Abstract
The interactions taking place between a dental (bio)material, the surrounding tissues of the host, and the biofilm that grows to permanently colonize this microenvironment are amazingly complex when analyzed in detail yet contribute to a crucial factor: the balance between health and disease conditions. From a microbiological point of view, this has a dramatic impact on the longevity of dental treatments. Researchers have long since tried to recreate, even if in parts, this complexity on a bench, both using a reductionistic approach as often performed in research and, more recently, by trying to create models approaching the most realistic behavior. These efforts yielded a wide range of bioreactor systems currently available. We hope that in a future not too far, bioreactor models will be able to reliably reproduce most clinical conditions, dramatically reducing the need for animal and clinical studies. Unfortunately, a universal bioreactor able to mimic any clinical situation still does not exist. Each model comes entwined with its advantages and limitations that must be acknowledged when choosing which model best fits a distinct experimental design. This situation, together with a reduced overall level of standardization, makes the comparison of the obtained results very difficult. This chapter presents an overview of the microbial communities and the bioreactor models that are most significant for studying the microbiological performances of dental materials.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bioreactors
- Microfluidics
- Biofilms
- Oral microcosm
- Defined consortium
- Streptococcus mutans
- Standardization
4.1 Introduction: The Need for Modeling Biofilms in the Lab
Teeth and any dental restorative material, including fixed and removable prosthodontic devices, are non-shedding surfaces, unlike the rest of the surfaces of our body that come into contact with the external environment. As explained in Chaps. 1 and 2, this leads to a unique sequence of events that begins with salivary pellicle formation on intraoral surfaces and finally leads to the development of a mature microbial biofilm firmly attached to these substrates. The presence of shear stresses is one of the most critical driving forces that modulate biofilm formation in the oral environment. In fact, it is primarily responsible for microbial growth as a biofilm community instead of planktonic cells, which can be easily washed away. In this sense, analysis of the fluidodynamics at the interface between microorganisms and hard surfaces is critical to explain many of the fundamental aspects of dental biofilms [1].
In this confined yet highly dynamic microenvironment, microorganisms, surface characteristics of the interface, an array of factors deriving from the host, and external factors such as, most importantly, nutrient intake all contribute to biofilm formation. All of these factors are involved in a biofilm’s community balance between health and disease conditions [2]. It is easy to understand that this system has an extreme implicit complexity and is also responsible for the very high inter- and intraindividual variability commonly observed [3, 4]. The design of most in vivo studies dealing with biofilm formation collides with this complexity even if only relatively simple research questions shall be answered. It is also noteworthy that many of the novel materials and technologies that are developed in a struggle to control and modulate microbial colonization and biofilm formation cannot be directly applied in vivo as a result of obvious ethical concerns.
A major part of the hospital-acquired infections is due to biofilm-forming pathogens [5]. Almost all infections of temporary and permanent indwelling devices are characterized by biofilm formation [6]. Many different bacterial species, such as Pseudomonas aeruginosa, Staphylococcus aureus, and even saprophyte species such as Candida albicans, are associated with biofilm infections of indwelling devices that can lead to the chronicization of a disease or to complete failure of the therapy in many different regions of the human body. To reduce the occurrence of such adverse events, the study of biofilms in the medical setting is, therefore, of highest importance. The in vivo approach to study biofilms is still extremely challenging due to the reduced possibility of controlling experimental parameters and, again, to the indispensable ethical concerns that may arise [7]. New strategies are required to simulate the clinical situation in vitro, and several experimental data have been published in the last years on biofilm formation under different conditions and strategies aimed to control their colonization of human tissues [8,9,10]. Several types of artificial systems, called bioreactors, have been proposed for this issue; basically, they try to mimic the environmental conditions of biofilm development on the surface or inside the human body. The ultimate aim of the bioreactors is to obtain biofilm structures that are functionally and morphologically similar to those found in health or disease conditions, by reproducing most of the conditions found in the human body [2, 11]. Most of the parameters that define these conditions are nowadays reproducible in vitro—for instance, the use of media that simulate the human fluid composition, its flow, the presence of nutrients, the oxygen levels, the adherence and growth substrates, and the temperature (Fig. 4.1). However, some parameters and conditions are still considerably challenging to reproduce; this includes, for example, the host immune response. The latter has a crucial influence on the growth and structure of biofilms, yet this interaction is still not possible to be reproduced in vitro.
Semi-thin section (150 μm wide) seen at optical microscopy of a S. mutans microcolony developing over the surface of the resin component of a dentin-bonding system (1:1 vol BisGMA:TEGDMA resin). The specimen was cultured in a continuous-flow bioreactor (MDFR) for 96 h. Cells and extracellular matrix are colored in violet. It can be seen that, immediately after adhering to the surface, bacteria start replicating forming a monolayer and producing the extracellular matrix in which they are embedded and that protects them. After that, biofilm formation takes place with the development of microcolonies and the production of an excess of extracellular matrix that forms a “tail,” here stained in light violet. The latter originates from the microcolony and is situated in an upward position due to the lack of hydrodynamic shear during specimen processing. Under flow conditions, the tail is oriented downstream and can be detached by high shear stresses or by the “decision” of the bacteria themselves through quorum sensing to depolymerize the extracellular matrix to be able to go and colonize other surfaces downstream. The necessity of replicating such behavior in vitro is paramount to approach the clinical behavior of the studied biofilms. (Specimen preparation and observation courtesy of Dr. Vincenzo Conte and Prof. Patrizia Procacci, University of Milan, Italy)
Despite that, the bioreactors allow for testing of a relatively large number of specimens under very defined conditions. The variability associated with the environmental conditions is thus significantly reduced, and the experimental parameters that are studied can be reliably controlled [7, 11, 12].
In the oral environment, biofilm development is a commonly occurring event. Researchers have attempted for years to find a way to disrupt and prevent biofilm formation, with generally poor results. The current trend is, on the contrary, to modulate the behavior of the oral biofilm in order to favor the growth of nonpathogenic species selectively and to reduce the development and metabolism of pathogenic ones. This ecological perspective on biofilm studies has a deep impact on in vitro modeling since the whole complexity of the multispecies oral microflora has to be consistently reproduced and maintained for the desired experimental duration [13, 14]. This approach needs to be matched with sophisticated methodologies that are capable of assessing the prevalence of the different components of the microflora. Such technologies have only been available for a few years and add to the complexity of these studies [15, 16].
