Abstract
In the 2017 WHO classification, chronic myeloid neoplasms include myeloproliferative neoplasms (MPNs), myelodysplastic/myeloproliferative neoplasms (MDS/MPNs), myelodysplastic syndrome (MDS), mastocytosis and myeloid/lymphoid neoplasms with eosinophilia with rearrangements in FGFR1, PDGFRA, PDGFRB, or PCM1-JAK2 fusions. This chapter focuses on the molecular and cytogenetic features of the chronic myeloid neoplasms, covering the underlying genetic abnormalities, and the molecular markers with important diagnostic, prognostic, therapeutic, and disease monitoring utilities.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Myeloproliferative neoplasms
- Myelodysplastic/myeloproliferative neoplasms
- Myelodysplastic syndromes
- Molecular
- Cytogenetic
- Diagnosis
- Prognosis
- Therapy
List of Frequently Asked Questions
-
1.
How many BCR-ABL1 fusion variants are there in chronic myeloid leukemia (CML)?
-
2.
Which molecular genetic techniques are commonly used for the diagnosis of chronic myeloid leukemia (CML)?
-
3.
What cytogenetic abnormalities are commonly seen in accelerated/blast-phase chronic myeloid leukemia (CML)?
-
4.
How is “complete response” to tyrosine kinase inhibitor (TKI) therapy defined in chronic myeloid leukemia (CML)?
-
5.
What tests are useful to monitor tyrosine kinase inhibitor (TKI) therapy in patients with chronic myeloid leukemia (CML)?
-
6.
What is the major cause of resistance to tyrosine kinase inhibitors (TKIs) in chronic myeloid leukemia (CML)? What are the therapeutic options for CML?
-
7.
What are the common molecular alterations in the BCR-ABL1-negative myeloproliferative neoplasms?
-
8.
Which molecular genetic abnormality is frequently associated with chronic neutrophilic leukemia (CNL)?
-
9.
How to distinguish chronic neutrophilic leukemia (CNL) from chronic myeloid leukemia (CML)?
-
10.
What molecular changes are associated with systemic mastocytosis?
-
11.
What is the underlying molecular abnormality of PDGFRA rearrangement?
-
12.
What are the common underlying genetic abnormalities involved in chronic myelomonocytic leukemia (CMML)?
-
13.
What are the prognostic significance of the genetic changes in chronic myelomonocytic leukemia (CMML)?
-
14.
In the 2017 WHO classification, chronic myelomonocytic leukemia (CMML) is further categorized into “proliferative CMML” and “dysplastic CMML.” What are the molecular genetic differences between these two types?
-
15.
Which genetic abnormalities are relatively common in atypical chronic myeloid leukemia (aCML), BCR-ABL1-negative?
-
16.
What are the major features to differentiate atypical chronic myeloid leukemia (aCML), BCR-ABL1-negative, from chronic neutrophilic leukemia (CNL)?
-
17.
Which genes are most commonly mutated in juvenile myelomonocytic leukemia (JMML)?
-
18.
What are the common molecular genetic abnormalities that are associated with myelodysplastic/myeloproliferative neoplasm with ring sideroblasts and thrombocytosis (MDS/MPN-RS-T)?
-
19.
What are the disease-defining chromosomal abnormalities in myelodysplastic syndrome (MDS)?
-
20.
What are the typical clinicopathological findings in patients with myelodysplastic syndrome (MDS) with isolated del(5q)?
-
21.
What are the common molecular abnormalities associated with MDS?
-
22.
How to differentiate idiopathic cytopenia of undetermined significance (ICUS), clonal hematopoiesis of indeterminate potential (CHIP), clonal cytopenia of undetermined significance (CCUS), and myelodysplastic syndrome (MDS) from each other?
Frequently Asked Questions
-
1.
How Many BCR-ABL1 Fusion Variants Are There in Chronic Myeloid Leukemia (CML)?
-
Chronic myeloid leukemia (CML) is a myeloproliferative disorder and characterized by a reciprocal chromosomal translocation between the Abelson oncogene (ABL) on chromosome 9q34.1 and the breakpoint cluster region (BCR) gene on chromosome 22q11.2, also known as Philadelphia chromosome (Ph). BCR-ABL is a constitutively active tyrosine kinase that promotes proliferation through several downstream signaling pathways involving RAS, RAF, JUN kinase, MYC, and STAT [1]. The most common conserved breakpoint in ABL1 gene occurs in the intron before exon 2 (a2) and rarely downstream of exon 2 (a3) [2, 3]. Breakpoints in ABL1 are mostly located in the 5′ of the second exon. The different breakpoints in the BCR gene result in different sizes of BCR-ABL1 fusion genes. Three breakpoint cluster regions in the BCR gene have been identified: major breakpoint cluster region (M-bcr), minor breakpoint cluster region (m-bcr), and micro-breakpoint cluster region (μ-bcr) [4, 5].
-
M-bcr breakpoints occur downstream of exon 13 (e13) or exon 14 (e14) and result in a p210 fusion protein. The p210 (M-bcr) is detected in majority (97–99%) of CML cases and also presents in B-lymphoblastic leukemia/lymphoma (40% of adults and 10% of pediatric B-ALL patients) [6].
-
m-bcr breakpoints occur after the exon 1 (e1) of the BCR gene and produce a smaller fusion protein p190. CML with p190 (m-bcr) is rare (<1%) and mimics chronic myelomonocytic leukemia with increased numbers of monocytes [7]. p190 is mostly associated with Ph-positive B-ALL (60% of adult and 90% of pediatric patients) [6, 8].
-
μ-bcr breakpoints occur beyond the exon 19 (e19) of BCR in the micro-region and encode a larger oncoprotein p230. The p230 (μ-bcr) is rare and associated with cases of neutrophilic CML that display predominant neutrophilic maturation and/or thrombocytosis [9].
-
-
2.
Which Molecular Genetic Techniques Are Commonly Used for the Diagnosis of Chronic Myeloid Leukemia (CML)?
-
The diagnosis of CML is based on the detection of BCR-ABL1 or Ph chromosome t(9,22) (q34.1;q11.2) [10]. Screening test is often performed using blood specimen with abnormal high granulocyte count in a proper clinical setting. The commonly used diagnostic methods for CML are summarized in Table 14.1.
-
Conventional cytogenetics is still an important tool for the detection of the Ph chromosome, and the bone marrow aspirate is the commonly used specimen. It’s routinely performed at the diagnosis which offers baseline information for monitoring clonal evolution. However, conventional cytogenetics has longer turnaround time due to the cell culture, low sensitivity (5–10%), and failure to detect cryptic translocations [11,12,13].
-
Fluorescence in situ hybridization (FISH) uses specific probes for BCR-ABL1 gene and can rapidly identify the abnormality with higher sensitivity and detection cryptic translocations. A wide range of specimens can be used, such as peripheral blood, bone marrow, and paraffin-embedded tissue. To be noted, additional chromosomal changes will be missed by FISH [5]. If the Ph chromosome is detected by conventional cytogenetics, FISH is not mandatory and should not replace conventional cytogenetics.
-
Qualitative reverse transcriptase PCR (RT-PCR) measures BCR-ABL1 transcripts on the mRNA level. Multiplex RT-PCR and nested RT-PCR are useful for detecting atypical BCR-ABL1 variants [11, 14,15,16]. Importantly, qualitative RT-PCR (low sensitivity) should not be used for monitoring molecular response during therapy, which requires quantitative RT-PCR.
-
Quantitative RT-PCR (qPCR) is a highly sensitive assay and required for the initial workup to establish the bassline level for BCR-ABL1 mRNA transcripts. Peripheral blood is more commonly used than bone marrow and makes monitoring less invasive [17, 18]. An international scale (IS) is recommended to standardize BCR -ABL1 mRNA level across different laboratories and is defined as the ratio of BCR-ABL1 transcripts to the internal control (such as ABL1 and GUSB) and reported as BCR-ABL1 percentage on a log scale (10%, 1%, 0.1%, 0.01%, and 0.032% correspond to 1, 2,3, 4, and 4.5 logs, respectively) [19]. To be noted, the low levels of BCR-ABL1 can be detected in normal individuals, and interpretation should be used with caution as the results do not indicate the disease of CML [20].
-
-
3.
What Cytogenetic Abnormalities Are Commonly Seen in Accelerated/Blast-Phase Chronic Myeloid Leukemia (CML)?
