Abstract
The effective use of intra-arterial radiopeptide therapy in scintigraphically confirmed liver malignancies that are positive for somatostatin receptors requires the understanding of many disciplines. Radiation physics, radiation biology, vascular anatomy, and modifiers of radiopeptide flux support the efforts of the medical team to infuse 111In-Octreotide in high doses for the treatment of neuroendocrine tumor patients. This chapter presents and discusses the key concepts of all disciplines combined for the application of a loco-regional, safe and effective liver-peptide therapy, which was, recently, according to the Netter-1 trial, suggested as the first-line therapy for the confrontation of neuroendocrine tumors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Auger and Internal Conversion electron emission of 111In
- Neuroendocrine tumors
- Indium’s tumouricidal efficacy
1.1 Introduction
Treatment modalities using irradiation comprise a potent cornerstone of anti-cancer therapy. Although each malignant tumor type has a different sensitivity profile to radiation, every malignancy, diffuse or solid retreats and succumbs more or less to the applied therapeutic radiation dose. The relatively new evolutionary treatment techniques that protect the radiation-sensitive normal liver parenchyma while still delivering sufficient radiation to malignant cells have dramatically increased the use of liver-tumor-directed radiation (loco-regional) therapy approaches. Being focused on liver tumors and specifically on neuroendocrine ones, these depend on the location of the disease, whether cancer has given metastases and spread to the other areas of the body, i.e. liver, bone, lymph nodes, and if the tumor is secreting hormones, responsible for symptoms. Treatment modalities against primary or metastatic neuroendocrine tumors can be categorised as (a) invasive, i.e. surgical resection, (b) minimally invasive, ablative, or loco-regional, i.e. selective trans-arterial (chemo) embolisation [TA(C)E], radiofrequency ablation [RFA], laser-induced thermotherapy [LIT], selective internal radiotherapy [SIRT] and (c) systemic treatment schemes.
With the development of intra-arterial infusions, the application of radiation to tumors of all origins and in all segments of the liver is a fact. Recent advances in medical oncology (individualised molecular profiling, antiangiogenic drugs and new systemic chemotherapeutics) have resulted in improved response rates, disease-related or progressive survival rates and median survival rates in many solid tumors. However, despite the elimination of the disease elsewhere in the body, the liver often remains a site of tumor resistance and, ultimately, the cause of patient death [1]. In addition, today, qualified interventional radiologists and the development of advanced and specialised catheters can help oncologic patients more than ever, and catheterising the feeding artery of inoperable solid tumors is a routine technique in most radiological centres that treat cancer patients. Nuclear medical devices and imaging agents allow the precise localisation of tumors that have not previously been imaged or irradiated and the detection of active tumors among already destroyed ones. Therapeutic radiation began in the early twentieth century with the successful fight against cancer. Today, patient survival can be predicted, whereas patients with no longer treatment-sensitive tumors or patients who cannot tolerate chemotherapy die. Overall, these data suggest that liver irradiation is not avoided or contraindicated, but rather the reverse—thus, why not use radiation for the affected liver? How can we use and optimise trans-arterial endo-hepatic radiation in favour of liver cancer patients?
1.2 Hepatic Intra-arterial Radiopeptide Flow Dynamics
Most blood of healthy hepatocytes is fed by the portal vein system, whereas a mediocre portion is supplied by the hepatic artery. In liver primary or metastatic tumor cells, most of the blood is delivered via the hepatic artery. Based on this different feeding pathway of benign and malignant cells in the liver, when radiopeptides in high dosage are infused intra-arterially from the hepatic artery, a very large portion of the applied radiation is targeted directly to the tumor cells and additionally attracted from the peptide receptors (Fig. 1.1); in parallel, healthy cells are protected as long as they are protected from radiation damage. There are also minor differences in the distribution of peptide analogues receptor binding due to their different receptor affinities.
According to rheology, there are two distinctly different types of fluid flow: the laminar and the turbulent one. In laminar flow, the fluid particles move along smooth paths in layers with every layer (lamina) sliding smoothly over its neighbour. In turbulent flow, the particles follow very irregular and erratic paths, and their velocity vectors vary repetitively, both in magnitude and direction. The laminar flow becomes unstable at high velocities and breaks down into turbulent flow [2]. Blood flow is laminar when the velocity gradient is smooth and continuous. It is observed that the insertion of a catheter in an artery affects the flow field, disturbs the pressure distribution, and enhances the resistance to flow [3, 4]. Consequently, to maintain the laminar character of flow on the course of 111In-Octreotide infusion either after simple catheterisation of the femoral—iliac arteries—aorta—proper hepatic artery (Fig. 1.2, GS Limouris, Chap. 7) or after the implementation of a drum-port system (IL Karfis, Chap. 8), steady low pressure should be performed by the nuclear physician or, in case the infusion is realised automatically, with the aid of an infusion-pump. Thus, gentle infusion, with steady low pressure, should be used to strictly avoid backflow [5, 6] (Fig. 1.3). Therefore, it is necessary to take into account such flow variables due to catheterisation. The cross-section of the vessel shows the laminate moving at different speeds; when closest to the edge of the vessel, the fluid moves slowly, though when near the centre, it moves quickly.
