Abstract
By restoring decayed, traumatized, or missing tooth tissues, dentists introduce a new substrate into the oral cavity, to which dental biofilm (plaque) can adhere and accumulate. Even though microbial adhesion and biofilm development and maturation on a dental material surface follow some general patterns, these processes also depend on the properties of the material itself. There are specific interactions between dental materials and the overlying biofilms. On the one hand, materials can directly affect biofilms by releasing bioactive compounds, which gives an opportunity for the biofilm control and the prevention of secondary caries and other oral infectious diseases. On the other hand, dental plaque has a potential to modify the restorative material’s surface properties, such as surface roughness and topography, which might boost bacterial accumulation and eventually compromise restoration’s longevity. Resin-based composites, which are the most commonly used restorative materials nowadays, seem to be particularly prone to biofilm-induced degradation, since a well-known cariogenic species, Streptococcus mutans, can produce enzymes with esterase activity, capable of breaking down the polymer matrix of composites. However, the regulatory mechanisms behind the production and activity of such enzymes within a large community of different species in dental plaque remain obscure.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
7.1.1 Biofilms and Dental Materials: General Terms
As mentioned already many times throughout this book, biofilms are surface-associated aggregates or communities of microbial cells, which are embedded in a self-produced extracellular matrix (ECM) or extracellular polymeric substance (EPS) [1]. The fact that they are developing at a surface or an interface distinguishes biofilm microbial cells substantially from their planktonic or free-living counterparts. First, in order to initially attach to the surface, microbial cells need to express phenotypes which would allow them to do so. Initial attachment allows cells to stay in close proximity and to start interacting with the cells from the same, but also from different bacterial species, thereby developing a complex multicellular community, in which they express a number of new, so-called emergent properties [2]. One of these properties is the production of ECM, which is essential for the structure and functioning of a biofilm.
Biofilms are one of the most ubiquitous modes of life on Earth. They colonize soil, natural aquatic systems, and all higher organisms including humans, but also industrial and potable water systems, medical devices, ship hulls, etc. It seems that solid-liquid interfaces between a solid surface and an aqueous medium are particularly suitable for biofilm development, due to their constant need for hydration [1]. One of these kinds of habitats is definitely an oral cavity. Oral cavity is a host of more than 700 microbial species, which grow either as planktonic cells or in the form of biofilms, widely known as dental plaque, developing on oral soft and hard tissues [3, 4]. In addition, dental plaque may develop on the surface of a wide variety of dental materials introduced into an oral cavity as a part of oral rehabilitation.
Even though biofilms have a number of important functions in nature, such as biogeochemical cycling and symbiotic relationship with a number of plant and animal species, including humans, their presence often has negative effects. Accumulation of different micro- (and macro-) organisms on the wetted surfaces or solid-liquid interfaces, commonly known as biofouling, might have a deleterious effect on the underlying surfaces themselves, as well as on the whole systems (artificial or living) these surfaces are part of [5]. Oral cavity is no exception here. Even though the oral microbiome, as a part of the whole human microbiome, plays a critical role in many metabolic, physiological, and immunological processes, such as maturation and differentiation of host mucosa and immune system, food digestion and nutrition, and protection from pathogenic microorganisms, it can, under certain circumstances, cause some of the most prevalent dental diseases such as caries, gingivitis, and periodontitis [4]. In addition, plaque accumulation on dental restorative materials can have a negative impact not only on the surrounding tissues, but also on the underlying materials, which might seriously affect their clinical performance.
As soon as they are introduced in the oral cavity, dental materials start interacting with oral bacteria. These interactions are of paramount importance in the process of the bacterial adhesion and biofilm formation and accumulation on the materials, and they remain important throughout the whole service of the material in mouth. Dental restorative materials include a broad spectrum of materials, such as metals and alloys, amalgams, ceramics, polymers, and composites, all of which interact with oral biofilms in a distinct manner. The interaction is per definition a mutual or reciprocal action or influence (Merriam-Webster’s dictionary). Since the effect of various bioactive and antibacterial materials on the biofilms has already been discussed in the previous few chapters, the main focus of this chapter will be the manners in which oral biofilms can affect the underlying restorative materials and the performance of dental restorations. Also, the focus will mainly be laid on the most commonly used dental materials for direct dental restorations, namely dental composites and dental amalgams. Even though dental amalgams have been the standard restorative for more than a century, their use has been gradually abandoned in many developed countries due to their poor esthetics, as well as health and environmental concerns [6, 7]. Dental composites, on the other hand, have become a gold standard for dental restorations, due to their ability to adhesively bond to a tooth, thereby supporting the preservation of healthy tooth tissues, their versatility, esthetics, easy handling, etc. Nevertheless, it seems that conventional dental composites have a shorter longevity and a higher replacement rate than amalgams, which has mainly been attributed to their higher susceptibility to secondary or recurrent caries (SC) [8,9,10]. In addition, composites seem to be less resistant to the degradation in a quite challenging environment such as the oral cavity, especially by biological factors including oral bacteria [11]. This has brought restorative material-biofilm interactions into the spotlight, since it could give a better insight into the secondary caries process and failures of different restorations and help improve new generations of restorative materials.
