Abstract
Wide European differences in cancer survival have been highlighted for decades. The most up-to-date world-wide trends in survival are available from the CONCORD programme. In Europe, data were provided for CONCORD by 157 population-based cancer registries in 31 countries, 22 of which provided data with national coverage.
During 2010–2014, age-standardised 5-year net survival in adults (15–99 years) was highest for melanoma of the skin (European range: 61–94%) and cancers of the prostate (68–94%) and breast (71–89%), followed by cervical cancer (54–80%), lymphoid malignancies (40–74%), cancers of the colon (45–68%) and rectum (42–68%), myeloid malignancies (23–58%), and ovarian (28–47%) and brain (21–42%) tumours. Survival was lower for cancers of the stomach (18–38%), oesophagus (5–24%), liver (4–21%), lung (8–20%) and pancreas (4–12%). In 21 European countries, 5-year survival for women diagnosed with breast cancer at an early or localised stage is on average 96.4%, but much lower (35–50%) for women diagnosed at an advanced stage.
There is a curvilinear relationship between 5-year net survival for breast cancer and the gross domestic product of each country, while the relationship between survival and total national expenditure on health, as a proportion of GDP, is more linear.
Real-world, observational studies of cancer survival, using population-based data on stage at diagnosis, treatment, lifestyle and socioeconomic status, are essential to quantify the extent to which these factors explain the wide international variations in survival.
Governments must recognise that population-based cancer registries are key policy instruments that can be used both to stimulate and to evaluate strategies for cancer control.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Population-based cancer registries
- Europe
- Net survival
- Disparities
- Stage at diagnosis
- Socioeconomic status
Introduction
Wide European differences in population-based survival from cancer have been highlighted for decades (Berrino et al. 1995, 1999, 2003; Capocaccia et al. 2009; De Angelis et al. 2014; Coleman et al. 2008; Allemani et al. 2015; Allemani et al. 2018).
The term disparity indicates a difference, especially one connected with unfair treatment. When we think about international differences in cancer survival, we generally focus our attention on disparities in relation to macro-economic indicators such as the gross domestic product (GDP) or total national expenditure on health (TNEH). Socioeconomic inequalities in health outcomes within a given country are generally examined with social class, unemployment or levels of education, but disparities in cancer survival may be geographical or racial (race/ethnicity). They may also reflect differential access to screening or optimal treatment.
Estimates of cancer survival obtained from data provided by population-based cancer registries are a key measure of the overall effectiveness of the health system in managing cancer. In contrast to clinical trials, which aim to achieve the highest possible survival in a group of patients selected by age, stage and lack of comorbidity, survival estimated from real-world data, obtained from population-based cancer registries, reflects the average survival achieved by all cancer patients, and therefore the overall quality of the health system in managing cancer, from early diagnosis to treatment and final outcome (Coleman 2014; Allemani 2017).
Population-based cancer registries routinely collect a basic data set on each person diagnosed with cancer in a population defined by residence in a country (national coverage) or a defined geographical area such as a province or state (regional coverage). The basic data set includes both patient characteristics (date of birth, sex and place of residence) and tumour characteristics (date of diagnosis; the topography, morphology and behaviour of the tumour, and the basis of diagnosis). Most cancer registries also collect information on each patient’s last known vital status (alive, dead, emigrated) and the date of the last known vital status. That information is essential for the estimation of survival.
The CONCORD protocol attempted to collect information on stage at diagnosis and the first course of treatment, on a voluntary basis. Unfortunately, most cancer registries do not yet collect stage at diagnosis or socioeconomic status systematically for every registered patient. Summary measures of socioeconomic status have not always been comparable between countries either. More recently, the European Deprivation Index (EDI) has largely resolved this problem (Guillaume et al. 2016), but this new European index has not yet been sufficiently widely used over a sufficient period of time to enable international comparisons of cancer survival using the EDI as a standardised measure of socioeconomic status.
The CONCORD programme provides the most up-to-date estimates of population-based survival trends world-wide. In this chapter, we will focus on geographical differences in cancer survival in Europe and offer a few examples of differences in the distribution of stage at diagnosis and stage-specific survival, and of survival by GDP and TNEH. We also provide a summary of the availability of data on socioeconomic status in Europe.
The CONCORD programme
The first cycle of the CONCORD programme included data for about two million adult patients (15–99 years) diagnosed during 1990–1994 with a cancer of the breast (women), colon, rectum or prostate, and followed up to 1999. Data were provided by 101 cancer registries in 31 countries, of which 16 with national coverage (Coleman et al. 2008).
The CONCORD programme established world-wide surveillance of trends in cancer survival for the first time in 2015 (CONCORD-2) by analysing data for 25,676,887 patients diagnosed during the 15 years from 1995 to 2009 with one of 10 common adult cancers (stomach, colon, rectum, liver, lung, breast (women), cervix, ovary or prostate, or leukaemia), and for 75,000 children (0–14 years) with acute lymphoblastic leukaemia (Allemani et al. 2015). These cancers represented 63% of the global cancer burden in 2009. Patients were followed up to 31 December 2009. The 279 participating registries covered a total population of 896 million people, in 67 countries that were home to two-thirds (4.8 billion) of the world’s population. In 40 countries, the data covered 100% of the national population.