Thus, patient-specific manoeuvres have to be used. In the case of main hepatic artery injection, radiation is distributed to both lobes of the liver. If the lesions are limited to one lobe, the catheter can be selectively inserted either into the left or right lobar artery supplying the affected lobe thus sparing the contra-lateral. In selected cases, hyper-selective, single-segment treatments can be considered.
1.2.1 Production and Physical Characteristics of 111In
111In is produced by cyclotron after cadmium-112 (112Cd) collision with protons of a 2.8 MeV energy according to the nuclear reaction 112Cd (p, 2n) 111In. 111In decays by a physical half-life time of 2.83 days, with emissions displayed in Table 1.1. The purity of the final product of 111In is affected by the undesired isotopes 110mIn, 110In and 114mIn that are not possible to be spared from 111In due to the similar chemical characteristics of these isotopes with 111In.
Isotopes 110mIn and 110In do not affect the dosimetry of radioisotopes labelled 111In, as these undesired isotopes have a minor presence and short half-life time (4.9 h and 1.1 h, respectively). On the contrary, 114mIn, which is produced from 114Cd according to a (p, n) nuclear reaction, has 49.51 days half-life time and decays through internal transition (96.9%) and electron capture (3.2%) with the emission of photons at (192, 558 and 725) keV. 114mIn affects dosimetry due to its long half-life time [5,6,7].
In the case of the main hepatic artery injection, radiation is distributed to both lobes of the liver. If the lesions are limited to one lobe, the catheter can be selectively inserted either into the left or right lobar artery supplying the affected lobe thus sparing the contra-lateral. In selected cases, hyper-selective (i.e. single-segment) treatments can be considered.
Patient-specific dosimetry calculations help the physician to optimise the planning of the treatment, avoid side effects to healthy tissue, and assign the administered dose for treatment results.
1.3 Recent Historical Background of Radioactive Infusions for Liver Tumors
The delivery of radioactive isotopes bonded with synthetic peptides to solid tumors dates back to 1994 when, for the first time, Eric Krenning [7] and Dick Kwekkeboom intravenously infused high doses of 111In-Octreotide (Sect. 1.9) to treat liver metastases of an abdominal glucagonoma (Fig. 1.4). Limouris et al. first reported the routine use of intra-arterial infusions of 111In-Octreotide [8] according to a particular protocol of specific bone marrow protective and nephroprotective as well character (Limouris et al. ‘Aretaieion Protocol’ [9]). Details of the aforementioned novelty were reported by Kontogeorgakos D [10], Troumpoukis N [11] and Karfis I [12] in their Ph.D. theses from the same Institute that published their results, after the catheterisation of the hepatic artery using 111In-Octreotide. In 2014, Pool et al. in a limited cohort of 3 patients, after preclinical, intra-arterial as well intravenous studies in rats observed a two-fold higher 111In-DTPA-TOC tumor uptake after intra-arterial administration than after intravenous injection; the clinical data (of patients) indicated that the intra-arterial administration of radiolabelled somatostatin analogues via the hepatic artery significantly increases radionuclide uptake in gastro-entero-pancreatic neuroendocrine tumors (GEP-NETs), sst2-positive, liver metastases up to 72 h post-injection, emphasising that the effect of the intra-arterial administration differs between patients who show a large variability in radioactivity increment in liver metastases [13]. Kratochwil [14, 15] reported on radiopeptide pharmacokinetics in the tumor using, not 111In-Octreoscan, but 117Lu-DOTA-TATE intra-arterially. Although worldwide, most clinical experiences derive from intravenous therapies using 177Lu, inoperable liver metastasised neuroendocrine tumor patients have been treated by our Institution exclusively intra-arterially using 111In-Octreotide with some exceptions where catheterisation was not possible.
