Abstract
The defects in intrinsic and innate immunity are a group of monogenic diseases in which there is a numeric and/or functional defect of the cellular components of innate immunity, not included in phagocyte defects or complement defects. It is a very diverse group of primary immunodeficiencies (PID) or inborn errors of immunity (IEI), both immunologically and clinically, but all share that (1) microbial susceptibility is usually very selective and from an early age (infant), and (2) commonly used immunological studies to discard a PID (lymphocyte studies, immunoglobulin dosage, protein vaccine responses) are usually normal; thus, innate immune PID’s diagnosis will require specific immunological tests.
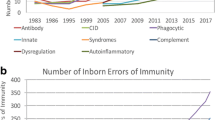
These deficiencies are encompassed in group VI of PID classification of the International Union of Immunological Societies expert committee (now called Inborn Errors of Immunity Committee) (Tangye et al., J Clin Immunol 40:24-64; 2020). They represent 1.5% of all PIDs (Modell et al., Immunol Res 66:367–80; 2018). This group is artificially divided into four subgroups depending on the microorganism to which patients manifest susceptibility (pyogenic bacteria, mycobacteria, virus, or fungus). In this chapter, we will follow this phenotypic approach (Bousfiha et al., J Clin Immunol 38:129–43; 2018), which we believe is more useful for clinicians when approaching a patient with a suspected PID.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Primary immunodeficiencies
- Innate immunity
- Toll-IL-1
- IFN-γ
- Mendelian susceptibility to mycobacterial disease
- Mucocutaneous candidiasis
- Herpes simplex encephalitis
- TLR3 pathway
- Asplenia
- Inborn errors of immunity
8.1 Introduction
The defects in intrinsic and innate immunity are a group of monogenic diseases in which there is a numeric and/or functional defect of the cellular components of innate immunity, not included in phagocyte defects or complement defects. It is a very diverse group of primary immunodeficiencies (PID) or inborn errors of immunity (IEI), both immunologically and clinically, but all share that (1) microbial susceptibility is usually very selective and from an early age (infant), and (2) commonly used immunological studies to discard a PID (lymphocyte studies, immunoglobulin dosage, protein vaccine responses) are usually normal; thus, innate immune PID’s diagnosis will require specific immunological tests.
These deficiencies are encompassed in group VI of PID classification of the International Union of Immunological Societies expert committee (now called Inborn Errors of Immunity Committee) [1]. They represent 1.5% of all PIDs [2]. This group is artificially divided into four subgroups depending on the microorganism to which patients manifest susceptibility (pyogenic bacteria, mycobacteria, virus, or fungus). In this chapter, we will follow this phenotypic approach [3], which we believe is more useful for clinicians when approaching a patient with a suspected PID. Accordingly, the chapter will be divided into four different sections: (1) predisposition to mycobacterial diseases (Mendelian susceptibility to mycobacterial disease, MSMD), (2) predisposition to pyogenic diseases (deficiencies in the Toll-IL1R pathway and congenital asplenia), (3) predisposition to viral diseases (susceptibility to HPV: epidermodysplasia verruciformis (HPV) and others; predisposition to severe viral infection: herpes simplex encephalitis (HSE)), and (4) predisposition to fungal diseases (predisposition to invasive fungal diseases and predisposition to mucocutaneous candidiasis).
8.2 Section 1: Predisposition to Mycobacterial Diseases
8.2.1 Defects in the IFN-γ Circuit
8.2.1.1 Introduction
Adverse events after bacille Calmette-Guerin vaccination , in the form of localized (BCGitis) [4, 5] or disseminated (BCGosis) [6] infections, some of them with a fatal outcome, were first reported in the 50s of the past century. The first report of BCGosis, which was suggested to be the first description of Mendelian susceptibility to mycobacterial disease (MSMD), was published during the 50s [7], and a fatal environmental mycobacteria (EM) infection in three relatives was reported in 1964 [8]. However, it was not until 1996 that the first genetic etiology of MSMD, autosomal recessive (AR) IFN-γR1 deficiency, was described in children with severe BCG or EM infection [9, 10].
8.2.1.2 Physiopathology and Genetics
Studies deciphering the genetic basis of MSMD have revealed the central role of IFN-γ-mediated immunity in the defense against mycobacteria (Fig. 8.1 and Table 8.1). Until date, mutations in 16 genes have been found to cause isolated MSMD or syndromic MSMD (Table 8.1). These genes are involved in IFN-γ production (IL12RB1 [11,12,13], IL12B [14, 15], IL12RB2 [16], IL23R [16], ISG15 [17, 18], SPPL2A [19, 20], TYK2 [21, 22], RORC [23], and IFNG [24]), the cellular responses to IFN-γ (IFNGR1 [9, 11, 25,26,27,28], IFNGR2 [29, 30], STAT1 [31,32,33], JAK1 [34], and CYBB [35,36,37]), or both (NEMO [36] and IRF8 [38]). Patients with syndromic MSMD, in contraposition to isolated MSMD, manifest a more complex clinical phenotype, with a predisposition to infection by other microorganisms or to other manifestations. Depending on the impact of the mutation (null or hypomorphic, resulting in complete or partial deficiency), the inheritance of the disease, the expression of the mutant allele (absent or detectable), or the mechanism responsible for the impaired function of the mutated protein, at least 30 different genetic etiologies of MSMD have been identified so far [20, 39]; IL-12Rβ1 deficiency and autosomal dominant (AD) IFN-γR1 deficiency are the first and second, respectively, most common defects [20, 24, 39, 40]. Mutations in STAT1 [41], IRF8 [38], and TYK2 [21, 22] cause isolated or syndromic MSMD depending of the pattern of inheritance and the functional impact of the mutation, and mutations in ISG15 [17, 18], RORC [23], and JAzK1 [34] were described only in patients with syndromic MSMD. With so many forms, the clinical boundaries of MSMD, particularly of some of the less frequent etiologies, are not fully defined, and at present, the genetic etiology remains unknown in about half of the patients.
Summary of molecules implicated in IFN-γ-mediated immunity . Molecules represented with bold characters are known to be cause of MSMD. Genes causing nonsyndromic forms are displayed in black, genes causing both syndromic and nonsyndromic forms in purple, and genes causing only syndromic forms in green
Recognition and phagocytosis of the bacilli by antigen-presenting cells (APC) and macrophages induce their activation and the production of an array of cytokines and chemokines, particularly tumor necrosis factor (TNF)-α, interferon-stimulated gene (ISG) 15, interleukin (IL)-12p70, and IL-23, which induce IFN-γ production by T, NK, and NKT cells. IL-12p40 (encoded by the IL12B gene) is common to IL-12p70 and IL-23. The IL-12Rβ1 molecule is shared by both the IL-12 and IL-23 receptor heterodimer, whereas IL-12Rβ2 and IL23R are unique to the IL-12 and IL-23 receptors, respectively. Tyk2 is a tyrosine kinase involved in IL-12R- and IL-23R-mediated signaling. ISG15 is secreted by many cell types, including myeloid cells and neutrophils, and it acts as a very potent IFN-γ-inducing cytokine in lymphocytes. ISG15 also encodes an intracellular interferon-induced ubiquitin-like protein that acts as a negative regulator of IFN-α/β, resulting in enhanced IFN-α/β immunity. The RORC gene encodes two protein isoforms that act as transcription factors: The nuclear orphan receptor γ (RORγ) is ubiquitously expressed, whereas the expression of RORγT is restricted to leukocytes. Patients with RORγ/RORγT deficiency show low numbers of ILC3, MAIT, and NKT cells and normal IFN-γ secretion by naïve or memory CD4+ T cells but strongly impaired IFN-γ production by Th1* cells and γδ T cells.
IFN-γ binding to the IFN-γ receptor, a heterodimer of IFN-γR1 and IFN-γR2, leads to activation of the tyrosine kinases Jak1 and Jak2 and to serine and tyrosine phosphorylation of the signal transducer and activator of transcription 1 (STAT1). Phosphorylated STAT1 forms a homodimer termed IFN-gamma-activated factor (GAF), which migrates into the nucleus and binds to the IFN gamma-activated sequence (GAS) to drive the expression of the target genes. Interferon regulatory factor 8 (IRF8) is a transcription factor induced by IFN-s, expressed in macrophages and dendritic cells. IRF8 binds to IFN-stimulated response elements (ISRE) and regulate the expression of many genes. SPPL2A encodes the signal peptide peptidase-like 2 A (SPPL2a), a protease with multiple substrates. A binding site for IRF8 has been identified in the Sppl2a promoter in mouse macrophages. Patients with SPPL2a deficiency have a deficit of conventional type 2 dendritic cells (cDC2). Both AD IRF8 and AR SPPL2a deficiencies confer a defect of IFN-γ production by mycobacterium-specific Th1* cells. NEMO encodes the nuclear factor-kappa B (NF-κB) essential modulator, which mediates signaling in the NF-κB pathway, required, among other signaling pathways, for TNF receptor- and CD40L-mediated activation. gp91phox, encoded by CYBB, is a major component of the phagocyte nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (PHOX) complex, required for effective intracellular killing of microorganisms.
8.2.1.3 Clinical Features
Mendelian susceptibility to mycobacterial diseases is a rare inherited condition characterized by a narrow vulnerability to poorly virulent mycobacteria, such as bacillus Calmette-Guerin (BCG) vaccines and environmental mycobacteria (EM), in otherwise healthy individuals. Tuberculosis, disseminated, extrapulmonary, or pulmonary, caused by the more virulent M. tuberculosis has been documented in some patients, particularly in deficiencies of IL-12Rβ1 [39, 42, 43], IFN-γR1 [26, 39], STAT1 [31, 39], or IL-12p40 [15, 44]. Besides the susceptibility to mycobacteria, some patients with isolated MSMD may also be susceptible to other intramacrophagic microorganisms: About half of the patients suffer from salmonellosis (frequently extra gastrointestinal), particularly nontyphoidal, and more rarely typhoidal; rare cases of infections caused by intramacrophagic fungi (histoplasmosis, coccidioidomycosis, paracoccidioidomycosis, candidiasis), parasites (Leishmaniasis, Toxoplasmosis), and bacteria (listeriosis, nocardiosis, klebsiellosis) have also been reported. Complete deficiencies of IFN-γR1 and IFN-γR2 rarely predispose to viral disease, particularly by herpes viruses [39]. In addition, since IL-12Rβ1 is also part of the IL-23 receptor and IL-12p40 is also a subunit of IL-23, patients with IL-12Rβ1 and IL-12p40 deficiencies are prone to mild forms of chronic mucocutaneous candidiasis (CMC) [15, 45]. Patients usually have a normal resistance to other microorganisms.
Patients can present with a wide range of clinical manifestations of mycobacterial disease, from local BCGitis to disseminated, invasive, and lethal infections. Disease onset is usually in childhood, but diagnosis in adolescence and adulthood has been reported. Usually, the most severe forms (for instance, AR complete IFN-γR1 or AR complete IFN-γR2 deficiency) show an early onset, and infections tend to be persistent and life-threatening in spite of antimycobacterial treatment. By contrast, the least severe forms (for instance, the partial -AR or AD- deficiencies of IFN-γR1 and IFN-γR2 or deficiencies of the IL-12/IL-23 receptors) can have a late onset and can improve with age, and the infections can be relatively circumscribed. In this context, osteomyelitis, even multifocal, by EM is common in patients with partial (AR or AD) IFN-γR1 and partial AD deficiency of STAT1 (and at a lesser extent in those with AR partial IFN-γR2 deficiency), whereas disseminated infections are classically observed in complete AR deficiencies of IFN-γR1, IFN-γR2, and STAT1 [20, 33, 39, 46,47,48,49,50,51,52]. Patients that survive to a mycobacterial disease may suffer from another mycobacterial infection or remain healthy; likewise, mycobacterial infections may or may not recur.
