Abstract
National and regional population-based registries are, provided diagnostic accuracy and full coverage of the target population, indispensable tools for epidemiological research. CML registries with a more comprehensive reporting may also provide complementary data on treatment outcome to those obtained from clinical trials. Reports from several European CML registries consistently show a crude annual incidence of 0.7–1.3/100,000, median age at diagnosis of 56–60 years and a male/female ratio of 1.2–1.7. The incidence of CML has been stable over time. Worldwide, variations in the reported incidence of CML may be due to methodological issues, but a true difference between different geographical areas and/or ethnical subgroups cannot be excluded. The prevalence of CML is less well known but has been estimated to 15–20/100,000 inhabitants with a steady increase due to the profound improvement in survival of these patients. In recent population-based studies, CML patients have an overall survival that is comparable to that shown in large clinical trials, though relative survival in patients >70 years is still decreased. The impact of socioeconomic factors and health-care settings related to long-term outcome, a possible increased risk of secondary cancer development and identification of adverse off-target effects related to the continuous administration of tyrosine kinase inhibitors are among areas of ongoing epidemiological research in CML.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
3.1 Population-Based Registries
Important data on cancer epidemiology (e.g. incidence, prevalence, age and sex distribution, overall and relative survival), including trends over time, may be obtained from well-established cancer registries covering either the entire population of a nation [1,2,3] or selected regions with well-defined populations [4,5,6]. In Sweden, the National Cancer Registry was formed already in 1958. All pathologists, cytologists and clinicians are obliged by law to report each occurrence of cancer that they diagnose or treat to this centralised, nationwide registry [7]. In the United States, the SEER registries collect data on all newly diagnosed cancers from a large number of hospitals, including patient demographics from 18 tumour registries, covering approximately 30% of the US population [8].
During the last 10–20 years, in CML and in other haematological cancers, diagnosis specific national or regional population-based registries aiming to collect more detailed data on demographics, baseline patient characteristics as well as on treatment and outcome have been established [9,10,11,12,13,14]. In particular, the British Haematological Malignancy Research Network (HMRN), established in 2004 and operating across 14 hospitals using a single haematopathology laboratory [14], the Dutch CML registry [3] and the national Swedish CML registry, founded in 2002 and covering >95% of all newly diagnosed cases of [13], have generated useful population-based data. At the international level, the European Treatment and Outcome Study (EUTOS) for CML has collected detailed population-based data from adult CML patients diagnosed in 2008–2012 in 20 European countries [15]. In addition to these kinds of population-based registries, epidemiological information on CML and other haematological malignancies may be obtained from national or regional health insurance databases [16,17,18] and from central laboratories receiving all diagnostic samples from a well-defined region [19].
Results from these and other relatively detailed population-based registries with full coverage of the target population are useful sources for epidemiological studies. By reducing the impact of selection on outcome, they may also provide important complementary data on treatment outcome to those obtained from clinical trials [11, 12, 20, 21]. Using such routine care data may also be helpful in evaluating adherence to guidelines and in improving the quality of care, including routines for diagnostics and follow-up [13, 22]. Moreover, useful information could be obtained by cross-linking to other population-based regional or national health care databases [23, 24]. Thus, by linking the Swedish CML registry to National Prescribed Drug Registry and National Patient Registry (information on diagnosis from in-hospital and outpatient doctor visits), important off-target effects following treatment with TKIs, in particular the increased risk of cardiovascular events following second-generation TKIs, have been studied [25].
Obviously, reliability of data from registries claiming to be population-based presupposes complete reporting, diagnostic accuracy, correct coding classification and a well-characterised background population of the registry catchment area(s) [26, 27]. However, delayed reporting, less stringent monitoring (as compared to clinical trials) and no detailed information on treatments are obvious limitations of population-based registries.
3.2 Incidence
3.2.1 Incidence of CML in the Total Adult Population
Published data on the annual incidence of CML varies from as low as 0.4/100,000 persons in some non-Western countries to 1.75/100,000 in the United States [3, 16, 28,29,30,31]. As the incidence of CML increases by age (Fig. 3.1), some of these variations are likely due to significant differences in the age distribution of the investigated population (e.g. Western vs. several non-Western countries) [32]. However, also figures on age-standardised incidence varies between different studies, although most European registries report figures in the range 0.7–1.0/100000 inhabitants (Table 3.1). Interestingly, a report from the EUTOs registry, based on population-based epidemiological data from 2287 patients aged ≥20 years and with cytogenetically confirmed CML diagnosed 2008–2012, showed that the raw incidence of CML varies from 0.69 (Poland) to 1.39 (Italy) per 100,000 persons. Correspondingly, age-standardised incidences varied from 0.70 (Poland, UK, Austria) to 1.28 (Italy) [15].
