Abstract
Current and recent users of combined oral contraceptives (COCs) have an increased risk of breast cancer, an effect which has not been consistently shown to be related to duration of use and which disappears within a few years of stopping. Current and recent users of COCs also have an increased risk of invasive cervical cancer, an effect which strengthens with prolonged use and which wears off after stopping. The risk of both ovarian and endometrial cancer is reduced in current users of COCs, a beneficial effect that increases with duration of use and persists for many years after stopping. Previous evidence that COC use may reduce the risk of colorectal cancer has not been confirmed in a number of more recent studies. Sparse evidence suggests that prolonged use of COCs increases the risk of hepatocellular carcinoma in women living in areas where the prevalence of hepatitis B virus is low. Lengthy follow-up of large cohort studies shows that the lifetime risk of any cancer in ever users of COCs is similar to that of never users. There have been comparatively few studies examining the cancer effects of progestogen-only contraceptives, especially in women who have used only these products. At the moment, it is prudent to assume these contraceptives have a similar pattern of breast and cervical cancer risk as COCs. Limited data indicates that users of non-hormonal intra-uterine devices may have a reduced risk of cervical cancer (any device), and endometrial cancer (for inert but not copper devices). Current evidence does not strongly suggest a changed risk of breast, cervical, endometrial or colorectal cancer among women who chose to be sterilised although they may be protected against ovarian cancer. Evidence linking vasectomy with an increased risk of prostate cancer is inconsistent and likely to be biased; an important association with testicular cancer has not emerged in the few studies conducted so far.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Combined oral contraceptives
- Progestogen-only contraceptives
- Intra-uterine devices
- Female sterilisation
- Male sterilisation
- Cancer
1 Introduction
Cancer is a major cause of morbidity and death among women, regardless of where they live. In 2018, an estimated 8.6 million women around the world experienced a new diagnosis of cancer, and 4.2 million died from the disease (Figs. 11.1 and 11.2; Table 11.1) [1, 2]. Overall, women have a near 1-in-6 chance of developing cancer before the age of 75; and a 1-in-10 chance of dying from it.
Major differences between populations in age and socioeconomic profile, the prevalence and distribution of key cancer risk factors, and competing risk of death from other causes, results in substantial geographical variations in the pattern of cancer incidence and mortality (Tables 11.2 and 11.3). These patterns also reflect important global differences in the availability of prevention, screening, diagnostic and treatment services for cancer. Breast cancer is the leading cause of cancer incidence among women in most (154 out of 185) countries around the world, with cervical cancer most frequent in nearly all (28) of the rest (Table 11.2). There is greater variation with respect to the leading cause of cancer-related death, partly because of comparatively high rates of case fatality for many cancers in low income countries. Thus, breast cancer is the leading cause of cancer-related mortality in 103 countries, cervical cancer in 42 countries and lung cancer in 28 countries (Table 11.3).
Soon after combined oral contraceptives (COCs) became available in the early 1960s, informed commentators expressed concern about the cancer potential of this novel method of birth control [3]. The critics highlighted research conducted in the 1930s that linked oestrogen to cancerous uterine and breast growths in mice and other animals. They also noted that clinical experience gained through the use of hormones to treat infertility or threatened miscarriage during the couple of decades before they were licensed as contraceptives mainly related to use by older women for short durations. This limited usage, the commentators argued, could not adequately inform regulators, clinicians or potential users about the long-term safety of hormones used for contraception by large numbers of healthy young women, for perhaps long durations. Even a small change in cancer risk could have profound public health consequences. Furthermore, the long latent period for cancer development in humans probably meant that a full evaluation of the cancer risks associated with the contraceptive pill would take many years.
Since these concerns were first raised, there have been many hundreds of animal, laboratory and epidemiological studies looking at the possible link between COCs and cancer. Fewer studies have assessed cancer risks among users of other methods of birth control. Investigating the carcinogenic potential of contraceptives has been complex and time-consuming for a number of reasons:
-
1.
It has been unclear whether changes seen in in vitro laboratory experiments, or in vivo studies of mice, rabbits, beagles, primates or other animals, are relevant to women.
-
2.
Although cancer is common, most events (76.6% of new cases and 85.5% of deaths) occur in women older than 50 years [1], the age by which most women have completed their reproductive life. The comparatively low incidence of most cancers among younger women has necessitated the prolonged follow-up of participants in cohort studies. It has also sometimes made the accurate recall of contraceptive use by participants in case-control studies questionable—especially in investigations recruiting older women who may have used multiple methods many years previously. Some studies, especially those only observing young women during their reproductive years, have had low statistical power to detect an altered cancer risk that might exist—either because not enough women used the contraceptive being studied or an insufficient number of cancers occurred. Another limitation of only studying women of reproductive age is the inability to determine whether important associations continue into, or emerge in, later years.
-
3.
Many women use a variety of contraceptives during their reproductive lives. It has sometimes been unclear whether effects seen in one group of contraceptive users reflects true effects of that method or persisting effects from a previously used method. Complicating matters further, different methods may have opposing effects; for example, condoms protect against cervical cancer whilst combined oral contraceptives appear to increase the risk during current and recent use. Even among users of only one method, formulation changes over time can make the assessment of risk associated with a particular product difficult. For example, the oestrogen content of combined oral contraceptives has been reduced, and new progestogens introduced, since this method of birth control was first marketed. Since most contraceptive pill users use more than one formulation during their lifetime, there has sometimes been uncertainty about whether an observed cancer association is due to the effects of the preparation used nearest to the cancer diagnosis, persistent effects from previously used products or perhaps both.
-
4.
Cancer risk may be influenced by when a contraceptive is used in a user’s reproductive life (e.g. at a young age), by duration of use or by time since last use. Some studies have not been able to examine all of these issues; many have simply compared ever with never users of a contraceptive. In addition, studies have categorised aspects of contraceptive use differently, sometimes hampering comparisons between studies.
-
5.
Confounding (the distortion of the relationship between exposure and outcome because of a third factor related to both exposure and outcome) is a particular consideration when interpreting results from observational epidemiological studies. Many reproductive (e.g. number of children, history of breastfeeding, age at first intercourse and number of sexual partners) and non-reproductive (e.g. smoking, body mass index, socioeconomic status and participation in screening services) characteristics may be potential confounding factors for different cancers in women using different contraceptives. Studies have varied greatly in the level of information collected about possible confounding factors, and the extent to which they have been allowed for in the statistical analyses.
These challenges mean that great care must be taken when interpreting findings from observational cohort or case-control studies of possible cancer risks associated with contraception. It is especially important to remember that statistical association does not necessarily mean causation; bias, chance or confounding may be alternative explanations for the association. This said, observational epidemiological research is the backbone of evidence that guides policy and clinical decision-making in relation to contraception. When considering the evidence, it is important to assess its totality without placing undue reliance on the findings from just one or two studies, or from a particular subgroup analysis. It is also important to remember that measures of relative risk assess the strength of an association (a key consideration when judging causation), whereas absolute risk is important when considering the clinical relevance of any association.
2 Breast Cancer
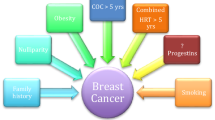
Breast cancer accounts for nearly a quarter of all cancers occurring in women around the world; nearly 2.1 million new cases and 630,000 deaths in 2018 [1, 2]. Hereditary (family history of breast or ovarian cancer) and genetic (such as BRCA1, BRCA2 and other breast cancer susceptibility mutations) factors account for less than 10% of cases [2]. A wide range of factors have been linked to increased breast cancer risk: menstrual (early age at menarche, older age at menopause), reproductive (nulliparity, late age at first birth, fewer children), exogenous hormone use (oral contraceptives and menopausal hormone therapy (MHT), anthropometry (greater weight, weight gain during adulthood, body fat distribution) and alcohol intake [4]. Breastfeeding and physical activity appear to be protective.
2.1 Combined Oral Contraceptives
Early epidemiological studies investigating whether COCs are associated with an altered risk of breast cancer provided contradictory and confusing evidence. Part of the problem arose from difficulties in comparing studies because investigators categorised aspects of contraceptive use differently, for instance, age at first use or duration of use. Important new insights were gained in 1996 when the Collaborative Group on Hormonal Factors in Breast Cancer published a re-analysis of original data from 54 studies conducted in 25 countries, representing 90% of the then available global data [5]. Each contributing study had at least 100 cases of breast cancer and supplied broadly similar data to the coordinating unit for re-analysis. The re-analysis found that ever users of COCs had a small, but statistically significant, increased risk of being diagnosed with breast cancer compared with never users; summary relative risk (RR) 1.07 (95% confidence interval [CI] 1.03–1.11). The increased risk of breast cancer occurred while women used COCs and for a few years afterwards, before it wore off. Thus, compared with never users, the RR in current users was 1.24 (95% CI 1.15–1.33); former users who stopped 1–4 years previously RR 1.16 (95% CI 1.08–1.23); former users who stopped 5–9 years previously RR 1.07 (95% CI 1.02–1.13); and former users who stopped more than 10 years previously RR 1.01 (95% CI 0.96–1.05). Cancers diagnosed in COC users were more likely to be localised to the breast, even among women who stopped COCs more than 10 years previously; the RR of spread beyond the breast in all ever users compared with never users was 0.88 (95% CI 0.81–0.95). The pattern of risk was essentially the same irrespective of age, country of residence, family history of breast cancer, ethnic group, reproductive history, duration of use, and dose or type of pill used. A notable exception was risk among women who started COCs before 20 years of age; these women had larger relative risks of breast cancer during current and recent (within 5 years of stopping) use than women beginning at an older age, but similar risks more years after stopping.
These results were generally reassuring, especially for the first generation of COC users exposed for relatively short durations to preparations containing a high (50 μg or more) or medium (30–35 μg) dose of oestrogen accompanied by an older progestogen. Nevertheless, important gaps in our knowledge remained. For example, there was little information about use before age 20 years (only 14% of women in the dataset began using COCs in their teens); most pill use was of short duration (median 3 years); and uncertainty remained about the long-term risk of breast cancer more than 20 years after stopping COC use, especially among women who started use whilst a teenager. It was also unclear whether the observed effects were a ‘class’ effect seen with all COCs, or limited to particular formulations; or whether temporal changes in pill composition had changed the risk.
Since 1996, there have been more than 40 studies examining different aspects of the association between COC use and breast cancer incidence. Most of them were included in a systematic review and meta-analysis conducted as part of a comprehensive Agency for Healthcare Research and Quality (AHRQ) evidence report, Oral Contraceptive Use for the Primary Prevention of Ovarian Cancer, published in 2013 [6, 7]. This report considered papers published between 2000 and 2012, relating to a number of outcomes (breast, colorectal, endometrial and ovarian cancer; venous thromboembolism, stroke and myocardial infarction). Twenty-three studies provided information about ever use of COCs and breast cancer, compared with never use; a modest but borderline statistically significant increased risk was found (summary odds ratio (OR) 1.08, 95% CI 1.00–1.17). Fourteen studies looked at duration of use, with no relationship seen. Eleven studies examined time since last use, observing a diminishing increased risk over time: 0–5 years (OR 1.21, 95% CI 1.04–1.41), 5–10 year (OR 1.17, 95% CI 0.98–1.38), 10–20 years (OR 1.13, 95% CI 0.97–1.31), >20 years (OR 1.02, 0.88–1.18). These results are consistent with the re-analysis of earlier studies [5].