In 2018, the third cycle of the CONCORD programme (CONCORD-3) updated the world-wide surveillance of cancer survival trends to include patients diagnosed from 2000 to 2014, with follow-up to 31 December 2014 (Allemani et al. 2018). It included data for 18 cancers or groups of cancers that collectively represented 75% of the global cancer burden in 2014: oesophagus, stomach, colon, rectum, liver, pancreas, lung, melanoma of the skin, breast (women), cervix, ovary and prostate in adults (15–99 years), and brain tumours, lymphomas and leukaemias in both adults and children (0–14 years). Trends and international variations in cancer survival were examined. Individual patient records for over 37.5 million cancer patients were included in the analyses. These data were provided by 322 population-based cancer registries in 71 countries and territories, of which 47 provided data with 100% national population coverage.
For some cancers where adequate data were available, survival analyses by stage at diagnosis, morphology and race/ethnicity (selected countries) have been published (Di Carlo et al. 2020; Alawadhi et al. 2019; Bannon et al. 2019; Bailey et al. 2018; OECD/European Union 2020; Weir et al. 2017). Analyses of the availability and timeliness of the first course of treatment are in preparation.
The Organisation for Economic Co-operation and Development (OECD) has included survival estimates from the CONCORD programme for 48 countries in its Health at a Glance publications since 2017 (Organisation for Economic Co-operation and Development 2019). This provides formal recognition by an international agency of the global coverage, methodological rigour and international comparability of the CONCORD survival estimates.
In Europe, data for CONCORD-3 were provided by 157 population-based cancer registries in 31 countries, 22 of which provided data with national coverage.
Results
Age-standardised 5-year net survival was highest for melanoma of the skin (European range: 61–94%) and cancers of the prostate (68–94%) and breast (71–89%), followed by cervical cancer (54–80%), lymphoid malignancies (40–74%), and cancers of the colon (45–68%) and rectum (42–68%) (Fig. 11.1a–c). Five-year survival in some countries reached almost 60% for myeloid malignancies in adults, although the range was very wide (23–58%), but less than 50% for cancers of the ovary (28–47%) and brain (21–42%), again with a very wide European range.
(a) Age-standardised 5-year net survival (%) for adults (15–99 years) diagnosed during 2010–2014 in Europe, by country: cancers of the oesophagus, stomach, colon, rectum, liver and pancreas. (Source: Allemani et al. 2018). Footnote: survival estimates are ranked from highest to lowest. Where data were available for more than one registry in a given country, the survival estimates were derived by pooling the data for that country, but excluding data from registries for which the estimates were considered less reliable because 15% or more of patients were (a) lost to follow-up or censored alive within 5 years of diagnosis, or if diagnosed in 2010 or later, before 31 December 2014 or (b) registered only from a death certificate or at autopsy or (c) with incomplete dates (i.e. unknown year of birth, unknown month or year of diagnosis or unknown year of last vital status). Data with 100% coverage of the national population. § Estimate flagged as less reliable because the only available estimates were from a registry or registries in this category. † Estimate not age-standardised (b) Age-standardised 5-year net survival (%) for adults (15–99 years) diagnosed during 2010–2014 in Europe, by country: cancers of the breast (women), cervix, ovary and lung, melanoma of the skin and cancer of the prostate (Source: Allemani et al. 2018). Footnote: survival estimates are ranked from highest to lowest. Where data were available for more than one registry in a given country, the survival estimates were derived by pooling the data for that country, but excluding data from registries for which the estimates were considered less reliable because 15% or more of patients were (a) lost to follow-up or censored alive within 5 years of diagnosis, or if diagnosed in 2010 or later, before 31 December 2014 or (b) registered only from a death certificate or at autopsy or (c) with incomplete dates (i.e. unknown year of birth, unknown month or year of diagnosis or unknown year of last vital status). Data with 100% coverage of the national population. § Estimate flagged as less reliable because the only available estimates were from a registry or registries in this category. † Estimate not age-standardised (c) Age-standardised 5-year net survival (%) for patients diagnosed during 2010–2014 in Europe, by country: adults (15–99 years) diagnosed with a tumour of the brain, or a myeloid or lymphoid malignancy, and children (0–14 years) diagnosed with a tumour of the brain, or a lymphoma or acute lymphoblastic leukaemia (ALL) (Source: Allemani et al. 2018). Footnote: survival estimates are ranked from highest to lowest. Where data were available for more than one registry in a given country, the survival estimates were derived by pooling the data for that country, but excluding data from registries for which the estimates were considered less reliable because 15% or more of patients were (a) lost to follow-up or censored alive within 5 years of diagnosis, or if diagnosed in 2010 or later, before 31 December 2014 or (b) registered only from a death certificate or at autopsy or (c) with incomplete dates (i.e. unknown year of birth, unknown month or year of diagnosis or unknown year of last vital status). Data with 100% coverage of the national population. § Estimate flagged as less reliable because the only available estimates were from a registry or registries in this category. † Estimate not age-standardised
Five-year survival was generally much lower for cancers of the stomach (18–38%), oesophagus (5–24%), liver (4–21%), lung (8–20%) and pancreas (4–12%).
