Abstract
Endolumenal surgery (ELS) is at the forefront of minimally invasive surgery. Endoscopic polypectomy methods have drastically changed over the past several years from biopsy forceps and snares to more advanced methods and endoscopic tissue resections such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). The boundaries of endoscopic surgery have been further advanced with suturing devices, stabilization platforms, and stenting. The following chapter will review technical aspects of endoscopic surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Endolumenal surgery
- Minimally invasive surgery
- Colonoscopy
- Polypectomy
- EMR
- ESD
- Colonic stenting
- Submucosal injection
-
Endolumenal surgery is the forefront of minimally invasive surgery and is rapidly developing.
-
Colon and rectal surgeons should be involved in the progression of endolumenal surgery as it will offer benefit to patients.
-
New endolumenal techniques can be used to address large polyps that once required resection and treat malignant large bowel obstructions.
Introduction
Colonoscopy was initially described as a way to screen patients for mucosal abnormalities in the colon and has been adopted as the standard for colorectal cancer screening and prevention. However, when retrograde colonoscopy was first described in 1969, “there were some who said it couldn’t be done, shortly followed by those who said it couldn’t be done safely, followed by those who declared that it required a tricky skill which few would be able to acquire” [1]. Time has proved otherwise. Colonoscopic polypectomy has been demonstrated to decrease the incidence of colorectal cancer and has been widely adopted by the medical community [2]. With advances in technology, colonoscopy has progressed dramatically, and flexible colonoscopy is now used with various platforms that enable advanced endoscopic surgical procedures to be effectively completed. Endolumenal surgery is a rapidly progressive field in gastrointestinal surgery performed by both surgeons and gastroenterologists that offers the benefits of non-invasive surgery done in an outpatient setting. However, endolumenal surgeons are confronted with the challenge of operating through a flexible scope in a confined space that is frequently moving. Similar to opponents of early colonoscopy, there are many physicians in various stages of opposition. Due to the benefits to the patient, endoscopic surgery has the potential to be the next leap forward in minimally invasive surgery. This chapter will discuss the technical aspects of endolumenal surgery, ranging from forceps polypectomy to endoscopic submucosal dissection and colonic stenting.
Forceps
There are three commonly available options for forceps polypectomy : cold biopsy forceps, jumbo cold biopsy forceps, and hot biopsy forceps. For cold biopsy, the standard forceps open to 6 mm, and jumbo cold forceps open to 8.6 mm. Jumbo biopsy forceps have been shown to be superior to standard cold forceps for complete resection [3]. Historically, hot biopsy forceps were commonly used for polyp resection with the theoretical benefit of fulgurating any remaining dysplastic tissue around the polyp. However, this theoretical advantage has been refuted. A retrospective review of 62 hot biopsy polypectomies demonstrated a 17% rate of persistent polypoid tissue on repeat endoscopy 1–2 weeks after the original treatment [4].
Additionally, hot biopsy is associated with an increased risk of delayed hemorrhage compared to cold biopsy [5]. Furthermore, hot biopsy alters the polyp morphology and creates more histological architectural distortion and fragmentation than cold biopsy [6]. For the aforementioned reasons, the European Society of GI Endoscopy (ESGE) has recommended against the use of hot biopsy forceps [7].
Cold biopsy forceps have also been described as an adjunct to difficult to remove large spreading polyps. While these polyps are typically removed with snare (described below), some polyps will not allow snare resection as the snare will slide over the polyp. In these situations, cold forceps are used to methodically avulse all visible polypoid tissue. Following avulsion of the mucosa, the submucosa and margins can be treated with soft coagulation from the tip of a hot snare. This technique, deemed CAST for Cold-forceps Avulsion with adjuvant Snare-Tip soft coagulation, has been reported as an effective and safe strategy for the management of non-lifting large laterally spreading (LST) colonic lesions [8]. CAST is easy to use, does not require additional equipment, and is useful adjunctive technique for organ sparing.
Snare
Endoscopic snare allows resection of larger lesions and more tissue compared to forceps. Incomplete resection of polyps by any method is associated with interval development of colorectal cancer in patients undergoing colonoscopy [9]. In removal of polyps <6 mm, snare excision has a higher rate of complete resection compared to forceps removal (93% for cold snare vs. 76% for cold biopsy forceps, p < 0.001) [10].
Snares vary in size, shape, and ability for coagulation. Hot snares are the traditional method for endoscopic snaring but have waned in popularity over recent years due to complications including increased risk of delayed bleeding and thermal injury. Use of a cold snare without electrocautery is associated with lower rate of post-polypectomy hemorrhage and shorter time for polypectomy and colonoscopy [11, 12]. Complete resection rates with cold snare are equivalent to hot snare [13]. Dedicated cold snares have been further improved with use of a thinner wire that more easily cuts tissue. Compared to traditional snares used without cautery, dedicated thin-wire cold snares have a higher rate of complete resection, especially with polyps 8–10 mm in size or sessile polyps [14]. The 2017 guidelines from ESGE recommend cold snare polypectomy as the preferred method for polyps <5 mm in size and strongly favor cold snare polypectomy for polyps 6–9 mm in size [7]. Hot snare polypectomy has been reserved for sessile polyps 10–19 mm in size after submucosal injection has been used to decrease the risk of thermal injury. Hot snare is also recommended for pedunculated polyps to decrease the rate of bleeding.
Bleeding after polypectomy is infrequent but may result in hospitalization, repeat colonoscopy, and poor patient experience. The rate of bleeding after polypectomy is approximately 1–2 per 1000 patients and is 10 times the rate of bleeding compared to colonoscopy without polypectomy [15]. Bleeding after cold snare polypectomy tends to be immediate and can be addressed at the time of initial colonoscopy, while bleeding after hot snare is often delayed and not apparent at the initial colonoscopy. Bleeding after hot snare occurs 0.1–0.7% of polypectomies and can occur up to 30 days after the procedure [16]. Prophylactic clip placement after routine polypectomy does not decrease the risk of delayed bleeding [17], and this practice should be avoided as it drastically increases the cost of the procedure without substantial benefit. Selective use of endoscopic clips is discussed later in the chapter.
Tips for Optimal Snaring
Polypectomy is required in 30–40% of all colonoscopies. To make polypectomy easier, the polyp should be positioned at the bottom half of the screen because the instrument channel on the colonoscope exits the scope at the 5 o’clock position. Occasionally, the lesion cannot be placed in the inferior aspect of the screen due to tortuosity of the colon or location behind a prominent fold. In those situations, working with the scope tip further away from the lesion may facilitate polypectomy by producing a favorable angle of attack to the polyp. Additionally, jumbo forceps removal may be technically easier for polyps in a challenging location if the size is small. If a snare is applicable, lesions are more easily grasped with dedicated cold snares, since they have a thinner wire that can grip the tissue better than an electrocautery compatible snare. If a hot snare is used after a lift for a larger lesion, consideration should be given for use of a non-oval-shaped snare. Snares with some angulation, like a hexagonal snare, tend to grasp tissue better as well as have a greater proximal opening compared to standard oval or round snares. Figure 5.1 shows different type of snares.
Care should be taken during polypectomy to ensure that complete resection of the polyp has been performed. In a prospective study of over 1400 patients, there was a 10% rate of incomplete resection for polyps 5–20 mm. Risk factors for incomplete resection included larger size and sessile serrated polyps vs. adenoma [18]. Any remaining polyp tissue after snare polypectomy can be removed with repeat snare excision or cold forceps avulsion.
