedlaender A, et al. Next generation sequencing and genetic alterations in squamous cell lung carcinoma: where are we today? Front Oncol. 2019;9:166.
Xu F, et al. A TP53-associated gene signature for prediction of prognosis and therapeutic responses in lung squamous cell carcinoma. Onco Targets Ther. 2020;9(1):1731943.
Kashima J, Kitadai R, Okuma Y. Molecular and morphological profiling of lung cancer: a foundation for “next-generation” pathologists and oncologists. Cancers (Basel). 2019;11(5):599.
Paik PK, et al. Next-generation sequencing of stage IV squamous cell lung cancers reveals an association of PI3K aberrations and evidence of clonal heterogeneity in patients with brain metastases. Cancer Discov. 2015;5(6):610–21.
Berland L, et al. Current views on tumor mutational burden in patients with non-small cell lung cancer treated by immune checkpoint inhibitors. J Thorac Dis. 2019;11(Suppl 1):S71–80.
Lindeman NI, et al. Updated molecular testing guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors: guideline from the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. J Mol Diagn. 2018;20(2):129–59.
McDowell EM, et al. The respiratory epithelium. V. Histogenesis of lung carcinomas in the human. J Natl Cancer Inst. 1978;61(2):587–606.
Travis WD, et al. Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol. 2015;10(9):1240–2.
Inamura K, et al. EML4-ALK lung cancers are characterized by rare other mutations, a TTF-1 cell lineage, an acinar histology, and young onset. Mod Pathol. 2009;22(4):508–15.
Heeke S, Hofman P. Tumor mutational burden assessment as a predictive biomarker for immunotherapy in lung cancer patients: getting ready for prime-time or not? Transl Lung Cancer Res. 2018;7(6):631–8.
Greillier L, Tomasini P, Barlesi F. The clinical utility of tumor mutational burden in non-small cell lung cancer. Transl Lung Cancer Res. 2018;7(6):639–46.
Alborelli I, et al. Tumor mutational burden assessed by targeted NGS predicts clinical benefit from immune checkpoint inhibitors in non-small cell lung cancer. J Pathol. 2020;250(1):19–29.
Umemura S, Tsuchihara K, Goto K. Genomic profiling of small-cell lung cancer: the era of targeted therapies. Jpn J Clin Oncol. 2015;45(6):513–9.
Kim YH, et al. Combined microarray analysis of small cell lung cancer reveals altered apoptotic balance and distinct expression signatures of MYC family gene amplification. Oncogene. 2006;25(1):130–8.
Rudin CM, et al. Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene in small-cell lung cancer. Nat Genet. 2012;44(10):1111–6.
Semenova EA, et al. Transcription factor NFIB is a driver of small cell lung cancer progression in mice and marks metastatic disease in patients. Cell Rep. 2016;16(3):631–43.
D’Amico D, et al. High frequency of somatically acquired p53 mutations in small-cell lung cancer cell lines and tumors. Oncogene. 1992;7(2):339–46.
Yokomizo A, et al. PTEN/MMAC1 mutations identified in small cell, but not in non-small cell lung cancers. Oncogene. 1998;17(4):475–9.
Yuan J, et al. Expression of p16 and lack of pRB in primary small cell lung cancer. J Pathol. 1999;189(3):358–62.
Balsara BR, Testa JR. Chromosomal imbalances in human lung cancer. Oncogene. 2002;21(45):6877–83.
Kim KB, Dunn CT, Park KS. Recent progress in mapping the emerging landscape of the small-cell lung cancer genome. Exp Mol Med. 2019;51(12):1–13.
Nishio Y, et al. Telomere length, telomerase activity, and expressions of human telomerase mRNA component (hTERC) and human telomerase reverse transcriptase (hTERT) mRNA in pulmonary neuroendocrine tumors. Jpn J Clin Oncol. 2007;37(1):16–22.
Simbolo M, et al. Lung neuroendocrine tumours: deep sequencing of the four World Health Organization histotypes reveals chromatin-remodelling genes as major players and a prognostic role for TERT, RB1, MEN1 and KMT2D. J Pathol. 2017;241(4):488–500.
Jones MH, et al. Two prognostically significant subtypes of high-grade lung neuroendocrine tumours independent of small-cell and large-cell neuroendocrine carcinomas identified by gene expression profiles. Lancet. 2004;363(9411):775–81.
Swarts DR, Ramaekers FC, Speel EJ. Molecular and cellular biology of neuroendocrine lung tumors: evidence for separate biological entities. Biochim Biophys Acta. 2012;1826(2):255–71.
Hiroshima K, et al. Distinction of pulmonary large cell neuroendocrine carcinoma from small cell lung carcinoma: a morphological, immunohistochemical, and molecular analysis. Mod Pathol. 2006;19(10):1358–68.
