Abstract
Poorly differentiated neuroendocrine neoplasms (G3 NEN) comprehend a wide variety of tumors, ranging from well-differentiated neoplasms with high proliferation index (Ki-67 higher than 25%) (G3 NET) to poorly differentiated carcinomas (NEC). Morphological, biological, and clinical characterization of G3 NEN is, therefore, crucial in order to define the correct diagnosis and subsequently the right treatment choices. Platinum/etoposide-based chemotherapy remains the standard of treatment for advanced NEC with high Ki-67, while the approach in G3 NEN can be challenging and needs further validation and studies to be clearly defined. In G3 NEN (with Ki-67 ranging from 20% to 50%), oxaliplatin- and temozolomide-based chemotherapy demonstrated to be active in first and second line. According to recent data, immunotherapy seems to improve first-line treatment results in lung NEC, while there are not definitive data in extrapulmonary G3 NEN yet. Finally, local treatment and PRRT can have a role even in poorly differentiated NEN, mainly in G3 NET.
As we know, neuroendocrine neoplasms can have a very unpredictable behavior, and the correct treatment choices need to be defined according to literature evidences and in multidisciplinary team.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction and Histopathological Classification and Characteristics
According to the WHO classification, NeuroEndocrine Carcinomas (NEC) are defined as poorly differentiated NeuroEndocrineNeoplasms (NEN) with Ki-67 > 20% and hence G3. Although lately, increasing evidence suggests that G3 NEN are not a homogenous entity and can be further subclassified into biologically different subgroups, according to both morphological and pathological characteristics other than Ki-67 alone. In fact, not all the neoplasms with high Ki-67 levels have histological characteristics of poor differentiation [1].
A separation based on the proliferative index (Ki-67 > 55%) showed to have clinical prognostic and predictive implication: NEC with Ki-67 > 55% has high sensitivity and good response to platinum-based chemotherapy but a poorer prognosis than G3 NEN in the lower proliferative range (20–55%) [2].
Recent data show that morphological differentiation associated with Ki-67 is essential in defining prognostic and pathological subgroups among G3 NEN, and therefore, a separation of well-differentiated G3 NeuroEndocrine Tumors (NET) from poorly differentiated G3 NEC is emerging [3].
The WHO 2017 classification for pancreatic NEN refers to these tumors as NET G3, whose median Ki-67 rate is 30% compared with 70–80% for GastroEnteroPancreatic (GEP) NEC. These neoplasms are different morphologic, molecular, clinical, and prognostic entities if compared to NEC. However, differentiation between the two and the pathological criteria for subdivision in G3 NEN and NEC are not entirely straightforward and are evolving to more precise criteria. Clinically, NET G3 and NEC differ substantially from NET G1–G2. The prognosis is worse: metastatic disease is usually present at diagnosis, and the treatment of metastatic disease is different. NET G3 can have high proliferative index but rarely exceed 50–60%, different response to chemotherapy (low benefit from platinum–etoposide-based chemotherapy, better with oxaliplatin and temozolomide), high expression of SRI, and Chromogranin A (100% vs. 70%) [3].
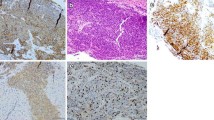
Based on an analysis by Milione et al., new insight in the GEP G3 NEN have been identified, with a median follow-up of 81 months, the median OS was 12.9 months. At multivariate analysis, morphological differentiation, Ki-67 index, MMRd, stage, and CD117 expression were independent prognostic markers in NECs. Three different prognostic categories of NECs were identified according to the degree of morphologic differentiation (well vs. poorly differentiated) and Ki-67 index (<55% vs. ≥55%). On this basis, median OS was 43.6 months in well-differentiated neoplasms with a Ki-67 index 20–55% (named type A), 24.5 months in poorly differentiated neoplasms with a Ki-67 index 20–55% (type B), and 5.3 months (p < 0.0001) in poorly differentiated neoplasms with a Ki-67 index ≥55% (type C) [3].
NET G3 is more frequent in younger patients, primary tumors mostly located in the pancreas (65%), and the disease appears metastatic since the diagnosis in 62–70%, sometimes appearing with functional syndrome (14%) compared to NEC (2%). For pancreatic primaries, the median Ki-67 has been reported in pancreatic NET G3 to be 29–47% (range, 21–80%), compared with pancreatic NEC with a median Ki-67 of 70–80% (range, 21–100%). Also the NET G3 prognosis is better than NEC. The median survival for metastatic patients was 41 months for GEP NET G3 versus 17 months for non–small cell GEP NEC. Several retrospective studies support the prognostic value of histological differentiation.
Till now, classification and diagnosis based on morphologic differentiation alone are challenging. The pathological and biological criteria for subdivision in G3 NEN have not been entirely established yet and are evolving to achieve a standardization.
The ENET Society recommends that a pathology report on GEP NEN G3 should include morphology concerning both differentiation (well-differentiated or poorly differentiated) and small cell versus large cell, as well as proliferation rate as an absolute Ki-67 value [4]. Moreover, it is important to establish histopathological criteria, marking the difference between NET G3 and NEC, because the Ki-67 value alone cannot distinguish between the subgroups. In fact, there is an overlapping of Ki-67 value among NET G3 and NEC, especially in the area of 30–50%, although a Ki-67 of greater than 60% is rare in NET G3 (Table 20.1).
2 Pulmonary Neuroendocrine Poorly Differentiated Neoplasms (LUNG NEN)
2.1 Histopathological Classification and Characteristics
The 2015 WHO classification has grouped the four histologic variants of lung NETs, namely typical carcinoid (TC), atypical carcinoid (AC), large-cell neuroendocrine carcinoma (LCNEC), and small-cell lung carcinoma (SCLC), into a unique box of neuroendocrine (NE) cell proliferations to facilitate their taxonomy and improve diagnostic recognition. Behaviorally, TCs are low-grade tumors with good prognosis. ACs are intermediate-grade tumors with a more aggressive clinical course benefitting from multimodality therapy.
LCNEC and SCLC are high-grade carcinomas with dismal prognosis usually treated by chemoradiotherapy. A grading system independent of histology could prove useful in the setting of a metastatic disease, where morphology alone could not match adequately with the pathologic and clinical grade to support the best therapy choices.
The classification of lung NETs is a process based on cytological and histological features other than the evaluation of mitotic count and necrosis extent. Defining criteria of carcinoids include organoid growth patterns (rosettes, trabeculae, ribbons, festoons, lobular nests, palisading), absent to focal punctate necrosis (not just apoptotic bodies), up to 10 mitoses per mm2.