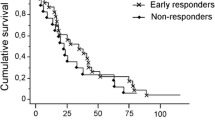
111In clinical studies and efficacy: According to our results in the first cohort of 17 inoperable liver metastasised GEP-NETs, treated with high doses of 111In-Octreoscan [Table 1.2], 1 of 17 (6%) patients achieved a complete response (CR), and 8 of 17 (47%) showed partial response (PR) and 3 (18%) stable disease (SD), whereas in the remaining 5 (29%) patients, the disease progressed, the therapy was discontinued and the patients died shortly thereafter. Consequently, 71% (CR + PR + SD) of the patients showed some radiological benefit from the treatment. Worldwide, only a limited number of authors reported on the efficacy of treatments in GEP-NET-patients using high doses of 111In-DTPA0 Octreotide. Our results in the CR/PR group (53%), compared favourably with published data (2/26 pts (8%) (Valkema et al. 2002) [16], 2/12 pts (17%) (Buscombe et al. 2003) [17], 2/26 pts (8%) (Anthony et al. 2002) [18], 2/29 pts (7%) (Delpassand et al. 2014)) [19]. Our patients with disease stabilisation (18% (3/17 pts)) differ from previous reports of 58% (15/26 pts) of Valkema et al. [16], 58% (7/12 pts) of Buscombe et al. [17], 81% (21/26 pts) of Anthony et al. [18], and 55% (16/29 pts) of Delpassand et al. [19]. The superiority of our results compared to those of the other authors might be explained by the intra-arterial route of infusions, where the tumor mean absorbed dose per session was estimated to be markedly higher compared to i.v. application (Table 1.3); a finding reported by other authors (Pool et al. 2009 [20], Kratochwil et al. 2010 [14], Kratochwil et al. 2011 [15]) too. The results of the clinical evaluation of the Auger electron emitter indium-111 conjugated to the somatostatin analogues that targets and exploits its receptor overexpression on neuroendocrine cells was very encouraging, particularly as it was thereafter proved for the eradication of small volume tumors (Limouris et al. 2008 [8], Reilly 2010 [21]). Summarising the results of previous studies, it might be concluded that the application of 111In-Octreotide leads to disease stabilisation (SD) in previously progressive tumors and clinical symptomatic and biochemical (Cr-A) improvement as well.
1.4 Physics of Radiation Therapy
1.4.1 Radiation Types
The radiant energy causing ionisation in the cell can be categorised into two types: electromagnetic (γ-rays, x-rays) and particulate (α-particles, β-minus and β-plus particles, internal conversion and Auger electrons, ordinary shell electrons). The electromagnetic radiation γ-rays and x-rays of the same energy are indistinguishable, and the only difference is their source; γ-rays are emitted exclusively from the nucleus, whereas x-rays are emitted only from the electron shells.
From the particulate radiation, the most massive α-particles are emitted from the nucleus, with a velocity of about 1/20 that of the speed of light and with energies ranging from 4 to 9 MeV. They consist of two protons (charge +2 as a helium nucleus stripped of its orbital electrons) and have a very high linear-energy-transfer (LET) rate (Quality Factor = 20). The LET is the energy fraction, deposited in an absorber (i.e. tissue) per centimetre of travel. The range of an α-particle in the matter is typically 4–5μm. Thus, α-particles cannot penetrate a sheet of paper or the epithelial layer of the skin. A single α-particle reaching the nucleus of a cell can deposit up to 1 Gy of radiation.
Ordinary electrons are found only in the electron shells (charge −1), and β-minus particles or negatrons (charge −1) are emitted exclusively from the nucleus. β-plus particles or positrons (charge +1) originate only from the nucleus too. In general, beta particles penetrate up to 3 mm of matter (tissue), while γ-rays and neutron rays completely penetrate the human body and end only in thick walls. Beta-minus particles possess a moderately high LET rate (Quality Factor = 1), allowing them to significantly contribute to the absorbed radiation dose. It is worth noting that there are beta-minus emitters that also emit γ-rays and are useful for both imaging and therapy. Regarding positrons, after having lost all their kinetic energy and having reached their rest mass, they interact with an electron in a process called annihilation, resulting in the total destruction of the positron and the electron and the release of two photons (γ-rays) whose energy is always 511 keV. The angle between the two photons is always 180°. Electromagnetic radiation, either as γ-rays or as x-rays, has an identical interaction with matter. Their LET rates are low, implying that much of the radiation escapes the body following the administration of γ-emitting isotopes. This minimises the radiation dose for patients and permits external imaging. To emphasise, that electromagnetic radiation is only linear and cannot be modified except by collision with tissue.
For photons, electron and proton radiation the damage is done primarily by activated radicals produced from atomic interactions called low linear-energy-transfer (low LET) radiation. On the contrary, the neutrons’ radiation is of a high linear-energy-transfer (high LET) and the damage happens primarily by nuclear interactions. If a tumor cell is damaged by low LET radiation, it has a good chance of repairing itself and continuing to grow. Regarding high LET radiation, the possibility of a damaged tumor cell repairing itself is very small. The energy absorbed by the cell can cause DNA/RNA damage, leading to cell death.
