Abstract
Currently, there are no drugs or other therapeutic agents approved by the U.S. Food and Drug Administration (FDA) to prevent or treat COVID-19. Current standard of care includes prevention of infection and control measures and supportive care, including supplemental oxygen and, when required, mechanical ventilatory support. This chapter outlines important drugs that have the potential to be used as Covid-19 remedies. Several landmark clinical trials are discussed, and clinical evidence is sought for the claims made for the efficacy of these drugs in treating Covid-19. Literature searches suggest that dexamethasone reduces mortality in severely ill patients and may also reduce the need of mechanical ventilation in such patients compared to the standard care. However, no irrefutable evidence was found for the efficacy claims of hydroxychloroquine. The role of many other drugs is still uncertain as there are very few large-scale randomized clinical trials to show their effectiveness in Covid-19. However, many new and exciting molecules are being tested in the laboratories. Large, randomized, controlled, double-blind trials are underway to investigate the safety and efficacy of several new and old drugs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Slowing the COVID-19 pandemic, which has already infected over 34 million people worldwide, and ultimately ending it will depend substantially on the scientists’ development of effective treatments. The initial effort to repurpose the existing drugs approved for other ailments to kill the virus and treat the COVID-19 makes sense. Worldwide, many laboratories are engaged in carrying out research on existing drugs to develop remedies for COVID-19. This will considerably shorten the total duration of drug discovery and development, which extends from laboratory investigations to initial toxicity testing to animal studies to safety studies in humans and, finally, large-scale clinical trials.

The interruption of COVID-19 spread depends on a combination of pharmacologic and nonpharmacologic interventions. Initial SARS-CoV-2 prevention includes social distancing, face masks, environmental hygiene, and handwashing [1]. Although the most important pharmacologic interventions to prevent SARS-CoV-2 infection are likely to be vaccines, the repurposing of established drugs for short-term prophylaxis is another more immediate option. Here are some of the medicines currently being used in various parts of the world as potential remedies for COVID-19.
Dexamethasone
In June 2020, scientists in the UK announced that an anti-inflammatory agent, dexamethasone, has shown to reduce mortality in a recent clinical trial in which more than 6000 severely sick COVID-19 patients were treated [2]. This represents a significant improvement over the current treatment options available for COVID-19 patients. Immediately, dexamethasone was authorized by the British government to be used in some patients, although its role in treating less severe COVID-19 infection was still not clear. The news of a preexisting, inexpensive medication reducing mortality in COVID-19 patients came as a pleasant surprise after the continuous negative news of what seemed to be an unstoppable spread of novel coronavirus. Although the complete clinical data were not available immediately, it was quite clear that this could be a breakthrough. The drug is available in large quantities in even developing countries and can be administered orally.
This trial’s results were compelling, although they have surprised many people who are actively involved in finding a cure for COVID-19. Many experts in the field suggested that if these results hold up in larger, more powered clinical trials, this drug could be a game-changer, especially for those COVID-19 patients who are critically ill.
Dexamethasone is an important drug, a steroid used to treat general inflammation and a host of other conditions. It is well known in medicine for many years. The drug has an excellent profile with a half-life of up to 54 hours. Since it is a nonspecific treatment because it does not block a specific inflammatory pathway, it has certain adverse effects. This is the drawback of this drug.
The results of the RECOVERY trial are particularly encouraging for severely ill COVID-19 patients. After less than a month of treatment, there was a 35% reduction in the mortality of severely ill patients who required ventilators. In patients who required supplemental oxygen but not ventilators, a 20% reduction in mortality was observed. However, it appears that the drug is not beneficial in less severely ill patients and may exacerbate the disease. Some studies also suggested that patients with acute respiratory distress syndrome can also benefit from the use of dexamethasone.
Two factors are crucial when managing COVID-19 patients with dexamethasone – selectiveness and timing. Initial investigations suggest that dexamethasone should not be used in patients who do not have severe symptoms of the disease and do not need additional oxygen, such as those requiring a ventilator. Even in patients in which dexamethasone is useful, it has certain drawbacks. It decreases an individual’s ability to fight the virus because it dampens the overall immunity. Its lack of selectivity in inhibiting inflammatory pathways makes patients susceptible to several untoward effects, which include but are not limited to psychosis, emotional disturbances, and worsening diabetes mellitus. Furthermore, dexamethasone should not be used in the early stages of the disease as it may hinder the immune system in clearing the virus from the body.
