Abstract
The incidence of accidental exposure and intoxication in pets is increasing with the rise in popularity and accessibility to cannabis and cannabinoid-containing products marketed for use in both pets and people. Exposure to synthetic cannabinoids is a growing concern as well. While the overall prognosis for unintentional exposures remains good, pets will no doubt receive more timely treatment from veterinarians who can quickly recognize the clinical signs associated with intoxication, understand when cases have the potential to become severe, and are aware of treatment protocols. This chapter encompasses the following: a brief outline of cannabinoid products and the endocannabinoid system; a summary of current published studies investigating the effects of cannabidiol (CBD) or delta-9-tetrahydrocannabinol (THC) including reported adverse effects; clinical signs of intoxication in dogs and cats as reported in the literature and to animal poison control centers; toxic doses of cannabinoids; and medical treatment approaches to cannabis intoxication in pets.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cannabis
- Medical marijuana
- THC
- CBD
- Cannabinoid
- Marijuana concentrates
- Synthetic cannabinoids
- Poisoning
- Toxicity
- Adverse effects
3.1 Introduction
Along with the increased popularity and accessibility to cannabis, the incidence of accidental exposure and intoxication in pets, as reported to Pet Poison Helpline, a 24/7 animal poison control center serving the United States (US) and Canada, has increased dramatically. With accidental pet intoxication on the rise, it is imperative for veterinary professionals to understand how the common types of cannabis products can impact their patients following intentional or inadvertent exposure. This chapter will review cannabinoid containing products along with synthetic marijuana products (synthetic cannabinoids or SCBs) which are illegal substances with a much greater affinity for cannabinoid receptors.
As therapeutic benefits of cannabinoids come to light and societal perceptions change, veterinary professionals are expected to see a continued increase in legalization and decriminalization of marijuana and individual cannabinoids, and thus likely to see an increase in inadvertent companion animal exposure and intoxication.
3.2 A Brief History of Cannabis
For many centuries, cannabis plants have been used to treat various ailments, for their psychotropic or intoxicating properties/recreational use, and in religious ceremonies. The use of cannabis for medical purposes is recorded back to 2700–2600 BCE for treatment of various maladies including constipation, rheumatic pain, malaria, menstrual health, venereal disease, headaches, fever reduction, appetite stimulation, and as a sleep aid. Use for these ailments continued well into the nineteenth century, particularly in 1839 when Irish physician W.B. O’Shaughnessy began investigating its usefulness in the treatment of seizures, tetanus, rabies, and rheumatism in animal studies. He recognized its benefits as an antispasmodic agent with anxiolytic and antiemetic properties, although he also noted side effects such as catalepsy (Adams and Martin 1996).
Over the last 60 years, scientists have gained considerable knowledge on the topic of the cannabis plant and its cannabinoid compounds. Delta-9-tetrahydrocannabinol, or THC, was identified as the major psychoactive cannabinoid in 1964 (Marzo et al. 2004). The structure of cannabidiol or CBD, the primary non-intoxicating cannabinoid, was discovered in 1963 (Long et al. 2005). The design of enantiomerically pure analogues or synthetic varieties of THC began in the 1960s in both the pursuit of analgesics and of endogenous receptors presumed present in mammals at which THC, CBD, and other cannabinoids act (Marzo et al. 2004; Obafemi et al. 2015). Cannabinoid receptors were discovered in 1988 and specific receptors CB1 and CB2 were cloned in 1990 and 1993 respectively, at which time they were identified as G-protein coupled receptors affected by endogenous cannabinoids, termed endocannabinoids, during the early 1990s (Marzo et al. 2004).
Marijuana and synthetic cannabinoids have progressed to be the most widely used illicit drugs in the world, and, over the past 60 years, most countries categorized them as drugs of abuse. However, the more recent legal fluidity of plant-based cannabinoids production and processing for sale is rapidly evolving. Synthetic cannabinoid varieties developed to mimic THC have also gained popularity for their intoxicating properties, most notably since 2009 (Obafemi et al. 2015).
Although considered a drug of abuse, the therapeutic benefits of THC specifically have not been ignored. Since the 1980s, synthetic THC-based medications dronabinol (Marinol®) and analogue nabilone (Cesamet®) have been used in treatment of inappetence and nausea in chemotherapy and AIDS patients (Janczyk et al. 2004; Marzo et al. 2004). In 2010, Sativex®, a 1:1 ratio of THC:CBD, was approved in many European countries as an oromucosal spray for treatment of spasticity due to multiple sclerosis. As of 2020, the drug was approved by more than 25 countries around the globe, including Canada, Israel, Australia, New Zealand, and in Latin America, but not in the US. In 2018, Epidiolex® (cannabidiol) was approved in the US by FDA for the treatment of seizures associated with two rare forms of human epilepsy (Greenwich Biosciences 2018).
3.3 The Endocannabinoid System Review
The endocannabinoid system is akin to the endogenous opioid system in which opioid receptors (i.e., delta, kappa, mu) are activated by endogenous opioid peptides (e.g., endorphins). Mammals have cannabinoid receptors in plasma membranes that are activated by endogenous ligands called endocannabinoids. The endocannabinoid system encompasses complex intracellular signaling including enzymes for ligand biosynthesis and inactivation. It plays a physiological role in several systems, namely neurological, inflammatory, and immune.
Anandamide (AEA) and 2-Arachidonoylglycerol (2-AG) are the two most commonly recognized and studied endocannabinoids. Both are produced “on demand” in response to stress. These endocannabinoids bind to G-protein coupled receptors and perform several neurotransmission functions, including inhibition (mostly) of adenylate cyclase, inhibition of voltage-gated calcium channels, stimulation of protein kinases, and stimulation of potassium channels. Receptor binding and subsequent effects ultimately translate into biological responses within a complex system designed for modulating neurotransmitter release (Marzo et al. 2004).
The primary targets for endocannabinoids and THC are cannabinoid receptors 1 and 2 (CB1 and CB2). These receptors are present on the postsynaptic neuron and act via retrograde synaptic signaling mechanisms to inhibit neurotransmitter release from presynaptic neurons (Pirone et al. 2015). Endocannabinoids are synthesized, as needed, from membrane phospholipids to act in an autocrine (upon the same cell) or paracrine (upon nearby cells) fashion and are quickly inactivated via hydrolysis after internalization into the cell (Marzo et al. 2004; Murray et al. 2007).
Endocannabinoids are 4-20 × less potent than THC and have a significantly shorter duration of action (Adams and Martin 1996). Administration of exogenous cannabinoids such as THC or synthetic analogues will disrupt the subtle endocannabinoid signaling process and may result in the common THC tetrad of delusions, hallucinations, paranoia, and sedation (Adams and Martin 1996; Murray et al. 2007).
-
CB1 receptors
-
Primarily located in the central nervous system (CNS) with lower concentrations in the peripheral nervous system (PNS).
-
In the CNS, CB1 is involved in cognitive function, emotion, motion/movement, hunger, and neuroprotection in both post-traumatic events and degenerative diseases.
-
Sensory and autonomic CB1 receptors are involved in pain perception, cardiovascular, gastrointestinal, and respiratory effects.