Survival varied widely between countries. Four of the five Nordic countries (Finland, Iceland, Norway and Sweden), together with Belgium, Germany and Switzerland, showed the highest age-standardised 5-year net survival for many cancers, while survival was generally lowest among most of the Eastern European countries (Bulgaria, Poland, Romania, Slovakia and the Russian Federation).
In some Southern and Eastern European countries, 5-year survival for liver, pancreas and lung cancer was similar to or higher than in the Northern European countries, although 5-year net survival for these cancers rarely exceeds 20% anywhere. Denmark is closing the survival gap with the other Nordic countries; for patients diagnosed during 2010–2014, 5-year survival in Denmark was among the highest in Europe for cancers of the rectum, breast, cervix and brain, and for melanoma of the skin and lymphoid malignancies.
In the United Kingdom (UK), survival for cancers of the stomach, pancreas, lung, ovary and brain was similar to that seen in some of the Eastern European countries. Five-year survival was high in the European range only for melanoma of the skin.
International variation in survival was more marked for cancers of the oesophagus, stomach, colon and rectum, and for melanoma of the skin and the lymphoid malignancies, especially for patients diagnosed during 2010–2014 (Figs. 11.1a–c and 11.2a–c).
(a) International variation in age-standardised 5-year net survival (%) for adults (15–99 years) diagnosed during 2010–2014, by European region: cancers of the oesophagus, stomach, colon, rectum, liver and pancreas (Source: Allemani et al. 2018). Footnote: funnel plot with each national survival estimate plotted against its statistical precision (the inverse of its variance). The target value is the pooled estimate for all participating countries in the same period. Only age-standardised estimates are included. Control limits for 95% and 99.8% are shown. The wider control limits to the left emphasise the increased variability expected between survival estimates that are less statistically precise, while the narrower limits to the right emphasise the reduced variability between more precise estimates (Quaresma et al. 2014) (b) International variation in age-standardised 5-year net survival (%) for adults (15–99 years) diagnosed during 2010–2014, by European region: cancers of the breast (women), cervix, ovary and lung, melanoma of the skin and cancer of the prostate (Source: Allemani et al. 2018). Footnote: funnel plot with each national survival estimate plotted against its statistical precision (the inverse of its variance). The target value is the pooled estimate for all participating countries in the same period. Only age-standardised estimates are included. Control limits for 95% and 99.8% are shown. The wider control limits to the left emphasise the increased variability expected between survival estimates that are less statistically precise, while the narrower limits to the right emphasise the reduced variability between more precise estimates (Quaresma et al. 2014) (c) International variation in age-standardised 5-year net survival (%) for patients diagnosed during 2010–2014, by European region: adults (15–99 years) diagnosed with a tumour of the brain or a myeloid or lymphoid malignancy, and children (0–14 years) diagnosed with a tumour of the brain or a lymphoma or acute lymphoblastic leukaemia (ALL) (Source: Allemani et al. 2018). Footnote: funnel plot with each national survival estimate plotted against its statistical precision (the inverse of its variance). The target value is the pooled estimate for all participating countries in the same period. Only age-standardised estimates are included. Control limits for 95% and 99.8% are shown. The wider control limits to the left emphasise the increased variability expected between survival estimates that are less statistically precise, while the narrower limits to the right emphasise the reduced variability between more precise estimates (Quaresma et al. 2014)
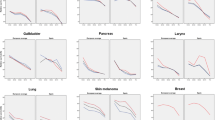
For many cancers, survival also varies widely within countries (Fig. 11.3a–c), although the variations are less marked for cancers with the best and worst prognosis. For most cancers, regional variation in the countries of Southern and Eastern Europe (France, Italy, Poland, Spain and the Russian Federation) was wider than in countries of Central Europe (Germany and Switzerland) and the UK.