Comparing with remdesivir, which is the only other drug showing beneficial effects in COVID-19 patients in a clinical trial, the results produced by dexamethasone are more impressive. Remdesivir is not reported to decrease the mortality in COVID-19 patients but only reduced the number of days patients had to remain hospitalized. On the other hand, dexamethasone reduced the death rate in severely ill COVID-19 patients.
After the trials’ results were announced, many clinicians were confident that they were more likely to give dexamethasone to severely ill COVID-19 patients, especially those on ventilators and whose condition is not improving. However, some were not happy with the full results still not available. Scientists need additional information on the trial to help identify further subsets of patients who could benefit the most from the dexamethasone treatment. The trial investigators responded that they acknowledge and understand the scientific community’s concern and will release the full data shortly.
The RECOVERY trial was evaluating many other treatment options besides dexamethasone. For example, Kaletra, an HIV drug combination, antimalarial drug hydroxychloroquine, and convalescent plasma were also investigated. The trial’s hydroxychloroquine arm was discontinued after 2 weeks when it became apparent that the patient outcome is not improving. The rest of the trial was continued until 6000 patients were enrolled in the trial. Investigators were looking for a drug that could reduce deaths by about 18% with 90% confidence. They found out that dexamethasone was the first one to achieve this target. After that, they started analyzing the data, and very early in the analysis, they found the clear advantage dexamethasone was offering to severely ill COVID-19 patients.
Chloroquine
The U.S. Food and Drug Administration revoked its emergency authorization for hydroxychloroquine, the controversial antimalarial drug promoted by President Donald Trump for treating the coronavirus. The agency said in a letter that the decision is based on new evidence that made it unreasonable to believe hydroxychloroquine and chloroquine “may be effective in diagnosing, treating or preventing” COVID-19, the illness caused by the virus. Citing reports of heart complications, the FDA said the drugs pose a greater risk to patients than any potential benefits.
Chloroquine is a synthetic 4-aminoquinoline that has been the mainstay of antimalarial therapy. It specifically binds to heme, preventing its polymerization to hemozoin. Its use to treat COVID-19 patients started after some studies reported its beneficial effects in treating the disease. Chloroquine and hydroxychloroquine have been previously promoted by certain study groups to prevent and treat SARS-CoV, among other conditions [3]. However, it was recently discovered that in vitro replication of SARS-CoV-2 can be inhibited by hydroxychloroquine [4]. However, other studies did not yield many encouraging results, and their outcome was mixed [5].
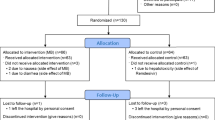
A recent clinical trial tested hydroxychloroquine for postexposure prophylaxis, and the results are now reported [6]. In this trial, all the data were reported by the participants who were recruited by the investigators through social media. Placebo or hydroxychloroquine was provided through the mail to participants who reported severe or moderate exposure to COVID-19 patients at the workplace or at home. Only 13% of the enrolled participants developed COVID-19-like symptoms but were confirmed by the PCR in only 3% of the participants. In this setting, the use of hydroxychloroquine did not offer any benefit compared to placebo in protecting participants from developing Covid-like symptoms in the Covid-naïve participants. On the other hand, hydroxychloroquine users reported common adverse effects much more frequently than those who received a placebo (40% vs 17%).
The study design of the trial itself had many limitations. There were no consistent means of verifying whether the participants reporting Covid-like symptoms have the infection. That is why the reported symptoms of Covid patients in the study were less specific [7]. Therefore, the exact number of Covid cases in the study is hard to know. Another problem was the inability to monitor patient compliance and adherence to the dosing schedule. In the study, patients receiving hydroxychloroquine reported less than optimal compliance. The median age of the participants enrolled in the study was 40 years, and most of them were free of coexisting diseases. Therefore, these were a rather low-risk participant group because those at high risk are much older and have comorbid conditions [8].
Another problem with this clinical trial was that hydroxychloroquine was started much later after symptoms appear in the patients (more than 3 days). This indicates that the aim of the trial was to prevent the COVID-19 symptoms rather than the prevention of SARS-CoV-2 infection.