On the contrary, SCLC and LCNEC are clustered into poorly differentiated tumors, showing trabecular to solid to diffuse growth patterns, extensive necrosis, mitotic count higher than 10 mitoses per mm2 with no upper limits and uneven cell expression for pan-NE markers, especially. LCNEC is a tumor category defined upon pan-NE IHC markers to exclude histological mimics such as LCC-NEM and basaloid carcinoma, or identify non-NE components in combined variants. The diagnosis of SCLC relies primarily upon morphology in both the lung and elsewhere. Ki-67 antigen has been extensively evaluated in lung NET with several diagnostic, prognostic, and grading implications. Although Ki-67 level is not currently accredited in lung NET subtyping due to some overlap of cut-off thresholds among biologically adjacent tumors, its distribution between low- to intermediate-grade and high-grade tumors has made it a very important prognostic and predictive factor. A Ki-67 level up to 20–25% has the highest specificity and sensitivity for low- to intermediate-grade versus high-grade tumors, in the setting of metastatic disease. It is important to note that Ki-67 reflects tumor biology, such an advantage holds particularly true for AC and LCNEC. Not unexpectedly, Ki-67 is typically 5% or less in TC and usually 80% or more in SCLC [5,6,7].
On the basis of actual knowledge, we can identify four different subgroups of lung NETS:
-
1.
First two groups comprehend low and low-to intermediate tumors, with Ki-67 lower than 20–25% (TC with Ki-67 < 5%) and AC and LCNEC with Ki-67 up to 20–25%, with mainly indolent clinical behavior. The second group includes low-to-moderate malignant tumors showing Ki-67 level up to 20–25%, which correspond mostly to AC and even some LCNEC with a molecular profile similar to carcinoids.
-
2.
The third group consists of moderate to higher malignant tumors with Ki-67 level ranging from 25% to 50–60%, biologically corresponding to more uncommon aggressive AC or LCNEC with a molecular profile similar to NSCLC. They can be treated with alkylating drugs or others chemotherapy (such as gemcitabine, paclitaxel, or vinorelbine), but they do not have good response to platinum/etoposide-based chemotherapy.
-
3.
The last group is composed of highly malignant tumors with Ki-67 ranging from 60% to 100%, biologically corresponding to aggressive SCLC and SCLC-like LCNEC on molecular grounds, which should be treated with platinum/etoposide-based chemotherapy and have a very poor prognosis.
2.2 Poorly Differentiated Lung Neuroendocrine Carcinomas NEC (SCLC and LCNEC) Treatment
Even though TNM staging classification has been approved for lung NEC, the old classification, dividing this category into limited stage (LS) and extended stage (ES) disease, remains a gold standard to define treatment strategy.
Lung NEC are characterized by a very aggressive behavior with fast clinical progression and metastatic spread and extremely low survival time in the absence of treatment, with most of the patients diagnosed with advanced disease at diagnosis.
2.2.1 Limited Stage Disease Treatment
2.2.1.1 Radiochemotherapy
Small- and large-cell neuroendocrine tumors of the lung which involve only thoracic organs (lung, nodes, and pleura) are considered limited stage (LS) disease and should undergo multimodal therapy, comprehending chemotherapy and radiotherapy, both sequentially or concomitant. In fact, chemotherapy alone results in poor intrathoracic disease control, with early failures occurring in 75–90% of patients. The addition of thoracic radiotherapy (TRT) to chemotherapy leads to a significantly lower rate of intrathoracic failure, to 30–60%.
In order to address this issue, two meta-analyses were performed [8, 9]. The results from both analyses confirmed that multimodal treatment can reduce risk of death and prolong progression free and overall survival (PFS and OS) over chemotherapy alone.
Platinum and etoposide doublets are the landmark chemotherapy for lung NEC, achieving high response rate (up to 70–80%) even though a rapid progressive disease often occurs after treatment discontinuation or during therapy. Adding radiotherapy (both sequentially and concomitantly) can improve and prolong response rate in limited disease with a reduction in death risk of 14% and prolonging OS and PFS and is considered the gold standard in LS disease.
2.2.1.2 Prophylactic Cranial Irradiation (PCI)
The incidence of central nervous system (CNS) metastases in lung NEC is very high, up to 50% even in limited disease with good response after radiochemotherapy, and is the main cause of disease progression and death. PCI demonstrated to reduce the risk of metastatic spread to the CNS and therefore to increase disease control rate and prolong survival time, with a reduction of relative risk for death of 16% [10].
PCI should be proposed in all patients achieving complete or major response after radiochemotherapy. Recent data support the use of prophylactic brain irradiation even in patients with extended disease, achieving major response after first-line chemotherapy. The factors associated with the recommendation for the use of PCI included the fitness of the patient, young age, and good response to chemotherapy. PCI was recommended by the majority of experts for non-elderly fit patients who had at least a partial response (PR) to chemotherapy [11].
2.2.2 Advanced Stage Disease Treatment
2.2.2.1 First-Line Chemotherapy
Small-cell lung cancer (SCLC) is highly sensitive to first-line chemotherapy, leading to rapid clinical and radiological improvement; unfortunately, this benefit is transient, and relapse is expected either during or shortly after completing chemotherapy. Upon relapse, SCLC is relatively refractory to second-line treatment, and survival with first-line platinum-based chemotherapy rarely exceeds 10 months. Despite this poor outcome, standard first-line therapy has been unchanged in the last three decades with platinum–etoposide combination being the most active treatment and should be considered even in elderly and patients in poor clinical conditions.
Platinum (cisplatin and/or carboplatin) and etoposide combination demonstrated to be very active and has been the standard of care for SCLC since 1990s. A randomized trial published in 1992 [12] confirmed the cisplatin and etoposide combination as the standard of care as first line in advanced SCLC, demonstrating better outcomes than CAV (cyclophosphamide, doxorubicin, and vincristine) with a 8.6 median OS and a 61% partial response (PR) and 10% complete response (CR) rate. Subsequent meta-analyses suggested improved survival with the use of first-line platinum-based regimens compared with other alkylating agents [13].
The next major advance to first-line therapy was the substitution of cisplatin with carboplatin, always in association with etoposide (both iv and oral). This regimen offered a different toxicity profile (higher hematological but lower gastrointestinal, clinical, and neurological toxicity rate) but was not associated with any difference in efficacy. The COCIS meta-analysis compared outcomes with these two platinum agents confirming substantial equivalence between cisplatin and carboplatin in combination with etoposide [14].
With the aim of improving the outcome of first-line therapy, other combinations chemotherapy have been investigated during last decades, with inconclusive and controversial results. The most promising one was cisplatin and irinotecan, although initial promising results in a Japanese phase III trial in comparison with platinum and etoposide, demonstrated higher survival (median OS 12.8 months vs. 9.4 months, p = 0.002) and 1-year survival rate (58.4% vs. 37.3%) [15], further studies failed to confirm this benefit, showing no substantial differences among irinotecan and etoposide in combination with platinum [16]. Although dismal, cisplatin and irinotecan could be considered as an alternative (even if not a new standard of care) to platinum-etoposide combination in first-line treatment of SCLC. Finally, maintenance chemotherapy after completion of first-line treatment did not demonstrate to improve patients’ outcome and should not be considered in advanced lung NEC.