Bioreactors, when coupled with specific instruments for measuring biofilm characteristics, can be used as tools to “sense” the behavior of the microenvironment in a more subtle way than many modern instruments [10, 17, 18]. These setups can use growth conditions and parameters that are, on purpose, far from clinical situations. In this way, minimal amounts of drug release can be detected, as well as material surface modifications, and even accelerated aging of the exposed interfaces can be simulated (Fig. 4.2). For instance, considering caries research, a recent study highlighted that the effect of fluoride on S. mutans biofilm formation is dependent on the bacterial strain that is employed [19].
Semi-thin section of the previous specimen observed using transmission microscopy after 96 h of biofilm formation. A nutrient medium (undefined mucin medium) highly enriched in sucrose (5 wt.%) continuously fed through the bioreactor inlet causes extra production of acidic catabolites, extracellular matrix, and, possibly, esterases by S. mutans cells. This situation is far from clinical situations where biofilms are not composed by a single species, pH close to the surface does not reach such low values for such extended time, and a human being is not continuously fed with high amounts of simple carbohydrates as its only nutritional intake. Nevertheless, these extremized conditions of “accelerated microbiological aging” show the initial degradation of the resin surface that is expressed as an initial staining of subsurface layer with the hydrophilic electron-dense dyes, lead citrate and uranyl acetate. This type of study can provide further insight, for instance, on the microbiological corrosion and deterioration of dental materials, and the microbiological reasons for failure of an adhesive interface between a resin-based composite restoration and natural tooth tissues. (Specimen preparation and observation courtesy of Dr. Vincenzo Conte and Prof. Patrizia Procacci)
4.2 The Choice of the Microbial Community
A broad range of bioreactor devices and systems is currently available for the investigation of oral biofilms. Nevertheless, strategic choices must be performed before selecting a specific device. Oral biofilms are complex communities in which hundreds of species coexist in the same ecological niche, expressing synergistic or antagonistic behavior among them, while, at the same time, establishing a symbiotic relationship with the host [20]. The selection of a specific inoculum depends on the individual requirements of the study or the research question. The microbiological model that most closely simulates this microenvironment is the artificial oral microcosm [21,22,23]. Microcosms are microbial communities that are grown in vitro to replicate as closely as possible the behavior of their in vivo counterparts. They have a microbiological composition similar to that of the oral environment they are replicating, and this is usually obtained by using biofilms that are sampled from the oral environment. Also, particular care is necessary to ensure that the experimental setup precisely reproduces the physicochemical conditions as well as the nutrient composition. Experiments performed using microcosms can take advantage of a setup that is quite similar to the oral environment, which enables the evaluation of the dynamic performance of the microbial community and ensures control over the experimental parameters that are studied. Dental plaque microcosms were used to provide a better knowledge of the microbial ecology and physiology of dental microbial ecosystems [11, 24,25,26] (Fig. 4.3).
An example of the complexity of the interactions between biofilms and dental materials’ surfaces. Confocal laser scanning microscopy was used to obtain a 3D reconstruction of an artificial oral microcosm grown in a bioreactor (MDFR) over a non-buffering surface of a conventional resin-based composite material. LIVE-DEAD stain used Syto-9 and propidium iodide to stain viable cells in green and dead cells in red, respectively. A thin layer of dead cells can be identified close to the surface, while the more external layers are all made of viable microbial cells. No antimicrobial compounds were used on this materials’ surface, yet the combination of reduced amount of nutrients and decreased clearance of acidic catabolites (that are not buffered by demineralization as happens on natural surfaces) makes the microenvironmental conditions close to the surface very hostile. From this point of view, the presence of a “tamper” layer of dead cells may be highly detrimental to the equilibrium between health and disease conditions, since, being dead indeed, it does not react. It may thus greatly prolong the contact of acidic catabolites and degradation compounds such as esterases with the surface, accelerating the deterioration of the material and secondary caries onset
There are, however, limitations related to the use of microcosms. The microbial communities have huge variability in composition due to site- and subject-specific heterogeneity of the inocula. This circumstance produces variable results when comparing results for different experimental runs and raises difficulties regarding the comparison of the results obtained by different workgroups. Specific microbial species whose presence might be essential to the experiment may not be present in the inoculum, while the presence of undesirable species may unpredictably influence the outcomes. It has to be noted, however, that microbial communities have an intrinsic capacity of adaptation that strictly depends on the microenvironmental conditions. Therefore, the latter may lead to communities expressing similar phenotypical behavior, even if the starting inocula are different. An example can be seen in the massive selective pressure that the presence of sucrose exerts on microbial communities, shifting their composition towards the prevalence of acidogenic species. The composition of microbial communities, however, cannot be easily controlled to comply with the experimental objectives, and this type of inoculum is also the most difficult to standardize [27, 28].
A simplification criterium can be applied to reproduce this complex microenvironment only in parts in order to comply with specific research questions. To do that, researchers are modeling biofilms made of single species, or defined consortia made of few species growing together. While these approaches may seem outdated nowadays, they still provide significant advantages over the more complex microcosm models. A reductionistic approach can be efficiently used to control the influence of single parameters and for screening purposes—for instance, when the influence of a wide array of active principles or adherence substrates has to be tested. An example can be the initial testing of an array of active principles that are intended to be incorporated into a dental material. Several compositions and concentrations have to be tested in the most efficient and less time-consuming way to select the most promising ones.
Defined consortia of few species can provide a simplified simulation of ecological phenomena that are relatively easy to study due to the known parameters such as the initial and final proportion of the different species. The use of defined consortia is based on the evidence that many biofilm-generated diseases are a result of the combined activity of a group of microbial species in which each member is only weakly virulent. Each species can play a specific role or function, allowing the consortium to persist and express pathogenicity [2, 29]. Recent findings have proposed the concept of low-abundance species, due to which few distinct pathogens are mainly responsible for the virulence of the whole community [30, 31].
Experiments performed using defined consortia and monospecies usually achieve a higher degree of reproducibility compared to microcosm-based biofilms, theoretically allowing for better comparison between experimental runs and among research groups. Many different defined consortia have been developed; nevertheless, literature data show that each research group developed consortia showing different compositions from one another. Thus, the lack of well-defined standard procedures makes comparisons among research groups somehow tricky. One of the first and most used defined consortium models is the “Marsh Consortium” [32]. It is composed of ten microbial species that were chosen to represent the main physiological and ecological groups within the oral cavity. The model has shown excellent stability over time and allows for relatively simple sampling. Many similar approaches have been developed over time [33,34,35].