Lifting
Flat lesions may require submucosal lift to separate the desired tissue for resection from the underlying colonic muscular wall and decrease the risk of full-thickness mechanical disruption or thermal injury from a hot snare. Common submucosal lifting agents include saline, hyaluronic acid, glycerol, dilute albumin, and proprietary gels. For most polyps, submucosal saline injection suffices and provides a lift that lasts approximately 3 minutes [19]. Normal saline has proven equivalent to other lifting solutions in terms of complete resection rate, post-procedural bleeding, and post-polypectomy syndrome or perforation [20]. For more complex lesions requiring a longer resection time, a more durable solution is desirable. Viscous solutions are often more durable and provide a more localized lift with less lateral diffusion. Multiple solutions exist, ranging from hydroxyethyl starch (hetastarch) to more expensive proprietary solutions like Eleview® (Medtronic, Dublin, Ireland) and ORISE® (Boston Scientific, Marlborough, MA) that can last for over 40 minutes [21].
Adequate lift is critical to allow for advanced endoscopic techniques. Ideal injections are submucosal, but endoscopic injections can be easily misplaced in deeper layers (subserosal or intramuscular). Addition of colored dye to the injected solution can help delineate the submucosal layer as the overlying mucosa is thin and the color of the solution will be readily appreciated. Correctly placed submucosal injections tend to create more focal and taller lifts, while subserosal or intramuscular injections will create a less prominent and broader lift [22]. Submucosal injection can be facilitated by starting to inject solution prior to putting the needle into the mucosa so that the injectant will push away submucosal layers once penetrating the overlying mucosa. Alternatively, the needle can be placed into the colon wall and then gently withdrawn back into the submucosal layer. It is easier to create a lift when injecting in a tangential direction to the bowel wall and avoiding injecting perpendicular to the bowel wall. Techniques for submucosal injection are also applicable to endoscopic tattoo placement to avoid tattoo dispersing throughout the abdomen. If a larger area is needed to lift, injections should be directed at the border of the prior submucosal cushion to stay in the submucosal plane (Fig. 5.2).
To perform a submucosal injection, the injection needle should be tangential (parallel) to the mucosa. Fluid is injected as the needle is advanced to push away the muscularis and create and submucosal expansion to lift the overlying tissue (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography ©2020. All Rights Reserved)
Submucosal lift injections can be performed in a dynamic technique to make a taller lift. The needle placement in the submucosa is confirmed with a small amount of injection to demonstrate an adequate lift plane followed by a large-volume rapid injection. During the large-volume injection, the needle and scope can be re-directed within the submucosa to generate a tall and long-lasting lift [23]. For lesions that are on a fold, submucosal injection should start on the proximal/oral part of the bowel to lift the lesion toward the scope. Lesions that do not lift may be due to entry into the incorrect plane, scarring from past attempts at injection or polypectomy, or related to more advanced lesions that have invaded into the submucosa.
Endoscopic Mucosal Resection
Lesions that are too large for simple polypectomy can be treated with endoscopic mucosal resection (EMR). EMR is regularly used for polyps ranging from 20 mm to 50 mm in size. EMR is a technique designed for sessile or flat lesions that are confined to the superficial layer of the colon wall. The most common EMR method is the lift and cut technique, in which the lesion is lifted with a submucosal injection followed by snare polypectomy. With expansion of the submucosal space, the polyp can be removed without injury to the muscular layer of the bowel. The goal is to completely remove the polyp with as few snare excisions as possible [7]. EMR is started with a submucosal injection to lift the lesion to create space for resection. Since lesions with EMR are often larger than simple polypectomy, a solution with a longer durability than saline is desired. The ESGE recommends the addition of a staining dye (e.g., methylene blue or indigo carmine) to the submucosal injection to help identify lesion margins and deep tissue injury. The submucosal lift protects the underlying muscularis propria while decreasing resistance in the desired resection plane. The lesion is then resected with snare in as few pieces as possible with care to make sure that the entire lesion is removed. A normal margin of 2–3 mm of healthy-appearing tissue should be included to ensure complete removal. To decrease the risk of leaving islands of polyp tissue, piecemeal snaring should be done sequentially with the snare aligned along the margin of the prior resection. If there are any small remaining amounts of polypoid tissue, these can be ablated with electrocautery or removed with forceps. Following resection, clips can be selectively placed for tissue approximation (Fig. 5.3). Hot snare is commonly used during EMR. However, cold snare has also been shown to be effective for piecemeal resection after submucosal lift for polyps up to 55 mm with a low rate of recurrent disease or complication [24].
The major drawback of EMR is that larger lesions cannot be excised in en bloc fashion. EMR has been shown to be safe and effective for lesions smaller than 20 mm [25]. Lesions greater than 2 cm are often excised in piecemeal fashion, which limits the pathologic assessment of the polyp. Piecemeal resection can theoretically allow small amounts of polypoid tissue to remain that would result in recurrent polyp growth. While early experience with EMR indicated recurrent polyp formation on follow-up colonoscopy in 30% of patients [26], a recent prospective multicenter trial of 1000 EMR procedures demonstrated a lower recurrence rate (17% overall). For smaller polyps (20 mm in size), recurrence rate was 5% [27]. Risk factors for recurrence were increased size (OR = 8.2 for polyp >40 mm vs. 20 mm), APC usage (OR = 2.4), and bleeding (OR = 1.6). APC usage likely results in superficial ablation of the polyp, but does not eradicate the polyp tissue. The lack of efficacy of APC has been confirmed with other studies evaluating APC versus avulsion for the treatment of small amounts of residual polyp tissue after EMR. Avulsion with hot biopsy forceps was associated with a significantly lower adenoma recurrence rate compared to ablation with APC (10% recurrence with avulsion vs. 59% recurrence with APC on follow-up colonoscopy in 1 study of 278 patients with EMR of colon lesion >2 cm) [28].
Clip
While routine use of prophylactic clips after polypectomy is discouraged due to cost, endoscopic clips can be used selectively to re-approximate mucosa after EMR or be placed on bleeding vessels in an effort to increase hemostasis. Risk factors for post-polypectomy bleeding include large polyp size, proximal location, use of anticoagulant or antiplatelet agents, and the presence of multiple comorbidities [29]. In a recent multicenter randomized control trial, endoscopic clip application to close the mucosal defects of polypectomies for non-pedunculated polyps larger than 20 mm was associated with a decreased rate of post-polypectomy bleeding [30]. The benefit of clip application was most pronounced in the proximal colon with an absolute risk reduction of 6.3% (9.6% bleed without clips vs. 3.3% bleed with clips, p < 0.001). Clip application for large polyps in the distal colon did not affect the rate of post-polypectomy bleeding. Application of clips has also been shown to decrease the rate of delayed bleeding even if complete mucosal re-approximation could not be accomplished [31]. Therefore, consideration should be given for selective use of clips following endoscopic resection of large polyps (>2 cm), particularly in the proximal colon.