Clinical penetrance of MSMD may be incomplete, and it usually correlates with the extent of IFN-γ-mediated immunity. Complete AR IFN-γR1 and IFN-γR2 deficiencies are fully penetrant, and they are always lethal in the absence of hematopoietic stem cell transplantation (HSCT). By contrast, clinical penetrance is partial, and even very low, in patients with deficiencies of the IL-12 and/or IL-23 receptors. Only 50–70% of adults with IL-12Rβ1 deficiency, who have abolished IL-12- and IL-23-mediated responses, are symptomatic by the age of 40 years [13, 20, 39]. However, the clinical penetrance of IL-12Rβ2 deficiency, which does not affect IL-23-mediated responses, and of IL-23R and of partial AR Tyk2 deficiencies, which show normal IL-12-mediated responses, is very low (about 0.5%), and most patients remain asymptomatic in adulthood [16, 20, 22]. Therefore, some of the genetic etiologies of MSMD do not segregate as a bona fide Mendelian trait.
Some of these disorders predispose to syndromic MSMD due to involvement of the mutated proteins in signaling pathways other than the IFN-γ circuit. The etiopathogenesis of syndromic STAT1, IRF8, and Tyk2 deficiencies is discussed in Table 8.1 [20, 39]. Jak1 is involved in the cellular responses to numerous cytokines, including IFN-γ, IFNs-I/III, IL-4, IL-7, IL-9, IL-15, IL-21, and IL-6, and the only reported patient with JAK1 deficiency suffered from atypical mycobacterial disease, and a history of viral, fungal, and parasitic skin infection was documented [42]. Patients with biallelic RORC mutations display impaired IL-17A/F secretion by T cells, predisposing patients to CMC [23]. The absence of intracellular ISG15 leads to enhanced IFN-α/β immunity, and ISG15 deficiency also results in autoinflammation characterized by intracranial calcifications and epileptic seizures, resembling Aicardi-Goutieres syndrome and spondyloenchondromatosis [20, 43]. A few cases of carcinogenesis, even at young ages, have been described in patients with isolated MSMD [53, 54], and the patient with JAK1 deficiency died from urothelial carcinoma at the age of 22 years [34]. Macrophage activation syndrome or vasculitis was also reported [20, 39, 43].
8.2.1.4 Diagnosis and Immunological and Molecular Tests
Before the diagnosis of MSMD, acquired and inherited immunodeficiencies predisposing to mycobacterial diseases must first be excluded [43]. Several acquired immunodeficiencies predispose to mycobacterial infections: immunosuppressive drugs for solid organ transplantation, HSCT, leukemia, during chemotherapy, or following HSCT and biologicals, particularly those against TNF-α-mediated immunity or human immunodeficiency virus infection (HIV; BCG vaccination is contraindicated in HIV-infected individuals). Environmental mycobacteria (EM) and M. tuberculosis infections are increasingly being reported in patients with congenital lung defects such as primary ciliary dyskinesia, pulmonary alveolar proteinosis, and cystic fibrosis.
Several PID or IEI need to be discarded, since they predispose to mycobacterial infections, albeit usually in patients with other infectious and immunological phenotypes [43], including (i) patients with PID involving defects in the number and/or function of T cells (severe combined immunodeficiencies and combined immunodeficiencies), (ii) chronic granulomatous disease (particularly susceptible to BCG and M. tuberculosis), and (iii) GATA2 deficiency, predisposing to disseminated EM infections, and less frequently to tuberculosis, which may be the first clinical presentation even in otherwise healthy adults, although they can also occur during childhood. GATA2 patients have a broader clinical spectra, including viral infections, particularly warts; hematological disorders (myelodysplastic syndrome/leukemia); pulmonary alveolar proteinosis; and other non-immunological anomalies [55,56,57]. Patients with GATA2 deficiency have characteristically monocytopenia and a deficiency of DC, and low numbers of B cells and NK cell as well as neutropenia are also characteristic, although this PID is progressive and these leukocyte populations are variably affected [55]. Patients with AD gain-of-function mutations in STAT1 usually suffer from CMC, although disseminated EM infections and other opportunistic infections were reported [58].
Children or adults with recurrent or severe/disseminated mycobacterial infectious disease caused by BCG, EM, Mtb, or Salmonella, and in whom other inborn or acquired conditions predisposing to mycobacterial infection have been excluded, should be suspected of having MSMD. MSMD should be also suspected in patients with severe infections by other intramacrophagic microorganisms. Routine hematological and immunological analysis for PID used to be normal in patients with MSMD, although monocytopenia and DC deficiency, like in patients with GATA2 deficiency, can be detected in patients with IRF8 and SPPL2a deficiency. MSMD diagnosis comprises complex functional tests that need to be performed in specialized immunology laboratories [59].
Evaluation of cytokine production, developed by Feinberg et al. [11], is the gold standard for study of IFN-γ circuit integrity. This assay is based on the measurement of IL-12p40, IL-12p70, and IFN-γ after whole blood or, less frequently, peripheral blood mononuclear cells (PBMCs) stimulation. Stimulation conditions comprise incubation with live BCG with or without hrIL-12p70 or hr-IFN-γ co-stimulation for 18 h (for IL-12 measurement) or 48 h (for IFN-γ and IL-12 measurements). Although powerful, this technique has several limitations: (1) the intrinsic variability observed yet in healthy controls that hampers interpretation of results; (2) if fresh whole blood is used, it should be performed during the first 48h after extraction; and (3) the use of BCG stimulation can be limiting in diagnostic laboratories following ISO 15189 regulations. In an attempt to solve limitations, different strategies have been developed, including the performance of the test in cryopreserved cells to eliminate time-from-extraction limitation and the use of phytohemagglutinin and lipopolysaccharide as stimuli to avoid the use of BCG.
Quantitation of IFN-γ levels in plasma is a fast and easy technique for detection of IFN-γR deficiencies since high levels of this cytokine are characteristic in these defects, especially in complete AR deficiencies [60]. Cytometric evaluation of the presence of the IFN-γR1, IFN-γR2, and IL-12Rβ1 receptors is also a very useful tool [13, 27, 39]. However, normal expression does not exclude a defect since there are forms (especially in IFN-γR deficiencies) in which normal (AR forms) or even high (AD forms) nonfunctional proteins are expressed [13, 25, 27, 28, 30, 39, 61, 62]. Finally, cytometric evaluation of receptors’ downstream signaling after specific stimulation (STAT1 phosphorylation after IFN-γ and IFN-α stimulation [29, 32, 33, 47, 61, 63,64,65] and STAT4 phosphorylation after IL-12 stimulation [44, 62]) can help detect defects of IFN-γR/STAT1- and IL-12R-mediated activation [32, 33, 47, 65]. Other studies, such as IFN-γ production after IL-23 and ISG15 co-stimulation, may be useful for the characterization of the functional deficiency.
Genetic confirmation of the diagnosis of MSMD is of outmost importance for treatment and genetic counseling. When functional defects suggest a specific defect, Sanger sequencing is the option of choice. NGS technology, both in the form of gene panels or whole exome sequencing (WES), can be also useful to screen for all genetic etiologies simultaneously. In a more research-like setting, whole genome sequencing (WGS) is used to detect new disease-causing variations in nonprotein-coding regions of the genome.
8.2.1.5 Treatment
The clinical spectrum of MSMD ranges from mild forms to severe life-threatening disease. Complete AR deficiencies of IFN-γR1 and IFN-γR2, and the rare cases of complete AR deficiencies of STAT1 and IRF8, are lethal in the absence of HSCT in spite of antimycobacterial treatment [20, 39, 41, 66,67,68,69,70,71,72,73]. Milder cases (partial deficiencies of IFNγ-R1, deficiencies of IL-12p40, IL-12Rβ1, IL-12Rβ2, IL-23R, or ISG15) have a more favorable outcome and may respond well to appropriate antibiotic therapy [13, 15, 20, 39, 43, 68]. Subcutaneous IFN-γ therapy, in combination with antibiotics, should be considered in those patients able to mount cellular responses, even residual, to the cytokine. Prophylactic antimycobacterial antibiotics are usually not required in the less severe forms of MSMD, although it should be evaluated individually, particularly in patients with recurrent infections. Likewise, rare patients require prophylaxis against salmonella. Accurate genetic diagnosis and the functional distinction between complete and partial defects, as well as a careful characterization of the immunological phenotype, are of the utmost importance to ensure the best possible management of MSMD patients.
8.2.1.6 Autoantibodies Against IFN-γ. A Phenocopy of Inborn Errors of IFN-γ
In 2004 and 2005, the first reports of the existence of neutralizing autoantibodies against IFN-γ in patients with disseminated mycobacterial diseases were published, and numerous cases have been described so far [43, 74,75,76,77], This condition is not considered MSMD, but it is included in this section because it is classified as a phenocopy of inborn errors of IFN-γ. This disorder affects predominantly, but not exclusively, adults of Asian descent [74,75,76]. Most patients suffer from infections by EM, but M. tuberculosis was documented in some cases [43]. This condition is frequently associated with infections by other intramacrophagic microorganisms such as Salmonella, Cryptococcus neoformans, Histoplasma capsulatum, or Penicillium marneffei. The most direct approach for detecting IFN-γ autoantibodies is by using an ELISA system and by observing IFN-γ level recovery after the addition of exogenous IFN-γ to patient serum [78]. It should be included in the differential diagnosis of MSMD. Treatment of patients with anti-IFN-γ autoantibodies is complex and requires the control of the infection with long-term antibiotics and reducing the titer of autoantibodies; for the last, rituximab and cyclophosphamide have been used [75, 79, 80].
8.3 Section 2: Predisposition to Pyogenic Diseases
8.3.1 Deficiencies of the Toll-IL1R Pathway
In humans, Toll-like receptors (TLRs) are upon the most important receptors of infectious agents on myeloid leukocytes, particularly monocytes, macrophages, and dendritic cells (DCs). Certain TLRs are also found on lymphocytes and nonhematopoietic cells, such as fibroblasts, oligodendrocytes, and epithelial cells.
Each of the 10 TLRs is able to sense molecular patterns derived from bacteria, mycobacteria, viruses, fungi, and parasites. TLR1/2/4/5/6/10 are surface receptors while TLR3/7/8/9 are intracellular. Except for TLR3, upon TLR1-9 ligation, the cascade downstream TLRs will activate, through NF-kB, the transcription of a proinflammatory program including IL-6, IL-1b, and TNF-α to control the infection.
Most TLRs (except TLR3, and partially TLR4) and IL-1 receptors (IL1-R) (responsible for the response to IL-1, IL-18) share a common cytoplasmic domain, named TIR domain and a common downstream cascade, in which MyD88 is a key adaptor. IRAK family members (such as IRAK-4 and IRAK-1) are selectively recruited to TLRs and IL-1Rs by MyD88 (Fig. 8.2). TLR3, signals independently of MyD88 through TRIF, and TLR4, can signal both via TIRAP/MyD88 or TRIF. TLR10 uniquely inhibits both MyD88-dependent and -independent pathway [81].
