Abstract
Transition from pediatric to adult healthcare for adolescents and young adults with chronic lung disease can be challenging. Individuals must develop illness self-management skills, including obtaining appropriate knowledge and the ability to independently engage in self-care behaviors. Various individual factors can facilitate or impede this process. Specifically, developmental and psychosocial variables play an important role. Understanding the role of these factors in the transition to adult care, and developing best practices to address them, is critical to helping individuals with chronic lung disease, and their families, successfully navigate transition in care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The transition from pediatric to adult healthcare has traditionally been conceptualized as the development of a steady progression of skills leading to independence over a predictable time period, similar to walking up a smooth slope. However, more often, the transition process is like riding an amusement park attraction, with many ups and downs, curves and bumps, and sometimes even moving backward. Although uncertainty during transition is typical, there are common areas of expected challenge. These range from broad factors related to the adolescent and young adult (AYA)’s culture and access to healthcare services, to specialized individual skills such as the ability to schedule a medical appointment. Although social-ecological and systemic factors play an important role in the transition process [1], individual factors are the best understood [2] and potentially most modifiable [3]. Chief among these individual factors are the AYA’s illness self-management knowledge, skills, and behaviors [4]. This chapter provides an overview of illness self-management and its role in healthcare transition, reviews the literature on self-management within chronic lung disease, identifies developmental and psychosocial variables impacting self-management, and provides recommendations for addressing these variables and promoting self-management during care transition.
Models of Illness Self-Management
Pediatric illness self-management can be defined as the “interaction of health behaviors and related processes that patients and families engage in to care for a chronic condition” [4]. Many models to explain these interactions exist including those that are disease-specific [5] and those that are more inclusive, including the classic Health Belief Model [6]. This model theorizes that appropriate self-management behaviors can be predicted by an individual’s perceptions of their illness (view of illness severity and belief in the benefits of following the healthcare plan) in comparison to their perceived barriers to following this plan. Although widely cited, a criticism of this model is the challenge of translating this theory into intervention [5].
In contrast, the Transtheoretical Model of Behavioral Change [7] matches intervention strategies to each stage in the model and hypothesizes that individuals move through predictable stages of change, similar to developmental stages, when developing behaviors to promote their health. However, this model relies on an individual’s ability to control and make changes independently and does not fully take into account systemic influences that are critical during the AYA period, such as the influence of caregivers.
A more recent model of illness self-management, the Pediatric Self-Management Model [4], takes into account systemic influences impacting AYAs, including individual, family, and community factors; while also categorizing influences into those that are considered fairly static (socioeconomic status) and those that are more modifiable (psychosocial distress). Categorizing influences into those that are challenging to change versus more amenable to change makes it easier to translate this model into targeted intervention strategies.
Although these models each focus on different influences on self-management, common among them is the understanding that successful illness self-management encompasses appropriate knowledge of the illness, including how to navigate challenges; and the engagement in recommended self-care behaviors or medical regimen adherence [8]. Illness-specific knowledge is generally best conceptualized as necessary, but not sufficient, in that it is the building block for independence, but knowledge in itself typically does not lead to significant change [9]. Interventions targeting both knowledge and medical regimen adherence have, to date, shown the strongest results [9, 10]. Medical regimen adherence is often defined as the extent to which a person’s behavior matches medical or health advice [11]. Along with knowledge, it is perceived as a central part of illness self-management and is a modifiable factor that is often the target of behavioral intervention [10].
Role of Illness Self-Management in Transition
Transition from pediatric to adult care is a multiyear process that is generally conceptualized as the time period when AYAs become more independent in their medical care while also receiving less support. However, this transition is often not a smooth process and, if poorly planned, can result in significant morbidity and mortality complications for the AYA [12]. Using knowledge of these potential complications, providers have developed best practices for promoting transition among individuals with chronic lung disease, including those with asthma [13], cystic fibrosis (CF) [14], and who are dependent on respiratory technology, such as receiving home ventilator support [15]. Best practice recommendations for transition specific to AYA post lung transplantation are limited [16], but best practices for transition among all solid organ transplant recipients have been developed [17].
Best practices generally stress the measurement of “transition readiness” among the AYA population [18, 19]. Illness-related “knowledge and self-management skills are the most common factors included in measures of transition readiness, suggesting a consensus regarding these issues as key contributors” [1]; thereby placing illness self-management in a central role for successful healthcare transition. To date, preliminary research has supported the role of illness self-management in the transition process. Measurement of transition readiness has been positively related to healthcare knowledge [18], self-management beliefs [20], and self-management behaviors [21]. Although there is preliminary evidence that participation in programs designed to promote transition readiness results in positive change [22], sustained evidence is lacking [23], and there are few current links between transition readiness and adult medical outcomes [22].
Role of Illness Self-Management in Chronic Lung Disease
Transition theory and preliminary evidence support the integral role that illness self-management plays in successful transition to adult care, including among those with chronic lung disease. Unfortunately, illness self-management skills are often lacking, especially during the AYA time period when medical regimen adherence is generally the poorest [24].