-
CB1 is responsible for the psychotropic effects of THC.
-
Activation inhibits retrograde release of acetylcholine, dopamine, GABA, serotonin, histamine, glutamate, and/or noradrenaline, among others.
-
-
CB2 receptors
Cannabinoid receptors are found in abundance within the epithelial tissues of the developing embryo with highest concentrations in the nervous system, sensory organs, and thyroid tissue. CB1 is important in the normal neuronal differentiation and axonal growth during neuronal development. The developed animal has highest CB1 concentration in the basal ganglia and cerebellum (Pirone et al. 2015). Endocannabinoid signaling is required for motor learning in the cerebellum, extinction of aversive memories in the amygdala, and as an aid in memory encoding.
For an in-depth understanding of the endocannabinoid system and receptor physiology, please see Chaps. 1 and 2 of this book.
3.4 Toxicity of Δ9-THC
THC, the primary intoxicating cannabinoid in the cannabis plant, is found in a range of products and formulations including edibles, oils, tinctures, topical salves/balms/etc., capsules, vaping liquids, hashish, and “concentrates”. It is also the compound upon which the potency of cannabis products, especially plants used for recreational purposes, is traditionally measured (Obafemi et al. 2015).
Other forms of THC can be found in the cannabis plant including THCA (tetrahydrocannabinolic acid) and THCV (tetrahydrocannabivarin), which are not intoxicating. Whereas new forms of the THC molecule, including THCB (Δ9-tetrahydrocannabutol) and THCP (tetrahydrocannabiphorol), in more recently discovered cultivars are dramatically more potent than the popular Δ9-THC. While not readily available on the legal or black market, these newly discovered cannabinoids may be a potential intoxicating substance to consider in the near future.
The concentration of THC in cultivated cannabis plants has increased in the US, mostly as a result of cross-breeding and hydroponic year-round growing operations (Adams and Martin 1996). In the 1960s, the average concentration of THC in cannabis plants was 1.5%, rising to 3.5% by the mid 1980s (ElSohly et al. 2016). As of 1995 and 2014, concentrations in plants used for recreational purposes increased from 4% to 12%, respectively, while the concentration of CBD simultaneously declined from 0.28% to <0.15% (ElSohly et al. 2016). This increase in potency correlates with a shift in production from cannabis to sinsemilla which are unpollinated, sterile flowering tops from the cultivated female cannabis plant. Sinsemilla is more potent than traditional marijuana and is gaining popularity in the US, presumably due to demand for plants with greater psychoactive effects (Adams and Martin 1996; ElSohly et al. 2016). In cannabis plants, THC is most concentrated in the flowering buds, followed by the leaves, stems and roots. The seeds do not contain notable levels of THC (Adams and Martin 1996).
The dose of THC found in cannabis products varies greatly with formulation. Marijuana joints (cigarettes) typically contain 0.5–1 g of plant material with THC concentrations varying from 0.4 to 20%. The average 1 g joint contains 150 mg of THC (Raber et al. 2015).
Commercial edible products may also contain widely varying amounts of THC, although typical doses for adults are ~10 mg per serving. The most common commercial edible products are chocolates and gummies. Brownies or cookies made using “marijuana butter” or various cooking oils that have been used to extract the lipid soluble THC from plant matter, are both commercially available and readily made at home. Marijuana butter/oil can contain very high concentrations of THC and pose a greater risk for poisoning than ingestion of plant material alone. Additionally, chocolate present in food may also lead to intoxication in pets. Human foods that also pose risk for poisoning in dogs are xylitol, grapes/raisins, and macadamia nuts. Other commonly sold THC containing food products are truffles, caramels, lollipops/hard candies, ice cream, savory baked goods, beverages, etc. Sachets of powdered THC intended to be added to foods and beverages are also available.
Processed cannabis products, referred to as “concentrates,” can contain >80–90% THC. These may be used recreationally or medically and require smaller doses to achieve stronger and more long-lasting effects compared to plant material. Concentrates come in varying formulations and compositions, sometimes divided into “hash”, concentrates made from dry or water based extractions, and techniques using solvents and CO2 (Raber et al. 2015). Hashish is a sticky resin collected from the flowering buds that may be shaped or formed into a cake, ball, sticks or slabs and typically contains about 10% THC. Hash oil is a liquid or semi-solid with a higher THC concentration than hashish, typically 20–50%.
Solvent-based concentrates are increasingly common products, often recreational, and made by soaking plant material in various solvents which are then boiled off. Such products are typically called RSO (Rick Simpson Oil) as an homage to the person who popularized the technique. Other names for solvent-based concentrates include “butane hash oil” (BHO), “honey oil,” “honeycomb,” “wax,” “shatter,” “budder”, “errl”, and “CO2 oil”. Together, these may be collectively referred to as “dabs”, the act of which inhaling them is called “dabbing” or “doing a dab” (Raber et al. 2015). In addition to containing THC, concentrates may be contaminated with high concentrations of solvents, pesticides, and other chemicals that can also complicate the clinical picture when ingested by pets.
3.4.1 Exposure Scenarios in Pets
The most common route of accidental exposure to cannabis products containing THC in companion animal patients is via ingestion, although some are exposed via inhalation from secondhand smoke or smoke intentionally blown in their face. Approximately 66% of the cannabis exposures reported to Pet Poison Helpline involve pets ingesting homemade or commercial edible goods (Pet Poison Helpline and SafetyCall International 2019—Database last accessed: 2019). The second most common source of cannabis exposures involve ingestion of plant material (~19%), followed by OTC medical cannabis preparations or prescription medications such as dronabinol and nabilone (~9%) (Pet Poison Helpline and SafetyCall International 2019—Database last accessed: 2019).
Legalization of both recreational and medical cannabis has also increased both the prevalence of and pet exposure to formulations such as vaping liquids, topical balms/salves/oils, and oral preparations such as oils, capsules, sublingual sprays, tinctures, etc. Doses and concentrations of such products can vary widely. Any of these products can also be mixed with other chemicals; a common example is the addition of peppermint essential oil to topical products.
3.4.2 Pharmacokinetics and Toxic Doses
For an in-depth discussion on pharmacokinetics of cannabis in dogs and cats, please see Chap. 2.
THC is readily absorbed when inhaled leading to a rapid onset of clinical signs. Absorption is slower and less predictable following ingestion. Consuming THC products with a fatty meal will increase absorption due to its lipophilic nature. The majority of THC is metabolized in the liver and undergoes enterohepatic recirculation, with a small amount excreted as metabolites in the urine (Fitzgerald et al. 2013). Due to its lipophilicity, THC is rapidly distributed into the tissues and crosses the blood-brain barrier (Sharma et al. 2012). This accounts for a short plasma but long biological half-life (Donaldson 2002). When large doses are ingested, it is not uncommon for animals, especially dogs, to remain symptomatic for 1–2 days. In rare cases, clinical signs may last 3–4 days as observed by Pet Poison Helpline.
The pharmacokinetic and toxic dose information listed below pertains to dogs unless otherwise indicated.
