Abstract
Zika virus (ZIKV) is a mosquito borne flavivirus that exhibits wide range of transmission routes including mosquito, transplacental, sexual contact, blood transfusion and organ transplantation. ZIKV is highly neurotropic which infects central nervous system (CNS) in adult and developing brain. As of 2021, at least 86 countries and territories have been reported with autochthonous transmission of ZIKV. Preexisting flavivirus specific sero-cross reactivity antibodies may results in antibody dependent enhancement (ADE) of ZIKV infection with significant higher viral load and severe disease outcomes. However, the mechanism of ADE has not been completely understood. Upon ZIKV infection, innate immune system, humoral immune response and cellular mediated response get activated. Even though, the virus has developed several immune escape strategies for successful infection. Currently there is no specific treatment available for ZIKV infection and the treatment relies on the symptomatic relief of the patients. However, several of the drug candidates have been discovered and are currently in the clinical trials. Molecules have been targeted against potential viral proteins including entry inhibitors, protease inhibitors and replication inhibitors. In spite of progress made in this area, the absence of clinically approved drug or vaccine increases the chances of recurrent outbreak in endemic regions and therefore needs utmost attention in this issue.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Zika virus
- Antibody dependent enhancement
- Zika syndrome
- Antivirals
- Guillain-Barré syndrome
- DENV infection
- STAT2 protein
- Galidesivir
- Non-steroidal anti-inflammatory drugs
1 Introduction
Zika virus (ZIKV) is a flavivirus which gets transmitted primarily via bite of infected Aedes aegypti mosquito. ZIKV is also transmitted from mother to fetus via crossing transplacental barrier, through sexual contact, (Musso et al. 2019) blood transfusion (Joob and Wiwanitkit 2019) and organ transplantation (Fig. 1) (Nogueira et al. 2017). The incubation period of ZIKV infection is 3–14 days from the exposure to the virus. Most of the individuals infected with ZIKV remain asymptomatic. However, mild symptoms for 2–7 days may arise in few individuals which ranges from fever, joint pain, rash, headache and malaise (Baud et al. 2017). During pregnancy, ZIKV infection in mother may cause intrauterine growth restriction, preterm birth and miscarriage as well as ZIKV may be transmitted to fetus which causes infants to be born with Zika syndrome (Teixeira et al. 2020) including cerebral atrophy, cortical and/or periventricular calcifications, corpus callosum abnormalities, ventriculomegaly, including congenital malformations like microcephaly (Ribeiro et al. 2017).
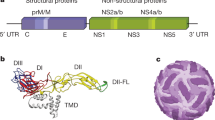
Adults and children infected with ZIKV are at the risk of neurological complications including neuropathy, myelitis, encephalomyelitis, encephalitis, meningoencephalitis, sensory polyneuropathy and Guillain-Barré syndrome (Muñoz et al. 2018). Neuropathological investigations of ZIKV infection have shown the presence of ZIKV in brain and cerebrospinal fluid samples (Fig. 2). These findings suggest that ZIKV is highly neurotropic which infects central nervous system (CNS) in adult and developing brain (Chimelli et al. 2017). ZIKV replication follows the similar mode of replication cycle as other flaviviruses. Dendritic cell-specific intercellular adhesion molecule 3-grabbing nonintegrin (DC-SIGN) is the primary cellular receptor involve in the receptor mediated internalization of ZIKV (Hamel et al. 2015). The acidic environment inside the endosomal compartment induces the fusion of viral envelope protein with endosomal membrane that results in release of ZIKV RNA into the cytoplasm (Agrelli et al. 2019). The positive sense RNA genome of ZIKV is a 10.8 Kb which comprised of ~100 nucleotides of 5′ untranslated region (UTR), a single open reading frame (ORF) of ~10 Kb and a 3′ UTR region of ~420 nucleotides (Wang et al. 2017). The single ORF encodes for a single polyprotein that gets processed into structural proteins as capsid (C), precursor membrane protein (prM), envelop (E) and non-structural proteins as NS1, NS2a, NS2b, NS3, NS4a, NS4b, and NS5 (Rossignol et al. 2017). These proteins assist in the replication of viral RNA at the endoplasmic reticulum surface where viral RNA and proteins assembled to generate immature virions. Upon furin-mediated cleavage of prM to M protein, these virions get mature in the trans-Golgi network and results in the process of egression (Rossignol et al. 2017).