Among all AYAs with chronic illness, medical knowledge has been correlated with medical regimen adherence [25], but education on its own has little evidence for prompting behavior change [10]. Further, having a cognitive deficit, especially impairment in executive function skills (organization, planning, working memory), may contribute to unique barriers to developing appropriate illness-related knowledge and skills [26].
Among AYAs with chronic lung disease, medical knowledge also plays an important role in illness self-management. There is some evidence that individuals diagnosed with asthma may be at greater risk for cognitive impairment, especially among executive function skills [27]. Further, poor health literacy (understanding of healthcare information) may negatively impact the ability to use asthma knowledge [28] and has been associated with poorer physical functioning [29]. In AYAs requiring invasive or noninvasive home ventilation, there is evidence of a cognitive impact, especially among executive function skills [30,31,32,33], but there is only preliminary evidence of the relationship between these impacts and illness-related knowledge [31]. Among individuals diagnosed with CF, there is preliminary evidence of higher rates of executive function deficit [34], but it has not been related to treatment knowledge. Although understudied, no apparent cognitive impairment has been identified in individuals that are post heart-lung transplantation [35].
Strong evidence exists supporting the prevalence and impact of poor medical regimen adherence among all AYAs with chronic illness. Recent estimates have reported that only between 10 and 35% of adolescents across chronic illness groups can be classified as adherent to their medical regimens [10]. Poor adherence is associated with numerous negative outcomes including increased healthcare use [36], and interventions that improve adherence have shown positive benefits to health [9].
Evidence of medical regimen adherence difficulties in AYAs with chronic lung disease is also strong. Among those with asthma, adolescents have been found to take <50% of prescribed doses of daily medications [37], and similar results have been found for adolescents with CF (medication possession ratios of 45–50% per pharmacy refill data) [38]. For those receiving noninvasive home ventilation, there have been mixed results from findings that only 27% use support for >3 hours to 72% using support for 8 hours [39]. The medical regimen adherence among those using invasive home ventilation is largely unknown. Finally, adherence rates among adolescents who have received lung transplantation are understudied, but a recent article using a large dataset of pediatric heart and lung transplant recipients found that physicians reported evidence of nonadherence to immunosuppressant medications at the rate of 34% [40].
According to the Health Belief Model, understanding of barriers to medical regimen adherence is key [6]. A wide range of barriers are present during the AYA period making them more susceptible to nonadherence. These include barriers related to the family system, healthcare system, and the community. During transition of care, 53% of young adults with CF were found to have a gap in care with 12% having a gap of at least 1 year [41]. Gaps in care of 1 year or more were associated with younger age at transfer and having an adult center in a different city than the pediatric center. Further, socioeconomic status (SES) may play a role as lower adherence to airway clearance in CF has been demonstrated among those with lower SES [42]. Another criterial influence on adherence during the AYA period is family, and especially caregiver, functioning. Parental depression has been associated with poorer adherence in both CF [43] and asthma [44]. Less parental supervision is related to decreased adherence in CF [45], and intervention to improve family support improved adherence in asthma [46].
Unfortunately, societal and family influences on illness self-management can be challenging to overcome. Thus, as the Transtheoretical Model of Behavioral Change suggests, focus on individual behavioral change may be an effective intervention target [7]. Although many individual factors are also largely nonmodifiable (sex, age, cognitive functioning), as the Pediatric Self-Management Model suggests, focusing intervention on modifiable factors is key [4]. Finally, Models of healthcare transition have also highlighted focus on modifiable individual characteristics such as treatment knowledge and medical regimen adherence [1,2,3]. Familiarity with typical adolescent development can aid in understanding of how knowledge develops over time as well as the interaction between knowledge and behavior. Further, psychosocial distress is a modifiable factor impacting illness self-management [10].
Adolescent Development and Illness Self-Management
Although developmental influences are largely nonmodifiable (except with time), familiarity with these influences can significantly increase understanding of the AYA and result in the development of practical intervention approaches. Physical development occurs rapidly in adolescence along with hormonal changes that can impact health functioning independently of illness self-management behaviors. For instance, earlier age at menarche has been associated with poorer adult lung function in epidemiological studies [47], and female sex hormones appear to play a role in CF pulmonary exacerbations [48]. Additionally, with rapid physical growth, appropriate drug dosing can become challenging during adolescence.
Along with physical changes, adolescents also experience cognitive changes, including the development of abstract reasoning, executive function skills, and metacognition (awareness of thought) [49]. However, these skills develop at different rates and, in certain cases, may be impeded in individuals with chronic lung disease as previously summarized. Importantly, impediments in cognitive skills have been related to worse illness self-management [26, 28, 31].