The term “biodeterioration” is suitably used when talking about the impairment of function and/or esthetic properties of synthetic polymer materials by microorganisms [5]. This is mainly done through the decomposition of the polymer chains by the microbial activity, or so-called biodegradation. In the remainder of this chapter, these terms will be used to discuss biofilm-induced alterations of dental composites and adhesives, since their organic component, a resinous matrix, which actually undergoes degradation, is a polymer in chemical terms. On the other hand, dental amalgams are composed of a mixture of metal alloys, and microbial deposition on amalgam restorations might induce a corrosion process, known as “biocorrosion.”
7.1.2 Relevant Aspects of Biofilms
Biofilm formation on hard oral surfaces, including dental materials, follows a general pattern and consists of the following steps: acquired pellicle formation, initial bacterial cell attachment or so-called primary/early colonization, secondary colonization or co-aggregation, and biofilm maturation, which could be followed by cell detachment and dispersion [12, 13]. This process is, however, affected by many factors, including a number of environmental and host factors (temperature, pH, oxygen levels, nutrient availability, shear stresses, antimicrobial peptides, etc.) and bacterial cell factors (hydrophobicity, presence of fimbriae and flagella, production of EPS), but also various properties of the substrate (surface roughness and topography, stiffness, charge, hydrophobicity, chemical composition) [1, 14]. It is thus no wonder that both quantitative and qualitative differences in biofilms growing on different dental materials have been reported. It has been shown that conventional composites accumulate more biofilms on their surface compared to amalgams and glass ionomer cements [15]. In addition, it seems that plaque growing on composites contains a higher proportion of cariogenic species, such as mutans streptococci and lactobacilli [16, 17]. This could be explained by the lack of antibacterial properties of composites compared to other two restoratives, or by the lack of buffering or pH-neutralizing abilities [18]. Nevertheless, it can definitely make composites more exposed and more susceptible to biodegradation, especially by cariogenic species, which as a matter of fact seem to have a higher biodegradation potential.
Irrespective of the substrate, the basic structure of mature biofilms includes densely packed microbial cells (from 108 to 1011 cells per gram wet weight), self-produced extracellular polymeric substance (EPS), and interstitial pores and channels which facilitate transport of water and metabolites [2]. EPS comprises the largest part of the biofilm mass (75–95%) and is of the greatest importance in the interactions between the biofilm and the substrate [13]. EPS mediates the biofilm growth at the surface of the substrate and it imparts various important properties to the biofilms, such as resource capture by sorption, enzyme retention and digestive capacities, intercellular interactions (competition and cooperation) and metabolism, and resistance to desiccation and antimicrobials.
EPS is actually capable of retaining and stabilizing extracellular enzymes secreted by bacterial cells, which allows it to function as a sort of an external digestive system. In this way, the concentration and thereby the efficacy of bacterial enzymes are substantially higher than in case of planktonic cells, where enzymes easily diffuse and get diluted after the secretion. This enzymatic system is important for the digestion of the nutrients taken up from the environment, but it also allows biofilm to attack the substrate it is attached to, as it will be discussed later in this chapter. In addition, processes of sorption and accumulation of various compounds from the environment and the compounds released from the substrate play an important role in the modulation of bioactivity and toxicity of dental materials. These two important functions of the EPS are schematically presented in Fig. 7.1 [2].
Capturing and retention of external resources as well as extracellular bacterial enzymes by EPS in biofilms [2]. (Permission obtained from Springer Nature, license number 4710220788887)
7.2 Biofilms and Amalgam Restorations
Dental amalgams have been for a long time considered a gold standard among restorative materials. Nevertheless, during the last two decades the use of amalgams has been on a steady decline, and in many developed countries it is nowadays merely used, or even banned, due to health and environmental concerns [19]. Minamata Convention on Mercury (2013) is an international treaty, which proposed a number of measures to decrease anthropogenic emission and release of mercury, including the phasedown of dental amalgams, and their replacement with mercury-free alternatives. However, due to a relatively simple and insensitive placement technique, high longevity, and unparalleled cost-effectiveness of amalgams, they are still widely used, especially in low- and middle-income countries [20].