Underwater EMR
Underwater EMR was described in 2012 as a method to avoid submucosal injection during resection of large polyps with EMR [32]. As described above, submucosal injection may be in the wrong layer leading to intramuscular injection. Furthermore, submucosal injection may make snare application more challenging as the snare may slip over the distended mucosa and not grasp the polyp. To perform underwater EMR, the air is evacuated and the lumen is filled with 500 mL to 1 L sterile water. The edges of the polyp are marked with APC. The polyp is removed in piecemeal fashion with a snare on cutting current to include all of the prior APC marks. Any small remnant tissue is treated hot biopsy coagulation. It is hypothesized that the water distends and flattens the colon to prevent the muscularis from being brought into the snare excision. When compared to traditional EMR, selective groups have demonstrated that underwater EMR allows increased complete macroscopic resection and decreased recurrence rates [33]. Additionally, underwater EMR has been used to increase rates of salvage endoscopic resection for recurrent polyps after past attempts at endoscopic resection [34].
Underwater techniques have also been applied to endoscopic submucosal dissection (ESD) [35]. Polyp resection while submerged in water can allow the edge of mucosa to float away from the submucosa and therefore improve the endoscopic view of the dissection plane. Additionally, submerging the process of ESD in fluid allows greater heat dissipation, which theoretically decreases thermal injury. Potential benefits of underwater endoscopic resection must be balanced against the increased time requirement for water instillation.
Endoscopic Submucosal Dissection
Whereas EMR is limited in terms of size of en bloc excision, ESD is useful for larger lesions where complete histological evaluation is desired. ESD was first popularized in Japan in the 1990s for treatment of early gastric cancer. The gastric wall is thick and therefore allows for safe submucosal dissection with a margin for error. Colonic ESD was first described in the early 2000s [36]. The thin wall of the colon makes colonic ESD more challenging due to increased risk of full-thickness injury. However, the benefit of ESD is a more complete resection with lower recurrence rate. In a retrospective study of over 350 patients comparing colonic ESD and EMR, colonic ESD has a sevenfold lower recurrence rate. However, the complete resection of ESD comes at the cost of a nearly fivefold increased rate of perforation (6.2% ESD perforation vs. 1.3% EMR perforation) [37].
Colonic ESD allows resection of large benign lesions that traditionally required surgical resection. Dissection is performed in the submucosal layer under the lesion using a dedicated electrosurgical knife. Recent studies have shown that only 20% of polyps that were deemed endoscopically unresectable and referred to a surgeon for resection have invasive malignancy on final pathology [38, 39]. The rate of malignancy is even lower when carefully evaluating polyp morphology (see patient selection for ESD below). Large polyps that appeared benign to the endoscopist have less than 10% cancer rate [40]. This data suggests that the vast majority of patients with large benign-appearing colonic polyps can be treated adequately with endoscopic resection, saving these patients the morbidity of a larger colon resection. Comparing ESD to laparoscopic formal resection, patients treated with ESD had a significantly shorter hospital stay and decreased hospital financial cost [41]. Complication rates were similar, but the severity of complications was less in the patients treated with ESD compared to surgical resection.
ESD Complications
Prior to considering any intervention, one must be aware of the potential complications. Similar to most endoscopic polypectomy techniques, the most common complications after ESD are abdominal pain, bleeding, perforation, and tumor recurrence. Post-ESD electrocoagulation syndrome is similar to post-polypectomy syndrome and can be seen in up to 40% of patients [42]. Post-ESD bleeding occurs in approximately 2–7% of patients [43, 44]. ESD is also associated with a 5–20% perforation rate [45]. Risk of perforation is associated with increased tumor size and the presence of fibrosis. Perforation during ESD of lesions that are malignant can result in potential tumor seeding of the abdomen, as evidenced from the more robust gastric cancer literature. In a review of 22 perforations during gastric ESD, 2 patients (9%) had peritoneal seeding [46]. Lastly, endoscopic methods at resection carry the potential for recurrence. Local recurrence after ESD is remarkably low (approximately 1%) [43]. Furthermore, none of the recurrences contained invasive cancer and all were adequately managed with repeat endoscopic resection in this series.
Patient Selection for ESD
Careful selection of patients for attempted EMR and ESD is key. Procedural selection is based on the size of the tumor and the risk of underlying carcinoma. If the lesion is <2 cm, EMR is often favored. ESD is typically reserved for lesions >2 cm without features of malignancy. For patients where the diagnosis is unclear, ESD is an acceptable technique for excisional biopsy of lesions that have an increased risk of carcinoma but should be used with caution as the risk of full-thickness injury may be increased due to distortion of the submucosa from malignant invasion or fibrosis.
When doing a colonoscopy or preparing for ESD, the potential for underlying malignancy can be assessed by endoscopic characterization of the polyp appearance. Appearance of the lesion is critical and can be evaluated with one of several available classification systems, including Paris, Kudo pit pattern, or Narrow-band Imaging International Colorectal Endoscopic (NICE) classification. The gross morphology of the lesion is described by the Paris pattern, which divides lesions into polypoid vs. non-polypoid appearance. The non-polypoid superficial lesions are then divided based on their level of protrusion into the lumen (slightly elevated, flat, slightly depressed, and excavated). There is a clear inverse relationship between superficial lesion protrusion and the risk of submucosal invasion [47]. However, there is significant inter-observer variability in the classification of polyps according to the Paris system, suggesting that a simpler three-category classification of pedunculated, elevated, or depressed may be more widely applicable [48]. Depressed lesions have an increased rate of malignancy.
Pit patterns are based on the specific arrangement of glands in different lesions and can help determine hyperplastic vs. adenomatous vs. malignant lesions [49]. Narrow-band imaging (NBI) is commonly available technology that filters light into specific blue and green waveforms that will highlight vessels and mucosal tissue. NBI can be used to classify the polyp as hyperplastic, adenomatous, or malignant based on lesion color, vascular pattern, and surface pattern according to the NICE classification (Fig. 5.4) [50]. Accurate endoscopic assessment allows appropriate selection of polyps for EMR/ESD and avoidance of polyps that are better treated with resection due to concern for underlying malignancy.
NICE classification. NICE, NBI International Colorectal Endoscopic; NBI narrow-band imaging (Reused with permission from Hayashi et al. [50]. Copyright © Elsevier 2013)
The ability of the polyp to lift after submucosal injection has also been used to assess the potential for invasive malignancy. If tumor extends into the submucosa, the submucosa will not expand with injection. In a study of over 270 lesions, non-lifting sign had an overall accuracy of 95% for detecting an invasive malignancy, with a sensitivity of 62%, specificity of 98%, positive predictive value of 80%, and negative predictive value of 95% [51]. Furthermore, inadequate lift dramatically increases the likelihood of full-thickness injury as the submucosal layer is not expanded and there is consequently no buffer. Lesions may not lift well if there is fibrosis from prior attempts at resection or if the injection is too deep in the colon wall. The multiple reasons why a polyp will not adequately lift may explain why endoscopic assessment is more sensitive than the non-lifting sign for detecting invasion in flat or depressed lesions. Thus, in patients where the polyp does not lift well, there remains a role for ESD as long as the polyp has a benign morphologic appearance.