Proton beam radiation therapy (PBRT) is a type of external beam radiation therapy (EBRT) that utilises protons precisely targeted to a specific tissue mass. Protons used in the same way as electrons have the ability to penetrate deep into tissues to reach tumors, while delivering less radiation to superficial tissues such as the skin. This may make PBRT more effective for inoperable tumors or for individuals in whom damage to healthy tissue would pose an unacceptable risk (Table 1.4). Furthermore, it is also well known that during proton therapy, neutrons are produced. This has been observed and proved, as protons are used for application in radiation therapy. It is also known that the neutron-absorbed dose is small. However, neutrons are highly biologically effective, and, thus, even a minimal absorbed dose might cause side effects in the patient, the most severe of which is the induction of a second primary cancer [22].
1.4.2 Auger Electrons
Auger electrons discovered in 1922 by the Austrian-Swedish physicist Lise Meitner (Fig. 1.5) [23] and in 1923 by the French physicist Pierre Auger (Fig. 1.6) [24] are formed when the vacancy created in an inner shell is filled with an electron of a higher energy level after electron capture. Most of the excess energy is delivered as X-ray energy, but one part is released as kinetic energy to another electron, which is then called an Auger electron [25,26,27,28,29,30]. A summary of the properties and characteristics of Auger electron emitters and their emissions can be seen in Table 1.5. Τoday, the Auger electron emitters mainly used for in vitro or in vivo therapy are 125I, 111In and 123I and to a lesser extent 67Ga, 99mTc and 201Tl [30, 31]. 125I is the most widely studied Auger electron emitter and has been used in many in vitro experiments to investigate the different effects of low-energy electrons on DNA27 [31,32,33,34,35,36,37].
However, its long half-life of 60 days makes it a little less practical for clinical applications. The physical half-life of the radionuclides should preferably be of the same order of magnitude as their biological half-life. A ‘too long’ physical half-life increases the amount of radionuclides that must be delivered to the tumor cells to allow for a reasonable amount of decay before excretion. On the other hand, a ‘to short’ physical half-life does not provide enough time for the targeting process. It is reasonable to assume that the most appropriate physical half-lives range from a few hours to a few days when targeting disseminated cells. Longer physical half-lives (up to one or a few weeks) may be desirable when high intakes of solid tumor masses are required.
The use of low-energy electrons has some advantages over the use of high-energy electron beta-emitters. Because of their long range, beta particles will overshoot single disseminated cells and small metastases [23, 31, 38,39,40,41,42] where most of the damage will be done to the surrounding healthy tissues. On the contrary, Auger electron emitters cause much less off-target effects than beta-emitters. On the other hand, for larger tumors, this cross-firing from beta-emitters will result in a more homogeneous deposition of energy in the tumor mass even if the radiopharmaceutical has an inhomogeneous distribution inside the tumor [40,41,42]. Additionally, for larger tumors, a much larger number of Auger-electron-emitting radionuclides is needed to cause the same cytotoxic effects, unless the Auger electrons are emitted inside the cell’s nucleus. In a study by Capello et al., the influence of tumor size on the effectiveness of 111In-Octreotide peptide receptor radionuclide therapy (PRRT) was evaluated [40]. In rats bearing small (<1 cm3) tumors, complete responses were observed, but only partial tumor regressions were observed in the rats bearing larger (>8 cm3) lesions. Auger-electron therapy can thus be conceptually compared with alpha- and beta-therapy, based largely on their path lengths and LET. Direct comparison of the various Auger electron-emitting isotopes with each other however is complicated by the diverse electron emission spectra of these isotopes. For example, 125I emits, on average, 12.2 Auger electrons per decay, compared to 6.8 Auger electrons emitted per decay by 111In. However, for 111In the average energy of the AE is higher, and it emits more than threefold higher energy conversion electrons and is accompanied by two gamma-photon emissions that are considerably higher in energy than the 35 keV photon from 125I (Table 1.1) [34, 43].
1.4.3 Radiation Dose
The dose of ionising radiation absorbed by the liver, a solid tumor, or other tissues has been a cornerstone of the design of clinical studies and trials. Earlier reports used the term roentgen (R), which is the ionisation in air, i.e. the exposure of gamma rays. The newer nomenclature uses the SI unit for the absorbed dose in tissue (1 Joule/kg = 1 Gray (Gy) = 100 rads = 100 cGy as the basic unit of measurement).