Methodological factors may explain some of these discrepancies. In particular, inclusion of patients with BCR-ABL-negative myeloproliferative disorders may account for the higher incidence of CML in some registries, such as SEERs reporting an incidence of 1.75/100,000, varying from 1.4 to 2.0 between different regions within the United States [29]. Moreover, incorrectly including referral patients in regional ‘population-based’ registries leads to an overestimation of the incidence. On the other hand, incomplete reporting of new CML cases will result in too low figs [34]. It is also possible that differences in health-care-seeking behaviours and reimbursement systems may lead to underreporting of, in particular, elderly patients in some registries. Several haematological registries have, therefore, made considerable efforts to catch all newly diagnosed cases of CML including those diagnosed at smaller hospitals [13, 31].
Although we hypothesise that the divergences in age-adjusted incidence reported so far are mainly due to methodological issues, a true difference between different geographical areas and/or ethnical subgroups cannot be excluded. Indeed, such differences have been shown in other haematological cancers such as chronic lymphocytic leukaemia and acute promyelocytic leukaemia [35, 36]. In CML, Chen et al., analysing the incidence of CML in different ethnical subgroups within the United States, showed a lower incidence in Asians as compared to Caucasians [29].
3.2.2 Age and Sex Differences
The incidence in CML increases by age, at least up to 75–80 years, with an annual incidence rising from 0.39 in young (20–29 years) to 1.52 in those 70 years or more [15, 37] (Fig. 3.1). According to the EUTOS registry report, the median age at diagnosis of CML in Europe is 56 years, in countries such as Germany and Sweden as high as 61–62 years (Table 3.1). The latter is about 10 years above the median age typically seen in clinical trials [15, 33]. In children, CML is a very rare disease with an incidence as low as 0.6–1.2 million children/year [38].
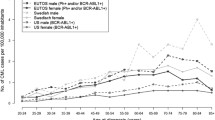
CML is more common in males than in females with male-to-female ratio varying between 1.2 and 1.7 in different studies [3, 13, 39]. The gender difference in incidence is slightly less prominent in younger age groups (Fig. 3.2).
Age-standardised annual incidence (adjusted to WSP) of CML diagnosed in 1970–2010 (n = 4393) (Data are obtained from the Swedish Cancer Registry (www.socialstyrelsen.se/register/halsodataregister/cancerregistret/inenglish). Note that data from 1970s and 1980s may be imprecise due to decentralised haematopathology and in most cases no cytogenetics
3.2.3 Has the Incidence of CML Increased over Time?
In several countries, cancer statistics are available since the 1970s or even earlier. Data from SEERs and the Dutch and Swedish Cancer Registries (Fig. 3.2) give no clear evidence of a change in incidence over time in CML [3, 29, 40]. However, changes in the classification system, the development of more accurate diagnostics by the centralisation of haematopathology to more specialised units and the introduction of cytogenetics make it very difficult to compare present figures on incidence with data from the mid-1980s and earlier.
3.3 Prevalence
Reliable data on the exact prevalence of CML are relatively scarce. In an epidemiological survey from northern France, Corn et al. reported prevalence for 1998, 2003 and 2007, respectively, of 5.8, 6.8 and 7.3 per 100,000 inhabitants. Due to the significant improvement in survival, following the introduction of imatinib and other TKIs [41], as well as the increasing life expectancy in the general population, the prevalence of CML is increasing [18, 42]. Thus, in a study from Sweden, the observed prevalence tripled from 1985 to 2012, from 3.9 to 11.9 per 100,000 inhabitants [43]. Assuming no further improvements in relative survival, the prevalence is projected to further increase to 15 per 100,000 in 2020 and 22.0 per 100,000 inhabitants by 2060 (Fig. 3.3). In the United States, based on an excess annual mortality in CML of 1.53, and an annual incidence of approximately 1/100,000, Huang et al. estimated that the prevalence of CML will increase from approximately 70,000 in 2010 (corresponding to a prevalence of as high as 22/100,000) to 112,000 in 2020 and reach a near plateau of 35 times the annual incidence in 2050 [44]. Obviously, this trend will have profound pharmacoeconomic consequences [45, 46].
3.4 Risk Factors for Developing CML
The aetiology of CML is essentially unknown. Ionising radiation is the only established risk factor, having been linked to CML in atomic bomb survivors [47]. Results from a recent population-based case-control study suggested a weak association between smoking and CML [48], but whether tobacco use actually contributes to the aetiology of the disease is not unambiguous. Nevertheless, smokers seem to have a higher risk of disease progression compared with non-smokers [49]. Results from a study based on data from the Swedish Cancer Registry suggest that patients with CML have a moderately increased prevalence of other malignancies and autoimmune diseases, preceding the diagnosis of CML. These findings suggest that a more general predisposition to cancer and/or immunological mechanisms may be involved in the pathogenesis of CML [43, 50]. As for heredity, two studies based on the Swedish Cancer Registry and Multigeneration Registry were unable to find any significant familial aggregation of CML [51, 52].