A trend of increasing breast cancer risk with longer duration of use was seen in the Danish Sex Hormone Register Study, a national data-linkage study published in 2017, of 11,517 incident breast cancers occurring during 19.6 million person-years observation of approximately 1.8 million women aged 15–49 years and living in Denmark between 1995 and 2012 [8]. The risk declined after stopping, although perhaps more slowly in women who had previously used COCs for long durations.
A third meta-analysis of 34 studies with information about pre-menopausal breast cancer risk, observed a slightly stronger effect among ever users compared with never users of COCs (OR 1.19, 95% CI 1.10–1.29) [9]. Parity did not appear to affect the risk, but women who used COCs before their first full-term pregnancy had a higher risk (OR 1.44, 95% CI 1.28–1.62) than those who used them afterwards (OR 1.15, 95% CI 1.06–1.26). In addition, the largest risk estimate was seen in women who used COCs for 4 or more years before their first full term pregnancy (OR 1.52, 95% CI 1.26–1.82). These results are compatible with the slightly stronger risk of breast cancer seen among women who start using COCs at a young age.
The AHRQ report considered papers published from year 2000 to maximise the proportion of women exposed to COC formulations similar to those currently on the market. Indirect assessments of the specific effects of different formulations, for example through the assignment of progestogen or oestrogenic potencies, are controversial [10]. Furthermore, simply grouping COCs by their oestrogen content ignores the biological effects of the accompanying progestogen (and vice versa). Most studies have been unable to look directly at the effects of specific formulations, partly because of insufficient study size or the lack of detailed, corroborated, information about COC use. In addition, as highlighted before, many women use a number of formulations during their reproductive lives, making it difficult to determine whether an altered risk associated with COC use is due to the pill currently/most recently taken, or a lingering effect from a previously used preparation. One recent case-control study in North America examined the association between exclusive use of a particular COC formulation (i.e. the use of that product only and no other COC) and breast cancer risk, among 2282 women with and 2424 women without breast cancer [11]. Thirty-eight different formulations were used, usually by only a few women. None of the ten formulations exclusively used by at least 50 women were associated with a significantly increased risk of breast cancer. Other recent studies looking at breast risk and specific formulations ignored any effects from previously used preparations [8, 12, 13]. Two found statistically significant variations in risk associated with specific formulations, although many comparisons were based on a small number of breast cancer cases and so lacked statistical power [12, 13]. The larger, Danish Sex Hormone Register Study, found most COC formulations examined were associated with an increased risk of breast cancer, with little evidence of important differences between products [8]. Until more data become available, it is best to assume that all of the numerous COCs currently on the market have a similar risk of breast cancer. Likewise, until robust data become available, non-oral forms of combined hormonal contraception (vaginal ring, patch or injectable) should be assumed to have the same breast cancer risk as COCs.
Each of the three longest running cohort studies in the world has now reported on breast cancer incidence or mortality among ever and never COC users, after at least 36 years’ follow-up [14,15,16,17,18]. None observed an increased risk of either outcome among ever users, indicating an absence of very long-term breast cancer risk from COCs available in the 1960s, 1970s and early 1980s. Time will tell whether this also applies to today’s products.
Most cases of breast cancer (even among those with a family history) occur in women without mutations on the breast cancer susceptibility genes, such as BRCA1 and BRCA2. Although the prevalence of these genes in the general population is low, they convey a greatly enhanced lifetime risk of both breast and ovarian cancer. Thus, compared to the roughly 12.5% lifetime risk among women in the United Kingdom (UK) general population, carriers of BRCA1 have a 60–90% and BRCA2 carriers a 45–80% lifetime risk of breast cancer [19]. Five studies published since 2000 were included in a meta-analysis for the AHRQ evidence report, examining breast cancer risk among BRCA1/2 mutation carriers [20]. There was a small, statistically non-significant, increased risk of breast cancer among carriers of both BRCA1 and BRCA2 mutations who were ever users of OCs, compared with never users (OR 1.12, 95% CI 0.93–1.58). Similar findings were found when carriers were examined separately (BRCA1 OR 1.19, 95% CI 0.92–1.55; BRCA2 OR 1.36, 95% CI 0.89–2.10). There was limited data about both duration and time since last use, with no consistent trends seen for either variable. Overall, the results suggest that there is no substantial difference in the relative risk estimates for breast cancer among COC users with each carrier type, which are similar to those seen in the general population.
The pattern of increased breast cancer risk in current and recent users, an inconsistent relationship with duration of use, and loss of effect after stopping COCs, does not fit with the usual model of carcinogenesis. Instead, it may reflect the promotion of tumours which have already started to develop. The tendency for COC users to have more localised tumours within the breast could be due to the earlier detection of disease in ever users versus never users although this preferential detection would have to persist for many years in order to account for the Collaboration Group’s observation of more localised cancers in ever users who stopped more than 10 years previously [5]. Alternative explanations include biological effects of COCs on tumour growth and risk of metastasis, or a combination of explanations.
The number of extra cases of breast cancer seen among COC users will depend heavily on the background incidence of breast cancer when they stop using this method of birth control. Many women stop using COCs before their mid-30s, when the background risk of breast cancer is low and so the absolute number of women affected is likely to be small. For example, the Collaborative Group on Hormonal Factors in Breast Cancer estimated that five extra cases of breast cancer will accumulate by the age of 40 for every 10,000 European or North American women who use COCs for 5 years between age 25 and 29 years [5]. The slightly higher RR seen among women who start COCs as a teenager (if real), will result in few, if any, extra cases of breast cancer, provided that such users stop using this method of birth control when the background risk of this cancer is still rare. Conversely, women who use COCs near their menopause have a higher background incidence of breast cancer, and so need to judge carefully whether other benefits outweigh the greater number of extra cases of breast cancer expected from such usage (perhaps 32 extra cases per 10,000 women who use COCs to the age 45) [5]. Current evidence does not suggest that women with BRCA1/2 mutations or a family history of either breast or ovarian cancer should avoid using COCs for contraception.
2.2 Progestogen-Only Contraceptives
Only 0.8% of data in the Collaborative Group on Hormonal Factors in Breast Cancer’s re-analysis related to oral progestogen-only products, and 1.5% injectable progestogens, mostly injectable depot medroxyprogesterone acetate (DMPA) [5]. The limited data, however, revealed a broadly similar pattern of breast cancer risk for progestogen-only products administered by either route to that of COCs (although the associated risk estimates were often statistically non-significant, with wide confidence intervals). Four studies have examined the breast cancer risk among users of injectable progestogen-only contraceptives since 1996 [8, 21,22,23]. One study of black South African women included 1664 cases with breast cancer and 1492 controls; compared with never users of hormonal contraceptives, the incidence of breast cancer was significantly increased in women who had exclusively used injectable contraceptives within the previous 10 years (OR 1.83, 95% CI 1.31–2.55), but not after 10 years (OR 1.08, 95% CI 0.82–1.43) [18]. The three other studies did not find an increased risk of breast cancer with current or recent [8, 21, 22], or any [21, 22], use of injectables although the number of women using these methods was often small.
Four studies have assessed breast cancer risk among users of progestogen-only pills [8, 23,24,25]. One North American study found no increased risk among exclusive current or past users of progestogen-only pills [24]. A Norwegian-Swedish study observed an increased risk among current and recent users of COCs and progestogen-only pill, but not exclusive users of progestogen-only products [25]. The third investigation, of black South African women, found a significantly increased risk of breast cancer among those within 10 years of stopping, but not thereafter [23]. The fourth, Danish Sex Hormone Register Study, found an increased risk of breast cancer among current or recent user of progestogen-only pills containing levonorgestrel, but not those with norethisterone or desogestrel [8]. This study was unable to examine the risk among exclusive users of progestogen-only products.
Neither of two studies assessing implantable progestogen-only contraceptives observed an increased risk of breast cancer among users although very few women used this method of birth control [8, 22].
Current or recent users of the levonorgestrel-releasing intrauterine system (LNG-IUS) in the Danish Sex Hormone Register Study had a small but statistically significant increased risk of breast cancer compared with never users of hormonal contraception (RR 1.21, 95% CI 1.11–1.33) [8]. An unknown proportion of the LNG-IUS users will have used COCs beforehand. It is possible, therefore, that at least part of the observed risk could be a hangover effect from previous COC usage, although evidence of a persistent increased risk in women who had used the LNG-IUS for more than 10 years argues against such an explanation. Another study of 93,843 women living in Finland and using the LNG-IUS for the treatment or prevention of menorrhagia observed a higher than expected incidence of breast cancer among LNG-IUS users (standardised incidence ratio [SIR] 1.19, 95% CI 1.13–1.25) [26]. A later paper found that both ductal and lobular breast cancers were increased among users, with the highest risk estimates among women who had purchased the contraceptive at least twice [27]. These results contradict a large post-authorisation safety study conducted for the European Health Authorities, in which 5113 women with breast cancer and younger than 50 years and 20,452 controls were identified in Finland and Germany; neither current nor ever users of the LNG-IUS had an increased risk of breast cancer compared with users of a copper-containing intraunterine device (Cu-IUD) [28]. This study included some participants who were also likely to be involved in a case-control study of breast cancer among Finnish women aged 20–60 years [29]. An increased risk of breast cancer was seen among exclusive users of the LNG-IUS in post-menopausal (Hazards Ratio [HR] 1.48, 95% CI 1.10–1.99), but not pre-menopausal (HR 0.79, 95% CI 0.54–1.17), women; both compared with never-users of any hormonal contraceptive. Three other studies, conducted in Finland [30], Norway [31] and Israel [32], did not observe an increased risk of breast cancer among users of the LNG-IUS.
Currently there is insufficient evidence to state with confidence whether progestogen-only contraceptives are associated with a different risk of breast cancer to that observed with COCs. It is noteworthy that randomised trials and observational studies in older women indicate that the addition of progestogen to oestrogen for MHT increases the risk of breast cancer above that of oestrogen alone [33, 34]. Until more data becomes available, it is prudent to assume that progestogen-only contraceptives, including the LNG-IUS, have the same breast cancer risk as COCs.
2.3 Non-Hormonal Intrauterine Devices
An analysis of over 66,000 women, recruited between 1997 and 2000 for the Shanghai Women’s Health Study in China, provided very limited evidence of no change in breast cancer risk among ever users of the IUD (type unknown) [35].
2.4 Female Sterilisation
Worldwide female sterilisation is the most commonly used method of modern contraception; used by an estimated 19% of married/in-union women aged 15–19 years in 2015 [36]. Researchers examining possible cancer effects of this method have rarely specified what procedure had been done; for instance, electrocoagulation of the fallopian tubes, tubal ligation, occlusion with spring, titanium clips or silicone rings; partial/total salpingectomy or hysteroscopic tubal occlusion [37].