Transplacental transmission of ZIKV. 70–80% of ZIKV infection during pregnancy may not transmit the virus to fetus. Whereas, 20–30% of ZIKV infection during pregnancy may transmit the ZIKV to fetus and may cause preterm birth and miscarriage (4–7%) and may be transmitted to fetus which results in microcephaly (4–6%) or asymptomatic cases with medium or long term sequelae
2 Epidemiology of Zika Virus Infection
In 1947, ZIKV is first identified in sentinel rhesus monkey in Uganda and later in 1952, identified in humans in Uganda and United Republic of Tanzania. However, little attention was paid until 2007, when a major outbreak of ZIKV reported in the Yap State of Micronesia. Consequently, in year 2013 outbreaks were reported in French Polynesia and subsequently in other Pacific Islands. Till date, the largest outbreak of ZIKV has been reported in Brazil in year 2015–2016 with over 200,000 cases where over 8000 babies were born with malformations caused by ZIKV (Hills et al. 2017). Recent epidemiological data helps in understanding of global Zika transmission and its associated challenges. As of 2021, at least 86 countries and territories have been reported with autochthonous transmission of ZIKV that includes Africa, America, South-East Asia and Western Pacific regions (Fig. 3) (https://www.who.int/health-topics/zika-virus-disease#tab=tab_1). Several factors including prevalence of mosquito vectors, global trade and travel, tropical/subtropical climate, poor waste management has causes recent emergence of Zika virus in countries like China, India, Indonesia, Maldives, Thailand, and Pakistan in recent years. Due to co-circulation of dengue in endemic tropical and sub-tropical region, it has been estimated that people living in 2 million square kilometer are at the highest risk of getting ZIKV infection (Messina et al. 2016). In these individuals, people may be diagnosed with co-infection with Zika and dengue both. A retrospective population based serological survey in Indonesia revealed that by the age of 5 years approximately 9% of the children had previous ZIKV infection. Seasonal patterns of ZIKV transmission in Thailand demonstrated that transmission coincided with dengue virus by sharing common mosquito vectors. In year 2018, ZIKV outbreak has been reported in Rajasthan, India (Saxena et al. 2019).
Epidemiology of ZIKV showing the countries or territories that have reported with ZIKV infection as well as areas where the mosquito are present or absent with no evidence of ZIKV transmission as per Centers for Disease Control and Prevention (https://wwwnc.cdc.gov/travel/files/zika-areas-of-risk.pdf)
3 Antibody-Dependent Enhancement
Preexisting flavivirus specific sero-cross reactivity antibodies may results in antibody dependent enhancement (ADE) of ZIKV infection with significant higher viral load and severe disease outcomes (Dejnirattisai et al. 2016). ADE has been studied extensively specifically with respect to secondary dengue infection, which is attributed by the observation that pre-existing antibodies that results in secondary infection such as DSS and/or DHF which is more severe form of DENV infection (Guzman et al. 2013). The cross-reactive antibodies facilitates the viral uptake that increases the severity of infection by forming a complex between the cross-reactive Abs and the viral particles and, hence, helping these particles to get internalized via Fc gamma receptor (Moi et al. 2010). Considerable degree of genetic similarities and structural homology among ZIKV and other flaviviruses, results in a generation of sero cross-reactivity antibodies (Rathore and St John 2020). Additionally, in vitro studies shows human monoclonal Abs (mAbs) to the DENV fusion loop epitope causing ADE of ZIKV in Fc receptor bearing cell lines which is shown to be facilitating ZIKV infection (Priyamvada et al. 2016). On the other hand, DENV patient derived mAbs to EDE1 (E dimer-epitope) which neutralizes all the four serotypes of DENV, in vitro, neutralizes ZIKV too, with a high potency, whereas EDE2 binds, but does not significantly neutralizes ZIKV (Fernandez et al. 2020). Similarly, when the convalescent plasma from DENV/WNV infected samples was transferred in vitro, enhancement of ZIKV infection has been found which is mediated through Fc gamma receptors (Swanstrom et al. 2016). Although, WNV mediated Abs shows less cross-reactivity to ZIKV in comparison to DENV-mediated Abs, but when studied, human polyclonal Abs against WNV is reported to be cross reactive towards ZIKV resulting in enhancement of ZIKV infection both in vivo and in vitro (Bardina et al. 2017). So far, ADE response during ZIKV infection has not been clearly understood.