Simplified schematic representation of Toll-IL1 pathway. Created with permission from BioRender.com
8.3.1.1 Deficiencies in IRAK-4 and MyD88
IRAK-4 deficiency was first described in 2003 [82] and MyD88 deficiency in 2008 [83]).
8.3.1.1.1 Clinical Features
The central clinical feature of IRAK-4 (OMIM #607676) and MyD88 (OMIM #612260) deficiencies is the high susceptibility to invasive and noninvasive infections with only a few Gram-positive and Gram-negative bacteria with absent or delayed signs of inflammation (local or systemic, including C-reactive protein elevation, fever) in the course of infections [84, 85]. Clinically, IRAK-4 and MyD88 deficiencies are indistinguishable (also named phenocopies) [86]. Infections usually have an acute course. During infection, some patients develop neutropenia, which is transient.
Invasive infections include sepsis, meningitis, arthritis, osteomyelitis, and deep inner organs/tissue abscesses. They are mainly caused by S. pneumoniae (70% of cases) and, to a lesser extent, by S. aureus and P. aeruginosa. Most patients suffer from their first invasive bacterial infection before the age of 2 years (85% of IRAK-4 deficiency patients and 92% of MyD88 deficiency patients, and before the age of 6 months in 42% of patients). One of the major causes of death is pneumococcal sepsis-meningitis at that early ages. The combination of invasive pneumococcal and staphylococcal disease is highly suggestive of a TIR deficiency. No invasive infections have been described after adolescence, suggesting that the MyD88-/IRAK-4-dependent TIR pathway becomes redundant once acquired immunity is fully functional and can ensure protection.
Noninvasive infections (cellulitis, furunculosis, folliculitis, lymphadenitis, usually necrotizing, and infections of the respiratory tract) are caused by S. aureus and, to a lesser extent, by pneumococcus and P. aeruginosa.
Infections by other Gram-positive and Gram-negative bacteria have also been observed, but IRAK-4- and MyD88-deficient patients are resistant to mycobacteria, viruses, fungi, and parasites.
Late umbilical cord separation (>2 weeks of age) has also been described in patients with IRAK-4 deficiency.
8.3.1.1.2 Immunological and Molecular Studies
8.3.1.1.2.1 Screening Tests
Evaluation of phagocyte respiratory oxidative burst using dihydrorhodamine test (DHR test), which is usually performed in the context of pyogenic infections to discard another primary immunodeficiency named chronic granulomatous disease (see Chap. 9), can raise the suspicion of deficiencies in IRAK-4/MyD88 because most patients display a specific pattern of responses, characterized by strongly diminished DHR responses to E. coli in the presence of normal DHR responses to phorbol myristate acetate (Alsina L, Vlagea A, manuscript in preparation).
8.3.1.1.2.2 Specific Tests
-
Shedding of CD62L in granulocytes after stimulation with specific agonists for different TLRs. Upon activation, granulocytes will cleave the ectodomain of a significant fraction of the CD62L present on the plasma membrane (Fig. 8.3).
-
Quantification of IL-6 and/or TNF-α production by whole blood or PBMC after stimulation with specific agonists of different TLRs. Responses across all TLRs (except for TLR3 and partially for TLR4), and the response to IL-1, IL-18, and IL-33, are abolished or diminished in IRAK-4 and MyD88 deficiencies [87, 88] (Fig. 8.4).
These tests cannot differentiate an IRAK-4 and MyD88 deficiency. Only genetics will confirm the mutation in IRAK-4 or MyD88.
8.3.1.1.2.3 Other Tests
-
There may be an elevation of IgE and IgG4 with normal levels of IgG, IgA, and IgM in one-third and two-thirds of patients, respectively. Production of specific antibodies against nonconjugated pneumococcal polysaccharides and isohemagglutinin levels are both diminished in one-third of patients [84].
Globally, no overt abnormalities in leukocyte subsets are observed in patients with IRAK-4 or MyD88 deficiencies except for a modest impact on IgM-dependent B-cell immunity, delaying its maturation: A diminished level of IgM+IgD+CD27+ B cells is observed, while IgM-IgD+CD27+-switched B cells are largely normal [89].
-
Genetics. Both diseases are autosomal recessive and show complete penetrance. A founder effect of MyD88 in “zingaros” (E402X/del) has been described (Rodriguez-Gallego C, manuscript in preparation).
8.3.1.1.3 Treatment and Prognosis
Antibiotic prophylaxis (daily trimethoprim-sulfamethoxazole and/or amoxicillin depending on the pattern of resistance to S. pneumoniae) is recommended, also intensive vaccination with conjugated and nonconjugated bacterial vaccines, including against pneumococcus, meningococcus, and H. influenzae (there is no vaccine contraindication) [90]. Immunoglobulin replacement therapy (IRT) is usually recommended. IRT and antibiotic prophylaxis are usually recommended up to at least 10–14 years old. In TIR defects, after 8 years of age, mortality associated with invasive infection is rare. Patients must be instructed to seek for medical attention upon any sign of infection.
8.3.1.2 Deficiency in IRAK-1
8.3.1.2.1 Clinical Features
Single patient described in 2017, with X-linked recessive complete IRAK-1 deficiency [91]. He presented a urinary tract infection by Klebsiella pneumoniae and two episodes of aspiration pneumonia before his death at 7 months old due to respiratory failure, probably ascribed to his severe congenital encephalopathy, which was later confirmed to be caused by MECP2 deficiency, in the context of an intrachromosomal deletion of about 112 kb on the long arm of the X chromosome (Xq28), which encompasses MECP2 and IRAK1.
With this single case, it is not possible to attribute a particular clinical phenotype to the lack of IRAK-1 since severe respiratory failure and pulmonary infections are commonly seen in patients with isolated MECP2 deficiency.
8.3.1.2.2 Immunological and Molecular Studies
-Fibroblasts from the IRAK-1- and MECP2-deficient patient responded poorly to all of the relevant TLR agonists tested. In contrast, IRAK-1- and MECP2-deficient fibroblasts from the patient displayed little or no impairment of IL-1R responses, by contrast to the results obtained for IRAK-4- or MyD88-deficient fibroblasts.
8.3.1.3 Deficiency in TIRAP
8.3.1.3.1 Clinical Features
Description in 2017 of a single family [92]. Autosomal recessive. Seven of the family members with the same genetic defect were healthy. The proband suffered from a pneumonia and sepsis due to S. aureus at 3 months of age. The difference in penetrance within family members was ascribed to the inability of the proband to develop antibodies against LTA (lipoteichoic acid), abundant in S. aureus, showing that human adaptive immunity had been able to rescue an inborn error of innate immunity in all family members, except for the proband, unable to produce specific antibodies.
8.3.1.3.2 Immunological and Molecular Studies
Responses to all TLR1/2, TLR2/6, and TLR4 agonists were impaired in the fibroblasts and leukocytes of all TIRAP-deficient individuals. However, the whole blood response to the TLR2/6 agonist staphylococcal lipoteichoic acid (LTA) was abolished only in the index case, the only family member lacking LTA-specific Abs. This defective response was reversed in the patient by anti-LTA mAb.
8.3.2 Isolated Congenital Asplenia
8.3.2.1 Clinical Features
Isolated congenital asplenia (ICA) is characterized by the absence of a spleen at birth without any other developmental defect. ICA predisposes individuals to life-threatening invasive infections early in childhood, caused by encapsulated bacteria, typically Streptococcus pneumoniae but occasionally Neisseria meningitidis and Haemophilus influenzae b [93].
A retrospective study in France showed that ICA affects at least 0.51 per 1 million newborns per year, but the incidence is probably higher (estimated 1 in 600,000) as individuals may not manifest until adulthood.
Asplenia can be suspected by the detection of Howell-Jolly bodies on a blood smear, which are the hallmark of the existence of a defect of spleen phagocytic function. Then, imaging tests can be performed to confirm the absence of spleen, such as ultrasound (US) or computed tomography (CT) scans of the abdomen, or even more sensitive and specific tests, such as selective spleen scintigraphy (SSS), which is performed using denatured erythrocytes labeled with Technetium-99m (Tc99m).
8.3.2.2 Immunological and Molecular Studies
RPSA gene is estimated to be responsible for 30–40% of ICA cases: 18 patients have been described to date bearing protein and nonprotein-coding mutations in RPSA, among a worldwide cohort of 73 patients with ICA. Most cases of ICA are sporadic, but multiplex kindreds exist, and the main mode of inheritance of ICA seems to be autosomal dominant (AD).
RPSA encodes for the ribosomal protein SA, a core component of the small subunit of the ribosome.
8.3.2.3 Treatment
Vaccines against encapsulated bacteria represent a major arm for the management of ICA patients. Annual influenza vaccination is recommended as well. Asplenia itself does not contraindicate the use of live attenuated vaccines. Antibiotic prophylaxis with penicillin V is recommended (amoxicillin is an alternative); the optimal duration of this antibiotic prophylaxis is still being debated (until 5 years old versus lifelong). In the case of allergy to penicillin, cotrimoxazole could be a valid alternative [94].
8.4 Section 3: Predisposition to Viral Diseases
8.4.1 Herpes Simplex Virus Encephalitis (HSE). Deficiencies of the TLR3 Pathway
8.4.1.1 Clinical Features
The primary infection by herpes simplex virus 1 (HSV-1) usually leads to symptoms involving the mucosa and skin, or most commonly asymptomatic infection. Other forms of HSV-1 infection exist, including a cutaneous form and eye infections consisting of keratitis and conjunctivitis. HSV-1 seroprevalence is high, demonstrating the typically benign nature of the infection [95]. Rarely does HSV-1 infect the CNS causing herpes simplex virus encephalitis (HSE). HSE is the most common form of sporadic viral encephalitis in Western countries, where it is estimated to occur in approximately two to four per 1,000.000 individuals per year [95, 96]. Peaks of HSE incidence occur between the ages of 6 months to 3 years, during primary HSV-1 infection, and in individuals older than 50 years, probably due to viral reactivation from latency.
Patients with impaired TLR3 immunity are susceptible to HSE. These patients remain normally resistant to other common viruses, as shown by positive serologic results to at least ten viruses without the occurrence of acute events. The patients have been also immunized with live vaccines with no adverse effect. HSV-1 infection outside the CNS is not usually observed. One TLR3-deficient patient developed CVB3 myocarditis in adulthood, and a mutation conferring TRAF3 deficiency was associated with development of multiple myeloma [97, 98].
8.4.1.2 Molecular Studies
Human defects in several components of TLR3 pathway (TLR3, TRIF, TRAF3, TBK1, IRF3, and UNC93B1) are known as genetic etiology of HSE, by impairing cortical neuron-intrinsic type I interferon (IFN) immunity to HSV-1 (Fig. 8.5), with incomplete clinical penetrance [99,100,101,102,103,104,105,106]. These patients have a similar cellular phenotype consisting in impaired TLR3 signaling in fibroblasts, which results in impaired antiviral IFN production, and enhanced viral replication and cell death following infection with HSV-1 and vesicular stomatitis virus (VSV). Patients suffer from HSE in the course of primary infection, without detectable HSV-1 dissemination, and they do not suffer from multiple episodes. TLR3 is expressed and can stimulate IFN production in neurons, astrocytes, oligodendrocytes, and microglial cells [107]. The role of TLR3 immunity in host defense against HSV-1 in the CNS was tested in induced pluripotent stem cells derived from UNC-93B- and TLR3-deficient patients and from healthy controls [108]. UNC-93B-deficient and TLR3-deficient derived oligodendrocytes and neurons were much more susceptible to HSV-1 infection than control cells, whereas deficient, derived, neural stem cells and astrocytes were not. The increased susceptibility observed in oligodendrocytes and neurons was found to be associated with impaired IFN-β and IFN-λ1 production by these cell types in response to HSV infection.