2.2.2.2 Second-Line Chemotherapy
Even if a high response rate is expected from first-line treatment, this result is of short duration, and a rapid disease progression is observed both during and within few months from the end of treatment. Second-line treatment has a very small probability to be active in SCLC, and topotecan is the only approved drug, with CAV (cyclophospamide, doxorubicin, vincristine) being potentially considered as an alternative in case of patients in good clinical conditions. The phase III trial comparing topotecan and best supportive care demonstrated an advantage in term of PFS (25.9 vs. 13 weeks) with topotecan over BSC (best supportive care), with a 7% PR (partial response) and 44% SD (stable disease), and a higher probability of symptoms control [17]. In order to improve this dismal results and define potential alternative, other drugs have been investigating in (irinotecan, paclitaxel, docetaxel), but any of them demonstrated an advantage among topotecan. Other new drugs have been compared with topotecan, but with disappointing results, for example, amrubicin and cabazitaxel did not show any advantage over topotecan in phase III trials. Prognostic and predictive factors for second-line topotecan activity are clinical conditions, LDH levels, and time to progression after first-line chemotherapy (when >90 days it was associated with better outcome). Finally in some cases, platinum/etoposide rechallenge could be considered in patients achieving good response to first-line chemotherapy and with a long time to relapse (3–6 months).
2.2.2.3 Immunotherapy
After a decade of failure in improving the results of first-line chemotherapy in SCLC, lately immunotherapy appeared to have partially changed the landscape of lung NEC. Given the founding of high rate of somatic mutations in SCLC immunotherapy was expected to be an effective treatment for SCLC. Phase I and II trials demonstrated promising results with anti-PD1 and PDL1 drugs in terms of survival rate in advanced stage disease in second- and third-line treatments (nivolumab and ipilimumab combination and pembrolizumab).
According to these promising results, concomitant immunotherapy and chemotherapy in first-line setting has been investigated. Despite the combination of cisplatin and etoposide with ipilimumab did not showed any improvement in patients outcome but increased treatment-related toxicity, other immunotherapies (atezolizumab and durvalumab) demonstrated to increase survival when administered with first-line chemotherapy.
The addiction of atezolizumab (anti-PDL1 antibody) to first-line chemotherapy (carboplatin and etoposide) was evaluated in the IMpower 133 [18], a phase I/III trial which included patients with advanced SCLC, who were randomized to receive chemotherapy with atezolizumab or placebo, followed by atezolizumab/placebo maintenance. Atezolizumab improved both PFS (HR 0.77; HR 0.77; 95% CI, 0.63–0.96) and OS, with an improvement from 10.3 months to 12.3 months and a HR of 0.70 (95% CI, 0.54–0.91). Atezolizumab improved the 1-year survival rate from 38.2 to 51.7%. There was no difference in response rate, and no new safety signals were identified.
Other than atezolizumab, durvalumab (an anti-PDL1 antibody) demonstrated to improve results of first-line platinum and etoposide in a phase III trial (CASPIAN) [19] in which we randomly assigned 805 patients to receive chemotherapy alone or in combination with durvalumab or durvalumab and tremelimumab, followed by durvalumab maintenance. The addition of the anti-PDL1 antibody again improved survival, with a median OS of 13 months with durvalumab compared with 10.3 months with chemotherapy. The 1-year survival rate was higher with durvalumab (54% vs. 40%), even in this case, no significant difference in term of PFS and response rate was observed.
These results, even if practice changing, need to be confirmed and further investigated, above all in terms of definition of predictive biomarker of response to define the subgroup of patients who can really benefit from immunotherapy; in fact, until now, PDL1 expression did not serve a predictive role in both study.
3 Extrapulmonary G3 Neuroendocrine Neoplasms
Extrapulmonary G3 NEN are very rare, they mostly arise in gastrointestinal tract (35–55%) with pancreas and colon representing the most frequently primary site followed by stomach and esophagus. They can be both small-cell and large-cell neuroendocrine carcinoma, mainly with high Ki-67% (above 60%) with the exception for primary pancreatic G3 NEN, which have a high Ki-67 level (>55%) in about 30% of cases. Other primary tumor sites are even more infrequent such as prostate, gynecological, and urothelial tract.
Unfortunately, due to the rarity of these tumors, prospective data regarding treatment strategy are lacking, and the consensus on treatment is mainly based upon retrospective data and mutuated from analogous lung NEC (despite potental differences both in terms of biology and treatment response).
On the basis of a retrospective analysis on 305 patients diagnosed with gastroenteropancreatic NEC (NORDIC NEC) [3], most extrapulmonary NEC are diagnosed in advanced and metastatic stage (60–65%) and have a poor prognosis. Ki-67% level, which is considered the main prognostic and predictive factor, appears higher than 55% mainly in esophageal and rectal tumor, while it was mainly lower in pancreatic neoplasia (only 33% with Ki-67 higher than 55%). Median OS is about 1–2 months in patients who do not receive oncological treatment and 11 months in patients who undergo chemotherapy.
3.1 Treatment of Extrapulmonary Neuroendocrine Carcinomas
3.1.1 First-Line Chemotherapy
Chemotherapy plays a prominent role in advanced extrapulmonary NEC, compared with their G1–2 counterpart. Median OS is about 11 months, and 1 month for patients receiving chemotherapy or not, respectively. Unfortunately, due to the small number of cases of extrapulmonary NEC, no prospective or randomized data are available in support of chemotherapy, so far the first-line treatment is mutuated from data regarding SCLC. Platinum and etoposide doublets remain the standard of care for extrapulmonary NEC; this is usually given for 4–6 cycles, with a RR (response rate) of 30%, with PFS of 4–5 months and OS of 11 months. As previously mentioned, there is no randomized trial investigating this regimen, but several retrospective studies confirm the efficacy and safety of this approach [20].
According to the NORDIC NEC study [3] response rate after first-line chemotherapy with platinum/etoposide combination was 31%, but it was different according to Ki-67 (higher in Ki-67 > 55% than 21–54%: 42% vs. 15% respectively) suggesting that high Ki-67 index may predict response rate. Patients with lower Ki-67 (<55%) had longer survival than those with higher Ki-67 levels (14 vs. 10 months). On the other side, ORR appears to be indipendent from tumor morphology or chromogranin A staining. Finally, colonic primary tumor had a worst prognosis (8 vs. 15 months) than other tumors.