-
The evolution of CML from chronic to accelerated phase (AP-CML) or blast phase (BP-CML) is caused by the development of subclones with new cytogenetic and molecular changes. Conventional cytogenetics is useful to detect the additional abnormalities when suspicious of accelerated or blast phase [23, 24]. The most common secondary karyotypic abnormalities in CML in the advanced stages include:
-
Trisomy 8
-
Isochromosome 17q
-
Trisomy 19
-
Secondary Ph
-
Abnormalities of 3q26.2
-
Complex karyotype
-
-
The additional chromosomal abnormalities (ACAs) are further subgrouped by occurring frequency into “major route” (trisomy 8, iso17q, a second Ph or trisomy 19) and “minor route” (−7, −17, +17. +21, -Y and abnormalities of 3q26) [25]. The presence of major route ACA at diagnosis has been associated with poor prognosis [26, 27]. Wang et al. proposed prognostic risk stratification based on the survival and prognosis with TKI therapy and divided ACAs into two groups. Group 1 includes trisomy 8, -Y, and a second Ph and is associated with good prognosis, whereas Group 2 includes i(17)(q10), −7/del7q, and 3q26.2 rearrangements with poor prognosis [28]. The patients with ACAs need to be monitored carefully for the evidence of therapy failure.
-
-
4.
How Is “Complete Response” to Tyrosine Kinase Inhibitor (TKI) Therapy Defined in Chronic Myeloid Leukemia (CML)?
-
TKIs can competitively bind to the ATP -binding pocket of the ABL1 tyrosine kinase domain (TKD) so that the downstream cascade signaling pathway is halted. TKI therapy is considered the standard first-line treatment for the patients with newly diagnosed chronic-phase CML (CP-CML). Complete response to TKI therapy is determined by three different measurements.
-
Complete hematologic response (CHR) includes WBC < 10 × 109/L, platelets <450 × 109/L, the absence of immature granulocytes in peripheral blood, and impalpable spleen.
-
Complete cytogenetic response (CCyR) is defined as the absence of Ph chromosomes, which correlates with BCR-ABL1 ≤1%. The goal of TKI therapy is to achieve a CCyR (≤1% BCR-ABL1 IS) within 12 months after first-line TKI therapy and to prevent disease progression to AP-CML or BP-CML.
-
The major molecular response (MMR) is defined as BCR-ABL1 (IS) ≤0.1% or 3-log reduction in BCR-ABL1 mRNA from the standardized baselines, if qPCR (IS) is not available. The deep molecular response (DMR) is defined as MR 4.0 (BCR-ABL1 IS ≤0.01%) or MR 4.5 (BCR-ABL1 IS ≤0.0032%) [29, 30].
-
-
5.
What Tests Are Useful to Monitor Tyrosine Kinase Inhibitor (TKI) Therapy in the Patients with Chronic Myeloid Leukemia (CML)?
-
Cytogenetic analysis is valuable to assess the degree of cytogenetic response and possible clonal evolution if there is disease progression or relapse.
-
Quantitative RT-PCR (qPCR) is recommended for all patients after initiating TKI therapy. The majority of CML patients achieve major or even deep molecular remissions with TKI therapy. To be noted, qPCR is the only method to monitor response after the patient has achieved in complete cytogenetic response (CCyR).
-
BCR-ABL kinase domain mutational analysis provides additional guidance in the selection of subsequent TKI therapy for patients who do not respond well with TKIs. 1-log increase in BCR-ABL1 transcript levels without loss of MMR should prompt bone marrow evaluation for loss of complete cytogenetic response (CCyR). The recommended tests to monitor the response to TKI are listed in Table 14.2.
-
-
6.
What Is the Major Cause of Resistance to Tyrosine Kinase Inhibitors (TKIs) in CML? What Are the Therapeutic Options for CML?
-
The introduction of tyrosine kinase inhibitors (TKIs) decreased mortality rates in CML. Point mutations in the BCR-ABL1 kinase domain are the major causes for the resistance of TKIs and associated with poor prognosis and higher risk of disease progression. Currently, there are five TKIs available: imatinib (first generation); dasatinib, nilotinib, and bosutinib (second generation); and ponatinib (third generation). The T315I mutation confers complete resistance to imatinib, dasatinib, nilotinib, and bosutinib [28,29,30]. See Table 14.3.
-
-
7.
What Are the Common Molecular Alterations in the BCR-ABL1 -Negative Myeloproliferative Neoplasms?
-
Polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF) are collectively known as Philadelphia chromosome-negative myeloproliferative neoplasms . The identification of driver mutations in JAK2, CALR, and MPL provides a better understanding of the pathogenesis as well as therapeutic options.
-
PV is more homogenous in the molecular level, and most of the patients with PV (95–98%) harbor JAK2 V617F mutation (exon 14), and the remainder of PV cases have small insertion or deletions in JAK2 exon 12 [31,32,33].
-
ET and PMF have more heterogeneous molecular abnormalities with the most common mutation being JAK2 V617F, followed by mutations in CALR (exon 9) and MPL (exon 10). These mutations are mutually exclusive to each other.
-
“Triple negative” refers to negative mutations in JAK2, CALR, and MPL genes. CALR mutations have been shown with favorable clinical courses, while “triple negative” is associated with a worse prognosis in PMF [34,35,36]. In the triple-negative MPNs, the mutations in ASXL1, EZH2, TET2, IDH1, IDH2, SF3B1, and SRSF2 are also helpful in determining the clonal nature of the disease [37,38,39,40]. The comparison of these three Ph-negative MPNs is summarized in Table 14.4.
-
-
8.
Which Molecular Genetic Abnormality Is Frequently Associated with Chronic Neutrophilic Leukemia (CNL) ?
-
Chronic neutrophilic leukemia (CNL) is a rare, aggressive myeloproliferative neoplasm that is characterized with sustained neutrophilic leukocytosis (WBC ≥25 × 109/L with mature neutrophils ≥80% of WBC and immature neutrophilic precursors<10% of WBC; ≥ 3 months), bone marrow granulocytic hyperplasia, and frequent splenomegaly. The differential diagnosis between CNL and aCML is listed in Table 14.6 (question 16).
-
The colony-stimulating factor 3 receptor (CSF3R) mutations were identified in most of the patients with CNL [41,42,43]. The 2017 WHO diagnostic criteria endorsed the presence of CSF3R T618I or another activating CSF3R mutation as an important clonal marker for the diagnosis of CNL [44].
-
There are two types of mutations in CSF3R: point mutations in the extracellular domain (exon 14)-activating JAK-STAT signaling pathway and less frequently, nonsense or frameshift mutations in the cytoplasmic tail (exon 17)-activating SRC tyrosine kinase [45]. In CNL, the most common mutation is the membrane proximal p.Thr618Ile (T618I) point mutation. Mutations in the cytoplasmic truncation mutations are often concurrent with T618I. The two distinct mutation regions and downstream kinases signaling pathways result in the different sensitivity to JAK2 inhibitors (e.g., ruxolitinib) and SRC inhibitors (dasatinib) [45, 46].
-
-
9.
How to Distinguish Chronic Neutrophilic Leukemia (CNL) from Chronic Myeloid Leukemia (CML)?
-
A rare form of CML with p230 BCR-ABL protein may demonstrate prominent neutrophilic maturation and is called neutrophilic-CML (N-CML).
-
Both N-CML and CNL share morphological features such as prominent neutrophilic leukocytosis, minimal granulocytic precursors in the peripheral blood, and hypercellular bone marrow consisting of hyperplastic granulocytic cells.
-
The clinical course of the patients with N-CML is milder with a lower total WBC count, absent or minimal precursors in the peripheral smear, less severe anemia, less prominent splenomegaly, and blastic transformation which occurs much later [9, 43].
-
N-CML is invariably associated with a BCR-ABL1 fusion and should be easily differentiated from CNL with proper molecular testing.
-
-
10.
What Molecular Changes Are Associated with Mastocytosis?
-
Detection of the KIT D816V (exon 17)-activating mutation in the bone marrow, blood, or other extracutaneous organs is counted as a minor criterion for the diagnosis of cutaneous and systemic mastocytosis. KIT D816V can be detected in more than 80% of the patients. KIT D816V is considered as a major therapeutic target in advanced systemic mastocytosis (SM). Though D816V mutation is resistant to imatinib and masitinib, several drugs have been developed (e.g., nilotinib, dasatinib, and midostaurin) to target this mutation. Wild-type KIT and other mutations such as K509I or F522C are sensitive to imatinib [47, 48].