Traditional theories of adolescent development can be applied to increase understanding of how illness self-management behaviors form and change over time. Piaget’s theory of cognitive development hypothesizes that adolescents move into “the formal operational stage” of cognitive development where they develop the capacity for abstract, scientific thinking [50]. During this time, adolescents begin to generate multiple solutions to problems and can solve abstract problems that they have never encountered in real life. Although there is some evidence that being in a family who is skillful at solving complex problems may aid an adolescent in adherence to a CF regimen [51], clinical interventions to improve problem-solving skills have not yet demonstrated improvement in adolescents’ CF adherence [52].
It may be that the development of abstract thought initially impedes an adolescent due to negative side effects. This includes the development of argumentativeness, self-consciousness, and self-focusing [49]. Whereas during childhood, an individual with chronic lung disease might follow their treatment regimen with little resistance; in adolescence, the teen may debate a parent or question the need to complete the regimen. Additionally, self-consciousness increases in adolescence with the development of the “imaginary audience” belief where adolescents feel that they are the focus of everyone’s attention [49]. This belief may result in an adolescent not wanting to disclose their illness or engage in medical care in front of others. Adolescents with CF have identified embarrassment and desire for social acceptance as barriers to adherence [53], and a study measuring asthma adherence in adolescence found that 53% of nonadherence episodes occurred while present with friends [54]. Another distorted cognition that results from self-focus is the “personal fable,” where an adolescent believes that they are unique and invulnerable to the same penalties as others [49]. This has obvious consequences for illness self-management in that an individual who does not believe that nonadherence to their medical regimen will cause harm is more likely to demonstrate poor adherence. This is at the heart of the Health Belief Model [6] and may be especially relevant for treatment regimens that are burdensome [55].
Erikson’s stages of psychosocial development is another classic developmental theory that can be applied to adolescent illness self-management [56]. Erikson theorized that the major personality achievement of adolescence is the development of “identity.” This includes making decisions about what defines you, your values, and your life goals [49]. During this stage, adolescents move away from family and spend more time with friends, and peer support plays a central role. This has important consequences for medical regimen adherence because improved adherence in adolescence has been positively related to more parental involvement and shared treatment responsibility across a wide range of medical illnesses [10], including asthma [46] and CF [45]. In contrast, evidence whether peer support results in improved adherence has been mixed [10]. No changes in adherence to asthma controller medication were found in adolescents participating in a peer coping support group compared to the control group [57].
Although family involvement appears to play a critical role in illness self-management into adolescence, the development of supportive friendships and peer support is critical to achieving identity as theorized by Erikson [49]; and prosocial peer support may buffer against feelings of self-consciousness, indirectly promoting adherence [58, 59]. There is some evidence that individuals with chronic lung disease may have more social withdrawal and poorer friendship quality including among those with neuromuscular disease requiring home ventilation [31], CF [60], and asthma [61]. Further, peer rejection has been found to play a significant role in the increased risk for adolescent depression [62], which in itself is related to worse illness self-management [63, 64].
Psychosocial Distress and Illness Self-Management
AYA psychosocial distress is another individual variable that negatively impacts illness self-management. Although psychosocial distress is typically modifiable, an AYA’s exposure to life stress or “negative life events” is not and has important long-term consequences [65]. Specifically, stress exposure has been related to poor health outcomes in asthma [66]. Further, exposure to acute stress results in physiological symptoms, such as bronchoconstriction, that can be harmful to those with lung disease [67].
Chronic stress can also contribute to internalizing symptoms, such as mood and anxiety disorders. Adolescents with chronic illness are, as a group, at higher risk for depressive and anxiety symptoms [68, 69]. Among AYAs with chronic lung disease, higher rates of anxiety and depression symptoms have been identified in those with CF [70] and asthma [71]. Much less is known about internalizing symptoms among children requiring home ventilation. Preliminary data from one study suggests that 77% of children were rated by their parents as having “excellent” or “good” emotional adjustment and 82% were “seldom” or “only sometimes” depressed, although parent-reported symptoms of depression were significantly higher among adolescents than younger children [72]. Data among children receiving lung transplant is also limited. One study examined depression symptoms among children pre- and post-heart-lung transplant. They found that 31% of children were rated above the cutoff on a depression screener pre-transplant, which was significantly higher than populations estimate, while only 13% were rated above the cutoff post-transplant [73].
Internalizing symptoms play an important role in illness self-management for individuals with chronic lung disease. The presence of these symptoms has been identified as a barrier to medical regimen adherence in CF [63] and has been associated with increased asthma symptomology [74]. However, the role of anxiety symptoms has been mixed in that some studies have shown that increased anxiety among children is related to improvements in medical regimen adherence [75], including among those with CF [76].