No impaired responses to TLR3, or other TLR, agonists are usually observed in peripheral blood mononuclear cells (PBMC) or whole blood cells from patients with deficiencies of TLR3 pathway. At present, the best laboratory screening test for these PID is the analysis of antiviral IFN production after stimulation by TLR3 agonists in fibroblasts. It is worth mentioning that some patients do not display any TLR3-IFN-related phenotype in fibroblasts, so detection of antiviral IFN production, as well as viral replication and cell death rates, after incubation with HSV-1 and VSV is the laboratory test of choice for detection of PID associated with impaired TLR3-mediated immunity.
Finally, it has been described three unrelated children suffering from influenza A virus (IAV) infection manifesting as acute respiratory distress syndrome (IAV-ARDS) caused by two loss-of-function (LOF) TLR3 mutations, previously described in autosomal dominant (AD) TLR3 deficiency underlying HSE. AD TLR3-deficient leukocytes produce normal amount of IFN-α upon stimulation with TLR3 agonist, HSV-1 or IAV. Therefore, AD TLR3 deficiency, caused by the same type of TLR3 LOF variants and even by the same TLR3 variant, accounts for at least two sporadic infectious diseases, HSE and IAV-ARDS, affecting isolated organs such as the CNS and the lung, respectively, in otherwise healthy children [106]. Although theoretically both severe infections can hit the same individual with TLR3 deficiency, the coalescence of these infections has not yet been described.
8.4.1.3 Treatment and Prognosis
Untreated, HSE is fatal in up to 70% of cases. Treatment with acyclovir significantly decreases the mortality rate, but up to 60% of patients suffer from long-term neurological sequelae of varying severity [109,110,111].
Inherited defects of the TLR3 pathway should be considered in the differential diagnosis of children with HSE. HSE is uncommon in reported patients with PID, even in those with T, B, and/or NK cell deficiencies [3].
8.4.2 Susceptibility to HPV: Epidermodysplasia Verruciformis (HPV) and Others
8.4.2.1 Clinical Features
Epidermodysplasia verruciformis (EV) is a rare Mendelian genodermatosis presenting with persistent, disseminated, flat warts and pityriasis versicolor-like skin lesions induced by human β-papillomaviruses (β-HPVs) which are lacking E5 and E8 open reading frames (ORF). Some patients develop nonmelanoma skin cancer.
8.4.2.2 Molecular Studies
Biallelic null mutations in TMC6 or TMC8 encoding EVER1 and EVER2, respectively, account for half of EV cases [112]. Moreover, it has been described biallelic deleterious mutations in CIB1, encoding calcium- and integrin-binding protein 1, CIB1. The formation of a multimer consisting of CIB1, EVER1, and EVER2 is required for CIB1 stability [113, 114]. Therefore, the disruption of the IFN-independent CIB1-EVER1-EVER2-dependent keratinocyte-intrinsic immunity underlies the selective susceptibility to β-HPVs in EV patients. One of the CIB mutations has been identified as a CIB1 splice-site founder mutation from Iranian origin with a common ancestor dating 650 years back [114].
8.4.2.3 Treatment and Prognosis
EV lesions are refractory to conventional therapies. Nonsurgical interventions with topical 5-fluorouracil, 5% imiquimod, tacalcitol, systemic retinoids combined with IFN-α, cimetidine, and topical 5-aminolevulinic acid photodynamic therapy yield inconsistent results. Approximately one-third of patients go on to develop malignancy with an average of 24 years between development of benign lesions and cancer. Invasive skin cancers are typically squamous cell carcinomas that often retain features of Bowen’s carcinomas. They develop slowly and are locally destructive [115].
8.4.3 WHIM Syndrome
8.4.3.1 Clinical Features
WHIM syndrome (WHIM) is a congenital immunodeficiency with characteristic clinical features that include susceptibility to HPV infection-induced warts, condyloma acuminata, and carcinomas; neutropenia, B cell lymphopenia, and hypogammaglobulinemia-related recurrent infections; and bone marrow myelokathexis characterized by myeloid hyperplasia and apoptosis [116, 117].
8.4.3.2 Molecular Studies
Specific mutations identified in WHIM patients include heterozygous C-terminus deletional mutations of portions of the intracellular carboxy terminus of the chemokine receptor, CXC chemokine receptor 4 (CXCR4). WHIM leukocytes have enhanced responses to stromal cell-derived factor-1 (SDF-1), the cognate ligand of CXCR4. Enhanced activity of CXCR4 delays release of mature neutrophils from the bone marrow resulting in neutropenia and senescence with apoptosis of mature neutrophils retained in the marrow [116, 117].
8.4.3.3 Treatment and Prognosis
Treatment for WHIM patients is not standardized but aims at mitigating hematologic defects and clinical symptoms associated with the disease. It is controversial whether the main driver for susceptibility to infection is leukopenia versus hypogammaglobulinemia or the combination of the two. There are no pharmacologic agents that have a demonstrated ability to prevent or treat warts in WHIM patients; topical cidofovir has proven useful in particular cases. The HPV vaccine is limited to a small subset of the most highly cancer-associated strains. Successful treatment of warts in WHIM patients is typically restricted to destructive therapies. Current therapies for neutropenia and infections in WHIM patients include G-CSF, GM-CSF, intravenous immunoglobulin (IVIg), and the newly tested CXCR4 antagonists such as plerixafor. While both G-CSF and GM-CSF have been used to increase and maintain circulating neutrophil counts in the normal range, G-CSF is probably the preferred and best tolerated agent. With hypogammaglobulinemia, administration of IVIg is effective at decreasing risk of infections. It has been reported that the hypogammaglobulinemia may improve following treatment with G-CSF. Use of prophylactic antibiotics in WHIM patients has not been evaluated statistically, but it is not unreasonable to extrapolate from studies in other primary immune deficiencies, neutropenias, or hypogammaglobulinemic states to support the use of antibiotic prophylaxis [116, 117].
The prognosis for WHIM patients depends in part on early recognition of the disorder, with aggressive medical intervention to reduce the frequency of recurrent bacterial infections and to detect and extirpate in the early stages any HPV lesions that appear to be dysplastic or malignant [116, 117].
8.4.4 Predisposition to Severe Virus Infections. The Critical Role of Type I and III Interferons
8.4.4.1 Clinical Features
Increasing numbers of patients suffering from severe viral diseases while remaining otherwise healthy have been reported in recent years. These patients routinely suffer from adverse reactions to live attenuated viral vaccines such as the yellow fever vaccine or the measles, mumps, and rubella (MMR) vaccine. Such patients often present with nonspecific symptoms, including rash in the site of inoculation, fevers, and lymphadenopathy. Besides these symptoms, the virus can disseminate and the patient may develop organ-specific features such as hepatitis, pneumonitis, hepatosplenomegaly, arthritis, or encephalitis, among others [118]. Additionally, this group of patients can also suffer from life-threatening diseases caused by viruses that, in most individuals, cause mild and self-limiting episodes, such as rhinovirus or influenza A. In these cases, patients present with fast-evolving lung infections that require hospitalization and can lead to acute respiratory distress syndrome (ARDS) [119, 120].
8.4.4.2 Molecular Studies
The genetic study of this group of patients has shown that deleterious mutations impairing immunity mediated by type I and III interferons are responsible for the disease (Fig. 8.1). Deficiency of MDA5 (encoded by IFIH1) that senses viral double-stranded RNAs (dsRNA) leads to impaired production of IFN-β and decreased induction of interferon-stimulated genes (ISG), hence reducing antiviral immunity. These defects are responsible for the severe disease that usually encompasses life-threatening rhinovirus and respiratory syncytial virus (RSV) infections [120,121,122]. Complete deficiency of the transcription factor IRF7 has been reported to cause severely reduced production of type I and type III interferons by leukocytes and plasmacytoid dendritic cells (pDCs) causing life-threatening infection by the influenza A virus H1N1 strain in addition to an adverse reaction to the MMR vaccine [119]. Deleterious biallelic mutations in the two chains of the receptor for type I interferons have been recently reported (IFN-αR1 and IFN-αR2) [118, 123]. These mutations altogether abolish type I interferon signaling, causing the patients to suffer from complications following MMR vaccination. Besides, one of the patients reported with IFN-αR1 deficiency suffers from a viscerotropic disease caused by the vaccine strain of the yellow fever virus [118]. Following stimulation by type I and III interferons, STAT1 and STAT2 are phosphorylated. These two molecules heterodimerize and, after binding IRF9, travel to the cell nucleus to induce the transcription of ISGs by binding the ISRE sequence (Fig. 8.5). Deficiencies in these three components have also been described. Deficiencies of STAT1 and STAT2 that completely abolish signaling downstream of the type I and III IFN receptors cause susceptibility to severe diseases by different viruses. While, as described at the beginning of this chapter, STAT1-deficient patients display elevated susceptibility to multiple viral infections such as HSV-I, CMV, or HHV6, STAT2 deficiency results in severe adverse reactions to the MMR vaccine, such as disseminated vaccine strain measles [41, 124,125,126,127,128,129,130]. In addition, STAT1 complete deficiency also impairs type II interferon signaling (IFN-γ specifically) accounting for the mycobacterial disease observed in these patients [31, 124,125,126,127]. IRF9 complete deficiency impairs type I, and likely type III, interferon signaling, causing life-threatening influenza A infection in addition to an adverse reaction to the MMR vaccine [131]. CD16 deficiency underlies severe herpes virus infection independent of immunity mediated by type I or III interferons by a mechanism involving impairment of spontaneous NK cytotoxicity and reduced expression of CD2 in NK cells [132, 133].
8.4.4.3 Treatment and Prognosis
Given the limited number of patients with each genetic defect, no standardized treatment has been proposed to date. In most cases, treatment has been based on antiviral therapy according to the type of virus identified in each patient and, in the most severe cases, with admission to intensive care unit (ICU), supportive care, assisted respiration, mechanical ventilation, and/or extracorporeal membrane oxygenation [119, 120]. Hematopoietic stem cell transplantation (HSCT) has been attempted in 3 STAT1-deficient patients with mixed results [125]. One patient with STAT2 deficiency responded positively during infectious episodes to intravenous immunoglobulin (IVIG).
8.5 Section 4: Predisposition to Fungal Infections
8.5.1 Introduction
Saprophytic and commensal fungi infect billions of people each year [134]. Among all known fungal species (more than 100,000), only 300 are able to cause diseases in humans [135]; thus, only some of them are considered medically relevant, including yeast (Candida spp.), mold (Aspergillus spp.), atypical fungus (Pneumocystis jirovecii), dimorphic fungi (Coccioides, Paracoccioides, and Histoplasma spp.), dermatophytes (Trichophyton spp.), and encapsulated fungi (Cryptococcus spp.).
The pathogenesis of the invasive and mucocutaneous fungal infections are largely different. While it seems that T-lymphocyte and IL-17 pathway determines the immune response involved in superficial infections, invasive infections are often seen related to quantitative or qualitative neutrophil disorders such as chronic granulomatous disease, autosomal recessive caspase recruitment domain-containing protein 9 (CARD9) deficiency, or neutropenic conditions [136].