The highest degree of simplification can be achieved when using monospecies biofilms. A trade-off in the simplicity of the microbiological approach can bring advantages in terms of standardization and experimental control, making experimental design and interpretation of the results more straightforward [36]. A single-species biofilm is definitely less complex but can provide outcomes that can be useful to develop assays or analytical techniques. It can also be applied when approaches to treat biofilms are targeted towards eradication rather than modulating. For instance, this is the case when surface modifications of a material are performed with the aim of preventing microbial adherence and biofilm formation. One possible strategy is to engineer a material both regarding its surface and its releasing capabilities based on the response to the “pioneer” bacteria, making the surfaces hostile for the first colonizers, thus hoping to prevent the development of a fully mature biofilm. Furthermore, monospecific biofilms are better indicated when specific physiological aspects of the biofilm are to be studied by evaluating the response of the test inoculum to defined experimental conditions. One of the most used monospecies models in caries research is based on Streptococcus mutans [37,38,39]. This species has been identified as one of the main agents associated with dental caries [40]. Its ability to produce large amounts of extracellular matrix makes it able to adhere stably and quickly colonize a wide variety of surfaces, including natural and artificial ones. Moreover, its acidogenicity confers to its biofilm the pathogenic characteristics that are essential in caries research [41,42,43]. The major limitation of monospecies biofilm models is that they do not exist in the mouth. In fact, S. mutans can be a minority species even in persons with active caries [44, 45] and is currently regarded as a marker of caries risk rather than the responsible agent for dental caries.
4.3 Types of Bioreactors
Many bioreactor models are available nowadays. The main difference among them can be drawn between static and dynamic bioreactors. Static bioreactors can still be used to study adhesion and early colonization steps. In the oral environment, biofilm formation is subjected to hydrodynamic stresses. Therefore, the subsequent stages of this process (i.e., biofilm formation) have to be studied with the use of more complex systems that are able to replicate these conditions. Furthermore, the mouth is a very complex environment that can be regarded as an open system, where there is an intermittent inlet of nutrients and a salivary flow that provides clearance and discards catabolites that are produced by microbial metabolism. Bioreactor systems able to reproduce these conditions have evolved into very sophisticated devices that can recently include microfluidic technologies. The difficulty in performing experiments using these devices is proportional to the complexity of such systems. For example, salivary flow and shear forces must be reduced to a minimum during the night, when there is no inlet of nutrients for an extended amount of time. This situation highlights the need for those systems to show a flexible operational envelope. The main types of bioreactors and their application will be shortly discussed, starting from basic designs to the ones with increased complexity.
4.3.1 Static Bioreactor Models
Agar plates are the simplest static model conceived and were used for long to mimic, to some extent, biofilm growth conditions at an air/substrate interface. The finite availability of nutrients poses an intrinsic limit to the biofilm development and to the incubation time. The possibility of this model to evaluate the susceptibility towards different antimicrobial active principles was demonstrated [46, 47]. The availability of nutrients embedded into the substrate makes biofilms developed over agar plate surfaces very different from those growing on hard surfaces, limiting its value when the purpose is to study the interaction of biofilms with the surfaces of dental materials (Fig. 4.4). This situation is more similar to the one occurring when biofilms colonize and infect soft tissues [48, 49]. The agar disk diffusion method for antibacterial compound testing is based on this kind of simple bioreactor model. Nevertheless, the results of this model were not proven to feature a good correlation with in vivo data when considering biofilms developed on the surfaces of indwelling devices [12]. The growth conditions that are reproduced by this model do not show satisfactory similarity with the in vivo clinical situation. An evolution of this model was the colony biofilm method, where biofilm formation was obtained on a semipermeable membrane placed on an agar plate. The usefulness of this model also resides in its use as a preliminary antimicrobial test [7, 50].
A static model that allows a better simulation of microbial adherence and early colonization on hard surfaces is the microtiter plate. This is a simple yet effective closed system that is designed to test a broad array of specimens while keeping control of the growth conditions. A typical assay evaluates the time-dependent adherence to the wells’ substrate, which is usually made of polystyrene, polypropylene, or polycarbonate [51, 52]. Furthermore, the substrate can be γ-irradiated to change its surface properties (increase in surface free energy) and better foster cell adherence (tissue culture-treated surfaces). This system can perform preliminary antimicrobial screening tests on a library of compounds (Fig. 4.5). Both the prevention of biofilm formation and the removal potential of antimicrobial compounds can be assessed by the addition of scalar concentrations of test compounds after inoculation or after “mature” biofilms are developed [11, 12]. Care must be taken, however, not to test just a layer of bacteria that is deposited on the bottom of the wells instead of a biofilm. To avoid that, plates must be gently washed at least a couple of times with a buffered isotonic solution to remove non-adhered cells. As such, the microplate model can be coupled with all sorts of high-throughput end-point biochemical quantitative assays, including the evaluation of viable biomass, extracellular matrix, and acid production. Optical measurements using transparent flat-bottomed plates can be performed in real time to plot the growth curves in a nondestructive way [53]. More recently, molecular bioassays can also be performed, for instance, to screen large numbers of strains for specific characteristics [35]. This model is quite a right choice for preliminary testing of dental materials since material samples can be fabricated in a relatively simple way to be press-fitted on the bottom of the plates, or be made with a smaller diameter to allow the collection of the specimen together with the overlying biofilm.
A 96-well microtiter plate test to assess the antimicrobial activity of a library of natural compounds and its derivatives against S. mutans biofilms. The adaptability of the system is evident, where multiple replicates can be obtained for each test and parameters such as dilution (for instance, determining the minimal concentration achieving biofilm eradication, MBC), contact time, and activity on different microbial strains can be conveniently studied in a single experimental run. All kind of colorimetric tests can be easily applied and standardized. Here, MTT-based assay, shown on the two plates on the right, is based on the reduction by viable and metabolically active cells of yellow MTT tetrazolium to purple formazan [23]
An evolution of the static plate model was developed and patented by the Biofilm Engineering Research Group of Calgary University [54], which is why it was marketed as the Calgary Biofilm Device, now available under the new appellation “MBEC Assay®’s Biofilm Inoculator” that stands for the determination of the minimum biofilm eradication concentration. The static microplate model was modified by adding pegs to the plate lid in correspondence to each well. The pegs are used as the substratum for biofilm formation, allowing high-throughput experiments in a simple way (Fig. 4.6). The culture medium can be easily exchanged by transferring the lid to another plate. This constitutes an advantage of this model over the static plate that allows extending the total incubation time well over 24–48 h. In the same way, screening of active principles can be performed without difficulty, and the MBEC can be obtained. Several versions of this device have been proposed by different research groups, with a broad spectrum of substrata, inocula, and growth media. As an example, saliva-coated hydroxyapatite disks were used as a substratum for antimicrobial studies using defined consortia [24, 55]. In this case, the specimens of a dental material to be tested are hanged from the lid and immersed into the culture broth, allowing biofilm to form on their surfaces.
