Abstract
This chapter’s primary focus is on system characteristics within the Quality Health Outcomes Model (QHOM), particularly workflow and turbulence. The idea of workflow originated in the manufacturing industry as managers sought to improve efficiency by removing bottlenecks to smooth out processes. Flow is reflected in smooth, continuous movement. Workflow in healthcare, however, is rarely smooth. Instead, it is turbulent, like the irregular motion characterized by the up- and downwind currents experienced in an airplane. For nurses, the idea of workflow is an oxymoron because the “flow” of work is irregular, not smooth. Instead, nurses’ work is typified by turbulence. Sources of turbulence for nurses include interruptions, handoffs, and patient turnover. Also, the use of workarounds may be a sign of turbulence. The system characteristics of poor flow and high turbulence tend to increase the cognitive complexity of nurses’ work. Cognitive complexity derives mainly from the invisible work of nursing. Cognitive workload, or mental effort, and cognitive stacking, or juggling numerous shifting priorities within a turbulent setting, escalate the cognitive complexity of nurses’ work. Together, poor workflow, high turbulence, and high cognitive complexity can contribute to work stress and cognitive failure, thereby adversely affecting patient safety and quality care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The concept of workflow is problematic when applied to nurses and clinical practice. Flow suggests smoothness and continuity. Rather than smooth, nurses’ work is inherently turbulent; the flow is nonlinear (Phillips 2018), disorderly, unstable (Gleick 1987), and “irregular” (Cornell et al. 2011, p. 410). Turbulence is evident as nurses move among patients throughout the shift as well as to and from centralized work areas such as the nurses’ station and medication rooms (Cornell et al. 2010; Jennings et al. 2011; Potter et al. 2004; Tucker and Spear 2006). Turbulence is the unifying characteristic in the patterns of work complexity identified by Ebright and colleagues (Ebright et al. 2003). The importance of scrutinizing turbulence was affirmed by Browne and Braden (2020), who noted, “managing turbulence rather than patient needs is becoming a priority for nurses” (p. 184). Turbulence is perpetuated by the highly unpredictable nature of nurses’ work. For example, nurses know that patient admissions will occur, but it is difficult to anticipate when they will happen (Jennings et al. 2013). Although medication administration seems orderly and predictable, it is filled with turbulence (Jennings et al. 2011), thereby altering workflow. As the workflow turbulence increases, the cognitive work of nursing becomes increasingly complex. The focus of this chapter, therefore, relates to workflow, turbulence, and cognitive complexity.
Workflow, Turbulence, and Cognitive Complexity: Specific Linkages with the QHOM
The primary construct from the QHOM (Mitchell et al. 1998) showcased in this chapter is the system (organization and microsystem). Workflow and turbulence are major concepts within the system construct. Features of turbulence with the most robust evidence for illustrating its effect on nurses’ work include interruptions, handoffs, and patient turnover. By reframing the client construct within the QHOM as the nurse, the way is opened to address the cognitive (mental) workload and resulting cognitive complexity that often stem from a turbulent workflow. To date, interventions to improve nurses’ work (e.g., smoothing workflow and mitigating turbulence) remain few. Those interventions that have been tried (i.e., not interrupting medication administration) have not had an enduring effect in making the system better and reducing nurses’ cognitive complexity.
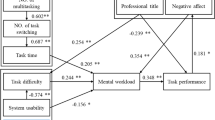
Consequently, the focus in this chapter is on describing the characteristics within the system (turbulence and workflow) and the client (nurses’ cognitive workload and complexity) that affect nurse outcomes (work stress and cognitive failures) (Fig. 5.1). Interventions will receive only brief mention. Nursing has been known as a high-stress profession since the 1960s (Menzies 1960). The role of turbulence as a potential contributor to work stress is a new slant on nurses’ work conditions. Therefore, the chapter aims to depict the nature of nurses’ work in the twenty-first century by exploring workflow, turbulence, cognitive workload, and cognitive complexity in acute care settings.
System Characteristics
Workflow
The workflow concept originated in the early 1900s as factory managers sought to remove bottlenecks and improve efficiency in manufacturing plants (Derksen 2014). According to the dictionary, workflow is a “sequence of steps involved in moving from the beginning to the end of a work process” (https://www.meeriam-webster.com/dictionary/workflow). Cain and Hague (2008) proposed that workflow includes a set of tasks grouped chronologically into a process and the people and resources needed to complete the tasks. Thus, workflow suggests a pattern that is repeatable such as the work done on an assembly line. Some quality improvement initiatives are designed to enhance workflow. For instance, “lean” is a set of principles adapted from The Toyota Production System that focus on ways to eliminate waste, especially wasted time (i.e., waiting), by standardizing practices (Lawal et al. 2014). Despite the usefulness of importing principles from other industries (e.g., airlines, manufacturing), healthcare is less predictable than machines where parts and interconnections work linearly. Instead, healthcare is a human system with people as the parts, not bolts and screws. Variation is thus inherent in healthcare because of the human element.
Workflow in Healthcare
As a human system, healthcare is considered a complex adaptive system (CAS) where unpredictability, nonlinearity, and surprises prevail (McDaniel et al. 2003; Plsek 2001). In CASs, the unexpected is normative (Plsek 2001). Features of CASs are chaos (Plsek 2001), disorder, instability (Gleick 1987), and nonlinear flow, yielding similarities to turbulence (Phillips 2018). Although commonly used, turbulence is an unsolved problem in physics with tremendous practical importance; the most important flows are turbulent (Phillips 2018). Therefore, it is conceivable that turbulence reflects workflow in healthcare systems.
The lack of smooth workflow in healthcare often stems from poorly designed systems. System problems that impede workflow or facilitate turbulence were termed “operational failures” by Tucker (2004) and “performance obstacles” by Gurses et al. (2009). Such problems illustrate why Carayon and colleagues stated, “The entire [healthcare] work system needs to be well designed for optimal performance” (Carayon et al. 2007, p. i54), emphasizing that patient safety is about the system. Similarly, Karsh and colleagues advocated for system redesign to improve performance and reduce hazards, highlighting that systems need to support the healthcare professionals who are delivering care (Karsh et al. 2006). The need to support staff who work in healthcare systems is at the heart of a recent report from the National Academy of Medicine that focuses on clinician burnout and professional well-being (National Academies of Sciences, Engineering, and Medicine 2019).
Nevertheless, turbulent workflow prevails in healthcare settings. Altered workflow has been linked to surgical errors (Wiegmann et al. 2007). Moreover, even when systems are redesigned and the desired goals achieved, there may also be unintended, undesirable consequences. Such unintended consequences are illustrated by investigators who assessed hospital redesign focused on enhancing patient-centeredness (Mikesell and Bromley 2012). Along with making the hospital more patient centered, the changes also created many inconveniences for the staff, especially nurses: Walking and telephone interruptions increased; time at the bedside and face-to-face exchanges with both patients and coworkers decreased (Mikesell and Bromley 2012).
Regardless of system redesign, the idea of workflow for nurses is an oxymoron. “There is little ‘flow’ in nurse workflow” (Cornell et al. 2010, p. 366); “nurse workflow actually lacks flow” (Myny et al. 2012, p. 432). Instead, nurses’ work is characterized by work complexity patterns (Ebright et al. 2003) and as noted earlier, the unifying characteristic in these patterns is turbulence. To understand nurses’ work it, therefore, becomes vital to understand turbulence.
Turbulence
Turbulence is a term commonly used in meteorology, oceanography, mathematics, physics, and engineering. In these fields, turbulence characterizes irregularities in flow, such as the up and down currents that may be experienced in an airplane or the choppy seas sometimes experienced on a ship or sailboat. Organizations face turbulence too when changes occur that are “nontrivial, rapid, and discontinuous” (Cameron and Kim 1987, p. 225). Turbulence is further evident when change exceeds an organization’s ability to adapt (McCann and Selsky 1984).
Turbulence in Healthcare
More than 35 years ago, Strauss and colleagues noted that hospital work was intrinsically complex and unpredictable (Strauss et al. 1997). Before the 1980s, acute care hospitals were regarded as placid settings, whereas in the 1980s, these same settings were considered turbulent (Beekun and Ginn 1993). The turbulence in the external healthcare environment (e.g., health policies, financing, and regulations) contributed to turbulence in the internal healthcare environment, those conditions within healthcare settings—both at the organizational and unit level (microsystem).