8.5.2 Predisposition to Invasive Fungal Diseases
8.5.2.1 Definition and Epidemiology
Invasive fungal diseases (IFDs) are considered the major cause of morbidity and death among immunocompromised and hospitalized pediatric patients [137] with an incidence of around two million people worldwide [135] and with high rates of mortality (30–50%) [138]. The most common fungi involved in IFDs are Candida, Aspergillus, Cryptococcus, and Pneumocystis spp. [135].
Two main PID cause special susceptibility to suffer IFDs: chronic granulomatous disease (CDG; see Chap. 9) and CARD9 deficiency.
8.5.2.1.1 CARD9 Deficiency (OMIM 607212)
8.5.2.1.1.1 Clinical Features and Pathogenesis (Fig. 8.6)
CARD9 is an essential molecule of the innate immune system involved in the control of certain fungi identified by specific pathogen recognition receptors (such as Dectin-1, Dectin-2, mannose receptor, MINCLE), determining the myeloid and epithelial cell response [137, 139, 140]. Its impairment results in a poor production of specific inflammatory cytokines and chemokines (IL-6, IL-23, etc.), which are necessary for the differentiation of the IL-17-producing T cells [140]. Since CARD9 plays a specific role in antifungal immune response, these patients exhibit an extreme susceptibility to fungal infections but not to bacterial or viral infections [139].
The innate immunity to fungal infections relies on different mechanisms, including phagocytosis or production of reactive oxygen species, which are CARD9-independent. However, some fungi like unopsonized yeast cells (e.g., Candida spp) depend directly on the CARD9 pathway [139, 140]. This probably explains the specific clinical expression described in CARD9-deficient patients, which is characterized by the spontaneous development of Candida spp. infections, predominantly in oral mucosae, central nervous system (CNS), bone, and subcutaneous tissues. Infections due to dark-walled molds and yeast-like fungi (Aspergillus, Exophiala, and Phialophora) have been described in these patients too [137, 139, 140].
The clinical penetrance of this deficiency seems to be globally complete [141], and fungal disease can occur at any age, from early childhood to late adulthood; therefore, all children and adults with an unexplained IFD should be screened for CARD9 mutations [141].
8.5.2.1.1.2 Immunological and Molecular Studies
Until now, CARD9 deficiency has been reported only in patients with autosomal recessive mutations since none of the heterozygous patients has presented any unusual infection [141].
In the largest published cohort of analyzed CARD9 patients (31 patients), the basic immunological tests including cell count (neutrophils, T, B, and NK lymphocytes and monocytes) as well as the T and B lymphocytes subsets phenotyping, proliferative response to mitogens, or oxidative burst test were normal. Hypereosinophilia and high serum IgE levels had been observed in almost 50% of the patients without atopy or allergic symptoms [141]. The proportion of IL17-producing T cells was low in almost 2/3 of the patients and the production of IL-17A after stimulation with different fungal triggers (C. albicans, P. verrucosa, E. spinifera, etc.) was low only in 1/3 of the patients.
CARD9 protein expression could be assessed by western blotting in PBMCs, neutrophils, monocyte-derived dendritic cells, or monocytes-derived macrophages. However, since the protein expression varies depending on the consequences of the mutation on the protein, the detection of the protein is not sufficient to discard the diagnosis of CARD9 deficiency [141]. Although some more experimental tests are available to asses CARD9 pathway, in clinical practice, in front of a CARD9 suspicion, a genetic test should be performed to confirm this disease [141].
8.5.2.1.1.3 Treatment and Prognosis
The treatment options in these patients are limited [139]. Chronic mucocutaneous candidiasis (CMC) should be managed by long-life treatment with topic or azole agents as first-line treatments and with systemic therapy (azoles agents or echinocandins) in case of an extensive or uncontrolled disease. Treatment duration should be adapted to fungal species involved in the infection and to the site (CNS, skin, etc.) [141].
In some cases, adjuvant treatments should be added to antifungal treatment [141]. In this sense, good results using granulocyte-macrophage colony-stimulating [142] or granulocyte colony-stimulating factors [143] have been published, though this approach seems not effective in all cases. A recent case with successful hematopoietic stem cells transplant (HSCT) has been published [144], but the potential utility of HSCT in this disease remains unclear [141].
In conclusion, currently there are no defined guidelines for these patients: Long-term antifungal treatments are often needed with a fast relapse observed after withdrawal; besides, there is a lack of information regarding the role of HSCT in this disease [141].
8.5.3 Predisposition to Chronic Mucocutaneous Candidiasis
Candida spp. is commensal yeast that commonly colonizes mouth, colon, or vagina in healthy people. This asymptomatic colonization can turn to disease due to certain acquired (broad-spectrum antibiotics, oral steroids) or inherited (PID) risk factors [136, 145].
Within inherited conditions, chronic mucocutaneous candidiasis (CMC) represents a phenotypic manifestation of an heterogenous group of PID characterized by increased susceptibility to chronic or recurrent superficial Candida spp. infections [146], mainly associated with IL-17-mediated impaired immunity (Fig. 8.7) including AD hyper-IgE syndrome, CARD9 deficiency (able to present CMC and invasive fungal infections), AD transducer and activator transcription 1 (STAT1 gain of function), mutations related to IL-17 signaling (IL-17 or IL-17 receptor mutations), IL-12 receptor β1 or PID with aberrant neutralizant autoantibodies versus TH-17-produced cytokines such as autoimmune polyendocrinopathy syndrome type I [136, 146].
Antifungal immunity involved in CMC (adapted from Okada et al. [136])
In this chapter, we will focus on those inborn errors of innate immunity with special risk of CMC: STAT1 GOF, IL17F, IL17RA, IL17RF, and ACT1 mutations [1].
8.5.3.1 STAT1 Gain-of-Function Mutation (GOF) (OMIM 614162)
Autosomal dominant heterozygous missense mutations of STAT1 have been identified in a growing number of patients since its description in 2011 [136, 147]. This mutation seems to be the major cause of CMC, detected in more than half of patients [136, 147].
8.5.3.1.1 Clinical Features
The clinical phenotype is variable, ranging from CMC to severe autoimmunity and life-threatening infections [147]. The symptoms usually start during childhood [147, 148].
In terms of infectious manifestations, CMC represents the main problem although patients can also develop viral (mainly herpes virus but also JC or varicella-zoster virus), mycobacterial, and bacterial (e.g., St. aureus) infections. CMC is described in the oral mucosae (most frequent), skin, esophageal, genital, or nails, and Candida albicans is the most frequent fungi involved. Despite this, other dermatophytic and mold fungi have been reported. In countries where other endemic mycosis exists, such as coccidiosis or histoplasmosis, severe disseminated infections can be observed [147]. Patients with STAT1 GOF can also develop bacterial infections, especially sinopulmonary that can evolve to bronchiectasis [147].
Other relevant manifestations are autoimmune and autoinflammatory events, described in 1/3 of the patients, including hypothyroidism, type 1 diabetes, autoimmune cytopenia, alopecia, or a complete IPEX-like phenotype [136, 148].
Less frequent but severe complications observed in these patients include vascular alterations, mainly intracranial aneurysms, conferring a risk of hemorrhage or death [147], and an increased cancer risk (currently 6%), being carcinomas of the upper gastrointestinal tract the most common [147].
8.5.3.1.2 Immunological and Molecular Studies
The majority of patients show normal values for the initial immunologic screening, including immunoglobulins, immunoglobulin isotypes, and lymphocytes subpopulations (T, B, and NK). In some cases, low memory B cells and low IgG2 or IgG4 levels have been reported [136, 147]. On the other hand, TH17 count is commonly low (almost 80%) [147].
The STAT1 phosphorization/dephosphorization assay could be useful when STAT1 GOF mutation is suspected. An increased phosphorylation of tyrosine 701 after IFN-γ stimulation can be observed associated with impairment in dephosphorization in some patients, resulting in an increased of STAT1 phosphorylation in response to certain stimulations [136, 147]. Currently, the results of this assay are not conclusive, and normal result does not preclude the diagnosis [147].
Finally, a genetic test should be considered for patients with unexplained CMC. Until now, STAT1-GOF mutations described are located in coil-coil domain or DNA-binding domain (the latter might confer poor prognosis) [136, 147].
8.5.3.1.3 Treatment and Prognosis
Most of the affected patients have been successfully treated with long-term topical and/or systemic antifungal prophylaxis. Fluconazole is the main first-line oral therapy, while nystatin seems to be a good topical alternative [136, 147]. Antibacterial prophylaxis with trimethoprim-sulfamethoxazole should be considered in case of recurrent and uncontrolled bacterial infections [136] as well as IRT [147].
Janus-associated kinase (JAK), an upstream signal transducer for STAT1, inhibitors are being considered increasingly although only case reports are published with different rates of success. Recalcitrant CMC seems to respond successfully as well as certain autoimmunity events such as cytopenias [149] or alopecia. However, the effect seems to be transitory, and the treatment requires long-term administration. Infectious screening (mainly viral) is recommended during treatment, and in the absence of new evidence, it seems advisable considering antiviral prophylaxis during jak-inh therapy with acyclovir or valacyclovir [147].
HSCT could be considered as a curative-intention treatment, but currently the results are disappointing with approximately 50% of patient’s survival. However, the use of JAK inhibitor as a bridge therapy followed by HSCT might improve the HSCT outcomes [147, 150].
Table 8.2 summarizes the clinical features, immunological studies, and treatment recommended in other PID related with IL-17 pathway.