3.5 Survival Rates and Non-disease-Related Prognostic Factors
3.5.1 Overall and Relative Survival in the Population-Based Setting
Results from a number of population-based studies have unanimously confirmed the significant improvement in survival in patients with CML diagnosed since the introduction of TKIs at the turn of the century [3, 28, 29, 40, 53]. Previous studies suggested that the survival rate in patients treated within clinical trials, or in large referral centres, was significantly better than that of all patients with CML [54]. However, results from these large population-based studies have shown almost equal figures on survival with that obtained from the more selected materials, with an estimated 5-year overall survival of 85% for patients diagnosed in chronic phase with no difference between males and females [31, 37]. Data from the EUTOS registry, including patients diagnosed in chronic phase and treated outside clinical trials, the 5-year probability of dying because of CML was 3, 4 and 15% depending on the prognostic risk group (ELTS) at diagnosis [55].
A close to normal relative survival over an observation period of more than 10 years has been reported in 1536 patients of CML study IV [56]. This is not only in younger patients since age in the TKI era has a much smaller impact on CML-related death than in the pre-TKI era [57]. Similar observations on relative survival, though in a smaller cohort of patients, have been published by Sasaki [58]. In a study from the Swedish CML registry, relative survival was reported to be close to normal (i.e. 1) in younger CML patients but still reduced in the elderly population (Fig. 3.4). It may be concluded that in countries where TKIs are easily available, most patients with CML diagnosed in chronic phase (CP) have a life expectancy that is not identical but still close to that of the normal population [41, 53]. However, the small group of patients (5–7%) diagnosed in accelerated (AP) or blastic phase (BP) still have a less favourable prognosis (Fig. 3.5) [59].
3.5.2 Age and Comorbidity
Apart from disease-related pre-treatment factors (e.g. stage, Sokal and ELTS scores, aberrant cytogenetics), which are beyond the scope of this overview, several non-disease-related factors might have an impact on the prognosis of CML. Several studies indicate that, even after the introduction of imatinib in 2001–2002, elderly CML patients (>70 years) have an inferior relative survival than younger ones [40, 60, 61]. Several reports show that elderly patients respond equally well as younger patients to treatment with imatinib [62, 63]. Possibly, a time lag in the introduction of imatinib and a persisting underuse TKIs in the elderly CML patients may explain the less impressive improvements in the elderly population [61, 64].
In another publication, based on patients participating in the German CML study IV, comorbidity, as measured by the Charlson comorbidity index [65] and separated from age in the analysis, was associated with worse survival but had no negative impact on response to imatinib [66]. However, comorbidities associated with significant organ failure or cognitive function may lead to lower treatment tolerability and, therefore, indirectly increase the risk of CML-related death [67].
3.5.3 Socioeconomy and CML
Even in economically more developed countries with equal availability to health care resources, socioeconomic factors may have an impact on the prognosis in patients with haematological cancers [68]. In CML, a population-based study from the UK showed that patients living in more deprived areas had poorer outcome in terms of relative survival, as well as a lower chance to obtain MMR, despite treatment with a TKI [31]. The authors speculate that non-adherence to TKI therapy may be the most important factor. However, in a later trial, based on linking the Swedish CML registry to several health databases, the authors concluded that the observed association between socioeconomic variables and survival could rather be explained by pre-treatment factors (e.g. comorbidities) [69].
Previous publications suggested that centralised care of patients with CML is important for achieving results comparable with those of clinical trials [10]. More recently, Lauseker et al., analysing the outcome of 1491 patients included in the German CML study IV, observed a survival advantage for patients treated initially at a teaching hospital compared to those treated in municipal hospitals and by office-based physicians, respectively [70]. The difference remained when adjusted for age, performance status and EUTOS score. Preliminary results from the Dutch registry suggest that patients with CML treated at smaller non-academic hospitals were less frequently monitored by cytogenetic and/or molecular assessments and were less often included in clinical trials [11, 12]. On the other hand, a report from the Swedish CML registry, based on 779 patients, was not able to find any difference in survival between patients living in university versus non-university catchment areas [13]. Apart from methodological issues, it may well be that the relative importance of centralised care in CML differs between countries due to differences in their health-care resources and organisation.
3.6 Do CML Patients Have an Increased Risk to Develop Other Cancers?
Studies on the risk of developing subsequent malignancies (other than MDS or acute leukaemia) after the diagnosis of CML have yielded conflicting results. Thus, in a study based on 1026 patients with CML, diagnosed in 1977–2008 and identified in the Danish Cancer Registry, Frederiksen et al. observed a 1.6-fold increased risk of developing a secondary malignancy as compared to the expected rate in the background population [71]. In a subsequent Swedish registry study, CML patients treated in the TKI era had a 1.5-fold increased risk of developing a secondary cancer as compared to the background population (matched by age, sex, health-care region and calendar year at diagnosis) [43, 50]. The authors speculated that this increased risk is more likely linked to the CML disease itself rather than to its treatment. However, other investigators, analysing different kinds of study populations, have found that patients with CML has only a borderline increased risk of secondary cancers [72] or no increased risk at all [73, 74]. Differences in patient numbers, selection, follow-up time and definition of ‘secondary cancer’ might explain these contradictory findings. Clearly, the question whether CML patients, nowadays mostly living an almost normal life span, have an increased risk of developing other malignancies needs to be further investigated.