A meta-analysis published in 2013 of four case-control and four cohort studies found no difference overall in breast cancer incidence among women who had been sterilised, compared with those who had not undergone this procedure (summary OR 0.97, 95% CI 0.84–1.09) [38]. There was inconsistency in the results of case-control studies, with one North American study finding an increased risk of breast cancer, and a smaller Korean study finding a protective effect. There was no evidence of serious heterogeneity among the cohort studies. A study not included in the meta-analysis looked at breast cancer mortality and found a reduced risk of death from breast cancer among sterilised women (adjusted RR 0.82, 95% CI 0.70–0.96) [39]. Another study not included in the meta-analysis compared observed versus age- and calendar-period expected breast cancer incidence rates among women undergoing reproductive surgical procedures in Ontario, Canada; tubal ligation before the age of 45, and after the age of 55, was associated with a reduced risk of breast cancer [40]. Subsequent studies [41, 42] have not observed an altered risk of breast cancer in association with tubal sterilisation, including the Million Women Study, which observed more than 60,000 cases of breast cancer occurring among almost 1.3 million women who contributed nearly 17 million person-years of follow up [41]. Overall, the evidence does not strongly suggest that women change their breast cancer risk if they choose to undergo tubal sterilisation.
3 Cervical Cancer
Although its incidence and mortality has been declining in large parts of the world, cervical cancer remains the leading type of cancer in many Sub-Saharan Africa and South-Eastern Asia countries [1, 2]. Globally, there were an estimated 570,000 new cases and 311,000 deaths from cervical cancer in 2018. A virtually necessary (but not sufficient) cause of cervical cancer is infection with an oncogenic type human papillomavirus (HPV). Important known co-factors include smoking, high number of full-term pregnancies, oral contraception and immunosuppression (particularly arising from human immunodeficiency virus [HIV] infection) [4]. The declines in cervical cancer incidence are thought to be because of improving socioeconomic circumstances, declining levels of persistent high-risk HPV infection and, where available, effective screening. The effective implementation of worldwide HPV vaccination programmes, accompanied by comprehensive screening programmes (especially for unvaccinated women), offers the potential to virtually eradicate this cancer. It has been estimated, for example, that the age-standardised annual incidence of cervical cancer in Australia will be less than 4 per 100,000 by 2028 (range 2021–2035) as a result of the implementation of extensive preventative measures [43].
3.1 Combined Oral Contraceptives
The International Collaboration of Epidemiological Studies of Cervical Cancer conducted a re-analysis of individual participant data of 11,170 women with invasive cervical cancer, 5403 women with cervical intraepithelial neoplasia grade 3 (CIN3) and 35,509 controls from 24 (of 35 eligible) studies to examine patterns of COC use and cervical cancer [44]. The reanalysis found an increased risk of invasive cervical cancer among current users, an effect which strengthened with prolonged use (5 or more years of user versus never user: RR 1.90, 95% CI 1.69–2.13). This elevated risk waned after stopping COCs, and had returned to that of never users by 10 years since last use. The pattern of risk estimates was similar among women likely to have had cervical screening and those not screened, and in women positive for high-risk types of HPV. The re-analysis was unable to consider the hormonal content of different COCs, or the effects of specific products. Published data from the mostly small studies not included in the re-analysis suggested similar patterns of relative risks.
Since the International Collaboration of Epidemiological Studies of Cervical Cancer’s re-analysis, most studies have not found an association between ever use of COCs and cervical cancer incidence [18, 23, 45, 46], or cervical cancer mortality [14, 17]. An exception was the Oxford-Family Planning Association Contraceptive Study which found a more than three-fold (RR 3.4, 95% CI 1.6–8.9) increased cervical cancer risk among ever users of COCs [16]. Another was the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study which also found an increased risk with ever use of COCs (HR 1.6, 95% CI 1.1–2.3) [47]. An occupational cohort study of women employed by the Shanghai Textile Industry Bureau found a reduced risk associated with ever COCs use, although the analysis included only one exposed case (RR 0.13, 95% CI 0.02–0.96) [48]. Ever use, however, may mask effects seen during current and recent use. Several of the recent studies reported a higher risk of cervical cancer in women who have used COCs for longer durations [16, 45, 46, 49] and observed a waning of risk with increasing time since last use [16, 18, 23, 45]. The more recent studies, therefore, are generally in line with the International Collaboration’s findings [44].
The pattern of risk of cervical cancer among COC users—an increased risk during current use which wanes relatively soon after stopping—is similar to that of breast cancer. Thus, like breast cancer, the extra number of cases of cervical cancer seen among COC users will depend on the background incidence of the disease when the COC is stopped. The International Collaboration of Epidemiological Studies of Cervical Cancer estimated that in more developed countries 5 years use of COCs from age 20 would result in two extra cases of cervical cancer by age 50 per 10,000 users; and 10 years use seven extra cases [44]. In less developed countries, where the incidence of cervical cancer is generally higher (and where preventative services are often absent), the corresponding figures are two and 10 extra cases per 10,000 users.
3.2 Progestogen-Only Contraceptives
Only 10 studies in the International Collaboration of Epidemiological Studies of Cervical Cancer’s re-analysis assessed progestogen-only products [44]. Risk estimates for progestogen-only pills could not be calculated because only 1% of cervical cancer cases and fewer than 1% of controls had ever used these products. An increased risk of cervical cancer was found for women who had used injectable progestogen-only contraceptives for 5 years or longer, compared with never users (RR 1.22, 95% CI 1.01–1.46), with no clear effect of time since last use. The risk estimates associated with injectable progestogen-only contraceptives use were similar, regardless of whether COCs had also been used.
The Johannesburg Cancer Case Control Study examined injectable progestogen-only contraceptive use and cervical cancer risk in 2182 women with cervical cancer and 1492 controls [23]. This setting was particularly useful as injectable progestogen-only contraceptives are used more often, and for longer periods, in South Africa than elsewhere in the world. The study found that, compared to never users of hormonal contraceptives, women who had only used injectable contraceptives and who were less than 10 years from stopping were more likely to have cervical cancer (OR 1.58, 95% CI 1.16–2.15). When both time since last use and duration of use were examined, the risk of cervical cancer diminished with increasing time since last use and was not related to duration of use. Further adjustment for number of previous Papanicolau (Pap) smears or HIV status did not affect the patterns of cervical cancer risk.
To date, only one nationwide study has examined use of the LNG-IUS and risk of cervical cancer; a cohort of Finnish women aged 30–49 years who were using the LNG-IUS for menorrhagia [26]. There was no evidence of an increased risk of cervical cancer overall (SIR 0.90, 95% CI 0.69–1.15), or cervical adenocarcinoma specifically (SIR 1.18, 95% CI 0.74–1.79). Further studies of progestogen-only contraceptives, particularly of the LNG-IUS, are needed in populations using these products for contraceptive reasons.
3.3 Non-Hormonal Intrauterine Devices
The most recent systematic review and meta-analysis to examine the association between use of an IUD and risk of cervical cancer evaluated all studies published to July 2016 [50]. Data from 16 out of 17 studies, relating to 4945 women with incident cervical cancer and 7537 women without, could be harmonised and included in the meta-analysis. Any use of an IUD was associated with a reduced risk of incident cervical cancer (summary OR 0.64, 95% CI 0.53–0.77). Similar results were found when the data were stratified by whether the included studies adjusted for possible confounding by socioeconomic status, smoking history, age at first intercourse, number of lifetime partners, HPV status, number of Pap smears and gravidity. The review could not examine the effects of duration of use. Neither could it look at type of IUD although the time and place of most studies suggested that the IUDs were unlikely to include the LNG-IUS. It is thought unlikely that the observed reduced risk of cervical cancer was due to the detection of cervical abnormalities at the time of IUD fitting, as the use of stains, such as acetowhite, for identifying abnormalities was not routine practice in the included studies [50]. An earlier pooled analysis of 26 epidemiological studies concluded that there was no association between IUD use and cervical HPV [51]. These reviews have led to the hypothesis that IUDs might protect against cervical cancer through the prevention of HPV infection progression to cervical cancer. Importantly, there is no evidence to suggest that IUDs increase the risk of cervical cancer.
3.4 Female Sterilisation
Studies into the possible relationship between tubal ligation and cervical cancer were stimulated by the hypothesis that tubal ligation leads to disrupted ovarian function causing hormonal changes, which, in turn, influences the cervical epithelium and cervical cancer risk. A case-control study of 272 women aged 30–77 years with newly-diagnosed squamous cell cervical cancer and 893 community controls living in China did not find an association between tubal ligation and cervical cancer (OR 1.08, 95% CI 0.81–1.44) [52]. Similarly, a hospital-based case-control study conducted in eight countries and involving 2339 women with squamous cervical cancer and 13,506 controls did not find an altered risk of cervical cancer among all women who had had a tubal sterilisation (RR 0.96, 95% CI 0.86–1.07) [53]. However, a reduced risk of cervical cancer was found among women previously screened for cervical cancer, aged 36 or older and within 5 years of their tubal ligation (RR 0.77, 95% CI 0.59–0.99) [53]. This reduced risk within 5 years of tubal ligation was apparent regardless of the frequency of Pap smears or age at first smear. A reduction in cervical cancer risk was not observed in women who had never participated in cervical screening. The authors of the study concluded that any association between altered cervical cancer risk and tubal ligation was due to differences in cervical screening rather than disrupted ovarian function.
A cohort study followed 65,232 Danish women who had tubal sterilisation between 1977 and 1993 for 605,631 person-years; it did not find an overall reduced risk of cervical cancer associated with this contraceptive method (SIR 0.94, 95% CI 0.8–1.1) [54]. In the first year after sterilisation, a higher risk estimate (SIR 1.21, 95% CI 0.7–1.9) was found, together with an increased risk of cervical intraepithelial neoplasia grade 3 (SIR 1.7, 95% CI 1.5–2.0); suggesting a screening effect in connection with tubal sterilisation, i.e. women having the procedure probably also having a Pap smear which led to the detection of cervical abnormalities around the time of sterilisation. In contrast to the findings of these studies, a cross-sectional ‘Study to Understand Cervical Cancer Endpoints and Determinants’ (SUCCEED) of 2004 women in the United States of America (USA), reported an increased risk of cervical cancer in women with tubal ligation even though women undergoing this procedure were less likely to have had Pap screening during the previous 5 years compared with women using other contraceptive methods [55]. The most recently conducted study, the UK Million Women Study, did not find an association between tubal ligation and cervical cancer (RR 0.98, 95% CI 0.83–1.15) [42]. Taken together with new evidence that tubal ligation does not materially alter hormone levels, the sparse evidence base does not suggest a true biological relationship between tubal sterilisation and cervical cancer.