More recently, retrospective data have been published, and platinum (both cisplatin and carboplatin) and etoposide combination chemotherapy has been confirmed as the standard of treatment, achieving a good response rate (from 40% to 65%), with 11.5 months OS and 6 months PFS. Tumor response was mainly unrelated to primary site, endocrine hyperfunction, or prior therapy experience (Table 20.2).
Another regimen which has been investigated is cisplatin/irinotecan, even in this case mutuated on results observed in phase III study in SCLC, a retrospective study for patients with advanced NECs included patients treated with both cisplatin/etoposide and cisplatin/irinotecan (Table 20.2). The response rate and OS (13 vs. 7 months) was higher in cisplatin/irinotecan arm; however, the difference was not statistically significant due to the imbalance with respect of primary site. Similar results were observed in another study, enrolling both extrapulmonary NEC and NET G3. Cisplatin and irinotecan combination was effective in NEC with a RR of 51% and 8 months median OS, but did not show any activity in NET G3 (no partial response observed, with a median OS of 5.4 months) meaning that while the combination of cisplatin and irinotecan may have activity in patients with poorly differentiated neuroendocrine tumors, it has little or no activity in patients with well-differentiated histologies.
According to clinical results of NORDIC NEC study, patients with Ki-67 lower than 55% did not have good response to platinum/etoposide (EP) combination (even with a better prognosis), suggesting the use of alternative chemotherapeutic regimen in this subgroup. On the basis of this further subclassification, retrospective data are available, and oxaliplatin- (FOLFOX or CAPOX) or temozolomide-based treatment can be considered as an alternative to EP in gastroenteropancreatic NEC with Ki-67 < 55% (Table 20.2).
3.1.2 Second-Line Chemotherapy
Evidence for second-line chemotherapy in patients with progressing disease after platinum-etoposide is very limited, and no prospective data are available; therefore, thee is not consensus regarding optimal second-line chemotherapy [20]. Overall response rate (observed in NORDIC NEC study) is quite low (about 18%) even if small retrospective series have documented higher response rate (30–40%, in selected patients), with short benefit and an estimated PFS of 3–4 months and OS lower than 6 months [3].
Actual data regarding second-line chemotherapy mainly derive from retrospective analysis on small number, in fact a low percentage of patients is able to receive further treatment after failure of first-line chemotherapy due to rapid clinical worsening related to tumor aggressiveness.
The most active regimens investigated are FOLFIRI, oxaliplatin-based chemotherapy (FOLFOX and CAPOX) and temozolomide (both alone or in combination with capecitabine). No prospective or randomized data have been available until now, and clinical results are mainly difficult to compare due to the heterogenous population included in these analyses (mainly both G3 NET and NEC).
FOLFIRI showed quite interesting results in retrospective analysis (comprehending both G3 NET and NEC), with 31% response, 31% stable disease with a median PFS of 4 months and 8 months OS (Table 20.3).
Another potential alternative is oxaliplatin-based chemotherapy (FOLFOX or CAPOX) (Table 20.3) which is demonstrated to be effective as second-line chemotherapy with a documented response rate of 20–40% and a median OS up to 6 months.
Finally, temozolomide can have a role in the treatment of progressive disease, both alone and in combination with capecitabine, it has demonstrated encouraging results especially in tumors with Ki-67 lower than 55% (Table 20.3).
Finally, some data are available for biological treatment, with some activities observed for both everolimus and sunitinib in GEP G3 NEN (both NETG3 and NEC), supporting further analysis in order both to confirm these data and to better define the role of these drugs other than identify predictive factors of response (Table 20.3).
Second-line chemotherapy should be considered according to clinical characteristics of patients, performance status, and tumor features. In some cases, platinum/etoposide re-treatment can be considered, in case of prolonged response to first-line chemotherapy (at least 3–6 months relapse free survival).
4 Treatment of Extrapulmonary G3 Neuroendocrine Tumor (NET)
The optimal sequence of treatments for NET G3 remains unclear, as this category has been recently identified. NET G3 is considered a molecularly, radiologically, and prognostically distinct entity compared to NEC and NET G1/G2. Although NET G3 have been treated mainly with platinum-based chemotherapy, retrospective data showed that this treatment has limited effectiveness in this group of neoplasms.
Predictive factors for treatment benefit in NET G3 are scarce, and few prospective studies are available. Much more research is, therefore, needed to aid clinicians selecting the best personalized therapy. Until further data are available, NET G3 treatment choice has to consider several factors: tumor differentiation, tumor stage, primary tumor location, Ki-67 index, and clinical course as well as each patient’s specific features. Again, most chemotherapy studies are a mixture of NET G3 and NEC and specific data on the NET G3 subgroup are few and based on a very small number of patients.
4.1 Chemotherapy
Chemotherapy has a central role in the treatment of advanced NET G3 and should be considered the standard of treatment in first-line setting. Several retrospective data and few prospective trial have been evaluating and investigating the role of chemotherapy and the potentially active drugs [35].
4.1.1 Temozolomide
The role of temozolomide, an alkylating agent, has been defined for advanced well-differentiated G1 and 2 pancreatic NET in multiple studies. It demonstrated to be effective, both as a single agent and in combination with capecitabine in NET G3 (other than G2), the main part of the results being about pancreatic NEN, and some reports about lung NET. The activity of CAPTEM (Capecitabine and Temozolomide) was recently evaluated in NEN G3: NET G3 had a better response compared to NEC group in terms of DCR (70% vs. 30%), PFS (15.3 months vs. 3.3 months), and median OS (22 months vs 4.6 months).
A retrospective Australian study reported the activity of CAPTEM in patients with metastatic NET G2 (66%) and G3 (34%). ORR was 46.9% in the overall population with 15.6% of patients having stable disease. A retrospective multicenter study evaluated the activity of temozolomide-based therapy in patients with G3 NENs, showing a time to treatment failure (TTF) in patients with well-differentiated G3 NETs was 5.8 months, OS and ORR for the same group were 30.1 months and 52%, respectively. The phase II clinical trial (ECOG-ACRIN EA2142) will better help to assess the activity of CAPTEM compared to platinum and etoposide combination in patients with advanced GEP-NEN G3 excluding small-cell histology (Table 20.4).
A number of studies have shown that O6-methylguanine-DNA methyltransferase (MGMT) can be a predictor of temozolomide efficacy in patients with advanced NENs. However, the mechanism behind the association between MGMT and temozolomide is unclear. A lack of MGMT deficiency in patients with NENs, as shown by immunohistochemistry, has been demonstrated in 24–51% of cases, whereas MGMT deficiency in cases of gastrointestinal NENs has not yet been reported. Further studies and clinical trials are required to demonstrate the relationship between MGMT and temozolomide.
Similar reports have been observed even in lung NEN, CAPTEM regimen is associated with a high response rate and a tolerable toxicity profile in lung NENs with 30% patients exhibited a partial response, 55% stable disease, and 10% progressive disease, and promising results in term of PFS and OS (Table 20.4).