-
Besides D816V, other oncogenic variants of KIT in exons 8, 9, 10, and 11 have been detected. In advanced systemic mastocytosis (SM) and especially in patients with systemic mastocytosis with associated hematological neoplasm (SM-AHN), somatic mutations have been detected in KIT and its signaling pathways [49,50,51].
-
-
11.
What Is the Underlying Molecular Abnormality of PDGFRA Rearrangement?
-
Myeloid/lymphoid neoplasms with eosinophilia involving recurrent genetic abnormalities of PDGFRA, PDGFRB, FGFR1, or PCM1-JAK2 are a specific disease entity defined by the 2017 WHO [44]. Tyrosine kinase inhibitors have been proven successful for the treatment of PDGFRA-, PDGFRB-, and PCM1-JAK2-related diseases. However, FGFR1-associated neoplasms are resistant to imatinib therapy and associated with a poor prognosis [52, 53].
-
FIP1L1-PDGFRA fusion gene results from an 800-kb cryptic interstitial deletion that includes the cysteine-rich hydrophobic domain 2 (CHIC2) loci at 4q12. The deletion disrupts the FIP1L1 and PDGFRA genes and fuses the 5′ part of FIP1L1 to the 3′ part of PDGFRA [53, 54].
-
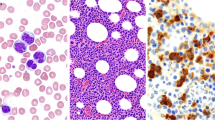
FIP1L1-PDGFRA fusion gene can only be detected by break-apart FISH or RT-PCR due to cryptic deletion [Fig. 14.1]. Since the CHIC2 gene is in this deleted region, the test is also referred as “FISH for CHIC2 deletion” [55, 56]. The FIP1L1-PDGFRA fusion has been identified in patients with increased eosinophilia associated with acute myeloid leukemia, mast cell neoplasms, and T-cell lymphoblastic lymphoma [57, 58].
-
-
12.
What Are the Common Underlying Genetic Abnormalities Involved in Chronic Myelomonocytic Leukemia (CMML) ?
-
Chronic myelomonocytic leukemia (CMML) is a clonal hematopoietic stem cell disorder with overlapping features of MDS and MPN and potential evolution to acute myeloid leukemia. It is characterized by the presence of sustained (>3 months) peripheral blood monocytosis (≥1 × 109/L; monocytes ≥10% of white blood cells count) with or without dysplastic changes in the bone marrow [44]. The BCR-ABL1 fusion and rearrangements of PDGFRA, PDGFRB, or FGFR1 are absent.
-
Clonal cytogenetic abnormalities are seen in about 20–40% of patients. Most common abnormalities include trisomy 8, monosomy 7, del (7q), trisomy 21, and complex karyotypes [59, 60].
-
Recurrent somatic gene mutations have been identified in up to 90% of CMML cases. These gene mutations in CMML are divided into three groups: regulate cell signaling molecules (KRAS, NRAS, CBL, PTPN11, FLT3, JAK2), splicing factors (SRSF2, SF3B1, ZRSF2, U2AF1), and epigenetic control of transcription such as DNA methylation (DNMT3A, IDH1, IDH2, and TET2) and histone modification (ASXL1, EZH2, and BCOR) [61,62,63,64,65,66,67,68,69,70,71]. Of these, the most frequent mutations involve TET2 (~60%), SRSF2 (~50%), ASXl1 (~40%), and the RAS signaling pathway (~30%). The triad of TET2, SRSF2, and ASXL1 mutations is very specific for CMML [72, 73].
-
-
13.
What Is the Prognostic Significance of the Genetic Changes in Chronic Myelomonocytic Leukemia (CMML)?
-
Karyotypic abnormalities occur in 20–30% of patients with CMML. The Spanish CMML-specific cytogenetic risk stratification (CPSS) system separates the patients into three prognostic groups: low risk (normal karyotype and isolated loss of Y chromosome), high risk (trisomy 8, chromosome 7 abnormalities and complex karyotype), and intermediate (all other karyotypic abnormalities). The 5-year overall survival (OS) was 35% for low-risk, 26% for intermediate, and 4% for high-risk groups [60, 74].
-
Mayo molecular model (MMM) that focused on the combination of hemoglobin, absolute monocyte, circulating immature myeloid cells and platelet values, and ASXL1. The univariate analysis showed a poor prognostic value of nonsense/frameshift ASXL1 mutations [75, 76].
-
CMML-specific prognostic scoring system (CPSS) was updated to include molecular mutations in RUNX1, NRAS, SETBP1, and ASXL1 in addition to the prior CPSS cytogenetic scores. The CPSS-Mol stratified CMML into four risk groups: low (0 risk factors), intermediate-1 (1 risk factor), intermediate-2 (2–3 risk factors), and high (≥4 risk factors) [77, 78]. NPM1 mutation in CMML is rare and tends to be associated with normal cytogenetics, dysplastic CMML, DNTM3A mutations, and high risk of AML transformation [79, 80].
-
-
14.
In the 2017 WHO Classification, Chronic Myelomonocytic Leukemia (CMML) Is Further Categorized into “ Proliferative CMML ” and “Dysplastic CMML.” What Are the Clinical and Molecular Genetic Differences Between These Two Types?
-
CMML is heterogeneous with different clinical manifestations and underlying molecular changes. CMML is further divided into “dysplastic CMML (WBC < 13 × 109/L)” and “proliferative CMML” (WBC ≥ 13 × 109/L) [Table 14.5]. If myelodysplasia is absent or minimal, a diagnosis of CMML can still be made if clonal cytogenetic or molecular abnormalities are present [44, 61, 81, 82].
-
(a) Schematic representation of the three probes for FIP1L1 (green), CHIC2 (red), and PDGFRA genes(aqua) that flank the 4q12 region. (b) The deletion of CHIC2 resulted in the fusion of 5′ of FIP1L1 to the 3′ part of PDGFRA. The absence of CHIC (red) signaling and the presence of the two flaking probes is indicative of the deletion of CHIC gene. (Credit for Jason Yuhas, Genomics Laboratory, Mayo Clinic, MN)
-
15.
Which Genetic Abnormalities Are Relatively Common in Atypical Chronic Myeloid Leukemia (aCML), BCR-ABL1 -Negative?
-
Atypical chronic myeloid leukemia (aCML) is a rare subtype of MDS/MPN. Patients tend to have severe anemia, thrombocytopenia, neutrophilic leukocytosis, granulocytic dysplasia, and splenomegaly. BCR-ABL1 fusions as well as the rearrangements of PDGFRA, PDGFRB, or FGFR1 are absent in aCML.
-
The most common cytogenetic abnormalities are gain of chromosome 8 and del(20q) [84, 85]. The other reported changes included −7/−7q and i17 (q); deletions of 5q, 13q, 17p, 12q, and 11q; t(6,8) (p23;q22); trisomy 14, 21, and 19; and complex karyotype [86]. However, none of these abnormalities is specific for aCML.
-
Currently, no specific molecular changes have been identified for aCML. Recurrent SETBP1 mutations, which are encountered in 12–33% of aCML patients, are associated with worse prognosis than aCMLs with wild-type SETBP1 [87,88,89]. However, SETBP1 mutations have also been described in patients with CMML (15%) and JMML (<3%) [89,90,91,92].
-
Somatic missense mutations involving ETNK1 have been found in 8.8% of aCML cases [93]. Other somatic mutations involving NRAS, KRAS, TET2, EZH2, JAK2, IDH2, CSF3R, SRSF2, RUNX1, CEBPA, ASXL1, and CBL have also been detected in aCML, although at a much lower frequency [72, 86, 88, 94].
-
-
16.
What Are the Major Features to Differentiate Atypical Chronic Myeloid Leukemia (aCML), BCR-ABL1 -Negative, from Chronic Neutrophilic Leukemia (CNL) ?
-
There are strong morphological and clinical resemblances between aCML and CNL. Lack of specific molecular markers makes the diagnosis challenging in some cases. It is important to incorporate clinical presentations, morphology, and molecular markers for an accurate diagnosis [Table 14.6].
-
-
17.
Which Genes Are Most Commonly Mutated in Juvenile Myelomonocytic Leukemia (JMML)?
-
Juvenile myelomonocytic leukemia (JMML) is a rare MDS/MPN disorder that occurs during infancy and early childhood, clinically characterized by the overproduction of myelomonocytic cells. It is associated with a poor prognosis and shares some clinical and molecular features with CMML.