References
Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunningham-Rundles C, Etzioni A et al (2020) Human inborn errors of immunity: 2019 update on the classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol 40:24–64
Modell V, Orange JS, Quinn J, Modell F (2018) Global report on primary immunodeficiencies: 2018 update from the Jeffrey Modell Centers Network on disease classification, regional trends, treatment modalities, and physician reported outcomes. Immunol Res 66(3):367–380
Bousfiha A, Jeddane L, Picard C, Ailal F, Bobby Gaspar H, Al-Herz W et al (2018) The 2017 IUIS phenotypic classification for primary immunodeficiencies. J Clin Immunol 38(1):129–143
Blumenthal B (1954) A case of cutaneous tuberculosis: provoked by BCG-vaccination? Acta Derm Venereol 34(6):474–481
Groth-Petersen E (1952) Tuberculous abscess associated with BCG vaccination. Ugeskr Laeger 114(42):1503–1504
Wasz-Hockert O (1954) Bacterial meningitis in connection with BCG vaccination; report of a case. Ann Med Intern Fenn 43(1):77–80
Casanova J-L (2015) Severe infectious diseases of childhood as monogenic inborn errors of immunity. Proc Natl Acad Sci U S A 112(51):7128–7137
Engbaek HC (1964) Three cases in the same family of fatal infection with M. Avium. Acta Tuberc Pneumol Scand 45:105–117
Jouanguy E, Altare F, Lamhamedi S, Revy P, Emile JF, NEWPORT M et al (1996) Interferon-gamma-receptor deficiency in an infant with fatal bacille Calmette-Guerin infection. N Engl J Med 335(26):1956–1961
Newport MJ, Huxley CM, Huston S, Hawrylowicz CM, Oostra BA, Williamson R et al (1996) A mutation in the interferon-gamma-receptor gene and susceptibility to mycobacterial infection. N Engl J Med 335(26):1941–1949
Feinberg J, Fieschi C, Doffinger R, Feinberg M, Leclerc T, Boisson-Dupuis S et al (2004) Bacillus Calmette Guérin triggers the IL-12/IFN-γ axis by an IRAK-4- and NEMO-dependent, non-cognate interaction between monocytes, NK, and T lymphocytes. Eur J Immunol 34(11):3276–3284
van de Vosse E, Haverkamp MH, Ramirez-Alejo N, Martinez-Gallo M, Blancas-Galicia L, Metin A et al (2013) IL-12Rβ1 deficiency: mutation update and description of the IL12RB1 variation database. Hum Mutat 34(10):1329–1339
de Beaucoudrey L, Samarina A, Bustamante J, Cobat A, Boisson-Dupuis S, Feinberg J et al (2010) Revisiting human IL-12Rβ1 deficiency: a survey of 141 patients from 30 countries. Medicine (Baltimore) 89(6):381–402
Altare F, Lammas D, Revy P, Jouanguy E, Döffinger R, Lamhamedi S et al (1998) Rapid publication inherited interleukin 12 deficiency in a child with Bacille Calmette-Guérin and Salmonella enteritidis disseminated infection. J Clin Invest 102(12):2035–2040
Prando C, Samarina A, Bustamante J, Boisson-Dupuis S, Cobat A, Picard C et al (2013) Inherited IL-12p40 deficiency: genetic, immunologic, and clinical features of 49 patients from 30 kindreds. Medicine (Baltimore) 92(2):109–122
Martínez-Barricarte R, Markle JG, Ma CS, Deenick EK, Ramírez-Alejo N, Mele F et al (2018) Human IFN-immunity to mycobacteria is governed by both IL-12 and IL-23. Sci Immunol 30(3)
Zhang X, Bogunovic D, Payelle-Brogard B, Francois-Newton V, Speer SD, Yuan C et al (2015) Human intracellular ISG15 prevents interferon-α/β over-amplification and auto-inflammation. Nature 517(7532):89–93
Bogunovic D, Byun M, Durfee LA, Abhyankar A, Sanal O, Mansouri D et al (2012) Mycobacterial disease and impaired IFN-γ immunity in humans with inherited ISG15 deficiency. Science 337(6102):1684–1688
Kong X-F, Martinez-Barricarte R, Kennedy J, Mele F, Lazarov T, Deenick EK et al (2018) Disruption of an anti-mycobacterial circuit between dendritic and Th cells in human SPPL2a deficiency. Nat Immunol 19(9):973
Rosain J, Kong XF, Martinez-Barricarte R, Oleaga-Quintas C, Ramirez-Alejo N, Markle J et al (2019) Mendelian susceptibility to mycobacterial disease: 2014–2018 update. Immunol Cell Biol 97(4):360–367
Kreins AY, Ciancanelli MJ, Okada S, Kong X-F, Ramírez-Alejo N, Kilic SS et al (2015) Human TYK2 deficiency: mycobacterial and viral infections without hyper-IgE syndrome. J Exp Med 212(10):1641–1662
Kerner G, Ramirez-Alejo N, Seeleuthner Y, Yang R, Ogishi M, Cobat A et al (2019) Homozygosity for TYK2 P1104A underlies tuberculosis in about 1% of patients in a cohort of European ancestry. Proc Natl Acad Sci U S A 116(21):10430–10434
Okada S, Markle JG, Deenick EK, Mele F, Averbuch D, Lagos M et al (2015) Impairment of immunity to Candida and Mycobacterium in humans with bi-allelic RORC mutations. Science 349(6248):606–613
Kerner G, Guérin A, Oleaga-Quintas C, Rosain J, Rappaport F, Le Voyer T, et al. (2019) Mycobacterial disease due to inherited IFN-gamma deficiency. ESID 2019; Brussels.
Jouanguy E, Dupuis S, Pallier A, Döffinger R, Fondanèche M-C, Fieschi C et al (2000) In a novel form of IFN-γ receptor 1 deficiency, cell surface receptors fail to bind IFN-γ. J Clin Invest 105(10):1429–1436
Dorman SE, Picard C, Lammas D, Heyne K, van Dissel JT, Baretto R et al (2004) Clinical features of dominant and recessive interferon γ receptor 1 deficiencies. Lancet 364(9451):2113–2121
Sologuren I, Boisson-Dupuis S, Pestano J, Vincent QB, Fernández-Pérez L, Chapgier A et al (2011) Partial recessive IFN-γR1 deficiency: genetic, immunological and clinical features of 14 patients from 11 kindreds. Hum Mol Genet 20(8):1509–1523
Jouanguy E, Lamhamedi-Cherradi S, Lammas D, Dorman SE, Fondanèche MC, Dupuis S et al (1999) A human IFNGR1 small deletion hotspot associated with dominant susceptibility to mycobacterial infection. Nat Genet 21(4):370–378
Rosenzweig SD, Schwartz OM, Brown MR, Leto TL, Holland SM (2004) Characterization of a dipeptide motif regulating IFN-receptor 2 plasma membrane accumulation and IFN-responsiveness. J Immunol 173(6):3991–3999
Moncada-Velez M, Martinez-Barricarte R, Bogunovic D, Kong X-F, Blancas-Galicia L, Tirpan C et al (2013) Partial IFN- R2 deficiency is due to protein misfolding and can be rescued by inhibitors of glycosylation. Blood 122(14):2390–2401
Chapgier A, Boisson-Dupuis S, Jouanguy E, Vogt G, Feinberg J, Prochnicka-Chalufour A et al (2006) Novel STAT1 alleles in otherwise healthy patients with mycobacterial disease. PLoS Genet 2(8):e131
Dupuis S (2001) Impairment of mycobacterial but not viral immunity by a germline human STAT1 mutation. Science 293(5528):300–303
Hirata O, Okada S, Tsumura M, Kagawa R, Miki M, Kawaguchi H et al (2013) Heterozygosity for the Y701C STAT1 mutation in a multiplex kindred with multifocal osteomyelitis. Haematologica 98(10):1641–1649
Eletto D, Burns SO, Angulo I, Plagnol V, Gilmour KC, Henriquez F et al (2016) Biallelic JAK1 mutations in immunodeficient patient with mycobacterial infection. Nat Commun 7:13992
Bustamante J, Arias AA, Vogt G, Picard C, Galicia LB, Prando C et al (2011) Germline CYBB mutations that selectively affect macrophages in kindreds with X-linked predisposition to tuberculous mycobacterial disease. Nat Immunol 12(3):213–221
Bustamante J, Picard C, Boisson-Dupuis S, Abel L, J-LL C (2011) Genetic lessons learned from X-linked Mendelian susceptibility to mycobacterial diseases. Ann N Y Acad Sci 1246:92–101
Bustamante J, Picard C, Fieschi C, Filipe-Santos O, Feinberg J, Perronne C et al (2006) A novel X-linked recessive form of Mendelian susceptibility to mycobacterial disease. J Med Genet 44(2):e65–e65
Hambleton S, Salem S, Bustamante J, Bigley V, Boisson-Dupuis S, Azevedo J et al (2011) IRF8 mutations and human dendritic-cell immunodeficiency. N Engl J Med 365(2):127–138
Bustamante J, Boisson-Dupuis SSS, Abel L, Casanova J-L (2014) Mendelian susceptibility to mycobacterial disease: Genetic, immunological, and clinical features of inborn errors of IFN gamma immunity. Semin Immunol 26(6):454–470
Filipe-Santos O, Bustamante J, Chapgier A, Vogt G, de Beaucoudrey L, Feinberg J et al (2006) Inborn errors of IL-12/23- and IFN-γ-mediated immunity: molecular, cellular, and clinical features. Semin Immunol 18(6):347–361
Chapgier A, Wynn RF, Jouanguy E, Filipe-Santos O, Zhang S, Feinberg J et al (2006) Human complete Stat-1 deficiency is associated with defective type I and II IFN responses in vitro but immunity to some low virulence viruses in vivo. J Immunol 176(8):5078–5083
Boisson-Dupuis S, El Baghdadi J, Parvaneh N, Bousfiha A, Bustamante J, Feinberg J et al (2011) IL-12Rβ1 deficiency in two of fifty children with severe tuberculosis from Iran, Morocco, and Turkey. Cardona P-J, editor. PLoS One 6(4):e18524
Boisson-Dupuis S, Bustamante J, El-Baghdadi J, Camcioglu Y, Parvaneh N, El Azbaoui S et al (2015) Inherited and acquired immunodeficiencies underlying tuberculosis in childhood. Immunol Rev 264(1):103–120
Fieschi C (2004) A novel form of complete IL-12/IL-23 receptor 1 deficiency with cell surface-expressed nonfunctional receptors. Blood 104(7):2095–2101
Ouederni M, Sanal O, Ikinciogullari A, Tezcan I, Dogu F, Sologuren I et al (2014) Clinical features of Candidiasis in patients with inherited interleukin 12 receptor β1 deficiency. Clin Infect Dis 58(2):204–213
Obinata K, Lee T, Niizuma T, Kinoshita K, Shimizu T, Hoshina T et al (2013) Two cases of partial dominant interferon-γ receptor 1 deficiency that presented with different clinical courses of bacille Calmette-Guérin multiple osteomyelitis. J Infect Chemother 19(4):757–760
Tsumura M, Okada S, Sakai H, Yasunaga S, Ohtsubo M, Murata T et al (2012) Dominant-negative STAT1 SH2 domain mutations in unrelated patients with Mendelian susceptibility to mycobacterial disease. Hum Mutat 33(9):1377–1387
Jirapongsananuruk O, Luangwedchakarn V, Niemela JE, Pacharn P, Visitsunthorn N, Thepthai C et al (2012) Cryptococcal osteomyelitis in a child with a novel compound mutation of the IL12RB1 gene. Asian Pac J Allergy Immunol 30(1):79–82
Boudjemaa S, Dainese L, Héritier S, Masserot C, Hachemane S, Casanova J-L et al (2016) Disseminated BCG osteomyelitis related to STAT 1 gene deficiency mimicking a metastatic neuroblastoma. Pediatr Dev Pathol 3:16-02-1778-CR.1
Shamriz O, Engelhard D, Rajs AP, Kaidar-Shwartz H, Casanova J-L, Averbuch D (2013) Mycobacterium szulgai chronic multifocal osteomyelitis in an adolescent with inherited STAT1 deficiency. Pediatr Infect Dis J 32(12):1345–1347