1.5 Radiobiology
From the turn of the century, attempts to gain an understanding of the effects of radiation in living tissue have been made, with observations reported by Hall [44] on skin reactions, primary erythema and collapse. Since then, clinical experience has been based on observations on normal and malignant tissue reaction and repair due to ionising radiation. The DNA must be damaged, unrepaired or improperly repaired to cause loss of reproductive ability or apoptosis (Fig. 1.7). According to Hall [44] and Kennedy et al. [45], it was estimated that in the presence of sufficient oxygen (>10 mm Hg), any form of radiation (x-rays, gamma rays, beta rays or electron emission in general) potentially interacts with the DNA. About 75% of DNA damage is indirect, with a photon striking a water molecule within 4 nm of the DNA strand (water is 80% of the cell). Kinetic energy from the incident photon is transmitted to an orbital electron of the water molecule and ejects it, which is now called a secondary electron. The energy that is transferred to a water molecule forms a free radical that is highly reactive, breaking the bonds of nearby DNA strands. Furthermore, a direct interaction of the secondary electron on the DNA strand is expected, which is referred to as a direct effect [44].
On a histological sample of normal (a) and tumor liver cells (b), 2μm (in blue) are super-imposed. The cellular membrane is delineated in green (arrow). The nuclei of normal (a) and tumor cells (b) are well distinguished. Comparing cell dimensions and distances between cell surface and nuclei obviously can be elicited that DNA lies within the micrometre range of 111In emissions. (Adapted and modified from Limouris et al. [4])
Roger Howell in his excellent ‘paper-chronical’ on Auger electrons and their exquisite capacity to finally serve as first-class endocellular radionuclide tumor killers reported on the extreme radiotoxicity of Auger electron emitters that prompted scientists to extensively investigate the radiobiological effects of Auger electron emitters as well as Auger electrons released as a consequence of the photoelectric effect [46]. Their efforts were punctuated by a series of international meetings that focused on the biological aspects of Auger processes. These began with the founding meeting in 1975 that was organised by Ludwig Feinendegen in Jülich, Germany. This meeting was followed by the first one, in 1987 in Charney Basset, UK, the second in 1991 in Amherst, USA, the third in 1995 in Lund, Sweden, the fourth in 1999 in Lund again, Sweden and the fifth in 2003 in Melbourne, Australia. The 2nd–5th proceedings contain a review of the published work of the previous meetings; Kassis [25]. Roger Howell’s manuscript [46] continued this tradition. It reviews articles related to the biophysical aspects of Auger processes that were published from 2004 to 2007, excluding articles published in the previous proceedings.
1.5.1 Modifiers of Radiation Response
According to Zeman [47] and Withers [48], oxygen is the most important biological modifier of radiation action at the cellular level and is the main reason for inducing radiation damage caused by free radicals; meanwhile, these damages can be repaired in a hypoxic state. The ratio of the radiation dose without oxygen compared to those with oxygen producing the same biological effect is referred to as the ‘oxygen enhancement ratio’ (OER). For x-rays, the OER lies between 2 and 3, i.e. a given x-ray image will provoke a 2–3 times stronger burden on the cell in the presence of oxygen than in a hypoxic environment [44]. Other factors affecting radiation efficiency are well known as the 4 ‘Rs,’ i.e. reoxygenation, repair of radiation damage, reassortment (rearrangement) of cells into more or less sensitive sections of the cell cycle (the S-phase is the most resistant to radiation and G2-M the most sensitive) and repopulation (rapidly dividing tumor populations), which can be overwhelmed by a continuous low radiation dose delivered for approximately more than 14 days. Repopulation may also become a problem after surgical resection, chemoembolisation, cryotherapy or radiofrequency ablation if hepatic hypertrophy is stimulated in the regional normal cells. The repair of radiation damage or ‘sub-lethal damage repair’ is improved in low-oxygen environments and with multiple radiation doses (fractionation). The break (typically 24 h) between each fraction of external radiotherapy offers the opportunity to repair DNA strand breaks in normal and malignant cells.
1.6 The Effects of Radiation on the Liver
Until recently, the liver was classified as a radio-resistant organ, though it is in fact highly radiosensitive [49]. Thus, it is not surprising that since the early 1960s [50, 51]acute transient effects or long-term (late effects) due to the ionising radiation in the liver have been described in the literature; the former has been described as an increase in liver transaminases, neutropenia and/or coagulopathy and the later as fibrosis, persistent enzyme degeneration, ascites, jaundice, and rarely, radiation-induced liver disease (RILD), and fatal veno-occlusive disease (VOD) [52,53,54]. RILD is often what is termed ‘radiation hepatitis’ and has been classically expected within 3 months of initiating radiation, with rapid weight gain, abdominal distension, liver enlargement and occasional ascites or jaundice, with elevation in serum alkaline phosphatase. Clinically, it is similar to the Budd-Chiari syndrome, but most patients survive, though some die of this disease with no evidence of tumor progression. It was reported that the entire liver cannot be treated with radiation above 30–35 Gy in conventional fractionation (1.8–2 Gy/day, 5 days per week), as RILD or VOD may occur [55].