4.1.2 Platinum-Based Chemotherapy
In general, first-line treatment for G3 NEC is platinum-based chemotherapy, and multiple retrospective cohorts suggest a low response to platinum-based therapy in NET G3 patients ranging from 0% to 17%. The NORDIC NEC study included patients with GEP NEN G3 treated with platinum-based regimens, demonstrated that G3 NET (Ki-67 <55%) had lower probability of response (even if better survival) compared to NEC with Ki-67 >55%, ORR was 15% vs. 42%, respectively, when treated with platinum/etoposide. According to these data, an alternative treatment should be considered in G3 NET and extrapulmonary NEC with Ki-67 lower than 55%. A retrospective analyses by Fazio et al. suggest that oxaliplatin-based chemotherapy can be active with a manageable safety profile in advanced NETs irrespectively of the primary sites and tumor grade [capecitabine/oxaliplatin (CAPOX), 6% gemcitabine/oxaliplatin (GEMOX), and 29% leucovorin/fluorouracil/oxaliplatin (FOLFOX-6)] [39]. Similar results have been observed in a study by Bajetta et al., which demonstrated activity of oxaliplatin and capecitabine combination in G3 NET with a 30% DCR (23% PR and 7% SD) in second-line treatment, this study demonstrated a lower activity profile in G1–2 NET and NEC (Table 20.4).
4.2 Biological Treatment
Both everolimus and sunitinib (both alone and in association with somatostatin analog (SSA) are the standard of care in progressive low to intermediate NET. While sunitinib demonstrated survival advantage only in pancreatic NET, everolimus is the standard of care in low to intermediate NET of pancreatic, lung, and non-functioning gastrointestinal origin. Some activity evidences have been shown for both drugs in G3 NET and NEC.
Everolimus: Actually, we only have some case reports, and a retrospective study about everolimus activity in NET G3. An Italian study included patients with advanced pancreatic NET G3 with a Ki-67 of 55% or less (median, 30%); everolimus was given mainly after first-line treatment. Median PFS was 6 months and OS was 28 months; 40% had disease stabilization for at least 12 months [33, 34].
Sunitinib seems to show activity also in NET G3. Mainly two studies have evaluated the activity of sunitinib in NEN G3 after progression to chemotherapy. In an open-label phase II, non-randomized prospective trial, 31 patients with GEP-NEN G3 (six patients with NET G3 were included) mainly pretreated with chemotherapy, received sunitinib. Among 31 patients, DCR was 58% while ORR was detected in 12.9%. There was no correlation between tumor differentiation and response to therapy.
In a larger retrospective study, 60 patients with pancreatic NEN treated with sunitinib ORR (in the overall population) was 33.3% with 48.3% stable disease; while G3 NET patient ORR was 60% and 30% SD; PFS in NET G3 was similar to well-differentiated NET (but PFS data was not statistically significant). Otherwise, NEC G3 had a worse prognosis and no response to sunitinib [32] (Table 20.4).
5 Immunotherapy in GEP G3 NEN
Immunotherapy has demonstrated to be active and improved patients’ survival in combination with first-line chemotherapy in SCLC. Evidence points to an important role of immune phenomena in the pathogenesis and treatment of NENS, and the presence of inflammatory infiltrated can be considered a poor prognostic factor. Even if still lacking, some evidences showed PDL1 expression in metastatic gastroenteropancreatic (GEP)-NENs, in particular in high-grade tumors, poorly differentiated NENs, and GEP-NECs. Furthermore, PD-1 and its ligands appear to be also expressed in well-differentiated intestinal and pancreatic NETs. This molecular and genetic profile could explain potential activity of immune check-point inhibitors in GEP G3 NEN [40].
Currently, there are only preliminary data on the effects of immune checkpoint inhibition from controlled trials in GEP NEN patients. Actual data regards mainly pembrolizumab which did not demonstrate high response rate, but a good percentage of disease control in G1–2 NET. Even the association of pembrolizumab with platinum containing chemotherapy in NEN G3 resulted in low response rate. Interesting and promising data derive from the DART trial [43]: the combination of immunotherapy with ipilimumab and nivolumab in the treatment of NEN G3 resulted in a 44% of ORR in NEN G3.
Although NEN G3 has high mutational burden, making them potential target for immune checkpoint inhibitors, the role of immunotherapy still remains unclear ant its role is a is currently evaluated in several phase II studies (Table 20.5).
6 Locoregional Therapy
Very little is known about the role of regional therapy such as surgery, radiation, ablative therapy, and embolotherapy in patients with G3 NEN. The treatment recommendation for patients with apparently localized disease is not based on prospective data, and supporting evidence from heterogenous studies is limited [3, 20]. Curative surgery is usually attempted in localized disease, although retrospective series indicate that it is rarely curative as a sole therapeutic modality. There is expert consensus that surgery alone is rarely curative and that patients with limited disease should probably receive multimodality-based treatment. Surgery, as a part of the treatment, can be curative in patients with localized disease even with regional nodal metastasis; however, retrospective data often do not distinguish between NET G3 and NEC G3. The 5-year survival for localized disease depends of the primary tumor site: 40–50% for colorectal, gastric, and pancreatic neoplasms and 25% for anal and esophageal primaries. Surgery as a part of the treatment should be considered for all localized GEP NEC with the exception for esophageal cancer [20].
Until more data become available, the locoregional approach for G3 NET should follow the treatment paradigms for NET G2 and intended curative resection/ablation suggest a survival benefit, especially in tumors with a Ki-67 less than 55%. Retrospective analysis showed a trend toward a better survival in patients with colorectal and pancreatic NEC who underwent primary tumor resection, in a multimodal approach (comprehending chemotherapy and radiotherapy) [44, 45].
In pancreatic NET G3, resection of primary tumor seems to be associated with better survival than chemotherapy alone, although debulking surgery cannot be recommended in NEC because of the tumor aggressiveness and the absence of clear benefit from retrospective data. An Italian retrospective analysis suggests that surgery with radical intent could be discussed in pancreatic G3 NEN, even though a better survival was observed in patients with Ki-67 lower than 55% and G3 NET. Given the high relapse rate observed after radical surgery, most clinicians would advocate platinum-based adjuvant therapy in this setting, while some authors propose neoadjuvant chemotherapy followed by definitive surgery, although data to support this approach are scarce [20].
In patients with important comorbidities or where the tumor’s anatomical site makes surgical resection not advisable due to high morbidity (i.e., esophagus), a definitive course of radiotherapy and chemotherapy is a reasonable treatment strategy. Debulking and locoregional treatment for liver metastasis are not recommended and also discouraged in poorly differentiated NEC.