-
The recurrent mutations in the RAS signaling pathway are the main driving events in JMML. About 90% of the patients harbor either a somatic or germline mutation in the genes of PTPN11, NF1, NRAS, KRAS, and CBL; these genetic mutations are largely mutually exclusive. Among these, the gain-of-function mutations in PTPN11 are the most common molecular genetic changes (35%) in JMML [95,96,97]. A recent study with RNA-sequencing detected ALK/ROS1 tyrosine kinase fusion (18%) in JMML patients without RAS pathway mutations [98]. Germline mutations in NF1 are present in 10% of children with JMML. In some cases, JMML may be the first sign of neurofibromatosis 1. The patients are mostly diagnosed after 5 years and have a higher blast count in BM and higher platelet count than the patients without NF1 [98, 99].
-
Noonan syndrome is the most common RASopathy, involving germline mutations in PTPN11 (~50%), SOS1, RAF1, RIT1, KRAS, or other genes of the RAS signaling pathway. Approximately 3% of neonates and infants with Noonan syndrome develop JMML [100].
-
-
18.
What Are the Common Molecular Genetic Abnormalities That Are Associated with Myelodysplastic/Myeloproliferative Neoplasm with Ring Sideroblasts and Thrombocytosis (MDS/MPN-RS-T)?
-
MDS/MPN-RS-T is characterized by thrombocytosis (≥450 × 109/L), refractory anemia and dyserythropoiesis with ring sideroblasts (≥15% of erythroid precursors) in the bone marrow. Somatic mutations in the spliceosome gene SF3B1 are associated with ring sideroblasts and are highly associated (65–90%) with MDS/MPN-RS-T [101,102,103].
-
SF3B1 mutations often coexist with JAK2 V617F (~50%) and less commonly CALR (0–3%) or MPL (1–3%) in MDS/MPN-RS-T [104,105,106]. SF3B1 mutations confer increased risk of thrombosis in patients with MDS/MPN-RS-T [107]. Mutations of TET2, ASXL1, SETBP1, and DNMT3A were also detected in several cohort studies [105].
-
The prognosis of MDS/PMN-RS-T is better than that of MDS-RS but inferior to that of ET. The patients with SF3B1 mutations had fewer cytopenias and longer event-free survival than those with wild-type [102]. The presence of a SF3B1 mutation is an independent predictor for a favorable clinical outcome, while ASXL1 or SETBP1 mutations are associated with poor prognosis [101, 105].
-
-
19.
What Are the Disease-Defining Chromosomal Abnormalities in Myelodysplastic Syndrome (MDS)?
-
Chromosomal abnormalities can be detected by cytogenetics in 50% of de novo MDS cases [110]. Of these, the most common abnormalities are monosomy 5/del(5q), trisomy 8, and monosomy 7/del(7q) [111]. Balanced chromosomal translocations are relatively rare (<2–3%) in MDS and are also important to help the diagnosis of MDS with equivocal morphological dysplastic features [112, 113]. The recurrent chromosomal abnormalities are summarized in Table 14.7. Presence of one of these chromosomal abnormalities is presumptive evidence of MDS in patients with otherwise unexplained refractory cytopenia and no morphologic evidence of dysplasia [45]. Complex chromosomal abnormalities are defined as multiple (≥3) chromosomal abnormalities and often associated with TP53 mutation and a poor clinical course [114].
-
It should be noted that certain cytogenetic alterations have been found in the normal elderly population, such as -Y. Without definitive morphological evidence, these cytogenetic changes are insufficient to establish a diagnosis of MDS.
-
-
20.
What Are the Typical Clinicopathological Findings in Patients with Myelodysplastic Syndrome (MDS) with Isolated del(5q)?
-
MDS with isolated del(5q) is defined by the presence of cytogenetic abnormality involving an interstitial deletion of the long arm of chromosome 5 (5q) with or without one additional cytogenetic abnormality (except del(7q) or monosomy 7) and in the absence of increased blasts [110, 111]. There are two common deleted regions (CDR): one is the region flanking 5q32–33.1 which is with 5q-syndrome that confers a good clinical course; the other one is 5q31.2 which is more common in patients with high-risk MDS and therapy-related myeloid neoplasms [112,113,114]. In the 2017 WHO classification, isolated del(5q) is the only cytogenetic abnormality to define a specific MDS subtype.
-
MDS with isolated del(5q) is one of the most common cytogenetic changes in patients with MDS (10–15%), and mostly affect elderly women and typically present macrocytic anemia, thrombocytosis, neutropenia, and hypolobated small megakaryocytes in the bone marrow [115].
-
Patients with MDS with isolated del(5q) generally have a favorable prognosis with a median survival and a low risk of transformation to AML [116, 117]. Gain of an additional clonal aberration with monosomy 7 or del(7q) was shown to confer a poor prognosis [118]. TP53 mutation has been found to correlate with a significantly worse outcome, which is helpful to further refine the prognostic risk [119, 120]. ASXL1 mutation is associated with a higher risk of AML transformation [111].
-
Lenalidomide , an immunomodulatory drug with efficacy in multiple myeloma (MM), is the standard therapy for the patients with MDS with isolated del(5q). However TP53 mutation has been shown to confer lenalidomide resistance [115].
-
-
21.
What Are the Common Molecular Abnormalities Associated with MDS?
-
Gene mutations in MDS can occur with or without chromosomal abnormalities and have been shown to have prognostic and therapeutic significance. The common driver genes mutated in MDS with mutational frequency and respective common associations are summarized in Table 14.8.
-
The driver genes are classified into several functional pathways including DNA methylation, RNA spliceosome machinery, histone modification, transcription, signal transduction, DNA repair, and cohesion complexes [121].
-
The most frequently mutated genes are SF3B1, TET2, SRSF2, and ASXL1 (>10%), followed by DNMT3A and RUNX1 (5–10%) [122]. Most of these mutations are associated with functional loss, instead of activating mutations. The wide spectrum of the mutations contributes to the different clinical courses in the patients with MDS.
-
Keep in mind that germline mutations in DDX41, RUNX1, GATA2, and TP53 may also occur, and it is crucial to screen the family members when bone marrow transplant is the treatment of choice.
-
-
22.
How to Differentiate Idiopathic Cytopenia of Undetermined Significance (ICUS) , Clonal Hematopoiesis of Indeterminate Potential (CHIP), Clonal Cytopenia of Undetermined Significance (CCUS), and Myelodysplastic Syndrome from Each Other?
-
ICUS, CHIP, and CCUS are considered precursor conditions that can progress to MDS, AML, or other hematologic malignancies [Table 14.9]. It is important to make accurate diagnosis for monitoring cytopenia and clinical follow-up.
-
ICUS is defined as persistent cytopenia (≥6 months) in one or more lineages and absence of fulfillment of the diagnostic criteria for MDS. CCUS is defined as persistent cytopenia (≥4 months) in one or more lineages as well as at least one somatic mutation in MDS-associated genes (allele burden ≥2% in bone marrow or peripheral blood).
-
CHIP is defined as the absence of persistent cytopenia but presents ≥1 somatic mutation in MDS-associated genes (≥2% variant allele frequency) [124, 125].
-
Case Presentation
Case 1
Learning Objectives
To become familiar with the underlying cytogenetic abnormalities for CML accelerated and blast phase.
Case History
A 30-year-old male with a history of CML (Philadelphia chromosome-positive, p210) presented with fever and diarrhea with CBC: Hb 10.9 g/dL; RBC 3.79 × 1012/L; MCV 89.7 fL; RDW 20.8%; WBC 11.0 × 109/L; and platelet 341 × 109/L. Peripheral blood smear was reviewed as no cytological abnormalities with no blasts identified.
Bone Marrow, Biopsy, and Aspirate
-
Bone marrow core biopsy with hypercellular bone marrow with abnormal interstitial infiltration of immature cells [Fig. 14.2a].
-
Bone marrow aspirate smear showed the immature cells have high N/C ratio, scant basophilic cytoplasm, fine chromatin, and conspicuous nucleoli, consistent with blast cells [Fig. 14.2b].
Differential Diagnosis
-
CML chronic phase
-
CML blast phase
-
CML accelerated phase
Ancillary Studies
-
IHC demonstrated that the blasts are mostly negative for CD34 and positive for TdT. On the flow cytometry analysis, the blasts are positive for CD19 and CD10 but are negative for CD20 and MPO.