References
Socialstyrelsen (The National Board of Health and Welfare), Sweden, 2019. Statistics on Cancer Incidence. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2020-12-7133.pdf
Storm HH, Michelsen EV, Clemmensen IH, Pihl J. The Danish cancer registry--history, content, quality and use. Dan Med Bull. 1997;44(5):535–9.
Thielen N, Visser O, Ossenkoppele G, Janssen J. Chronic myeloid leukemia in the Netherlands: a population-based study on incidence, treatment, and survival in 3585 patients from 1989 to 2012. Eur J Haematol. 2016;97(2):145–54.
Harrison SJ, Johnson PR, Holyoake TL. The Scotland leukaemia registry audit of incidence, diagnosis and clinical management of new patients with chronic myeloid leukaemia in 1999 and 2000. Scott Med J. 2004;49(3):87–90.
Maynadie M, Girodon F, Manivet-Janoray I, Mounier M, Mugneret F, Bailly F, Favre B, Caillot D, Petrella T, Flesch M, Carli PM. Twenty-five years of epidemiological recording on myeloid malignancies: data from the specialized registry of hematologic malignancies of Cote d'Or (Burgundy, France). Haematologica. 2011;96(1):55–61.
Osca-Gelis G, Puig-Vives M, Saez M, Gallardo D, Lloveras N, Marcos-Gragera R. Population-based incidence of myeloid malignancies: fifteen years of epidemiological data in the province of Girona, Spain. Haematologica. 2013;98(8):e95–7.
Barlow L, Westergren K, Holmberg L, Talback M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48(1):27–33.
SEER. SEER cancer statistics review (CSR) 1975–2017 2020.
Corm S, Roche L, Micol JB, Coiteux V, Bossard N, Nicolini FE, Iwaz J, Preudhomme C, Roche-Lestienne C, Facon T, Remontet L. Changes in the dynamics of the excess mortality rate in chronic phase-chronic myeloid leukemia over 1990-2007: a population study. Blood. 2011;118(16):4331–7.
Faber E, Muzik J, Koza V, Demeckova E, Voglova J, Demitrovicova L, Chudej J, Markuljak I, Cmunt E, Kozak T, Tothova E, Jarosova M, Dusek L, Indrak K. Treatment of consecutive patients with chronic myeloid leukaemia in the cooperating centres from the Czech Republic and the whole of Slovakia after 2000--a report from the population-based CAMELIA registry. Eur J Haematol. 2011;87(2):157–68.
Geelen IGP, Thielen N, Janssen J, Hoogendoorn M, Roosma TJA, Willemsen SP, Valk PJM, Visser O, Cornelissen JJ, Westerweel PE. Impact of hospital experience on the quality of tyrosine kinase inhibitor response monitoring and consequence for chronic myeloid leukemia patient survival. Haematologica. 2017a;102(12):e486–9.
Geelen IGP, Thielen N, Janssen J, Hoogendoorn M, Roosma TJA, Willemsen SP, Visser O, Cornelissen JJ, Westerweel PE. Treatment outcome in a population-based, 'real-world' cohort of patients with chronic myeloid leukemia. Haematologica. 2017b;102(11):1842–9.
Hoglund M, Sandin F, Hellstrom K, Bjoreman M, Bjorkholm M, Brune M, Dreimane A, Ekblom M, Lehmann S, Ljungman P, Malm C, Markevarn B, Myhr-Eriksson K, Ohm L, Olsson-Stromberg U, Sjalander A, Wadenvik H, Simonsson B, Stenke L, Richter J. Tyrosine kinase inhibitor usage, treatment outcome, and prognostic scores in CML: report from the population-based Swedish CML registry. Blood. 2013;122(7):1284–92.
Smith A, Roman E, Howell D, Jones R, Patmore R, Jack A, N. Haematological Malignancy Research. The Haematological Malignancy Research Network (HMRN): a new information strategy for population based epidemiology and health service research. Br J Haematol. 2010;148(5):739–53.
Hoffmann VS, Baccarani M, Hasford J, Lindoerfer D, Burgstaller S, Sertic D, Costeas P, Mayer J, Indrak K, Everaus H, Koskenvesa P, Guilhot J, Schubert-Fritschle G, Castagnetti F, Di Raimondo F, Lejniece S, Griskevicius L, Thielen N, Sacha T, Hellmann A, Turkina AG, Zaritskey A, Bogdanovic A, Sninska Z, Zupan I, Steegmann JL, Simonsson B, Clark RE, Covelli A, Guidi G, Hehlmann R. The EUTOS population-based registry: incidence and clinical characteristics of 2904 CML patients in 20 European countries. Leukemia. 2015;29(6):1336–43.