Similar to internalizing symptoms, the presence of externalizing symptoms (disruptive behaviors) can impact illness self-management. Rates of externalizing symptoms among those with chronic lung disease may vary by disease type, and studies are generally focused on school-aged or younger children. Among children with CF, mean externalizing behaviors have not been found to differ significantly from community samples on broad-based measures such as the Child Behavior Checklist [77]. However, children with asthma have been found to have more disruptive behaviors than community samples [78]. Further, children with more severe asthma were found to be at higher risk for oppositional behaviors into later childhood and adolescence [79]. Rates of disruptive behaviors among those requiring home ventilation and who have received lung transplantation appear to be largely unknown.
Although rates of disruptive behaviors differ among chronic illness groups, illness self-management may be problematic for those demonstrating elevations [80]. Among school-aged children with CF and asthma, child oppositional behavior was the barrier most frequently cited by caregivers as impacting respiratory treatment adherence [81]. Further, direct observation of children with CF completing respiratory treatments found that child cooperation during individual treatments was related to higher respiratory adherence rates over 3 months [82]. These preliminary findings support that disruptive behaviors may be another important psychosocial variable impacting adherence and may be a useful intervention target.
Best Practices for Assessing and Promoting Illness Self-Management in AYA
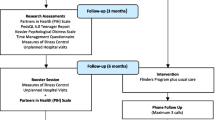
Taken together, the transition to independent illness self-management among AYA is a complex process full of potential developmental and psychosocial barriers. However, screening and assessment of these barriers, and clinical intervention focused on promoting knowledge and skill development, should be considered the best practice during the transition period [2]. Models of illness self-management suggest that key factors to the understanding of transition from pediatric to adult healthcare include recognizing that change happens in stages over time, involves systemic influences, and includes many barriers [4, 6, 7]. Further, focusing intervention on modifiable factors is optimal [4]. Models of healthcare transition suggest that aspects of illness self-management, including medical-related knowledge and medical regimen adherence, are modifiable individual influences that are crucial to optimizing transition readiness [1].
Although developmental change during adolescence is not modifiable, interventions can be tailored based on known developmental challenges for the purpose of improving knowledge and adherent behaviors. Education should be tailored based on the individual developmental level of the AYA while ensuring understanding through teach-back methods [83] and skill demonstration [84]. Further, independence and increased responsibility should not be granted based on age, but on behavior that is closely supervised by caregivers [45, 46]. Adolescent feelings of self-consciousness and the desire for increased peer engagement can be addressed through frank discussions of the adolescent’s preferences regarding disclosure of illness and coaching on how to share this information [85]. An adolescent’s belief in their uniqueness can be accommodated by ensuring that they are part of medical decision-making in a developmentally appropriate manner [86]. Finally, an adolescent’s feeling of invulnerability can be addressed by careful screening of risk-taking behaviors [87] and ensuring that safety nets (typically caregivers) are in place while an adolescent is transitioning to independent self-management behaviors.
In contrast to developmental level, psychosocial distress in AYA is an area that is amenable to change. Empirically-supported treatment for adolescent mood and anxiety disorders includes cognitive-behavioral therapy; and treatment for disruptive behaviors includes behavioral management training and multisystemic family therapy [88]. Psychotropic medication evaluation by appropriate child pychiatric specialists should also be considered for mood and disruptive behaviors that are clinically significant [89]. Treatment of adjustment to illness and chronic life stress may include training in health promotion strategies and intervention to boost factors related to resilience [90].
Illness self-management should be routinely screened while meeting with AYAs without caregivers present. Screening should begin by assuming nonadherence and asking specific questions related to doses missed over a certain time frame. The best practice in medical regimen adherence measurement suggests that multiple methods and sources of information should be integrated, including self-report, medical variables, electronic methods if available, and co-informants such as caregivers [91]. Screening should also include assessment of common barriers such as avoidance, forgetting, and time management [92].
Depending on supports available in the clinic, optimal screening may also include screening for mood, anxiety, or behavioral disorders [93]. A number of national organizations supporting children with chronic illness recommend routine depression and anxiety screening beginning in adolescence, including the American Diabetes Association [94]; the North American Society For Pediatric Gastroenterology, Hepatology, and Nutrition [95]; and the Cystic Fibrosis Foundation [70]. The American Academy of Pediatrics also recommends depression screening in adolescence and points out that those with chronic illness, including asthma, should be considered higher risk [96].
Data obtained from screening methods can then be used to implement in-clinic interventions designed to promote AYA illness self-management behaviors. As previously reviewed, intervention should include education along with behavioral strategies. This may include reminders (including the use of technology), problem-solving, increased family involvement and monitoring, and follow-up/accountability on the part of the AYA [10]. In general, multicomponent interventions may be the most effective, although effect sizes for adherence interventions, to date, are generally small [97]. Interventions delivered in-clinic may be sufficient for some AYA, but for those that are experiencing multiple life stressors, clinically significant mood or behavioral concerns, or for whom poor illness self-management is a chronic problem, referral to a health psychologist is recommended.