4 Understanding the Host-Immune Response
Nucleic acid receptors such as RIG-I-like receptors (RLRs) activate upon binding to the viral RNA and initiate the release of interferon (IFN) via stimulating IFN receptor subunits that activates the JAK-STAT pathways and thereby establishes an antiviral state (Rehwinkel and Gack 2020). ZIKV NS1 protein has been shown to involve in the immune escape mechanism by inhibiting the type 1 IFN signaling pathway (Xia et al. 2018). In addition, NS5 protein has been shown to degrade the STAT2 protein that results in inhibition of IFN signaling pathway (Grant et al. 2016). Humoral immune response confers first-line of protection against flaviviral infection. B cell mediated antibody response is crucial in any viral infection and may results in the development of effective vaccines. The E, prM and NS1 protein has been found to elicit stronger antibody response which has been utilized in several studies that shows protection against ZIKV infection in various models (Amrun et al. 2020). Strong B cell response suggests a crucial role in ZIKV infection that helps us to identify B cell epitopes identified specifically from NS1 protein which have been found to be preventive upon challenged with ZIKV (Kam et al. 2019). Similarly, envelope has been found to contain B cell epitopes especially from the domain III region and has been found to protect mice upon challenged with ZIKV infection (Yang et al. 2017). Cell mediated immune response also plays a crucial role in prevention of viral infections. Both CD8+ and CD4+ T cells are involved in cell mediated immune responses during ZIKV infection (Winkler et al. 2017). Protective role CD8+ T cells in during ZIKV infection has been validated by observing susceptibility of infected mice towards the ZIKV infection in its absence (Elong Ngono et al. 2017). In addition, adoptive transfer of ZIKV specific CD8+ T cells has been found to protect mice challenged with ZIKV infection by reducing the viral load (Huang et al. 2017).
5 Investigational Medicines for the Treatment of Zika
Currently there is no specific treatment available for ZIKV infection. However, the treatment relies on the symptomatic relief of the patients. According to CDC, the recommended treatment for ZIKV infection is to take plenty of rest, enough fluid intakes to prevent dehydration, acetaminophen for reducing fever and pain and not to use aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs) until dengue has been ruled out (https://www.cdc.gov/zika/symptoms/treatment.html). Considering the replication cycle of ZIKV, several of the potential drugs targets have been identified for the development of effective antiviral drugs. Inhibitors that can interfere with the interaction of viral envelope protein with host cell receptors may be used for the development of potential entry inhibitors. One of the natural product nanchangmycin derived from Streptomyces nanchangensis, has been shown to act via inhibition of AXL receptors and abolishment of viral internalization process via receptor mediated endocytosis (Rausch et al. 2017). Compound screening of entry inhibitor has revealed ZINC33683341 molecule as a potential entry inhibitor during ZIKV infection (Fernando et al. 2016). RNA dependent RNA polymerases have been well characterized and explored drug targets due to its essential role in virus replication and production of progeny virus. Nucleoside analogues including its phosphoramidate product have been shown be a promising RdRp inhibitors. Several of the potential drug candidates have been investigated against ZIKV. 3′-O-methylribonucleosides and 2′-C-methylated ribonucleoside has been found to exhibits inhibitory effect on ZIKV replication with less toxicity (Boehr et al. 2019). Adenosine analogues named as NITD008 has been shown as a potent anti-ZIKV activity in cell culture model where in it reduces the viremia and prevent virus