ESD Technique
Ideal polyps for ESD are polyps larger than 2 cm where invasion is not suspected. These are frequently laterally spreading tumors (LST) or polyps. For ESD, the mucosa is first marked outside of the edge of the lesion. This should be done with 2–3 mm normal mucosal margin. Although this step is not critical, it can be helpful for visualizing the borders. Submucosal injection should be performed outside of the coagulation marks so that there is a cushion under the endoscopic knife to decrease the risk of perforation. Once the lift is started, future injections should be directed at the edge of the prior lift to stay in the same plane and avoid the underlying muscularis propria. Once a submucosal lift has been established, the distal (anal) border of the mucosa around the lesion is incised in semicircular fashion with an endoscopic knife (Fig. 5.5). Complete circumferential incision will result in increased leak of submucosal fluid with greater difficulty of subsequent lift. After partial incision, further dissection proceeds tangential (parallel) to the submucosa to prevent injuring the colon wall by getting out of plane. Visualization is aided with a clear cap distal attachment to allow the endoscope to elevate the overlying mucosa and create traction. Additionally, positioning the patient in a manner that uses gravity to allow the polyp tissue to fall away from the colon wall will also improve exposure. Vessels are easily seen from the addition of a blue dye to the injection and are coagulated for hemostasis. As dissection continues, repeat submucosal injection is periodically used to expand the submucosa in front of the dissection.
ESD procedural steps (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography ©2020. All Rights Reserved). (a) 2-3 mm margin is marked followed by (b) submucosal injection. (c) Endoscopic knife dissection of the distal (anal) portion of the lesion. (d) Careful submucosal dissection with repeated submucosal injection as needed. (e) Removal of the polyp intact to allow complete pathologic analysis. Polyp can be pinned on a corkboard for orientation. (f) Final dissection. Vessels can be seen and coagulated. Selective closure is used
Occasionally, a hybrid method with ESD and EMR can be useful and time efficient. ESD techniques are used to define the resection borders, perform the lift, and get the dissection started. Afterward, the remaining central dissection can be done with a large snare in an effort to save time. Hybrid ESD can be performed with similar en bloc resection rates and shorter procedural time [52]. However, the recurrence rate following hybrid ESD is higher than conventional ESD alone [53].
Following resection, routine colonoscopic review of the resection bed should be performed to look for any full-thickness defect or exposed vessels. Small defects can be closed with clips or endoscopic suturing techniques (below). Larger perforations can be closed with an over-the-scope clip. Over-the-scope clips involve pulling the defect into a specially designed cap and then releasing a large multipronged clip over the defect to approximate the edges. Exposed vessels can be treated with minimum coagulation to decrease the risk of bleeding. The lesion is then placed in a net for removal and stretched onto a board with pins for histology.
As would be expected of any new procedure, there is a learning curve with ESD. ESD has been pioneered out of Japan due to the high incidence of gastric cancer treated with gastric ESD. The infrequency of early gastric cancer in the Western hemisphere limits the training opportunity for ESD techniques. Basic skills can be achieved through practice on ex vivo models. When transitioning to patient care, rectal lesions are in a more forgiving location due to the presence of the mesorectum, which will cover inadvertent full-thickness injuries. Even in high-volume centers, endoscopists may require up to 30 supervised cases prior to achieving technical proficiency of colonic ESD [54]. Endoscopists should expect a continued learning curve that may take years to master. In a single-center experience of 200 colonic ESD procedures, the perforation rate decreased from 12% during the first 100 cases to 2% in the second 100 cases [55]. Additionally, the en bloc resection rate increased from 80% to 92% over the 200 cases. Prior to developing an ESD program, one should achieve familiarity with methods of endoscopic closure and hemostasis to develop an arsenal of tools that can alleviate common complications.
Postoperative Care
As with most colonoscopy, patients treated with EMR can go home the same day. Patients treated with ESD may benefit from overnight observation. There is no need for prophylactic antibiotics. Abdominal x-rays are frequently used after a difficult dissection to look for the presence of free air. No dietary restrictions are necessary afterward.
Controversies with ESD Versus EMR
Critics of ESD may argue that en bloc resection of large, endoscopically benign-appearing colonic lesions is unnecessary as the rate of malignancy is <10% and that those lesions can be adequately treated with EMR [40]. Whereas ESD often involves advanced training and greater technical proficiency, EMR techniques are readily available with no specific setup and minimal additional training. Even though EMR has a higher recurrence rate, recurrences are usually detected with follow-up surveillance endoscopy and can be treated with repeat endoscopic interventions [27]. The downside of EMR is the piecemeal excision, which can be detrimental in polyps with carcinoma. In comparison, ESD can be curative for superficial carcinomas that invade upper 1/3 of the submucosa or <1000 μm (Sm1), as these lesions carry a low rate of lymph node metastasis [56]. However, this is a narrow population window for treatment. In comparing ESD and EMR, patients treated with ESD had a similar or higher rate of requiring subsequent surgery as patients treated with EMR [57]. In a study of over 1100 patients treated with colorectal ESD, the prevalence of invasive cancer was 19% [58]. Half of those were Sm2 and required surgical resection. Therefore, only 10% of patients treated with ESD had the benefit of complete resection of a superficial malignancy and avoidance of surgery. However, most would agree that there are certain patients with high-risk tumors that would benefit from en bloc resection to allow complete histologic analysis and potentially avoid major surgery. As a result of this potential benefit, ESD techniques are likely to continue to progress.
Endoscopic Suturing
Closure of large defects after ESD or EMR is challenging with traditional clip placement. In 2006, an over-the-scope endoscopic suturing platform was developed (OverStitch®, Apollo Endosurgery Inc., Austin, TX). The device requires a dual-channel endoscope and employs an endoscopic grasper to hold the oral side of the mucosa to pass the suture. The suture is then passed through the distal (anal) side of the mucosa to close the defect. Partial-thickness or full-thickness bites with the suture can be done to close the defect. The suture can be used in interrupted fashion or run as one long suture for more advanced endoscopists. Once facile with the device, endoscopic suturing is a time-efficient way to close large defects and may prevent the need for overnight observation [59]. Endoscopic suturing has been also used to effectively close full-thickness defects without the need for trans-abdominal operative intervention [60].
Stabilization Platforms
Advanced endoscopy can be challenging due to the lumenal folds and intra-procedural motion of the colon. Multiple stabilization platforms have been developed in an effort to allow more complex endoscopic surgery.
The DiLumen® (Lumendi Ltd., London, UK) is a double-balloon platform that fits over any colonoscope. The device is advanced over the scope to the desired location. The after-balloon is inflated, and then the fore-balloon is advanced beyond the target and inflated to create a therapeutic zone that is flat and smooth. The fore-balloon can also be used to create counter traction during ESD by attaching two small circles with suture to the balloon and then clipping the edge of the polyp resection to the circles [61]. When the fore-balloon is advanced, the edge of the resected mucosa is elevated to provide traction.
The ORISE Tissue Retractor System® (Boston Scientific, Marlborough, MA, USA) platform combines a stabilization cage along with two working channels to pass additional angled graspers to create counter tension. The flexible system is advanced over any colonoscope with a current working length of 40 cm. The lesion is placed at the 6 o’clock position and cage is then expanded to create a stable platform for surgery. Special graspers can be advanced to grasp tissue and then elevate the tissue to make dissection easier (Fig. 5.6) [62]. Endolumenal surgical platforms are rapidly progressing to simplify endoscopic resection techniques and allow resection of more complex lesions.