Chang CS, Lee K, Yang YH, Lin MT, Hsu CN. Estimation of CML incidence: disagreement between national cancer registry and health claims data system in Taiwan. Leuk Res. 2011;35(5):e53–4.
Foulon S, Cony-Makhoul P, Guerci-Bresler A, Delord M, Solary E, Monnereau A, Bonastre J, Tubert-Bitter P. Using healthcare claims data to analyze the prevalence of BCR-ABL-positive chronic myeloid leukemia in France: a nationwide population-based study. Cancer Med. 2019;8(6):3296–304.
Lauseker M, Gerlach R, Tauscher M, Hasford J. Improved survival boosts the prevalence of chronic myeloid leukemia: predictions from a population-based study. J Cancer Res Clin Oncol. 2016;142(7):1441–7.
Nguyen LT, Guo M, Naugler C, Rashid-Kolvear F. Incidence of chronic myeloid leukemia in Calgary, Alberta, Canada. BMC Res Notes. 2018;11(1):780.
Castagnetti F, Di Raimondo F, De Vivo A, Spitaleri A, Gugliotta G, Fabbiano F, Capodanno I, Mannina D, Salvucci M, Antolino A, Marasca R, Musso M, Crugnola M, Impera S, Trabacchi E, Musolino C, Cavazzini F, Mineo G, Tosi P, Tomaselli C, Rizzo M, Siragusa S, Fogli M, Ragionieri R, Zironi A, Soverini S, Martinelli G, Cavo M, Vigneri P, Stagno F, Rosti G, Baccarani M. A population-based study of chronic myeloid leukemia patients treated with imatinib in first line. Am J Hematol. 2017;92(1):82–7.
Kurtovic-Kozaric A, Hasic A, Radich JP, Bijedic V, Nefic H, Eminovic I, Kurtovic S, Colakovic F, Kozaric M, Vranic S, Bovan NS. The reality of cancer treatment in a developing country: the effects of delayed TKI treatment on survival, cytogenetic and molecular responses in chronic myeloid leukaemia patients. Br J Haematol. 2015;172:420.
Geelen IGP, Thielen N, Janssen J, Hoogendoorn M, Roosma TJA, Valk PJM, Visser O, Cornelissen JJ, Westerweel PE. Omitting cytogenetic assessment from routine treatment response monitoring in chronic myeloid leukemia is safe. Eur J Haematol. 2018;100(4):367–71.
Berglund A, Holmberg L, Tishelman C, Wagenius G, Eaker S, Lambe M. Social inequalities in non-small cell lung cancer management and survival: a population-based study in Central Sweden. Thorax. 2010;65(4):327–33.
Gunnarsson N, Hoglund M, Stenke L, Wallberg-Jonsson S, Sandin F, Bjorkholm M, Dreimane A, Lambe M, Markevarn B, Olsson-Stromberg U, Wadenvik H, Richter J, Sjalander A. Increased prevalence of prior malignancies and autoimmune diseases in patients diagnosed with chronic myeloid leukemia. Leukemia. 2016;30(7):1562–7.
Dahlen T, Edgren G, Lambe M, Hoglund M, Bjorkholm M, Sandin F, Sjalander A, Richter J, Olsson-Stromberg U, Ohm L, Back M, Stenke L, Swedish CMLG, C. M. L. R. G. the Swedish. Cardiovascular events associated with use of tyrosine kinase inhibitors in chronic myeloid Leukemia: a population-based cohort study. Ann Intern Med. 2016;165(3):161–6.
Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45(5):747–55.
Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods part II. Completeness. Eur J Cancer. 2009;45(5):756–64.
Beinortas T, Tavoriene I, Zvirblis T, Gerbutavicius R, Jurgutis M, Griskevicius L. Chronic myeloid leukemia incidence, survival and accessibility of tyrosine kinase inhibitors: a report from population-based Lithuanian haematological disease registry 2000-2013. BMC Cancer. 2016;16:198.
Chen Y, Wang H, Kantarjian H, Cortes J. Trends in chronic myeloid leukemia incidence and survival in the United States from 1975 to 2009. Leuk Lymphoma. 2013;54(7):1411–7.
Rohrbacher M, Hasford J. Epidemiology of chronic myeloid leukaemia (CML). Best Pract Res Clin Haematol. 2009;22(3):295–302.
Smith AG, Painter D, Howell DA, Evans P, Smith G, Patmore R, Jack A, Roman E. Determinants of survival in patients with chronic myeloid leukaemia treated in the new era of oral therapy: findings from a UK population-based patient cohort. BMJ Open. 2014;4(1):e004266.
Mendizabal AM, Younes N, Levine PH. Geographic and income variations in age at diagnosis and incidence of chronic myeloid leukemia. Int J Hematol. 2016;103(1):70–8.