4 Ovarian Cancer
Worldwide, there were 295,414 incident cases of ovarian cancer in 2018, and 184,799 deaths—the second highest number of deaths of all gynaecological malignancies [1, 2]. Many symptoms of ovarian cancer are vague, resulting in many women being diagnosed with advanced staged disease. Thus, survival after diagnosis is poorer than for most other cancers; overall global age-standardised 5-year survival rate is 30–40% [56]. Many risk factors associated with an elevated risk of ovarian cancer are those which influence the lifetime number of, and breaks between, ovulations and levels of sex hormones. Older age, nulliparity, infertility, never having breastfed, history of endometriosis, diabetes, breast, endometrial or colorectal cancer, MHT, family history of ovarian cancer, BRCA1/BRCA2 gene mutations, Lynch Syndrome and Peutz-Jeghers Syndrome have been associated with an increased risk of ovarian cancer [4]. Conversely, parity, breastfeeding, COCs, tubal ligation and hysterectomy appear to reduce ovarian cancer risk.
4.1 Combined Oral Contraceptives
Previous research has shown a reduced risk of ovarian cancer in COC users, a protective effect which increases with duration of use and which persists for many years after stopping [16,17,18, 57,58,59,60,61,62]. For example, in a reanalysis of data from 45 epidemiological studies including 23,257 women with ovarian cancer and 87,303 controls, compared with never users, the RR in users of COCs for less than 1 year was 1.00 (99% CI 0.91–1.10); 1–4 years RR 0.78 (99% CI 0.73–0.83); 5–9 years RR 0.64 (99% CI 0.59–0.69); 10–14 years RR 0.56 (99% CI 0.50–0.62); 15+ years RR 0.42 (99% CI 0.36–0.49) [57]. Results by time since last use were: current and less than 10 years previously RR 0.57 (99% CI 0.50–0.64); 10–19 years previously RR 0.67 (99% CI 0.62–0.73); 20–29 years previously RR 0.76 (99% CI 0.71–0.81); 30+ years RR 0.86 (99% CI 0.76–0.97). The COCs assessed in the re-analysis, and most other studies, usually contained a high or medium dose of oestrogen combined with an older progestogen. Evidence regarding contemporary hormonal contraception, however, is starting to emerge.
A report from the Danish Sex Hormone Register Study included 1249 incident ovarian cancers occurring during 21.4 million person-years observation between 1995 and 2014; compared with never users, current or recent users (RR 0.58, 95% CI 0.49–0.68) and former users (RR 0.77, 95% CI 0.66–0.91) of any hormonal contraception had a reduced risk of ovarian cancer [63]. The protective effect among current users got stronger the longer that women used hormonal contraception, and persisted up to 10 years after stopping. Most of the hormonal contraception usage related to COC use. These results support previous findings [57], and indicate a similar protection resulting from currently available COCs as older products. Furthermore, there was little suggestion of major variations in protective effects according to the progestogen content of the COC, or tumour type.
The pattern of protection during and for many years after stopping COC use has resulted in a profound public health benefit. The Collaborative Group on Epidemiological Studies of Ovarian Cancer estimated that 200,000 cases of ovarian cancer have been prevented by oral contraceptives in high income countries over the past 50 years, and 100,000 deaths [57]. These numbers will increase substantially in the future.
4.2 Progestogen-Only Contraceptives
Few studies have examined the possible relationship between injectable DMPA contraceptives and ovarian cancer risk [23, 63,64,65]. Two case-control studies that investigated exclusive use of injectable DMPA contraceptives found ORs of 0.3 (95% CI 0.1–1.2) [65] and 0.35 (95% CI 0.17–0.71) [23]. A recent analysis of ovarian cancer outcomes in the Danish Sex Hormone Register Study reported an increased risk of ovarian cancer among DMPA users, compared with never users of hormonal contraception [63]. This estimate, however, was based on a small number of ovarian cancers and a very small period of observation, resulting in very imprecise risk estimates. Other progestogen-only products did not appear to change the risk of ovarian cancer risk in the Danish study, although the evidence was limited because few women in the study were exclusive users of progestogen-only contraceptives.
A data-linkage study in Finland compared the incidence of ovarian cancer among 93,843 women aged 30–49 years and using an LNG-IUS for menorrhagia between 1994 and 2007, with the incidence in the general population; it found a SIR of 0.60 (95% CI 0.45–0.76) [23]. The reduced risk was seen with mucinous, endometrioid and serous ovarian carcinomas [66]. Similarly, the Norwegian Women and Cancer Study found a reduced risk of epithelial ovarian cancer among ever users of the LNG-IUS (RR 0.53, 95% CI 0.32–0.88, compared with never users [31]. These Finnish and Norwegian studies adjusted for several confounders, including ever use of oral contraceptives. However, neither study was able to examine the risk among women who had exclusively used an LNG-IUS. It is possible, therefore, that the observed reduced risk of ovarian cancer among LNG-IUS users was because of persisting protective effects of previous COC use. Overall, there is currently insufficient evidence to conclude whether progestogen-only products, per se, change the risk of ovarian cancer among users.
4.3 Non-Hormonal Intrauterine Devices
Few studies, particularly prospective investigations, have examined whether the IUD affects a user’s risk of ovarian cancer. IUDs are commonly used in Asian countries; for example, 55.6% of women recruited to the Shanghai Women’s Health Study had used an IUD, more than half for at least 20 years [67]. This study of 70,259 women aged 40–79 years accumulated nearly 900,000 person-years of observation and found that, compared to never users of an IUD, users for at least 20 years had a reduced risk of ovarian cancer (HR 0.62, 95% CI 0.40–0.97). Similar patterns of reduced risk among long-term users were found when the analysis was restricted to IUD-users only, i.e. when the comparator group was women with less than 12 years IUD use. After 28 years of prospective follow-up, the North American Nurses’ Health Study I found an increased risk of ovarian cancer (RR 1.76, 95% CI 1.08–2.85) among women who reported ever using an IUD [68]. Most of the IUD use in the Shanghai Women’s Health Study was between 1975 and 1990, of the stainless steel ring [67]; whereas most of the IUD use in the Nurses’ Health Study I occurred during the 1970s and 1980s [68], and was likely to be the plastic Dalkon Shield. Neither of these studies, therefore, provide information about the ovarian cancer risks associated with the now commonly used copper-containing IUDs. The mechanism(s) by which IUDs might influence ovarian cancer risk remains unclear.
4.4 Female Sterilisation
Although a number of studies have investigated ovarian cancer risk in relation to tubal ligation, most have been too small to examine method-specific risks [69]. Several meta-analyses have examined the association between tubal ligation and the risk of ovarian cancer [70,71,72,73]; all found a protective effect, ranging between a 29% and 34% reduction. The protective effect appears to be the same regardless of age at tubal ligation, persists for at least three decades [72] and is consistent in different populations, including BRCA mutation carriers [71] and African American women [74]. In a pooled analysis of 7942 women with invasive ovarian cancer from 13 population-based case-control studies, tubal ligation was associated with a reduced risk of serous (high grade), mucinous, endometrioid and clear cell invasive ovarian cancers [72] However, the size of the risk reductions differed by histological type, with greatest reductions for clear cell and endometrioid, intermediate for mucinous and smallest for high grade serous type—suggesting different mechanisms of action for different types of ovarian cancer.
The mechanism by which tubal ligation might reduce ovarian cancer risk has not yet been established. Suggested theories [75] include the prevention of inflammatory or carcinogenic substances, such as talc, ascending the vagina to the ovaries or tubal ligation stopping the transportation of malignant cells from the endometrium or fallopian tube during retrograde menstruation.
4.5 High Risk Groups
Up to 15% of all ovarian cancers can be attributed to BRCA1 or BRCA2 mutations. Women who are BRCA mutation carriers have a greater risk of ovarian cancer than women who are BRCA-negative; compared to an approximate 2% lifetime risk among women in the UK general population, BRCA1 carriers have a 40–60% and BRCA2 carriers a 10–30% lifetime risk of ovarian cancer [19]. The AHRQ report included a meta-analysis of four studies (three case-control and one cohort), which found that ever use of COCs was associated with a reduced ovarian cancer incidence in women who were either BRCA1 or BRCA2 carriers; OR 0.58 (95% CI 0.46–0.73) [6]. This protective effect was of similar magnitude to that derived from general population studies. The AHRQ report also tried to consider the influence of COCs in women not known to be BRCA1 or BRCA2 gene mutation carriers but who have an increased risk of ovarian cancer because of a family history of breast or ovarian cancer [6]. Few studies have looked at this issue and a meta-analysis could not be conducted due to differences in both the definitions used for family history and against whom the COC users were compared.
A recent meta-analysis identified three case-control studies and one prospective cohort study which examined tubal ligation in relation to ovarian cancer risk in BRCA mutation carriers [70]. The summary OR for ovarian cancer after tubal ligation in BRCA1 carriers in the case-control studies was 0.69 (95% CI 0.53–0.89) and in BRCA2 carriers 0.73 (95% CI 0.42–1.24) [76]. The prospective study reported an RR of 0.42 (95% CI 0.22–0.80) in BRCA1 carriers and RR 0.47 (95% CI 0.18–1.21) in BRCA2 carriers.
Studies of ovarian cancer in high risk women are sparse, and often small in size. Although there is no evidence to suggest that women at high risk of ovarian cancer should avoid using COCs or tubal ligation for contraception, the evidence-base is insufficient to recommend the use of COCs for the primary prevention ovarian cancer, particularly when other potential benefits and harms are considered [6].
5 Endometrial Cancer
Cancer of the corpus uteri (mostly endometrial) is estimated to be the sixth most frequent cancer in women worldwide, with more than 382,000 new cases and 89,929 deaths in 2018 [1, 2]. Factors associated with a raised risk of endometrial cancer include: older age, menstrual (early menarche, late menopause), reproductive (nulliparity), exogenous hormones (unopposed oestrogen), family history of endometrial cancer (and of colorectal cancer in close relatives), personal history of polycystic ovary syndrome, endometrial hyperplasia, obesity, diabetes, any previous cancer, Lynch syndrome and use of tamoxifen [4]. Factors associated with a reduced endometrial cancer risk include: COCs, IUDs, late age at first or last birth, smoking and high parity.
5.1 Combined Oral Contraceptives
The Collaborative Group on Epidemiological Studies of Endometrial Cancer examined the association between COC use and risk of endometrial cancer in an individual participant re-analysis of 27,276 women with endometrial cancer and 115,743 controls from 36 studies [77]. The overall relative risk between ever and never users of oral contraceptives was 0.69 (95% CI 0.67–0.72). The protective effect was apparent in current users, an effect that strengthened with longer durations of use; reducing by nearly a quarter (RR 0.76, 95% CI 0.73–0.78) for every 5 years of use. Thus, the risk of endometrial cancer was estimated to halve with 10–15 years usage. The median age at diagnosis of endometrial cancer was 63 years, so most women in the re-analysis had stopped using COCs many years previously—the protective effect remained for more than 30 years after last use. The effects varied by tumour histology with strong risk reductions in ever users of COCs for type I and type II tumours but not for the much rarer uterine sarcoma.