(a) Regional variation in age-standardised 5-year net survival (%) in European countries with more than one participating population-based cancer registry: adults (15–99 years) diagnosed during 2010–2014 with a cancer of the oesophagus, stomach, colon, rectum, liver or pancreas (Source: Allemani et al. 2018). Footnote: Each box-plot shows the range of survival estimates among all cancer registries for which suitable estimates were obtained in each country. Survival estimates considered less reliable are not included. The vertical line inside each box represents the median survival estimate among all contributing registries (the central value in the range, or 50th centile). The box covers the interquartile range (IQR) between the lower and upper quartiles (25th and 75th centiles). Where there are only a few widely scattered estimates, the median may be close to the lower or upper quartile. The extreme limits of the box-plot are 1.5*IQR below the lower quartile and 1.5*IQR above the upper quartile. Open circles indicate ‘outlier’ values, outside this range (b) Regional variation in age-standardised 5-year net survival (%) in European countries with more than one participating population-based cancer registry: adults (15–99 years) diagnosed during 2010–2014 with a cancer of the breast (women), cervix, ovary or lung, melanoma of the skin or cancer of the prostate (Source: Allemani et al. 2018). Footnote: Each box-plot shows the range of survival estimates among all cancer registries for which suitable estimates were obtained in each country. Survival estimates considered less reliable are not included. The vertical line inside each box represents the median survival estimate among all contributing registries (the central value in the range, or 50th centile). The box covers the interquartile range (IQR) between the lower and upper quartiles (25th and 75th centiles). Where there are only a few widely scattered estimates, the median may be close to the lower or upper quartile. The extreme limits of the box-plot are 1.5*IQR below the lower quartile and 1.5*IQR above the upper quartile. Open circles indicate ‘outlier’ values, outside this range (c) Regional variation in age-standardised 5-year net survival (%) in European countries with more than one participating population-based cancer registry: adults (15–99 years) diagnosed with a tumour of the brain, or myeloid or lymphoid malignancy, and children (0–14 years) diagnosed with a tumour of the brain, or lymphoma or acute lymphoblastic leukaemia (ALL) (Source: Allemani et al. 2018). Footnote: Each box-plot shows the range of survival estimates among all cancer registries for which suitable estimates were obtained in each country. Survival estimates considered less reliable are not included. The vertical line inside each box represents the median survival estimate among all contributing registries (the central value in the range, or 50th centile). The box covers the inter-quartile range (IQR) between the lower and upper quartiles (25th and 75th centiles). Where there are only a few widely scattered estimates, the median may be close to the lower or upper quartile. The extreme limits of the box-plot are 1.5*IQR below the lower quartile and 1.5*IQR above the upper quartile. Open circles indicate ‘outlier’ values, outside this range
Five-year survival has increased steadily for many cancers between 2000–2004 and 2010–2014, particularly for cancers of the colon and rectum and the lymphoid malignancies (data not shown), but for some of the most common cancers, such as those of the lung, liver, pancreas and oesophagus, age-standardised 5-year net survival remains stubbornly below 20%.
OECD recently included CONCORD estimates of age-standardised 5-year net survival by stage at diagnosis for women diagnosed with breast cancer during 2010–2014 in 21 European countries in Health at a Glance: Europe 2020 (OECD/European Union 2020) (Fig. 11.4). Across Europe as a whole, approximately 50% of women were diagnosed at an early stage and 10% at an advanced stage. Five-year survival for women diagnosed at an early or localised stage is on average 96.4% in the EU, but survival for women diagnosed at an advanced stage remains much lower, ranging between 35% and 50%.
Age-standardised 5-year net survival (%) for breast cancer, by stage at diagnosis: Europe, women diagnosed during 2010–2014. Footnote: Stage was categorised according to the seventh edition of the Tumour, Nodes, Metastasis (TNM) staging system (Sobin et al. 2009). Early or localised stage refers to tumours without lymph node involvement or metastasis (T1–3, N0, M0); ‘advanced stage’ to large tumours with ulceration or involvement of the chest wall, or those that had metastasised to other organs (T4, any N, M0 or M1). The EU average is unweighted. 1. Coverage is less than 100% of the national population for stage-specific survival estimates. 2. Coverage is less than 100% of the national population. 3. Survival estimates for advanced stage are not age-standardised. 4. Data for 2004–2009. Source: CONCORD programme, London School of Hygiene and Tropical Medicine. Reproduced with permission from OECD: Fig. 6.21 in (OECD/European Union 2020)
There is a curvilinear relationship between 5-year net survival for breast cancer and the gross domestic product of each country. The relationship reaches an asymptote around a GDP of US$30,000 to US$35,000 per head of population. Above a certain level of wealth, 5-year survival levels appear to plateau. The relationship between 5-year survival and total national expenditure on health as a proportion of GDP is more linear (Verhoeven et al. 2020).
Other European Studies
Women with breast cancer with a higher socioeconomic position in Sweden have been shown to have a lower risk of death after controlling for tumour characteristics, treatment, comorbidity and lifestyle factors (relative risk [SRR] 0.82; 95% CI 0.70–0.97) (Lundqvist et al. 2016). This study suggests the need to examine further the impact of screening attendance, use of contraceptives, lifestyle and reproductive variables. Similar inequalities have been shown in England after screen-detection and the timeliness and appropriateness of treatment were taken into account (Woods et al. 2016).
A pooled analysis of 18 case-control studies has shown that women with a lower level of education who were diagnosed with ovarian cancer had more advanced disease than those with a higher level of education, after adjusting for age and race/ethnicity (odds ratio [OR] 1.15; 95% CI 1.03–1.28) (Praestegaard et al. 2016).