induced cell death (Deng et al. 2016). This compound has been also found to inhibit DENV replication. However, due to associated toxicity, the NITD008 has been discontinued from the pipeline of drug discovery for ZIKV. One of the nucleoside analogue named as 7DMA which has been designed for the treatment of HCV has been found as a potent inhibitor of ZIKV infection in cell culture and animal model (Zmurko et al. 2016). However, it has not been successful in clinical trial. Similarly, the clinically approved HCV drug, sofosbuvir has been extensively studied for its activity against ZIKV infection. In both cell culture and model, sofosbuvir has been found to exhibit potent antiviral activity (Bullard-Feibelman et al. 2017). FDA has considered the sofosbuvir as a pregnancy class B drug for the treatment of HCV infection and therefore it might be an ideal drug candidate for ZIKV treatment in pregnant women. In addition, ribavirin which has been also developed as an anti-HCV drug, found to exhibit antiviral properties against ZIKV infection (Kamiyama et al. 2017). Galidesivir which is an adenosine analogue drug developed for filoviruses and YFV has been shown to be effective against ZIKV infection (Lim et al. 2017). In addition to nucleoside based analogues drugs, several of the non-nucleoside drug candidates have been tested. NS2B-NS3 protease of ZIKV is the most targeted ZIKV proteins for the development of antivirals due to its crucial role in replication and maturation. A boric acid containing dipeptides inhibitors have been designed which showed strong antiviral activity. This compound has been found to exhibits broad spectrum anti-flaviviral activity (Lei et al. 2016). Similarly, a pyrazole ester derivative has been developed as a covalent inhibitor of protease activity (Li et al. 2018). Apart from these drug candidates, complementary and alternative medicine in alliance with conventional medicine may be used for Zika therapeutics and prevention (Saxena et al. 2016).
6 Conclusions
Zika virus is an emerging mosquito-borne flavivirus infection that causes Zika syndrome and various neurological complications in adults. The absence of clinically approved drug or vaccine increases the chances of recurrent outbreak in endemic regions. Several of the vaccine candidates have been developed while understanding the immunogenicity of ZIKV proteins and host cellular response during infection. Presence of flavivirus sero-cross reactivity antibodies may results in antibody dependent enhancement (ADE) of ZIKV infection that significantly increases the viral load with severe disease outcomes. Currently there is no specific treatment available for ZIKV infection and the treatment relies on the symptomatic relief of the patients. However, several of the drug candidates have been discovered and are currently in the clinical trials.
7 Future Perspectives
Intense research is required for the better understanding of ZIKV pathogenesis in various models focusing on developmental biology, transplacental transmission and neurological complications. In addition, basic research long-term cohort studies needs to be conducted for the better understanding of the disease impact as well as assessment of the risk for coming future. In this regard, leading heath organizations should establish a surveillance monitoring system in endemic areas of flaviviruses for co-infection cases that will help us to understand more about ADE of ZIKV infection. Due to increased risk associated with pregnant women and related congenital abnormalities, non-essential travelling to the affected areas needs to be avoided by travelers. Due to absence of clinically approved vaccine or drug, personal protective measures need to be compelled.
References
Agrelli A, de Moura RR, Crovella S, Brandão LAC. ZIKA virus entry mechanisms in human cells. Infect Genet Evol. 2019;69:22–9. https://doi.org/10.1016/j.meegid.2019.01.018.