Amalgams are alloys of mercury and other metals, such as silver, tin, copper, and metallic elements added to improve their physical and mechanical properties (ADA, 2011). Dental amalgams are the only metallic materials for direct tooth restorations, and their interactions with the oral environment differ substantially from the interactions of dental composites or glass ionomer cements, which both consist of inorganic as well as organic components. Amalgams have arguably the highest longevity among direct restoratives, and it seems that they perform particularly better compared to composites in patients with high caries risk [21]. A closer look into the specific interactions between amalgams and oral biofilms could perhaps offer an explanation for their higher resilience in oral cavity.
Accumulation of oral biofilms on the surface of dental amalgams has a potential to cause a bacterium-induced corrosion or so-called biocorrosion. With regard to its mechanism, biocorrosion belongs to concentration cell type of corrosion, which is an electrochemical corrosion that occurs when there is a difference in the electrolyte composition within one system. For instance, when the surface of an alloy is covered by biofilm or another kind of debris, which can produce an electrolyte different from the one at the rest of the surface (saliva), corrosion might take place. Accumulation of bacterial metabolic products, including organic acids, causes the drop in local pH, which together with the depletion of oxygen leads to the formation of a corrosion cell. This further causes the release of metal ions and the formation of corrosion products [22] (Fig. 7.2). This process is especially accelerated in surface defects, such as pits and cracks, since these areas are oxygen deprived. It is therefore important to polish amalgam restorations, in order to obtain a smooth and homogenous surface less prone to plaque accumulation and corrosion.
Biocorrosion has a two-sided effect on dental amalgam restorations. On the one hand, it can lead to the release of free metal ions from amalgam, especially zinc, copper, and tin, and at much lower rate silver and mercury [23]. The release of metal ions due to corrosion process is important from the aspect of biocompatibility and toxicity of amalgams, and it has therefore been a research focus for a long time. It appears that the presence of biofilms at the surface of amalgam restorations plays another role here since they can capture and accumulate the released ions by sorption process, which actually retards their release into the oral environment [24]. On the other hand, corrosion leads to the formation of solid nonmetallic compounds, such as oxides, hydroxides, and chlorides of tin, copper, and zinc. These products mostly stay bound to amalgam structure or form a layer on top of it. Even though the formation of corrosion products might affect the mechanical properties of amalgams and lead to increased abrasion and fragmentation, there is also a positive aspect of it. Namely, the formation of corrosion products at amalgam-tooth interface, where a so-called crevice corrosion often occurs, can seal the interfacial gap and prevent microleakage and its consequences, such as postoperative sensitivity and secondary caries [25]. Owing to this phenomenon, amalgams could be considered the only restorative materials with a self-sealing capacity.
It should also be mentioned that not all amalgams are equally prone to biocorrosion, or for that matter to any type of corrosion. High-copper amalgams are reported to be more electrochemically stable than low-copper amalgams. The reason for this is that in high-copper amalgams the amount of tin-mercury phase (gamma two, γ2) is reduced, or it is completely replaced by copper-tin phase (eta prime, ƞ′), which is more resistant to corrosion. This resistance to corrosion contributes to improved mechanical properties and clinical performance of high-copper amalgams, but what is also important, it does not affect considerably their self-sealing abilities [25].
Finally, biocorrosion of dental amalgams should be distinguished from amalgam tarnishing, which is a discoloration (darkening) of amalgam restoration surface due to the formation of a thin, adherent, and insoluble film at its surface, consisting mainly of silver and copper sulfides. Although they negatively affect the esthetics of amalgam restorations (loss of luster), they do not seem to affect mechanical and functional properties of amalgams, and are even considered to act protectively against the corrosion.
7.3 Biodeterioration of Dental Composites
As mentioned above, dental composites seem to accumulate more plaque compared to dental amalgams and glass ionomer cements. This makes them in a way more exposed to the adverse effects of biofilms or biodeterioration. Nevertheless, dental composites are the most commonly used restorative materials and it is of utmost importance to have a better understanding of the damage they might suffer due to plaque accumulation and the biodegradation processes taking place in oral cavity.
Biodeterioration of composites is considered to be able to seriously compromise the function and longevity of composite restorations, and it has been therefore extensively investigated during the last decade. It appears that various properties of dental composite restorations could be altered through the biofilm accumulation and the biodeterioration process, such as their surface properties (roughness and topography), mechanical properties, marginal integrity, and esthetics. The extent of these alterations, their clinical relevance, and the potential clinical repercussions will be discussed in the following paragraphs. Following that, the underlying mechanisms of biodeterioration and composite biodegradation will be tackled, as well as the current approaches to improve the resistance of contemporary composites to biodegradation.