7 Peptide Receptor Radionuclide Therapy (PRRT)
Peptide receptor radionuclide therapy (PRRT) delivers highly localized radiation by targeting specific somatostatin receptors on tumor cells. PRRT is comprised of three main components: a high activity radionuclide (177Lutetium or 90Yttrium), linked via a chelator (DTPA or DOTA) to a somatostatin receptor (SSR)-binding ligand which is typically a somatostatin analog (octreotide or octreotate). PRRT has been approved for somatostatin-positive GEP-NETs after failure of previous therapy, according to the results of NETTER 1 phase III trial, which did not include G3 NET [46].
Peptide receptor radionuclide therapy (PRRT) has previously not been recommended for GEP NEN G3 due to the assumption that these tumors lacked SSR expression, and the growth rate was too rapid to expect any benefit from PRRT. However, several retrospective studies have shown that high-grade tumors can display a high tumor SSR expression, and these patients seem to benefit from PRRT [29]. Last evidences demonstrate that NET G3 can have somatostatin receptor expression (87–92% positive on SRI), so PRRT could be a potential therapeutic option in these patients. SRI positivity has been reported for both NET G3 and NEC, and expression of somatostatin receptor 2A has been shown with immunohistochemistry.
According to these evidences, some studies evaluated PRRT in progressive G3 NEN [47, 48], demonstrating interesting activity profile, which need to be further confirmed. The larger one included 149 patients with progressive disease NEN G3. Results from these studies are mainly based on patients with pancreatic primary NET G3 or low NEC (Ki-67 <55%). However, the PFS and OS seem impressive as second- and third-line therapies, especially for the NET G3 and low NEC group (40% PR and 38% SD, with median OS of 44 and 19 months in NEN G3 and low NEC, respectively). For NEN G3 with a Ki-67 <55% and specifically the low NEC subgroup, available data suggest a possible substantial benefit of PRRT. The outcomes of PRRT in GEP NEN G3 with a Ki-67 >55% are based on limited number of cases, and a possible benefit is therefore difficult to assess, additionally response rate was similar between NEC and G3 NET (40–50%), the duration of response was limited in NEC with frequent immediate progression. Another potential option is the combination of PRRT and chemotherapy in NEN G3, several studies have used concomitant chemotherapy including infusional 5FU, oral capecitabine or capecitabine and temozolomide with favorable responses and acceptable toxicity for patients with metastatic NEN.
Pending further research such as NETTER 2 (https://clinicaltrials.gov/ct2/show/NCT03972488) investigating the role of PRRT in high grade G2 and G3 NEN with Ki-67 <55% is warranted to define the effective role of PRRT in G3 NEN. Up to now PRRT for high-grade GEP NEN with a high uptake on SRI showed promising response rates, disease control rates, progression-free survival, and overall survival. Until further data are available, PRRT could be considered for all NET G3 cases and NEC cases with a Ki-67 21–55% with high uptake on SRI even if it cannot be considered a standard of care yet. The crucial clinical questions are to decide which NEN G3 patients should be offered PRRT and when it should be used. ENETS guidelines recommend that PRRT can be considered in SRI-positive NET G3 [20], with Ki-67 <55% and could be discussed in NEC with SRI, whereas the National Comprehensive Cancer Network (NCCN) recommend only the use of PRRT in GEP NEN when Ki-67 is ≤20%.
References
Lloyd RVOR, et al. WHO classification of tumours of endocrine organs (World Health Organization classification of tumors). 4th ed. IARC Press; 2017.
Sørbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, Dueland S, Hofsli E, Guren MG, Ohrling K, Birkemeyer E, Thiis-Evensen E, Biagini M, Gronbaek H, Soveru LM, Olsen IH, Federspiel B, Assmus J, Janson ET, Knigge U. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3); the NORDIC NEC study. Ann Oncol. 2013;24(1):152–60.
Milione M, Maisonneuve P, Spada F, Pellegrinelli A, SPaggiari P, Albarello L, Pisa E, Barberis M, Vanoli A, Buzzoni R, Pusceddu S, Concas L, Sessa F, Solcia E, Capella C, Fazio N, La Rosa S. The clinicopathologic heterogeneity of Grade 3 gastroenteropancreatic neuroendocrine neoplasms: morphological differentiation and proliferation identify different prognostic categories. Neuroendocrinology. 2017;104(1):85–93.
Tang LH, Basturk O, Sue JJ, Klimstra DS. A practical approach to the classification of WHO Grade 3 (G3) well-differentiated neuroendocrine tumor (WD-NET) and poorly differentiated neuroendocrine carcinoma (PD-NEC) of the pancreas. Am J Surg Pathol. 2016;40(9):1192–202.
Travis W, Brambilla E, Burke A, et al. WHO classification of tumours of the lung, pleura, thymus and heart (World Health Organization classification of tumours). 4th ed. IARC Press; 2015.
Caplin ME, Baudin E, Ferolla P, Filosso P, Garcia-Yuste M, Oberg K, Pelosi G, Perren A, Rossi RE, Travis WD, ENETS consensus conferend partecipants. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol. 2015;26:1604–20.
Rindi G, Klersy C, Inzani F, Fellegara G, Ampollini L, Ardissoni A, Campanini N, Carbognani N, De Pas TM, Galetta D, Granone PL, Righi L, Rusca M, Spaggiari L, TIseo M, Viale G, Volante M, Papotti M, Pelosi G. Grading the neuroendocrine tumors of the lung: an evidence-based proposal. Endocr Relat Cancer. 2013;21:1–16.
Warde P, Payne D. Does thoracic irradiation improve survival and local control in limited-stage small-cell carcinoma of the lung? A meta-analysis. J Clin Oncol. 1992;10:890–5.
Pignon JP, Arriagada R, Ihde DC, et al. A meta-analysis of thoracic radiotherapy for small-cell lung cancer. N Engl J Med. 1992;327:1618–24.
Aupérin A, Arriagada R, Pignon JP, Le Péchoux C, Gregor A, Stephens RJ, Kristjansen PE, Johnson BE, Ueoka H, Wagner H, Aisner J. Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic cranial irradiation overview collaborative group. N Engl J Med. 1999;341(7):476–84.
Putora PM, Glatzer M, Belderbos J, Besse B, Blackhall F, Califano F, Cappuzzo F, De Marinis F, Dziadziuszko R, Felip E, Faivre Finn C, Früh M, Garrido P, Le Pechoux C, McDonald F, Nestle U, Novello S, O’Brien M, Paz Ares L, Peeter S, Pöttgen C, Ramella S, Reck M, Slotman B, EGC T, Van Houtte P, Wrsteel V, Widder J, Mornex F, De Ruysscher D. Prophylactic cranial irradiation in stage IV small cell lung cancer: selection of patients amongst European IASLC and ESTRO experts. Radiother Oncol. 2019;133:163–6.