Amrun SN, Yee WX, Abu Bakar F, et al. Novel differential linear B-cell epitopes to identify Zika and dengue virus infections in patients [published correction appears in Clin Transl Immunology. 2020 Feb 19;9(2):e01118]. Clin Transl Immunol. 2019;8(7):e1066. Published 26 July 2019. https://doi.org/10.1002/cti2.1066.
Bardina SV, Bunduc P, Tripathi S, et al. Enhancement of Zika virus pathogenesis by preexisting antiflavivirus immunity. Science. 2017;356(6334):175–80. https://doi.org/10.1126/science.aal4365.
Baud D, Gubler DJ, Schaub B, Lanteri MC, Musso D. An update on Zika virus infection. Lancet. 2017;390(10107):2099–109. https://doi.org/10.1016/S0140-6736(17)31450-2.
Boehr AK, Arnold JJ, Oh HS, Cameron CE, Boehr DD. 2’-C-methylated nucleotides terminate virus RNA synthesis by preventing active site closure of the viral RNA-dependent RNA polymerase. J Biol Chem. 2019;294(45):16897–907. https://doi.org/10.1074/jbc.RA119.010214.
Bullard-Feibelman KM, Govero J, Zhu Z, et al. The FDA-approved drug sofosbuvir inhibits Zika virus infection. Antiviral Res. 2017;137:134–40. https://doi.org/10.1016/j.antiviral.2016.11.023.
Chimelli L, Melo ASO, Avvad-Portari E, et al. The spectrum of neuropathological changes associated with congenital Zika virus infection. Acta Neuropathol. 2017;133(6):983–99. https://doi.org/10.1007/s00401-017-1699-5.
Dejnirattisai W, Supasa P, Wongwiwat W, et al. Dengue virus sero-cross-reactivity drives antibody-dependent enhancement of infection with Zika virus. Nat Immunol. 2016;17(9):1102–8. https://doi.org/10.1038/ni.3515.
Deng YQ, Zhang NN, Li CF, et al. Adenosine analog NITD008 is a potent inhibitor of Zika virus. Open Forum Infect Dis. 2016;3(4):ofw175. Published 30 Aug 2016. https://doi.org/10.1093/ofid/ofw175.
Elong Ngono A, Vizcarra EA, Tang WW, et al. Mapping and role of the CD8+ T cell response during primary Zika virus infection in mice. Cell Host Microbe. 2017;21(1):35–46. https://doi.org/10.1016/j.chom.2016.12.010.
Fernandez E, Dejnirattisai W, Cao B, et al. Human antibodies to the dengue virus E-dimer epitope have therapeutic activity against Zika virus infection [published correction appears in Nat Immunol. 2020 Mar;21(3):354]. Nat Immunol. 2017;18(11):1261–9. https://doi.org/10.1038/ni.3849.
Fernando S, Fernando T, Stefanik M, Eyer L, Ruzek D. An approach for Zika virus inhibition using homology structure of the envelope protein. Mol Biotechnol. 2016;58(12):801–6. https://doi.org/10.1007/s12033-016-9979-1.
Grant A, Ponia SS, Tripathi S, et al. Zika virus targets human STAT2 to inhibit type I interferon signaling. Cell Host Microbe. 2016;19(6):882–90. https://doi.org/10.1016/j.chom.2016.05.009.
Guzman MG, Alvarez M, Halstead SB. Secondary infection as a risk factor for dengue hemorrhagic fever/dengue shock syndrome: an historical perspective and role of antibody-dependent enhancement of infection. Arch Virol. 2013;158(7):1445–59. https://doi.org/10.1007/s00705-013-1645-3.
Hamel R, Dejarnac O, Wichit S, et al. Biology of Zika virus infection in human skin cells. J Virol. 2015;89(17):8880–96. https://doi.org/10.1128/JVI.00354-15.
Hills SL, Fischer M, Petersen LR. Epidemiology of Zika virus infection. J Infect Dis. 2017;216(suppl_10):S868–74. https://doi.org/10.1093/infdis/jix434.