7.3.1 Effect on Surface Properties of Composites
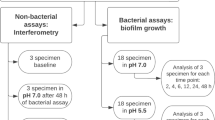
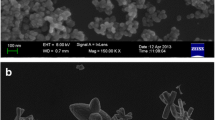
Since biofilms attach and develop at the restoration surface, that is expectedly the part of a restoration first affected by microbial degradation. Influence of biodegradation on the surface properties of composites, such as surface roughness, topography, and surface hardness, has therefore been most extensively investigated in literature to date. Several studies demonstrated that cariogenic species S. mutans can degrade the surface of dental composites, and thereby increase the surface roughness and change the surface topography [26, 27]. This has gained a lot of attention since the increase in surface roughness can boost further bacterial accumulation. Nevertheless, it seems that this effect depends on the type of biofilm used in in vitro studies. Gregson et al. (2012) have shown that cariogenic species S. mutans can noticeably change surface topography of composites and increase its roughness, while a non-cariogenic species S. sanguinis does not exhibit the same biodegradation potential [28]. In another in vitro study a significant increase in surface roughness of two composites after 6-week incubation with S. mutans single-species biofilms was found, while there was no significant increase in roughness after the exposure to a multispecies model, consisting of S. mutans, S. sanguinis, A. naeslundii, and F. nucleatum [29] (Fig. 7.3). Even though it was shown that few other oral species, such as S. gordonii and A. naeslundii, also have the ability to degrade the composite surface and increase its roughness [28, 30], most of the studies are focused exclusively on the “old villain” S. mutans. However, in the light of the latest research, which suggests that biodegradation potential of S. mutans diminishes when co-cultured with other species, clinical relevance of the in vitro studies on composite biodegradation using single-species models with S. mutans should be questioned, especially considering the fact that dental plaque is a community of more than 700 species.
Root mean square (RMS) roughness values of the samples of two composites measured by atomic force microscopy (AFM) at lower (a) and higher (b) resolution, at baseline (Baseline), and after 6-week incubation under the following conditions: in sterile bacterial growth medium (BHI), with S. mutans biofilm (S. mutans), with mixed four-species biofilm (Mixed), in sterile bacterial growth medium with pH adjusted to 5 (BHI(pH 5)), and in cholesterol esterase solution in PBS (CE) [29]. (Permission obtained from Elsevier, license number 4710221190144)
Another critical question here is whether the increase in surface roughness observed in the abovementioned in vitro studies is clinically relevant and whether it can actually lead to an increase in bacterial accumulation. Teughels et al. tried to determine a critical value of surface roughness above which a significant increase in bacterial accumulation can be observed [31]. The obtained average roughness (Ra) value of 200 nm (which corresponds to root mean square (RMS) value of 220 nm) is way much higher than the roughness measured on biofilm-exposed composite surfaces in in vitro studies, which approximately ranged from 10 to 50 nm [26, 29]. It therefore seems that the ability of certain oral bacterial species, such as S. mutans, to degrade the surface of dental composites has no potential to seriously compromise a clinical performance of composite restorations. It should however be kept in mind that bacterial degradation is only one of the modes of material degradation taking place in oral cavity. Its effect on restoration surface should be therefore investigated in combination with mechanical degradation or wear, in order to determine the possible synergistic effects.
7.3.2 Effect on Mechanical Properties and Wear
Apart from surface roughness and topography, it has been suggested that biofilms can affect other mechanical properties of composites, such as the surface hardness and the wear rate. The results of several in vitro studies, however, disputed this. No decrease in flexural strength and surface hardness was detected in composite specimens incubated with S. mutans, S. sanguinis, and S. gordonii biofilms for 6 weeks [28]. In another study, no change in surface hardness was detected after 1 month of incubation with S. mutans biofilm [26].
There is also no scientific evidence to date that the exposure of composites to biofilms or to the organic acids at the concentration found in dental plaque can increase the abrasion and wear of a composite surface [32, 33]. In addition, it is worth mentioning that biofilms hardly ever develop at the sites which typically experience wear, such as occlusal surfaces.
Based on the present literature it could be concluded that bacterial degradation of dental composites takes place at and is limited to the outer material surface, without affecting materials’ inner (bulk) structure and thereby their mechanical qualities.