Turbulence in the External Environment
Acute care hospitals were confronted with turbulence in the 1980s when massive external changes were implemented to deal with the skyrocketing cost of healthcare (Bazzoli et al. 2004). The turbulence was primarily due to alterations in healthcare financing and restructuring. The financing changes (i.e., prospective vs. retrospective payment) imposed a business model onto the health systems; the restructuring efforts shifted patients from inpatient to outpatient settings (e.g., ambulatory surgery; Jennings 2008a).
The effects of hospital restructuring exerted a profound influence on the registered nurse’s (RN) work role (e.g., less time for direct patient care), workload (a complex combination of higher patient acuity, scheduling, and fluctuating census), and control over work (bureaucratic hierarchy vs. professional, collegial control; Norrish and Rundall 2001). Turbulence has persisted: ongoing, “nontrivial, rapid” (Cameron and Kim 1987, p. 225) changes remain normative in twenty-first-century healthcare. In 2020, major upheaval was experienced in the external environment when the COVID-19 outbreak was deemed a pandemic by the World Health Organization (WHO 2020). The coronavirus pandemic exemplifies how external turbulence may yield turbulence within the internal healthcare environment. Although some external forms of turbulence may be inevitable, others can be reduced, potentially reducing their internal environment effects.
Turbulence in the Internal Environment
Although organizational turbulence is important, the focus here is on the unit level (microsystem) “where the work happens; it is where the ‘quality’ experienced by the patient is made or lost” (Berwick 2002, p. 84). Work at the unit level in acute care settings is described as occurring in a hyperdynamic, turbulent environment where nurses’ workflow is “irregular” (Cornell et al. 2011, p. 410).
Tucker and Spear (2006) referred to the “staccato pace” (p. 650) of nurses’ work, suggesting that workflow is choppy, not smooth: nurses switched among patients about every 11 min. They switched among locations about 13 times/hour (Tucker and Spear 2006). Choppy workflow suggests turbulence. In a decade-old characterization of turbulence in the acute care environment, Jennings (2008b) suggested that communication and workload were the major components comprising turbulence. Communication included interruptions, handoffs (where information might be lost), and noise. Workload included large patient assignments, patient turnover (admissions, discharges, transfers), and equipment/supply issues. In a later study, Cornell et al. (2011) connected turbulence to cognition by raising questions about how turbulence features affect critical thinking and the cognitive workload nurses must manage. In Jennings’ characterization of turbulence, cognitive workload per se was not addressed (Jennings 2008b). Rather, ideas related to cognitive workload (i.e., decision-making, cognitive stacking, simultaneous demands, unfamiliar work, time pressure) were parsed into the communication and workload components, illustrating the interplay among these workplace characteristics.
Sources of Turbulence in Nurses’ Work
Although little research has been done for the explicit purpose of examining turbulence in acute care settings, there is evidence that turbulence disrupts patient safety and quality care. In the 1990s, Salyer (1995) conducted the first known exploration of turbulence in acute care. Nurses on units with more turbulence—defined as higher patient turnover and fluctuating patient acuity—had poorer communication and interpersonal relationships (Salyer 1995). Poor communication is a factor in sentinel events (Comprehensive Accreditation Manual for Hospitals 2013) and preventable adverse events (Gosbee 1998). Poor interpersonal relationships impair teamwork (Chap. 10); together, good communication and teamwork can advance system safety (IHI Multimedia Team 2017). In this way, turbulence may diminish the quality of care.
In 2007, Bosco (2007) completed a secondary analysis using data from the Impact of Unit Characteristics on Patient Outcomes (IMPACT) study where turbulence serendipitously emerged as a latent variable (Verran et al. 2003). The investigators represented turbulence as a composite variable comprised of five constructs: (a) the number of patients per day on a unit, (b) accessibility of needed resources, (c) distance required to access resources, (d) responsiveness of support services, and (e) perceived environmental uncertainty. Bosco (2007) found that turbulence directly affected medication errors and patients’ perception of being well cared for, further suggesting a link between turbulence, quality care, patient safety, and patient outcomes.
Jennings et al. (2011, 2013) sought to understand better how turbulence affected patients and staff by conducting an ethnographic study on inpatient medical and surgical units. Medication administration (Jennings et al. 2011) and patient turnover (Jennings et al. 2013) were related to, and at times the source of, turbulence; both were also strongly tied to patient safety and quality care.
Most recently, Browne and Braden (2020) initiated a study to develop a preliminary measure of nursing turbulence in critical care. Their work was prompted by a belief that workload, which does not have a standard definition, was inadequate to encompass all nursing activities. Although there are questions about how turbulence was operationalized, the initial findings illustrated that turbulence and workload are separate concepts, thereby contradicting the conceptual assertion that turbulence is a characteristic of nurses’ workload (Swiger et al. 2016). Refinement of the relationship between turbulence and workload warrants further exploration as the turbulent healthcare environment (i.e., lack of smooth workflow) appears to elevate nurses’ cognitive workload (Cornell et al. 2011; Myny et al. 2012). Greater cognitive workload contributes to the cognitive complexity of nurses’ work. Primary sources of turbulence for which the evidence is most robust include interruptions, handoffs, and patient turnover. Also, nurses may use workarounds to overcome system impediments created by turbulence to get the work done.
Interruptions
Interruptions are characteristic of nurses’ work (Jennings et al. 2011) and a significant source of turbulent workflow. More than 20 years ago, it was noted that “being ‘interrupted’ is an unremarkable and normative experience of nursing practice and one that is taken for granted” (Waterworth et al. 1999, p. 165). More recent explorations illuminating the inseparability of the tasks comprising nurses’ work underscore that nursing remains inherently and highly interruptive (Hopkinson and Weigand 2017; Jennings et al. 2011).
Most interruptions (similar although not synonymous terms are distractions and disruptions) are communication and relationship driven (Reed et al. 2018). They are a product of healthcare workers’ preference to communicate synchronously, face to face or via the telephone (Coiera and Tombs 1998; Edwards et al. 2009; Fairbanks et al. 2007; Parker and Coiera 2000). They also are a product of verbal interactions with patients (Rivera-Rodriguez and Karsh 2010; Weigl et al. 2017) and patients’ families (Rivera-Rodriguez and Karsh 2010).
Technology represents a communication modality that serves as a significant source of interruptions (Chap. 6). Some technologies facilitate human communication (e.g., mobile work phones, patient intercoms). Other technologies communicate with nurses by alarming (e.g., physiological monitors, bar code medication administration [BCMA], intravenous infusion pumps; Powell-Cope et al. 2008; Zuzelo et al. 2008). These technologies exert “a profound impact on workflow” (Aarts et al. 2007, p. S4). When alarms are continually sounding, nurses may experience sensory and cognitive overload, referred to as alarm or alert fatigue (Sendelbach and Funk 2013), which may increase cognitive workload (Woods and Patterson 2001).
Although concerns with patient safety have yielded an emphasis on the potentially harmful effects of interruptions, it is essential to remember that there are benefits as well (Grundgeiger and Sanderson 2009; Hopkinson and Jennings 2013; Li et al. 2012; Rivera-Rodriguez and Karsh 2010). For instance, interruptions may direct attention to avoiding a medication error or creating a pause that might otherwise have yielded an error. Thus, reducing or stopping interruptions is unrealistic and perhaps even unwise. For the most part, however, interruptions are viewed as undesirable.
The Anatomy of an Interruption
Interruptions are highly complicated phenomena due, in part, to the many components comprising an interruption. Components include the complexity of the primary task, the duration of the interruption (longer interruptions have a bigger impact), the type of interruption, when the interruption occurs in the task sequence (interruptions that occur at the beginning of a task are the least disruptive; Couffe and Michael 2017; Magrabi et al. 2011), and whether memory prompts are used to facilitate recovery after an interruption (Coiera 2012). Additional considerations surrounding interruptions include the complexity of both the primary and interrupting tasks, the similarity of the primary and interrupting tasks, and the interruption’s modality (e.g., face to face or a device alarm; Magrabi et al. 2011).
Regardless of the components comprising an interruption, all interruptions share three attributes: (a) intrusion of a secondary, unplanned, unscheduled task; (b) a break in continuity when the primary task currently in progress is suspended unexpectedly before its completion; and (c) the resumption of the primary task after the interruption (Brixey et al. 2007). An often overlooked feature of interruptions is that they occur internally; people can choose to acknowledge or ignore an interruption regardless of the interruption source (e.g., people, telephones, alarms; Brixey et al. 2007; Jett and George 2003; Rivera-Rodriguez and Karsh 2010). Such choices often come easier for more experienced nurses (Patterson et al. 2011).