-
Suggested lethal dose >3–9 g plant material (THC dominant)/kg, but a real LD50 has not been established (Donaldson 2002) (https://www.tandfonline.com/doi/pdf/10.1080/24734306.2018.1434470, https://www.sciencedirect.com/science/article/pii/0041008X73903104?via%3Dihub)
-
Clinical signs in dogs (oral ingestion) starting at 0.3–0.4 mg/kg THC, possibly lower have been observed in Pet Poison Helpline cases; however, the reported doses in these cases is based on the package label which, due to lack of regulatory oversight, may not be accurate (Pet Poison Helpline and SafetyCall International 2019). (See Toxicity of CBD—Sect. 3.5 for more information.)
-
Tmax 1–2 h (oral)
-
Onset of signs: minutes (inhaled); 1–2 h (oral) (Pet Poison Helpline and SafetyCall International 2019)
-
Experimentally, in fasted dogs dosed orally with THC, the onset of neurological signs such as ataxia, tremors, hyperesthesia, hypothermia, and hypertonia were ~4 h post-dosing (Vaughn et al. 2020)
-
-
Excretion: 85% in feces via biliary excretion; 15% renally excreted
-
Half-life (biological): 30 h; 80% of THC is excreted within 5 days (Fitzgerald et al. 2013)
-
Clinical recovery after ingestion occurs within 24 h in most cases, potentially up to 72 h (Donaldson 2002; Pet Poison Helpline and SafetyCall International 2019)
Interactions between THC and CBD have been documented, with CBD often touted as an antagonist of THC; however, this is not always the case. Data suggest CBD can potentiate the psychoactive and physiological effects of THC as well. The exact mechanism(s) for interaction is still being investigated and depends on whether CBD is given before THC or the two are dosed simultaneously. The ratio of CBD to THC also plays a considerable role in expected signs, with higher dose ratios (e.g., 8.1) resulting in antagonistic effects of CBD on THC, whereas ratios of 1.5–1.8 have resulted in potentiation of effects from THC. Therefore, when THC is given simultaneously in combination with CBD, the dose at which adverse effects occur may be less than had an equivalent dose of THC been administered alone. This phenomenon was observed in a canine escalating dose study by Vaughn et al. which compared adverse effects in dogs divided into three groups: dogs dosed with CBD (~2–62 mg/kg), THC (~2–49 mg/kg), and CBD/THC (ratio 1.5:1, ~1.5 mg/kg CBD + 1 mg/kg THC to ~12 mg/kg CBD + 8 mg/kg THC) (Vaughn et al. 2020). Dogs in the CBD/THC arm experienced more severe adverse effects (severe ataxia and/or lethargy), resulting in cessation of dosing halfway through the trial, whereas dogs dosed with CBD alone or THC alone were allowed finish.
3.4.3 Clinical Signs of Poisoning
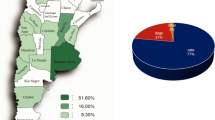
Exposure to THC is associated with a high morbidity but low mortality rate meaning that clinical signs are common, but death is very rare. Common signs of exposure in dogs include lethargy, CNS depression, ataxia, vomiting (especially if plant material was ingested), urinary incontinence/dribbling, increased sensitivity to motion or sound, mydriasis, hyperesthesia, ptyalism, and bradycardia (Donaldson 2002; Janczyk et al. 2004; Pet Poison Helpline and SafetyCall International 2019). See Fig. 3.1 for signs reported to Pet Poison Helpline and Fig. 3.2 for the percentage of cases in which veterinary intervention was recommended. Acute onset urinary incontinence, especially in younger animals, is not commonly observed with other toxin exposures and serves as a helpful indicator for veterinary staff to consider THC exposure. Less common signs include agitation, aggression, bradypnea, hypothermia, hypotension, tachycardia, and nystagmus (Janczyk et al. 2004; Pet Poison Helpline and SafetyCall International 2019; Vaughn et al. 2020). Rare signs include seizures or comatose conditions. Although seizures are uncommon, it has been suggested that a higher expression of CB1 receptors on GABA releasing, rather than on glutamatergic terminals, in the neocortex could explain pro- or anti-convulsant effects in a dose dependent nature. Additionally, seizures may be caused by co-ingestants such as chocolate or other drugs.
Clinical signs associated with exposure to marijuana (i.e., THC containing products; ~3750 patients), synthetic cannabinoids (~70 patients), and CBD predominant cases (~350 patients) as reported to Pet Poison Helpline between 2010–2019. Canines represent ~87% of the displayed data, and cats ~10%. The remainder includes equines, livestock, and exotics. Confirmation of exposure was not obtained in all cases, nor could co-ingestants such as chocolate or other toxicants be ruled-out. Therefore, these data are meant to portray general trends only. Additional clinical signs were reported but excluded from the graphic due to space limitations
Comparison of the ultimate recommended management site for dogs and cats exposed to marijuana (i.e., THC containing products), synthetic cannabinoids, and CBD-predominant containing products for Pet Poison Helpline cases. Referral for veterinary intervention is based on a thorough patient risk assessment which includes patient signalment, dose, expected or current clinical signs, current and prior medical history, and co-ingestants or concomitant medications
Fatality in pets from THC intoxication is very rare and not well described in veterinary literature. Two canine euthanasias were reported in conjunction with the ingestion of baked goods made with marijuana butter although the cases became complicated and the exact cause of death was not determined (Meola et al. 2012). No confirmed fatalities or deaths thought to be a result from THC exposure have been reported to Pet Poison Helpline, despite consultation on many thousand cases (Pet Poison Helpline and SafetyCall International 2019).
3.5 Toxicity of CBD
Cannabidiol (CBD) is the most well-known and widely discussed non-intoxicating phytocannabinoid with concentrations ranging from 0.3 to 4.2% in cannabis plants—although this is ever changing with selective breeding of various cultivars (Long et al. 2005).
Despite their ubiquity on the consumer market, OTC products containing CBD are not FDA-approved, nor do they have any regulatory oversight. As of 2020, there was only one CBD product in the United States with regulatory approval, the human prescription pharmaceutical Epidiolex®. Approved by FDA in 2018, Epidiolex® is formulated as an oral solution (100 mg/mL) and labeled for the treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome in patients 2 years of age and older (Greenwich Biosciences 2018).
The lack of regulatory oversight for CBD containing products has resulted in a ‘buyer beware’ situation due to concerns over product quality. In 2015, the FDA tested various OTC “CBD containing products”, including those marketed specifically for pets, and found many did not contain the amount of CBD stated on the label (if any) while others contained unlabeled THC (US Food and Drug Administration 2018). Since then, regulators and numerous independent laboratories have repeatedly tested OTC “CBD-predominant” products and found similar results. For example, a product may contain only a small fraction of or several times the amount of labeled CBD. The same product may contain very large amounts of THC and/or synthetic cannabinoids, both of which can lead to severe clinical signs in pets or people. In a veterinary paper published by Wakshlag et al. (2020) the researchers found very similar results for veterinary labeled products as described above. (https://doi.org/10.2147/VMRR.S248712). The lack of regulation for pet products leaves consumers vulnerable to unscrupulous manufacturers and poor quality products.