-
Flow cytometry on the bone marrow showed 22% blasts with B-ALL phenotype that are positive for CD34 (partial), CD19, CD10 (partial), CD45 (dim), CD13 (partial), CD33 (dim), HLA-DR, CD38, and CD9 (partial) and negative for CD3, CD15, CD16, CD117, CD2, CD7, CD56, CD36, CD64, CD20, and MPO.
-
Cytogenetic: 46,XY,add(5)(q13),t(9;22)(q34;q11.2) [4]/46,Y,t(X;5)(p10;p10),add(5)(q13),t(9;22)(q34;q11.2),der(17)t(5;17)(q13;q21) [4]/46,XY,t(2;21)(p13;q22),add(5)(q13),t(9;22)(q34;q11.2) [1]/46,XY [10]. Of the 20 metaphases, 10 were normal, and 10 had a t(9,22)(q34;q11.2) and additional abnormalities.
-
FISH analysis: 1.8% of nuclei had BCR-ABL1 fusion.
-
Molecular studies: BCR-ABL1 RT-qPCR result of 1.47 (IS).
Final Diagnosis
Chronic myeloid leukemia , BCR-ABL1-positive, blast phase (22% B-lymphoblasts)
Take Home Messages
-
1.
CML can progress into blast phase with increased blast, ≥ 20% in the blood or bone marrow, or the presence of extramedullary blast proliferation.
-
2.
Progression is often associated with additional cytogenetic changes including a second Ph chromosome, trisomy 8, trisomy 19, and isochromosome 17q.
-
3.
The blast lineage can be myeloid (70–80%) or lymphoid (20–30%). The prognosis of the blast phase is poor.
Case 2
Learning Objectives
To become familiar with the molecular basis of essential thrombocythemia .
Case History
A 46-year-old male presented with thrombocytosis for a few years. He denies headaches, dizziness, blurred vision, fevers, chills, weight loss, or night sweat. JAK2 mutation analysis from outside the hospital showed negative for V617F. Current CBC: Hb 15.4 g/dL; RBC 4.70 × 1012/L; MCV 94.5 fL; RDW 12.9%; WBC 6.6 × 109/L; platelet 1151 × 109/L.
Bone Marrow, Biopsy and Aspirate
-
Normocellular bone marrow with trilineage hematopoietic maturation and increased number of large megakaryocytes dispersed throughout. No significant increase in erythropoiesis or granulopoiesis [Fig. 14.3a].
-
The megakaryocytes are presented with abundant mature cytoplasm and hypersegmented (staghorn-like) nuclei. Some form loose clusters [Fig. 14.3b].
Differential Diagnosis
-
Reactive thrombocytosis
-
Essential thrombocythemia
-
Primary myelofibrosis
-
Polycythemia vera
Ancillary Studies
-
Iron stain, bone marrow aspirate: increased storage iron. Sideroblasts present. No ring sideroblasts seen
-
Reticulin stain, bone marrow biopsy: no increase in reticulin fibrosis, grade 0 of 3
-
Cytogenetics (bone marrow): 46, XY [20]
-
Molecular analysis (JAK2, CALR, and MPL mutation): positive for CALR mutation [Fig. 14.3c]. Negative for JAK2 V617F and MPL mutation
Final Diagnosis
Essential Thrombocythemia
Take Home Messages
-
1.
ET is characterized with an elevated platelet count (≥ 450 × 109/L) on routine CBC and presence of a clonal marker. In most cases (>95%), mutations of one of the three genes (JAK2, CALR, and MPL) can be detected, and they are mutually exclusive.
-
2.
The majority of CALR mutational changes are insertion or deletion in exon 9 resulting in truncated protein. The 52-bp deletion (type 1) and the 5-bp insertion (type 2) are the most frequent CALR mutations.
-
3.
Triple-negative ETs have a better prognosis, whereas triple-negative PMFs are associated with a worse survival rate.
-
4.
Morphology is important to distinguish ET from prefibrotic/early primary myelofibrosis (PMF), which may also present as thrombocytosis [Table 14.4]. The patients with ET have a low risk of progression to acute leukemia and superior overall survival than those with pre-PMF.
Case 3
Learning Objectives
To become familiar with the diagnostic criteria for systemic mastocytosis .
Case History
A 56-year-old female with a history of urticaria pigmentosa presented with persistent diarrhea. Image studies showed mild hepatomegaly, significant splenomegaly, and mild thickening of the stomach walls. The biopsy of the colon demonstrated mast cell infiltration. The tryptase level was 498 ng/ml. Current CBC: Hb 8.2 g/dL; RBC 2.6 × 1012/L; MCV 91.7 fL; RDW 16.2%; WBC 2.7 × 109/L (lymphocytes 1%, monocytes 9%, eosinophil 17%); platelet 23 × 109/L.
Bone Marrow, Biopsy, and Aspirate (BM-184793)
-
Abnormal paratrabecular infiltration of dense spindle-shaped cells with increased eosinophils [Fig. 14.4a]
Differential Diagnosis
-
1.
Reactive mastocytosis
-
2.
Systemic mastocytosis
Ancillary Studies
-
On immunohistochemistry stain, the neoplastic cells are strongly positive for CD117 [Fig. 14.4b] and CD25 [Fig. 14.4c].
-
Cytogenetics (bone marrow): 46,XX [20].
-
Molecular analysis (bone marrow): positive for KIT p.Asp816Val.
Final Diagnosis
Systemic mastocytosis
Take Home Messages
-
1.
The diagnosis for systemic mastocytosis requires one major criterion and at least one minor criterion; or ≥ 3 minor criteria are met.
-
2.
The major criterion is the presence of multifocal clusters of mast cells (≥15 mast cells in aggregates) in the bone marrow and/or extramedullary site(s).
-
3.
The minor criteria include atypical morphology of mast cells (≥25% of mast cells), activating mutation at codon 816 of KIT, abnormal expression CD25, with or without CD2, and serum total tryptase >20 ng/ml.
Case 4
Learning Objectives
To become familiar with the diagnostic criteria for chronic myelomonocytic leukemia .
Case History
A 64-year-old male was referred with progressive drop in hemoglobin, white blood cell count, and platelet count over several years. He also complained of intermittent left-sided abdominal pain and low back pain. He denied any recurrent infection or bleeding tendencies. Imaging showed mild splenomegaly. Current CBC: Hb 8.1 g/dL; RBC 2 × 1012/L; MCV 90 fL; RDW 14%; WBC 3.2 × 109/L; platelet 106 × 109/L. White blood cell differential showed absolute monocytosis with monocytes 36%.
Bone Marrow, Biopsy, and Aspirate
-
Hypercellular marrow with granulocytic and megakaryocytic proliferation. Frequent small forms dysplastic megakaryocytes with monolobated and/or hyperchromatic nuclei are noted [Fig. 14.5a and b].
-
Marrow aspirate smear demonstrated the dysgranulopoiesis with hypolobated/pseudo-Pelger-Huet and hypogranular forms. Blasts are minimally increased (4%) [Fig. 14.5c].
Differential Diagnosis
-
1.
Atypical chronic myeloid leukemia, BCR-ABL1-negative
-
2.
Chronic myelomonocytic leukemia
-
3.
Myelodysplastic syndrome with multilineage dysplasia
-
4.
Reactive monocytosis
Ancillary Studies
Iron stains (bone marrow aspirate): normal stainable storage iron. Sideroblasts present. Rare ring sideroblasts are not seen.
Cytogenetics (bone marrow): 46, XY [20].
Molecular analysis: pathogenic mutations detected as follows:
-
1.
TET2: c.538C > T; p.Gln180* (6%)
c.774dup; p.Glu259* (14%)
c.2524dup; p.Ser842Phefs*4 (6%)
c.4546C > T; p.Arg1516* (7%)
-
2.
ZRSR2: c.122-1G > A; p.? (89%)
Final Diagnosis
Chronic myelomonocytic leukemia-0 (CMML-0)
Take Home Messages
-
1.
CMML is characterized by persistent monocytosis (≥1 × 109/L and ≥ 10% of WBC) in the peripheral blood as well as dysplastic changes in the bone marrow. Cytopenias and splenomegaly are common. It is divided into proliferative type (WBC ≥ 13 × 109/L) and dysplastic type (<13 × 109/L).
-
2.
The most common molecular mutations in CMML are TET2, SRSF2, ASXL1, and SETBP1.
-
3.