An important feature of interruptions involves the temporal context of nurses’ work. When time is fixed, such as with shift lengths, interruptions compete for time, potentially contributing to a sense of feeling hurried and fostering the use of workarounds (Brown 2019; Coiera 2012). Over 20 years ago, Perlow (1999) referred to time pressure at work, the sense of having too much to do and not enough time to do it, as “time famine” (p. 57). More recently, Krichbaum et al. (2011) addressed how unexpected occurrences during a nurse’s shift create a sense of time scarcity.
Nevertheless, managing time in the context of an interruption-filled environment is accomplished by task-switching and multitasking, both of which affect cognition. Task-switching involves shifting from one task to another (Rubinstein et al. 2001; Walter et al. 2014). For instance, a nurse might stop medication administration to answer a question from a family member. By contrast, multitasking involves doing more than one task at a time (Mark 2015; Morgan et al. 2013; Walter et al. 2014). For instance, a nurse might continue with medication administration while answering a mobile work telephone call.
Multitasking is more common than task-switching. Findings from a US study showed that nurses on inpatient units used multitasking 34% of the time (Kalisch and Aebersold 2010). Findings from an Australian study showed that of 28,809 tasks observed among nurses on inpatient units, 800 involved task-switching and 4482 involved multitasking (Walter et al. 2014). This amount of multitasking equates to dealing with 14.1 multitasking events/hour (Walter et al. 2014), close to twice the number of task-switching events. Multitasking has many additional considerations. These include whether the multitasking is voluntary (internally motivated; the individual chooses) or forced (externally prompted) and the task modalities involved (e.g., button pressing, visual, auditory; Douglas et al. 2017). Issues surrounding task-switching and multitasking further reveal the turbulent nature of nurses’ workflow.
Interruptions, including task-switching and multitasking, may create a perception of higher workload (Grundgeiger and Sanderson 2009; Myny et al. 2012), including higher cognitive workload (Rivera-Rodriguez and Karsh 2010). The causal chain, however, remains unclear. For instance, is it that more interruptions leave workers with perceptions of higher workloads, or is it that higher workloads yield more chances for being interrupted (Coiera 2012; Weigl et al. 2012)?
Handoffs
Numerous terms are used for care transition events (e.g., handoff, handover; Cohen and Hilligoss 2010). From their critical literature review, Cohen and Hilligoss (2010) proposed handoff as the prevailing term defining it as “the exchange between health professionals of information about a patient accompanying either a transfer of control over, or of responsibility for that patient” (p. 494). The care transition itself alters workflow and, if ineffective, these communication events create patient safety risks (Dracup and Morris 2008; Gandhi 2005; Kohn et al. 2001; Ong and Coiera 2011; Wachter and Shojania 2005). The information exchange inherent to handoffs raised concerns with The Joint Commission in 2006 (Friesen et al. 2008). Because of the potential safety risks associated with inadequate communication during handoffs and the complexity involved in handoff communication, patient handoffs were earmarked as a potential sentinel event (The Joint Commission 2017).
Adequate communication, however, is complex and involves more than passing along information. The information must be correct, complete, and understood by the receiver (Hilligoss and Cohen 2011). Thus, a handoff is not a one-way communication event but rather a conversation in which there is “active co-construction of an understanding of the patient” (Cohen et al. 2012, p. 4). Also affecting communication is whether the exchange occurs between individuals from the same profession or between individuals with different professional backgrounds (Chap. 10). Nurses, for instance, tend to focus on the “big picture” using “broad and narrative” descriptions (Leonard et al. 2004, p. i86); physicians tend to focus on bullet points of critical information (Leonard et al. 2004). This chapter focuses on handoffs between nurses, both within-unit handoffs, typically referred to as shift reports, and between-unit handoffs, or intrahospital transfers.
Shift report is a frequently studied, routinely occurring within-unit handoff where nurses ending their shift handoff responsibilities and patient information to nurses starting their shift. Report at shift change creates an anticipatable pause in the usual workflow. The flow of report information, however, is altered by interruptions during the reporting process and high noise levels, such as when a report occurs in a central place like the nurses’ station (Staggers and Jennings 2009). Turbulent workflow is also typical during shift reports because oncoming nurses rarely receive reports from a single nurse due to how patient assignments are made. The flow of shift reports becomes choppy or turbulent as nurses go “through a process of ‘finding’ each other” to give and receive a report (Staggers and Jennings 2009, p. 395). Shift length (e.g., 12 h, 8 h) also adds to the turbulent workflow of shift report. In one of the few investigations in which varied shift schedules were addressed (i.e., a mixture of 8- and 12-h shifts), the schedules were viewed as “disjointed and confused” (Kalisch et al. 2008, p. 134) and an impediment to handoffs.
Templates for standardizing handoffs pertain primarily to shift report handoffs. Yet, these must be viewed with caution because of differing informational needs and expectations among nurses giving reports, nurses receiving the report, and the nurse’s level of experience (Carroll et al. 2012; Welsh et al. 2010). Standardized communication protocols are exemplified by the well-known SBAR (Situation, Background, Assessment, Recommendation; Cornell et al. 2013) and the more recently developed I-PASS (Illness severity, Patient summary, Action list, Situation awareness and contingency plans, and Synthesis by the receiver; Starmer et al. 2014, 2017). Although various regulatory agencies recommend standardizing handoffs, the need for a two-way conversation and co-construction with the patient argues against rigid standardization (Hilligoss and Cohen 2011).
Handoffs related to intrahospital transfers involve nurses from different units; a nurse from the sending unit reports to a nurse on the receiving unit. Between-unit handoffs vary based on where the patient is coming from and going to (e.g., from intensive care to acute care; Ong and Coiera 2011). Between-unit handoffs are highly unpredictable because, unlike shift reports, they do not occur at a designated time (Hilligoss and Cohen 2013). Between-unit transfers and their associated handoffs, therefore, create disruptions in care and workflow (Blay et al. 2017; Jennings et al. 2013). Although between-unit handoffs have more layers of complexity than shift report handoffs, between-unit handoffs have received less attention in the literature.
Communication is especially prone to compromise during between-unit handoffs because patients are moving across unit (Hilligoss and Cohen 2013) and departmental (Ong and Coiera 2011) boundaries, “from one entire clinical microsystem to another” (Beach et al. 2017, p. 1190). Staff from different clinical microsystems do not know each other very well, or at all. The staff from each unit is unaware of what is occurring on the other unit. Also, the nurses involved in the handoff are not co-located, often communicating via telephone, and unable to observe body language.
Regardless of whether nurses are on the sending or receiving units (Ong and Coiera 2011), the turbulent workflow exhibits common properties that alter nurses’ work. For instance, delays occur when a nurse on the receiving unit is not available to take the sending unit report. Delays may prolong a patient’s stay on the sending unit, disrupting the workflow on that unit, as well as possibly hurrying through the handoff when it finally occurs, potentially yielding a less complete and accurate report (Abraham and Reddy 2010). Microsystem culture also comes into play. Emergency department (ED) nurses, for example, strive to move patients quickly to be ready for the arrival of more acute patients (Rosenberg et al. 2018). Also, the rapid movement of patients from the ED to inpatient beds is regarded as a quality indicator (www.ihi.org/resources/Pages/Measures/TimefromEDtoInpatientBEdmedian.aspx). Thus, the goals of the ED microsystem may contribute to turbulence on the admitting unit.
The layers of complexity associated with between-unit transfers also involve whether an intermediary is a part of the information exchange. Charge nurses or clinical leaders, for example, may give or take a report, passing the information from or to the bedside nurse (Whittaker and Ball 2000). In these instances, important information often is lost, yielding inadequate handoffs (Lin et al. 2013).
Patient Turnover
Patient arrivals and departures also create disruptions and contribute to turbulent workflow (Blay et al. 2017, 2014). However, patient turnover—admissions, discharges, and transfers—is a major component of nurses’ work. When patient turnover is high, workload increases (Myny et al. 2012; Park et al. 2016), and nursing care may become fragmented (Lin et al. 2013).