Conclusion
Developmental and psychosocial challenges to illness self-management during transition are common but unique to each individual patient. Understanding of common barriers can help providers know how to screen for and address self-management challenges. Additionally, focus on ensuring illness-related knowledge and bolstering medical regimen adherence throughout childhood into early adolescence may result in a smoother transition during AYA. Adding illness self-management screening and intervention strategies into clinical care can help an AYA’s transition experience to be a thrilling, but ultimately successful, ride.
References
Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37(6):883–95.
Blum RW, Hirsch D, Kastner TA, Quint RD, Sandler AD, Anderson SM, et al. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304–6.
Campbell F, Biggs K, Aldiss SK, O’Neill PM, Clowes M, Mcdonagh J, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev. 2016;4:CD009794.
Modi AC, Pai AL, Hommel KA, Hood KK, Cortina S, Hilliard ME, et al. Pediatric self-management: a framework for research, practice, and policy. Pediatrics. 2012;129:e473–85.
La Greca AM, Bearman KJ. Adherence to pediatric treatment regimens. In: Handbook of pediatric psychology. 3rd ed. New York: The Guilford Press; 2003. p. 119–40.
Becker MH, Drachman RH, Kirscht JP. Predicting mothers’ compliance with pediatric medical regimens. J Pediatr. 1972;81:843–54.
Prochaska, JO, DiClemente CC. The transtheoretical approach: Crossing traditional boundaries of therapy. Homewood, Ill: Dow Jones-Irwin, 1984.
Lozano P, Houtrow A. Supporting self-management in children and adolescents with complex chronic conditions. Pediatrics. 2018;141:S233–41.
Graves MM, Roberts MC, Rapoff M, Boyer A. The efficacy of adherence interventions for chronically ill children: a meta-analytic review. J Pediatr Psychol. 2010;35:368–82.
Hommel KA, Ramsey RR, Rich KL, Ryan JL. Adherence to pediatric treatment regimens. In: Handbook of pediatric psychology. 5th ed. New York: The Guilford Press; 2017. p. 119–33.
Haynes R. Introduction. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in health care. Baltimore: John’s Hopkins University Press; 1979.
Pai ALH, Ostendorf HM. Treatment adherence in adolescents and young adults affected by chronic illness during the health care transition from pediatric to adult health care: a literature review. Child Health Care. 2011;40:16–33.
Jones MR, Frey SM, Riekert K, Fagnano M, Halterman JS. Transition readiness for talking with providers in urban youth with asthma: associations with medication management*. J Adolesc Health. 2019;64:265–71.
Patel A, Dowell M, Giles BL. Current concepts of transition of care in cystic fibrosis. Pediatr Ann. 2017;46:e188–92.
Agarwal A, Willis D, Tang X, Bauer M, Berlinski A, Com G, et al. Transition of respiratory technology dependent patients from pediatric to adult pulmonology care. Pediatr Pulmonol. 2015;50:1294–300.
Taylor L, Tsang A, Drabble A. Transition of transplant patients with cystic fibrosis to adult care: today’s challenges. Prog Transplant. 2006;16:329–34.
Gold A, Martin K, Breckbill K, Avitzur Y, Kaufman M. Transition to adult care in pediatric solid-organ transplant: development of a practice guideline. Prog Transplant. 2015;25:131–8.
Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ - transition readiness assessment questionnaire. J Pediatr Psychol. 2011;36:160–71.
Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, et al. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14:415–22.
Sawicki GS, Kelemen S, Weitzman ER. Ready, set, stop: mismatch between self-care beliefs, transition readiness skills, and transition planning among adolescents, young adults, and parents. Clin Pediatr (Phila). 2014;53:1062–8.
Gilleland J, Amaral S, Mee L, Blount R. Getting ready to leave: transition readiness in adolescent kidney transplant recipients. J Pediatr Psychol. 2012;37:85–96.
Devine K, Monaghan M, Schwartz L. Transition in pediatric psychology: adolescents and young adults. In: Handbook of pediatric psychology. New York: The Guilford Press; 2017. p. 620–31.
Davis AM, Brown RF, Taylor JL, Epstein RA, McPheeters ML. Transition care for children with special health care needs. Pediatrics. 2014;134:900–8.
Masterson TL, Wildman BG, Newberry BH, Omlor GJ. Impact of age and gender on adherence to infection control guidelines and medical regimens in cystic fibrosis. Pediatr Pulmonol. 2011;46:295–301.
Carbone L, Zebrack B, Plegue M, Joshi S, Shellhaas R. Treatment adherence among adolescents with epilepsy: what really matters? Epilepsy Behav. 2013;27:59–63.
McNally K, Rohan J, Pendley JS, Delamater A, Drotar D. Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care. 2010;33:1159–62.
Irani F, Barbone JM, Beausoleil J, Gerald L. Is asthma associated with cognitive impairments? A meta-analytic review. J Clin Exp Neuropsychol. 2017;39:965–78.
Rosas-Salazar C, Apter AJ, Canino G, Celedón JC. Health literacy and asthma. J Allergy Clin Immunol. 2012;129:935–42.
Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. J Gen Intern Med. 2006;21:813–7.
Schwengel DA, Dalesio NM, Stierer TL. Pediatric obstructive sleep apnea. Anesthesiol Clin. 2014;32:237–61.
Snow WM, Anderson JE, Jakobson LS. Neuropsychological and neurobehavioral functioning in Duchenne muscular dystrophy: a review. Neurosci Biobehav Rev. 2013;37:743–52.
Sasannejad C, Ely EW, Lahiri S. Long-term cognitive impairment after acute respiratory distress syndrome: a review of clinical impact and pathophysiological mechanisms. Crit Care. 2019;23:352.
Koltsida G, Konstantinopoulou S. Long term outcomes in chronic lung disease requiring tracheostomy and chronic mechanical ventilation. Semin Fetal Neonatal Med. 2019;24:101044.
Piasecki B, Turska-Malińska R, Matthews-Brzozowska T, Mojs E. Executive function in pediatric patients with cystic fibrosis, inflammatory bowel disease and in healthy controls. Eur Rev Med Pharmacol Sci. 2016;20:4299–304.
Wray J, Radley-Smith R. Beyond the first year after pediatric heart or heart-lung transplantation: changes in cognitive function and behaviour. Pediatr Transplant. 2005;9:170–7.
McGrady ME, Hommel KA. Medication adherence and health care utilization in pediatric chronic illness: a systematic review. Pediatrics. 2013;132:730–40.
Drotar D, Bonner MS. Influences on adherence to pediatric asthma treatment: a review of correlates and predictors. J Dev Behav Pediatr. 2009;30:574–82.
Quittner AL, Zhang J, Marynchenko M, Chopra PA, Signorovitch J, Yushkina Y, et al. Pulmonary medication adherence and health-care use in cystic fibrosis. Chest. 2014;146:142–51.
Amin R, Al-Saleh S, Narang I. Domiciliary noninvasive positive airway pressure therapy in children. Pediatr Pulmonol. 2016;51:335–48.
Killian MO. Psychosocial predictors of medication adherence in pediatric heart and lung organ transplantation. Pediatr Transplant. 2017. http://orcid.org/000.-0002-2287-9007.
Sawicki GS, Ostrenga J, Petren K, Fink AK, D'Agostino E, Strassle C, Schechter MS, Rosenfeld M. Risk factors for gaps in care during transfer from pediatric to adult cystic fibrosis programs in the united states. Ann Am Thorac Soc. 2018;15(2):234–40. https://doi.org/10.1513/AnnalsATS.201705-357OC.
Oates GR, Stepanikova I, Gamble S, Gutierrez HH, Harris WT. Adherence to airway clearance therapy in pediatric cystic fibrosis: socioeconomic factors and respiratory outcomes. Pediatr Pulmonol. 2015;50:1244–52.
Barker DH, Quittner AL. Parental depression and pancreatic enzymes adherence in children with cystic fibrosis. Pediatrics. 2016;137:e20152296.
Wood BL, Brown ES, Lehman HK, Khan DA, Lee MJ, Miller BD. The effects of caregiver depression on childhood asthma: pathways and mechanisms. Ann Allergy Asthma Immunol. 2018;121:421–7.
Modi AC, Marciel KK, Slater SK, Drotar D, Quittner AL. The influence of parental supervision on medical adherence in adolescents with cysticfibrosis: Developmental shifts from pre to late adolescence. Children’s Health Care. 2008;37(1):78–82. https://doi.org/10.1080/02739610701766925.
Duncan CL, Hogan MB, Tien KJ, Graves MM, Chorney JML, Zettler MD, et al. Efficacy of a parent-youth teamwork intervention to promote adherence in pediatric asthma. J Pediatr Psychol. 2013;38:617–28.
Gill D, Sheehan NA, Wielscher M, Shrine N, Amaral AFS, Thompson JR, et al. Age at menarche and lung function: a Mendelian randomization study. Eur J Epidemiol. 2017;32:701–10.
Sutton S, Rosenbluth D, Raghavan D, Zheng J, Jain R. Effects of puberty on cystic fibrosis related pulmonary exacerbations in women versus men. Pediatr Pulmonol. 2014;49:28–35.
Berk LE. Development through the lifespan, 6/e © 2014. Development; 2014.
Inhelder B, Piaget J. An essay on the construction of formal operational structures. In: The growth of logical thinking: from childhood to adolescence. New York: Basic Books; 1958.
DeLambo KE, Ievers-Landis CE, Drotar D, Quittner AL. Association of observed family relationship quality and problem-solving skills with treatment adherence in older children and adolescents with cystic fibrosis. J Pediatr Psychol. 2004;29:343–53.
Quittner AL, Eakin MN, Alpern AN, Ridge AK, McLean KA, Bilderback A, et al. Clustered randomized controlled trial of a clinic-based problem-solving intervention to improve adherence in adolescents with cystic fibrosis. J Cyst Fibros. 2019;18:879–85.