Hydroxychloroquine is a relatively safe drug, which has been emphasized previously [3]. However, careful analysis of such studies indicates that the potential for cardiotoxicity was high, especially in patients with comorbid conditions [9]. Most of the COVID-19 patients are older and with other preexisting diseases. This trial, although did report mild adverse effects of hydroxychloroquine, did not mention any cardiac effect as these could not be assessed.
The fear of SARS-CoV-19 justifies the urgent search for treatments, and therefore advocacy of hydroxychloroquine and its widespread use makes sense. But it should be the scientific evidence that should drive the clinical decisions rather than social media and unfounded political remarks. It appeared for a while that social and political forces were driving the global COVID-19 research agenda [10]. At one time, more than 200 clinical trials were listed on ClinicalTrials.gov website, many of which were intended for the prevention of the disease. What would be the fate of these trials in the face of results by Boulware and colleagues? Since Boulware and colleagues’ results are inconclusive and even provocative, the results of these trials, which are much larger and more scientifically sound designs, would be interesting.
On June 15, 2020, FDA has revoked the emergency authorization to use chloroquine and hydroxyl chloroquine in hospitalized COVID-19 patients when a clinical trial is unavailable or participation is not feasible. This decision was based on recent data and a large clinical trial that did not show any benefit of these medications in the speed of recovery or in decreasing the likelihood of death. These outcomes of the clinical trial make sense and are consistent with the recent studies which show that these drugs are unable to inhibit viral mRNA or kill the virus. Hence, FDA determined that the legal criteria for the emergency use authorization are no longer met.
Remdesivir
Viruses from the corona family hijack the cellular machinery after entering the host cell. To replicate inside the host cell, their RNA-dependent RNA polymerase (RDRP) uses the host raw material to replicate [11]. This enzyme is an especially attractive drug target for it is highly conserved because of the evolutionary constraints on its function. This approach of blocking the replicating enzyme in the virus has previously yielded dividends in the treatment of hepatitis C infection, as illustrated by the discovery and development of sofosbuvir [12].
The virus that causes COVID-19-SARS-CoV-2 is a member of coronaviruses. Its treatment targets would be similar to other coronaviruses such as those that caused SARS and MERS, namely, SARS-CoV-1 and MERS-CoV, respectively. A recent study was conducted on the potential of remdesivir to treat COVID-19 [13]. This study has resulted in some confusion regarding the outcome of the trial due to the study design issues.
Remdesivir is a prodrug and must be activated to its active form by several enzymes, including esterases, amidases, and kinases. Once inside, the active drug inhibits viral RDRP [14]. This approach has been historically very effective, although coronaviruses can detect nucleotide sequences errors and correct it [15, 16]. However, remdesivir has the ability to escape from this corrective action of coronaviruses. Similarly, laboratory experiments indicate that a mutation in the viral enzyme would lead to resistance against remdesivir, but such versions of the viruses are less fit and much less pathogenic [15].
Several animal studies show that remdesivir is effective against many viruses. When given postexposure to rhesus monkeys infected with MERS-CoV, it protected the monkeys from severe lung damage, and when given as a pretreatment, it protected the monkeys from infection [17]. Similarly, when given 24 hours postexposure to African green monkeys infected with Nipah virus, it protected monkeys from this infection, which is a cause of fatal encephalitis [18]. It also protected rhesus monkeys from the Ebola virus when given parenterally for 12 days [19].
Remdesivir treatment 12 hours prior to infecting the rhesus monkeys with SARS-CoV-2 protected them from severe lung damage and reduced respiratory symptoms in a randomized control laboratory trial of 12 rhesus monkeys [20]. Whether this efficacy and potency are translated into human clinical trials is a different matter. In another study, Ebola mortality was compared in four groups, one of which was given remdesivir, and the other three were given different antibody treatments. In a randomized control trial in 681 patients, the mortality in the remdesivir group was 53%, which was significantly worse than 35% observed in the most potent antibody group [21]. However, the authors also shared that the patients in the remdesivir group had much severe symptoms.
Many of the initial studies on the effects of remdesivir in COVID-19 stem from small clinical studies or personal experiences [22]. However, the results of some short clinical trials are now being reported. In several studies spanning three contents and over 20 hospitals, the combined results of 53 of 61 patients suggest some protective effects of remdesivir in COVID-19 patients [13]. The mortality rate was 13% in the remdesivir group after 18-day treatment. Among patients who were ventilated, mortality was 5%. The likelihood of patient improvement was 68% after an 18-day treatment period (40–80% with a 95% confidence interval). Common and less severe adverse effects were experienced by 60% of patients, while serious adverse effects were reported by 23% of patients. Rashes, diarrhea, hypotension, and renal impairment were the most frequently encountered adverse effects. This study has some obvious limitations. The trial did not have a randomized control arm; there was no information on the initially treated eight patients, and the follow-up was relatively short. The sample size of the trial was also small precluding generalizability of the study.