7.3.3 Effect on Tooth-Composite Interface
Integrity of the tooth-restoration interface is crucial to achieving high longevity and optimal clinical performance of composite restorations. It seems, however, that during restoration service in oral cavity this interface may considerably deteriorate, which may eventually lead to the restoration failure [34]. Deterioration is a consequence of mechanical as well as biochemical degradation of different components of the interface, such as tooth mineral tissue, dentin collagen fibers, and adhesive layer. This can further lead to a so-called micro- and nanoleakage of bacteria and their metabolites, which can cause tooth sensitivity and development of secondary caries. It has recently been demonstrated that bacteria from dental plaque can significantly contribute to the interfacial degradation. As already mentioned above, S. mutans has an esterase activity at the levels that can degrade dental composites and adhesives [27].
Even though composite biodegradation taking place at the restoration surface might not have serious clinical consequences, as discussed above, the same cannot be said for the biodegradation happening at the tooth-composite interface. It has been demonstrated that enzymes similar to the ones produced by S. mutans could degrade the adhesive layer and create a gap large enough to allow bacterial colonization and formation of a biofilm [35]. This is particularly important since it has recently been shown that interfacial gaps of only around 30 μm in size could lead to the progression of secondary caries next to a composite restoration [36], which is considerably lower than previously thought [37, 38].
Biofilm degradation of the tooth-composite interface is also reflected on the bond strength between dentin and composite. Li et al. demonstrated a reduction in bond strength after specimen exposure to multispecies biofilms, especially in the presence of sucrose in the growth medium [39]. The observed reduction in bond strength has not been attributed only to the dentin demineralization, but also to the hydrolysis of the adhesive resin by either bacterium-produced acids or bacterium-produced enzymes.
7.3.4 Effect on Esthetic Properties of Composites
Excellent esthetic properties are one of the greatest assets of dental composites, and one of the main reasons for their high popularity among patients and dentists. Nevertheless, during their service in the mouth, the appearance of composite restorations can significantly deteriorate, and the discoloration they undergo can be per se a reason for the restoration replacement, especially in the esthetic zone. The percentage of composite restorations replaced due to bulk and marginal discoloration has been reported to range from 3% to as high as 22%, and was often reported to be the second or third most common reason for the replacement [40,41,42]. Furthermore, it appears that the staining of composite fillings is associated with patient’s poor oral hygiene, and accumulation of oral biofilms is often stated as an important intrinsic factor affecting color stability of composites [43, 44].
Nevertheless, the literature about the direct influence of biofilms on the deterioration of esthetic properties of composites is quite scarce. A relatively recent study investigated the effect of S. mutans biofilm on the color and translucency of experimental composites with and without bioactive glass fillers [45]. The results showed no difference in the change of optical properties after the exposure of the control composite to S. mutans culture and to the growth medium alone, which implies the absence of any direct effect of bacteria whatsoever. S. mutans biofilms were used in this study because of the high production of acids, which were long considered contributing factors to the color change of composites. There is, however, no sound scientific evidence for that, and more research with multispecies biofilm models is needed to get a better insight into direct effects of oral bacteria on optical properties of composites.
On the other hand, biodegradation of composites and adhesives could affect esthetics of composite restorations indirectly. An increased roughness of composite surface also means a larger surface for the adsorption of pigments from foods and beverages. It has been shown that different polishing techniques and initial roughness of composites can influence their color stability, but it seems that this depends to a great extent on the type of composite material [46]. Also, biodegradation of the adhesive bond can lead to the leakage and accumulation of pigments at the tooth-composite interface and cause marginal discoloration, which, as already mentioned, can be a reason for the restoration replacement.
7.3.5 Mechanisms of Bacterial Degradation
Composite biodegradation is based on the hydrolysis of the chemical bonds present in resin polymer matrix, such as ester, urethane, and amide bonds. Hydrolytic reaction can be catalyzed or facilitated by acids, bases, and also different enzymes, when we talk about enzymatic hydrolysis and enzymatic degradation. Bacteria from dental biofilms are known to be able to efficiently produce organic acids under cariogenic challenge, especially so-called cariogenic bacterial species, such as mutans streptococci and lactobacilli, which are present at higher proportions in cariogenic biofilms. Therefore, it has long been considered that the main mechanism of microbial degradation of composites in oral cavity is an acid-catalyzed hydrolysis [47]. During the recent years, however, it has been demonstrated that S. mutans species can produce enzymes from the class of esterases, similar to cholesterol esterase (CE) and pseudocholinesterase (PCE) found in saliva, which are able to degrade methacrylate monomers within composite matrix, such as TEGDMA and BisGMA. Moreover, the produced esterase remains stable and active even at low pH level of 5.5, which is found in cariogenic plaque [48]. The mechanism of microbial degradation of resin composites and adhesives can be thus regarded as a combination of acid- and enzyme-catalyzed hydrolytic degradation. Nevertheless, a recent study, which investigated the effect of biofilms on the surface of resin composites, suggested that bacterial enzymes, rather than acids, play a role in microbial degradation of composites, since no effect of bacterial growth medium with low pH (pH = 5) on the tested composites was observed [29] (Fig. 7.3).