Sasaki Y, Nomura A, Kusuhara K, Takada H, Ahmed S, Obinata K et al (2002) Genetic basis of patients with bacille Calmette-Guerin osteomyelitis in Japan: identification of dominant partial interferon-gamma receptor 1 deficiency as a predominant type. J Infect Dis 185(5):706–709
Arend S (2001) Multifocal osteomyelitis caused by nontuberculous mycobacteria in patients with a genetic defect of the interferon-Î3 receptor. Neth J Med 59(3):140–151
Cardenes M, Angel-Moreno A, Fieschi C, Sologuren I, Colino E, Molines A et al (2010) Oesophageal squamous cell carcinoma in a young adult with IL-12R beta 1 deficiency. J Med Genet 47(9):635–637
Toyoda H, Ido M, Nakanishi K, Nakano T, Kamiya H, Matsumine A et al (2010) Multiple cutaneous squamous cell carcinomas in a patient with interferon gamma receptor 2 (IFN gamma R2) deficiency. J Med Genet 47(9):631–634
Donadieu J, Lamant M, Fieschi C, de Fontbrune FS, Caye A, Ouachee M et al (2018) Natural history of GATA2 deficiency in a survey of 79 French and Belgian patients. Haematologica 103(8):1278–1287
Sologuren I, Martínez-Saavedra MT, Solé-Violán J, de Borges de Oliveira E, Betancor E, Casas I et al (2018) Lethal influenza in two related adults with inherited GATA2 deficiency. J Clin Immunol 38(4):513–526
Cohen JI, Dropulic L, Hsu AP, Zerbe CS, Krogmann T, Dowdell K et al (2016) Association of GATA2 deficiency with severe primary Epstein-Barr virus (EBV) infection and EBV-associated cancers. Clin Infect Dis 63(1):41–47
Toubiana J, Okada S, Hiller J, Oleastro M, Gomez ML, Becerra JCA et al (2016) Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood 127(25):3154–3164
Esteve-Solé A, Sologuren I, Martínez-Saavedra MT, Deyà-Martínez À, Oleaga-Quintas C, Martinez-Barricarte R et al (2018) Laboratory evaluation of the IFN-γ circuit for the molecular diagnosis of Mendelian susceptibility to mycobacterial disease. Crit Rev Clin Lab Sci 55(3):184–204
Fieschi C, Dupuis S, Picard C, Smith CI, Holland SM, Casanova JL (2001) High levels of interferon gamma in the plasma of children with complete interferon gamma receptor deficiency. Pediatrics 107(4):E48
Kong X-FF, Vogt G, Itan Y, Macura-Biegun A, Szaflarska A, Kowalczyk D et al (2013) Haploinsufficiency at the human IFNGR2 locus contributes to mycobacterial disease. Hum Mol Genet 22(4):769–781
Ehlayel M, de Beaucoudrey L, Fike F, Nahas SA, Feinberg J, Casanova J-LL et al (2008) Simultaneous presentation of 2 rare hereditary immunodeficiencies: IL-12 receptor beta1 deficiency and ataxia-telangiectasia. J Allergy Clin Immunol 122(6):1217–1219
Rosenzweig SD, Dorman SE, Uzel G, Shaw S, Scurlock A, Brown MR et al (2004) A novel mutation in IFN-gamma receptor 2 with dominant negative activity: biological consequences of homozygous and heterozygous states. J Immunol 173(6):4000–4008
Kong X-FF, Vogt G, Chapgier A, Lamaze C, Bustamante J, Prando C et al (2010) A novel form of cell type-specific partial IFN-gammaR1 deficiency caused by a germ line mutation of the IFNGR1 initiation codon. Hum Mol Genet 19(3):434–444
Sampaio EP, Bax HI, Hsu AP, Kristosturyan E, Pechacek J, Chandrasekaran P et al (2012) A novel STAT1 mutation associated with disseminated mycobacterial disease. J Clin Immunol 32(4):681–689
Naviglio S, Soncini E, Vairo D, Lanfranchi A, Badolato R, Porta F (2017) Long-term survival after hematopoietic stem cell transplantation for complete STAT1 deficiency. J Clin Immunol 37(7):701–706
Salem S, Langlais D, Lefebvre F, Bourque G, Bigley V, Haniffa M et al (2014) Functional characterization of the human dendritic cell immunodeficiency associated with the IRF8(K108E) mutation. Blood 124(12):1894–1904
Ying W, Liu D, Dong X, Wang W, Hui X, Hou J et al (2019) Current status of the management of mendelian susceptibility to mycobacterial disease in mainland China. J Clin Immunol 39(6):600–610
Reed B, Dolen WK (2018) The child with recurrent mycobacterial disease. Curr Allergy Asthma Rep 18(8):44
Olbrich P, Martínez-Saavedra MT, Perez-Hurtado JM, Sanchez C, Sanchez B, Deswarte C et al (2015) Diagnostic and therapeutic challenges in a child with complete Interferon-γ Receptor 1 deficiency. Pediatr Blood Cancer 62(11):2036–2039
Martínez-Barricarte R, Megged O, Stepensky P, Casimir P, Moncada-Velez M, Averbuch D et al (2014) Mycobacterium simiae infection in two unrelated patients with different forms of inherited IFN-γR2 deficiency. J Clin Immunol 34(8):904–909
Bandari AK, Muthusamy B, Bhat S, Govindaraj P, Rajagopalan P, Dalvi A et al (2019) A novel splice site mutation in IFNGR2 in patients with primary immunodeficiency exhibiting susceptibility to mycobacterial diseases. Front Immunol 10:1964
Oleaga-Quintas C, Deswarte C, Moncada-Vélez M, Metin A, Krishna Rao I, Kanık-Yüksek S et al (2018) A purely quantitative form of partial recessive IFN-γR2 deficiency caused by mutations of the initiation or second codon. Hum Mol Genet 27(22):3919–3935
Phoompoung P, Ankasekwinai N, Pithukpakorn M, Foongladda S, Umrod P, Suktitipat B et al (2017) Factors associated with acquired anti IFN-γ autoantibody in patients with nontuberculous mycobacterial infection. PLoS One 12(4):1–10
Hong GH, Ortega-Villa AM, Hunsberger S, Chetchotisakd P, Anunnatsiri S, Mootsikapun P et al (2019) Natural history and evolution of anti-interferon-γ autoantibody-associated immunodeficiency syndrome in Thailand and the United States. Intergovernmental panel on climate change, editor. Clin Infect Dis 58(12):7250–7257
Liew WK, Thoon KC, Chong CY, Tan NWH, Cheng DT, Chan BSW et al (2019) Juvenile-onset immunodeficiency secondary to anti-interferon-gamma autoantibodies. J Clin Immunol 39(5):512–518
Doffinger R, Helbert MR, Barcenas-Morales G, Yang K, Dupuis S, Ceron-Gutierrez L et al (2004) Autoantibodies to interferon-γ in a patient with selective susceptibility to mycobacterial infection and organ-specific autoimmunity. Clin Infect Dis 38(1):e10–e14
Chi CY, Chu CC, Liu JP, Lin CH, Ho MW, Lo WJ et al (2013) Anti-IFN-γ autoantibodies in adults with disseminated nontuberculous mycobacterial infections are associated with HLA-DRB1*16:02 and HLA-DQB1*05:02 and the reactivation of latent varicella-zoster virus infection. Blood 121(8):1357–1366
Patel SY, Ding L, Brown MR, Lantz L, Gay T, Cohen S et al (2005) Anti-IFN-gamma autoantibodies in disseminated nontuberculous mycobacterial infections. J Immunol 175(7):4769–4776
Chetchotisakd P, Anunnatsiri S, Nanagara R, Nithichanon A, Lertmemongkolchai G (2018) Intravenous cyclophosphamide therapy for anti-IFN-gamma autoantibody-associated Mycobacterium abscessus infection. J Immunol Res 2018:1–7
Jiang S, Li X, Hess NJ, Guan Y, Tapping RI (2016) TLR10 is a negative regulator of both MyD88-dependent and -independent TLR signaling. J Immunol 196(9):3834–3841
Picard C, Puel A, Bonnet M, Ku C-L, Bustamante J, Yang K et al (2003) Pyogenic bacterial infections in humans with IRAK-4 deficiency. Science 299(5615):2076–2079
von Bernuth H, Picard C, Jin Z, Pankla R, Xiao H, Ku C-L et al (2008) Pyogenic bacterial infections in humans with MyD88 deficiency. Science 321(5889):691–696
Picard C, von Bernuth H, Ghandil P, Chrabieh M, Levy O, Arkwright PD et al (2010) Clinical features and outcome of patients with IRAK-4 and MyD88 deficiency. Medicine (Baltimore) 89(6):403–425
Picard C, Casanova JL, Puel A (2011) Infectious diseases in patients with IRAK-4, MyD88, NEMO, or IκBα deficiency. Clin Microbiol Rev 24(3):490–497
Alsina L, Israelsson E, Altman MC, Dang KK, Ghandil P, Israel L et al (2014) A narrow repertoire of transcriptional modules responsive to pyogenic bacteria is impaired in patients carrying loss-of-function mutations in MYD88 or IRAK4. Nat Immunol 15(12):1134–1142
Frans G, Meyts I, Picard C, Puel A, Zhang S-Y, Moens L et al (2014) Addressing diagnostic challenges in primary immunodeficiencies: laboratory evaluation of Toll-like receptor- and NF-κB-mediated immune responses. Crit Rev Clin Lab Sci 51(2):112–123
von Bernuth H, Ku C-L, Rodriguez-Gallego C, Zhang S, Garty B-Z, Maródi L et al (2006) A fast procedure for the detection of defects in Toll-like receptor signaling. Pediatrics 118(6):2498–2503
Weller S, Bonnet M, Delagreverie H, Israel L, Chrabieh M, Maródi L et al (2012) IgM+IgD+CD27+ B cells are markedly reduced in IRAK-4-, MyD88-, and TIRAP- but not UNC-93B-deficient patients. Blood 120(25):4992–5001
Routes J, Abinun M, Al-Herz W, Bustamante J, Condino-Neto A, De La Morena MT et al (2014) ICON: diagnóstico precoz de inmunodeficiencias congénitas. J Clin Immunol 34(4):398–424
Della Mina E, Borghesi A, Zhou H, Bougarn S, Boughorbel S, Israel L et al (2017) Inherited human IRAK-1 deficiency selectively impairs TLR signaling in fibroblasts. Proc Natl Acad Sci U S A 114(4):E514–E523
Israel L, Wang Y, Bulek K, Della Mina E, Zhang Z, Pedergnana V et al (2017) Human adaptive immunity rescues an inborn error of innate immunity. Cell 168(5):789–800.e10
Bolze A, Boisson B, Bosch B, Antipenko A, Bouaziz M, Sackstein P et al (2018) Incomplete penetrance for isolated congenital asplenia in humans with mutations in translated and untranslated RPSA exons. Proc Natl Acad Sci U S A 115(34):E8007–E8016
Aguilar C, Malphettes M, Donadieu J, Chandesris O, Coignard-Biehler H, Catherinot E et al (2014) Prevention of infections during primary immunodeficiency. Clin Infect Dis 59(10):1462–1470
Whitley RJ, Miller RL (2001) Review immunologic approach to herpes simplex virus. Viral Immunol 14(3):466–473. Mary Ann Liebert, Inc
Najioullah F, Bosshard S, Thouvenot D, Boibieux A, Menager B, Biron F et al (2000) Diagnosis and surveillance of herpes simplex virus infection of the central nervous system. J Med Virol 61(4):468–473
Annunziata CM, Davis RE, Demchenko Y, Bellamy W, Gabrea A, Zhan F et al (2007) Frequent engagement of the classical and alternative NF-κB pathways by diverse genetic abnormalities in multiple myeloma. Cancer Cell 12(2):115–130
Keats JJ, Fonseca R, Chesi M, Schop R, Baker A, Chng WJ et al (2007) Promiscuous mutations activate the noncanonical NF-κB pathway in multiple myeloma. Cancer Cell 12(2):131–144
Guo Y, Audry M, Ciancanelli M, Alsina L, Azevedo J, Herman M et al (2011) Herpes simplex virus encephalitis in a patient with complete TLR3 deficiency: TLR3 is otherwise redundant in protective immunity. J Exp Med 208(10):2083–2098