A compassionate use program is available for remdesivir as it once existed for penicillin for treating acute infective endocarditis (Dolphin A, Cruickshank R, 1945). However, there are some very important differences between the two. In the case of the compassionate use of penicillin for infective endocarditis, it should be recalled that mortality of endocarditis was high compared to COVID-19. Furthermore, it is hard to establish evidence of treatment benefit in an open, uncontrolled trial. Therefore, the mere existence of a compassionate use program does not guarantee the safety and efficacy of the treatment.
Whether or not remdesivir offers any benefit in COVID-19 could be ascertained by large, well-powered, randomized, double-blind, controlled, well-masked, preferably multicentered trials. Currently, there are more than two dozen different clinical trials; enrolling over 25,000 patients are underway to investigate the effects of remdesivir in COVID-19. However, only about one-fifth of these are double-blind. Many of these are just observational studies. Another thing that could help is preparing standard protocols for these clinical trials for easy comparison of the data. Designing adaptive clinical trials would facilitate interim analyses and decide if a treatment should be stopped or evaluated further. The adaptive design will also help in evaluating multiple treatments at once.
Angiotensin-Converting Enzyme Inhibitors
SARS-CoV-2 infection is not severe in most people, but in some, it can lead to severe inflammation, respiratory depression, and death due to multiorgan failure [23]. The virus enters the cell by endocytosis when the cell-surface protein ACE2 interacts with the viral protein spike in the lung. ADAM metallopeptidase domain 17 (ADAM 17) activity is increased due to this endocytosis, which results in the release of ACE2 from the cell membrane. The loss of ACE2 abolishes its protective role in the cell and causes further release of proinflammatory cytokines in the circulation when the renin-angiotensin-aldosterone system is left uninhibited [24]. In patients with preexisting cardiovascular disease, this inflammation and stress further aggravate the patient’s condition [25]. Other factors that play important roles in the observed association between death due to COVID-19 and cardiovascular disease include myocardial depression, viral infection of the heart, endothelial denudation, and cardiomyopathy. These effects may further aggravate preexisting arrhythmias, increase the oxygen demand of the heart, and hasten heart failure [26].
Factors such as old age and patient gender also affect the disease outcome in COVID-19 patients. Older age was found significantly associated with cardiovascular events and death in influenza [25]. Differences in the disease outcome and gender were also observed during the 2003 epidemic of severe acute respiratory syndrome (SARS) [27]. These differences in the disease outcome (death) may be because women can fight infections better than men owing to stronger immunity [28]. Furthermore, it is also known that male mice have a higher susceptibility to SARS-CoV-1 than female mice in the animal models. This could be partly explained by the increased concentrations of inflammatory markers such as neutrophils and macrophages [29]. Animal studies also reveal that female mice’s mortality due to SARS-CoV-1 is increased when estrogen receptor antagonists are used or after ovariectomy. This risk due to gender is further enhanced by advanced age [29]. These observations suggest there is a strong protective effect of female sex and younger age as indicated by the increased survival linked to these two variables in COVID-19.
In a recent study, survival among COVID-19 patients is increased when statins or ACE inhibitors were used [26]. Since this study was not a randomized controlled clinical trial, the effects of confounders cannot be overlooked. These could be chance associations. Therefore, it cannot be established that ACE inhibitors or statins are increasing the survival of COVID-19 patients. Hence, in individual patients who do not have any routine indication of these drugs, this study does not provide evidence to initiate those patients on ACE inhibitors or statins. Whether or not these medications can offer any benefit in COVID-19 patients could be established by randomized controlled clinical trials that would evaluate the roles of these medications in detail.
Several studies show that in-hospital deaths, increased risk of severe disease, or increased risk of SARS-CoV-2 infection is not associated with the use of ACE inhibitors or ARBs. These studies alleviate the concerns that ACE inhibitors and ARBs may predispose individuals to severe COVID-19 disease due to the inhibition of the renin-angiotensin-aldosterone system (RAAS). These studies have different study designs and diverse populations. Still, most of these were observational and were published in reputable journals such as the New England Journal of Medicine and JAMA Cardiology.