Similar results have been found for lung cancer, with patients from a lower socioeconomic position slightly more likely to present with later-stage disease (OR 0.92, 0.84–0.99) (Dalton et al. 2011). The more deprived patients were much less likely to receive lung cancer surgery (OR 0.61; 0.56–0.66) or chemotherapy (OR 0.80; 0.68–0.95), although no difference was seen for receipt of radiotherapy (OR 1.07; 0.87–1.32) (Forrest et al. 2013).
A recent systematic review has shown that patients with a lower socioeconomic position tend to have lower survival from colon and rectal cancers (Manser and Bauerfeind 2014). This may be due to lower compliance with screening programmes and a more advanced stage at diagnosis. Differences in access to care, compliance with treatment and the quality of treatment may also play a role. Another systematic review, carried out before the introduction of screening in the Netherlands, showed that colorectal cancer patients with a low socioeconomic position are generally less likely to receive adjuvant or neo-adjuvant treatment (Aarts et al. 2010).
A regional population-based study in England has suggested that elimination of the differences in survival from melanoma of the skin between socioeconomic groups and between men and women could reduce deaths within 5 years of diagnosis by approximately 11% (215 deaths a year) on a national scale (Rutherford et al. 2015).
Discussion
Government policy may be designed to minimise the impact of socioeconomic position on disease outcomes in several ways: first, by acting to reduce social inequality per se; then by reducing exposure to risk factors that may also be prognostic factors, such as smoking or obesity; and finally by developing policy to ensure that socioeconomic position does not influence referral for diagnosis or access to optimal treatment.
For example, socioeconomic inequalities in cancer survival in the UK were first identified 40 years ago (Silman and Evans 1981). Twenty-year trends in those socioeconomic inequalities have been documented (Coleman et al. 1999). The UK subsequently developed several strategies designed to reduce these inequalities in cancer survival (Expert Advisory Group on Cancer 1995; Department of Health 2000, 2007, 2011). Despite substantial investment in health personnel and equipment in the early 2000s, the impact of these strategies on socioeconomic inequalities in cancer survival has been disappointing (Exarchakou et al. 2018a, b; Fowler et al. 2017; Ellis et al. 2012; Rachet et al. 2010; All-Party Parliamentary Group on Breast Cancer 2010; National Cancer Intelligence Network 2010; Department of Health 2008).
As the former Chief Medical Officer of the American Cancer Society has put it: ‘Equal treatment yields equal outcome among equal patients, but there is no equal treatment’ (Brawley 2006). He was referring to the wide and persistent differences in lung cancer survival between blacks and whites in the United States (US), where race and ethnicity are often seen as partial surrogates for socioeconomic status, especially in access to health insurance and health care. The Veterans Health Administration, a federal system that provides health care for US military personnel and their families, has also shown that patients who receive the same treatment obtain similar outcomes, regardless of race or socioeconomic status (Akerley et al. 1993).
In the UK, extended follow-up of patients recruited to large, well-conducted, randomised controlled trials of treatment for colorectal and testicular cancers, in which there was no difference in outcome between the various arms of the trials, did not show the socioeconomic inequalities in survival seen in population-based studies that include all patients (Nur et al. 2008, 2012). These studies also suggest that, as in the US, the persistent socioeconomic inequalities in cancer survival must somehow be related to differential access to optimal treatment, whether that arises from patient delay in seeking health care, medical delay in referral, or differential navigation or access to treatment within the healthcare system (Lyratzopoulos et al. 2003, 2012, 2013, 2014).
One of the main limitations of the studies analysing socioeconomic differences is that they use various measures of socioeconomic position, often categorised differently. Education, disposable income, occupation, housing tenure and place of residence are only some of the indicators found in the literature.
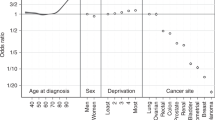
A recent world-wide survey of population-based cancer registries, carried out as part of the VENUSCANCER project, funded by the European Research Council, has shown that each population-based cancer registry in Europe holds different types of socioeconomic data. In Eastern European countries, these data are not available at all, whereas in the Nordic countries, France and Slovenia, several variables are available on the socioeconomic position of all registered patients (Fig. 11.5). In Poland, data on education level are available in 3 of the 5 registries that responded.
Availability of socioeconomic data (%) in population-based cancer registries in 2019: Europe. Footnote: The number of registries replying to the survey in each country is shown in parentheses (see text). (VENUSCANCER project 2017)
A standardised measure to compare social inequalities in health between countries with different economies, social structures and healthcare systems is now available (Guillaume et al. 2016). The European Deprivation Index is a weighted combination of aggregated variables from each national census that are most highly correlated with a country-specific individual deprivation indicator. The EDI is now available in France, Italy, Portugal, Spain, Slovenia and England (Guillaume et al. 2016; Ribeiro et al. 2017; Zadnik et al. 2018). When it is more widely used, this new index will help overcome the absence or incomplete collection of comparable socioeconomic data for each person in routine health databases, including cancer registries.