Examples of endoscopic surgical platforms that create a therapeutic working zone with creation of counter traction to aid in dissection. (a) The ORISE TRS platform by Boston Scientific (Marlborough, MA) has a stabilization cage with two available retractors to provide counter tension. Image provided by Boston Scientific Corporation. (b) The DiLumen C2 platform by Lumendi (Westport, CT) has a fore and aft balloon to straighten and stabilize the colon with two available retractors to create tension (Reused with permission from Lumendi, LLC)
Approach to Referral for Unresectable Polyp
Surgeons are frequently referred large polyps that are considered endoscopically challenging for consideration for colectomy. Historically, colectomy was performed with only a 20% malignancy rate, suggesting that 80% of patients were over-treated with colectomy [38]. Patients often come with photos from their endoscopy, and it is a challenge to determine if the polyp will be endoscopically resectable.
Colored endoscopy photos and the pathology must be closely evaluated. If the photos are good quality, the lesion can be closely evaluated for ulceration, contour of the mucosal surface of the polyp, and vascular pattern. Similar to the above section on patient selection, features of malignancy should prompt colectomy instead of endoscopic attempts at resection. If the photographs are poor, repeat colonoscopy with attempts for ESD or EMR should be performed. If the colonoscopy is done in the operating room, a step-up approach of progressively more invasive techniques can be perforrmed. Resection can be attempted with endolumenal surgery and if unsuccessful, the patient can have combined endoscopic and laparoscopic surgery (CELS) or laparoscopic colectomy if warranted. The patient is consented for all three procedures prior to starting. The least invasive technique is attempted first followed by progressively more invasive techniques to remove the polyp. The benefit to the patient is that the polyp is removed at one sitting. The downfall of this approach relates to scheduling constraints. However, as one masters the ESD technique and preoperative assessment, selected cases can be easily scheduled in endoscopy units either with conscious sedation or monitored anesthesia care to avoid utilizing an operating room.
Colonic Stenting
Endolumenal advances have also been made in the treatment of large bowel obstruction. Historically, large bowel obstructions have been treated with abdominal surgery and formation of an ostomy due to dilation of the bowel, inability to prep, and emergent indication. Self-expanding metallic stents delivered endoscopically offer a minimally invasive solution to large bowel obstruction. Colonic self-expanding metal stents are uncovered to allow tissue ingrowth and prevent migration. Outcomes following stent placement have been controversial [63]. Colonic stenting is currently utilized in two situations: (1) a bridge to surgery in left-sided colonic obstructions and (2) palliation of malignant large bowel obstruction. There is no role for prophylactic stenting.
As a bridge to surgery in left-sided obstructions, stenting can avoid the need for stoma formation if the obstruction can be relieved and then colonic edema resolves to allow primary anastomosis. Patients treated with colonic stenting as a bridge to resection have a fivefold decreased likelihood of permanent stoma formation with a significant increase in primary anastomosis and decrease in wound infection rates [64]. However, stent placement does have complications, including perforation rate of 5%, migration rate of 4–10%, and repeat obstruction in 30% [65]. Due to stent related complications, two randomized controlled trials of colonic stents were closed early [66, 67]. Concerns about the oncologic safety of stenting as a bridge to surgery exist [68, 69]. The only published guidelines on intraluminal colonic stents as a bridge to surgery are from the ESGE from 2014 and are based on meta-analyses showing increased rates of local recurrence without differences in overall survival [70]. These guidelines state that colonic stenting should not be the preferred method of treatment for left-sided obstructions in an otherwise healthy patient but could be considered in patients with a higher anesthetic risk (ASA ≥3 or age >70). At least two systematic reviews/meta-analyses published since then have concluded that the use of stenting as a bridge to surgery is oncologically safe with a similar 5-year survival, disease-free survival, and local recurrence rates as emergent surgery [71, 72]. Therefore, the use of stents in this setting is currently at the discretion of the individual surgeon based on experience and an assessment of the risks and benefits for a given patient’s unique clinical presentation.
In the palliative setting, endoscopic stenting has been recommended by the ESGE as the preferred method of treatment [70]. According to a recent meta-analysis, stent placement for palliation has a similar mortality rate to emergent surgery with a shorter hospital stay and decreased stoma rate [73]. A separate study showed that long-term stent placement allowed 95% of patients to avoid stoma formation [74].
Prior to considering any colonic stenting, water-soluble contrast enema should be performed to evaluate the relevant anatomy. For obstructions, it is important to map out the location of the tumor, length of stenosis, and the lumen caliber. Alternatively, CT with rectal contrast can provide similar information while also demonstrating potential extrinsic causes and metastatic potential. If no contrast makes it across the lesion, stenting is less likely to be successful as it will be very challenging to pass a guidewire and increase risk of false passage of the guidewire resulting in potential perforation.
Based on personal experience, stenting colonic obstructions secondary to extrinsic causes (i.e., intra-abdominal metastatic disease resulting in colonic luminal narrowing or obstruction) is associated with an increased rate of migration and perforation, likely because the colon wall is not thickened and the mucosa is normal and does not allow stent ingrowth. Therefore, palliative stent placement is usually reserved for intrinsic obstructing lesions. Patients are counseled regarding the risks of stent placement. Either inability to place the stent or procedural complication is followed by emergent surgery with diverting colostomy formation [75].
Stenting Technique
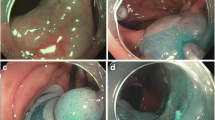
Contrasted enema study is performed (either under fluoroscopy or in CT) to develop a roadmap. Fluoroscopy is used to guide placement. A guidewire is placed across the lesion. Confirmation of location can be done by exchanging the guidewire for a catheter to inject contrast and air to confirm intraluminal location. Haustrations should be seen with double-contrast injection. The appropriate size stent is selected, with favor given to the largest diameter and longest stent available. Shorter stents are chosen for rectal lesions to avoid stent placement within 5 cm of the anus, which may result in significant tenesmus. The stent is passed under fluoroscopy guidance. A metallic clip can be placed 5 cm distal to the lesion as a radio-opaque marker for the landing zone of the distal aspect of the stent (Fig. 5.7). Balloon dilation of the stent is not recommended. The scope is not passed through the stent after placement to avoid potential stent dislodgement. Abdominal x-rays are performed in recovery to confirm location and rule out obvious free air (Fig. 5.8). Stent expansion will occur over the next 48 hours and the patient is monitored closely afterward for clinical result. Stool softeners are prescribed to help avoid fecal obstruction of the stent.
Endoscopic stent placement of obstructing colon lesion. A guidewire is used to cross the lesion (a). Catheter can be advanced to instill contrast and air to confirm luminal location proximally. The sheathed stent is then advanced over the guidewire under fluoroscopy guidance (b). A clip can be placed 5 cm distal to the lesion to align with the distal marker on the stent, and then the sheath is withdrawn to deploy the stent under fluoroscopy (c). The stent will straddle the lesion and expand over the following 48 hours (d). Note that the clip and the distal marker are aligned
Endoscopic stent placement. (a) The lumen in the obstructing mass is carefully selected and a guidewire is passed. Guidewire is exchanged for a catheter to inject contrast and air to confirm location. (b) Self-expanding metallic stent is then deployed. (c) Postoperative x-ray shows waist (red arrow) in the stent corresponding to the tumor location
Stenting Anastomotic Leaks
Esophageal covered stents have been used in the colon and rectum to treat contained anastomotic leaks with case reports documenting success [76, 77]. The stent will block further extravasation of stool and may allow healing of the sinus. However, there is a high rate of stent migration, which may require stent replacement. In reported small cohort studies, covered stents are left in place without fecal diversion ranging from 20 to 50 days. Following removal, repeat water-soluble enema study is performed. Successful closure was seen in 80–100% of patients.