1.7 The Rationale for 111In-Octreoscan Therapy
The unique vascular supply of the liver is well described and understood by radiologists and surgeons but less well by other specialists. A brief review is presented later (Sect. 1.7.1).
1.7.1 Anatomic Vascular Summary
The portal venous system supplies 80% or more of the blood supply to the normal liver [56]. The hepatic artery, with branches to the gallbladder, duodenum and stomach, provides up to 20% of the required blood supply to the normal liver. However, in the presence of tumor growth in the liver, the hepatic artery is the main supplier of blood, from 80 to 100%. The tumor vessel growth is many times more concentrated in the periphery of the tumor compared to the tumor centre and normal liver, in a ratio of 3:1 up to 20:1, and is abnormal in their consistency [57]. These data have been shown to be reliable in many trials [57,58,59].
1.7.2 Preclinical Reports on Blood Supply in Tumors
Breedis and Young performed a series of animal studies with numerous species, including rabbits, rats, mice and 13 human livers with metastatic solid tumors [56]. They demonstrated that 80–100% of the blood supply to tumors comes from the hepatic artery. The same results were reported by Ackerman et al. [58] and Lien and Ackerman [57] in rat carcinosarcoma liver metastases, using either 131I-tagged human serum albumin (RISA) or resin microspheres labelled with 90Y. Hepatic arterial infusions were compared with those of the portal vein in tumor intake versus normal liver tissue. Results showed that tumors larger than 30 mg received 75% of their blood supply from the hepatic artery, with an estimated tumor-to-normal tissue ratio of 3:1.
1.9 Commercially Available 111In-Octreoscan for Human Medical Use
111In-Octreoscan contains 111In-labelled octreotide, which is a somatostatin analogue; it is also known as an OctreoScan®, a brand name for 111In-labelled pentetreotide; pentetreotide is a DTPA-conjugated form of octreotide, originally manufactured by Mallinckrodt Nuclear Medicine LLC, which now is part of Curium. It is particularly useful for the management of neuroendocrine tumors.
References
Kennedy S, Dezarn WA, McNeillie. 90Y microspheres; concepts and principles. In: Bilbao J-I, Reiser MF, editors. Liver microembolization with 90Y microspheres. Berlin-Heidelberg: Springer; 2014. p. 1–10.
Evans DH, McDicken WN, Skidmore R, et al. Doppler ultrasound: physics, instrumentation, and clinical applications. Wiley; 1989.
Taylor KJW, Burns PN, Wells PNT. Clinical applications of doppler ultrasound. Raven: Press; 1987.
Zaman A, Ali N, Sajid M, et al. Numerical and analytical study of two-layered unsteady blood flow through catheterized artery. PLoS One. 2016;11(8):e0161377.
Lyra ME, Andreou M, Georgantzoglou A, et al. Radionuclides used in nuclear medicine therapy—from production to dosimetry, current medical imaging reviews. Bentham Science Publishers. 2013;9:51–75.
Lyra-Georgosopoulou M, Limouris GS. Blood flow and arterial infusion by implanted port in- 111 octreotide therapy. Interv Med Clin Imaging. 2019;2(1):1–8.
Krenning EP, Kooij PPM, Bakker WH. Radiotherapy with a radiolabelled somatostatin analogue, [111In-DTPA-D. Phe1]-octreotide; a case history. Ann N Y Acad Sci. 1994;733:496–506.
Limouris GS, Chatziioannou A, Kontogeorgakos D, et al. Selective hepatic arterial infusion of In- 111-DTPA-Phe1-octreotide in neuroendocrine liver metastases. Eur J Nucl Med Mol Imaging. 2008;35:1827–37.
Limouris GS, Karfis I, Chatziioannou A, et al. Super-selective hepatic arterial infusions as established technique (“ARETAIEION” Protocol) of [177Lu] DOTA-TATE in inoperable neuroendocrine liver metastases of gastro-entero-pancreatic (GEP) tumors. Q J Nucl Med Mol Imaging. 2012;56(6):551–8.
Kontogeorgakos D. PhD thesis, Medical School, National and Kapodistrian University of Athens-Greece; 2006.
Troumpoukis N. PhD thesis, Medical School, National and Kapodistrian University of Athens-Greece; 2016.
Karfis I. PhD thesis, Medical School, National and Kapodistrian University of Athens-Greece; 2016.