Since the Collaborative Group on Epidemiological Studies of Endometrial Cancer’s findings were published, several studies have considered the very remote effects of COCs on endometrial cancer risk [17, 18, 61]. The Nurses’ Health Study I accumulated 3.6 million person-years of observation during 36 years of follow-up; ever use of COCs was not associated with uterine or endometrial cancer mortality (HR 0.81, 95% CI 0.63–1.03) [17]. The UK Royal College of General Practitioners’ (RCGP) Oral Contraception Study amassed over 1.2 million person-years of observation after 44 years of follow-up; ever users of COCs had a reduced risk of endometrial cancer (RR 0.66, 95% CI 0.48–0.89) [18]. Assuming that this finding reflects a true relationship, it was estimated that a third of endometrial cancers that would have occurred among ever users of COCs in this study had been prevented by this method of birth control [18]. The third study, the National Institutes of Health—American Association of Retired Persons (NIH-AARP) Diet and Health Study of nearly 200,000 mostly post-menopausal women also found a reduction in incident endometrial cancer (HR 0.78, 95% CI 0.70–0.86) in ever users of COCs [61]. Regardless of age at study recruitment (age 60 or younger, or over 60), longer durations of use were associated with stronger risk reductions.
Two recent papers have provided evidence that currently available COCs are associated with similar endometrial cancer benefits to those seen with older products [78, 79]. The Collaborative Group on Epidemiological Studies of Endometrial Cancer estimated that 400,000 cases of endometrial cancer had been prevented by COC in high income countries over the past 50 years, including 200,000 cases between 2005 and 2014 [77]. These numbers will increase substantially in the future.
5.2 Progestogen-Only Contraceptives
Research into the endometrial cancer risks associated with progestogen-only contraceptives (especially progestogen-only pills and injectable DMPA) has been hampered by the small number of women studied who were exclusive users of these products [80].
The LNG-IUS thins the endometrium and so may influence endometrial cancer risk. The Epidemiology of Endometrial Cancer Consortium pooled data from 14 case-control and four cohort studies to investigate the endometrial cancer risk associated with different types of IUD [81]. Hormone-releasing devices were not associated with endometrial cancer risk (adjusted OR 0.97, 95% CI 0.44–2.14), although few women had used these contraceptives. A data-linkage study of 93,843 women in Finland who had used the LNG-IUS for menorrhagia found that LNG-IUS users had a reduced risk of any type of corpus uteri cancer, compared to that expected from national incidence data (SIR 0.59, 95% CI 0.45–0.77), and of endometrial adenocarcinoma (SIR 0.46, 95% CI 0.33–0.64) [26]. Risk reductions were more pronounced in women who had used two or more devices. However, the study was unable to adjust for prior use of COCs, whose protective effects on the endometrium are known to be long lasting. The Norwegian Women and Cancer Study of 104,380 women also reported a reduced risk of endometrial cancer among 9146 ever users of the LNG-IUS (RR 0.22, 95% CI 0.13–0.40), without any evidence of differences when comparing ever and never users of COCs [31]. Further studies are required to ascertain the effects of the LNG-IUS on endometrial cancer risk in women using this product for contraceptive purposes. Until more information becomes available, it is assumed that progestogen-only products confer the same endometrial cancer protection as COCs.
5.3 Non-Hormonal Intrauterine Devices
All IUDs, regardless of whether they also contain hormones, elicit a local foreign body inflammatory reaction in the uterus which may have long-term consequences for the endometrium [81]. The Epidemiology of Endometrial Cancer Consortium pooled analysis found a protective association overall with ever use of any type of IUD (pooled OR 0.81, 95% CI 0.74–0.90) [81]. Inert IUDs were associated with a reduced risk of endometrial cancer (pooled OR 0.69, 95% CI 0.58–0.82), but not copper IUDs (pooled OR 0.89, 95% CI 0.66–1.21). Among users of inert IUDs, older age at last use, increasing duration of use and recency of use were associated with a reduced risk of endometrial cancer. There was no evidence of effect modification of the relationship between any type of IUD use and endometrial cancer by ever use of COCs.
5.4 Female Sterilisation
It has been suggested that tubal ligation could prevent endometrial cancer by stopping the transport of premalignant or malignant cells from the fallopian tubes to the uterus. A USA case-control study of 437 cases of endometrial cancer and 3200 controls aged 20–54 years did not find a reduced risk of endometrial cancer with tubal ligation after adjustment for parity and age (OR 0.87, 95% CI 0.63–1.20) [82]. Another US case-control study of 405 cases and 297 controls also did not find an association between tubal sterilisation and endometrial cancer after allowing for age, parity and COC use (OR 1.4, 95% CI 0.8–2.4) [83]. Protective effects were also absent in the Women’s Health Initiative (WHI) Observational and Dietary Modification Study conducted in the USA (HR 0.97, 95% CI 0.81–1.17) [84] and the Million Women Study conducted in the UK (RR 0.98, 95% CI 0.93–1.03) [42].
A data-linkage study in Denmark followed 65,232 women from the date of their sterilisation for a total of 643,761 person-years, and compared their incidence of endometrial cancer with that expected from national incidence data; the SIR was of borderline significance—0.70 (95% CI 0.5–1.0) [54]. The study, however, could not account for previous OC use and no relationship was found between time since operation and endometrial cancer risk. The NRG Oncology/Gynecologic Oncology Group 210 Trial examined the association between tubal ligation and endometrial carcinoma stage and mortality in 4489 women with well-characterised endometrial carcinoma [85]. Women who had previously had a tubal ligation were less likely to present with stage III (OR 0.63, 95% CI 0.52–0.78), or stage IV (OR 0.14, 95% CI 0.08–0.24), than stage I disease. After allowing for these differences in staging, tubal ligation was not associated with any mortality benefit. The largest study to date has followed a cohort of more than five million women living in Sweden, of which 80,765 had tubal ligation, for more than 123,000,000 person-years [86]. After adjustment for age, parity, calendar time and education, tubal ligation was associated with a reduced risk of endometrial cancer (HR 0.73, 95% CI 0.65–0.83). However, data regarding COC and MHT use were only available for the final 5 years of study follow-up, so their possible influence on the relationship between tubal ligation and endometrial cancer could not be assessed.
Overall, the evidence does not suggest a strong relationship between tubal ligation and altered endometrial cancer risk.
5.5 Women With Lynch Syndrome
An estimated 5% of endometrial cancers are attributed to an inherited genetic predisposition to cancer [87]. Lynch syndrome (or hereditary nonpolyposis colorectal cancer, HNPCC syndrome) is an autosomal-dominant disorder caused by a germline mutation in a mismatch repair gene. Depending on the mismatch repair gene affected, the cumulative risk of endometrial cancer by age 70 in women with Lynch syndrome is estimated to be between 40% and 60% [86]. Despite these large lifetime risks, the influence of hormonal contraceptives on endometrial cancer risk in women with Lynch syndrome has received little attention. To explore the potential of progestogen to prevent endometrial cancer in this high-risk group, a randomised controlled trial examined the short-term effect of DMPA and the COC on the endometrium of 51 women with Lynch syndrome [88]. It found a significant decrease in endometrial epithelial proliferation in women using either hormonal contraceptive. This suggests that women with Lynch syndrome respond normally to short-term progestogens, and suggests an alternative method of reducing endometrial cancer risk (rather than hysterectomy). These findings are supported by those from a retrospective cohort study of 1128 women (mean age 40.6 years, standard deviation 11.3) with Lynch syndrome which investigated hormonal factors and endometrial cancer risk [89]. Compared with never users, ever users of hormonal contraceptives for at least 1 year had a lower risk of endometrial cancer (HR 0.39, 95% CI 0.23–0.64). Further studies of this high-risk group of women are needed.
6 Colorectal Cancer
In 2018, there were approximately 820,000 new cases of, and nearly 400,000 deaths from, colorectal cancer in women worldwide; making it the third most common cancer among women (Figs. 11.1 and 11.2) [1, 2]. Familial (family history of colorectal cancer and adenomatous polyps) and genetic (MLH1, MLH2 and other mutations) factors contribute to only a small proportion of cases. Important factors linked to an increased risk of colorectal cancer include personal characteristics (being tall and having a history of: adenomatous polyps, inflammatory bowel disease, type II diabetes mellitus) and environmental/lifestyle factors (some aspects of diet, such as red and processed meat, physical inactivity, excess body weight, smoking, heavy alcohol intake) [4]. Other aspects of diet, for instance whole grains and fibre, MHT and aspirin intake appear to be protective.
6.1 Combined Oral Contraceptives
More than 25 case-control and cohort studies have investigated whether COCs are associated with an altered colorectal cancer incidence. Virtually all investigations have looked at ever use of COCs, mostly in post-menopausal women. Early studies were often limited by low levels of COC use and the small number of cancers included. While several early case-control studies suggested an increased risk of colorectal cancer among ever users of COCs [90, 91], most indicated a reduced risk (although not necessarily with statistical significance). Three meta-analyses have summarised the accumulating evidence [7, 92, 93]; the latest up to mid 2012 [7]. Each reported a statistically significant reduced summary OR between ever and never users of COCs; for colorectal cancers combined [7, 92, 93], and colon and rectal cancer separately [92, 93]. For example, the most recent meta-analysis of 11 studies published between 2000 and 2012 in English, reported a summary OR of 0.86 (95% CI 0.78–0.95) [7]. There was no evidence of a relationship with duration of use in the ten studies examining this aspect of usage. The two earlier meta-analyses also found tentative evidence of a stronger protective effect with more recent use [92, 93]. One case-control study of ever use of hormonal contraception (birth control pills or hormonal implants/injections used for contraception), observed similar size reductions in risk of colorectal cancer among women meeting the screening criteria for Lynch syndrome as those seen in women without a family history of the cancer [94].
Results from cohort studies reporting since 2012 [16,17,18, 93,94,95,96,99] or not included in the last meta-analysis [15, 100], have not provided consistent evidence of a protective effect among ever users of COCs—for either colorectal cancer incidence or mortality. The studies included the NIH-AARP Study (approximately 200,000 women followed) [95, 100], the Million Women Study (approximately 1.3 million women followed) [97], and the WHI Observational Study (more than 93,000 women followed) [98]. Other papers included prolonged follow-up of the Nurses’ Health Study I (up to 30 years) and Nurses’ Health Study II (up to 19 years) [17, 96], the Oxford-Family Planning Association Contraceptive Study (up to 42 years) [15, 16], and the RCGP Oral Contraception Study (up to 44 years) [18]. Ever users of COCs did not have a significantly different incidence of colorectal cancer to that of never users in six of the eight studies [16, 96, 97, 99, 100]. Exceptions were the RCGP [18] and WHI [98] studies, which both found a significantly reduced incidence of colorectal cancer among ever users compared with never users. None of the three papers looking at death from colorectal cancer found a protective effect from COC use [15, 17, 95].