3.5.1 Published Therapeutic and Adverse Effects
There is limited data regarding the safety and adverse effects of CBD in pets although this is an emerging area of research. Recent articles on the subject are discussed below.
A randomized, placebo-controlled, blinded, cross-over study published in 2018 by Gamble et al. demonstrated statistically significant reduction of pain and an increase in activity in a group of 16 pet dogs with concurrent osteoarthritis at Cornell University (Gamble et al. 2018). The dogs were given 2 mg/kg of CBD oil by mouth twice a day for 4 weeks. Dogs were also allowed to remain on NSAIDs, fish oil, and/or glucosamine/chondroitin supplements during the study. Laboratory work showed a statistically significant, progressive increase in alkaline phosphatase (ALP) from baseline through week 4 of CBD treatment in nine dogs (56%).
A study performed at Colorado State University examined the safety, toxicity, and pharmacokinetics of CBD in 30 purpose-bred beagle dogs (McGrath et al. 2018). Dogs received CBD via transdermal cream applied to the ear, oral capsules, or oral oil tinctures at ~10 mg/kg or ~20 mg/kg daily for 6 weeks (due to formulation inconsistencies, the dosages were less than the goal dosage of 10 and 20 mg/kg). Adverse effects included diarrhea in all dogs, with 20% (6/30) exhibiting single episodes of vomiting. The authors suspected the episodes of diarrhea were due to CBD administration but extenuating causes such as dietary variation and stress may have had an impact. Only dogs receiving oral CBD experienced vomiting although no correlation with respect to formulation or dose was identified. Erythematous pinnae were reported in all but one dog receiving the transdermal formulation. The only reported clinically significant laboratory change was a dose-dependent elevation in ALP in 11 dogs (36%) receiving oral CBD. Significant changes, defined as more than two times the high end of the normal range (140 IU/L), were first documented at week 2 and progressed through week 6. Most elevations ranged from 400–600 IU/L, with one dog peaking ~1000 IU/L. Both fasting and post-prandial bile acids remained normal in all dogs, including those with elevated ALP. Other reported effects that were not necessarily attributed to CBD administration included nasal and ocular discharge, salivary staining of the feet or ventral abdomen, transient and intermittent elevated nictitans and body temperature, weight-bearing lameness, and transient isosthenuria, hyposthenuria, and/or proteinuria.
In 2019, Deabold et al. published a study on the pharmacokinetics and safety of whole-plant CBD dominant products in dogs and cats. Eight healthy, purpose-bred beagle dogs received 2 mg/kg of a 50% mix of CBD and CBDA in a soft chew formulation twice daily, while fasted, for 12 weeks. Serum chemistry values, including ALP and ALT, remained within the normal reference range for all dogs during the 12 weeks. Diarrhea was the most commonly recorded adverse event and occurred intermittently in all dogs. A small number of vomiting episodes were also recorded. Eight healthy, purpose-bred domestic shorthair cats received 2 mg/kg of a 50% mix of CBD and CBDA in an infused fish formulation twice daily, while fasted, for 12 weeks. Although changes in CBC parameters occurred, none were considered clinically significant. Serum chemistry values remained within reference ranges with the exception of one cat. The affected cat had an elevated aminotransferase (ALT) noted at week 4 (first measurement since week 0) of ~300 U/L. ALT decreased but remained elevated at the 8- and 12-week measurements, measuring ~150 U/L each time. The researcher noted after publication that the ALT in this one cat did return to normal. No clinical signs related to the cat’s elevated ALT were observed. Other adverse effects included licking and head shaking during oil administration, pacing, chomping/chewing, gagging, vomiting, hypersalivation, being uncooperative, and grimacing. No diarrhea was observed in any cat. Food consumption and body weight remained consistent and ongoing physical exams revealed no abnormalities or changes in behavior over the 12 weeks. As with any study, it should be noted that recorded adverse events are not necessarily directly caused by the product and should not be interpreted as such. Of interest, the Cmax of CBD in cats was approximately 1/5 that of dogs, suggesting larger doses may be needed for therapeutic effect. For more detail on the pharmacokinetics reported in this study, see Chap. 2.
In 2020, Vaughn et al. published a randomized, placebo-controlled, blinded, parallel study in dogs comparing effects from escalating doses of three cannabis oil formulations containing predominantly CBD, THC, or a CBC/THC combination (1/5:1). Twenty healthy, purpose bread Beagle dogs were divided into groups of four with the intent of administering 10 escalating doses to fasted dogs, by oral gavage, with at least 3 days between administrations. In addition to laboratory diagnostics and measurement of plasma cannabinoids, all adverse events were recorded and categorized as mild, moderate, or severe/medically significant. The dogs in the CBD group were initially dosed ~2 mg/kg, with the 10th and final dose at ~62 mg/kg. Although adverse events were documented in the CBD arm, they were all classified as mild, defined as “activities of daily life were not impacted, and no intervention was indicated”. The vast majority of these effects were GI related (nausea, emesis, diarrhea), although constitutional effects (lethargy, hyperesthesia), neurological effects (muscle tremor, ataxia), and those classified as ocular, dermatological, and respiratory were also noted. Unlike some of the other studies, minimal impact on hepatic enzyme elevation was noted. In the CBD group, one dog developed a 2.9-fold increase in ALP (127 U/L) compared to baseline (44 U/L) 24 h following its 10th dose (~62 mg/kg). Seven days after the 10th dose, the concentration had dropped to 93 U/L. At no point, did this animal’s ALP exceed the normal reference range of 5–131 U/L. Overall, the authors concluded that the escalating doses of CBD were well tolerated by all dogs. The dogs in the THC and CBD/THC group developed more clinically significant adverse effects as compared to those in the CBD group. See the Toxicity of THC—Sect. 3.4 in this chapter for more detail on these two groups.
In people, dose-related elevation of alanine transaminase (ALT) and aspartate aminotransferase (AST) have also been reported. During clinical trials for Epidiolex®, enzyme elevation typically occurred in the first 2 months. In approximately two-thirds of cases, resolution occurred following discontinuation or dose reduction of the drug (or concurrent agents resulting in drug interactions); in one-third of cases, enzyme elevation resolved without dose reduction (Greenwich Biosciences 2018).
The reason for increased hepatic enzyme elevation, in all species, is thought to be due to induction of various cytochrome p450 enzymes in the liver, although more research and data is needed for a full understanding. Drug interactions can also play a role in elevated hepatic enzymes. In people, ALT elevation was more common in patients concurrently taking valproate (Greenwich Biosciences 2018).
CBD can also inhibit certain cytochrome P450 enzymes. Both inhibition and induction can lead to drug-drug interactions. This is an area of considerable concern and research, especially in human medicine. For example, in people, CBD is metabolized by CYP3A4 and CYP2C19. Concurrent administration of other drugs which also inhibit these enzymes can result in inhibition or slowed metabolism of these medications (Narimatsu et al. 1990). Dogs and cats also express CYP450 2C19 although data regarding interaction with CBD is lacking as enzyme nomenclature does not imply a one to one functional comparison (Greb and Puschner 2018). Regardless, monitoring of hepatic enzymes in animals chronically exposed to CBD is strongly recommended.