Much of the interest in patient turnover relates to staffing (Chap. 4). Although the midnight census is commonly used to reflect staffing needs, in a review article, Park et al. (2016) concluded that the midnight census was inadequate because it could lead to understaffing. There also is not a standard way to measure patient turnover rates. Moreover, turnovers vary by day of the week, time of day, and unit type (Park et al. 2016). For instance, Jennings and colleagues found that patient turnover rates were 1.6 times higher on a surgical unit than a medical unit (Jennings et al. 2013). In practical terms, there were times when surgical nurses cared for twice as many patients as suggested by the number of patients at the beginning and end of their shifts because their entire set of patients had turned over—all five or six patients were discharged, and five or six new patients were admitted (Jennings et al. 2013). These findings illustrate that different nursing specialties may be exposed to different turbulence sources from patient turnover. For instance, despite the high turnover in the surgical unit, they could better predict when most patients would arrive based on the operating room schedule. On the medical unit, by contrast, the number of ED and direct admissions was “predictably unpredictable” (Jennings et al. 2013, p. 558).
Misconceptions and nuances involving patient turnover include that the events are not equivalent: they vary by type, whether they can be anticipated, the intensity of the work involved, and the turnover event’s timing (Jennings et al. 2013). Evaluating turnover type showed that admissions were more turbulent than discharges. There were subtypes within admissions that varied based on how the patient entered an inpatient unit—direct admissions, ED, postanesthesia care, or a transfer from another floor. Direct admissions created the greatest turbulence; they were likened to “a code” because of workflow disruption. Anticipating patient turnover was possible with discharges; they were known in advance, offering nurses some ability to plan their shift. The turnover event’s intensity was related to what tasks were done before the patient reached the unit and how many were left for the admitting nurse to complete. The timing of turnover events made a difference in the degree of the turbulent workflow. Turnovers that occurred proximate to shift report created tremendous turbulence—these events were usually admissions with patients moving from one microsystem to another (e.g., ED to acute care). Admissions that were clustered in quick succession, rather than staggered, also were more disruptive. Moreover, regardless of when it occurred, each turnover event was associated with a handoff, creating the potential for a communication failure.
Workarounds as a Sign of Turbulence
Articulation work refers to organizing tasks and workers’ efforts “in the service of workflow” to overcome bottlenecks (Strauss 1988, p. 164). Articulation work is used to manage time (Star 1991; Star and Strauss 1999; Strauss 1985, 1988). As time contracts (i.e., more to do in a finite period), the importance of articulation work expands (Hampson and Junor 2005). In more recent years, the idea of workarounds has replaced the concept of articulation work as a way to consider system impediments that obstruct workflow (Koopman and Hoffman 2003). Workarounds are ways to “circumvent or temporarily ‘fix’ an evident or perceived workflow block” (Debono et al. 2013, p. 4). Thus, workarounds are a form of articulation work (Jennings et al. 2011).
Workarounds, however, tend to be viewed more negatively than positively (Debono et al. 2013). The negative view of workarounds is illustrated in a comment about bar code medication administration (BCMA), where deviations from prescribed protocols were referred to as “violations or workarounds” (Koppel et al. 2008, p. 409). In an extensive analysis of BCMA, however, these same authors concluded that shortcomings of the technology and workflow disruptions “encourage workarounds” (Koppel et al. 2008, p. 408). In general, automated technologies contribute to workarounds (Koopman and Hoffman 2003) and workarounds accompany the introduction of technology into healthcare (Ash et al. 2004; Novak and Lorenzi 2008; Patterson et al. 2002; Pingenot et al. 2009).
At the crux of workarounds is the need for nurses to save time, avoid waiting, and overcome system inefficiencies to care for patients (Brown 2019). Thus, workarounds are not about bad actors, but clumsy system designs and turbulent workflow. Workarounds are best viewed as a sign of turbulence in the environment. “Understanding nurses’ practice and their perception of workaround behaviours is at the heart of … improve[ing] healthcare at the bedside, where care is delivered” (Debono et al. 2013, p. 14).
Client Characteristics
Cognitive Complexity
Whereas workflow and turbulence are system characteristics, cognitive issues relate to the mental demands required of nurses to manage the turbulent workflow (Baethge and Rigotti 2013; Cornell et al. 2011; Grundgeiger and Sanderson 2009; Laxmisan et al. 2007; Myny et al. 2012; Patterson et al. 2011; Rivera-Rodriguez and Karsh 2010; Woods and Patterson 2001). More than the tasks per se, turbulence heightens the cognitive workload that contributes to the cognitive complexity of nurses’ work. Nurses “weave together the many facets of the [healthcare] service and create order in a fast flowing and turbulent work environment” (Allen 2004, p. 279). As such, the “nature of nursing practice … involves covert cognitive behaviors as well as overt physical activities …” (Potter et al. 2004, p. 102). The covert behaviors equate to nurses’ invisible work (Star and Strauss 1999). Invisible cognitive behaviors like “… attention switching … decisions … play the most critical role” in errors (Zhang et al. 2004, p. 194).
The literature addressing cognition is voluminous. This section is limited to considering the role of turbulence and altered workflow in creating cognitive complexity. The invisible work of nursing—cognitive workload (mental effort) and cognitive stacking—are cognitive challenges that illustrate the cognitive complexity of nurses’ work.
Visible and Invisible Work
Nursing is often depicted as a set of visible tasks, many of which are portrayed as straightforward and routine, although few are. The visible tasks overshadow much of nurses’ work, the work that is “hidden” (Star 1991, p. 270), reflecting a “tension between formal task descriptions and overt … ‘behind the scenes’ work” (Star and Strauss 1999, p. 9). Nurses from neonatal, pediatric, and adult intensive care units included invisible work, such as mental and temporal demands, as part of their subjective workload (Tubbs-Cooley et al. 2018). In a synthesis of 54 publications, Allen (2004) identified nurses’ overarching role as an intermediary. This role was less visible than the tasks nurses accomplished in caring for individual patients. Intermediary functions included managing the multiple agendas within healthcare systems, managing interprofessional relationships, and serving as “information broker[s]” (Allen 2004, p. 276).
Also, the simplistic view of nurses’ work as tasks disguises the cognitive complexity often involved in completing each task. Medication administration exemplifies this complexity; more is involved than following the five rights (right patient, drug, dose, route, time; Grissinger 2010). Moreover, medication work is not a discrete task with identifiable beginnings and endings (Jennings et al. 2011). Instead, medication administration is inseparable from other nursing work because care activities are woven together as nurses strive to manage time well (Jennings et al. 2011), thus increasing the cognitive complexity. Medication administration has mistakenly been referred to as a procedural task executed automatically (Li et al. 2012). The idea of automatic execution is refuted by findings from several studies in which nurses’ thought processes and clinical reasoning during medication administration were identified (Dickson and Flynn 2012; Eisenhauer et al. 2007; Jennings et al. 2011; Pingenot et al. 2009). Nurses must also manage interruptions during medication administration (Biron et al. 2009; Dickson and Flynn 2012; Jennings et al. 2011), including those arising from technology and physical space limitations (Jennings et al. 2011). Strategies to “administer as many medications ‘on time’ as possible” (Jennings et al. 2011, p. 1448) further illustrate that medication administration exemplifies the invisible, highly complex cognitive work that is embedded in a visible task.
Cognitive Workload
Cognition and cognitive abilities are features of cognitive workload. Cognition involves intellectual activities like thinking, reasoning, or remembering (https://www.merriam-webster.com/dictionary/cognitive) and thus relates to information processing. Cognitive abilities involve three interdependent concepts: (a) attention or deciding which stimuli to process and act upon (e.g., working memory; Couffe and Michael 2017; Parker and Coiera 2000); (b) storing information for later retrieval (Grundgeiger and Sanderson 2009; Li et al. 2012; Rivera-Rodriguez and Karsh 2010); and (c) executive processes or goal-directed behavior (e.g., planning, reasoning, problem-solving; Patterson et al. 2011; Sitterding and Ebright 2015).
Cognitive workload refers to short-term or working memory (i.e., attention), where information is actively processed (Parker and Coiera 2000). The limits of working memory were noted in Miller’s (1956) classic paper, where he suggested that we can remember seven digits—plus or minus two. Along with its limited capacity, working memory is limited in duration, with accuracy persisting for 20 s or less (Parker and Coiera 2000). When working memory is taxed, in other words when cognitive workload is high, errors are more likely (Reason 1990). Nursing workload measures, however, typically focus on the number of patients assigned to each nurse (Carayon and Gurses 2008; Holden et al. 2011; Swiger et al. 2016), a metric that fails to consider cognitive workload.