It is difficult to reconcile these latest results from the summary estimates produced by the meta-analyses. Each study has allowed for a varying number of potential confounding factors. An important possible confounder is use of MHT; past users of COCs are more likely to use MHT later in life, and MHT has been found to reduce the risk of colorectal cancer in observational studies and clinical trials [101]. While some studies with statistically significant protective effects among COC users have adjusted for MHT use, other have not; and some studies not showing a significant reduction have also adjusted for MHT (which should result in an apparent reduced risk among COC users if MHT use were confounding the results). Many of the early studies with a low prevalence of COC use are also likely to have a low level of MHT usage, providing further evidence against a strong confounding effect from MHT use. All of the women in the latest publications were post-menopausal, with most ever users of COCs having stopped many years previously. It is likely, therefore, that most of the COC use related to preparations with high- or medium-doses of oestrogen accompanied by older progestogens; similar to those used by many participants in the studies included in the meta-analyses. Nearly all of the studies so far have only assessed ever use of COCs. It could be that COCs (at least with older products) are associated with a protective colorectal cancer effect during current and recent use, which declines over time resulting in no association being observed in ever users who stopped many years previously. Such an explanation, however, does not explain the protective findings seen in the WHI [98] and RCGP [18] studies. Importantly, none of the recent studies have suggested an increased risk of colorectal cancer among ever users. New studies looking at current and recent use of contemporary COCs are needed. Information is also needed about progestogen-only contraceptives.
6.2 Non-Hormonal Intrauterine Devices
There is very limited evidence, from a cohort study in China, of no change in risk of either colon or rectal cancer among ever users of the IUD (type unknown) [35].
6.3 Female Sterilisation
The Million Women Study accrued 18,197 cases of colorectal cancer during nearly 17 million person-years of follow-up; no association was seen in women who had ever undergone tubal ligation, compared with those not having this procedure (RR 0.99, 95% CI 0.96–1.03) [42]. These results are supported by limited evidence from a study of women in China [35]. A Canadian study of 730,000 women who underwent a number of gynaecological surgical procedures, observed a lower colorectal cancer incidence among those who had undergone bilateral tubal sterilisation, compared with that expected from population incident data (RR 0.81, 95% CI 0.70–0.93) [102]. Collectively, the evidence does not suggest a substantial change in colorectal risk as a consequence of tubal ligation.
7 Anal Cancer
Most studies looking at the risk of colorectal cancer have probably also included a small proportion of anal cancer cases. The Million Women Study examined reproductive risk factors among 517 cases of anal cancer; compared with never use, ever use of COCs was associated with an increased risk of anal cancer (RR 1.51, 95% CI 1.24–1.83), with a stronger effect seen in women who had used COCs for more than 4 years (RR 1.68, 95% CI 1.37–2.07) and no evidence of important differences between squamous carcinoma and adenocarcinoma [103]. No such association was observed in an earlier case-control study conducted in Denmark and Sweden [104]. The Million Women Study also observed a higher risk of anal cancer among women who had undergone tubal ligation; RR 1.39, 95% CI 1.13–1.70 [103]. The biological mechanisms by which these findings might occur is unclear.
8 Liver Cancer
Liver cancer (predominantly hepatocellular cancer) is the ninth commonest cause of new cancer in women worldwide; nearly 250,000 cases in 2018 (Fig. 11.1) [1, 2]. Very poor survival rates mean that liver cancer is the sixth most common cause of cancer death in women; an estimated 233,000 deaths in 2018 (Fig. 11.2). The main risk factors for hepatocellular carcinoma are chronic infection with hepatitis B virus (HBV) or hepatitis C virus (HCV), aflatoxin-contaminated foodstuffs, heavy alcohol intake, obesity, smoking and type II diabetes [4]. The relative importance of each risk factor varies around the world. The widespread adoption of HBV vaccination into national immunisation programmes is greatly reducing the incidence of HBV-associated hepatocellular cancer.
8.1 Combined Oral Contraceptives
A meta-analysis published in 2007, of 12 case-control studies, found a modest, statistically non-significant, increased risk of hepatocellular carcinoma among ever users of COCs, compared with never users (age- and sex-adjusted summary OR 1.57, 95% CI 0.96–2.54) [105]. Most of the studies were small, conducted in areas with a low prevalence of HBV (USA, UK and other European countries), and adjusted for a varying number of potential confounders, such as alcohol intake, hepatic infections, diabetes and obesity. Most studies were conducted at a time when COCs continued to have a high or medium dose of oestrogen, combined with an older progestogen. Study differences in how prolonged use was categorised prevented meta-analysis by duration of use. Nevertheless, longer durations of COCs use were associated with higher ORs (between 2.0 and 20.1) than shorter use (OR range 0.3–2.6). Two studies conducted in countries where HBV is endemic, found no association between COC use and hepatocellular cancer, irrespective of duration or recency of use. This suggests that COCs do not enhance an already higher background risk of hepatocellular cancer in women living in these areas.
Neither the Oxford Family Planning Association Contraceptive Study nor the RCGP Oral Contraceptive Study found an increased risk of incident liver or gallbladder cancer combined among ever users of COCs, compared with never users (RR 1.4, 95% CI 0.4–4.2 [16] and 0.87, 95% CI 0.45–1.69 [18], respectively). Ever use of COCs was also not associated with death from liver or gallbladder cancer combined in the RCGP Oral Contraception study (RR 0.65, 95% CI 0.30–1.39) [14]; or Nurses’ Health Study 1 (RR 0.98, 95% CI 0.74–1.30) [17]. All of these risk estimates were based on data from prolonged follow-up, with no sign of a risk emerging many years after stopping COCs.
Although sparse, evidence suggests a possible link between prolonged use of COCs and hepatocellular carcinoma in populations where the prevalence of HBV infection is low; the risk is presumed to be masked in HBC endemic populations because of the high risk of hepatocellular carcinoma from HBV infection itself. In most low HBV prevalent countries, however, the incidence of hepatocellular carcinoma is low, so the number of extra cases of hepatocellular cancer among COCs users in these areas will be very small—especially since there is no evidence of a persisting effect after COCs are stopped.
8.2 Female Sterilisation
Tubal sterilisation was not associated with liver cancer in the Million Women Study analysis which included 1267 cases of liver cancer; RR between women who had this operation and those who had not 0.98 (95% CI 0.85–1.13) [42].
9 Other Cancers
9.1 Combined Oral Contraceptives
In 2008, a Working Group of the International Agency for Research on Cancer evaluated and summarised available evidence about the possible carcinogenic risks associated with COCs [106]. It concluded that the use of COCs is unlikely to alter the risk of cancer of the thyroid, lung, stomach, urinary tract, gallbladder, pancreas, or the risk of lymphoma, cutaneous melanoma and tumours of the central nervous system. Publications since this evaluation have not provided consistent, strong evidence to contradict the Working Group’s conclusions.
10 Net Cancer Effects
Contraceptives have diverse cancer effects in different organs. As well as wanting to know whether a particular contraceptive changes the risk of cancer at a specific site, many women, their health care providers and other advisors want to know whether its use affects the lifetime risk of any cancer. In other words, they want to know the overall balance of lifetime cancer risks and benefits. Cohort studies with prolonged follow-up into older age (when most cancers occur) provide the best, direct information about net cancer effects of contraceptives.
10.1 Combined Oral Contraceptives
The RCGP Oral Contraception Study accrued over 1.2 million person-years of observation during 44 years of follow-up, and found no difference in the incidence of any cancer among ever and never users of COCs (RR 0.96, 95% CI 0.90–1.03) [18]. This contrasts with a modest reduction in the incidence of any cancer among ever users of COCs, compared with never users, seen in the NIH-AARP Diet and Health Study after 26 years of follow-up (RR 0.97, 95% CI 0.95–0.99) [61].
An earlier report from the RCGP Oral Contraception Study, of mortality after 39 years of follow-up, observed a reduced risk of death from any cancer in ever users compared with never users of COCs (RR 0.85, 95% CI 0.78–0.93) [14]. No such benefit was found in the Oxford Family Planning Association Contraceptive Study during over 600,000 person-years of observation accumulated during 41 years of follow-up (RR 0.9, 95% CI 0.8–1.0) [15]. Neither was an all-cancer mortality benefit seen in the Nurses’ Health Study I during 3.6 million person-years of observation amassed over 36 years of follow up (RR 1.01, 95% CI 0.7–1.06) [17].
All of these cohort studies with prolonged follow-up have assessed women living in the UK or the USA. Their results, therefore, may not reflect the experience of COC users in other parts of the world. It is reassuring, however, that in two areas of the world with both high rates of COC usage and high incidence of cancer, there is no indication of an increased lifetime risk of any cancer among ever users of this method of contraception.
10.2 Other Reversible Contraceptives
A study of over 250,000 Chinese textile workers followed for up to 11 years found no association between monthly combined injectable contraceptives and the incidence of any of 12 common cancers (RR 0.91, 95% CI 0.81–1.03), although the power of the study to detect an increase was low because few women used this contraceptive [107]. This study also assessed the combined cancer risk among oral contracptive users (RR 0.94, 95% CI 0.88–1.01) although there was also limited use of this contraceptive. A smaller study of 67,000 inhabitants of Shanghai, followed for a median of 7.5 years, found no changed overall risk of 11 common cancers among ever users of any contraceptive-which included COCs, injections, IUD and tubal sterilisation (HR 1.02, 95% CI 0.92–1.12) [35].
10.3 Female Sterilisation
The RCGP study observed, after an average of 28 years of follow-up, a similar risk of any incident cancer among women who had a tubal sterilisation as that of those who did not have this operation (HR 0.92, 95% CI 0.78–1.08) [108]. Tubal sterilisation was not associated with an altered risk of any of 26 cancers during 17.6 million person-years of observation accumulated by the Million Women Study (RR 1.00, 0.98–1.01) [42].
11 Male Sterilisation
In 2015, an estimated 28 million married or in-union couples relied on male sterilisation (vasectomy) for contraception [35].
11.1 Prostate Cancer
Prostate cancer is the second most common cancer in men, accounting for 1,280,000 new cases and 359,000 deaths in 2018 [1, 2]. Since the early 1990s, numerous studies have investigated whether vasectomy is linked with prostate cancer. These studies have been summarised in a number of systematic reviews and meta-analyses, with some finding a small effect [107,108,111] and others no effect [110,111,114]. The most recent meta-analysis included all epidemiological studies to March 2017; 16 cohort studies (including 2.56 million participants followed for between 1.8 and 24 years) and 33 case-control studies (with 44,536 participants) [111]. There was a weak association between vasectomy and prostate cancer in seven cohort studies with a low risk of bias (summary RR 1.05, 95% CI 1.02–1.09) and no significant association in the six case-control studies at low risk of bias (summary OR 1.06, 95% CI 0.88–1.29). Similar non-significant relationships were seen between vasectomy and high-grade, advanced-stage, or fatal prostate cancer. When studies with high or moderate risk of bias were included, the summary risk estimates moved away from the null. These results suggest that bias is a likely explanation for any associations seen in individual observational studies. Detection bias has been a particular concern. Most cases of prostate cancer are not clinically significant and many will go undiagnosed unless detected through screening. Different levels of assessment among men undergoing and not undergoing sterilisation (e.g. through pre-vasectomy screening or post-operation monitoring of vasectomised men) could result in spurious associations emerging between vasectomy and prostate cancer. Even if real, the strength of association is so modest that the public health consequences will be small, perhaps a 0.6% absolute increase in lifetime risk of prostate cancer [111]. This level of risk should not stop clinicians from offering vasectomy to couples wishing to have permanent contraception.