A standard MBEC assay 96-well plate is displayed where hydroxyapatite-coated pegs are attached to the lid of the plate and are used as substrate for biofilm formation. It is apparent that biofilms developed on the pegs can be transferred to new plates containing fresh culture medium, or any reagents, by just repositioning the lid. (The picture is courtesy of Dr. Amin Omar, chief operating officer at Innovotech Inc.)
The main drawback of these devices is related to their design, which includes a closed environment with a finite source of nutrients and in which catabolites and eluted compounds become more and more concentrated with time. This situation does not commonly occur in the oral environment. Under these conditions, swift microbial growth occurs in the first moments, followed by a stationary phase. This limitation can nevertheless make this model ideal for measuring the amount of active principles leaking out of the material and concentrating on the supernatant broth, or their activity on the overgrowing biofilms. Furthermore, hydrodynamic stress that is paramount to the development and structure of oral biofilms is absent, which is another drawback. It is clear that the growth of biofilms closely mimicking in vivo conditions requires systems such as intermittent- or continuous-flow devices, where the flow provides nutrients and, at the same time, allows washout of catabolites and eluted compounds. A modification of this model to partially overcome its drawbacks consists of merely inserting the plates into an orbital shaker to provide shear stress. This transforms the model into a straightforward dynamic one that, notwithstanding its still huge limitations such as the presence of a finite amount of nutrients and the radial inhomogeneity of shear stress across the well, allows to provide many of the conditions offered by much more complex dynamic models.
4.3.2 Dynamic Bioreactor Models
A better approximation of the oral environment can only be achieved in vitro by taking into account and replicating the environmental characteristics that influence the growth of oral biofilms. Two main aspects deeply influence oral biofilm development, namely the presence of different interfaces (air/liquid, liquid/substratum) and the hydrodynamic stresses induced by the flow of saliva and nutrients over the substratum surfaces. These aspects determine the transport rate of oxygen, nutrients, active compounds, and catabolites in and out of the biofilm structures. The flow is the primary source of hydrodynamic stress, which is an influential driving factor for the morphology and structure of biofilms. Therefore, it is essential for a bioreactor system to reproduce these conditions in order to develop a biofilm closely resembling in vivo ones.
The research group led by Dr. Philip D. Marsh made a first step approaching the complexity of oral environmental conditions. They developed a continuous culture of oral bacteria in planktonic state and, while the bioreactor was running, they realized that biofilm developed on the vessel walls, possibly simulating dental plaque formation [32]. The research group refined their model by introducing removable hydroxyapatite specimens as growth substratum that were suspended inside the vessel [56]. Furthermore, sucrose addition was performed to select a cariogenic environment.
Another relatively simple approach to model oral biofilm formation was introduced by the constant-depth film fermentor (CDFF) [57, 58]. It consists of a glass vessel with a stainless steel top and bottom plates, containing ports for sampling and inlet/outlet system for nutrients. A high number of specimens can be simultaneously tested (15 PTFE pans allowing 5 specimens each), and the specimens are fitted into the bottom plate. The latter rotates under a scraper blade that helps in diffusing the nutrient medium over the surface of the plate and regulates biofilm depth. The system can be stopped, and sampling pans can be removed aseptically, allowing to study incubation time as a parameter on the same experimental run.
This system was one of the first high-throughput bioreactor devices that allow virtually any substrate to be tested for biofilm formation, providing a suitable platform for the study of the microbiological behavior of dental materials. Great attention was paid afterward in the design of bioreactors to ensure the easiness of testing for different materials. A variant of this model, called nCDFF (nonconstant depth film fermentor), included the possibility to form biofilms without thickness constraint (Fig. 4.7).
Differences between a standard CDFF and the nCDFF model. (Available from Lüdecke C, Jandt CD, Siegismund D, Kujau MD, Zang E, Rettenmayr M, Bossert J, Roth M. Reproducible Biofilm Cultivation of Chemostat-Grown Escherichia coli and Investigation of Bacterial Adhesion on Biomaterials Using a Non-Constant-Depth Film Fermenter. https://doi.org/10.1371/journal.pone.0084837)
A variation of this model sharing a similar concept is the rotating disk reactor, RDR (Fig. 4.8). The bioreactor includes a vessel that allows an inlet and outlet of nutrient broth with the presence of a constant amount inside the vessel. At the bottom of the vessel, a magnetic rotor is used as a specimen holder (up to 18 coupons). The hydrodynamic stress generated by this device is easily controlled by adjusting the speed of the rotor. The reactor design was studied to ensure easiness of operation, also including sterilization procedures. The system is flexible, being adaptable to several different studies, ranging from the study of the biofilm exopolysaccharide matrix formation to the rheology of oral biofilms [59, 60]. The operational envelope of this bioreactor was extensively studied, and it was registered as a standard test method for the evaluation of biofilms (ASTM E2196-02). The main advantage of the system includes its simplicity and easiness of use, especially when the hydrodynamic stress parameter is analyzed. The relatively low number of specimens that can be tested at the same time is, however, a limitation.
Schematic representation of the rotating disk reactor. (Obtained from BioSurface Technologies Corporation. http://biofilms.biz/)
The Robbins device is a flow-through system also used in medical biofilm studies [61, 62]. It consists of a plastic or metal tube into which specimen-containing coupons can be inserted, becoming part of the tube wall (Fig. 4.9). This system provides similar advantages to the CDFF in terms of high-throughput testing of different substrata and the possibility to aseptically remove every single coupon. Similar to in vivo biofilms, the structure, thickness, and morphology of the biofilm growing on the coupons are influenced by the hydrodynamic parameters of the flow rather than by the scraping activity of a blade, or the velocity of a specimen-holding rotor.
One of the customizations of the modified Robbins device, resulting in the Bio-inLine Biofilm Reactor. (Obtained from BioSurface Technologies Corporation. http://biofilms.biz/)
The drip-flow bioreactor was conceived by the Center for Biofilm Engineering of Montana State University [7, 63]. It consists of several parallel independent flow cells that have the dimensions of a microscopy slide. Each flow cell has a lid that can be separately unscrewed to collect the specimens. The name of the reactor is due to the nutrient inlet that drips over the surface of the specimen directly, preventing backward contamination of the tubing. The bioreactor is operated at a 10° inclination so that gravity provides continuous flow with hydrodynamic stress over the specimens’ surfaces. The system is therefore used for simulating biofilm formation at the air/liquid interface under relatively low shear stress conditions and allows to study biofilm formation on the surface of any material. This system has also been registered as a standard test method for the evaluation of biofilms (ASTM E2647-13). The possibility to easily place or remove specimens allowed the system to be used in several studies that tested the antimicrobial efficacy of oral hygiene products, such as toothpastes or mouthwashes [64,65,66]. The system still includes some limitations, for instance the low number of specimens that can be tested, the difficulty of temperature control, and the need for complicated, multichannel pumps to operate the flow in parallel to the flow cells reliably.