Dziuban EJ, Saab-Abazeed L, Chaudhry SR, Streetman DS, Nasr SZ. Identifying barriers to treatment adherence and related attitudinal patterns in adolescents with cystic fibrosis. Pediatr Pulmonol. 2010;45:450–8.
Mulvaney SA, Ho YX, Cala CM, Chen Q, Nian H, Patterson BL, et al. Assessing adolescent asthma symptoms and adherence using mobile phones. J Med Internet Res. 2013;15:e141.
Bishay LC, Sawicki GS. Strategies to optimize treatment adherence in adolescent patients with cystic fibrosis. Adolesc Health Med Ther. 2016;7:117–24.
Erikson EH. Identity, youth and crisis. New York: WW Norton Company, 1968.
Mosnaim G, Li H, Martin M, Richardson DJ, Belice PJ, Avery E, et al. The impact of peer support and mp3 messaging on adherence to inhaled corticosteroids in minority adolescents with asthma: a randomized, controlled trial. J Allergy Clin Immunol Pract. 2013;1:485–93.
Janicke DM, Gray WN, Kahhan NA, Follansbee Junger KW, Marciel KK, Storch EA, et al. Brief report: the association between peer victimization, prosocial support, and treatment adherence in children and adolescents with inflammatory bowel disease. J Pediatr Psychol. 2009;34:769–73.
Helms SW, Dellon EP, Prinstein MJ. Friendship quality and health-related outcomes among adolescents with cystic fibrosis. J Pediatr Psychol. 2015;40:349–58.
Kostakou K, Giannakopoulos G, Diareme S, Tzavara C, Doudounakis S, Christogiorgos S, et al. Psychosocial distress and functioning of Greek youth with cystic fibrosis: a cross-sectional study. Biopsychosoc Med. 2014;8:13.
Baker SE, Niec LN, Meade J. A comparison of friendship quality and social functioning among children with perinatally acquired HIV, children with persistent asthma, and healthy children of HIV-positive mothers. J Pediatr Psychol. 2012;37:580–90.
Platt B, Kadosh KC, Lau JYF. The role of peer rejection in adolescent depression. Depress Anxiety. 2013;30:809–21.
Hilliard ME, Eakin MN, Borrelli B, Green A, Riekert KA. Medication beliefs mediate between depressive symptoms and medication adherence in cystic fibrosis. Health Psychol. 2015;34:496–504.
McCormick King ML, Mee LL, Gutiérrez-Colina AM, Eaton CK, Lee JL, Blount RL. Emotional functioning, barriers, and medication adherence in pediatric transplant recipients. J Pediatr Psychol. 2014;39:283–93.
Marum G, Clench-Aas J, Nes RB, Raanaas RK. The relationship between negative life events, psychological distress and life satisfaction: a population-based study. Qual Life Res. 2014;23:601–11.
Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2005;5:23–9.
McQuaid EL, Fritz GK, Nassau JH, Lilly MK, Mansell A, Klein RB. Stress and airway resistance in children with asthma. J Psychosom Res. 2000;49:239–45.
Pinquart M, Shen Y. Depressive symptoms in children and adolescents with chronic physical illness: an updated meta-analysis. J Pediatr Psychol. 2011;36:375–84.
Pinquart M, Shen Y. Anxiety in children and adolescents with chronic physical illnesses: a meta-analysis. Acta Paediatrica Int J Paediatr. 2011;100:1069–76.
Quittner AL, Abbott J, Georgiopoulos AM, Goldbeck L, Smith B, Hempstead SE, et al. International committee on mental health in cystic fibrosis: Cystic Fibrosis Foundation and European cystic fibrosis society consensus statements for screening and treating depression and anxiety. Thorax. 2016;71:26–34.
Lu Y, Mak KK, van Bever HPS, Ng TP, Mak A, Ho RCM. Prevalence of anxiety and depressive symptoms in adolescents with asthma: a meta-analysis and meta-regression. Pediatr Allergy Immunol. 2012;23:707–15.
Lumeng JC, Warschausky SA, Nelson VS, Augenstein K. The quality of life of ventilator-assisted children. Pediatr Rehabil. 2001;4:21–7.
Wray J, Radley-Smith R. Depression in pediatric patients before and 1 year after heart or heart-lung transplantation. J Heart Lung Transplant. 2004;23:1103–10.
Richardson LP, Lozano P, Russo J, McCauley E, Bush T, Katon W. Asthma symptom burden: relationship to asthma severity and anxiety and depression symptoms. Pediatrics. 2006;118:1042–51.
Wu YP, Aylward BS, Steele RG. Associations between internalizing symptoms and trajectories of medication adherence among pediatric renal and liver transplant recipients. J Pediatr Psychol. 2010;35:1016–27.
White T, Miller J, Smith GL, McMahon WM. Adherence and psychopathology in children and adolescents with cystic fibrosis. Eur Child Adolesc Psychiatry. 2009;18:96–104.