Peng WX, et al. Array-based comparative genomic hybridization analysis of high-grade neuroendocrine tumors of the lung. Cancer Sci. 2005;96(10):661–7.
Terra SB, et al. Molecular characterization of pulmonary sarcomatoid carcinoma: analysis of 33 cases. Mod Pathol. 2016;29(8):824–31.
Ushiki A, et al. Genetic heterogeneity of EGFR mutation in pleomorphic carcinoma of the lung: response to gefitinib and clinical outcome. Jpn J Clin Oncol. 2009;39(4):267–70.
Toyokawa G, et al. The first case of lung carcinosarcoma harboring in-frame deletions at exon19 in the EGFR gene. Lung Cancer. 2013;81(3):491–4.
Fallet V, et al. High-throughput somatic mutation profiling in pulmonary sarcomatoid carcinomas using the LungCarta™ Panel: exploring therapeutic targets. Ann Oncol. 2015;26(8):1748–53.
Liang X, et al. Mutation landscape and tumor mutation burden analysis of Chinese patients with pulmonary sarcomatoid carcinomas. Int J Clin Oncol. 2019;24(9):1061–8.
Manabe S, et al. Analysis of targeted somatic mutations in pleomorphic carcinoma of the lung using next-generation sequencing technique. Thorac Cancer. 2020;11(8):2262–9.
Italiano A, et al. EGFR and KRAS status of primary sarcomatoid carcinomas of the lung: implications for anti-EGFR treatment of a rare lung malignancy. Int J Cancer. 2009;125(10):2479–82.
Pelosi G, et al. Multiparametric molecular characterization of pulmonary sarcomatoid carcinoma reveals a nonrandom amplification of anaplastic lymphoma kinase (ALK) gene. Lung Cancer. 2012;77(3):507–14.
Liu X, et al. Next-generation sequencing of pulmonary sarcomatoid carcinoma reveals high frequency of actionable MET gene mutations. J Clin Oncol. 2016;34(8):794–802.
Zhao J, et al. Clinicopathologic features and genomic analysis of pulmonary blastomatoid carcinosarcoma. BMC Cancer. 2020;20(1):248.
Macher-Goeppinger S, et al. Expression and mutation analysis of EGFR, c-KIT, and β-catenin in pulmonary blastoma. J Clin Pathol. 2011;64(4):349–53.
Nakatani Y, et al. Aberrant nuclear localization and gene mutation of beta-catenin in low-grade adenocarcinoma of fetal lung type: up-regulation of the Wnt signaling pathway may be a common denominator for the development of tumors that form morules. Mod Pathol. 2002;15(6):617–24.
Wu Q, et al. Primary pulmonary lymphoepithelioma-like carcinoma is characterized by high PD-L1 expression, but low tumor mutation burden. Pathol Res Pract. 2020;216(8):153043.
Falk N, et al. Primary pulmonary salivary gland-type tumors: a review and update. Adv Anat Pathol. 2016;23(1):13–23.
Xie XH, et al. Clinical features, treatment, and survival outcome of primary pulmonary NUT midline carcinoma. Orphanet J Rare Dis. 2020;15(1):183.
Sholl LM, et al. Primary pulmonary NUT midline carcinoma: clinical, radiographic, and pathologic characterizations. J Thorac Oncol. 2015;10(6):951–9.
French CA, et al. BRD-NUT oncoproteins: a family of closely related nuclear proteins that block epithelial differentiation and maintain the growth of carcinoma cells. Oncogene. 2008;27(15):2237–42.
Schwartz BE, et al. Differentiation of NUT midline carcinoma by epigenomic reprogramming. Cancer Res. 2011;71(7):2686–96.
Lindeman NI, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Mol Diagn. 2013;15(4):415–53.
Drilon A. TRK inhibitors in TRK fusion-positive cancers. Ann Oncol. 2019;30(Suppl 8):viii23–30.
Hellmann MD, et al. Nivolumab plus Ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018;378(22):2093–104.
National Comprehensive Cancer Network (N.C.C.N®). Non-Small Cell Lung Cancer (Version 8.2020). September 15, 2020 [Accessed: October 20, 2020]; Available from: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
Consortium TAPG. AACR project GENIE: powering precision medicine through an international consortium. Cancer Discov. 2017;7(8):818–31.
Mogi A, Kuwano H. TP53 mutations in nonsmall cell lung cancer. J Biomed Biotechnol. 2011;2011:583929.
Roeper J, et al. TP53 co-mutations in EGFR mutated patients in NSCLC stage IV: a strong predictive factor of ORR, PFS and OS in EGFR mt+ NSCLC. Oncotarget. 2020;11(3):250–64.
Yatabe Y, Matsuo K, Mitsudomi T. Heterogeneous distribution of EGFR mutations is extremely rare in lung adenocarcinoma. J Clin Oncol. 2011;29(22):2972–7.