Conclusion
Endolumenal approaches to surgery are rapidly advancing and offer patients a minimally invasive approach that can result in a shorter hospital stay and more rapid return to normal activity with less morbidity. Surgeons are the ideal provider for endolumenal procedures. Patients can be stepped up from endolumenal surgery to CELS to formal resection based on the nature of the colonic lesions. Additionally, surgeons have a firm understanding of the anatomic constraints and the ability to repair potential complications. Although endolumenal surgery is considered challenging at present, it will likely continue to progress and gain more popularity over time with increased patient benefits. Advancing technology and flexible endorobotics will undoubtedly facilitate this evolution.
Abbreviations
- ESGE:
-
European Society of GI Endoscopy
- EMR:
-
Endoscopic mucosal resection
- ESD:
-
Endoscopic submucosal dissection
- CELS:
-
Combined endoscopic-laparoscopic surgery
- ELS:
-
Endolumenal surgery
References
Wolff WI. Colonoscopy: history and development. Am J Gastroenterol. 1989;84(9):1017–25.
Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329(27):1977–81.
Aslan F, Cekic C, Camci M, Alper E, Ekinci N, Akpinar Z, Alpek S, Arabul M, Unsal B. What is the most accurate method for the treatment of diminutive colonic polyps?: standard versus jumbo forceps polypectomy. Medicine (Baltimore). 2015;94(15):e621.
Peluso F, Goldner F. Follow-up of hot biopsy forceps treatment of diminutive colonic polyps. Gastrointest Endosc. 1991;37(6):604–6.
Weston AP, Campbell DR. Diminutive colonic polyps: histopathology, spatial distribution, concomitant significant lesions, and treatment complications. Am J Gastroenterol. 1995;90(1):24–8.
Monkemuller KE, Fry LC, Jones BH, Wells C, Mikolaenko I, Eloubeidi M. Histological quality of polyps resected using the cold versus hot biopsy technique. Endoscopy. 2004;36(5):432–6.
Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, Jover R, Langner C, Bronzwaer M, Nalankilli K, Fockens P, Hazzan R, Gralnek IM, Gschwantler M, Waldmann E, Jeschek P, Penz D, Heresbach D, Moons L, Lemmers A, Paraskeva K, Pohl J, Ponchon T, Regula J, Repici A, Rutter MD, Burgess NG, Bourke MJ. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017;49(3):270–97.
Tate DJ, Bahin FF, Desomer L, Sidhu M, Gupta V, Bourke MJ. Cold-forceps avulsion with adjuvant snare-tip soft coagulation (CAST) is an effective and safe strategy for the management of non-lifting large laterally spreading colonic lesions. Endoscopy. 2018;50(1):52–62.
Leung K, Pinsky P, Laiyemo AO, Lanza E, Schatzkin A, Schoen RE. Ongoing colorectal cancer risk despite surveillance colonoscopy: the Polyp Prevention Trial Continued Follow-up Study. Gastrointest Endosc. 2010;71(1):111–7.
Lee CK, Shim JJ, Jang JY. Cold snare polypectomy vs. Cold forceps polypectomy using double-biopsy technique for removal of diminutive colorectal polyps: a prospective randomized study. Am J Gastroenterol. 2013;108(10):1593–600.
Shinozaki S, Kobayashi Y, Hayashi Y, Sakamoto H, Lefor AK, Yamamoto H. Efficacy and safety of cold versus hot snare polypectomy for resecting small colorectal polyps: systematic review and meta-analysis. Dig Endosc. 2018;30(5):592–9.
Yamashina T, Fukuhara M, Maruo T, Tanke G, Marui S, Sada R, Taki M, Ohara Y, Sakamoto A, Henmi S, Sawai Y, Saito S, Nishijima N, Nasu A, Komekado H, Sekikawa A, Asada M, Tumura T, Kita R, Kimura T, Osaki Y. Cold snare polypectomy reduced delayed postpolypectomy bleeding compared with conventional hot polypectomy: a propensity score-matching analysis. Endosc Int Open. 2017;5(7):E587–94.
Kawamura T, Takeuchi Y, Asai S, Yokota I, Akamine E, Kato M, Akamatsu T, Tada K, Komeda Y, Iwatate M, Kawakami K, Nishikawa M, Watanabe D, Yamauchi A, Fukata N, Shimatani M, Ooi M, Fujita K, Sano Y, Kashida H, Hirose S, Iwagami H, Uedo N, Teramukai S, Tanaka K. A comparison of the resection rate for cold and hot snare polypectomy for 4–9 mm colorectal polyps: a multicentre randomised controlled trial (CRESCENT study). Gut. 2018;67(11):1950–7.
Horiuchi A, Hosoi K, Kajiyama M, Tanaka N, Sano K, Graham DY. Prospective, randomized comparison of 2 methods of cold snare polypectomy for small colorectal polyps. Gastrointest Endosc. 2015;82(4):686–92.
Rabeneck L, Paszat LF, Hilsden RJ, Saskin R, Leddin D, Grunfeld E, Wai E, Goldwasser M, Sutradhar R, Stukel TA. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology. 2008;135(6):1899–906, 1906 e1.
Singaram C, Torbey CF, Jacoby RF. Delayed postpolypectomy bleeding. Am J Gastroenterol. 1995;90(1):146–7.
Nishizawa T, Suzuki H, Goto O, Ogata H, Kanai T, Yahagi N. Effect of prophylactic clipping in colorectal endoscopic resection: a meta-analysis of randomized controlled studies. United European Gastroenterol J. 2017;5(6):859–67.
Pohl H, Srivastava A, Bensen SP, Anderson P, Rothstein RI, Gordon SR, Levy LC, Toor A, Mackenzie TA, Rosch T, Robertson DJ. Incomplete polyp resection during colonoscopy-results of the complete adenoma resection (CARE) study. Gastroenterology. 2013;144(1):74–80 e1.
Fujishiro M, Yahagi N, Kashimura K, Mizushima Y, Oka M, Enomoto S, Kakushima N, Kobayashi K, Hashimoto T, Iguchi M, Shimizu Y, Ichinose M, Omata M. Comparison of various submucosal injection solutions for maintaining mucosal elevation during endoscopic mucosal resection. Endoscopy. 2004;36(7):579–83.
Ferreira AO, Moleiro J, Torres J, Dinis-Ribeiro M. Solutions for submucosal injection in endoscopic resection: a systematic review and meta-analysis. Endosc Int Open. 2016;4(1):E1–E16.
Castro R, Libanio D, Pita I, Dinis-Ribeiro M. Solutions for submucosal injection: what to choose and how to do it. World J Gastroenterol. 2019;25(7):777–88.
Sandhu J, Winkler C, Yan X, Sharabi A, Grimes Z, Shantha Kumara HMC, Cekic V, Whelan R. Sclerotherapy needle injections can expand the subserosal and muscularis propria layers and cause a stable mucosal lift in ESD/EMR patients. Surg Endosc. 2019;33(3):949–58.
Sanchez-Yague A, Kaltenbach T, Raju G, Soetikno R. Advanced endoscopic resection of colorectal lesions. Gastroenterol Clin N Am. 2013;42(3):459–77.
Piraka C, Saeed A, Waljee AK, Pillai A, Stidham R, Elmunzer BJ. Cold snare polypectomy for non-pedunculated colon polyps greater than 1 cm. Endosc Int Open. 2017;5(3):E184–9.