The mutation profile of this case provides clonal evidence; although not entirely specific, is extremely helpful for the definitive diagnosis.
Case 5
Learning Objectives
To become familiar with the clinical presentation and diagnostic criteria for MDS with isolated del(5q) (correlation and comparison with Case 6).
Case History
A 80-year-old female presented with fatigue, and she denies any recent weight loss, night sweats, or fever. No history of pulmonary or cardiovascular diseases. No exposure to chemotherapy, radiation, or mutagens and normal levels of folate, vitB12, copper, iron/ferritin, TSH, and LDH. Current CBC: Hb 7.2 g/dL; RBC 1.8 × 1012/L; MCV 122.7 fL; RDW17%; WBC 2.5 × 109/L; PLT 159 × 109/L.
Bone Marrow, Biopsy, and Aspirate
-
Many small and monolobated forms distributed in loose clusters [Fig. 14.6a]
-
Bone marrow smears of the same case [Fig. 14.6b]
Differential Diagnosis
-
1.
Myelodysplastic syndrome with isolated del(5q)
-
2.
Myelodysplastic syndrome with single lineage dysplasia
Ancillary Studies
Iron stain (bone marrow aspirate): normal storage iron, sideroblasts are present, no ring sideroblasts.
On immunohistochemical stain, CD61 highlights many small hypolobated/monolobated megakaryocytes [Fig. 14.6c]
Cytogenetic (bone marrow): 46,XX,del(5)(q15q33) [18]/46,XX [1]
Molecular analysis (bone marrow): negative for TP53 gene mutation
Final Diagnosis
Myelodysplastic syndrome with isolated del(5q).
Take Home Messages
-
1.
MDS syndrome with isolated del(5q) is characterized by macrocytic anemia with or without other cytopenia and/or thrombocytosis with female predominance.
-
2.
Bone marrow shows increased megakaryocytes with non-lobated and hypolobated nuclei. Blast count<5%. Of note, similar findings can be seen in MDS with inv(3).
-
3.
Can present with one additional cytogenetic abnormality, other than monosomy 7 or del(7q).
-
4.
TP53 mutation is associated with increased risk of leukemia and poor survival.
Case 6
Learning Objectives
To become familiar with the classification for MDS .
Case History
An 80-year-old male presented with fatigue for several months. He has been followed up for several years for a history of mild asymptomatic splenomegaly without any demonstrable underlying hematological disorder. He denies having recurrent infections, fevers, chills, nausea, vomiting, diarrhea, overt bleeding, skin changes, lymphadenopathy, unintentional weight loss, and drenching night sweats. Current CBC: Hb 8.4 g/dL; RBC 2.2 × 1012/L; MCV 110.4 fL; RDW 18.8%; WBC 5 × 109/L; platelet 166 × 109/L.
Bone Marrow, Biopsy, and Aspirate
-
Both erythroid and myeloid lineages show full range of maturation with normal morphology. Blasts are not increased.
-
Abnormal megakaryocytes with many monolobated forms [Fig. 14.7a and b].
-
Iron stain shows storage iron present without ring sideroblasts.
Differential Diagnosis
-
1.
Myelodysplastic syndrome with single lineage dysplasia
-
2.
Myelodysplastic syndrome with isolated del(5q)
Ancillary Studies
Iron stains (bone marrow aspirate): normal stainable storage iron. Sideroblasts present. Rare ring sideroblasts seen (1% of erythroid precursors)
Cytogenetics (bone marrow): 46,XY,del(5)(q13q33) [1]/46,idem,del(7)(q22q34) [7]/46, XY [11]
Molecular analysis: TP53 Arg175Cys, a variant of uncertain clinical significance
Final Diagnosis
Myelodysplastic syndrome with single lineage dysplasia (MDS-SLD) .
Take Home Messages
-
1.
The diagnostic criteria for MDS-SLD include single cytopenia or bicytopenia and ≥ 10% dysplastic cells in one cell line and blasts <5%. The diagnosis requires correlation with clinical and other laboratory tests to exclude nutrition, toxic metals, medications, and other factors that can also cause dysplastic changes.
-
2.
Patients with MDS with isolated del(5q) have a relatively better prognosis and reduced risk of progression to AML. Chromosomal 7 abnormalities are associated with worse prognosis and reduced overall survival. MDS with isolated del(5q) as well as del7q/monosomy 7 should be best diagnosed as MDS-SLD.
References
Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2014 update on diagnosis, monitoring, and management. Am J Hematol. 2014;89(5):547–56.
Melo JV. The diversity of BCR-ABL fusion proteins and their relationship to leukemia phenotype. Blood. 1996;88(7):2375–84.
Foroni L, et al. Guidelines for the measurement of BCR-ABL1 transcripts in chronic myeloid leukaemia. Br J Haematol. 2011;153(2):179–90.
Bennour A, et al. Comprehensive analysis of BCR/ABL variants in chronic myeloid leukemia patients using multiplex RT-PCR. Clin Lab. 2012;58(5–6):433–9.
Bennour A, Saad A, Sennana H. Chronic myeloid leukemia: relevance of cytogenetic and molecular assays. Crit Rev Oncol Hematol. 2016;97:263–74.
Faderl S, Jeha S, Kantarjian HM. The biology and therapy of adult acute lymphoblastic leukemia. Cancer. 2003;98(7):1337–54.
Melo JV, et al. P190BCR-ABL chronic myeloid leukaemia: the missing link with chronic myelomonocytic leukaemia? Leukemia. 1994;8(1):208–11.
Hochhaus A, et al. A novel BCR-ABL fusion gene (e6a2) in a patient with Philadelphia chromosome-negative chronic myelogenous leukemia. Blood. 1996;88(6):2236–40.
Pane F, et al. Neutrophilic-chronic myeloid leukemia: a distinct disease with a specific molecular marker (BCR/ABL with C3/A2 junction). Blood. 1996;88(7):2410–4.
Rowley JD. Letter: a new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature. 1973;243(5405):290–3.
Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2020 update on diagnosis, therapy and monitoring. Am J Hematol. 2020; 96(6):691–709.
Yeung CC, Egan D, Radich JP. Molecular monitoring of chronic myeloid leukemia: present and future. Expert Rev Mol Diagn. 2016;16(10):1083–91.
Chereda B, Melo JV. Natural course and biology of CML. Ann Hematol. 2015;94(Suppl 2):S107–21.
Mondal BC, et al. e19a2 BCR-ABL fusion transcript in typical chronic myeloid leukaemia: a report of two cases. J Clin Pathol. 2006;59(10):1102–3.
Schoch C, et al. Comparison of chromosome banding analysis, interphase- and hypermetaphase-FISH, qualitative and quantitative PCR for diagnosis and for follow-up in chronic myeloid leukemia: a study on 350 cases. Leukemia. 2002;16(1):53–9.
Tohami T, Nagler A, Amariglio N. Laboratory tools for diagnosis and monitoring response in patients with chronic myeloid leukemia. Isr Med Assoc J. 2012;14(8):501–7.
Akard LP, et al. Correlations between cytogenetic and molecular monitoring among patients with newly diagnosed chronic myeloid leukemia in chronic phase: post hoc analyses of the rationale and insight for Gleevec high-dose therapy study. Arch Pathol Lab Med. 2014;138(9):1186–92.
Radich JP, et al. Chronic myeloid Leukemia, version 1.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2018;16(9):1108–35.
Hughes T, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108(1):28–37.
Bose S, et al. The presence of typical and atypical BCR-ABL fusion genes in leukocytes of normal individuals: biologic significance and implications for the assessment of minimal residual disease. Blood. 1998;92(9):3362–7.
Deininger MW. Milestones and monitoring in patients with CML treated with imatinib. Hematology Am Soc Hematol Educ Program. 2008;(1):419–26.
Apperley JF. Chronic myeloid leukaemia. Lancet. 2015;385(9976):1447–59.
Feldman E, et al. The emergence of Ph-, trisomy −8+ cells in patients with chronic myeloid leukemia treated with imatinib mesylate. Exp Hematol. 2003;31(8):702–7.
Griesshammer M, et al. Karyotype abnormalities and their clinical significance in blast crisis of chronic myeloid leukemia. J Mol Med (Berl). 1997;75(11–12):836–8.
Mitelman F. The cytogenetic scenario of chronic myeloid leukemia. Leuk Lymphoma. 1993;11(Suppl 1):11–5.