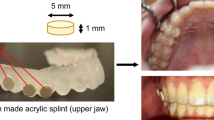
Brambilla et al. proposed a modification of the drip-flow bioreactor, overcoming some of the limitations of the model [66]. The reactor was operated in a horizontal position, and a low dam was included in the design downstream of the specimen trays to maintain the specimen surfaces immersed in the flowing medium (Figs. 4.10 and 4.11). As with many bioreactors, the system is designed to be entirely placed inside an incubator for optimal temperature control (Fig. 4.12). From the point of view of flow characteristics, this system shows many similarities with the Robbins device, with the addition of an air/liquid interface. Specimens having the exact dimensions of the bottom of 96-well plates are press-fitted on customized polytetrafluoroethylene (PTFE) trays at the bottom of the flow cells. Up to 27 specimens in each flow cell can be simultaneously tested, allowing this bioreactor to be a high-throughput, very adaptable system for the testing of dental materials [17, 23, 65].
An operating modified drip-flow bioreactor [65]. All tubing are connected through disposable Luer lock and valves, thus ensuring easy and low-cost modifications, such as additional inlets for sucrose pulsing or antimicrobial solution testing
Placing the whole bioreactor, including the distribution pumps and the main vessels containing the sterile medium, inside an incubator provides optimal temperature control over other more simplistic solutions such as a thermostatic bath or table that often do not allow for homogeneous heat distribution to the whole system [17]
The Center for Disease Control (CDC) developed its own biofilm reactor [22, 67]. It is made of a cylindrical vessel in which eight specimen-containing rods (three specimens per rod) are suspended from the lid. Similar to the rotating disk reactor, an inlet and outlet provide a flow of nutrients and a constant volume is maintained inside the vessel in which specimens are immersed. A magnetic stirrer at the bottom of the vessel can indirectly provide a wide range of hydrodynamic stress by agitating the nutrient broth. Specimens can be assessed at different time points by aseptically removing the rods. This bioreactor was used to provide two standard methods (ASTM E2562-12 and ASTM E2871-13) for biofilm development and test of antimicrobial compounds under high hydrodynamic stress and continuous flow (Fig. 4.13). The system was not initially developed for the study of medical and oral biofilms; therefore several modifications of the system were performed, mainly regarding the growth medium and the control of the temperature and the hydrodynamic flow conditions. Several authors used this system for the development of oral biofilms. Rudney et al. [22] were able to develop oral microcosm biofilms using this model, while Li et al. [68] used the system to study the effect of sucrose pulsing on the biofilm development over the surfaces of dental restorative materials. The main limitation of the system is related to the low amount of specimens that can be tested at the same time.
Schematic representation of the CDC Biofilm Reactor. (Obtained from BioSurface Technologies Corporation. http://biofilms.biz/)
4.3.3 Microfluidic Bioreactor Models
More recently, bioreactor systems were developed using microfluidic techniques allowing them to overcome some limitations, such as the relatively large volume of nutrients and biomass that are usually required by the previously described bioreactors. These techniques make it possible to reduce the dimensions of the test environment for better spatial and temporal control of biofilm community formation. Indeed, microfluidic bioreactor systems are small enough to approach the microscopic dimension range. For this reason, they can be efficiently used to study cell interactions during the very first steps in biofilm formation and with the adherence substrate. In the latter case, high interest is due to the study of nanopatterned materials.
Microfluidic devices are built to reproduce the physical effects occurring at the micron scale, including an increase in the surface-to-volume ratio. As a consequence, physical parameters such as capillary forces, fluidic resistance, and surface tension become fundamental in controlling these effects. In particular, laminar flow conditions can be obtained to reach better control. In these conditions, the effect of diffusion becomes predominant over other effects such as turbulence, convection, and gravitational forces. The exchanges of nutrients and catabolites, and, more generally, the energy transfer between a biofilm and the surrounding flow, can be more efficiently controlled and investigated [12, 69, 70]. A very high number of replicates can also be provided for high-throughput analyses. However, the miniaturization of the devices dramatically increases their complexity, which, in turn, increases the difficulty of operating such systems and their inherent costs. In fact, the real microfluidic dynamics of biofilms are very poorly known as it is a relatively new research field. Therefore, no approach is currently able to reproduce real microfluidic conditions and standardization of such systems appears problematic. These systems have been mainly developed for the study of cell cultures, and, then, they were adapted for biofilm development as well. They are often built to provide an answer to a defined research question based on a reductionistic approach rather than to recreate the whole complexity of the clinical situation.
A microfluidic device was developed by Groisman et al. [71] to produce biofilms inside chemostat microchambers, where better control of the microenvironment could be achieved. Kim et al. [72] developed a microfluidic bioreactor based on a two-layer flow cell. The device was built to study the effect of a gradient in the concentration of an active principle or signaling molecule. A total of eight microfluidic flow cells were used to simultaneously expose developed biofilms to different concentrations using a gradient generator based on diffusive mixing (Fig. 4.14). Another device was conceived by Benoit et al. [70] to develop a high number of independent biofilm communities at the same time under a continuous flow using the format of a 96-well plate. This device can be used as a high-throughput system for biofilm screening, and its compatibility with plate readers allows very fast and adaptable biofilm assays. Busscher and van der Mei [73] provided a comprehensive review of flow displacement systems for studying microbial adhesion.