11.2 Testicular Cancer
Testicular cancer is uncommon, accounting for roughly 1% of all cancers in men. A systematic review and meta-analysis of eight studies published between 1980 and 2017 found two studies reporting a positive association between vasectomy and testicular cancer, and six showing no effect; summary OR 1.10, 95% CI 0.93–1.30) [115]. Five studies were conducted in the USA and three in England. Most were not recent studies. This relatively sparse evidence-base does not suggest an important association between vasectomy and subsequent testicular cancer.
References
Global Cancer Observatory. International Agency for Research on Cancer, Lyon. 2018. http://gco.iarc.fr/. Accessed 12 May 2019.
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68:394–424.
Marks L. Sexual chemistry: a history of the contraceptive pill. London: Yale University Press; 2001.
Your Cancer Type. Cancer Research UK, London. 2019. https://www.cancerresearchuk.org/about-cancer/type. Accessed 24 July 2019.
Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53,297 women with breast cancer and 100,239 women without breast cancer from 54 epidemiological studies. Lancet. 1996;347:1713–27.
Havrilesky LJ, Gierisch JM, Moorman PG, et al. Oral contraceptive use for the primary prevention of ovarian cancer. Evid Rep Technol Assess. 2013;212:1–514.
Giersch JM, Coeytaux RR, Urrutia RP, et al. Oral contraceptive use and risk of breast, cervical, colorectal and endometrial cancer: a systematic review. Cancer Epidemiol Biomark Prev. 2013;22:1931–43.
Mørch LS, Skovlund CW, Hannaford PC, et al. Contemporary hormonal contraception and the risk of breast cancer. New Eng J Med. 2017;377:2228–39.
Kahlenbom C, Modugno F, Potter DM, et al. Oral contraceptive use as a risk factor for premenopausal breast cancer: a meta-analysis. Mayo Clin Proc. 2006;81:1290–302.
Sturtevant FM. Breast cancer and oral contraceptives: critique of the proposition that high potency progestogen products counter excess risk. Biomed Pharmacother. 1984;38:371–9.
Marchbanks PA, Curtis KM, Mandel MG, et al. Oral contraceptive formulation and risk of breast cancer. Contraception. 2012;85:342–50.
Hunter DJ, Colditz GA, Hankinson SE, et al. Oral contraceptive use and breast cancer: a prospective study of young women. Cancer J Epidemiol Biomarkers Prev. 2010;19:2496–502.
Beaber EF, Buist DSM, Barlow WE, et al. Recent oral contraceptive use by formulation and breast cancer risk among women 20 to 49 years of age. Cancer Res. 2014;74:4078–89.
Hannaford PC, Iversen L, Macfarlane TV, et al. Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners’ Oral Contraception Study. BMJ. 2010;340:c927.
Vessey M, Yeates D, Flynn S. Factors affecting mortality in a large cohort study with special reference to oral contraceptive use. Contraception. 2010;82:221–9.
Vessey M, Yeates D. Oral contraceptive use and cancer: final report from the Oxford-Family Planning Association contraceptive study. Contraception. 2013;88:678–83.
Charlton BM, Rich-Edwards JW, Colditz GA, et al. Oral contraceptive use and mortality after 36 years of follow-up in the Nurses’ Health Study: prospective cohort study. BMJ. 2014;349:g6356.
Iversen L, Sivasubramaniam S, Lee AJ, et al. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017;216:580.
A Beginners Guide to BRCA1 and BRCA2. The Royal Marsden NHSA Foundation Trust, London. 2013. https://shared-d7-royalmarsden-publicne-live.s3.amazonaws.com/files_trust/s3fs-public/beginners-guide-to-brca1-and-brca2.PDF. Accessed 19 July 2019.
Moorman PG, Havrilesky LJ, Gierisch JM, et al. Oral contraceptives and risk of ovarian cancer and breast cancer among high-risk women: a systematic review and meta-analysis. J Clin Oncol. 2013;31:4188–98.
Shapiro S, Rosenberg L, Hoffman M, et al. Risk of breast cancer in relation to the use of injectable progestogen contraceptives and combined estrogen/progestogen contraceptives. Am J Epidemiol. 2000;151:396–403. Erratum: 2000;151:1134.
Strom BL, Berlin JA, Weber AL, et al. Absence of an effect of injectable and implantable progestin-only contraceptives on subsequent risk of breast cancer. Contraception. 2004;69:353–60.
Urban M, Banks E, Egger S, et al. Injectable and oral contraceptive use and cancers of the breast, cervix, ovary, and endometrium in black South African women: case-control study. PLoS Med. 2012;9:e1001182.
Marchbanks PA, McDonald JA, Wilson HG, et al. Oral contraceptives and the risk of breast cancer. New Engl J Med. 2002;346:2025–32.
Kumle M, Weiderpass E, Braaten T, et al. Use of oral contraceptives and breast cancer risk: the Norwegian-Swedish women’s lifestyle and health cohort study. Cancer Epidem Biomar. 2002;11:1375–81.
Soini T, Hurskainen R, Grénman S, et al. Cancer risk in women using the levonorgestrel-releasing intrauterine system in Finland. Obstet Gynecol. 2014;124:292–9.
Soini T, Hurskainen R, Grénman S, et al. Levonorgestrel-releasing intrauterine system and the risk of breast cancer: a nationwide cohort study. Acta Oncol. 2016;55:188–92.
Dinger J, Bardenheuer K, Minh TD. Levonorgestrel-relesing and copper intrauterine devices and the riks of breast cancer. Contraception. 2001;83:211–7.
Heikkinen S, Koskenvuo M, Malila N, et al. Use of exogenous hormone and the risk of breast cancer: results from self-reported survey data with validity assessment. Cancer Causes Control. 2016;27:249–58.
Backman T, Rauramo I, Jaakkola K, et al. Use of the levonorgestrel-relesing intrauterine system and breast cancer. Obstet Gynecol. 2005;106:813–7.
Jareid M, Thalabard J-C, Aarflot M, et al. Levonorgestrel-releasing intrauterine system is associated with a decreased risk of ovarian and endometrial cancer, without increased risk of breast cancer. Results from the NOWAC study. Gynecol Oncol. 2018;149:127–32.
Siegelmann-Danieli N, Katzir I, Landes JV, et al. Does levonorgestrel-releasing intrauterine system increase breast cancer risk in peri-menopausal women? An HMO perspective. Breast Cancer Res Treat. 2018;167:257–62.
Manson JE, Chlebowski RT, Stefanick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013;310:1353–68.
Collaborative Group on Hormonal Factors in Breast Cancer. Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet. 2019;
Dorjgochoo T, Shu XO, Li HL, et al. Use of oral contraceptives, intrauterine devices and tubal sterilization and cancer risk in a large prospective study, from 1996 to 2006. Int J Cancer. 2009;124:2442–9.
Trends in Contraceptive Use Worldwide 2015 (2015) United Nations, Department of Economic and Social Affairs, Population Division. http://www.un.org/en/development/desa/population/publications/pdf/family/trendsContraceptiveUse2015Report.pdf. Accessed 5 Mar 2018.
Patil E, Jensen JT. Update on permanent contraception options for women. Curr Opin Obstet Gynecol. 2015;27:465–70.
Gaudet MM, Patel AV, Sun J, et al. Tubal sterilization and breast cancer incidence: results from the cancer prevention study II nutrition cohort and meta-analysis. Am J Epidemiol. 2013;177:492–9.
Calle EE, Rodriguez C, Walker KA, et al. Tubal sterilization and risk of breast cancer mortality in US women. Cancer Causes Control. 2001;12:127–35.
Kreiger N, Sloan M, Cotterchio M, et al. The risk of breast cancer following reproductive surgery. Eur J Cancer. 1999;35:97–101.
Nichols HB, Baird DD, DeRoo LA, et al. Tubal ligation in relation to menopausal symptoms and breast cancer risk. Br J Cancer. 2013;109:291–5.
Gaitskell K, Coffey K, Green J, et al. Tubal ligation and incidence of 26 site-specific cancers in the Million Women Study. Br J Cancer. 2016;26:1033–7.
Hall MT, Simms KT, Lew J-B, et al. The projected timeframe until cervical cancer elimination in Australia: a modelling study. Lancet Public Health. 2019;4:e19–27.
International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical cancer and hormonal contraceptives: collaborative reanalysis of individual data for 16573 women with cervical cancer and 35509 women without cervical cancer from 24 epidemiological studies. Lancet. 2007;370:1609–21.
Nojomi M, Modaresgilani M, Mozafari N, et al. Cervical cancer and duration of using hormonal contraceptives. Asia-Pc J Clin Oncol. 2008;4:107–12.
Vanakankovit N, Taneepanichskul S. Effect of oral contraceptives on risk of cervical cancer. J Med Assoc Thail. 2008;91:7–12.
Roura E, Travier N, Waterboer T, et al. The influence of hormonal factors on the risk of developing cervical cancer and pre-cancer: results from the EPIC Cohort. PLoS One. 2016;11:e0147029.
Rosenblatt KA, Gao DL, Ray RM, et al. Oral contraceptives and the risk of all cancers combined and site-specific cancers in Shanghai. Cancer Causes Control. 2009;20:27–34.
Hannaford PC, Selvaraj S, Elliott AM, et al. Cancer risk among oral contraceptive users: cohort data from the Royal College of General Practitioner’s Oral Contraception Study. Br Med J. 2007;335:651–4.
Cortessis VK, Barrett M, Brown Wade N, et al. Intrauterine device use and cervical cancer. A systematic review and meta-analysis. Obstet Gynecol. 2017;130:1226–36.
Castellsagué X, Vaccarella S, de Sanjosé S, et al. Intrauterine device use, cervical infection with human papillomavirus, and risk of cervical cancer: a pooled analysis of 26 epidemiological studies. Lancet Oncol. 2011;12:1023–31.
Li H, Thomas DB, Jin S, et al. Tubal sterilization and use of an IUD and risk of cervical cancer. J Womens Health Gend Based Med. 2000;9:303–10.
Li H, Thomas DB. World Health Organization Collaborative Study of Neoplasia and Steroid Contraceptives. Contraception. 2000;61:323–8.
Kjaer SK, Mellemkjaer L, Brinton LA, et al. Tubal sterilization and risk of ovarian, endometrial and cervical cancer. A Danish population-based follow-up study of more than 65000 sterilized women. Int J Epidemiol. 2004;33:596–602.
Mathews CA, Stoner JA, Wentzensen N, et al. Tubal ligation frequency in Oklahoma women with cervical cancer. Gynecol Oncol. 2012;127:278–82.
Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25676887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015;385:977–1010.
Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23257 women with ovarian cancer and 87303 controls. Lancet. 2008;371:303–14.
Tsilidis KK, Allen NE, Key TJ, et al. Oral contraceptive use and reproductive factors and risk of ovarian cancer in the European Prospective Investigation into Cancer and Nutrition. Br J Cancer. 2011;105:1436–42.
Moorman PG, Alberg AJ, Bandera EV, et al. Reproductive factors and ovarian cancer risk in African-American women. Ann Epidemiol. 2016;26:654–62.
Bethea TN, Palmer JR, Adams-Campbell LL, et al. A prospective study of reproductive factors and exogenous hormone use in relation to ovarian cancer risk among Black women. Cancer Causes Control. 2017;28:385–91.