Conclusions
Further investigation of the patient and healthcare system factors that contribute to socioeconomic inequalities in survival is needed to help develop policies and other interventions that ensure equitable access to appropriate investigation and treatment.
The VENUSCANCER questionnaire has shown that population-based data on the socioeconomic status of patients with cancer are not yet available in many European countries, or in many other countries world-wide. More widespread and systematic collection of the data required to generate the European Deprivation Index in cancer registries in Europe would help to standardise the collection of socioeconomic information in countries where this kind of research is currently difficult or impossible.
The European Network of Cancer Registries could consider championing the idea that population-based cancer registries should systematically collect indicators of socioeconomic position for all registered patients.
Real-world, observational studies of cancer survival, using population-based data on stage at diagnosis, treatment, lifestyle and socioeconomic status, are essential if we are to quantify the extent to which differences in these factors explain the wide international variations in survival.
It is crucial for governments to recognise that population-based cancer registries are key policy instruments that can be used to evaluate both the impact of cancer prevention strategies and the effectiveness of the national health system in managing all patients who are diagnosed with cancer, regardless of their socioeconomic status.
References
Aarts MJ, Lemmens VE, Louwman MW, Kunst AE, Coebergh JW. Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer. 2010;46:2681–95. https://doi.org/10.1016/j.ejca.2010.04.026
Akerley WL, Moritz TE, Ryan LS, Henderson WG, Zacharski LR. Racial comparison of outcomes of male Department of Veterans Affairs patients with lung and colon cancer. Arch Intern Med. 1993;153:1681–8.
Alawadhi E, Al-Awadi A, Elbasmi A, Coleman MP, Allemani C. Cancer survival by stage at diagnosis in Kuwait: a population-based study. J Oncol. 2019;2019:1–9. https://doi.org/10.1155/2019/8463195
Allemani C. The importance of global surveillance of cancer survival for cancer control: the CONCORD programme. Cancer Control. 2017:19–22.
Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang X-S, Bannon F, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). The Lancet. 2015;385:977–1010. https://doi.org/10.1016/S0140-6736(14)62038-9
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, Bonaventure A, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37,513,025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. The Lancet. 2018;391:1023–75. https://doi.org/10.1016/S0140-6736(17)33326-3
All-Party Parliamentary Group on Breast Cancer. Tackling cancer inequalities – one year on. London: All Party Parliamentary Group on Cancer; 2010.
Bailey C, Richardson LC, Allemani C, Bonaventure A, Harewood R, Moore AR, Stewart SL, Weir HK, Coleman MP, CONCORD Working Group. Adult leukemia survival trends in the United States by subtype: a population-based registry study of 370,994 patients diagnosed during 1995-2009. Cancer. 2018;124:3856–67. https://doi.org/10.1002/cncr.31674
Bannon F, Di Carlo V, Harewood R, Engholm G, Ferretti S, Johnson CJ, Aitken JF, et al. Survival trends for primary liver cancer, 1995–2009: analysis of individual data for 578,740 patients from 187 population-based registries in 36 countries (CONCORD-2). Ann Cancer Epidemiol. 2019;3:6–31. https://doi.org/10.21037/ace.2019.07.01
Berrino F, Sant M, Verdecchia A, Capocaccia R, Hakulinen T, Estève J. In: Berrino F, Sant M, Verdecchia A, Capocaccia R, Hakulinen T, Estève J, editors. Survival of cancer patients in Europe: the EUROCARE study (IARC Scientific Publications No. 132). Lyon: International Agency for Research on Cancer; 1995.
Berrino F, Capocaccia R, Estève J, Gatta G, Hakulinen T, Micheli A, Sant M, Verdecchia A. In: Berrino F, Capocaccia R, Estève J, Gatta G, Hakulinen T, Micheli A, Sant M, Verdecchia A, editors. Survival of cancer patients in Europe: the EUROCARE-2 study (IARC Scientific Publications No. 151). Lyon: International Agency for Research on Cancer; 1999.
Berrino F, Capocaccia R, Coleman MP, Estève J, Gatta G, Hakulinen T, Micheli A, Sant M, Verdecchia A. Survival of cancer patients diagnosed in Europe: the EUROCARE-3 study. Ann Oncol. 2003;14(Suppl. 5):1–155.
Brawley OW. Lung cancer and race: equal treatment yields equal outcome among equal patients, but there is no equal treatment. J Clin Oncol. 2006;24(3):332–3. https://doi.org/10.1200/JCO.2005.03.7077
Capocaccia R, Gavin A, Hakulinen T, Lutz JM, Sant M. Survival of cancer patients diagnosed in Europe, 1995-2002: the EUROCARE-4 study. Eur J Cancer. 2009;45(Suppl. 6):901–1094.
Coleman MP. Cancer survival: global surveillance will stimulate health policy and improve equity. Lancet. 2014;383:564–73. https://doi.org/10.1016/S0140-6736(13)62225-4
Coleman MP, Babb P, Damiecki P, Grosclaude PC, Honjo S, Jones J, Knerer G, et al. Cancer survival trends in England and Wales 1971–1995: deprivation and NHS region (studies on medical and population subjects no. 61). London: The Stationery Office; 1999.