Mehra and colleagues [30] showed that various cardiovascular and noncardiovascular adverse effects had been associated with in-hospital deaths. Especially, smoking older age (>65), congestive cardiac failure, coronary disease, cardiac rhythm problems, and chronic obstructive pulmonary disease are independently associated with in-hospital deaths. These adverse effects increased the risk of in-hospital death. On the other hand, the use of ACE inhibitors was not associated with in-hospital deaths. This analysis was described in a study that collected the observational data of 8910 patients from Europe, North America, and Asia, admitted in 169 different hospitals to investigate the link between in-hospital death and drug therapy and cardiovascular events.
The severity of COVID-19 and the risk of SARS-CoV-2 infection were not associated with the use of ACE inhibitors and ARBs in another trial conducted in Italy by Mancia and colleagues [31]. Although the use of these medications was lower in controls compared to cases, no evidence of increased adverse effects or risk of severe infection was found in the control group. This analysis was a result of a population-based case-control study in which 6272 cases and 30,759 matched controls were recruited to investigate the possible link between these drugs (ACE inhibitors and ARBs) and the severity of the disease and the risk of infection.
Previous use of ACE inhibitors and ARBs was not associated with the risk of infection or its severity in another observation controlled trial [32]. Propensity score models and Bayesian analysis revealed that both ACE inhibitors and ARBs are not associated with a high risk of severe COVID-19 infection or a higher risk of disease. This study was conducted in 12,594 patients enrolled in a health network in New York, USA, and were screened for COVID-19 infection.
In another cohort of patients, overlap propensity score weighting did not show an association between the use of cardiovascular medications (ACE inhibitors and ARBs) and the risk of a positive Covoid-19 infection [33]. These were the results of a study conducted by Mehta and colleagues in Florida, USA, in a cohort of 18,472 COVID-19 patients.
Another case-population study conducted in Spain also ruled out any link between ACE inhibitors and ARBs and increased risk to COVID-19 [34]. Conditional logistic regression analyses revealed that the use of ACE inhibitors and ARBs to blunt RAAS was not associated with a higher risk of the disease compared to other cardiovascular drugs. This study, which was conducted in 1139 COVID-19 patients admitted to seven hospitals in Spain, also revealed that ACE inhibitors and ARBs are associated with a lower risk of COVID-19 in diabetic patients. Taken together, these investigations indicate that the use of RAAS inhibitors is not associated with an enhanced risk of COVID-19 severity or other unusual untoward effects.
Spike Protein Inhibitors
Novel coronavirus targets human cells through a highly glycosylated protein called S protein, which binds human angiotensin-converting enzyme 2 (ACE-2) [35]. This initial binding step is followed by the internalization of the virus in human cells. This binding of S protein, through its receptor-binding domain, to ACE-2 is a prerequisite for viral entry and subsequent pathogenesis of the disease [36]. The high affinity of S protein toward ACE-2 is thought to be an important underlying factor in the rapid spread of the disease. The absence of an early high-resolution crystal structure of S protein made the initial efforts to virtually screen or design S protein inhibitors extremely hard [37]. Publishing of a high-resolution (3.5 A), CryoEM structure of the S protein was recently reported [36]. This has made the design and virtual screening of the S protein inhibitors relatively easier.
It was recently shown that Affimer reagents were able to bind S protein from SARS-COV-2, which protected the human cells from COVID-19 infection. This work is a collaboration between the Center for Virus Research, University of Glasgow, and Affimer biotherapeutics and reagents manufacturer Avacta Group plc. These laboratory findings could become a potential therapy for COVID-19.
In a recent statement, the company stated that they had generated more several potent inhibitors of S protein, which could block the first step of viral entry into human cells. They said that their preliminary data is highly encouraging. Their collaborator, Professor David Bhella, at the University of Glasgow, seems to agree. According to him, these spike protein inhibitory compounds could neutralize any attempt of viral entry in the human cell through the ACE-2 receptor.