Rohrbacher M, Berger U, Hochhaus A, Metzgeroth G, Adam K, Lahaye T, Saussele S, Muller MC, Hasford J, Heimpel H, Hehlmann R. Clinical trials underestimate the age of chronic myeloid leukemia (CML) patients. Incidence and median age of Ph/BCR-ABL-positive CML and other chronic myeloproliferative disorders in a representative area in Germany. Leukemia. 2009;23(3):602–4.
McQuilten ZK, Wood EM, Polizzotto MN, Campbell LJ, Wall M, Curtis DJ, Farrugia H, McNeil JJ, Sundararajan V. Underestimation of myelodysplastic syndrome incidence by cancer registries: results from a population-based data linkage study. Cancer. 2014;120(11):1686–94.
Gale RP, Cozen W, Goodman MT, Wang FF, Bernstein L. Decreased chronic lymphocytic leukemia incidence in Asians in Los Angeles County. Leuk Res. 2000;24(8):665–9.
Matasar MJ, Ritchie EK, Consedine N, Magai C, Neugut AI. Incidence rates of the major leukemia subtypes among US Hispanics, Blacks, and non-Hispanic Whites. Leuk Lymphoma. 2006;47(11):2365–70.
Hoglund M, Sandin F, Simonsson B. Epidemiology of chronic myeloid leukaemia: an update. Ann Hematol. 2015;94(Suppl 2):S241–7.
de la Fuente J, Baruchel A, Biondi A, de Bont E, Dresse MF, Suttorp M, Millot F, B. F. M. G. S. G. C. M. L. C. International. Managing children with chronic myeloid leukaemia (CML): recommendations for the management of CML in children and young people up to the age of 18 years. Br J Haematol. 2014;167(1):33–47.
Radivoyevitch T, Jankovic GM, Tiu RV, Saunthararajah Y, Jackson RC, Hlatky LR, Gale RP, Sachs RK. Sex differences in the incidence of chronic myeloid leukemia. Radiat Environ Biophys. 2014;53(1):55–63.
Bjorkholm M, Ohm L, Eloranta S, Derolf A, Hultcrantz M, Sjoberg J, Andersson T, Hoglund M, Richter J, Landgren O, Kristinsson SY, Dickman PW. Success story of targeted therapy in chronic myeloid leukemia: a population-based study of patients diagnosed in Sweden from 1973 to 2008. J Clin Oncol. 2011;29(18):2514–20.
Bower H, Bjorkholm M, Dickman PW, Hoglund M, Lambert PC, Andersson TM. Life expectancy of patients with chronic myeloid Leukemia approaches the life expectancy of the general population. J Clin Oncol. 2016;34(24):2851–7.
Delord M, Foulon S, Cayuela JM, Rousselot P, Bonastre J. The rising prevalence of chronic myeloid leukemia in France. Leuk Res. 2018;69:94–9.
Gunnarsson N, Hoglund M, Stenke L, Wallberg Jonsson S, Sandin F, Bjorkholm M, Dreimane A, Lambe M, Markevarn B, Olsson-Stromberg U, Wadenvik H, Richter J, Sjalander A. Increased prevalence of prior malignancies and autoimmune diseases in patients diagnosed with chronic myeloid Leukemia. Blood. 2015a;126(23):1586.
Huang X, Cortes J, Kantarjian H. Estimations of the increasing prevalence and plateau prevalence of chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Cancer. 2012;118(12):3123–7.
Kantarjian HM, Fojo T, Mathisen M, Zwelling LA. Cancer drugs in the United States: Justum Pretium--the just price. J Clin Oncol. 2013;31(28):3600–4.
Ohm L, Lundqvist A, Dickman P, Hoglund M, Persson U, Stenke L, Carlsson KS, Bjorkholm M. Real-world cost-effectiveness in chronic myeloid leukemia: the price of success during four decades of development from non-targeted treatment to imatinib. Leuk Lymphoma. 2015;56(5):1385–91.
Heyssel R, Brill B, Woodbury LA, Nishimura ET, Ghose T, Hishino T, Yamasaki M. Leukemia in hiroshima atomic bomb survivors. Blood. 1960;15 (3):313–31.
Musselman JR, Blair CK, Cerhan JR, Nguyen P, Hirsch B, Ross JA. Risk of adult acute and chronic myeloid leukemia with cigarette smoking and cessation. Cancer Epidemiol. 2013;37(4):410–6.
Lauseker M, Hasford J, Saussele S, Kremers S, Kraemer D, Lindemann W, Hehlmann R, Pfirrmann M, German CMLSG. Smokers with chronic myeloid leukemia are at a higher risk of disease progression and premature death. Cancer. 2017;123(13):2467–71.
Gunnarsson N, Stenke L, Hoglund M, Sandin F, Bjorkholm M, Dreimane A, Lambe M, Markevarn B, Olsson-Stromberg U, Richter J, Wadenvik H, Wallvik J, Sjalander A. Second malignancies following treatment of chronic myeloid leukaemia in the tyrosine kinase inhibitor era. Br J Haematol. 2015b;169(5):683–8.