Diagram of the microfluidic device by Jeongyun Kim et al. and its evident complexity. The device consists of a glass coverslip and two PDMS layers—a bottom layer with a diffusive mixer and eight microchambers and a top layer with the pneumatic elements for opening and closing microvalves that separate the diffusive mixer and bacterial seeding ports from the microchambers. The top layer also contains a bacterial seeding port for introducing bacteria into the microchambers
4.4 The Quest for Standardization
4.4.1 Standardization of Bioreactor Systems
It is clear from the previous descriptions that a high number of bioreactor systems are nowadays in use for the analysis of oral biofilms in vitro. Many of these systems are not standardized or have been standardized for different environments rather than the oral environment. A considerable limitation of oral biofilm models has been that, because of their complexity, dynamicity, and adaptation capability, they are difficult to standardize or characterize. Indeed, the validation of a system is much easier than its standardization. The proof of concept and validation of a bioreactor system imply that it works predictably; that is, it is capable of reproducing the desired microenvironment. Also, the repeatability of the results obtained under defined working conditions is ensured. Standardization comes with a higher level of complexity that includes the isolation and investigation of all the possible parameters that may influence the working conditions of the system. The behavior of the system under these conditions (operational envelope) has to be known to control and reduce the sources of variability. A standard method has to comply with all of the following concepts [7]:
-
Repeatability (different runs of the bioreactor must produce comparable results)
-
Reproducibility (different laboratories using the same system must produce comparable results)
-
Ruggedness (minor changes in the standard operating procedure do not significantly affect the results)
-
Responsiveness (the capacity of the system to obtain the expected performances)
-
Reasonability (any operator can run the system, given specific instructions, without the need for a too high amount of time and consumables)
-
Relevance (the outcomes of that system are within the research field to which that system is applied)
Of course, any modification of the operational envelope of a standardized bioreactor system implies that additional studies must be performed to confirm that the system maintains standard operational capability.
4.4.2 Standardization of Biofilm Analysis Techniques
Advancements in the biofilm analysis methods allowed for better characterization, which, in turn, made it possible to achieve significant progress towards standardization. The first methods for identification and quantification of microorganisms in oral microcosms were based on denaturing gradient gel electrophoresis (DGGE) or checkerboard DNA–DNA hybridization. These methodologies could screen for a limited number of microbial species [24, 74]. More recent methodologies based on the identification of DNA with a large array of probes (human oral microbial identification microarray, HOMIM) or high-throughput direct identification of microbial species (next-generation sequencing based on massive parallel sequencing, HOMINGS) were able to identify virtually any microorganism that constitutes a biofilm community [75]. These latter methodologies also allowed to quantify the biodiversity of a biofilm and to assess shifts towards the prevalence of pathogenic species [76].
Due to the different bioreactor systems used and the increasing amount of biofilm data that is being gathered, there is a great need for standardization both of the bioreactor systems and of the biofilm analysis techniques, making possible direct comparisons among experiments differing in space (different research teams) and time. The first step in this direction has been made with the creation of two online platforms. The first one, MIABiE17 (minimum information about a biofilm experiment), is aimed to start providing guidelines about the minimum information that is to be acquired during an experiment involving biofilms. The other platform, BiofOmics18, is a systematic and standardized database that collects data about biofilm experiments.
4.5 Conclusions
Although a wide range of bioreactors are currently available, it is clear from this discussion that a universal bioreactor system that can be adapted to all clinical situations does not exist. Each model has its own advantages and limitations that must be acknowledged when choosing the model that best fits a distinct experimental design. There are some devices designed to study low fluid shear stresses, whereas others are more suitable for experiments under higher fluid shear stress. Some are appropriate when biofilm activity has to be evaluated, while other systems are better applied to the study of the biofilm structure. Furthermore, the operational flexibility of these models provides researchers with a spectrum of different models, often with overlapping characteristics. This situation, together with a reduced overall level of standardization, makes the comparison of the obtained results very difficult. Future studies in this field should be aimed at the standardization of the devices and analysis techniques.
From a materials science point of view, the science of biofilm development and bioreactor systems is most often difficult to be understood, given the high level of standardization that exists for the testing of the mechanical, physical, and chemical characteristics of a material. Furthermore, some research groups tend to use bioreactors as a “tool” to obtain simple answers about the antimicrobial activity of newly designed materials. While a quest for simplification of procedures and standardization of methods is always desirable, this approach often leads to undervaluing, or neglecting, many aspects that are intrinsic to the complexity of the material-host-biofilm interactions, and may lead to misinterpreting experimental results.
References
Simões M, Pereira MO, Sillankorva S, Azeredo J, Vieira MJ. The effect of hydrodynamic conditions on the phenotype of Pseudomonas fluorescens biofilms. Biofouling. 2007;23(3–4):249–58.
Marsh PD, Zaura E. Dental biofilm: ecological interactions in health and disease. J Clin Periodontol. 2017;44(S18):S12–22.
Peterson SN, Meissner T, Su AI, Snesrud E, Ong AC, Schork NJ, Bretz WA. Functional expression of dental plaque microbiota. Front Cell Infect Microbiol. 2014;4:108.
Senneby A, Davies J, Svensäter G, Neilands J. Acid tolerance properties of dental biofilms in vivo. BMC Microbiol. 2017;17(1):165.
Köves B, Magyar A, Tenke P. Spectrum and antibiotic resistance of catheter-associated urinary tract infections. GMS Infect Dis. 2017;5:Doc06.
Tenke P, Köves B, Nagy K, Hultgren SJ, Mendling W, Wullt B, Grabe M, Wagenlehner FM, Cek M, Pickard R, Botto H. Update on biofilm infections in the urinary tract. World J Urol. 2012;30(1):51–7.
Gomes IB, Meireles A, Gonçalves AL, Goeres DM, Sjollema J, Simões LC, et al. Standardized reactors for the study of medical biofilms: a review of the principles and latest modifications. Crit Rev Biotechnol. 2018;38(5):657–70.
Vickery K, Hu H, Jacombs AS, Bradshaw DA, Deva AK. A review of bacterial biofilms and their role in device-associated infection. Healthc Infect. 2013;18(2):61–6.
Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science. 1999;284(5418):1318–22.
Koo H, Allan RN, Howlin RP, Stoodley P, Hall-Stoodley L. Targeting microbial biofilms: current and prospective therapeutic strategies. Nat Rev Microbiol. 2017;15(12):740–55.
McBain AJ. Chapter 4: In vitro biofilm models: an overview. Adv Appl Microbiol. 2009;69:99–132.
Azeredo J, Azevedo N, Briandet R, Cerca N, Coenye T, Costa AR, Desvaux M, Di Bonaventura G, Hébraud M, Jaglic Z, Kačániová M. Critical review on biofilm methods. Crit Rev Microbiol. 2016;43(3):313–51.
Cazzaniga G. Resin-based composites modulate oral biofilm formation, PhD thesis. University of Milan, 2017. https://doi.org/10.13130/g-cazzaniga_phd2017-02-2314.
Marsh PD. In sickness and in health - what does the oral microbiome mean to us? An ecological perspective. Adv Dent Res. 2018;29(1):60–5.
Kroes I, Lepp PW, Relman DA. Bacterial diversity within the human subgingival crevice. Proc Natl Acad Sci U S A. 1999;96:14547–52.
Kawamura Y, Kamiya Y. Metagenomic analysis permitting identification of the minority bacterial populations in the oral microbiota. J Oral Biosci. 2012;54(3):132–7.