Repici A, Pellicano R, Strangio G, Danese S, Fagoonee S, Malesci A. Endoscopic mucosal resection for early colorectal neoplasia: pathologic basis, procedures, and outcomes. Dis Colon Rectum. 2009;52(8):1502–15.
Buchner AM, Guarner-Argente C, Ginsberg GG. Outcomes of EMR of defiant colorectal lesions directed to an endoscopy referral center. Gastrointest Endosc. 2012;76(2):255–63.
Moss A, Williams SJ, Hourigan LF, Brown G, Tam W, Singh R, Zanati S, Burgess NG, Sonson R, Byth K, Bourke MJ. Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut. 2015;64(1):57–65.
Holmes I, Kim HG, Yang DH, Friedland S. Avulsion is superior to argon plasma coagulation for treatment of visible residual neoplasia during EMR of colorectal polyps (with videos). Gastrointest Endosc. 2016;84(5):822–9.
Albeniz E, Fraile M, Ibanez B, Alonso-Aguirre P, Martinez-Ares D, Soto S, Gargallo CJ, Ramos Zabala F, Alvarez MA, Rodriguez-Sanchez J, Mugica F, Nogales O, Herreros de Tejada A, Redondo E, Pin N, Leon-Brito H, Pardeiro R, Lopez-Roses L, Rodriguez-Tellez M, Jimenez A, Martinez-Alcala F, Garcia O, de la Pena J, Ono A, Alberca de Las Parras F, Pellise M, Rivero L, Saperas E, Perez-Roldan F, Pueyo Royo A, Eguaras Ros J, Zuniga Ripa A, Concepcion-Martin M, Huelin-Alvarez P, Colan-Hernandez J, Cubiella J, Remedios D, ICX B, Lopez-Viedma B, Cobian J, Gonzalez-Haba M, Santiago J, Martinez-Cara JG, Valdivielso E, Guarner-Argente C, Endoscopic Mucosal Resection Endoscopic Spanish Society G. A scoring system to determine risk of delayed bleeding after endoscopic mucosal resection of large colorectal lesions. Clin Gastroenterol Hepatol. 2016;14(8):1140–7.
Pohl H, Grimm IS, Moyer MT, Hasan MK, Pleskow D, Elmunzer BJ, Khashab MA, Sanaei O, Al-Kawas FH, Gordon SR, Mathew A, Levenick JM, Aslanian HR, Antaki F, von Renteln D, Crockett SD, Rastogi A, Gill JA, Law RJ, Elias PA, Pellise M, Wallace MB, Mackenzie TA, Rex DK. Clip closure prevents bleeding after endoscopic resection of large colon polyps in a randomized trial. Gastroenterology. 2019;157(4):977–984 e3.
Albeniz E, Alvarez MA, Espinos JC, Nogales O, Guarner C, Alonso P, Rodriguez-Tellez M, Herreros de Tejada A, Santiago J, Bustamante-Balen M, Rodriguez Sanchez J, Ramos-Zabala F, Valdivielso E, Martinez-Alcala F, Fraile M, Elosua A, Guerra Veloz MF, Ibanez Beroiz B, Capdevila F, Enguita-German M. Clip closure after resection of large colorectal lesions with substantial risk of bleeding. Gastroenterology. 2019;157(5):1213–21. e4
Binmoeller KF, Weilert F, Shah J, Bhat Y, Kane S. “Underwater” EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest Endosc. 2012;75(5):1086–91.
Schenck RJ, Jahann DA, Patrie JT, Stelow EB, Cox DG, Uppal DS, Sauer BG, Shami VM, Strand DS, Wang AY. Underwater endoscopic mucosal resection is associated with fewer recurrences and earlier curative resections compared to conventional endoscopic mucosal resection for large colorectal polyps. Surg Endosc. 2017;31(10):4174–83.
Kim HG, Thosani N, Banerjee S, Chen A, Friedland S. Underwater endoscopic mucosal resection for recurrences after previous piecemeal resection of colorectal polyps (with video). Gastrointest Endosc. 2014;80(6):1094–102.
Yoshii S, Akasaka T, Hayashi Y, Tsujii Y, Nagai K, Higashino K, Ishihara R, Iijima H, Takehara T. “Underwater” endoscopic submucosal dissection: a novel method for resection in saline with a bipolar needle knife for colorectal epithelial neoplasia. Surg Endosc. 2018;32(12):5031–6.
Yamamoto H, Kawata H, Sunada K, Sasaki A, Nakazawa K, Miyata T, Sekine Y, Yano T, Satoh K, Ido K, Sugano K. Successful en-bloc resection of large superficial tumors in the stomach and colon using sodium hyaluronate and small-caliber-tip transparent hood. Endoscopy. 2003;35(8):690–4.
Saito Y, Fukuzawa M, Matsuda T, Fukunaga S, Sakamoto T, Uraoka T, Nakajima T, Ikehara H, Fu KI, Itoi T, Fujii T. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc. 2010;24(2):343–52.
Bertelson NL, Kalkbrenner KA, Merchea A, Dozois EJ, Landmann RG, De Petris G, Young-Fadok TM, Etzioni DA. Colectomy for endoscopically unresectable polyps: how often is it cancer? Dis Colon Rectum. 2012;55(11):1111–6.
Alder AC, Hamilton EC, Anthony T, Sarosi GA Jr. Cancer risk in endoscopically unresectable colon polyps. Am J Surg. 2006;192(5):644–8.
Gorgun E, Benlice C, Church JM. Does cancer risk in colonic polyps unsuitable for polypectomy support the need for advanced endoscopic resections? J Am Coll Surg. 2016;223(3):478–84.
Gamaleldin M, Benlice C, Delaney CP, Steele S, Gorgun E. Management of the colorectal polyp referred for resection: a case-matched comparison of advanced endoscopic surgery and laparoscopic colectomy. Surgery. 2018;163(3):522–7.
Jung D, Youn YH, Jahng J, Kim JH, Park H. Risk of electrocoagulation syndrome after endoscopic submucosal dissection in the colon and rectum. Endoscopy. 2013;45(9):714–7.
Gorgun E, Benlice C, Abbas MA, Steele S. Experience in colon sparing surgery in North America: advanced endoscopic approaches for complex colorectal lesions. Surg Endosc. 2018;32(7):3114–21.
Saito Y, Sakamoto T, Nakajima T, Matsuda T. Colorectal ESD: current indications and latest technical advances. Gastrointest Endosc Clin N Am. 2014;24(2):245–55.
Kim ES, Cho KB, Park KS, Lee KI, Jang BK, Chung WJ, Hwang JS. Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy. 2011;43(7):573–8.
Hirao M, Yamada T, Michida T, Nishikawa K, Hamakawa T, Mita E, Mano M, Sekimoto M. Peritoneal seeding after gastric perforation during endoscopic submucosal dissection for gastric cancer. Dig Surg. 2018;35(5):457–60.