Lab animal reproductive toxicity studies with CBD revealed evidence of toxicity. Pregnant rabbits dosed orally at 0, 50, 80, or 125 mg/kg/day throughout organogenesis displayed decreased fetal body weights and increased fetal structural variations at the highest dose tested; this dose was also associated with maternal toxicity (Greenwich Biosciences 2018). Pregnant rats dosed at 0, 75, 150, or 250 mg/kg/day throughout the period of organogenesis displayed embryo-fetal mortality at the highest dose tested (Greenwich Biosciences 2018). When administered orally to rats, at doses of 75, 150, or 250 mg/kg/day throughout pregnancy and lactation, the following effects were observed: decreased growth, delayed sexual maturation, and neurobehavioral changes (decreased activity). Adverse effects on male reproductive organ development (small testes in adult offspring) and fertility were observed in the offspring at the mid and high dose. All effects occurred in the absence of maternal toxicity (Greenwich Biosciences 2018). It is important to note the dosages used in toxicity studies are considerably higher than thereputic dosges.
3.5.2 Clinical Signs of Poisoning
Due to the lack of intoxicating properties and wide margin of safety, less severe effects are expected in cases of pet exposure/overdose of CBD compared to those of THC containing products. However, exposure can be complicated by poor quality CBD products that may contain unlabeled THC or other agents such as synthetic cannabinoids.
Of the CBD exposures reported to Pet Poison Helpline from 2009 to 2019, the majority of cases (53%) remained asymptomatic. The most commonly reported clinical signs were lethargy/CNS depression, ataxia, vomiting, urinary incontinence, trembling, hyperesthesia, agitation, mydriasis, hypersalivation, and lateral recumbency (see Fig. 3.1). Many of these signs are consistent with pets exposed to THC/marijuana. As such signs are not expected with pets exposed to CBD alone, even in fairly large acute doses, the possibility that these signs may have been caused by adulterated products must be considered. Regardless, the overall lesson to the treating veterinarian is that patients exposed to CBD-containing products may become symptomatic. This reminds us that the adage, “treat the patient, not the poison” should be heeded. See Fig. 3.2 for the percentage of CBD exposure cases in which Pet Poison Helpline recommended veterinary intervention.
Other risks of accidental CBD product ingestion include exposure to carriers such as oils (aspiration), alcohols, toxic human foods, or a massive number of treats or novel food sources that could result in GI upset or other issues. Although significant systemic health effects are unlikely when ingested, IV dosing of 150–200 mg/kg in rhesus macaques did lead to tremors, hypopnea, respiratory arrest, and cardiac arrest in a dose dependent nature (Rosenkrantz et al. 1981). Such severe signs would not be anticipated following oral exposure in small animals.
3.5.3 Retrospective Study on CBD Cases Reported to Animal Poison Control
To further explore the development and spectrum of clinical signs following CBD exposures in pets, Pet Poison Helpline performed a retrospective study focused on 2 years of cases originating in the US or Canada. The study included any case originating between January 1, 2018 and January 12, 2020 that was documented in Pet Poison Helpline’s database. All cases were searched for any exposure to CBD-containing products which resulted in 346 patients. A “CBD-predominant product” was defined as any commercial, OTC, prescription, or homemade product which was labeled as containing CBD. Commonly reported products included pet treats; oral oils/capsules/tinctures marketed for use in either people or pets; topical balms, salves, or lotions marketed for use on people; human foods; vaping liquids; etc. Many of the products were labeled as “full spectrum”. To avoid clinical complication due to coingestants or THC, any patient with documented evidence of exposure to products other than CBD were excluded. This includes products with labeled THC. CBD containing foods, even those containing chocolate, were allowed to remain in the study group. This reduced the total number of included patients to 256. Species, age, and weight ranges are described in Table 3.1.
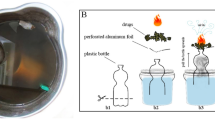
Patients were categorized by the general type of CBD containing products to which the pet was exposed. The three most common, in descending order, were: pet treats 27% (n = 69); oral oils/capsules/tinctures marketed for use in people 26% (n = 67); and oral oils/capsules/tinctures marketed for use in pets 16% (n = 42). See Fig. 3.3 for full product category lists and associated patients counts.
Number of patients exposed to CBD-containing products, categorized by product type, over a 2-year period as reported to Pet Poison Helpline. Whenever possible and reasonable, the dose of CBD that the patient was exposed to was recorded. In some instances, the dose or concentration of CBD in the product was not listed on the product label or the package was too destroyed by the pet to read the labeled dose. As has been discussed elsewhere in this chapter, at the time this data was collected there was no regulatory oversight of OTC CBD containing products for pets or people, meaning that there were greater concerns for product quality and less confidence that the dose listed on the label matched the actual dose present in the product. See Fig. 3.4 for the reported clinical signs associated with specified dose ranges of CBD from this study
Clinical signs associated with the specified CBD dose range as reported to Pet Poison Helpline in 256 patients. Individual patients may have exhibited more than one clinical sign. The total number of patients that developed clinical signs in this study group was 95 (37%). Signs which occurred in only one patient were excluded from this graphic. As these cases involve reports spontaneously made to an animal poison control center by a pet owner or veterinary professional, confirmation of exposure could not be obtained in all cases and the product dose was recorded at face value based on the label. As is the nature of spontaneously reported adverse event data, not all patients underwent medical evaluation, nor were these cases evaluated for causality. Therefore, these data are meant to portray general trends only. Based on the spectrum of clinical signs reported and significant concerns with OTC product quality in the US at the time this data was collected, there is a strong suspicion that some of these supposedly “CBD only” containing products were adulterated with THC, synthetic cannabinoids, or other substances. The product exposure categories were also individually reviewed with respect to the percentage of symptomatic patients. The only product in which 100% (n = 8) of exposed patients were symptomatic was vaping liquid. The category with the second highest percentage of symptomatic patients was pets exposed to oral oils and tinctures marketed for use in people, in which 50% (n = 34) of patients were symptomatic. This was followed by human foods with no chocolate (43%, n = 6), human topical formulations (41%, n = 12), oral oils and tinctures marketed for use in pets (33%, n = 14), human foods with chocolate (33%, n = 7), and pet treats (20%, n = 14)
3.6 Synthetic Cannabinoid Exposure
While this chapter focuses on plant derived cannabinoids, synthetic cannabinoids (SCBs), initially created many decades ago, became popular for recreational use in the US around 2000 and were marketed as a “legal high”. These compounds are dissolved in solvents and applied to dried plant material, intended to be smoked as an alternative to marijuana (Williams et al. 2015). They are often sold under a multitude of street names such as K2, Spice, Skunk, Wild Greens, Purple Haze, etc. They are typically packed in small sachets/envelopes and sometimes labeled as “incense” or “potpourri” and carry a “warning” stating they are “not for human consumption” to avoid detection by an unwitting public or law enforcement. In addition to containing SCBs, these products may have added chemicals/drugs such as caffeine or other stimulants. Although initially legally available in gas stations, head shops, tattoo parlors, etc., many of these products were banned by the 2011 Synthetic Drug Control Act.