Fabarius A, et al. Impact of unbalanced minor route versus major route karyotypes at diagnosis on prognosis of CML. Ann Hematol. 2015;94(12):2015–24.
Verma D, et al. Survival outcomes for clonal evolution in chronic myeloid leukemia patients on second generation tyrosine kinase inhibitor therapy. Cancer. 2010;116(11):2673–81.
Wang W, et al. Risk stratification of chromosomal abnormalities in chronic myelogenous leukemia in the era of tyrosine kinase inhibitor therapy. Blood. 2016;127(22):2742–50.
Thompson PA, Kantarjian HM, Cortes JE. Diagnosis and treatment of chronic myeloid leukemia in 2015. Mayo Clin Proc. 2015;90(10):1440–54.
Vinhas R, et al. Current trends in molecular diagnostics of chronic myeloid leukemia. Leuk Lymphoma. 2017;58(8):1791–804.
Baxter EJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365(9464):1054–61.
Kralovics R, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352(17):1779–90.
Pietra D, et al. Somatic mutations of JAK2 exon 12 in patients with JAK2 (V617F)-negative myeloproliferative disorders. Blood. 2008;111(3):1686–9.
Michiels JJ, et al. 2016 WHO clinical molecular and pathological criteria for classification and staging of Myeloproliferative neoplasms (MPN) caused by MPN driver mutations in the JAK2, MPL and CALR genes in the context of new 2016 WHO classification: prognostic and therapeutic implications. Maedica. 2016;11(1):5–25.
Tefferi A, et al. CALR vs JAK2 vs MPL-mutated or triple-negative myelofibrosis: clinical, cytogenetic and molecular comparisons. Leukemia. 2014;28(7):1472–7.
Barbui T, et al. The 2016 revision of WHO classification of myeloproliferative neoplasms: clinical and molecular advances. Blood Rev. 2016;30(6):453–9.
Lundberg P, et al. Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Blood. 2014;123(14):2220–8.
Vannucchi AM, et al. Mutations and prognosis in primary myelofibrosis. Leukemia. 2013;27(9):1861–9.
Guglielmelli P, et al. The number of prognostically detrimental mutations and prognosis in primary myelofibrosis: an international study of 797 patients. Leukemia. 2014;28(9):1804–10.
Swerdlow SH, Campo E, Harris N, Jaffe E, Pileri S, Stein H. WHO classification of tumours of haematopoietic and lymphoid tissues, vol. 2. 4th ed; IRAC: Lyon 2017.
Pardanani A, et al. CSF3R T618I is a highly prevalent and specific mutation in chronic neutrophilic leukemia. Leukemia. 2013;27(9):1870–3.
Szuber N, Tefferi A. Chronic neutrophilic leukemia: new science and new diagnostic criteria. Blood Cancer J. 2018;8(2):19.
Maxson JE, et al. Oncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. N Engl J Med. 2013;368(19):1781–90.
Arber DA, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Elliott MA, Tefferi A. Chronic neutrophilic leukemia: 2018 update on diagnosis, molecular genetics and management. Am J Hematol. 2018;93(4):578–87.
Fleischman AG, et al. The CSF3R T618I mutation causes a lethal neutrophilic neoplasia in mice that is responsive to therapeutic JAK inhibition. Blood. 2013;122(22):3628–31.
Valent P, Akin C, Metcalfe DD. Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts. Blood. 2017;129(11):1420–7.
Pardanani A. Systemic mastocytosis in adults: 2019 update on diagnosis, risk stratification and management. Am J Hematol. 2019;94(3):363–77.
Wilson TM, et al. Clonal analysis of NRAS activating mutations in KIT-D816V systemic mastocytosis. Haematologica. 2011;96(3):459–63.
Traina F, et al. Single nucleotide polymorphism array lesions, TET2, DNMT3A, ASXL1 and CBL mutations are present in systemic mastocytosis. PLoS One. 2012;7(8):e43090.
Schwaab J, et al. Comprehensive mutational profiling in advanced systemic mastocytosis. Blood. 2013;122(14):2460–6.
Reiter A, Gotlib J. Myeloid neoplasms with eosinophilia. Blood. 2017;129(6):704–14.
Gotlib J. World Health Organization-defined eosinophilic disorders: 2017 update on diagnosis, risk stratification, and management. Am J Hematol. 2017;92(11):1243–59.
Vardiman JW. The World Health Organization (WHO) classification of tumors of the hematopoietic and lymphoid tissues: an overview with emphasis on the myeloid neoplasms. Chem Biol Interact. 2010;184(1–2):16–20.
Gotlib J, et al. The FIP1L1-PDGFRalpha fusion tyrosine kinase in hypereosinophilic syndrome and chronic eosinophilic leukemia: implications for diagnosis, classification, and management. Blood. 2004;103(8):2879–91.
Cools J, et al. A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med. 2003;348(13):1201–14.
Schwaab J, et al. Diagnostic challenges in the work up of hypereosinophilia: pitfalls in bone marrow core biopsy interpretation. Ann Hematol. 2016;95(4):557–62.
Metzgeroth G, et al. Recurrent finding of the FIP1L1-PDGFRA fusion gene in eosinophilia-associated acute myeloid leukemia and lymphoblastic T-cell lymphoma. Leukemia. 2007;21(6):1183–8.
Patnaik MM, et al. Chronic myelomonocytic leukaemia: a concise clinical and pathophysiological review. Br J Haematol. 2014;165(3):273–86.
Such E, et al. Cytogenetic risk stratification in chronic myelomonocytic leukemia. Haematologica. 2011;96(3):375–83.
Cervera N, et al. Gene mutations differently impact the prognosis of the myelodysplastic and myeloproliferative classes of chronic myelomonocytic leukemia. Am J Hematol. 2014;89(6):604–9.
Damm F, et al. BCOR and BCORL1 mutations in myelodysplastic syndromes and related disorders. Blood. 2013;122(18):3169–77.
Daver N, et al. FLT3 mutations in myelodysplastic syndrome and chronic myelomonocytic leukemia. Am J Hematol. 2013;88(1):56–9.
Ernst T, et al. Transcription factor mutations in myelodysplastic/myeloproliferative neoplasms. Haematologica. 2010;95(9):1473–80.
Gelsi-Boyer V, et al. Genome profiling of chronic myelomonocytic leukemia: frequent alterations of RAS and RUNX1 genes. BMC Cancer. 2008;8:299.
Grossmann V, et al. Molecular profiling of chronic myelomonocytic leukemia reveals diverse mutations in >80% of patients with TET2 and EZH2 being of high prognostic relevance. Leukemia. 2011;25(5):877–9.
Itzykson R, et al. Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oncol. 2013;31(19):2428–36.
Kohlmann A, et al. Next-generation sequencing technology reveals a characteristic pattern of molecular mutations in 72.8% of chronic myelomonocytic leukemia by detecting frequent alterations in TET2, CBL, RAS, and RUNX1. J Clin Oncol. 2010;28(24):3858–65.
Makishima H, et al. Mutations of e3 ubiquitin ligase cbl family members constitute a novel common pathogenic lesion in myeloid malignancies. J Clin Oncol. 2009;27(36):6109–16.
Onida F, et al. Prognostic factors and scoring systems in chronic myelomonocytic leukemia: a retrospective analysis of 213 patients. Blood. 2002;99(3):840–9.
Patnaik MM, et al. Spliceosome mutations involving SRSF2, SF3B1, and U2AF35 in chronic myelomonocytic leukemia: prevalence, clinical correlates, and prognostic relevance. Am J Hematol. 2013;88(3):201–6.
Mughal TI, et al. An international MDS/MPN working Group’s perspective and recommendations on molecular pathogenesis, diagnosis and clinical characterization of myelodysplastic/myeloproliferative neoplasms. Haematologica. 2015;100(9):1117–30.
Padron E, et al. An international data set for CMML validates prognostic scoring systems and demonstrates a need for novel prognostication strategies. Blood Cancer J. 2015;5:e333.
Tang G, et al. Cytogenetic risk stratification of 417 patients with chronic myelomonocytic leukemia from a single institution. Am J Hematol. 2014;89(8):813–8.
Patnaik MM, et al. ASXL1 and SETBP1 mutations and their prognostic contribution in chronic myelomonocytic leukemia: a two-center study of 466 patients. Leukemia. 2014;28(11):2206–12.
Wassie EA, et al. Molecular and prognostic correlates of cytogenetic abnormalities in chronic myelomonocytic leukemia: a Mayo Clinic-French consortium study. Am J Hematol. 2014;89(12):1111–5.