Communication, time pressure, and cognitive shifts all contribute to nurses’ cognitive workload. Communication events are defined as “any action taken in order to relay information to another clinician” (Edwards et al. 2009, p. 630). Communication may also occur as a part of multitasking, such as completing documentation while talking (Edwards et al. 2009). As noted previously, communication is a major contributor to interruptions. Both high communication load and interruptions create demands on working memory (Parker and Coiera 2000).
Time pressure is also associated with increased cognitive workload and possibly cognitive failure (Elfering et al. 2013). Woods and Patterson (2001) noted that as operational tempo increases and situations become more critical, information processing must also increase to keep pace with the activities, thereby increasing the cognitive workload and yielding greater cognitive complexity. For instance, Grayson et al. (2005) found that nursing personnel, 84% of whom were RNs, reported more errors when they perceived their work conditions as more hectic; errors were often related to missing patient information.
Potter et al. (2004, 2005) added to the understanding of nurses’ cognitive workload by illustrating the repetitive pathways nurses traveled, the interruptions nurses experienced, and the cognitive shifts that nurses had to make. For instance, while observing one nurse caring for six patients over 10 h, investigators documented 128 links (physical movement between locations such as a patient’s room and the nurse’s station), 43 interruptions, and 71 cognitive shifts. These observations illustrate the challenge to short-term memory due to the cognitive shifts involved in task-switching (Potter et al. 2004).
Cognitive Stacking
Ebright et al. (2003) identified three patterns in RN work performance: work complexity, cognitive factors, and care management strategies. One care management strategy was labeled “stacking” and defined as the nurses’ ability to “[move] on to other activities to prevent downtime when not able to complete something because of waiting … or the inability to access resources” (Ebright et al. 2003, p. 636). Stacking involves managing time and changing priorities. Nurses constantly shift among tasks as they reorganize their work to avoid waiting (Biron et al. 2009; Ebright et al. 2003; Hall et al. 2010; Jennings et al. 2011; Tucker and Spear 2006) and to alter priorities based on patients’ clinical conditions (Ebright et al. 2003; Patterson et al. 2011).
Potter et al. (2005) built on Ebright’s idea of stacking (Ebright et al. 2003) and developed a way to calculate cognitive stacking to reflect the cognitive demands nurses handle. Based on observations of seven RNs, Potter et al. (2005) determined that nurses managed an average cognitive stack of 11 tasks and a maximum cognitive stack of 16. Both the average and the maximum stack exceed Miller’s (1956) magic number of working memory being able to handle seven plus or minus two, illustrating that working memory is stressed if not exceeded because of the increased cognitive workload. Although similar to a mental “to-do” list, a nurse’s cognitive stack has more potential patient safety consequences (Patterson et al. 2011).
To advance the concept of cognitive stacking, Patterson et al. (2011) sought to understand how RNs prioritize activities. They developed a 7-level hierarchy of priorities among nursing tasks. Threatening clinical concerns were at the top of the hierarchy, as were activities with high uncertainty (Patterson et al. 2011). Experienced nurses prioritized differently than those with less experience. For instance, they understood trade-offs better, such as how delaying some tasks could increase the workload at the end of the shift (Patterson et al. 2011). More recently, task juggling, which resembles stacking, is another term to help nurses stay on track (Renolen et al. 2018). Juggling and stacking contribute to nurses’ cognitive complexity and thus influence the outcomes of work stress and cognitive failure.
Client (Nurse) Outcomes
Work Stress
Nursing has long been regarded as a stressful profession, largely due to the nature of the work and the working conditions (Jennings 2008c). Stress is a complicated phenomenon because it may be a stimulus, a response, or an interaction (Jennings 2008c). Consequently, various perspectives seek to explain stress, all of which note that stress involves perception and interpretation of incidents in the work setting. Lazarus and Folkman (1984), for instance, adopted a psychological stance stating that stress is “a particular relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and endangering his or her well-being” (p. 19).
Work stress is at the crux of concerns about nurses’ work environment and patient safety. Findings from two studies conducted in Switzerland showed that conditions such as time pressure, cognitive demands, and workflow interruptions contributed to high job stress (Elfering et al. 2006) and low job satisfaction (Baethge and Rigotti 2013). Although turbulence per se was not mentioned in the Swiss studies, the findings reflect that workflow issues and cognitive demands contribute to work stress. One might surmise that reducing environmental turbulence or diminishing nursing workflow irregularities could reduce some of nurses’ work-related stress.
Cognitive Failure
Cognitive failure refers to lapses in memory, perception, and action (Broadbent et al. 1982), yielding “mistakes on everyday tasks that a person normally is capable of completing without error” (Elfering et al. 2011, p. 194). Carrigan and Barkus (2016) conducted a systematic review of 45 articles focused on healthy people (e.g., US military personnel, undergraduate students) who experienced cognitive failures or “brain farts” (p. 30). From their review, Carrigan and Barkus noted a variety of factors that contributed to cognitive failures—some were stable characteristics, such as neuroticism and trait anxiety, and some were variable characteristics, such as times of high stress and chaotic environmental conditions. High work stress and turbulent workflow may predispose healthcare workers to cognitive failures.
Elfering et al. (2011) illustrated an association between job characteristics and work-related cognitive failures among 96 nurses in 11 Swiss hospitals. As expected, cognitive workload increased when task stressors (e.g., interruptions, time pressure) increased, enhancing the likelihood of cognitive failure. In a second study involving 165 nurses in 7 Swiss hospitals, the investigators confirmed that workflow interruptions (i.e., turbulence) were likely triggers of errors (Elfering et al. 2015). Elfering et al. (2015) recommended work redesign to reduce cognitive failure and improve patient safety.
Implications and Future Directions
As showcased in this chapter, turbulent workflow is a significant characteristic of the system within which nurses work. Turbulence adds to the cognitive complexity of nurses’ work with the potential to contribute to work stress and cognitive failure. The implications are clear. First, attention is needed to focus on how systems might be redesigned to improve nurses’ workflow and reduce turbulence. Second, and perhaps more immediately achievable, interventions are needed to improve nurses’ work (e.g., smoothing workflow and mitigating turbulence). Third, and very achievable, is to increase simulation training in nursing education to better prepare student nurses for the practice setting’s reality. Perhaps less time on learning bed baths and more time learning to manage interruptions would alleviate some work stress and cognitive failures.
Leaders at the organizational and unit levels need to be educated to recognize workarounds and turbulence as warning signs and examine other data reflective of turbulence. Patient turnover and handoffs are two such data points. Examining patient flow resulting from turnover can pinpoint hours of the day when turnover is least disruptive for all units involved, affording opportunities for optimizing workflow. Because handoffs are a companion to patient turnover, examining patient turnover might also improve information exchange during the handoff. As part of patient turnover, early identification of patients for discharge and arranging for discharges early in the day might be used as incentives.
New hospital construction needs to involve a cadre of individuals such as architects, human factors engineers, and practicing nurses to ensure that clunky features within existing work systems are not replicated in new facilities. Healthcare leaders and administrators need to participate in this work too, helping to design hospitals of the future that are built to maximize efficiency and minimize turbulence. Any additional costs associated with designing and constructing turbulence-reducing hospitals must be weighed against the cost of continually recruiting nurses to replace those who leave the workplace due to stress and burnout, as well as the cost associated with unsafe patient care.
It might also be helpful to develop measures of turbulent workflow; human factors engineers would be important allies in such endeavors. It seems there is sufficient evidence, however, that the nurses’ work environment is turbulent. Thus, rather than measure what seems like a given, it would be more beneficial to invest time and resources into improving practice environments. Diminishing turbulence was an explicit suggestion from Myny et al. (2012). More generally, Carayon and Gurses (2008) recommended redesigning work systems to reduce nurses’ workload. Even modest investments might yield substantial returns. For instance, mobile work telephones were implemented to minimize nurses need to walk to a central nurses’ station to get or return telephone calls. What was not anticipated, however, was the highly interruptive nature of mobile work telephones. These interruptions are one of many examples of practices that need to be thought through more fully to minimize unwanted consequences of work system redesign. Similarly, it is essential to determine whether care quality is affected by implementing interventions to improve the practice environment (Swiger et al. 2017).
Finally, a word of caution for the future of existing measures of nurses’ work environments (Chaps. 4 and 13); workflow and turbulence are not reflected in these measures. Moreover, a family of measures was developed using data from the 1980s. Nursing practice has changed immensely since those measures were developed. The trio of measures are the Nursing Work Index (NWI; Kramer and Hafner 1989), the Nursing Work Index-Revised (NWI-R; Aiken and Patrician 2000), and the Practice Environment Scale of the Nursing Work Index (PES-NWI; Lake 2002, 2007) (Chap. 4). The PES-NWI is especially prominent because of its wide use (Swiger et al. 2017; Warshawsky and Havens 2011). Therefore, leaders must consider what work environment measures reflect about contemporary environments, realizing that turbulence sources are not represented.