Even though bacterium-produced acids have little contribution to the degradation of composite surface, their role in the interfacial degradation seems to be quite prominent. Apart from the demineralization of tooth mineral tissues, which is an important aspect of interfacial degradation, bacterium-produced acids could also be responsible for the activation of certain proteolytic enzymes present in saliva and in dentin. These enzymes are known as matrix metalloproteinases (MMPs) and cysteine cathepsins, and they are considered to play a part in the interfacial breakdown by degrading collagen fibrils in hybrid layer [49].
7.3.6 Susceptibility/Resistance to Biodegradation
Not all composites are equally prone to hydrolytic degradation, and the susceptibility to degradation largely depends on the material composition. In the first instance it is determined by the silanated filler fraction, as highly filled composites show a higher resistance to the biodegradation than composites with a lower filler content. This is no surprise considering the fact that the resin matrix is a vulnerable component of composites when it comes to chemical degradation, and in highly filled composites a smaller matrix surface is exposed to the activity of enzymes [50].
In addition, susceptibility to degradation is determined by the resin matrix chemistry, as certain types of resin monomers are more prone to hydrolysis than others. Ester bonds, which are present in most of the currently used monomers, are particularly susceptible to degradation. However, the presence of other chemical groups on monomer molecules and their interactions can affect their stability considerably. Among most commonly used resin monomers, which are presented in Fig. 7.4, triethylene glycol dimethacrylate (TEGDMA) seems to be the most susceptible to degradation [51]. A possible reason for this is the presence of ethylene glycol segments, which attract water molecules and increase the water uptake, leading to a higher chance for hydrolysis [11]. Aromatic cross-linking monomer bisphenol A-glycidyl methacrylate (BisGMA) and its ethoxylated version (BisEMA) are more stable than TEGDMA, due to the presence of hydrophobic aromatic rings in their backbone, which partly protect polar groups from water and hydrolysis. Nevertheless, their susceptibility to hydrolytic degradation is still quite high [52]. On the other hand, monomers containing urethane groups, such as urethane dimethacrylate (UDMA), but also urethane-modified BisGMA, show considerably lower susceptibility to degradation compared to other monomers present in contemporary composite materials [51, 52]. Urethane groups can form hydrogen-bonded structures which can restrict the access of enzymes to the cleavage sites, thereby delaying enzymatic reaction and protecting ester bonds in their vicinity from the hydrolysis. In addition, the elimination of hydroxyl groups by the formation of urethane links in urethane-modified BisGMA leads to an increased hydrophobicity of the monomer and a higher resistance to hydrolytic attack.
In the last years, much research has been devoted to designing new monomers with different chemistries, which would have a higher resistance to biodegradation in oral cavity. Several studies reported quite promising results with experimental monomers for composites, as well as for adhesive resins. Gonzalez-Bonet et al. synthesized and tested an ether-based monomer triethylene glycol divinylbenzyl ether (TEG-DVBE), which showed no signs of degradation in PBS, cholesterol esterase (CE), and pseudocholine esterase (PCE) solutions, compared with BisGMA and TEGDMA, which degraded at different levels [53]. Another group tested a quaternary methacrylamide-based ammonium fluoride and demonstrated a high resistance of this antibacterial monomer to hydrolysis in acidic environment [54].
7.4 Conclusions
Interactions between dental restorative materials and oral biofilms might be an important determinant of their clinical performance. Certain qualities of restorative materials, such as antibacterial and pH-neutralizing effect and lower plaque accumulation, but also higher resistance to bacterial degradation and biodeterioration in the oral cavity, can contribute to an improved longevity of dental restorations. This can explain superior longevity and resistance to secondary caries of dental amalgams, which do not seem to be adversely affected by oral biofilms. They can even benefit from the biocorrosion, since the solid by-products of corrosion can seal the gap at the tooth-restoration interface, thereby preventing microleakage and development of secondary caries.
On the other hand, dental composites seem to be more vulnerable to biodeterioration, which might affect various composite properties. The effect of biofilms on surface roughness and mechanical properties, such as surface hardness and wear, seems not to pose a clinical problem. However, bacterial degradation can contribute to the disintegration of the tooth-composite interface in multiple ways, including the breakdown of the adhesive layer, tooth mineral tissues, and dentin collagen. Interfacial degradation, in its turn, can lead to marginal discoloration and deterioration of composite’s appearance. Nevertheless, the direct effect of oral biofilms, as well as the combined effect of biofilms and exogenous discoloring factors on esthetic properties of composite restorations, has been scarcely investigated and is still not clear.