Huang H, Li S, Zhang Y, et al. CD8+ T cell immune response in immunocompetent mice during Zika virus infection. J Virol. 2017;91(22):e00900-17. Published 27 Oct 2017. https://doi.org/10.1128/jvi.00900-17.
Joob B, Wiwanitkit V. Zika virus, blood donation and transfusion transmission risk. Hematol Transfus Cell Ther. 2019;41(3):278. https://doi.org/10.1016/j.htct.2018.11.001.
Kam YW, Leite JA, Amrun SN, et al. ZIKV-specific NS1 epitopes as serological markers of acute Zika virus infection. J Infect Dis. 2019;220(2):203–12. https://doi.org/10.1093/infdis/jiz092.
Kamiyama N, Soma R, Hidano S, et al. Ribavirin inhibits Zika virus (ZIKV) replication in vitro and suppresses viremia in ZIKV-infected STAT1-deficient mice. Antiviral Res. 2017;146:1–11. https://doi.org/10.1016/j.antiviral.2017.08.007.
Lei J, Hansen G, Nitsche C, Klein CD, Zhang L, Hilgenfeld R. Crystal structure of Zika virus NS2B-NS3 protease in complex with a boronate inhibitor. Science. 2016;353(6298):503–5. https://doi.org/10.1126/science.aag2419.
Li Y, Zhang Z, Phoo WW, et al. Structural insights into the inhibition of Zika virus NS2B-NS3 protease by a small-molecule inhibitor. Structure. 2018;26(4):555–64.e3. https://doi.org/10.1016/j.str.2018.02.005.
Lim SY, Osuna C, Lakritz J, Chen E, Yoon G, Taylor R, MacLennan S, Leonard M, Giuliano E, Mathis A, Berger E. Galidesivir, a direct-acting antiviral drug, abrogates viremia in rhesus macaques challenged with Zika virus. In: Open forum infectious diseases. Oxford University Press; 2017.
Messina JP, Kraemer MU, Brady OJ, et al. Mapping global environmental suitability for Zika virus. Elife. 2016;5:e15272. https://doi.org/10.7554/eLife.15272.
Moi ML, Lim CK, Takasaki T, Kurane I. Involvement of the Fc gamma receptor IIA cytoplasmic domain in antibody-dependent enhancement of dengue virus infection. J Gen Virol. 2010;91(Pt 1):103–11. https://doi.org/10.1099/vir.0.014829-0.
Muñoz LS, Parra B, Pardo CA. Neuroviruses emerging in the Americas study. Neurological implications of Zika virus infection in adults. J Infect Dis. 2018; 217(8):1334.
Musso D, Ko AI, Baud D. Zika virus infection—after the pandemic. N Engl J Med. 2019;381(15):1444–57. https://doi.org/10.1056/NEJMra1808246.
Nogueira ML, Estofolete CF, Terzian AC, et al. Zika virus infection and solid organ transplantation: a new challenge. Am J Transplant. 2017;17(3):791–5. https://doi.org/10.1111/ajt.14047.
Priyamvada L, Quicke KM, Hudson WH, et al. Human antibody responses after dengue virus infection are highly cross-reactive to Zika virus. Proc Natl Acad Sci U S A. 2016;113(28):7852–7. https://doi.org/10.1073/pnas.1607931113.
Rathore APS, St John AL. Cross-reactive immunity among flaviviruses. Front Immunol. 2020;11:334. Published 26 Feb 2020. https://doi.org/10.3389/fimmu.2020.00334.
Rausch K, Hackett BA, Weinbren NL, et al. Screening bioactives reveals nanchangmycin as a broad spectrum antiviral active against Zika virus. Cell Rep. 2017;18(3):804–15. https://doi.org/10.1016/j.celrep.2016.12.068.
Rehwinkel J, Gack MU. RIG-I-like receptors: their regulation and roles in RNA sensing [published online ahead of print, 13 Mar 2020]. Nat Rev Immunol. 2020;1–15. https://doi.org/10.1038/s41577-020-0288-3.