Pool SE, Kam BLR, Koning GA, et al. [111In-DTPA] Octreotide tumor uptake in GEPNET liver metastases after intra-arterial administration: an overview of preclinical and clinical observations and implications for tumor radiation dose after peptide radionuclide therapy. Cancer Biother Radioph. 2014;29(4):179–87, Mary Ann Liebert, Inc.
Kratochwil C, Giesel FL, López-Benítez R. Intra-individual comparison of selective arterial versus venous 68Ga-DOTATOC PET/CT in patients with gastro-enteropancreatic neuro-endocrine tumors. Clin Cancer Res. 2010;16(10):2899–905.
Kratochwil C, Lopez-Benıtez R, Mier W. Hepatic arterial infusion enhances DOTATOC radiopeptide therapy in patients with neuroendocrine liver metastases. Endocr Relat Cancer. 2011;18:595–602.
Valkema R, De Jong M, Bakker WH, et al. Phase I study of peptide receptor radionuclide therapy with [111In-DTPA°] octreotide: the Rotterdam experience. Semin Nucl Med. 2002;32(2):110–22.
Buscombe JR, Caplin ME, Hilson JW. Long-term efficacy of high-activity 111In-pentetreotide therapy in patients with disseminated neuroendocrine tumors. J Nucl Med. 2003;44:1–6.
Anthony LB, Woltering EA, Espanan GD. Indium-111-pentetreotide prolongs survival in gastroenteropancreatic malignancies. Semin Nucl Med. 2002;32(2):123–32.
Delpassand ES, Samarghandi A, Zamanian S, et al. Peptide receptor radionuclide therapy with 177Lu-DOTATATE for patients with somatostatin receptor–expressing neuroendocrine tumors. Pancreas. 2014;43(4):518–25.
Pool SE, Kam B, Breeman WAP. Increasing intrahepatic tumor uptake of 111In-DTPA-octreotide by loco regional administration. Eur J Nucl Med Mol Imaging. 2009;36:S427.
Reilly MN. Monoclonal antibody and peptide-targeted radiotherapy of cancer, Chapter 9. Hoboken, NJ: Wiley; 2010.
Schneider U, Hälg R. The impact of neutrons in clinical proton therapy. Front Oncol. 2015;5:235. https://doi.org/10.3389/fonc.2015.00235.
Meitner L. Über die Entstehung der Strahl-Spektren radioaktiver Substanzen. Zeitschrift für Physik A, Hadrons and Nuclei. 1922;9(1)
Auger P. Sur les rayons secondaires produits dans un gaz par des rayons X. CRAS. 1923;177:3.
Kassis A. The amazing world of auger electrons. Int J Radiat Biol. 2004;80(11–12):789–803.
Adelstein SJ, Merrill C. Sosman Lecture. The Auger process: a therapeutic promise? AJR. 1993;160(4):707–13.
Kassis A. Cancer therapy with Auger electrons: are we almost there? J Nucl Med. 2003;44(9):1479–81.
Kassis A. Radiotargeting agents for cancer therapy. Expert Opin Drug Deliv. 2005;2(6):981–91.
Sofou S. Radionuclide carriers for targeting of cancer. Int J Nanomedicine. 2008;3(2):181–99.
Boswell CA, Brechbiel MW. Auger electrons: lethal, low energy, and coming soon to a tumor cell nucleus near you. J Nucl Med. 2005;46(12):1946–7.
Adelstein SJ, Kassis AI. Strand breaks in plasmid DNA following positional changes of Auger-electron-emitting radionuclides. Acta Oncol. 1996;35(7):797–801.
Cornelissen B, Vallis KA. Targeting the nucleus: an overview of Auger-electron radionuclide therapy. Curr Drug Discov Technol. 2010;7(4):1570–638, Bentham Science Publishers Ltd
Buchegger F, Perillo-Adamer F, Dupertuis YM, et al. Auger radiation targeted into DNA: a therapy perspective. Eur J Nucl Med Mol Imaging. 2006;33:1352–63.
Humm JL, Howell RW, Rao DV. Dosimetry of Auger-electron emitting radionuclides: report no. 3 of AAPM Nuclear Medicine Task Group No. 6. Med Phys. 1994;21(12):1901–15.
Adelstein SJ, Kassis AI. Radiobiologic implications of the microscopic distribution of energy from radionuclides. Int J Rad Appl Instrum B. 1987;14(3):165–9.
Kassis AI, Harapanhalli RS, Adelstein SJ. Strand breaks in plasmid DNA after positional changes of Auger electron-emitting iodine125: direct compared to indirect effects. Radiat Res. 1999;152(5):530–8.
Kassis AI, Harapanhalli RS, Adelstein SJ. Comparison of strand breaks in plasmid DNA after positional changes of Auger electron emitting iodine-125. Radiat Res. 1999;151(2):167–76.