Zhang J, et al. Intratumor heterogeneity in localized lung adenocarcinomas delineated by multiregion sequencing. Science. 2014;346(6206):256–9.
Sherwood J, et al. Mutation status concordance between primary lesions and metastatic sites of advanced non-small-cell lung cancer and the impact of mutation testing methodologies: a literature review. J Exp Clin Cancer Res. 2015;34:92.
Chang YL, Wu CT, Lee YC. Surgical treatment of synchronous multiple primary lung cancers: experience of 92 patients. J Thorac Cardiovasc Surg. 2007;134(3):630–7.
Arai J, et al. Clinical and molecular analysis of synchronous double lung cancers. Lung Cancer. 2012;77(2):281–7.
Girard N, et al. Comprehensive histologic assessment helps to differentiate multiple lung primary nonsmall cell carcinomas from metastases. Am J Surg Pathol. 2009;33(12):1752–64.
Gerlinger M, et al. Genomic architecture and evolution of clear cell renal cell carcinomas defined by multiregion sequencing. Nat Genet. 2014;46(3):225–33.
Chang JC, et al. Comprehensive next-generation sequencing unambiguously distinguishes separate primary lung carcinomas from intrapulmonary metastases: comparison with standard histopathologic approach. Clin Cancer Res. 2019;25(23):7113–25.
Schneider F, et al. Morphological and molecular approach to synchronous non-small cell lung carcinomas: impact on staging. Mod Pathol. 2016;29(7):735–42.
Awad MM, et al. MET exon 14 mutations in non-small-cell lung cancer are associated with advanced age and stage-dependent MET genomic amplification and c-met overexpression. J Clin Oncol. 2016;34(7):721–30.
Li Y, et al. Identification of MET exon14 skipping by targeted DNA- and RNA-based next-generation sequencing in pulmonary sarcomatoid carcinomas. Lung Cancer. 2018;122:113–9.
U.S. Food & Drug Administration (FDA). List of Cleared or Approved Companion Diagnostic Devices (In Vitro and Imaging Tools). 2020 [cited October 27, 2020]; Available from: https://www.fda.gov/medical-devices/vitro-diagnostics/list-cleared-or-approved-companion-diagnostic-devices-vitro-and-imaging-tools
Layfield LJ, et al. Molecular testing strategies for pulmonary adenocarcinoma: an optimal approach with cost analysis. Arch Pathol Lab Med. 2019;143(5):628–33.
Nam SK, et al. Effects of fixation and storage of human tissue samples on nucleic acid preservation. Korean J Pathol. 2014;48(1):36–42.
Kim L, Tsao MS. Tumour tissue sampling for lung cancer management in the era of personalised therapy: what is good enough for molecular testing? Eur Respir J. 2014;44(4):1011–22.
Baloglu G, et al. The effects of tissue fixation alternatives on DNA content: a study on normal colon tissue. Appl Immunohistochem Mol Morphol. 2008;16(5):485–92.
Bellevicine C, et al. How to prepare cytological samples for molecular testing. J Clin Pathol. 2017;70(10):819–26.
Mikubo M, et al. Calculating the tumor nuclei content for comprehensive cancer panel testing. J Thorac Oncol. 2020;15(1):130–7.
Burghel GJ, et al. The importance of neoplastic cell content assessment and enrichment by macrodissection in cancer pharmacogenetic testing. J Clin Pathol. 2019;72(10):721–2.
Villatoro S, et al. Prospective detection of mutations in cerebrospinal fluid, pleural effusion, and ascites of advanced cancer patients to guide treatment decisions. Mol Oncol. 2019;13(12):2633–45.
Gandara DR, et al. Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat Med. 2018;24(9):1441–8.
Leighl NB, et al. Clinical utility of comprehensive cell-free DNA analysis to identify genomic biomarkers in patients with newly diagnosed metastatic non–small cell lung cancer. Clin Cancer Res. 2019;25(15):4691–700.
Rijavec E, et al. Liquid biopsy in non-small cell lung cancer: highlights and challenges. Cancers (Basel). 2019;12(1):17.
Revelo AE, et al. Liquid biopsy for lung cancers: an update on recent developments. Ann Transl Med. 2019;7(15):349.
Chabon JJ, et al. Circulating tumour DNA profiling reveals heterogeneity of EGFR inhibitor resistance mechanisms in lung cancer patients. Nat Commun. 2016;7:11815.
Thress KS, et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med. 2015;21(6):560–2.
Dagogo-Jack I, et al. Tracking the evolution of resistance to ALK tyrosine kinase inhibitors through longitudinal analysis of circulating tumor DNA. JCO Precis Oncol. 2018;2:1–14.