Michels KA, Brinton LA, Pfeiffer RM, et al. Oral contraceptive use and risks of cancer in the NIH-AARP Diet and Health Study. Am J Epidemiol. 2018;187:1630–41.
McGuire V, Hartge P, Liao LM, et al. Parity and oral contraceptive use in relation to ovarian cancer risk in older women. Cancer Epidemiol Biomark Prev. 2016;25:1059–63.
Iversen L, Fielding S, Lidegaard Ø, et al. Association between contemporary hormone contraception and ovarian cancer in women of reproductive age in Denmark: prospective, nationwide cohort study. BMJ. 2018;362:k3609.
Wilailak S, Vipupinyo C, Suraseranivong V, et al. Depot medroxyprogesterone acetate and epithelial ovarian cancer: a multicentre case-control study. BJOG. 2012;119:672–7.
The WHO Collaborative Study of Neoplasia and Steroid Contraceptives. Depot-medroxyprogesterone acetate (DMPA) and risk of epithelial ovarian cancer. Int J Cancer. 1991;49:191–5.
Soini T, Hurskainen R, Grénman S, et al. Impact of levonorgestrel-releasing intrauterine system use on the cancer risk of the ovary and fallopian tube. Acta Oncol. 2016;55:1281–4.
Huang Z, Gao Y, Wen W, et al. Contraceptive methods and ovarian cancer risk among Chinese women: a report from the Shanghai Women’s Health Study. Int J Cancer. 2015;137:607–14.
Tworoger SS, Fairfield KM, Colditz GA, et al. Association of oral contraceptive use, other contraceptive methods, and infertility with ovarian cancer risk. Am J Epidemiol. 2007;166:894–901.
Rice MS, Hankinson SE, Tworoger SS. Tubal ligation, hysterectomy, unilateral oophorectomy, and risk of ovarian cancer in the Nurses’ Health Studies. Fertil Steril. 2014;102:192–198.e3.
Cubula D, Widschwendter M, Májek O, et al. Tubal ligation and the risk of ovarian cancer: review and meta-analysis. Hum Reprod Update. 2011;17:55–67.
Rice MS, Murphy MA, Tworoger SS. Tubal ligation, hysterectomy and ovarian cancer: a meta-analysis. J Ovarian Res. 2012;5:13.
Sieh W, Salvador S, McGuire V, et al. Tubal ligation and risk of ovarian cancer subtypes: a pooled analysis of case-control studies. Int J Epidemiol. 2013;42:579–89.
Wang C, Liang Z, Lui X, et al. The association between endometriosis, tubal ligation, hysterectomy and epithelial ovarian cancer: meta-analyses. Int J Environ Res Public Health. 2016;13:1138.
McNamara C, Abbott SE, Bandera EV, et al. Tubal ligation and ovarian cancer risk in African American women. Cancer Causes Control. 2017;28:1033–41.
Cibula D, Widschwendter M, Zikan M, et al. Underlying mechanisms of ovarian cancer risk reduction after tubal ligation. Acta Obstet Gynecol Scand. 2011;90:559–63.
Antoniou AC, Rookus M, Andrieu N, et al. Reproductive and hormonal factors, and ovarian cancer risk for BRCA1 and BRCA2 mutation carriers: results from the International BRCA1/2 Carrier Cohort Study. Cancer Epidemiol Biomark Prev. 2009;18:601–10.
Collaborative Group on Epidemiological Studies on Endometrial Cancer. Endometrial cancer and oral contraceptives: an individual participant meta-analysis of 27276 women with endometrial cancer from 36 epidemiological studies. Lancet Oncol. 2015;16:1061–70.
Iversen L, Fielding S, Lidegaard O, et al. Contemporary hormonal contraception and risk of endometrial cancer in women younger than age 50: A retrospective cohort study in Danish women. Contraception. 2020;102:152–8.
Burchardt NA, Shafrir AL, Kaaks R, et al. Oral contraceptive use by formulation and endometrial risk among women born in 1947–1964: The Nurses’ Health Study II, a prospective cohort study. Eur J Epi. 2020.
Mueck AO, Seeger H, Rabe T. Hormonal contraception and risk of endometrial cancer: a systematic review. Endocr Relat Cancer. 2010;17:R263–71.
Felix AS, Guadet MM, La Vecchia CL, et al. Intrauterine devices and endometrial cancer risk: a pooled analysis of the Epidemiology of Endometrial Cancer Consortium. Int J Cancer. 2015;136:E410–22.
Castellsaque X, Thompson WD, Dubrow R. Tubal sterilization and the risk of endometrial cancer. Int J Cancer. 1996;65:607–12.
Lacey JV, Brinton LA, Mortel R, et al. Tubal sterilization and risk of cancer of the endometrium. Gynecol Oncol. 2000;79:482–4.
Winer I, Lehman A, Wactawski-Wende J, et al. Tubal ligation and risk of endometrial cancer: findings from the Women’s Health Initiative. Int J Gynecol Cancer. 2016;26:464–71.
Felix AS, Brinton LA, McMeekin DS, et al. Relationships of tubal ligation to endometrial carcinoma stage and mortality in the NRG oncology/gynecologic oncology group 210 trial. J Natl Cancer Inst. 2015;107:djv158.
Falconer H, Yin L, Altman D. Association between tubal ligation and endometrial cancer risk: a Swedish population-based cohort study. Int J Cancer. 2018;143:16–21.
Meyer LA, Broaddus RR, Lu KH. Endometrial cancer and Lynch Syndrome: clinical and pathological considerations. Cancer Control. 2009;16:14–22.
Lu KH, Loose DS, Yates MS, et al. Prospective multicentre randomized intermediate biomarker study of oral contraceptive versus depo-provera for prevention of endometrial cancer in women with Lynch syndrome. Cancer Prev Res. 2013;6:774–81.
Dashti SG, Chau R, Ouakrim DA, et al. Female hormone factors and the risk of endometrial cancer in Lynch Syndrome. JAMA. 2015;314:61–71.
Weiss NS, Daling JR, Chow WH. Incidence of cancer of the large bowel in women in relation to reproductive and hormonal factors. J Natl Cancer Inst. 1981;67:57–60.
Kune GA, Kune S, Watson LF. Oral contraceptive use does not protect against large bowel cancer. Contraception. 1990;41:19–25.
Fernandez E, La Vecchia C, Balducci A, et al. Oral contraceptives and colorectal cancer risk: a meta-analysis. Br J Cancer. 2001;84:722–7.
Bosetti C, Bravi F, Negri E, et al. Oral contraceptives and colorectal cancer risk: a systematic review and meta-analysis. Hum Reprod Update. 2009;15:489–98.
Campbell PT, Newcomb P, Gallinger S, et al. Exogenous hormones and colorectal cancer risk in Canada: associations stratified by clinically defined familial risk of cancer. Cancer Causes Control. 2007;18:723–33.
Arem H, Park Y, Felix AS, et al. Reproductive and hormonal factors and mortality among women with colorectal cancer in the NIH-AARP Diet and Health Study. Br J Cancer. 2015;113:562–8.
Charlton BM, Wu K, Zhang X, et al. Oral contraceptive use and colorectal cancer in the Nurses’ Health Study I and II. Cancer Epidemiol Biomark Prev. 2015;24:1214–21.
Burón Pust A, Alison R, Blanks R, et al. Heterogeneity of colorectal cancer risk by tumour characteristics: large prospective study of UK women. Int J Cancer. 2017;140:1082–90.
Murphy N, Xu L, Zervoudakis A, et al. Reproductive and menstrual factors and colorectal cancer incidence in the Women’s Health Initiative Observational Study. Br J Cancer. 2017;116:117–25.
Wong TS, Chay WY, Tan MH, et al. Reproductive factors, obesity and risk of colorectal cancer in a cohort of Asian women. Cancer Epidemiol. 2019;58:33–43.
Zervoudakis A, Strickler HD, Park Y, et al. Reproductive history and risk of colorectal cancer in postmenopausal women. J Natl Cancer Inst. 2011;103:826–34.
Lin KJ, Cheung WY, Lai JY, et al. The effect of estrogen vs. combined estrogen-progestogen therapy on the risk of colorectal cancer. Int J Cancer. 2012;130:419–30.
Cape DB, Kreiger N. Gynaecological surgical procedures and risk of colorectal cancer in women. Eur J Cancer Prev. 1999;8:495–500.
Coffey K, Beral V, Green J, et al. Lifestyle and reproductive risk factors associated with anal cancer in women aged over 50 years. Br J Cancer. 2016;112:1568–74. Erratum in: Br J Cancer 2016;114;e16.
Frisch M, Glimelius B, Wohlfahrt J, et al. Tobacco smoking as a risk factor in anal carcinoma: an antiestrogenic mechanism? J Natl Cancer Inst. 1999;91:708–15.
Maheshwari S, Sarraj A, Kramer J, et al. Oral contraception and the risk of hepatocellular carcinoma. J Hepatol. 2007;47:506–13.
IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 100A. Pharmaceuticals. A Review of Human Carcinogens. Lyon: International Agency for Research on Cancer; 2012.
Rosenblatt KA, Gao DL, Ray RM, et al. Monthly injectable contraceptives and the risk of all cancers combined and site-specific cancers in Shanghai. Contraception. 2007;76:40–4.
Iversen L, Hannaford PC, Elliott AM. Tubal sterilization, all-cause death, and cancer among women in the United Kingdom: evidence from the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2007;196:447.e1–8.
Bernal-Delgado E, Latour-Pérez J, Pradas-Arnal F, et al. The association between vasectomy and prostate cancer: a systematic review of the literature. Fertil Steril. 1998;70:191–200.
Dennis LK, Dawson DV, Resnick MI. Vasectomy and the risk of prostate cancer: a meta-analysis examining vasectomy status, age at vasectomy, and time since vasectomy. Prostate Cancer Prostatic Dis. 2002;5:193–203.
Bhindi B, Wallis CJD, Nayan M, et al. The association between vasectomy and prostate cancer: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:1273–86.
Shang Y, Han G, Li J, et al. Vasectomy and prostate cancer risk: a meta-analysis of cohort studies. Sci Rep. 2015;5:9920.
Zhang XL, Yan JJ, Pan SH, et al. Vasectomy and the risk of prostate cancer: a meta-analysis of cohort studies. Int J Clin Exp Med. 2015;8:17977–85.
Liu LH, Kang R, He J, et al. Vasectomy and risk of prostate cancer: a systematic review and meta-analysis of cohort studies. Andrology. 2015;3:643–9.
Duan H, Deng T, Chen Y, et al. Association between vasectomy and risk of testicular cancer: a systematic review and meta-analysis. PLoS One. 2018;13:e0194606.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hannaford, P.C., Iversen, L. (2021). Contraception Cancer Risks and Benefits. In: Meriggiola, M.C., Gemzell-Danielsson, K. (eds) Female and Male Contraception. Trends in Andrology and Sexual Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-70932-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-70932-7_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70931-0
Online ISBN: 978-3-030-70932-7
eBook Packages: MedicineMedicine (R0)