Abstract
As surgeons who care for patients with inflammatory bowel diseases (IBD), it is crucial that we are versed in the medical therapies to which our patients have been exposed. The treating colorectal surgeon should be able to manage these medications in the perioperative period and will regularly be called on as part of the multidisciplinary team to collaborate on the management on these therapies as part of surgical decision-making. The type and timing of medical therapy may also have implications for the type and timing of surgical intervention. In this chapter, we will review the most commonly prescribed medical therapies for Crohn’s disease (CD). We will focus the role of each class of medications has in the induction and maintenance of remission, their efficacy, commonly prescribed forms and dosing schedules, side-effect profiles, and the general treatment strategies used to approach these complex patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Crohn’s disease
- 5-Aminosalicylates
- Probiotics
- Antibiotics
- Budesonide
- Immunomodulators (IMM):Thiopurines & Methotrexate
- Corticosteroids
- Tumor necrosis factor inhibitors
- Leukocyte-trafficking agents
- Anti-IL 12
-
Antibiotics, probiotics, diets, and fecal transplant do not appear offer clinically significant benefit for treatment of Crohn’s disease.
-
Exclusive enteral nutrition is beneficial in children but has not yet be shown to be of benefit in adults.
-
5-Aminosalicylates are widely recognized to have role in treatement of mucosal ulcerative colitis, but have a very limited role in the treatment of CD.
-
Budesonide is efficacious for induction of clinical remission for CD patients when compared with placebo.
-
Systemic steroids are indicated for induction of remission, but not for maintenance of remission due to its side effects; steroid dependency is an indication for surgery.
-
Thiopurine and methotrexate monotherapy is not efficacious for induction of remission, but for maintenance of remission as a steroid-sparing agent; these medications are most commonly used in combination with biologics to decrease immunogenicity to the biologic agent.
-
Biologic agents are indicated for induction and maintenance of remission in patients with moderate-to-severe Crohn’s disease.
-
Biosimilars present no differences in efficacy or safety compared to their originator compounds and have the advantage of lower cost.
-
Therapeutic drug monitoring (TDM) of drug levels and anti-drug antibodies (ADA) allows more precise management of patients with Crohn’s disease.
History
The first case series describing regional enteritis was published in 1932 by a group of physicians at Mount Sinai Medical Center in New York City [1,2,3]. A senior surgeon, Dr. A.A. Berg, operated on 12 patients with terminal ileitis, and Drs. Leon Ginzburg and Gordon Oppenheimer wrote the initial manuscript. Of note, after Dr. Berg declined to be involved as a coauthor, Dr. Burrill Crohn was brought in as a third contributing author with two additional patients. At that time, the journal’s publication policy was to order the authors alphabetically – thus Dr. Crohn was the first author, and regional enteritis subsequently became known as Crohn’s disease, not Berg’s disease, nor Ginzburg- Oppenheimer disease [3, 4].
Introduction
As surgeons who care for patients with inflammatory bowel diseases (IBD), just as we expect IBD-gastroenterologists (GI) to be facile with surgical treatment options, it is their expectation that we be facile with the medical therapies to which our patients are exposed. The treating colorectal surgeon should be able to manage these medications in the perioperative period, and may be called upon as part of the multidisciplinary team to provide perspective on initiation, continuation, or escalation of medical therapies as part of surgical decision-making. The types and timing of medical therapy may also have implications for the type and timing of surgical intervention. In this chapter, we will review the profiles of the most commonly prescribed medical therapies for Crohn’s disease (CD). We will focus the role of each class of medications has in the induction and maintenance of remission, efficacy, commonly prescribed forms and dosing schedules, side-effect profiles, and perioperative management for these complex patients. Interested readers are referred to the recommendations of the American Gastroenterology Association (AGA) 2013 Guideline on Medical Management in Crohn’s [5], the American College of Gastroenterology (ACG) 2018 Crohn’s Guideline [6, 7], and the European Crohn’s and Colitis Organization (ECCO) 2020 Crohn’s Guideline [8]. A summary of the treatment recommendations for these guidelines is shown in Table 46.1.
The AGA guideline [5], which is now the oldest and due to be updated, was limited to 9 recommendations on the use of thiopurines, methotrexate (MTX), and TNF inhibitors (TNFi’s) for the induction of remission and maintenance of remission, while the ACG guideline is the most comprehensive and made a total of 60 recommendations which were stratified based on the severity of illness; mild-to-moderately severe disease/low-risk disease vs. moderate-to-severe disease/moderate-to-high-risk disease vs. severe fulminant disease vs. perianal disease. The ACG guideline also made recommendations regarding postoperative prophylaxis including smoking cessation and that intra-abdominal abscesses should be treated with antibiotics and either radiologic or surgical drainage [2]. Finally, the recently updated ECCO guideline recommendations were stratified in a manner similar to the AGA’s based on induction (10 recommendations) and maintenance (13 recommendations) of remission, plus perianal disease (7 recommendations) for a total of 30 recommendations.