Coleman MP, Quaresma M, Berrino F, Lutz JM, De Angelis R, Capocaccia R, Baili P, et al. Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Oncol. 2008;9:730–56. https://doi.org/10.1016/S1470-2045(08)70179-7
Dalton SO, Frederiksen BL, Jacobsen E, Steding-Jessen M, Osterlind K, Schuz J, Osler M, Johansen C. Socioeconomic position, stage of lung cancer and time between referral and diagnosis in Denmark, 2001-2008. Br J Cancer. 2011;105:1042–8. https://doi.org/10.1038/bjc.2011.342
De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, Pierannunzio D, Trama A, et al. Cancer survival in Europe 1999–2007 by country and age: results of EUROCARE-5 – a population-based study. Lancet Oncol. 2014;15:23–34. https://doi.org/10.1016/S1470-2045(13)70546-1
Department of Health. The NHS cancer plan. Department of Health: London, UK; 2000.
Department of Health. (2007). Cancer reform strategy: equality impact assessment. https://webarchive.nationalarchives.gov.uk/20130104214031; http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsLegislation/DH_081005. Accessed 15 November 2020.
Department of Health. 2008. Tackling health inequalities: 2007 status report on the programme for action, ed. Department of Health. London: Department of Health.
Department of Health. Improving outcomes: a strategy for cancer. London: Department of Health; 2011.
Di Carlo V, Estève J, Johnson C, Girardi F, Weir HK, Wilson RJ, Minicozzi P, et al. Trends in short-term survival among 18,601 patients diagnosed during 2001-2013 with distant-stage cutaneous melanoma in the United States (CONCORD-3) [epub ahead of print]. JNCI Cancer Spectrum. 2020; https://doi.org/10.1093/jncics/pkaa078.
Ellis L, Coleman MP, Rachet B. How many deaths would be avoidable if socioeconomic inequalities in cancer survival in England were eliminated? A national population-based study, 1996-2006. Eur J Cancer. 2012;48:270–8.
Exarchakou A, Maringe C, Ellis E, Coleman MP. Health inequalities – a challenge to current health policy. Socio-economic inequalities in 5-year cancer survival: avoidable premature deaths among patients diagnosed in England in 2010. In: Davies SC, Pearson-Stuttard J, editors. Report of the Chief Medical Officer, 2018: Health 2040 – better health within reach. London: Department of Health and Social Care; 2018a.
Exarchakou A, Rachet B, Belot A, Maringe C, Coleman MP. Impact of national cancer policies on cancer survival trends and socioeconomic inequalities in England, 1996-2013: population-based study. BMJ. 2018b;360:k764. https://doi.org/10.1136/bmj.k764
Expert Advisory Group on Cancer. A policy framework for commissioning cancer services (Calman-Hine report). London: Department of Health; 1995.
Forrest LF, Adams J, Wareham H, Rubin G, White M. Socioeconomic inequalities in lung cancer treatment: systematic review and meta-analysis. PLoS Med. 2013;10:e1001376. https://doi.org/10.1371/journal.pmed.1001376.
Fowler H, Belot A, Njagi EN, Luque-Fernandez MA, Maringe C, Quaresma M, Kajiwara M, Rachet B. Persistent inequalities in 90-day colon cancer mortality: an English cohort study. Br J Cancer. 2017;117(9):1396–404. https://doi.org/10.1038/bjc.2017.295.
Guillaume E, Pornet C, Dejardin O, Launay L, Lillini R, Vercelli M, Mari-Dell’Olmo M, et al. Development of a cross-cultural deprivation index in five European countries. J Epidemiol Community Health. 2016;70:493–9. https://doi.org/10.1136/jech-2015-205729.
Lundqvist A, Andersson E, Ahlberg I, Nilbert M, Gerdtham U. Socioeconomic inequalities in breast cancer incidence and mortality in Europe-a systematic review and meta-analysis. Eur J Pub Health. 2016;26:804–13. https://doi.org/10.1093/eurpub/ckw070
Lyratzopoulos G, West CR, Williams EMI. Socioeconomic variation in colon cancer tumour factors associated with poorer prognosis. Br J Cancer. 2003;89:828–30.
Lyratzopoulos G, Neal RD, Barbiere JM, Rubin GP, Abel GA. Variation in number of general practitioner consultations before hospital referral for cancer: findings from the 2010 National Cancer Patient Experience Survey in England. Lancet Oncol. 2012;13:353–65.