3.6.1 Clinical Effects
Synthetic cannabinoids are engineered to cause potent psychotropic effects. They have a higher affinity for cannabinoid receptors than traditional marijuana, which results in more severe clinical effects (Gugelmann et al. 2014; Williams et al. 2015). In people, synthetic cannabinoids are 2–3 times more likely to cause sympathomimetic effects including tachycardia and hypertension, five times more likely to cause hallucinations, and have a higher incidence of seizures in comparison to marijuana (Murphy et al. 2012). Other signs may include cyclical agitation, aggression and incontinence in people (Gugelmann et al. 2014). Rare but significant cases of acute kidney injury have been reported in humans as well (Murphy et al. 2012).
Clinical effect data in animals exposed to SCBs is limited, although similar signs to those seen in humans have been reported. Exposure typically occurs via ingestion or, less often, inhalation. A case report involving both a pet owner and a dog affected by SCBs reported hyperesthesia, tremors, miosis, hyper-responsiveness to stimuli, ataxia, seizure-like activity, aggression and mild respiratory acidosis in the dog (Gugelmann et al. 2014). Similar signs were observed in the pet owner. Another case report involving presumptive SCB intoxication detailed signs of progressive ataxia, inappropriate mentation, hypothermia, stupor, and intermittent aggression with rapid progression to comatose condition, apnea, tremors, and opisthotonos (Williams et al. 2015). Cases reported to Pet Poison Helpline are more likely to involve severe signs such as tremors and seizures, when compared to marijuana, and all cases were deemed serious enough to warrant veterinary evaluation (see Figs. 3.1 and 3.2). These data seem to mirror the increase in severity of signs described in human medicine.
3.6.2 Pharmacokinetics
The pharmacokinetics of SCBs may be similar to other cannabinoids, although limited information is available. The oral bioavailability of various SCB products is likely low as case reports in people have indicated milder signs of shorter duration post-inadvertent ingestion of baked goods laced with SCBs (Obafemi et al. 2015).
3.7 Diagnosis of Poisoned Pets
There is no reliable point-of-care test available to detect the presence of cannabis or synthetic cannabinoids in veterinary patients. The OTC human urine drug screen assays designed to detect marijuana exposure are ineffective for SCB detection in both people and animals and often yield false negatives in veterinary patients exposed to marijuana/THC (Teitler 2009). Liquid chromatography mass spectrometry (LC/MS) remains the gold standard for drug screening in both humans and animals. Due to the wide variability of SCBs, clinicians wishing to submit samples for testing are advised to consult with the diagnostic lab prior to sending.
The reason(s) for which most human urine drug screens often yield false negative results in veterinary species is unknown and likely multifactorial. Possibilities include the differences in urinary THC metabolites produced in dogs or cats, as compared to people; impacts from laboratory handling (THC binds to glass and rubber stoppers); and increased patient water consumption resulting in dilute urine (Donaldson 2002; Fitzgerald et al. 2013).
False positives when human urine screens are used may also occur. In people, NSAIDs such as ibuprofen, naproxen, and niflumic acid, and efavirenz (antiviral drug) may cause false positives depending on the brand of test. Whether or not these agents could affect testing with dog or cat urine is not known (Saitman et al. 2014).
3.7.1 Non-specific Diagnostics
Routine diagnostics can alert clinicians to secondary intoxications or unrelated medical problems, as well as help guide supportive care treatments.
-
Radiographs: Monitor for evidence of ingested foil, other packaging materials, or batteries in the instance of a vaporizer pen ingestion, and the rare risk for foreign body obstruction if baggies, pipes, or vape pens are consumed.
-
CBC/chemistry/pre-fluid urinalysis: Following acute exposure to most cannabinoids, no immediate lab abnormalities are expected. Therefore, use these tests to rule out underlying issues, other causes, and/or establish normal baselines.
-
Initial diagnostics: PCV/TP to monitor hydration status; electrolytes (monitor sodium if multi-dose activated charcoal is given and monitor potassium if severely symptomatic); blood glucose (monitor intermittently in severely affected patients); renal profile (in the event hypotension leads to hypoperfusion); liver enzymes, especially in patients with chronic exposure.
3.7.2 Differential Diagnoses
The clinical signs for THC/marijuana and SCBs are non-specific and differential diagnoses must be considered if exposure cannot be confirmed. Differentials may include but are not limited to alcohols (ethanol, methanol, ethylene glycol, diethylene glycol, propylene glycol), opiates, benzodiazepines, muscle relaxants, tranquilizers, bromethalin (neurotoxic rodenticide), macrocyclic lactones (ivermectin, milbemycin), and illicit drugs (LSD, PCP, hallucinogenic mushrooms).
3.8 Treatment for Patients Exposed to Toxic Doses of Cannabinoids
3.8.1 Decontamination
-
1.
Emesis
-
(a)
Emesis should be considered if all the following conditions are met:
-
(i)
A toxic dose was ingested.
-
(ii)
Exposure was within the last 30–60 min or a significant amount of material remains in the stomach.
-
(iii)
The patient is asymptomatic and at low risk for aspiration.
-
(iv)
Spontaneous vomiting has not occurred. Spontaneous vomiting is usually secondary to irritation of GI tract from plant material.
-
(i)
-
(b)
Emetics
-
(i)
Dogs: Apomorphine (0.03 mg/kg IV) or hydrogen peroxide, 3% (1–2 mL/kg PO, food in the stomach increases chance of success).
-
(ii)
Cats: Dexmedetomidine (7–10 mcg/kg IM), hydromorphone (0.1 mg/kg SQ), or xylazine (0.44 mg/kg IM). Reverse as needed with atipamezole or naloxone. Do not use hydrogen peroxide or apomorphine in cats.
-
(i)
-
(a)
-
2.
Activated charcoal
-
(a)
Multi-dose activated charcoal may be considered in asymptomatic patients who are well hydrated and at low risk for aspiration.
-
(i)
Administer one dose of activated charcoal (1–2 g/kg PO) with sorbitol to start the series.
-
(ii)
Administer a half-dose of activated charcoal (or 0.5–1 g/kg PO) without sorbitol every 6–8 h × 1–2 additional doses.
-
(iii)
Have patients on IV fluids when receiving multi-dose charcoal and monitor serum sodium q 12 h. If acute CNS signs occur, check serum sodium STAT.
-
(iv)
Do not administer if the patient is at increased risk for aspiration, hypernatremia, dehydrated, or not passing stool prior to re-dosing.
-
(i)
-
(a)
-
3.
Gastric lavage
-
(a)
Massive ingestions may benefit from gastric lavage with patients under anesthesia and airway secured. A dose of activated charcoal with sorbitol may be placed through the stomach tube.
-
(a)
-
4.
Enemas
-
(a)
If suspect material is noted upon rectal exam, enemas may expedite clearance.
-
(a)
3.8.2 Supportive Care
-
1.
In general, most animals recover with appropriate supportive care.
-
2.