Workflow for nurses is an oxymoron—nurses’ work in a flow that is turbulent. Although workflow is a significant issue within the nursing profession, there is little evidence of remediating the turbulent working conditions. Practicing nurses deal with turbulence from many sources. They use ingenious strategies to function as best they are able for patients and themselves despite the turbulent workflow. To keep nurses interested in acute care and bedside practice, it is imperative that we reduce the turbulent flow that prevails in acute care settings, making them safer for patients and better for the nurses who practice in them.
References
Aarts J, Ash J, Berg M (2007) Extending the understanding of computerized physician order entry: implications for professional collaboration, workflow and quality of care. Int J Med Inform 76S:S4–S13
Abraham J, Reddy MC (2010) Challenges to inter-departmental coordination of patient transfers: a workflow perspective. Int J Med Inform 79:112–122
Aiken LJ, Patrician PA (2000) Measuring organizational traits of hospitals: the revised nursing work index. Nurs Res 49:146–153
Allen D (2004) Re-reading nursing and re-writing practice: towards an empirically based reformulation of the nursing mandate. Nurs Inq 11:271–283
Ash JS, Berg M, Coiera E (2004) Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc 11:104–112
Baethge A, Rigotti T (2013) Interruptions to workflow: their relationship with irritation and satisfaction with performance, and the mediating roles of time pressure and mental demands. Work Stress 27:43–63
Bazzoli GJ, Dynan L, Burns LR, Yap (2004) Two decades of organizational change in health care: what have we learned. Med Care Res Rev 613:247–331
Beach C, Cheung DS, Apker J, Horwitz LI, Howell EE, O’Leary KJ, Patterson ES et al (2017) Improving interunit transitions of care between emergency physicians and hospital medicine physicians: a conceptual approach. Acad Emerg Med 19:1188–1195
Beekun RI, Ginn GO (1993) Business strategy and interorganizational linkages within the acute care hospital industry: an expansion of the Miles and Snow typology. Hum Relat 46:1291–1318
Berwick DM (2002) A user’s manual for the IOM’s ‘Quality Chasm’ report. Health Aff 21:80–90
Biron AD, Lavoie-Tremblay M, Loiselle CG (2009) Characteristics of work interruptions during medication administration. J Nurs Scholarsh 41(4):330–336
Blay N, Duffield CM, Gallagher R, Roche M (2014) A systematic review of time studies to assess the impact of patient transfers on nurse workload. Int J Nurs Pract 20:662–673
Blay N, Roche MA, Duffield C, Gallagher R (2017) Intrahospital transfers and the impact on nursing workload. J Clin Nurs 26:4822–4829
Bosco CL (2007) The relationship between environmental turbulence, workforce ability and patient outcomes. University of Arizona, Tucson, AZ
Brixey JJ, Robinson DJ, Johnson CW, Johnson TR, Turley JP, Zhang JJ (2007) A concept analysis of the phenomenon interruption. Adv Nurs Sci 30(1):E26–E42
Broadbent DE, Cooper PF, FitzGerald P, Parkes KR (1982) The cognitive failures questionnaire (CFQ) and its correlates. Br J Clin Psychol 21:1–16
Brown T (2019) The American medical system is one giant workaround. The New York Times, Section A, Sept 6. p. 23.
Browne J, Braden CJ (2020) Nursing turbulence in critical care: relationships with nursing workload and patient safety. Am J Crit Care 29:182–191
Cain C, Hague S (2008) Organizational workflow and its impact on work quality. In: Hughes R (ed) Patient safety and quality: an evidence-based handbook for nurses, AHRQ Publication No. 08-0043. Agency for Healthcare Research and Quality, Rockville, MD, pp 2-217–2-244
Cameron KS, Kim MU (1987) Organizational effects of decline and turbulence. Adm Sci Q 32(2):222–240
Carayon P, Gurses AP (2008) Nursing workload and patient safety—A human factors engineering perspective. In: Hughes R (ed) Patient safety and quality: an evidence-based handbook for nurses, AHRQ Publication No. 08-0043. Agency for Healthcare Research and Quality, Rockville, MD, pp 2-203–2-216
Carayon P, Hundt AS, Karsh B-T, Gurses AP, Slvarado CJ, Smith M, Brennan PF (2007) Work system design for patient safety: the SEIPS model. Qual Saf Health Care 15(Suppl 1):i50–i58
Carrigan N, Barkus E (2016) A systematic review of cognitive failures in daily life: healthy populations. Neurosci Biobehav Rev 63:29–42
Carroll JS, Williams M, Gallivan TM (2012) The ins and outs of change of shift handoffs between nurses: a communication challenge. BMJ Qual Saf 21:586–593
Cohen MD, Hilligoss PB (2010) The published literature on handoffs in hospitals: deficiencies identified in an extensive review. BMJ Qual Saf Health Care 19:493–497
Cohen MD, Hilligoss B, Amaral ACK-B (2012) A handoff is not a telegram: an understanding of the patient is co-constructed. Crit Care 16:303
Coiera E (2012) The science of interruption. [Editorial]. BMJ Qual Saf Health Care 21:357–360
Coiera E, Tombs V (1998) Communication behaviours in a hospital setting: an observational study. Br Med J 316:673–676
Comprehensive Accreditation Manual for Hospitals (2013) Sentinel events (SE). https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/topics-library/camh_2012_update2_24_sepdf.pdf?db=web&hash=FD320B7BAF3E08EC28B44AA51CB21ABE
Cornell P, Herrin-Griffith D, Keim C, Petschonek S, Sanders AM, D’Mello S et al (2010) Transforming nursing workflow, Part 1. The chaotic nature of nurse activities. J Nurs Adm 40:366–373
Cornell P, Riordan M, Townsend-Gervis M, Mobley R (2011) Barriers to critical thinking. Workflow interruptions and task switching among nurses. J Nurs Adm 41:407–414
Cornell P, Gervis MT, Yates L, Vardaman JM (2013) Improving shift report focus and consistency with the Situation, Background, Assessment, Recommendation protocol. J Nurs Adm 43:422–428
Couffe C, Michael GA (2017) Failures due to interruptions or distractions: a review and a new framework. Am J Psychol 130(2):163–181
Debono DS, Greenfield D, Travaglia JF, Long JF, Black D, Johnson J, Braithwaite J (2013) Nurses’ workarounds in acute healthcare settings: a scoping review. BMC Health Serv Res 13:175
Derksen M (2014) Turning men into machines? Scientific management, industrial psychology, and the “human factor”. J Hist Behav Sci 50(2):148–165
Dickson GL, Flynn L (2012) Nurses’ clinical reasoning: processes and practices of medication safety. Qual Health Res 22:3–16
Douglas HE, Raban MZ, Walter SR, Westbrook JI (2017) Improving our understanding of multi-tasking in healthcare: drawing together the cognitive psychology and healthcare literature. Appl Ergon 59:45–55
Dracup K, Morris PE (2008) Passing the torch: the challenge of handoffs. [Editorial]. Am J Crit Care 17:95–97
Ebright PR, Patterson ES, Chalko BA, Render M (2003) Understanding the complexity of registered nurse work in acute care settings. J Nurs Adm 33:630–638
Edwards A, Fitzpatrick L-A, Augustine S, Trzebucki A, Cheng SL, Presseau C et al (2009) Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform 78:629–637
Eisenhauer LA, Hurley AC, Dolan N (2007) Nurses’ reported thinking during medication administration. J Nurs Scholarsh 39(1):82–87
Elfering A, Semmer NK, Grebner S (2006) Work stress and patient safety: observer-rated work stressors as predictors of characteristics of safety-related events reported by young nurses. Ergonomics 49:457–469
Elfering A, Grebner S, Dudan A (2011) Job characteristics in nursing and cognitive failure at work. Saf Health Work 2:194–200
Elfering A, Grebner S, de Tribolet-Hardy F (2013) The long arm of time pressure at work: cognitive failure and commuting near accidents. Eur J Work Organ Psychol 22:737–749
Elfering A, Grebner S, Ebener C (2015) Workflow interruptions, cognitive failure and near-accidents in health care. Psychol Health Med 20:139–147
Fairbanks RJ, Bisantz AM, Sunm M (2007) Emergency department communication links and patterns. Ann Emerg Med 50:396–406