Kudo S, Lambert R, Allen JI, Fujii H, Fujii T, Kashida H, Matsuda T, Mori M, Saito H, Shimoda T, Tanaka S, Watanabe H, Sung JJ, Feld AD, Inadomi JM, O'Brien MJ, Lieberman DA, Ransohoff DF, Soetikno RM, Triadafilopoulos G, Zauber A, Teixeira CR, Rey JF, Jaramillo E, Rubio CA, Van Gossum A, Jung M, Vieth M, Jass JR, Hurlstone PD. Nonpolypoid neoplastic lesions of the colorectal mucosa. Gastrointest Endosc. 2008;68(4 Suppl):S3–47.
van Doorn SC, Hazewinkel Y, East JE, van Leerdam ME, Rastogi A, Pellise M, Sanduleanu-Dascalescu S, Bastiaansen BA, Fockens P, Dekker E. Polyp morphology: an interobserver evaluation for the Paris classification among international experts. Am J Gastroenterol. 2015;110(1):180–7.
Kudo S, Rubio CA, Teixeira CR, Kashida H, Kogure E. Pit pattern in colorectal neoplasia: endoscopic magnifying view. Endoscopy. 2001;33(4):367–73.
Hayashi N, Tanaka S, Hewett DG, Kaltenbach TR, Sano Y, Ponchon T, Saunders BP, Rex DK, Soetikno RM. Endoscopic prediction of deep submucosal invasive carcinoma: validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest Endosc. 2013;78(4):625–32.
Kobayashi N, Saito Y, Sano Y, Uragami N, Michita T, Nasu J, Matsuda T, Fu KI, Fujii T, Fujimori T, Ishikawa T, Saito D. Determining the treatment strategy for colorectal neoplastic lesions: endoscopic assessment or the non-lifting sign for diagnosing invasion depth? Endoscopy. 2007;39(8):701–5.
Bae JH, Yang DH, Lee S, Soh JS, Lee S, Lee HS, Lee HJ, Park SH, Kim KJ, Ye BD, Myung SJ, Yang SK, Byeon JS. Optimized hybrid endoscopic submucosal dissection for colorectal tumors: a randomized controlled trial. Gastrointest Endosc. 2016;83(3):584–92.
Milano RV, Viale E, Bartel MJ, Notaristefano C, Testoni PA. Resection outcomes and recurrence rates of endoscopic submucosal dissection (ESD) and hybrid ESD for colorectal tumors in a single Italian center. Surg Endosc. 2018;32(5):2328–39.
Sakamoto T, Saito Y, Fukunaga S, Nakajima T, Matsuda T. Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum. 2011;54(10):1307–12.
Hisabe T, Nagahama T, Hirai F, Matsui T, Iwashita A. Clinical outcomes of 200 colorectal endoscopic submucosal dissections. Dig Endosc. 2012;24 Suppl 1:105–9.
Burgess NG, Bourke MJ. Endoscopic resection of colorectal lesions: the narrowing divide between East and West. Dig Endosc. 2016;28(3):296–305.
Fujiya M, Tanaka K, Dokoshi T, Tominaga M, Ueno N, Inaba Y, Ito T, Moriichi K, Kohgo Y. Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc. 2015;81(3):583–95.
Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010;72(6):1217–25.
Kantsevoy SV, Bitner M, Mitrakov AA, Thuluvath PJ. Endoscopic suturing closure of large mucosal defects after endoscopic submucosal dissection is technically feasible, fast, and eliminates the need for hospitalization (with videos). Gastrointest Endosc. 2014;79(3):503–7.
Kantsevoy SV, Bitner M, Hajiyeva G, Mirovski PM, Cox ME, Swope T, Alexander K, Meenaghan N, Fitzpatrick JL, Gushchin V. Endoscopic management of colonic perforations: clips versus suturing closure (with videos). Gastrointest Endosc. 2016;84(3):487–93.
Kantsevoy SV, Wagner A, Mitrakov AA, Thuluvath AJ, Berr F. Rectal reconstruction after endoscopic submucosal dissection for removal of a giant rectal lesion. VideoGIE. 2019;4(4):179–81.
Kantsevoy SV, Bitner M, Piskun G. New endoscopic platform for endoluminal en bloc tissue resection in the gastrointestinal tract (with videos). Surg Endosc. 2016;30(7):3145–51.
Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, Noya G, Sagar J. Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol. 2013;22(1):14–21.
Huck K, Hanenberg H, Gudowius S, Fenk R, Kalb R, Neveling K, Betz B, Niederacher D, Haas R, Gobel U, Kobbe G, Schindler D. Delayed diagnosis and complications of Fanconi anaemia at advanced age–a paradigm. Br J Haematol. 2006;133(2):188–97.
Han SH, Lee JH. Colonic stent-related complications and their management. Clin Endosc. 2014;47(5):415–9.
Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL. Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc. 2011;25(6):1814–21.
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P, Collaborative Dutch Stent-In Study G. Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol. 2011;12(4):344–52.
Sagar J. Role of colonic stents in the management of colorectal cancers. World J Gastrointest Endosc. 2016;8(4):198–204.
Maruthachalam K, Lash GE, Shenton BK, Horgan AF. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007;94(9):1151–4.
van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, JM DW, Donnellan F, Dumonceau JM, Glynne-Jones RG, Hassan C, Jimenez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbeau JM, Sabbagh C, Sagar J, Tanis PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A, European Society of Gastrointestinal E. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014;46(11):990–1053.
Cao Y, Gu J, Deng S, Li J, Wu K, Cai K. Long-term tumour outcomes of self-expanding metal stents as ‘bridge to surgery’ for the treatment of colorectal cancer with malignant obstruction: a systematic review and meta-analysis. Int J Color Dis. 2019;34(11):1827–38.
Amelung FJ, Burghgraef TA, Tanis PJ, van Hooft JE, Ter Borg F, Siersema PD, Bemelman WA, Consten ECJ. Critical appraisal of oncological safety of stent as bridge to surgery in left-sided obstructing colon cancer; a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2018;131:66–75.
Ribeiro IB, Bernardo WM, Martins BDC, de Moura DTH, Baba ER, Josino IR, Miyahima NT, Coronel Cordero MA, Visconti TAC, Ide E, Sakai P, de Moura EGH. Colonic stent versus emergency surgery as treatment of malignant colonic obstruction in the palliative setting: a systematic review and meta-analysis. Endosc Int Open. 2018;6(5):E558–67.
Repici A, Fregonese D, Costamagna G, Dumas R, Kahler G, Meisner S, Giovannini M, Freeman J, Petruziello L, Hervoso C, Comunale S, Faroux R. Ultraflex precision colonic stent placement for palliation of malignant colonic obstruction: a prospective multicenter study. Gastrointest Endosc. 2007;66(5):920–7.
Gunnells D, Whitlow C. Malignant bowel obstructions. Semin Colon Rectal Surg. 2019;30(3):100684.
DiMaio CJ, Dorfman MP, Gardner GJ, Nash GM, Schattner MA, Markowitz AJ, Chi DS, Gerdes H. Covered esophageal self-expandable metal stents in the nonoperative management of postoperative colorectal anastomotic leaks. Gastrointest Endosc. 2012;76(2):431–5.
Cooper CJ, Morales A, Othman MO. Outcomes of the use of fully covered esophageal self-expandable stent in the management of colorectal anastomotic strictures and leaks. Diagn Ther Endosc. 2014;2014:187541.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Johnston, W.F., Gorgun, E. (2022). Endoscopic Management of Polyps and Endolumenal Surgery. In: Steele, S.R., Hull, T.L., Hyman, N., Maykel, J.A., Read, T.E., Whitlow, C.B. (eds) The ASCRS Textbook of Colon and Rectal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-66049-9_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-66049-9_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-66048-2
Online ISBN: 978-3-030-66049-9
eBook Packages: MedicineMedicine (R0)