Zhang SY, Jouanguy E, Ugolini S, Smahi A, Elain G, Romero P et al (2007) TLR3 deficiency in patients with herpes simplex encephalitis. Science 317(5844):1522–1527
Pérez de Diego R, Sancho-Shimizu V, Lorenzo L, Puel A, Plancoulaine S, Picard C et al (2010) Human TRAF3 adaptor molecule deficiency leads to impaired toll-like receptor 3 response and susceptibility to herpes simplex encephalitis. Immunity 33(3):400–411
Sancho-Shimizu V, Pérez De Diego R, Lorenzo L, Halwani R, Alangari A, Israelsson E et al (2011) Herpes simplex encephalitis in children with autosomal recessive and dominant TRIF deficiency. J Clin Invest 121(12):4889–4902
Herman M, Ciancanelli M, Ou YH, Lorenzo L, Klaudel-Dreszler M, Pauwels E et al (2012) Heterozygous TBK1 mutations impair TLR3 immunity and underlie herpes simplex encephalitis of childhood. J Exp Med 209(9):1567–1582
Casrouge A, Zhang SY, Eidenschenk C, Jouanguy E, Puel A, Yang K et al (2006) Herpes simplex virus encephalitis in human UNC-93B deficiency. Science 314(5797):308–312
Andersen LL, Mørk N, Reinert LS, Kofod-Olsen E, Narita R, Jørgensen SE et al (2015) Functional IRF3 deficiency in a patient with herpes simplex encephalitis. J Exp Med 212(9):1371–1379
Lim HK, Huang SXL, Chen J, Kerner G, Gilliaux O, Bastard P et al (2019) Severe influenza pneumonitis in children with inherited TLR3 deficiency. J Exp Med 216(9):2038–2056
Zhang SY, Herman M, Ciancanelli MJ, Pérez de Diego R, Sancho-Shimizu V, Abel L et al (2013) TLR3 immunity to infection in mice and humans. Curr Opin Immunol 25:19–33
Lafaille FG, Pessach IM, Zhang SY, Ciancanelli MJ, Herman M, Abhyankar A et al (2012) Impaired intrinsic immunity to HSV-1 in human iPSC-derived TLR3-deficient CNS cells. Nature 491(7426):769–773
Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL et al (2008) The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 47(3):303–327
Abel L, Plancoulaine S, Jouanguy E, Zhang S-Y, Mahfoufi N, Nicolas N et al (2010) Age-dependent mendelian predisposition to herpes simplex virus type 1 encephalitis in childhood. J Pediatr 157(4):623–629.e1
Kneen R, Michael BD, Menson E, Mehta B, Easton A, Hemingway C et al (2012) Management of suspected viral encephalitis in children—Association of British Neurologists and British Paediatric Allergy, Immunology and Infection Group National Guidelines. J Infect 64(5):449–477
Ramoz N, Rueda LA, Bouadjar B, Montoya LS, Orth G, Favre M (2002) Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet 32(4):579–581
de Jong SJ, Créquer A, Matos I, Hum D, Gunasekharan V, Lorenzo L et al (2018) The human CIB1–EVER1–EVER2 complex governs keratinocyte-intrinsic immunity to β-papillomaviruses. J Exp Med 215(9):2289–2310
Vahidnezhad H, Youssefian L, Saeidian AH, Mansoori B, Jazayeri A, Azizpour A et al (2019) A CIB1 splice-site founder mutation in families with typical epidermodysplasia verruciformis. J Invest Dermatol 139(5):1195–1198
Leiding JW, Holland SM (2012) Warts and all: human papillomavirus in primary immunodeficiencies. J Allergy Clin Immunol 130:1030–1048. NIH Public Access
Heusinkveld LE, Yim E, Yang A, Azani AB, Liu Q, Gao JL et al (2017) Pathogenesis, diagnosis and therapeutic strategies in WHIM syndrome immunodeficiency. Expert Opin Orphan Drugs 5:813–825
Kawai T, Malech HL (2009) WHIM syndrome: congenital immune deficiency disease. Curr Opin Hematol 16:20–26
Hernandez N, Bucciol G, Moens L, Le Pen J, Shahrooei M, Goudouris E et al (2019) Inherited IFNAR1 deficiency in otherwise healthy patients with adverse reaction to measles and yellow fever live vaccines. J Exp Med 216(9):2057–2070
Ciancanelli MJ, Huang SX, Luthra P, Garner H, Itan Y, Volpi S et al (2015) Infectious disease. Life-threatening influenza and impaired interferon amplification in human IRF7 deficiency. Science 348(6233):448–453
Lamborn IT, Jing H, Zhang Y, Drutman SB, Abbott JK, Munir S et al (2017) Recurrent rhinovirus infections in a child with inherited MDA5 deficiency. J Exp Med 214(7):1949–1972
Asgari S, Schlapbach LJ, Anchisi S, Hammer C, Bartha I, Junier T et al (2017) Severe viral respiratory infections in children with IFIH1 loss-of-function mutations. Proc Natl Acad Sci U S A 114(31):8342–8347
Zaki M, Thoenes M, Kawalia A, Nürnberg P, Kaiser R, Heller R et al (2017) Recurrent and prolonged infections in a child with a homozygous IFIH1 nonsense mutation. Front Genet 8:130
Duncan CJ, Mohamad SM, Young DF, Skelton AJ, Leahy TR, Munday DC et al (2015) Human IFNAR2 deficiency: lessons for antiviral immunity. Sci Transl Med 7(307):307ra154
Boisson-Dupuis S, Kong XF, Okada S, Cypowyj S, Puel A, Abel L et al (2012) Inborn errors of human STAT1: allelic heterogeneity governs the diversity of immunological and infectious phenotypes. Curr Opin Immunol 24(4):364–378
Burns C, Cheung A, Stark Z, Choo S, Downie L, White S et al (2016) A novel presentation of homozygous loss-of-function STAT-1 mutation in an infant with hyperinflammation-A case report and review of the literature. J Allergy Clin Immunol Pract 4(4):777–779
Dupuis S, Jouanguy E, Al-Hajjar S, Fieschi C, Al-Mohsen IZ, Al-Jumaah S et al (2003) Impaired response to interferon-alpha/beta and lethal viral disease in human STAT1 deficiency. Nat Genet 33(3):388–391
Vairo D, Tassone L, Tabellini G, Tamassia N, Gasperini S, Bazzoni F et al (2011) Severe impairment of IFN-gamma and IFN-alpha responses in cells of a patient with a novel STAT1 splicing mutation. Blood 118(7):1806–1817
Hambleton S, Goodbourn S, Young DF, Dickinson P, Mohamad SM, Valappil M et al (2013) STAT2 deficiency and susceptibility to viral illness in humans. Proc Natl Acad Sci U S A 110(8):3053–3058
Moens L, Van Eyck L, Jochmans D, Mitera T, Frans G, Bossuyt X et al (2017) A novel kindred with inherited STAT2 deficiency and severe viral illness. J Allergy Clin Immunol 139(6):1995–1997.e9
Shahni R, Cale CM, Anderson G, Osellame LD, Hambleton S, Jacques TS et al (2015) Signal transducer and activator of transcription 2 deficiency is a novel disorder of mitochondrial fission. Brain 138(Pt 10):2834–2846
Hernandez N, Melki I, Jing H, Habib T, Huang SSY, Danielson J et al (2018) Life-threatening influenza pneumonitis in a child with inherited IRF9 deficiency. J Exp Med 215(10):2567–2585
de Vries E, Koene HR, Vossen JM, Gratama JW, von dem Borne AE, Waaijer JL et al (1996) Identification of an unusual Fc gamma receptor IIIa (CD16) on natural killer cells in a patient with recurrent infections. Blood 88(8):3022–3027
Grier JT, Forbes LR, Monaco-Shawver L, Oshinsky J, Atkinson TP, Moody C et al (2012) Human immunodeficiency-causing mutation defines CD16 in spontaneous NK cell cytotoxicity. J Clin Invest 122(10):3769–3780
Brown GD, Denning DW, Levitz SM (2012) Tackling human fungal infections. Science 336(6082):647
Schmiedel Y, Zimmerli S (2016) Common invasive fungal diseases: an overview of invasive candidiasis, aspergillosis, cryptococcosis, and Pneumocystis pneumonia. Swiss Med Wkly 146(February):w14281
Okada S, Puel A, Casanova J-L, Kobayashi M (2016) Chronic mucocutaneous candidiasis disease associated with inborn errors of IL-17 immunity. Clin Transl Immunol 5(12):e114
Pana ZD, Roilides E, Warris A, Groll AH, Zaoutis T (2017) Epidemiology of invasive fungal disease in children. J Pediatr Infect Dis Soc 6(1):S3–S11
Lanternier F, Cypowyj S, Picard C, Bustamante J, Lortholary O, Casanova JL et al (2013) Primary immunodeficiencies underlying fungal infections. Curr Opin Pediatr 25:736–747
Drummond RA, Franco LM, Lionakis MS (2018) Human CARD9: A critical molecule of fungal immune surveillance. Front Immunol 9(AUG):1–7
Alves de Medeiros AK, Lodewick E, Bogaert DJA, Haerynck F, Van daele S, Lambrecht B et al (2016) Chronic and invasive fungal infections in a family with CARD9 deficiency. J Clin Immunol 36(3):204–209
Corvilain E, Casanova JL, Puel A (2018) Inherited CARD9 deficiency: invasive disease caused by ascomycete fungi in previously healthy children and adults. J Clin Immunol 38(6):656–693
Gavino C, Cotter A, Lichtenstein D, Lejtenyi D, Fortin C, Legault C et al (2014) CARD9 deficiency and spontaneous central nervous system candidiasis: Complete clinical remission with GM-CSF therapy. Clin Infect Dis 59(1):81–84
Celmeli F, Oztoprak N, Turkkahraman D, Seyman D, Mutlu E, Frede N et al (2016) Successful granulocyte colony-stimulating factor treatment of relapsing Candida Albicans meningoencephalitis caused by CARD9 deficiency. Pediatr Infect Dis J 35(4):428–431
Queiroz-Telles F, Mercier T, Maertens J, Sola CBS, Bonfim C, Lortholary O et al (2019) Successful allogenic stem cell transplantation in patients with inherited CARD9 deficiency. J Clin Immunol 39(5):462–469
Huppler AR, Bishu S, Gaffen SL (2012) Mucocutaneous candidiasis: The IL-17 pathway and implications for targeted immunotherapy. Arthritis Res Ther 14(4)
Carey B, Lambourne J, Porter S, Hodgson T (2019) Chronic mucocutaneous candidiasis due to gain-of-function mutation in STAT1. Oral Dis 25(3):684–692
Olbrich P, Freeman AF (2018) STAT1 and STAT3 mutations: important lessons for clinical immunologists. Expert Rev Clin Immunol 14(12):1029–1041
Toubiana J, Okada S, Hiller J, Oleastro M, Lagos Gomez M, Aldave Becerra JC et al (2016) Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood 127(25):3154–3164
Weinacht KG, Charbonnier LM, Alroqi F, Plant A, Qiao Q, Wu H et al (2017) Ruxolitinib reverses dysregulated T helper cell responses and controls autoimmunity caused by a novel signal transducer and activator of transcription 1 (STAT1) gain-of-function mutation. J Allergy Clin Immunol 139(5):1629–1640.e2
Leiding JW, Okada S, Hagin D, Abinun M, Shcherbina A, Balashov DN et al (2018) Hematopoietic stem cell transplantation in patients with gain-of-function signal transducer and activator of transcription 1 mutations. J Allergy Clin Immunol 141:704–717.e5
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Alsina, L. et al. (2021). Defects in Intrinsic and Innate Immunity. In: D'Elios, M.M., Baldari, C.T., Annunziato, F. (eds) Cellular Primary Immunodeficiencies. Rare Diseases of the Immune System. Springer, Cham. https://doi.org/10.1007/978-3-030-70107-9_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-70107-9_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70106-2
Online ISBN: 978-3-030-70107-9
eBook Packages: MedicineMedicine (R0)