Resin chemistry plays a crucial role in the resistance of composites to bacterial degradation. The research on designing new, more biochemically stable formulations of resin monomers is gaining increasing attention, and encouraging results have already been reported. Improved biostability of dental composites would help to improve their clinical performance and prolong their service in mouth.
References
Donlan RM. Biofilms: microbial life on surfaces. Emerg Infect Dis. 2002;8(9):881–90.
Flemming HC, et al. Biofilms: an emergent form of bacterial life. Nat Rev Microbiol. 2016;14(9):563–75.
Samaranayake L, Matsubara VH. Normal oral flora and the oral ecosystem. Dent Clin N Am. 2017;61(2):199–215.
Kilian M, et al. The oral microbiome—an update for oral healthcare professionals. Br Dent J. 2016;221(10):657–66.
Flemming HC. Biodeterioration of synthetic materials—a brief review dedicated to Professor Dr. Wolfgang Sand on the occasion of his 60th birthday. Mater Corros—Werkstoffe Und Korrosion. 2010;61(12):986–92.
Forss H, Widstrom E. From amalgam to composite: selection of restorative materials and restoration longevity in Finland. Acta Odontol Scand. 2001;59(2):57–62.
Sunnegardh-Gronberg K, et al. Selection of dental materials and longevity of replaced restorations in Public Dental Health clinics in northern Sweden. J Dent. 2009;37(9):673–8.
Opdam NJ, et al. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater. 2007;23(1):2–8.
Bernardo M, et al. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc. 2007;138(6):775–83.
Moraschini V, et al. Amalgam and resin composite longevity of posterior restorations: a systematic review and meta-analysis. J Dent. 2015;43(9):1043–50.
Delaviz Y, Finer Y, Santerre JP. Biodegradation of resin composites and adhesives by oral bacteria and saliva: a rationale for new material designs that consider the clinical environment and treatment challenges. Dent Mater. 2014;30(1):16–32.
Marsh PD. Dental plaque as a biofilm and a microbial community—implications for health and disease. BMC Oral Health. 2006;6(Suppl 1):S14.
Huang R, Li M, Gregory RL. Bacterial interactions in dental biofilm. Virulence. 2011;2(5):435–44.
Song F, Koo H, Ren D. Effects of material properties on bacterial adhesion and biofilm formation. J Dent Res. 2015;94(8):1027–34.
Zhang N, et al. Do dental resin composites accumulate more oral biofilms and plaque than amalgam and glass ionomer materials? Materials (Basel). 2016;9(11):888.
Svanberg M, Mjor IA, Orstavik D. Mutans streptococci in plaque from margins of amalgam, composite, and glass-ionomer restorations. J Dent Res. 1990;69(3):861–4.
Thomas RZ, et al. Bacterial composition and red fluorescence of plaque in relation to primary and secondary caries next to composite: an in situ study. Oral Microbiol Immunol. 2008;23(1):7–13.
Nedeljkovic I, et al. Lack of buffering by composites promotes shift to more cariogenic bacteria. J Dent Res. 2016;95(8):875–81.
Kopperud SE, et al. The post-amalgam era: Norwegian dentists’ experiences with composite resins and repair of defective amalgam restorations. Int J Environ Res Public Health. 2016;13(4):441.
Fisher J, et al. The Minamata convention and the phase down of dental amalgam. Bull World Health Organ. 2018;96(6):436–8.
Opdam NJ, et al. 12-year survival of composite vs. amalgam restorations. J Dent Res. 2010;89(10):1063–7.
Anusavice KJ, Phillips RW. Phillips’ science of dental materials. 11th ed. St. Louis, MO: Saunders; 2003. p. xxv, 805 p.
Marek M. Interactions between dental amalgams and the oral environment. Adv Dent Res. 1992;6:100–9.
Steinberg D, Blank O, Rotstein I. Influence of dental biofilm on release of mercury from amalgam exposed to carbamide peroxide. J Biomed Mater Res B Appl Biomater. 2003;67(1):627–31.
Mahler DB, Pham BV, Adey JD. Corrosion sealing of amalgam restorations in vitro. Oper Dent. 2009;34(3):312–20.
Beyth N, et al. Streptococcus mutans biofilm changes surface-topography of resin composites. Dent Mater. 2008;24(6):732–6.