Buchegger F, Vieira JM, Blaeuenstein P, et al. Preclinical Auger and gamma radiation dosimetry for fluorodeoxyuridine-enhanced tumour proliferation scintigraphy with [123I] iododeoxyuridine. Eur J Nucl Med Mol Imaging. 2003;30(2):239–46.
Carlsson J, Forssell Aronsson E, Hietala SO, et al. Tumor therapy with radionuclides: assessment of progress and problems. Radiother Oncol. 2003;66(2):107–17.
Capello A, Krenning E, Bernard B, et al. 111In-labelled somatostatin analogues in a rat tumour model: somatostatin receptor status and effects of peptide receptor radionuclide therapy. Eur J Nucl Med Mol Imaging. 2005;32(11):1288–95.
Essand M, Gronvik C, Hartman T, et al. Radio-immunotherapy of prostatic adenocarcinomas: effects of 131I-labelled E4 antibodies on cells at different depth in DU 145 spheroids. Int J Cancer. 1995;63(3):387–94.
O’Donoghue JA, Bardies M, Wheldon TE. Relationships between tumor size and curability for uniformly targeted therapy with beta emitting radionuclides. J Nucl Med. 1995;36(10):1902–9.
Eckerman K, Endo A, Eds. MIRD (2008) Radionuclide data and decay schemes. 2nd ed. Reston, VA: The Society of Nuclear Medicine.
Hall Ε. Radiobiology for the radiologist. 5th ed. Philadelphia: Lippincott, Williams & Wilkins; 2000. p. 5–16, 80–87.
Kennedy AS, Raleigh JA, Varia MA. Proliferation and hypoxia in human squamous cell carcinoma of the cervix: first report of combined immunohistochemical assays. Int J Radiat Oncol Biol Phys. 1997;37(4):897–905.
Howell RW. Auger processes in the 21st century. Int J Radiat Biol. 2008;84(12):959–75.
Zeman Ε. Biologic basis of radiation oncology. In: Gunderson L, Tepper J, editors. Clinical radiation oncology. 1st ed. Philadelphia: Churchill Livingstone; 2000. p. 1–41.
Withers HR. Gastrointestinal cancer: radiation oncology. In: Kelsen DP, Daly JM, Levin B, Kern SE, Tepper JE, editors. Gastrointestinal oncology: principles and practice. 1st ed. Philadelphia: Lippincott Williams & Wilkins; 2002. p. 83–96.
Mornex F, Gérard F, Ramuz O. Late effects of radiations on the liver. Cancer Radiother. 1997;1(6):753–9.
Ingold J, Reed G, Kaplan Η. Radiation hepatitis. Am J Roentgenol. 1965;93:200–8.
Ogata K, Hizawa K, Yoshida Μ. Hepatic injury following irradiation: a morphologic study Tokushima. J Exp Med. 1963;9:240–51.
Lawrence TS, Robertson JM, Anscher MS. Hepatic toxicity resulting from cancer treatment. Int J Radiat Oncol Biol Phys. 1995;31(5):1237–48.
Austin-Seymour MM, Chen GT, Castro JR. Dose volume histogram analysis of liver radiation tolerance. J Radiat Oncol Biol Phys. 1986;12:31–5.
Dawson LA, Ten Haken RK, Lawrence TS. Partial irradiation of the liver. Semin Radiat Oncol ll. 2001;3:240–6.
Fajardo LF, Berthrong M, Anderson RE. Chapter 15, Liver, radiation pathology. 1st ed. New York: Oxford University; 2001. p. 249–57.
Breedis C, Young G. The blood supply of neoplasms in the liver. Am J Pathol. 1954;30:969–84.
Lien WM, Ackerman NB. The blood supply of experimental liver metastases II: a microcirculatory study of the normal and tumor vessels of the liver with the use of perfused silicone rubber. Surgery. 1970;68(2):334–40.
Ackerman NB, Lien WM, Kondi ES, et al. The blood supply of experimental liver metastases I: the distribution of hepatic artery and portal vein blood to “small” and “large” tumors. Surgery. 1970;66(6):1067–72.
Meade VM, Burton MA, Gray BN, et al. Distribution of different sized microspheres in experimental hepatic tumors. Eur J Cancer Clin Oncol. 1987;23(1):37–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Limouris, G.S. (2021). The Efficacy of Auger and Internal Conversion Electron Emission of 111In for Treating Neuroendocrine Tumors. In: Limouris, G.S. (eds) Liver Intra-arterial PRRT with 111In-Octreotide. Springer, Cham. https://doi.org/10.1007/978-3-030-70773-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-70773-6_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70772-9
Online ISBN: 978-3-030-70773-6
eBook Packages: MedicineMedicine (R0)