Bjorkholm M, Kristinsson SY, Landgren O, Goldin LR. No familial aggregation in chronic myeloid leukemia. Blood. 2013;122(3):460–1.
Gunnarsson N, Hoglund M, Stenke L, Sandin F, Bjorkholm M, Dreimane A, Lambe M, Markevarn B, Olsson-Stromberg U, Wadenvik H, Richter J, Sjalander A. No increased prevalence of malignancies among first-degree relatives of 800 patients with chronic myeloid leukemia: a population-based study in Sweden. Leukemia. 2017;31(8):1825–7.
Bjorkholm M, Bower H, Dickman PW, Lambert PC, Höglund M, Andersson TM-L. Temporal trends in chronic myeloid Leukemia outcome using the loss in expectation of life: a Swedish population-based study. Blood. 2015;126(23):2779.
Pulte D, Gondos A, Redaniel MT, Brenner H. Survival of patients with chronic myelocytic leukemia: comparisons of estimates from clinical trial settings and population-based cancer registries. Oncologist. 2011;16(5):663–71.
Pfirrmann M, Baccarani M, Saussele S, Guilhot J, Cervantes F, Ossenkoppele G, Hoffmann VS, Castagnetti F, Hasford J, Hehlmann R, Simonsson B. Prognosis of long-term survival considering disease-specific death in patients with chronic myeloid leukemia. Leukemia. 2015;30:48.
Hehlmann R, Lauseker M, Saussele S, Pfirrmann M, Krause S, Kolb HJ, Neubauer A, Hossfeld DK, Nerl C, Gratwohl A, Baerlocher GM, Heim D, Brummendorf TH, Fabarius A, Haferlach C, Schlegelberger B, Muller MC, Jeromin S, Proetel U, Kohlbrenner K, Voskanyan A, Rinaldetti S, Seifarth W, Spiess B, Balleisen L, Goebeler MC, Hanel M, Ho A, Dengler J, Falge C, Kanz L, Kremers S, Burchert A, Kneba M, Stegelmann F, Kohne CA, Lindemann HW, Waller CF, Pfreundschuh M, Spiekermann K, Berdel WE, Muller L, Edinger M, Mayer J, Beelen DW, Bentz M, Link H, Hertenstein B, Fuchs R, Wernli M, Schlegel F, Schlag R, de Wit M, Trumper L, Hebart H, Hahn M, Thomalla J, Scheid C, Schafhausen P, Verbeek W, Eckart MJ, Gassmann W, Pezzutto A, Schenk M, Brossart P, Geer T, Bildat S, Schafer E, Hochhaus A, Hasford J. Assessment of imatinib as first-line treatment of chronic myeloid leukemia: 10-year survival results of the randomized CML study IV and impact of non-CML determinants. Leukemia. 2017;31(11):2398–406.
Pfirrmann M, Baccarani M, Saussele S, Guilhot J, Cervantes F, Ossenkoppele G, Hoffmann VS, Castagnetti F, Hasford J, Hehlmann R, Simonsson B. Prognosis of long-term survival considering disease-specific death in patients with chronic myeloid leukemia. Leukemia. 2016;30(1):48–56.
Sasaki K, Strom SS, O'Brien S, Jabbour E, Ravandi F, Konopleva M, Borthakur G, Pemmaraju N, Daver N, Jain P, Pierce S, Kantarjian H, Cortes JE. Relative survival in patients with chronic-phase chronic myeloid leukaemia in the tyrosine-kinase inhibitor era: analysis of patient data from six prospective clinical trials. Lancet Haematol. 2015;2(5):e186–93.
Soderlund S, Dahlen T, Sandin F, Olsson-Stromberg U, Creignou M, Dreimane A, Lubking A, Markevarn B, Sjalander A, Wadenvik H, Stenke L, Richter J, Hoglund M. Advanced phase chronic myeloid leukaemia (CML) in the tyrosine kinase inhibitor era—a report from the Swedish CML register. Eur J Haematol. 2017;98(1):57–66.
Brunner AM, Campigotto F, Sadrzadeh H, Drapkin BJ, Chen YB, Neuberg DS, Fathi AT. Trends in all-cause mortality among patients with chronic myeloid leukemia: a surveillance, epidemiology, and end results database analysis. Cancer. 2013;119(14):2620–9.
Ector G, Visser O, Westerweel PE, Janssen J, Blijlevens NMA and Dinmohamed AG. Primary therapy and relative survival among elderly patients with chronic myeloid leukemia: a population-based study in the Netherlands, 1989–2017. Leukemia 2020.
Breccia M, Alimena G. The role of comorbidities in chronic myeloid leukemia. Leuk Res. 2013;37(7):729–30.
Gugliotta G, Castagnetti F, Palandri F, Breccia M, Intermesoli T, Capucci A, Martino B, Pregno P, Rupoli S, Ferrero D, Gherlinzoni F, Montefusco E, Bocchia M, Tiribelli M, Pierri I, Grifoni F, Marzocchi G, Amabile M, Testoni N, Martinelli G, Alimena G, Pane F, Saglio G, Baccarani M, Rosti G. Frontline imatinib treatment of chronic myeloid leukemia: no impact of age on outcome, a survey by the GIMEMA CML Working Party. Blood. 2011;117(21):5591–9.