Lyratzopoulos G, Abel GA, Brown CH, Rous BA, Vernon SA, Roland M, Greenberg DC. Socio-demographic inequalities in stage of cancer diagnosis: evidence from patients with female breast, lung, colon, rectal, prostate, renal, bladder, melanoma, ovarian and endometrial cancer. Ann Oncol. 2013;24:843–50. https://doi.org/10.1093/annonc/mds526
Lyratzopoulos G, Wardle J, Rubin G. Rethinking diagnostic delay in cancer: how difficult is the diagnosis? BMJ. 2014;349
Manser CN, Bauerfeind P. Impact of socioeconomic status on incidence, mortality, and survival of colorectal cancer patients: a systematic review. Gastrointest Endosc. 2014;80(42–60):e49. https://doi.org/10.1016/j.gie.2014.03.011
National Cancer Intelligence Network. Evidence to March 2010 on cancer inequalities in England. London: National Cancer Action Team; 2010.
Nur U, Rachet B, Parmar MKB, Sydes M, Cooper N, Lepage C, Northover JMA, James R, Coleman MP, Collaborators A. No socioeconomic inequalities in colorectal cancer survival within a randomised clinical trial. Br J Cancer. 2008;99:1923–8.
Nur U, Rachet B, Parmar MK, Sydes MR, Cooper N, Stenning S, Read G, Oliver T, Mason M, Coleman MP. Socio-economic inequalities in testicular cancer survival within two clinical studies. Cancer Epidemiol. 2012;36:217–21.
OECD/European Union. Health at a glance: Europe 2020: State of Health in the EU Cycle, OECD Publishing, Paris: OECD/EU. 2020. https://doi.org/10.1787/82129230-en
Organisation for Economic Co-operation and Development. Health at a glance 2019: OECD indicators. In Health at a Glance. 2019. Paris: OECD Publishing.
Praestegaard C, Kjaer SK, Nielsen TS, Jensen SM, Webb PM, Nagle CM, Hogdall E, et al. The association between socioeconomic status and tumour stage at diagnosis of ovarian cancer: a pooled analysis of 18 case-control studies. Cancer Epidemiol. 2016;41:71–9. https://doi.org/10.1016/j.canep.2016.01.012
Quaresma M, Coleman MP, Rachet B. Funnel plots for population-based cancer survival: principles, methods and applications. Stat Med. 2014;33:1070–80. https://doi.org/10.1002/sim.5953
Rachet B, Ellis L, Maringe C, Nur U, Chu T, Quaresma M, Shah A, et al. Socioeconomic inequalities in cancer survival in England after the NHS cancer plan. Br J Cancer. 2010;103:446–53.
Ribeiro AI, Mayer A, Miranda A, Pina MF. The Portuguese version of the European deprivation index: an instrument to study health inequalities. Acta Medica Portuguesa. 2017;30:17–25. https://doi.org/10.20344/amp.7387
Rutherford MJ, Ironmonger L, Ormiston-Smith N, Abel GA, Greenberg DC, Lyratzopoulos G, Lambert PC. Estimating the potential survival gains by eliminating socioeconomic and sex inequalities in stage at diagnosis of melanoma. Br J Cancer. 2015;112(Suppl 1):116–23. https://doi.org/10.1038/bjc.2015.50
Silman AJ, Evans SJ. Regional differences in survival from cancer. Community Med. 1981;3:291–7.
Sobin LH, Gospodarowicz M, Wittekind C. TNM classification of malignant tumours. New York: Wiley; 2009.
VENUSCANCER project, 2017, funded by the European Research Council. https://cordis.europa.eu/project/id/772345.
Verhoeven D, Allemani C, Kaufman C, Mansel R, Siesling S, Anderson B. Breast cancer: global quality care optimizing care delivery with existing financial and personnel resources. ESMO Open. 2020;4(Suppl 2):e000861. https://doi.org/10.1136/esmoopen-2020-000861
Weir HK, Stewart S, Allemani C, White M, Thomas C, White A, Coleman MP. Population-based cancer survival (2001–2009) in the United States: findings from the CONCORD-2 study. Cancer. 2017;123:4963–8. https://doi.org/10.1002/cncr.31028
Woods LM, Rachet B, O'Connell D, Lawrence G, Coleman MP. Impact of deprivation on breast cancer survival among women eligible for mammographic screening in the West Midlands (UK) and New South Wales (Australia): women diagnosed 1997–2006. Int J Cancer. 2016;138:2396–403. https://doi.org/10.1002/ijc.29983
Zadnik V, Guillaume E, Lokar K, Žagar T, Primic Žakelj M, Launoy G, Launay L. Slovenian version of the European deprivation index at municipal level Slovenian. J Public Health. 2018;57:47–54. https://doi.org/10.2478/sjph-2018-0007
Acknowledgements
The authors would like to thank all staff members of the cancer registries participating in the CONCORD programme. Without their assiduous work, population-based research would not be possible.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Allemani, C., Coleman, M.P., Zadnik, V., Launoy, G., Minicozzi, P. (2021). Disparities in Cancer Survival in Adults in Europe: The CONCORD Programme. In: Launoy, G., Zadnik, V., Coleman, M.P. (eds) Social Environment and Cancer in Europe. Springer, Cham. https://doi.org/10.1007/978-3-030-69329-9_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-69329-9_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-69328-2
Online ISBN: 978-3-030-69329-9
eBook Packages: MedicineMedicine (R0)