Ionescu A, Brambilla E, Hahnel S. Does recharging dental restorative materials with fluoride influence biofilm formation? Dent Mater. 2019;35(10):1450–63.
Hahnel S, Wastl DS, Schneider-Feyrer S, Giessibl FJ, Brambilla E, Cazzaniga G, Ionescu A. Streptococcus mutans biofilm formation and release of fluoride from experimental resin-based composites depending on surface treatment and S-PRG filler particle fraction. J Adhes Dent. 2014;16(4):313–21.
Nassar HM, Gregory RL. Biofilm sensitivity of seven Streptococcus mutans strains to different fluoride levels. J Oral Microbiol. 2017;9(1):1328265.
Chow J, Lee SM, Shen Y, Khosravi A, Mazmanian SK. Host–bacterial symbiosis in health and disease. Adv Immunol. 2010;107:243–74.
Kim Y-S, Kang S-M, Lee E-S, Lee JH, Kim B-R, Kim B-I. Ecological changes in oral microcosm biofilm during maturation. J Biomed Opt. 2016;21(10):101409.
Rudney JD, Chen R, Lenton P, Li J, Li Y, Jones RS, Reilly C, Fok AS, Aparicio C. A reproducible oral microcosm biofilm model for testing dental materials. J Appl Microbiol. 2012;113(6):1540–53.
Ionescu AC, Cazzaniga G, Ottobelli M, Garcia-Godoy F, Brambilla E. Substituted nano-hydroxyapatite toothpastes reduce biofilm formation on enamel and resin-based composite surfaces. J Funct Biomater. 2020;11(2):36.
Ledder RG, Gilbert P, Pluen A, Sreenivasan PK, Vizio WD, McBain AJ. Individual microflora beget unique oral microcosms. J Appl Microbiol. 2006;100(5):1123–31.
Robinson CJ, Bohannan BJM, Young VB. From structure to function: the ecology of host-associated microbial communities. Microbiol Mol Biol Rev. 2010;74(3):453–76.
Kuramitsu HK, He X, Lux R, Anderson MH, Shi W. Interspecies interactions within oral microbial communities. Microbiol Mol Biol Rev. 2007;71(4):653–70.
Sim CPC, Dashper SG, Reynolds EC. Oral microbial biofilm models and their application to the testing of anticariogenic agents. J Dent. 2016;50:1–11.
ten Cate JM. Models and role models. Caries Res. 2015;49(S1):3–10.
Rickard AH, Gilbert P, High NJ, Kolenbrander PE, Handley PS. Bacterial coaggregation: an integral process in the development of multispecies biofilms. Trends Microbiol. 2003;11(2):94–100.
Hajishengallis G, Liang S, Payne MA, Hashim A, Jotwani R, Eskan MA, McIntosh ML, Alsam A, Kirkwood KL, Lambris JD, Darveau RPA. Low-abundance biofilm species orchestrates inflammatory periodontal disease through the commensal microbiota and the complement pathway. Cell Host Microbe. 2011;10(5):497–506.
Nibali L, Henderson B. The human microbiota and chronic disease: dysbiosis as a cause of human pathology. Hoboken, NJ: John Wiley & Sons; 2016. p. 560.
Marsh PD, Hunter JR, Bowden GH, Hamilton IR, McKee AS, Hardie JM, et al. The influence of growth rate and nutrient limitation on the microbial composition and biochemical properties of a mixed culture of oral bacteria grown in a chemostat. J Gen Microbiol. 1983;129(3):755–70.
Shu M, Wong L, Miller JH, Sissons CH. Development of multispecies consortia biofilms of oral bacteria as an enamel and root caries model system. Arch Oral Biol. 2000;45(1):27–40.
McKee AS, McDermid AS, Ellwood DC, Marsh PD. The establishment of reproducible, complex communities of oral bacteria in the chemostat using defined inocula. J Appl Bacteriol. 1985;59(3):263–75.
Burmølle M, Webb JS, Rao D, Hansen LH, Sørensen SJ, Kjelleberg S. Enhanced biofilm formation and increased resistance to antimicrobial agents and bacterial invasion are caused by synergistic interactions in multispecies biofilms. Appl Environ Microbiol. 2006;72(6):3916–23.
Lin NJ. Biofilm over teeth and restorations: what do we need to know? Dent Mater. 2017;33(6):667–80.
Zanin ICJ, Gonçalves RB, Junior AB, Hope CK, Pratten J. Susceptibility of Streptococcus mutans biofilms to photodynamic therapy: an in vitro study. J Antimicrob Chemother. 2005;56(2):324–30.
Fernández CE, Tenuta LMA, Cury JA. Validation of a cariogenic biofilm model to evaluate the effect of fluoride on enamel and root dentine demineralization. PLoS One. 2016;11(1):e0146478.
Zhang A, Chen R, Aregawi W, He Y, Wang S, Aparicio C, et al. Development and calibration of biochemical models for testing dental restorations. Acta Biomater. 2020;109:132–41.
Forssten SD, Björklund M, Ouwehand AC. Streptococcus mutans, caries and simulation models. Nutrients. 2010;2(3):290–8.
Philip N, Suneja B, Walsh L. Beyond Streptococcus mutans: clinical implications of the evolving dental caries aetiological paradigms and its associated microbiome. Br Dent J. 2018;224(4):219.
Banas JA, Drake DR. Are the mutans streptococci still considered relevant to understanding the microbial etiology of dental caries? BMC Oral Health. 2018;18(1):129.
Matsumoto-Nakano M. Role of Streptococcus mutans surface proteins for biofilm formation. Jpn Dent Sci Rev. 2018;54(1):22–9.
Childers NK, Momeni SS, Whiddon J, Cheon K, Cutter GR, Wiener HW, et al. Association between early childhood caries and colonization with Streptococcus mutans genotypes from mothers. Pediatr Dent. 2017;39(2):130–5.
Hajishengallis E, Parsaei Y, Klein MI, Koo H. Advances in the microbial etiology and pathogenesis of early childhood caries. Mol Oral Microbiol. 2017;32(1):24–34.
Yu OY, Zhao IS, Mei ML, Lo EC-M, Chu C-H. Dental biofilm and laboratory microbial culture models for cariology research. Dent J. 2017;5(2):21.
Balouiri M, Sadiki M, Ibnsouda SK. Methods for in vitro evaluating antimicrobial activity: a review. J Pharm Anal. 2016;6(2):71–9.
Milho C, Andrade M, Boas DV, Alves D, Sillankorva S. Antimicrobial assessment of phage therapy using a porcine model of biofilm infection. Int J Pharm. 2019;557:112–23.