Compared to antibodies, small-molecule inhibitors, such as those analyzed by the Avacta Group and University of Glasgow team, offer many advantages. Because of their small sizes, high concentrations of these inhibitors could be used without significant solubility issues. Since these compounds are made through combinatorial chemistry techniques, scaling up their production will not be a big challenge. Another critical advantage of Avacta Group compounds is that many of these investigative therapies are bispecific or trispecific, meaning they bind to more than place on the spike protein, ensuring maximum effectiveness of the therapy.
Further work is underway to understand the nature of binding Avacta compounds to spike protein, which could provide insights into the mechanistic aspects of the inhibition. On the other hand, Avacta is actively looking for a large pharmaceutical industry partner for the large-scale production of the compounds once its efficacy and potency are established. The promising aspect of these compounds is that they could be given to the healthcare worker for prophylaxis and the patients for treating the disease.
There is also an increasing interest of the research community in targeting S protein for furin-like cleavage site to generate the so-called furin inhibitors. The presence of a furin-like cleavage site in the genomic sequence of SARS-COV-2 further elevated the interest in designing and developing such inhibitors. This furin-like cleavage site in the S protein has implications for the pathogenicity of the virus and its life cycle.
Conclusions
This chapter discusses several drugs currently in clinical and laboratory studies in addition to several landmark trials and combines the available information with the personal experiences of clinicians with COVID-19 patients. We discussed important clinical trials, including the one that demonstrates a significant decrease in mortality with dexamethasone use. Another important clinical trial that was discussed showed that the use of remdesivir decreases in the number of days a patient with COVID-19 had to spend in a hospital. However, many of the studies show no benefit to the patients, and some are inconclusive. Other studies demonstrate improvement in patients’ symptoms, but the evidence was low. One of the major problems in comparing the results from different studies and trials is the lack of uniform study design. However, based on the available evidence, dexamethasone and remdesivir are perhaps the best of the available remedies for COVID-19. ACE inhibitors and ARBs could also be used in COVID-19 patients for cardiovascular indications, and they do not increase the severity or the frequency of known adverse effects. We could not find any worthwhile evince that supports the use of chloroquine or hydroxychloroquine in COVID-19 patients. Many new and exciting molecules are being tested in the laboratories. Some old and new drugs are being investigated in the large, randomized, controlled trial worldwide to treat and prevent COVID-19. The research and medical community’s hard work represents a great hope for humanity to overcome this pandemic ultimately.
References
Cohen MS, Corey L (2020) Combination prevention for COVID-19. Science 368:551
Recovery Trial Group (2020) Dexamethasone in hospitalized patients with COVID-19 — preliminary report. N Engl J Med. https://doi.org/10.1056/NEJMoa2021436
Rolain J-M, Colson P, Raoult D (2007) Recycling of chloroquine and its hydroxyl analogue to face bacterial, fungal and viral infections in the 21st century. Int J Antimicrob Agents 30:297–308
Yao T-T, Qian J-D, Zhu W-Y, Wang Y, Wang G-Q (2020) A systematic review of lopinavir therapy for SARS coronavirus and MERS coronavirus – a possible reference for coronavirus disease-19 treatment option. J Med Virol 92:556–563
Hernandez AV, Roman YM, Pasupuleti V, Barboza JJ, White CM (2020) Hydroxychloroquine or chloroquine for treatment or prophylaxis of COVID-19: a living systematic review. Ann Intern Med 173:287–296
Boulware DR, Pullen MF, Bangdiwala AS et al (2020) A randomized trial of hydroxychloroquine as postexposure prophylaxis for COVID-19. N Engl J Med 383:517–525
Tostmann A, Bradley J, Bousema T et al (2020) Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020. Euro Surveill Bull Eur Sur Mal Transm Eur Commun Dis Bull. https://doi.org/10.2807/1560-7917.ES.2020.25.16.2000508
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323:1239–1242
Magagnoli J, Narendran S, Pereira F, Cummings TH, Hardin JW, Sutton SS, Ambati J (2020) Outcomes of hydroxychloroquine usage in United States Veterans Hospitalized with COVID-19. Med N Y N. https://doi.org/10.1016/j.medj.2020.06.001