Sheehan J, Massie J, Hay M, Jaffe A, Glazner J, Armstrong D, et al. The natural history and predictors of persistent problem behaviours in cystic fibrosis: a multicentre, prospective study. Arch Dis Child. 2012;97:625–31.
McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: a meta-analysis. J Dev Behav Pediatr. 2001;22:430–9.
Goodwin RD, Robinson M, Sly PD, McKeague IW, Susser ES, Zubrick SR, et al. Severity and persistence of asthma and mental health: a birth cohort study. Psychol Med. 2013;43:1313–22.
Malee K, Williams P, Montepiedra G, McCabe M, Nichols S, Sirois PA, et al. Medication adherence in children and adolescents with HIV infection: associations with behavioral impairment. AIDS Patient Care STDS. 2011;25:191–200.
Modi AC, Quittner AL. Barriers to treatment adherence for children with cystic fibrosis and asthma: what gets in the way? J Pediatr Psychol. 2006;31:846–58.
Butcher JL, Nasr SZ. Direct observation of respiratory treatments in cystic fibrosis: parent-child interactions relate to medical regimen adherence. J Pediatr Psychol. 2015;40:8–17.
Ha Dinh TT, Bonner A, Clark R, Ramsbotham J, Hines S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: a systematic review. JBI Database System Rev Implement Rep. 2016;14:210–47.
Mosnaim GS, Pappalardo AA, Resnick SE, Codispoti CD, Bandi S, Nackers L, et al. Behavioral interventions to improve asthma outcomes for adolescents: a systematic review. J Allergy Clin Immunol Pract. 2016;4:130–41.
Venetis MK, Chernichky-Karcher S, Gettings PE. Disclosing mental illness information to a friend: exploring how the disclosure decision-making model informs strategy selection. Health Commun. 2018;33:653–63.
Grootens-Wiegers P, Hein IM, van den Broek JM, de Vries MC. Medical decision-making in children and adolescents: developmental and neuroscientific aspects. BMC Pediatr. 2017;17:120.
Klein DA, Paradise SL, Landis CA. Screening and counseling adolescents and young adults: a framework for comprehensive care. Am Fam Physician. 2020;101:147–58.
Christophersen ER, VanScoyoc SM. Treatments that work with children: empirically supported strategies for managing childhood problems. 2nd ed. Washington, DC: American Psychological Association; 2013.
Strawn JR, Dobson ET, Giles LL. Primary pediatric care psychopharmacology: focus on medications for ADHD, depression, and anxiety. Curr Probl Pediatr Adolesc Health Care. 2017;47:3–14.
Aujoulat I, Dechêne S, Lahaye M. Non-disease specific health promotion interventions for chronically ill adolescents in medical settings: a systematic review. Front Public Health. 2018;6:301.
Quittner AL, Espelage DL, Ievers-Landis C, Drotar D. Measuring adherence to medical treatments in childhood chronic illness: considering multiple methods and sources of information. J Clin Psychol Med Settings. 2000;7:41–54.
Quittner AL, Pedreira PB, Bernstein R, McLean LA, Nicolais CJ, Saez-Flores E, Riekert KA. Development of the adherence barriers questionnaire-cystic fibrosis (ABQ-CF): frequently endorsed barriers from openended interviews. Pediatr Pulmonol. 2016;51:465.
Quittner AL, Abbott J, Hussain S, Ong T, Uluer A, Hempstead S, et al. Integration of mental health screening and treatment into cystic fibrosis clinics: evaluation of initial implementation in 84 programs across the United States. Pediatr Pulmonol. 2020;55:2995–3004.
American Diabetes Association. Standards of Medical Care in Diabetes, 2018. Diabetes Care 2018;41(Suppl. 1).
Rufo PA, Denson LA, Sylvester FA, Szigethy E, Sathya P, Lu Y, et al. Health supervision in the management of children and adolescents with IBD: NASPGHAN recommendations. J Pediatr Gastroenterol Nutr. 2012;55:93–108.
Zuckerbrot RA, Cheung A, Jensen PS, REK S, Laraque D. Guidelines for adolescent depression in primary care (GLAD-PC): part I. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018;141:e20174081.
Pai ALH, McGrady M. Systematic review and meta-analysis of psychological interventions to promote treatment adherence in children, adolescents, and young adults with chronic illness. J Pediatr Psychol. 2014;39:918–31.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Butcher, J.L. (2021). Developmental and Psychosocial Challenges for Self-Management and Maintaining Adherence to Chronic Therapies. In: Brown, C.D., Crowley, E. (eds) Transitioning Care from Pediatric to Adult Pulmonology. Respiratory Medicine. Humana, Cham. https://doi.org/10.1007/978-3-030-68688-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-68688-8_4
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-68687-1
Online ISBN: 978-3-030-68688-8
eBook Packages: MedicineMedicine (R0)