Friesen MA, White SV, Byers JF (2008) Handoffs: implications for nurses. In: Hughes R (ed) Patient safety and quality: an evidence-based handbook for nurses, AHRQ Publication No. 08-0043. Agency for Healthcare Research and Quality, Rockville, MD, pp 2-285–2-332
Gandhi TK (2005) Fumbled handoffs: one dropped ball after another. Ann Intern Med 142:352–358
Gleick J (1987) Chaos. Making a new science. Penguin Books, New York, NY, pp 121–123
Gosbee J (1998) Communication among health professionals: human factors engineering can help make sense of the chaos. Br Med J 316(7132):642
Grayson D, Boxerman S, Potter P, Wolf L, Dunagan C, Sorock G, Evanoff B (2005) Do transient working conditions trigger medical errors? In: Henriksen K, Battles JB, Marks ES, Lewin DI (eds) Advances in patient safety: from research to implementation. Vol. 1, Research findings, AHRQ Publication No. 05-0021-1. Agency for Healthcare Research and Quality, Rockville, MD, pp 53–64
Grissinger M (2010) The five rights. A destination without a map. PT 35:542
Grundgeiger T, Sanderson P (2009) Interruptions in healthcare: theoretical views. Int J Med Inform 78:293–307
Gurses AP, Carayon P, Wall M (2009) Impact of performance obstacles on intensive care nurses’ workload, perceived quality and safety of care, and quality of working life. HSR: Health Service Res 44(part 1):422–443
Hall LM, Pedersen C, Fairley L (2010) Losing the moment. Understanding interruptions to nurses’ work. J Nurs Adm 40:169–176
Hampson I, Junor A (2005) Invisible work, invisible skills: interactive customer service as articulation work. New Technology. Work Employm 20:166–181
Hilligoss B, Cohen MD (2011) Hospital handoffs as multi-functional situated routines: implications for researchers and administrators. Adv Health Care Manag 11:91–132
Hilligoss B, Cohen MD (2013) The unappreciated challenges of between-unit handoffs: negotiating and coordinating across boundaries. Ann Emerg Med 61:155–160
Holden RJ, Scanlon MC, Patel NR, Kaushal R, Escoto KH, Brown RL et al (2011) A human factors framework and study of the effect of nursing workload on patient safety and employee quality of working life. BMJ Qual Saf 20:15–24
Hopkinson SG, Jennings BM (2013) Interruptions during nurses’ work: a state-of-the-science review. Res Nurs Health 36:38–53
Hopkinson SG, Weigand DL (2017) The culture contributing to interruptions in the nursing work environment: an ethnography. J Clin Nurs 26:5093–5102
Institute for Healthcare Improvement [IHI] Multimedia Team (2017) Teamwork and communication: the keys to building a strong patient safety culture. IHI_%20Teamwork%20and%20Communication_%20Multimedia%202017.html
Jennings BM (2008a) Restructuring and mergers. In: Hughes R (ed) Patient safety and quality: an evidence-based handbook for nurses, AHRQ Publication No. 08-0043. Agency for Healthcare Research and Quality, Rockville, MD, pp 2-93–2-109
Jennings BM (2008b) Turbulence. In: Hughes R (ed) Patient safety and quality: an evidence-based handbook for nurses, AHRQ Publication No. 08-0043. Agency for Healthcare Research and Quality, Rockville, MD, pp 2-193–2-202
Jennings BM (2008c) Work stress and burnout among nurses: role of the work environment and working conditions. In: Hughes R (ed) Patient safety and quality: an evidence-based handbook for nurses, AHRQ Publication No. 08-0043. Agency for Healthcare Research and Quality, Rockville, MD, pp 2-137–2-158
Jennings BM, Sandelowski M, Mark B (2011) The nurse’s medication day. Qual Health Res 21:1441–1451
Jennings BM, Sandelowski M, Higgins MK (2013) Turning over patient turnover: an ethnographic study of admissions, discharges, and transfers. Res Nurs Health 36:554–566
Jett QR, George JM (2003) Work interrupted: a closer look at the role of interruptions in organizational life. Acad Manag Rev 28:494–507
Kalisch BJ, Aebersold M (2010) Interruptions and multi-tasking in nursing care. Jt Comm J Qual Patient Saf 36:126–132
Kalisch BJ, Begeny S, Anderson C (2008) The effect of consistent nursing shifts on teamwork and continuity of care. J Nurs Adm 38:132–137
Karsh B-T, Holden RJ, Alper SJ, Or CKL (2006) A human factors engineering paradigm for patient safety: designing to support the performance of the healthcare professional. BMJ Qual Saf Health Care 15:i59–i65
Kohn LT, Corrigan JM, Donaldson MS (eds) (2001) To err is human. Building a safer health system. National Academy Press, Washington, DC
Koopman P, Hoffman RR (2003) Work-arounds, make-work, and kludges. IEEE Intell Syst 18(6):70–75
Koppel R, Wetterneck T, Telles JL, Karsh B-T (2008) Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc 15:408–423
Kramer M, Hafner LP (1989) Shared values: impact on staff nurse satisfaction and perceived productivity. Nurs Res 38:172–177
Krichbaum KE, Peden-McAlpine C, Diemert C, Koenig P, Mueller C, Savik K (2011) Designing a measure of complexity compression in registered nurses. West J Nurs Res 33(1):7–25
Lake ET (2002) Development of the practice environment scale of the nursing work index. Res Nurs Health 25:176–188
Lake ET (2007) The nursing practice environment: measurement and evidence. Med Care Res Rev 64:104S–122S
Lawal AK, Rotter T, Kinsman L, Sari N, Harrison L, Jeffery C et al (2014) Lean management in health care: definition, concepts, methodology and effects reported (systematic review protocol). Syst Rev 3:103
Laxmisan A, Hakimzada F, Sayan OR, Green RA, Zhang J, Patel VL (2007) The multi-tasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform 76:801–811
Lazarus RS, Folkman S (1984) Stress, appraisal, and coping. Springer, New York, NY
Leonard M, Graham S, Bonacum D (2004) The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 13(Suppl 1):i85–i90
Li SYW, Magrabi F, Coiera E (2012) A systematic review of the psychological literature on interruption and its patient safety implications. J Am Med Inform Assoc 19:6–12
Lin F, Chaboyer W, Wallis M, Miller A (2013) Factors contributing to the process of intensive care patient discharge: an ethnographic study informed by activity theory. Int J Nurs Stud 50:1054–1066
Magrabi F, Li SYW, Dunne AG, Coiera E (2011) Challenges in measuring the impact of interruption on patient safety and workflow outcomes. Methods Inf Med 50:447–453
Mark G (2015) Multi-tasking in the digital age. Morgan & Claypool, San Rafael, CA
McCann JE, Selsky J (1984) Hyperturbulence and the emergence of type 5 environments. Acad Manag 9:460–470
McDaniel RR, Jordan ME, Fleeman BF (2003) Surprise, surprise, surprise! A complexity science view of the unexpected. Health Care Manag Rev 28:266–278
Menzies IEP (1960) Nurses under stress. Int Nurs Rev 7:9–16
Mikesell L, Bromley E (2012) Patient centered, nurse averse? Nurses’ care experiences in a 21st-century hospital. Qual Health Res 22:1659–1671
Miller GA (1956) The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev 63:81–97
Mitchell PH, Ferketich S, Jennings B (1998) Quality health outcomes model. Image J Nurs Sch 30(1):43–46
Morgan B, D’Mello S, Abbott R, Radvansky G, Haass M, Tamplin A (2013) Individual differences in multi-tasking ability and adaptability. Human Fact J Human Fact Ergon Soc 55:776–788
Myny D, Van Hecke A, De Bacquer D, Verhaeghe S, Gobert M, Defloor T, Van Goubergen D (2012) Determining a set of measurable and relevant factors affecting nursing workload in the acute care hospital setting: a cross-sectional study. Int J Nurs Stud 49:427–436
National Academies of Sciences, Engineering, and Medicine (2019) Taking action against clinician burnout: a systems approach to professional well-being. The National Academies Press, Washington, DC
Norrish BR, Rundall TG (2001) Hospital restructuring and the work of registered nurses. Milbank Quart 79(1):55–79
Novak LL, Lorenzi NM (2008) Barcode medication administration: supporting transitions in articulation work. AMIA Symp Proc 2008:515–519
Ong M-S, Coiera E (2011) A systematic review of failures in handoff communication during intrahospital transfers. Jt Comm J Qual Patient Saf 37:274–284, AP1–AP6