Elena C, et al. Integrating clinical features and genetic lesions in the risk assessment of patients with chronic myelomonocytic leukemia. Blood. 2016;128(10):1408–17.
Laborde RR, et al. SETBP1 mutations in 415 patients with primary myelofibrosis or chronic myelomonocytic leukemia: independent prognostic impact in CMML. Leukemia. 2013;27(10):2100–2.
Peng J, et al. Chronic myelomonocytic leukemia with nucleophosmin (NPM1) mutation. Eur J Haematol. 2016;96(1):65–71.
Vallapureddy R, et al. Nucleophosmin 1 (NPM1) mutations in chronic myelomonocytic leukemia and their prognostic relevance. Am J Hematol. 2017;92(10):E614–e618.
Ricci C, et al. RAS mutations contribute to evolution of chronic myelomonocytic leukemia to the proliferative variant. Clin Cancer Res. 2010;16(8):2246–56.
Tanaka TN, Bejar R. MDS overlap disorders and diagnostic boundaries. Blood. 2019;133(10):1086–95.
Abdel-Wahab O, et al. Concomitant analysis of EZH2 and ASXL1 mutations in myelofibrosis, chronic myelomonocytic leukemia and blast-phase myeloproliferative neoplasms. Leukemia. 2011;25(7):1200–2.
Hernandez JM, et al. Clinical, hematological and cytogenetic characteristics of atypical chronic myeloid leukemia. Ann Oncol. 2000;11(4):441–4.
Talati C, Padron E. An exercise in extrapolation: clinical Management of Atypical CML, MDS/MPN-unclassifiable, and MDS/MPN-RS-T. Curr Hematol Malig Rep. 2016;11(6):425–33.
Wang SA, et al. Atypical chronic myeloid leukemia is clinically distinct from unclassifiable myelodysplastic/myeloproliferative neoplasms. Blood. 2014;123(17):2645–51.
Meggendorfer M, et al. Specific molecular mutation patterns delineate chronic neutrophilic leukemia, atypical chronic myeloid leukemia, and chronic myelomonocytic leukemia. Haematologica. 2014;99(12):e244–6.
Patnaik MM, et al. Targeted next generation sequencing and identification of risk factors in World Health Organization defined atypical chronic myeloid leukemia. Am J Hematol. 2017;92(6):542–8.
Piazza R, et al. Recurrent SETBP1 mutations in atypical chronic myeloid leukemia. Nat Genet. 2013;45(1):18–24.
Kosmider O, et al. Mutation of the colony-stimulating factor-3 receptor gene is a rare event with poor prognosis in chronic myelomonocytic leukemia. Leukemia. 2013;27(9):1946–9.
Trimarchi T, Ntziachristos P, Aifantis I. A new player SETs in myeloid malignancy. Nat Genet. 2013;45(8):846–7.
Makishima H, et al. Somatic SETBP1 mutations in myeloid malignancies. Nat Genet. 2013;45(8):942–6.
Gambacorti-Passerini CB, et al. Recurrent ETNK1 mutations in atypical chronic myeloid leukemia. Blood. 2015;125(3):499–503.
Reiter A, et al. Molecular basis of myelodysplastic/myeloproliferative neoplasms. Haematologica. 2009;94(12):1634–8.
Caye A, et al. Juvenile myelomonocytic leukemia displays mutations in components of the RAS pathway and the PRC2 network. Nat Genet. 2015;47(11):1334–40.
Niemeyer CM. JMML genomics and decisions. Hematology Am Soc Hematol Educ Program. 2018;2018(1):307–12.
Stieglitz E, et al. The genomic landscape of juvenile myelomonocytic leukemia. Nat Genet. 2015;47(11):1326–33.
Murakami N, et al. Integrated molecular profiling of juvenile myelomonocytic leukemia. Blood. 2018;131(14):1576–86.
Niemeyer CM, et al. Chronic myelomonocytic leukemia in childhood: a retrospective analysis of 110 cases. European working group on Myelodysplastic syndromes in childhood (EWOG-MDS). Blood. 1997;89(10):3534–43.
Strullu M, et al. Juvenile myelomonocytic leukaemia and Noonan syndrome. J Med Genet. 2014;51(10):689–97.
Malcovati L, Cazzola M. Refractory anemia with ring sideroblasts. Best Pract Res Clin Haematol. 2013;26(4):377–85.
Papaemmanuil E, et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011;365(15):1384–95.
Malcovati L, et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood. 2015;126(2):233–41.
Ceesay MM, et al. The JAK2 V617F mutation is rare in RARS but common in RARS-T. Leukemia. 2006;20(11):2060–1.
Patnaik MM, Tefferi A. Refractory anemia with ring sideroblasts (RARS) and RARS with thrombocytosis: “2019 update on diagnosis, risk-stratification, and management”. Am J Hematol. 2019;94(4):475–88.
Jeromin S, et al. Refractory anemia with ring sideroblasts and marked thrombocytosis cases harbor mutations in SF3B1 or other spliceosome genes accompanied by JAK2V617F and ASXL1 mutations. Haematologica. 2015;100(4):e125–7.
Visconte V, et al. SF3B1, a splicing factor is frequently mutated in refractory anemia with ring sideroblasts. Leukemia. 2012;26(3):542–5.
Haase D. Cytogenetic features in myelodysplastic syndromes. Ann Hematol. 2008;87(7):515–26.
Shallis RM, Ahmad R, Zeidan AM. The genetic and molecular pathogenesis of myelodysplastic syndromes. Eur J Haematol. 2018;101(3):260–71.
Nagata Y, Maciejewski JP. The functional mechanisms of mutations in myelodysplastic syndrome. Leukemia. 2019;33(12):2779–94.
List A, Ebert BL, Fenaux P. A decade of progress in myelodysplastic syndrome with chromosome 5q deletion. Leukemia. 2018;32(7):1493–9.
Ogawa S. Genetics of MDS. Blood. 2019;133(10):1049–59.
Ribezzo F, et al. Rps14, Csnk1a1 and miRNA145/miRNA146a deficiency cooperate in the clinical phenotype and activation of the innate immune system in the 5q-syndrome. Leukemia. 2019;33(7):1759–72.
McNerney ME, Godley LA, Le Beau MM. Therapy-related myeloid neoplasms: when genetics and environment collide. Nat Rev Cancer. 2017;17(9):513–27.
Lee JH, List A, Sallman DA. Molecular pathogenesis of myelodysplastic syndromes with deletion 5q. Eur J Haematol. 2019;102(3):203–9.
Germing U, et al. Survival, prognostic factors and rates of leukemic transformation in 381 untreated patients with MDS and del(5q): a multicenter study. Leukemia. 2012;26(6):1286–92.
Mallo M, et al. Impact of adjunct cytogenetic abnormalities for prognostic stratification in patients with myelodysplastic syndrome and deletion 5q. Leukemia. 2011;25(1):110–20.
Schanz J, et al. New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol. 2012;30(8):820–9.
Pellagatti A, et al. Whole-exome sequencing in del(5q) myelodysplastic syndromes in transformation to acute myeloid leukemia. Leukemia. 2014;28(5):1148–51.
Jädersten M, et al. TP53 mutations in low-risk myelodysplastic syndromes with del(5q) predict disease progression. J Clin Oncol. 2011;29(15):1971–9.
Gill H, Leung AY, Kwong YL. Molecular and cellular mechanisms of myelodysplastic syndrome: implications on targeted therapy. Int J Mol Sci. 2016;17(4):440.
Papaemmanuil E, et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 2013;122(22):3616–27. quiz 3699
Greenberg PL. Molecular and genetic features of myelodysplastic syndromes. Int J Lab Hematol. 2012;34(3):215–22.
DeZern AE, Malcovati L, Ebert BL. CHIP, CCUS, and other acronyms: definition, implications, and impact on practice. Am Soc Clin Oncol Educ Book. 2019;39:400–10.
Steensma DP, et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126(1):9–16.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Li, J., Zheng, G. (2021). Myeloproliferative Neoplasms, Myelodysplastic/Myeloproliferative Neoplasms, and Myelodysplastic Syndromes. In: Ding, Y., Zhang, L. (eds) Practical Oncologic Molecular Pathology. Practical Anatomic Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-73227-1_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-73227-1_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73226-4
Online ISBN: 978-3-030-73227-1
eBook Packages: MedicineMedicine (R0)