Roth BJ, Johnson DH, Einhorn LH, Schacter LP, Cherng NC, Cohen HJ, Crawford J, Randolph JA, Goolow JL, Broun GO, et al. Randomized study of cyclophosphamide, doxorubicin, and vincristine versus etoposide and cisplatin versus alternation of these two regimens in extensive small-cell lung cancer: a phase III trial of the Southeastern Cancer Study Group. J Clin Oncol. 1992;10(2):282–91.
Chute JP, Chen T, Feigal E, Simon R, Johnson BE. Twenty years of phase III trials for patients with extensive-stage small-cell lung cancer: perceptible progress. J Clin Oncol. 1999;17(6):1794–801.
Rossi A, Di Maio M, Chiodini P, Rudd RM, Okamoto H, Skarlos DV, et al. Carboplatin- or cisplatin-based chemotherapy in first-line treatment of small-cell lung cancer: the COCIS meta-analysis of individual patient data. J Clin Oncol. 2012;30(14):1692–8.
Noda K, Nishiwaki Y, Kawahara M, Negoro S, Sugiura T, Yokoyama A, et al. Irinotecan plus cisplatin compared with etoposide plus cisplatin for extensive small-cell lung cancer. N Engl J Med. 2002;346(2):85–91.
Hanna N, Bunn PA Jr, Langer C, Einhorn L, Guthrie T Jr, Beck T, Ansari R, Ellis P, Byrne M, Morrison M, Hariharan S, Wang S, Sandler A. Randomized phase III trial comparing irinotecan/cisplatin with etoposide/cisplatin in patients with previously untreated extensive stage disease small-cell lung cancer. J Clin Oncol. 2006;24(13):2038–43.
O’Brien ME, Ciuleanu TE, Tsekov H, Shpayk Y, Cucevià B, Huhasz G, Thatcher N, Ross GA, Dane GC, Crofts T. Phase III trial comparing supportive care alone with supportive care with oral topotecan in patients with relapsed small-cell lung cancer. J Clin Oncol. 2006;24:5441–7.
Horn L, Mansfield AS, Szczesna A, Havel L, Krzakowski M, Hochmair MJ, Huemer F, Losonczy G, Jhonson ML, Nichio M, Reck M, Mok T, other for the IMpower133 Study Group. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379:2220–9.
Paz-Ares L, DvorkinM CY, Reinmuth N, Hotta K, Trukhin D, Statsenko G, Hochmair MJ, Özgüroğlu M, Ji JH, Voitko O, Poltoratskiy A, Ponce S, Verderame F, Havel L, Bondarenko I, Kazarnowicz A, Losoncdy G, Conev NV, Armstron J, Byrne B, Shire N, Jiang H, Goldman H, CASPIAN investigators. Durvalumab plus platinum-etoposide versus platinum-etoposide in first line treatment of extensive-stage small cell lung cancer (CASPIAN): a randomized, controlled, open-label phase 3 trial. Lancet. 2019;394:1929–39.
Garcia-Carbonero R, Rinke A, Valle JW, Fazio N, Capli M, Gorbounova V, O’Connor J, Eriksson B, Sorbye H, Kulke M, Chen J, Falkerby J, Costa F, de Herer W, Lombard-Bohas C, Pavel M, Anteibes Consensus Conference Participants. ENETS consensus guidelines for the standard of care in neuroendocrine neoplasms: systemic therapy-chemotherapy. Neuroendocrinology. 2017;105(3):281–94.
Moertel CG, Kvols LK, O’Connell MJ, Rubin J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin. Evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer. 1991;68(2):227–32.
Mitry E, Baudin E, Ducreux M, Sabourin JC, Rufié P, Aparico T, Lasser P, Elias D, Duvillard P, Schlumberger M, Rougier P. Treatment of poorly differentiated neuroendocrine tumours with etoposide and cisplatin. Br J Cancer. 1999;81:1351–5.
Frizziero M, Spada F, Lamarca A, Kordatou Z, Barriuso J, Nuttall C, McNamara MG, Hubner RA, Mansoor W, Manoharan P, Fazio N, Valle JW. Carboplatin in combination with oral or intravenous etoposide for extra-pulmonary, poorly-differentiated neuroendocrine carcinomas. Neuroendocrinology. 2019;109:100–12.
Isawa S, Morizane C, Okusaka T, Ueno H, Ikeda M, Kondo S, Tanaka T, Nakachi K, Mitsunaga S, Kojima Y, Hagihara A, Hiroaka N. Cisplatin and etoposide as first-line chemotherapy for poorly differentiated neuroendocrine carcinoma of the hepatobiliary tract and pancreas. Jpn J Clin Oncol. 2010;40(4):313–8.
Du Z, Wang Y, Zhou Y, Wen F, Li Q. First-line irinotecan combined with 5-fluorouracil and leucovorin for high-grade metastatic gastrointestinal neuroendocrine carcinoma. Tumori. 2013;99(1):57–60.
Li J, Lu Z, Li Z, Liu Y, Yang L, Li J, Hang X, Zhou X, Wang X, Gong J, Gao J, Li Y, Shen L. Irinotecan plus cisplatin followed by octreotide long-acting release maintenance treatment in advanced gastroenteropancreatic neuroendocrine carcinoma: IPO-NEC study. Oncotarget. 2017;8:25669–78.
Rogowski W, Wachula E, Gorzelak A, Lebiedzinska A, Sulzyc-Bielicka V, Izycka-Swieszewska E, et al. Capecitabine and temozolomide combination for treatment of high-grade well-differentiated neuroendocrine tumour and poorly-differentiated neuroendocrine carcinoma. Retrospective analysis. Endokrynol Pol. 2019;70(4):313–7.
Bajetta E, Catena L, Procopio G, De Dosso S, Bichiaso E, Ferrari L, Martinetti A, Platania M, Verzoni E, Formisano B, Bajetta R. Are capecitabine and oxaliplatin (XELOX) suitable treatments for progressing low-grade and high-grade neuroendocrine tumours? Cancer Chemother Pharmacol. 2007;59:637–42.
Hentic O, Hammel P, Couvelard A, Rebours V, Zappa M, Palazzo M, Goujon G, Gillet A, Lévy P, Ruszniewski P. FOLFIRI regimen: an effective secondline chemotherapy after failure of etoposide-platinum combination in patients with neuroendocrine carcinomas grade 3. Endocr Relat Cancer. 2012;19:751–7.
Hadoux J, Malka D, Planchard D, Scoazec JY, Caramella C, Guigav J, Boige V, Leboullex S, Burtin P, Berdelou A, Loriot Y, Duvillard Y, Chougnet CN, Déandréis D, Schlumberger M, Borget I, Ducreux M, Baudin E. Post-first-line FOLFOX chemotherapy for grade 3 neuroendocrine carcinoma. Endocr Relat Cancer. 2015;22:289–98.