Park SH, Weaver L, Mejia-Johnson L, Vukas R, Zimmerman J (2016) An integrative literature review of patient turnover in inpatient hospital settings. West J Nurs Res 38:629–655
Parker J, Coiera E (2000) Improving clinical communication: a view from psychology. J Am Med Inform Assoc 7:453–461
Patterson ES, Cook RI, Render ML (2002) Improving patient safety by identifying side effects from introducing bar coding in medication administration. J Am Med Inform Assoc 9:540–553
Patterson ES, Ebright PR, Saleem JJ (2011) Investigating stacking: how do registered nurses prioritize their activities in real-time? Int J Ind Ergon 41:389–393
Perlow LA (1999) The time famine: toward a sociology of work time. Adm Sci Q 44:57–81
Phillips L (2018) Turbulence, the oldest unsolved problem in physics. arstechnica.com/science/2018/10/turbulence-the-oldest-unsolved-problem-in-physics
Pingenot A, Shanteau J, Sengstacke DN (2009) Description of inpatient medication management using cognitive work analysis. CIN: Comput Informat Nurs 27:379–392
Plsek P (2001) Redesigning health care with insights from the science of complex adaptive systems. In: Institute of Medicine Committee on Quality of Health Care in America (Ed.), Crossing the Quality Chasm. National Academy Press, Washington, DC, pp 309–322
Potter P, Boxerman S, Wolf L, Marshall J, Grayson D, Sledge J, Evanoff B (2004) Mapping the nursing process. A new approach for understanding the work of nursing. J Nurs Adm 34:101–109
Potter P, Wolf L, Boxerman S, Grayson D, Sledge J, Dunagan C, Evnaoff B (2005) Understanding the cognitive work of nursing in the acute care environment. J Nurs Adm 35:327–335
Powell-Cope G, Nelson AL, Patterson ES (2008) Patient care technology and safety. In: Hughes R (ed) Patient safety and quality: an evidence-based handbook for nurses, AHRQ Publication No. 08-0043. Agency for Healthcare Research and Quality, Rockville, MD, pp 3-207–3-220
Reason J (1990) Human error. Cambridge. Cambridge University Press, England
Reed C, Minnick AF, Dietrich MS (2018) Nurses’ responses to interruptions during medication tasks: a time and motion study. Int J Nurs Stud 82:113–120
Renolen A, Hoye S, Hjalmhult E, Danbolt LJ, Kirkevold M (2018) “Keeping on track”—Hospital nurses’ struggles with maintaining workflow while seeking to integrate evidence-based practice into their daily work: a grounded theory study. Int J Nurs Stud 77:179–188
Rivera-Rodriguez AJ, Karsh B-T (2010) Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care 19:304–312
Rosenberg A, Britton MC, Feder S, Minges K, Hodshon B, Chaudhry SI et al (2018) A taxonomy and cultural analysis of intra-hospital patient transfers. Res Nurs Health 41:378–388
Rubinstein JS, Meyer DE, Evans JE (2001) Executive control of cognitive processes in task switching. J Exp Psychol 27:753–797
Salyer J (1995) Environmental turbulence. Impact on nurse performance. J Nurs Adm 25(4):12–20
Sendelbach S, Funk M (2013) Alarm fatigue. A patient safety concern. AACN Adv Crit Care 24:378–386
Sitterding MC, Ebright P (2015) Information overload: a framework for explaining the issues and creating solutions. In: Sitterding MC, Broome ME (eds) Information overload. American Nurses Association, Silver Spring, MD, pp 11–33
Staggers N, Jennings BM (2009) The content and context of change of shift report on medical and surgical units. J Nurs Adm 39:393–398
Star SL (1991) The sociology of the invisible: the primacy of work in the writings of Anselm Strauss. In: Maines DR (ed) Social organization and social process. Essays in honor of Anselm Strauss. Aldine de Gruyter, Hawthorne, NY, pp 265–283
Star SL, Strauss AL (1999) Layers of silence, arenas of voice: the ecology of visible and invisible work. Comput Support Cooperat Work (CSCW) 8:9–30
Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, et al for the I-PASS Study Group (2014) Changes in medical errors after implementation of a handoff programs. N Engl J Med 371:1803–1812
Starmer AJ, Schnock KO, Lyons A, Hehn RS, Graham DA, Keohane C, Landrigan CP (2017) Effects of the I-PASS nursing handoff bundle on communication quality and workflow. BMJ Qual Saf 26:949–957
Strauss A (1985) Work and the division of labor. Sociol Q 26:1–19
Strauss A (1988) The articulation of project work: an organizational process. Sociol Q 29:163–178
Strauss A, Fagerhaugh S, Suczek B, Wiener C (1997) Social organization of medical work. Transaction, New Brunswick, NJ
Swiger PA, Vance DE, Patrician PA (2016) Nursing workload in the acute-care setting: a concept analysis of nursing workload. Nurs Outlook 64:244–254
Swiger PA, Patrician PA, Miltner RS, Raju D, Breckenridge-Sproat S, Loan LA (2017) The practice environment scale of the nursing work index: an updated review and recommendations for use. Int J Nurs Stud 74:76–84
The Joint Commission (September 12, 2017) Sentinel event alert 58: inadequate handoff communication. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_58_hand_off_comms_9_6_17_final_(1).pdf
Tubbs-Cooley HL, Mara CA, Carle AC, Gurses AP (2018) The NASA Task Load Index as a measure of overall workload among neonatal, paediatric and adult intensive care nurses. Intens Crit Care Nurs 46:64–69
Tucker AL (2004) The impact of operational failures on hospital nurses and their patients. J Oper Manag 22:151–169
Tucker AL, Spear SJ (2006) Operational failures and interruptions in hospital nursing. HSR: Health Service Res 41(3, Part 1):643–662
Verran JA, Effken J, Lamb G (2003) Impact of nursing unit characteristics on outcomes. RO1HS11973. Agency for Healthcare Research & Quality
Wachter RM, Shojania KG (2005) Handoffs and fumbles. In: Internal bleeding. Rugged Land, New York, NY, pp 159–179
Walter SR, Li L, Dunsmuir WTM, Westbrook JI (2014) Managing competing demands through task-switching and multi-tasking: a multi-setting observational study of 200 clinicians over 1000 hours. BMJ Qual Saf 23:231–241
Warshawsky NE, Havens DS (2011) Global use of the practice environment scale of the nursing work index. Nurs Res 60:17–31
Waterworth S, May C, Luker K (1999) Clinical ‘effectiveness’ and ‘interrupted’ work. Clin Eff Nurs 3(4):163–169
Weigl M, Muller A, Vincent C, Angerer P, Sevdalis N (2012) The association of workflow interruptions and hospital doctors’ workload: a prospective observational study. BMJ Qual Saf 21:399–407
Weigl M, Beck J, Wehler M, Schneider A (2017) Workflow interruptions and stress at work: a mixed-methods study among physicians and nurses of a multidisciplinary emergency department. BMJ Open:7
Welsh CA, Flanagan ME, Ebright P (2010) Barriers and facilitators to nursing handoffs: recommendations for redesign. Nurs Outlook 58:148–154
Whittaker J, Ball C (2000) Discharge from intensive care: a view from the ward. Intens Crit Care Nurs 16:135–143
Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM (2007) Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery 142:658–665
Woods DD, Patterson ES (2001) How unexpected events produce an escalation of cognitive and coordinative demands. In: Hancock PA, Desmond PA (eds) Stress, workload, and fatigue. Lawrence Erlbaum, Mahwah, NJ, pp 290–301
World Health Organization (2020) WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020
Zhang J, Patel VL, Johnson TR, Shortliffe EH (2004) A cognitive taxonomy of medical errors. J Biomed Inform 37:193–204
Zuzelo PR, Gettis C, Hansell AW, Thomas L (2008) Describing the influence of technologies on registered nurses’ work. Clin Nurse Spec 22:132–140
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Jennings, B.M. (2021). Workflow, Turbulence, and Cognitive Complexity. In: Baernholdt, M., Boyle, D.K. (eds) Nurses Contributions to Quality Health Outcomes. Springer, Cham. https://doi.org/10.1007/978-3-030-69063-2_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-69063-2_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-69062-5
Online ISBN: 978-3-030-69063-2
eBook Packages: MedicineMedicine (R0)