Bourbia M, et al. Cariogenic bacteria degrade dental resin composites and adhesives. J Dent Res. 2013;92(11):989–94.
Gregson KS, Shih H, Gregory RL. The impact of three strains of oral bacteria on the surface and mechanical properties of a dental resin material. Clin Oral Investig. 2012;16(4):1095–103.
Nedeljkovic I, et al. Biofilm-induced changes to the composite surface. J Dent. 2017;63:36–43.
Willershausen B, et al. The influence of oral bacteria on the surfaces of resin-based dental restorative materials—an in vitro study. Int Dent J. 1999;49(4):231–9.
Teughels W, et al. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006;17(Suppl 2):68–81.
de Paula AB, et al. Biodegradation and abrasive wear of nano restorative materials. Oper Dent. 2011;36(6):670–7.
de Gee AJ, et al. Influence of enzymes and plaque acids on in vitro wear of dental composites. Biomaterials. 1996;17(13):1327–32.
Hashimoto M, et al. In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. J Dent Res. 2000;79(6):1385–91.
Kermanshahi S, et al. Biodegradation of resin-dentin interfaces increases bacterial microleakage. J Dent Res. 2010;89(9):996–1001.
Maske TT, et al. Minimal gap size and dentin wall lesion development next to resin composite in a microcosm biofilm model. Caries Res. 2017;51(5):475–81.
Thomas RZ, et al. Approximal secondary caries lesion progression, a 20-week in situ study. Caries Res. 2007;41(5):399–405.
Kuper NK, et al. Gap size and wall lesion development next to composite. J Dent Res. 2014;93(7 Suppl):108S–13S.
Li Y, et al. Degradation in the dentin-composite interface subjected to multi-species biofilm challenges. Acta Biomater. 2014;10(1):375–83.
Chrysanthakopoulos NA. Reasons for placement and replacement of resin-based composite restorations in Greece. J Dent Res Dent Clin Dent Prospects. 2011;5(3):87–93.
Burke FJ, et al. Influence of patient factors on age of restorations at failure and reasons for their placement and replacement. J Dent. 2001;29(5):317–24.
Mjor IA, Moorhead JE, Dahl JE. Reasons for replacement of restorations in permanent teeth in general dental practice. Int Dent J. 2000;50(6):361–6.
Asmussen E, Hansen EK. Surface discoloration of restorative resins in relation to surface softening and oral hygiene. Scand J Dent Res. 1986;94(2):174–7.
Ceci M, et al. Discoloration of different esthetic restorative materials: a spectrophotometric evaluation. Eur J Dent. 2017;11(2):149–56.
Hyun HK, Ferracane JL. Influence of biofilm formation on the optical properties of novel bioactive glass-containing composites. Dent Mater. 2016;32(9):1144–51.
Guler AU, et al. Effects of polishing procedures on color stability of composite resins. J Appl Oral Sci. 2009;17(2):108–12.
Borges MA, et al. Degradation of polymeric restorative materials subjected to a high caries challenge. Dent Mater. 2011;27(3):244–52.
Huang B, et al. Esterase from a cariogenic bacterium hydrolyzes dental resins. Acta Biomater. 2018;71:330–8.
Zhang SC, Kern M. The role of host-derived dentinal matrix metalloproteinases in reducing dentin bonding of resin adhesives. Int J Oral Sci. 2009;1(4):163–76.
Finer Y, Santerre JP. Influence of silanated filler content on the biodegradation of bisGMA/TEGDMA dental composite resins. J Biomed Mater Res A. 2007;81(1):75–84.
Finer Y, Santerre JP. The influence of resin chemistry on a dental composite’s biodegradation. J Biomed Mater Res A. 2004;69(2):233–46.
Hagio M, et al. Degradation of methacrylate monomers in human saliva. Dent Mater J. 2006;25(2):241–6.
Gonzalez-Bonet A, et al. Preparation of dental resins resistant to enzymatic and hydrolytic degradation in oral environments. Biomacromolecules. 2015;16(10):3381–8.
Decha N, et al. Synthesis and characterization of new hydrolytic-resistant dental resin adhesive monomer HMTAF. Des Monomers Polym. 2019;22(1):106–13.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Nedeljkovic, I. (2021). Effect of Oral Biofilms on Dental Materials: Biocorrosion and Biodeterioration. In: Ionescu, A.C., Hahnel, S. (eds) Oral Biofilms and Modern Dental Materials . Springer, Cham. https://doi.org/10.1007/978-3-030-67388-8_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-67388-8_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67387-1
Online ISBN: 978-3-030-67388-8
eBook Packages: MedicineMedicine (R0)