McCoach CE, et al. Clinical utility of cell-free DNA for the detection of ALK fusions and genomic mechanisms of ALK inhibitor resistance in non–small cell lung cancer. Clin Cancer Res. 2018;24(12):2758–70.
Soria JC, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25.
Chan TA, et al. Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol. 2019;30(1):44–56.
Chalmers ZR, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017;9(1):34.
Alexandrov LB, et al. Signatures of mutational processes in human cancer. Nature. 2013;500(7463):415–21.
Carbone DP, et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N Engl J Med. 2017;376(25):2415–26.
Socinski MA, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–301.
Langer C, et al. OA04.05 KEYNOTE-021: TMB and outcomes for carboplatin and pemetrexed with or without pembrolizumab for nonsquamous NSCLC. J Thorac Oncol. 2019;14(10, Supplement):S216.
Garassino M, et al. OA04.06 evaluation of TMB in KEYNOTE-189: pembrolizumab plus chemotherapy vs placebo plus chemotherapy for nonsquamous NSCLC. J Thorac Oncol. 2019;14(10, Supplement):S216–7.
Bevins N, et al. Comparison of commonly used solid tumor targeted gene sequencing panels for estimating tumor mutation burden shows analytical and prognostic concordance within the cancer genome atlas cohort. J Immunother Cancer. 2020;8(1):e000613.
Chaudhary R, et al. A scalable solution for tumor mutational burden from formalin-fixed, paraffin-embedded samples using the Oncomine Tumor Mutation Load Assay. Transl Lung Cancer Res. 2018;7(6):616–30.
Rizvi H, et al. Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung cancer profiled with targeted next-generation sequencing. J Clin Oncol. 2018;36(7):633–41.
Li R, et al. Choosing tumor mutational burden wisely for immunotherapy: a hard road to explore. Biochim Biophys Acta Rev Cancer. 1874;2020(2):188420.
Wang Z, et al. Assessment of blood tumor mutational burden as a potential biomarker for immunotherapy in patients with non-small cell lung cancer with use of a next-generation sequencing cancer gene panel. JAMA Oncol. 2019;5(5):696–702.
Imperial R, et al. Matched whole-genome sequencing (WGS) and whole-exome sequencing (WES) of tumor tissue with circulating tumor DNA (ctDNA) analysis: complementary modalities in clinical practice. Cancers (Basel). 2019;11(9):1399.
U.S. Food & Drug Administration (FDA). FDA approves pembrolizumab for adults and children with TMB-H solid tumors. June 17, 2020; Available from: https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-pembrolizumab-adults-and-children-tmb-h-solid-tumors
Merino DM, et al. Establishing guidelines to harmonize tumor mutational burden (TMB): in silico assessment of variation in TMB quantification across diagnostic platforms: phase I of the Friends of Cancer Research TMB Harmonization Project. J Immunother Cancer. 2020;8(1):e000147.
Büttner R, et al. Implementing TMB measurement in clinical practice: considerations on assay requirements. ESMO Open. 2019;4(1):e000442.
Brahmer J, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–35.
Rittmeyer A, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389(10066):255–65.
Miura Y, Sunaga N. Role of immunotherapy for oncogene-driven non-small cell lung cancer. Cancers (Basel). 2018;10(8):245.
Biton J, et al. TP53, STK11, and EGFR mutations predict tumor immune profile and the response to anti-PD-1 in lung adenocarcinoma. Clin Cancer Res. 2018;24(22):5710–23.
Giroux Leprieur E, et al. Circulating tumor DNA evaluated by Next-Generation Sequencing is predictive of tumor response and prolonged clinical benefit with nivolumab in advanced non-small cell lung cancer. Onco Targets Ther. 2018;7(5):e1424675.
Iijima Y, et al. Very early response of circulating tumour-derived DNA in plasma predicts efficacy of nivolumab treatment in patients with non-small cell lung cancer. Eur J Cancer. 2017;86:349–57.
Looney T, et al. TCR beta chain convergence defines the tumor infiltrating T cell repertoire of melanoma and non-small cell lung carcinoma. Ann Oncol. 2018;29:viii19–20.
Jermann P, et al. TCR-beta repertoire convergence and evenness are associated with response to immune checkpoint inhibitors. Ann Oncol. 2019;30:v851.
Han J, et al. TCR repertoire diversity of peripheral PD-1(+)CD8(+) T cells predicts clinical outcomes after immunotherapy in patients with non-small cell lung cancer. Cancer Immunol Res. 2020;8(1):146–54.
Pao W, et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A. 2004;101(36):13306–11.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Zheng, R., Zhang, L. (2021). Lung Cancer. In: Ding, Y., Zhang, L. (eds) Practical Oncologic Molecular Pathology. Practical Anatomic Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-73227-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-73227-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73226-4
Online ISBN: 978-3-030-73227-1
eBook Packages: MedicineMedicine (R0)