Antiemetics as needed. Do not use maropitant or antiemetics with a prokinetic effect if the patient is at risk for a foreign body obstruction.
-
3.
IV fluids 1–1.5× maintenance; adjust as needed for perfusion changes. IV fluids are not expected to expedite or enhance excretion of cannabinoids to a large degree.
-
4.
Thermoregulation
-
(a)
Warming or cooling therapy as needed. Hypothermia is more common with marijuana/THC exposure while hyperthermia is more commonly associated with SCB exposure. Do not cool below 103.5 °F.
-
(a)
-
5.
Oxygen therapy if respiratory depression.
-
6.
Nursing care
-
(a)
Generalized nursing care should be provided to obtunded or profoundly sedate patients including body rotation, ocular lubrication q 4–6 h, etc.
-
(b)
Keep the patient clean and dry. Although rarely necessary, an incontinent patient may benefit from a temporary urinary catheter.
-
(a)
3.8.3 Monitoring
-
1.
Mildly affected patients may be monitored at home if kept in a safe environment with no fall risk.
-
2.
Monitor vitals and blood pressure q 1–6 h depending on patient status.
-
3.
Monitor laboratory values as needed:
-
(a)
PCV/TP to monitor hydration status, especially if giving activated charcoal.
-
(b)
Electrolytes: Monitor sodium if administering multi-dose activated charcoal and potassium if severely symptomatic.
-
(c)
Blood glucose, intermittently, in severely affected patients.
-
(d)
BUN/creatinine if hypotension leads to hypoperfusion.
-
(e)
Liver enzymes, especially in patients with chronic exposure or if hypotension leads to hypoperfusion.
-
(a)
3.8.4 Medications
-
1.
Agitation: butorphanol (0.1–0.4 mg/kg IM or IV), diazepam (0.5–1.0 mg/kg IV PRN), or ± acepromazine (0.01–0.2 mg/kg slow IV, IM or SQ, titrate dose for effect). Avoid acepromazine in hypotensive patients.
-
2.
Tremors: methocarbamol (44–220 mg/kg slow IV to effect, select dose based on severity of signs). Re-dose PRN.
-
3.
Seizures: diazepam, phenobarbital, propofol, levetiracetam
-
4.
Bradycardia: atropine
3.8.5 Intravenous Lipid Emulsion and Extracorporeal Therapy
ILE has been suggested for marijuana and SCB intoxications in pets and used with varied success (Fitzgerald et al. 2013; Meola et al. 2012; Pet Poison Helpline and SafetyCall International 2019; Williams et al. 2015). The potential therapeutic benefit of ILE is based upon the knowledge that THC and cannabinoids are extremely lipophilic. All pharmacologically active cannabinoid compounds have a LogP > 4.5 (Thomas et al. 1990).
-
THC (CSID:15266 n.d.):
-
LogP = 7.68
-
LogD at pH 7.4 = 7.25
-
-
CBD (CSID:559095 n.d.):
-
LogP = 7.03
-
LogD at pH 7.4 = 6.43
-
The veterinary toxicologists at Pet Poison Helpline do not routinely recommend the use of ILE in cases of marijuana or SCB exposure, in part because of scant supportive data, both in the literature and from the Pet Poison Helpline database, but also because ILE may negatively impact the effect of therapies such as sedatives or anticonvulsants. If a patient’s clinical signs are severe enough to consider ILE, consultation with an animal poison control center is highly recommended prior to starting.
The use of extracorporeal therapy (ECT) has been described in one case report (Culler and Vigani 2019). In this case the dog ingested synthetic THC oil and presented with extreme anxious behavior, dysphoria, severe/frantic vocalization, severe hyperesthesia, and seizures refractory to anticonvulsants, necessitating general anesthesia and mechanical ventilation. The dog was concurrently hyperlipidemic, so ILE was not attempted. ECT was accomplished using both a hemoperfusion cartridge and hemodialysis filter in series. Within 1 h of initiating ECT, the dog’s mechanical ventilation was discontinued. Throughout ECT, the patient’s neurological status progressively improved. At the end of the 3h session, the dog was described as alert, responsive, and ambulatory with no signs of seizure activity. Six hours after ECT, the dog was quiet, alert, slightly ataxic but eating readily. The patient had radiographic evidence of aspiration pneumonia prior to ECT and, as such, remained in ICU for 36 h for IV antibiotic and nebulizer treatment. One-week post discharge, the dog was reportedly normal.
3.9 Prognosis
Most companion animals recover from acute, accidental cannabis exposures within 24–36 h. Severe cases may be affected for up to 72 h, barring secondary complications. Prognosis is generally good with supportive care.
3.10 Conclusion
Cannabis, THC, CBD, and SCB exposures and intoxications have been increasing in frequency in both human and veterinary medicine. Veterinary professionals are expected to see an increase in inadvertent companion animal exposure and intoxications as the additional therapeutic benefits of cannabinoids come to light, societal perceptions change, legislators and regulators move toward legalization and decriminalization, and access to cannabinoid products increases. Vigilant and careful physical exams with attentive and empathetic history taking skills devoid of judgment are imperative to help in diagnosing and treating companion animal patients.
References
Adams, I. B., & Martin, B. R. (1996). Cannabis: Pharmacology and toxicology in animals and humans. Addiction, 91(11), 1585–1614.
CSID:15266. (n.d.). Accessed June 24, 2018, from http://www.chemspider.com/Chemical-Structure.15266.html.
CSID:559095. (n.d.). Accessed June 24, 2018, from http://www.chemspider.com/Chemical-Structure.559095.html?rid=79a89166-d9cf-41ea-9313-8366b7493a83.
Culler, C. A., & Vigani, A. (2019). Successful treatment of a severe cannabinoid toxicity using extracorporeal therapy in a dog. Journal of Veterinary Emergency and Critical Care, 29(6), 674–679. https://doi.org/10.1111/vec.12899.
Deabold KA, Schwark WS, Wolf L, Wakshlag JJ. Single-Dose Pharmacokinetics and Preliminary Safety Assessment with Use of CBD-Rich Hemp Nutraceutical in Healthy Dogs and Cats. Animals (Basel). 2019 Oct 19;9(10):832. doi: 10.3390/ani9100832. PMID: 31635105; PMCID: PMC6826847.
Donaldson, C. W. (2002, June). Marijuana exposure in animals. Veterinary Medicine, 437–439.
ElSohly, M. A., Mehmedic, Z., Foster, S., Gon, C., Chandra, S., & Church, J. C. (2016). Changes in cannabis potency over the last 2 decades (1995–2014): Analysis of current data in the United States. Biological Psychiatry, 79(7), 613–619. https://doi.org/10.1016/j.biopsych.2016.01.004.
Fitzgerald, K. T., Bronstein, A. C., & Newquist, K. L. (2013). Marijuana poisoning. Topics in Companion Animal Medicine, 28(1), 8–12. https://doi.org/10.1053/j.tcam.2013.03.004.
Gamble, L.-J., Boesch, J. M., Frye, C. W., et al. (2018). Pharmacokinetics, safety, and clinical efficacy of cannabidiol treatment in osteoarthritic dogs. Frontiers in Veterinary Science, 5, 165. https://doi.org/10.3389/fvets.2018.00165.