Welin S, Sorbye H, Sebjornsen S, Knappskog S, Busch C, Oberg S. Clinical effect of temozolomide-based chemotherapy in poorly differentiated endocrine carcinoma after progression on first-line chemotherapy. Cancer. 2011;117:4617–22.
Pellat A, Dreyw C, Couffignal C, Walter T, Lombard-Bohas C, Niccoli P, Seits JF, Hentic O, Andre T, Coriat R, Fauvre S, Zappa M, Rusziewski P, Pote N, Couvelard A, Raymond E. Clinical and biomarker evaluations of sunitinib in patients with grade 3 digestive neuroendocrine neoplasms. Neuroendocrinology. 2018;107(1):24–31.
Okuyama H, Ikeda M, Okusaka T, Furukawa M, Hosokawa A, Kojima Y, Hara H, Murohisa G, Shioji K, Asagi A, Mizuno N, Kojima M, Yamanaka T, Furuse J. A phase II trial of everolimus in patients with advanced pancreatic neuroendocrine carcinoma refractory or intolerant to platinum-containing chemotherapy (NECTOR trial). Neuroendocrinology. 2020;110(11–12):988–93.
Panzuto F, Rinzivillo M, Spada F, Antonuzzo L, Ibrahim T, Campana A, Fazio N, Delle Fave G. Everolimus in pancreatic neuroendocrine carcinoma G3. Pancreas. 2017;46(3):402–5.
Chan D, Singh S. Current chemotherapy use in neuroendocrine tumors. Endocrinol Metab Clin N Am. 2018;47:603–14.
Chan D, Bergsland EK, Chan JA, Gadgil R, Halfdanarson R, Horbaker K, Kelly V, Kunz PL, McGarrah PW, Raj NP, Reidy DL, Thawer A, Whitman LJ, Wu L, Singh S. Temozolomide in grade III neuroendocrine neoplasms (G3 NENs): a multicenter retrospective review. J Clin Oncol. 2019;37(suppl):321.
Sahu A, Jeffors M, Lai-Kwon J, Thai A, Hicks RJ, Micheal M. CAPTEM in metastatic well-differentiated intermediate to high grade neuroendocrine tumors: a single centre experience. J Oncol. 2019;2019:9032753.
Thomas K, Voros BA, Meadows-Taylor M, Smeltzer MP, Gri R, Boudreaux JP, Thiagarajan R, Woltering EA, Ramirez RA. Outcomes of capecitabine and temozolomide (CAPTEM) in advanced neuroendocrine neoplasms (NENs). Cancers. 2020;12:206.
Spada F, Antonuzzo L, Marconcini R, Radice D, Antonuzzo A, Ricci S, Di Costanza D, Fontana A, Gelsomino F, Luppi G, Nobili E, Galdy S, Cella CA, Sonzogni A, Pisa E, Barberis M, Fazio N. Oxaliplatin-based chemotherapy in advanced neuroendocrine tumors: clinical outcomes and preliminary correlation with biological factors. Neuroendocrinology. 2016;103(6):806–14.
Weber M, Fottner C. Immune checkpoint inhibitors in the treatment of patients with neuroendocrine neoplasia. Oncol Res Treat. 2018;41:306–12.
Mehnert JM, Rugo HS, O’Neil BH, Santoro A, Schellens JHM, Cohen RB, Doi T, Ott PA, Pishvaian MJ, Puzanov I, Aung KL, Hsu C, Le Tourneau C, Soria JC, Élez E, Tamura K, Gould M, Zaho G, Stein K, Piha-Paul SA. Pembrolizumab for patients with PD-L1-positive advanced carcinoids or pancreatic neuroendocrine tumors: results from the KEYNOTE-028 study. J Clin Oncol. 2017;28(suppl 5):abstr 4270.
Vijayvergia N, et al. Pembrolizumab monotherapy in patients with previously treated metastatic high-grade neuroendocrine neoplasms: joint analysis of two prospective, non-randomised trials. Br J Cancer. 2020;122(9):1309–14.
Patel SP, Othus M, Chae YW, Giles FJ, Hansel DE, Singh PP, Fontaine A, Shah MH, Kasi A, Al Baghdadi T, Matrana M, Gatalica Z, Korn WM, Hayward J, McLeod C, Chen HX, Sharon E, Maerson E, Ryan CW, Plets M, Blanke CD, Zurzrock R. A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors (DART SWOG 1609) in patients with nonpancreatic neuroendocrine tumors. Clin Cancer Res. 2020;26(10):2290–6.
Galleberg RB, Knigge U, Tiensuu Janson E, Vestermark LW, Haugvik SP, Ladekarl M, Langer SW, Grønbæk H, Osterlund P, Hjortland GO, Assmus J, Tang J, Tang L, Perren A, Sorbye H. Results after surgical treatment of liver metastases in patients with highgrade gastroenteropancreatic neuroendocrine carcinomas. Eur J Surg Oncol. 2017;43(9):1682–9.
Fields AC, Lu P, Vierra BM, Hu F, Irani J, Bleday R, Goldberg JE, Nash GM, Melnitchouk N. Survival in patients with high-grade colorectal neuroendocrine carcinomas: the role of surgery and chemotherapy. Ann Surg Oncol. 2019;26:1127–33.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, Mittra E, Kunz PL, Kulke MH, Jacene H, Bushnell D, O’Doriso TM, et al., for the NETTER-1 Trial Investigators. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35.
Sorbye H, Kong G, Grozinsky-Glasberg S. PRRT in high-grade gastroenteropancreatic neuroendocrine neoplasms (WHO G3). Endocr Relat Cancer. 2020;27:R67–77.
Carlsen EA, Fazio N, Granberg D, Grozinsky-Glasberg S, Ahmadzadhfar H, Grana CM, Zandee WT, Cwikla J, Walter MA, Oturai PS, TInke A, Weaver A, Frilling A, Gritti S, Arveshoug AK, Meirovitz A, Knigge U, Sorbye H. Peptide receptor radionuclide therapy in gastroenteropancreatic NEN G3: a multicenter cohort study. Endocr Relat Cancer. 2019;26(2):227–39.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Squadroni, M., Barile, R., Beretta, G. (2021). Therapy in Poorly Differentiated Neuroendocrine Neoplasms (NEN G3). In: Beretta, G., Berruti, A., Bombardieri, E., Fazio, N., Goletti, O. (eds) Neuroendocrine Neoplasia Management. Springer, Cham. https://doi.org/10.1007/978-3-030-72830-4_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-72830-4_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-72829-8
Online ISBN: 978-3-030-72830-4
eBook Packages: MedicineMedicine (R0)