Ribeiro BG, Werner H, Lopes FPPL, et al. Central nervous system effects of intrauterine Zika virus infection: a pictorial review. Radiographics. 2017;37(6):1840–50. https://doi.org/10.1148/rg.2017170023.
Rossignol ED, Peters KN, Connor JH, Bullitt E. Zika virus induced cellular remodelling. Cell Microbiol. 2017;19(8). https://doi.org/10.1111/cmi.12740.
Saxena SK, Elahi A, Gadugu S, Prasad AK. Zika virus outbreak: an overview of the experimental therapeutics and treatment. Virusdisease. 2016;27(2):111–5. https://doi.org/10.1007/s13337-016-0307-y.
Saxena SK, Kumar S, Sharma R, Maurya VK, Dandu HR, Bhatt MLB. Zika virus disease in India—update October 2018. Travel Med Infect Dis. 2019;27:121–2. https://doi.org/10.1016/j.tmaid.2018.10.022.
Swanstrom JA, Plante JA, Plante KS, et al. Dengue virus envelope dimer epitope monoclonal antibodies isolated from dengue patients are protective against Zika virus. mBio. 2016;7(4):e01123-16. Published 19 July 2016. https://doi.org/10.1128/mbio.01123-16.
Teixeira FME, Pietrobon AJ, Oliveira LM, Oliveira LMDS, Sato MN. Maternal-fetal interplay in Zika virus infection and adverse perinatal outcomes. Front Immunol. 2020; 11:175. Published 14 Feb 2020. https://doi.org/10.3389/fimmu.2020.00175.
Wang A, Thurmond S, Islas L, Hui K, Hai R. Zika virus genome biology and molecular pathogenesis. Emerg Microbes Infect. 2017;6(3):e13. Published 22 Mar 2017. https://doi.org/10.1038/emi.2016.141.
Winkler CW, Myers LM, Woods TA, et al. Adaptive immune responses to Zika virus are important for controlling virus infection and preventing infection in brain and testes. J Immunol. 2017;198(9):3526–35. https://doi.org/10.4049/jimmunol.1601949.
Xia H, Luo H, Shan C, et al. An evolutionary NS1 mutation enhances Zika virus evasion of host interferon induction. Nat Commun. 2018;9(1):414. Published 29 Jan 2018. https://doi.org/10.1038/s41467-017-02816-2.
Yang M, Dent M, Lai H, Sun H, Chen Q. Immunization of Zika virus envelope protein domain III induces specific and neutralizing immune responses against Zika virus. Vaccine. 2017;35(33):4287–94. https://doi.org/10.1016/j.vaccine.2017.04.052.
Zika epidemiology update, World Health Organization. https://www.who.int/emergencies/diseases/zika/zika-epidemiology-update-july-2019.pdf?ua=1. Accessed May 2020.
Zika virus Treatment. Centre for Disease control and Prevention. https://www.cdc.gov/zika/symptoms/treatment.html. Accessed May 2020.
Zmurko J, Marques RE, Schols D, Verbeken E, Kaptein SJ, Neyts J. The viral polymerase inhibitor 7-Deaza-2′-C-Methyladenosine is a potent inhibitor of in vitro Zika virus replication and delays disease progression in a robust mouse infection model. PLoS Negl Trop Dis. 2016;10(5):e0004695. Published 10 May 2016. https://doi.org/10.1371/journal.pntd.0004695.
Acknowledgements
The authors are grateful to the Vice Chancellor, King George’s Medical University (KGMU), Lucknow, India, for the encouragement of this work. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kumar, S., Nyodu, R., Maurya, V.K., Saxena, S.K. (2021). Zika Virus Disease: Progress and Prospects. In: Ahmad, S.I. (eds) Human Viruses: Diseases, Treatments and Vaccines . Springer, Cham. https://doi.org/10.1007/978-3-030-71165-8_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-71165-8_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71164-1
Online ISBN: 978-3-030-71165-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)