Morgan SJ, Lippman SI, Bautista GE, Harrison JJ, Harding CL, Gallagher LA, et al. Bacterial fitness in chronic wounds appears to be mediated by the capacity for high-density growth, not virulence or biofilm functions. PLoS Pathog. 2019;15(3):e1007511.
Bahamondez-Canas TF, Heersema LA, Smyth HD. Current status of in vitro models and assays for susceptibility testing for wound biofilm infections. Biomedicine. 2019;7(2):34.
Pierce CG, Uppuluri P, Tummala S, Lopez-Ribot JL. A 96 well microtiter plate-based method for monitoring formation and antifungal susceptibility testing of Candida albicans biofilms. JoVE J Vis Exp. 2010;44:e2287.
Skogman ME, Vuorela PM, Fallarero A. A platform of anti-biofilm assays suited to the exploration of natural compound libraries. JoVE J Vis Exp. 2016;118:e54829.
Kampf G. Antiseptic stewardship for wound and mucous membrane antiseptics. In: Kampf G, editor. Antiseptic stewardship: biocide resistance and clinical implications. Cham: Springer International Publishing; 2018. p. 689–94.
Ceri H, Olson ME, Stremick C, Read RR, Morck D, Buret A. The Calgary Biofilm Device: new technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J Clin Microbiol. 1999;37(6):1771–6.
Brown JL, Johnston W, Delaney C, Short B, Butcher MC, Young T, et al. Polymicrobial oral biofilm models: simplifying the complex. J Med Microbiol. 2019;68(11):1573–84.
Bradshaw DJ, Marsh PD, Schilling KM, Cummins D. A modified chemostat system to study the ecology of oral biofilms. J Appl Bacteriol. 1996;80(2):124–30.
Peters AC, Wimpenny JWT. A constant-depth laboratory model film fermentor. Biotechnol Bioeng. 1988;32(3):263–70.
Rozenbaum RT. Antimicrobial and nanoparticle penetration and killing in infectious biofilms, PhD thesis. Rijksuniversiteit Groningen, 2019. http://hdl.handle.net/11370/0f2d1f8e-8898-4fb3-af42-7e8fd68c58e5.
Cotter JJ, O’Gara JP, Stewart PS, et al. Characterization of a modified rotating disk reactor for the cultivation of Staphylococcus epidermidis biofilm. J Appl Microbiol. 2010;109:2105–17.
Möhle RB, Langemann T, Haesner M, Augustin W, Scholl S, Neu TR, et al. Structure and shear strength of microbial biofilms as determined with confocal laser scanning microscopy and fluid dynamic gauging using a novel rotating disc biofilm reactor. Biotechnol Bioeng. 2007;98(4):747–55.
Kharazmi A, Giwercman B, Høiby N. Robbins device in biofilm research. In: Methods in enzymology. New York: Academic Press; 1999. p. 207–15.
Jass J, Costerton JW, Lappin-Scott HM. Assessment of a chemostat-coupled modified Robbins device to study biofilms. J Ind Microbiol. 1995;15(4):283–9.
Goeres DM, Hamilton MA, Beck NA, Buckingham-Meyer K, Hilyard JD, Loetterle LR, et al. A method for growing a biofilm under low shear at the air–liquid interface using the drip flow biofilm reactor. Nat Protoc. 2009;4(5):783–8.
Ledder RG, McBain AJ. An in vitro comparison of dentifrice formulations in three distinct oral microbiotas. Arch Oral Biol. 2012;57(2):139–47.
Ionescu A, Wutscher E, Brambilla E, Schneider-Feyrer S, Giessibl FJ, Hahnel S. Influence of surface properties of resin-based composites on in vitro Streptococcus mutans biofilm development. Eur J Oral Sci. 2012;120(5):458–65.
Brambilla E, Ionescu A, Cazzaniga G, Edefonti V. The influence of antibacterial toothpastes on in vitro Streptococcus mutans biofilm formation: a continuous culture study. Am J Dent. 2014;27(3):7.
Yoon HY, Lee SY. Establishing a laboratory model of dental unit waterlines bacterial biofilms using a CDC biofilm reactor. Biofouling. 2017;33(10):917–26.
Li Y, Carrera C, Chen R, Li J, Lenton P, Rudney JD, et al. Degradation in the dentin–composite interface subjected to multispecies biofilm challenges. Acta Biomater. 2014;10(1):375–83.
Yawata Y, Nguyen J, Stocker R, Rusconi R. Microfluidic studies of biofilm formation in dynamic environments. In: O’Toole GA, editor. J Bacteriol. 2016;198(19):2589–95.
Benoit MR, Conant CG, Ionescu-Zanetti C, Schwartz M, Matin A. New device for high-throughput viability screening of flow biofilms. Appl Environ Microbiol. 2010;76(13):4136–42.
Groisman A, Lobo C, Cho H, Campbell JK, Dufour YS, Stevens AM, et al. A microfluidic chemostat for experiments with bacterial and yeast cells. Nat Methods. 2005;2(9):685–9.
Kim J, Hegde M, Kim SH, Wood TK, Jayaraman A. A microfluidic device for high throughput bacterial biofilm studies. Lab Chip. 2012;12(6):1157–63.
Busscher HJ, van der Mei HC. Microbial adhesion in flow displacement systems. Clin Microbiol Rev. 2006;19(1):127–41.
Gellen LS, Wall-Manning GM, Sissons CH. Checkerboard DNA-DNA hybridization technology using digoxigenin detection. In: Hilario E, Mackay J, editors. Protocols for nucleic acid analysis by nonradioactive probes. Totowa, NJ: Humana Press; 2007. p. 39–67.
Mougeot J-LC, Stevens CB, Cotton SL, Morton DS, Krishnan K, Brennan MT, et al. Concordance of HOMIM and HOMINGS technologies in the microbiome analysis of clinical samples. J Oral Microbiol. 2016;8(1):30379.
Adams SE, Arnold D, Murphy B, Carroll P, Green AK, Smith AM, et al. A randomised clinical study to determine the effect of a toothpaste containing enzymes and proteins on plaque oral microbiome ecology. Sci Rep. 2017;7(1):43344.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ionescu, A.C., Brambilla, E. (2021). Bioreactors: How to Study Biofilms In Vitro. In: Ionescu, A.C., Hahnel, S. (eds) Oral Biofilms and Modern Dental Materials . Springer, Cham. https://doi.org/10.1007/978-3-030-67388-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-67388-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67387-1
Online ISBN: 978-3-030-67388-8
eBook Packages: MedicineMedicine (R0)