Greb, A., & Puschner, B. (2018). Cannabinoid treats as adjunctive therapy for pets: Gaps in our knowledge. Toxicology Communications, 2(1), 10–14. https://doi.org/10.1080/24734306.2018.1434470.
Greenwich Biosciences. (2018, December). Epidiolex full prescribing information.
Gugelmann, H., Gerona, R., Li, C., Tsutaoka, B., Olson, K. R., & Lung, D. (2014). ‘Crazy Monkey’ poisons man and dog: Human and canine seizures due to PB-22, a novel synthetic cannabinoid. Clinical Toxicology, 52(6), 635–638. https://doi.org/10.3109/15563650.2014.925562.
Janczyk, P., Donaldson, C. W., & Gwaltney, S. (2004). Two hundred and thirteen cases of marijuana toxicoses in dogs. Veterinary and Human Toxicology, 46(1), 19–21.
Landa, L., Sulcova, A., & Gbelec, P. (2016). The use of cannabinoids in animals and therapeutic implications for veterinary medicine: A review. Veterinární Medicína, 61(3), 111–122. https://doi.org/10.17221/8762-VETMED.
Long, E., Malone, D., & Taylor, D. (2005). The pharmacological effects of cannabidiol. Drugs of the Future, 30, 747.
Marzo, V. D., Bifulco, M., & Petrocellis, L. D. (2004). The endocannabinoid system and its therapeutic exploitation. Nature Reviews Drug Discovery, 3(9), 771–784. https://doi.org/10.1038/nrd1495.
McGrath, S., Bartner, L. R., Rao, S., Kogan, L. R., & Hellyer, P. W. (2018). A report of adverse effects associated with the administration of cannabidiol in healthy dogs. AHVMA Journal, 52, 34–38.
Meola, S. D., Tearney, C. C., Haas, S. A., Hackett, T. B., & Mazzaferro, E. M. (2012). Evaluation of trends in marijuana toxicosis in dogs living in a state with legalized medical marijuana: 125 dogs (2005-2010): THC toxicosis. Journal of Veterinary Emergency and Critical Care, 22(6), 690–696. https://doi.org/10.1111/j.1476-4431.2012.00818.x.
Murphy, T. D., Weidenbach, K. N., Houten, C. V., et al. (2012). Acute kidney injury associated with synthetic cannabinoid use – Multiple States, 2012. MMWR. Morbidity and Mortality Weekly Report, 62(6), 93–98.
Murray, R. M., Morrison, P. D., Henquet, C., & Forti, M. D. (2007). Cannabis, the mind and society: The hash realities. Nature Reviews. Neuroscience, 8(11), 885–895. https://doi.org/10.1038/nrn2253.
Narimatsu, S., Watanabe, K., Matsunaga, T., et al. (1990). Inhibition of hepatic microsomal cytochrome P450 by cannabidiol in adult male rats. Chemical & Pharmaceutical Bulletin, 38(5), 1365–1368.
Obafemi, A. I., Kleinschmidt, K., Goto, C., & Fout, D. (2015). Cluster of acute toxicity from ingestion of synthetic cannabinoid-laced brownies. Journal of Medical Toxicology, 11(4), 426–429. https://doi.org/10.1007/s13181-015-0482-z.
Pet Poison Helpline & SafetyCall International. (2019). Pet poison helpline case database. Minneapolis, MN: Pet Poison Helpline & SafetyCall International, PLLC. Database last accessed: 2019
Pirone, A., Lenzi, C., Coli, A., Giannessi, E., Stornelli, M. R., & Miragliotta, V. (2015). Preferential epithelial expression of type-1 cannabinoid receptor (CB1R) in the developing canine embryo. Springerplus, 4(1). https://doi.org/10.1186/s40064-015-1616-0.
Raber, J. C., Elzinga, S., & Kaplan, C. (2015). Understanding dabs: Contamination concerns of cannabis concentrates and cannabinoid transfer during the act of dabbing. The Journal of Toxicological Sciences, 40(6), 797–803. https://doi.org/10.2131/jts.40.797.
Rosenkrantz, H., Fleischman, R. W., & Grant, R. J. (1981). Toxicity of short-term administration of cannabinoids to rhesus monkeys. Toxicology and Applied Pharmacology, 58(1), 118–131.
Saitman, A., Park, H.-D., & Fitzgerald, R. L. (2014). False-positive interferences of common urine drug screen immunoassays: A review. Journal of Analytical Toxicology, 38(7), 387–396. https://doi.org/10.1093/jat/bku075.
Sharma, P., Murthy, P., & MMS, B. (2012). Chemistry, metabolism, and toxicology of cannabis: Clinical implications. Iranian Journal of Psychiatry, 7(4), 149–156.
Teitler, J. B. (2009). Evaluation of a human on-site urine multidrug test for emergency use with dogs. Journal of the American Animal Hospital Association, 45(2), 59–66. https://doi.org/10.5326/0450059.
Thomas, B. F., Compton, D. R., & Martin, B. A. (1990). Characterization of the lipophilicity of natural and synthetic analogs of L\9-tetrahydrocannabinol and its relationship to pharmacological potency. Journal of Pharmacology and Experimental Therapeutics, 255, 7.
US Food & Drug Administration. (2018). Warning letters and test results for cannabidiol-related products. Accessed June 26, 2018, from https://www.fda.gov/NewsEvents/PublicHealthFocus/ucm484109.htm.
Vaughn, D. M., Kulpa, J., & Paulionis, L. (2020). Preliminary investigation of the safety of escalating cannabinoid doses in healthy dogs. Frontiers in Veterinary Science. https://doi.org/10.3389/fvets.2020.00051.
Wakshlag, J. J., Cital, S., Eaton, S. J., Prussin, R., & Hudalla, C. (2020). Cannabinoid, terpene, and heavy metal analysis of 29 over-the-counter commercial veterinary hemp supplements. Veterinary Medicine (Auckl), 11, 45–55. https://doi.org/10.2147/VMRR.S248712. PMID: 32346530; PMCID: PMC7169471.
Williams, K., Wells, R. J., & McLean, M. K. (2015). Suspected synthetic cannabinoid toxicosis in a dog. Journal of Veterinary Emergency and Critical Care, 25(6), 739–744. https://doi.org/10.1111/vec.12378.
Acknowledgments
The author would like to express her gratitude to Amanda Poldoski, DVM, at Pet Poison Helpline for her data interpretation and creation of the figures in this text; to Holly Hommerding, DVM, DABT at Pet Poison Helpline for her previous research and writing on this topic; and to Morgan Maisel, DVM/MPH candidate 2019, for her work analyzing Pet Poison Helpline’s CBD and synthetic cannabinoid cases.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Brutlag, A. (2021). Toxicology. In: Cital, S., Kramer, K., Hughston, L., Gaynor, J.S. (eds) Cannabis Therapy in Veterinary Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-68317-7_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-68317-7_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-68316-0
Online ISBN: 978-3-030-68317-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)