Sayare S (2020) He was a science star. Then he promoted a questionable cure for COVID-19. N. Y. Times
Amirian ES, Levy JK (2020) Current knowledge about the antivirals remdesivir (GS-5734) and GS-441524 as therapeutic options for coronaviruses. One Health Amst Neth 9:100128
Xie Y-C, Ogah CA, Jiang X, Li J, Shen J (2016) Nucleoside inhibitors of hepatitis C virus NS5B polymerase: a systematic review. Curr Drug Targets. https://doi.org/10.2174/1389450117666151209123751
Grein J, Ohmagari N, Shin D et al (2020) Compassionate use of remdesivir for patients with severe COVID-19. N Engl J Med 382:2327–2336
Gordon CJ, Tchesnokov EP, Feng JY, Porter DP, Gotte M (2020) The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus. J Biol Chem AC120:013056
Agostini ML, Andres EL, Sims AC et al (2018) Coronavirus Susceptibility to the Antiviral Remdesivir (GS-5734) Is Mediated by the Viral Polymerase and the Proofreading Exoribonuclease. mBio. https://doi.org/10.1128/mBio.00221-18
Pruijssers AJ, Denison MR (2019) Nucleoside analogues for the treatment of coronavirus infections. Curr Opin Virol 35:57–62
de Wit E, Feldmann F, Cronin J, Jordan R, Okumura A, Thomas T, Scott D, Cihlar T, Feldmann H (2020) Prophylactic and therapeutic remdesivir (GS-5734) treatment in the rhesus macaque model of MERS-CoV infection. Proc Natl Acad Sci U S A 117:6771–6776
Lo MK, Feldmann F, Gary JM et al (2019) Remdesivir (GS-5734) protects African green monkeys from Nipah virus challenge. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aau9242
Warren TK, Jordan R, Lo MK et al (2016) Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature 531:381–385
Williamson BN, Feldmann F, Schwarz B et al (2020) Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. bioRxiv. https://doi.org/10.1101/2020.04.15.043166
Mulangu S, Dodd LE, Davey RT et al (2019) A randomized, controlled trial of ebola virus disease therapeutics. N Engl J Med 381:2293–2303
Bhatraju PK, Ghassemieh BJ, Nichols M et al (2020) COVID-19 in critically ill patients in the Seattle Region — case series. N Engl J Med. https://doi.org/10.1056/NEJMoa2004500
Siddiqi HK, Mehra MR (2020) COVID-19 illness in native and immunosuppressed states: a clinical–therapeutic staging proposal. J Heart Lung Transplant 39:405–407
Wang K, Gheblawi M, Oudit GY (2020) Angiotensin converting enzyme 2: a Double-Edged Sword. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.120.047049
Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL (2016) Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol 1:274–281
Mehra MR, Ruschitzka F (2020) COVID-19 illness and heart failure. JACC Heart Fail 8:512–514
Karlberg J, Chong DSY, Lai WYY (2004) Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol 159:229–231
Klein SL, Flanagan KL (2016) Sex differences in immune responses. Nat Rev Immunol 16:626–638
Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S (2017) Sex-based differences in susceptibility to SARS-CoV infection. J Immunol Baltim Md 1950(198):4046–4053
Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN (2020) Cardiovascular disease, drug therapy, and mortality in COVID-19. N Engl J Med 382:e102
Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G (2020) Renin–angiotensin–aldosterone system blockers and the risk of COVID-19. N Engl J Med 382:2431–2440
Reynolds HR, Adhikari S, Pulgarin C et al (2020) Renin–angiotensin–aldosterone system inhibitors and risk of COVID-19. N Engl J Med 382:2441–2448
Mehta N, Kalra A, Nowacki AS et al (2020) Association of use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.1855
de Abajo FJ, Rodríguez-Martín S, Lerma V et al (2020) Use of renin–angiotensin–aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. The Lancet 395:1705–1714
Lu R, Zhao X, Li J et al (2020) Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet Lond Engl 395:565–574
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh C-L, Abiona O, Graham BS, McLellan JS (2020) Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 367:1260–1263
Gruber CC, Steinkellner G (2020) Wuhan coronavirus 2019-nCoV – what we can find out on a structural bioinformatics level. https://doi.org/10.6084/m9.figshare.11752749.v3
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ahmed, S., Rehman, H., Salar, R., Bin-Jumah, M.N., Sultan, M.T., Moga, M. (2021). Drugs for the Treatment of COVID-19. In: Zia-Ul-Haq, M., Bin-Jumah, M.N., Alothman, S.I., Henidi, H.A. (eds) Alternative Medicine Interventions for COVID-19. Springer, Cham. https://doi.org/10.1007/978-3-030-67989-7_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-67989-7_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67988-0
Online ISBN: 978-3-030-67989-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)