Lauseker M, Gerlach R, Worseg W, Haferlach T, Tauscher M, Hasford J, Hoffmann VS. Differences in treatment and monitoring of chronic myeloid leukemia with regard to age, but not sex: results from a population-based study. Eur J Haematol. 2019;103(4):362–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Saussele S, Krauss MP, Hehlmann R, Lauseker M, Proetel U, Kalmanti L, Hanfstein B, Fabarius A, Kraemer D, Berdel WE, Bentz M, Staib P, de Wit M, Wernli M, Zettl F, Hebart HF, Hahn M, Heymanns J, Schmidt-Wolf I, Schmitz N, Eckart MJ, Gassmann W, Bartholomaus A, Pezzutto A, Leibundgut EO, Heim D, Krause SW, Burchert A, Hofmann WK, Hasford J, Hochhaus A, Pfirrmann M, Muller MC, K. Schweizerische Arbeitsgemeinschaft fur Klinische and C. M. L. S. G. the German. Impact of comorbidities on overall survival in patients with chronic myeloid leukemia: results of the randomized CML study IV. Blood. 2015;126(1):42–9.
Mohammadi M, Cao Y, Glimelius I, Bottai M, Eloranta S, Smedby KE. The impact of comorbid disease history on all-cause and cancer-specific mortality in myeloid leukemia and myeloma - a Swedish population-based study. BMC Cancer. 2015;15:850.
Bhayat F, Das-Gupta E, Smith C, McKeever T, Hubbard R. The incidence of and mortality from leukaemias in the UK: a general population-based study. BMC Cancer. 2009;9:252.
Larfors G, Sandin F, Richter J, Sjalander A, Stenke L, Lambe M, Hoglund M. The impact of socio-economic factors on treatment choice and mortality in chronic myeloid leukaemia. Eur J Haematol. 2017;98(4):398–406.
Lauseker M, Hasford J, Pfirrmann M, Hehlmann R, German CMLSG. The impact of health care settings on survival time of patients with chronic myeloid leukemia. Blood. 2014;123(16):2494–6.
Frederiksen H, Farkas DK, Christiansen CF, Hasselbalch HC, Sorensen HT. Chronic myeloproliferative neoplasms and subsequent cancer risk: a Danish population-based cohort study. Blood. 2011;118(25):6515–20.
Sasaki K, Kantarjian HM, O'Brien S, Ravandi F, Konopleva M, Borthakur G, Garcia-Manero G, Wierda WG, Daver N, Ferrajoli A, Takahashi K, Jain P, Rios MB, Pierce SA, Jabbour EJ, Cortes JE. Incidence of second malignancies in patients with chronic myeloid leukemia in the era of tyrosine kinase inhibitors. Int J Hematol. 2019;109(5):545–52.
Gugliotta G, Castagnetti F, Breccia M, Albano F, Iurlo A, Intermesoli T, Abruzzese E, Levato L, D'Adda M, Pregno P, Cavazzini F, Stagno F, Martino B, La Barba G, Sora F, Tiribelli M, Bigazzi C, Binotto G, Bonifacio M, Caracciolo C, Soverini S, Foa R, Cavo M, Martinelli G, Pane F, Saglio G, Baccarani M, Rosti G, P. Gruppo Italiano Malattie Ematologiche dell'Adulto - Chronic Myeloid Leukemia Working. Incidence of second primary malignancies and related mortality in patients with imatinib-treated chronic myeloid leukemia. Haematologica. 2017;102(9):1530–6.
Miranda MB, Lauseker M, Kraus MP, Proetel U, Hanfstein B, Fabarius A, Baerlocher GM, Heim D, Hossfeld DK, Kolb HJ, Krause SW, Nerl C, Brummendorf TH, Verbeek W, Fauser AA, Prummer O, Neben K, Hess U, Mahlberg R, Ploger C, Flasshove M, Rendenbach B, Hofmann WK, Muller MC, Pfirrmann M, Hochhaus A, Hasford J, Hehlmann R, Saussele S. Secondary malignancies in chronic myeloid leukemia patients after imatinib-based treatment: long-term observation in CML Study IV. Leukemia. 2016;30(6):1255–62.
Acknowledgements
The authors appreciate the work of all clinicians reporting all newly diagnosed cases of CML to the Swedish CML registry.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
Nothing to disclose.
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Höglund, M., Sandin, F., Simonsson, B., Stenke, L. (2021). Epidemiology of Chronic Myeloid Leukaemia. In: Hehlmann, R. (eds) Chronic Myeloid Leukemia. Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-71913-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-71913-5_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71912-8
Online ISBN: 978-3-030-71913-5
eBook Packages: MedicineMedicine (R0)