In contrast to ulcerative colitis (UC), for which surgery is curative for the colonic and rectal manifestations of disease, patients with CD have a life-long disease for which surgery only manages the complications of the inflammatory, fibrostenotic, penetrating, and neoplastic manifestations of disease. Surgery will often “reset the clock,” and many patients will be able to be managed expectantly without ongoing medical therapy and a colonosocpy 6 months after ileocolic resection to assess disease activity. However, those with high-risk phenotypes (Table 46.2) will require active postoperative medical therapy to prevent or delay post-operative recurrence (POR).
Microbiome Therapies
Antibiotics
Overall, antibiotics are probably not efficacious for induction or maintenance of remission in CD [9,10,11]. A systematic review with meta-analysis from 2011 found that in active CD, compared to placebo, antibiotics may be efficacious (RR 0.85, 95% CI 0.73–0.99, p = 0.03); however this pooled analysis combined a number of different antibiotics, and the excessive heterogeneity precluded definitive conclusions. The Cochrane collaboration updated their review in 2019 and found 13 randomized controlled trials (RCT) examining the role of antibiotics for the induction and maintenance of remission [12]. They concluded that although antibiotics may be modestly beneficial, this may not be clinically significant based on moderate- to high-quality evidence. Although there was high-quality evidence that antibiotics are safe, efficacy for maintenance of remission was not demonstrated and remains uncertain. Therefore, the ACG and ECCO guidelines do not recommend them for induction or maintenance of remission, nor for maintenance of remission, consistent with North American practice [11].
Although antibiotics likely do not have a definitive role in the induction or maintenance of remission for luminal or perianal CD, they obviously have a role in the management of septic complications of penetrating CD; aspirates from percutaneously or intraoperatively drained abdominopelvic abscesses should be sent for aerobic, anaerobic, and fungal cultures with sensitivities to guide optimal management [6, 13]. The Toronto Consensus statement concluded that antibiotics only have a role in initial symptomatic control of perianal disease [14]. Of note, ciprofloxacin has recently had a black box warning for tendinopathy, especially in older patients also receiving corticosteroids [15]. Low-dose metronidazole may be used to decrease drainage. The principles of management of perianal CD are covered in another chapter.
Probiotics
Probiotics are beneficial microorganisms that can alter the gut’s microbiota, metabolic activity, and immunomodulation to confer patient benefit. These bacteria and fungi alter microbial diversity through competitive inhibition of other microbes, enhance mucosal barrier function via the production of short-chain fatty acids, and interact with intestinal dendritic cells to instigate an anti-inflammatory response. The microorganisms must be of human origin, nonpathogenic, and able to survive the gastrointestinal transit in order to be beneficial. Unfortunately, multiple meta-analyses suggest that probiotics are ineffective for induction and maintenance of remission in patients with CD and may not be without risks [16,17,18].
Dietary Interventions
Similarly, dietary interventions have failed to demonstrate efficacy for the induction and maintenance of remission [19]. The Cochrane group performed a meta-analysis of 18 RCTs including 1,878 patients who received dietary intervention. Interventions included high-fiber, low-refined carbohydrate diets, low-microparticle diets, low-calcium diets, symptom-guided diets, and highly restricted organic diets. In general, efficacy was suggested by several of the diets, particularly the symptom-based and several restrictive diets; but overall the studies were heterogenous, prone to bias, and of low- or very-low quality of evidence. The authors made no firm conclusions but did note that there are several well-designed ongoing RCTs in over 500 patients examining this topic, and that the meta-analysis would be updated subsequently.
Fecal Transplant
The other manner in which a patient’s microbiota can be altered is via fecal microbiota transplant (FMT). This management has proven useful in treating recurrent Clostridium difficile infections (CDI), but has not been adequately studied nor shown efficacy in CD. A recent small pilot RCT of 17 patients with CD who achieved remission with steroids and underwent FMT did not demonstrate the primary efficacy endpoint, although endoscopic scores and C-reactive protein (CRP) levels were significantly better in the FMT-treated patients [20]. A meta-analysis suggested FMT may have efficacy in UC but not Crohn’s; no safety concerns were raised by this study [21]. The Cochrane groups meta-analysis on this topic suggested a lack of available studies of FMT for CD, with no studies examining the role of FMT for induction of remission in CD [22]. Interestingly, a separate meta-analysis of FMT for CDI in IBD patients demonstrated efficacy, just as in the non-IBD population [23]. Of note, on March 12, 2020 the Food & Drug Administration (FDA) released a Safety Alert after 2 patients with chornic medical conditions who received FMT for CDI died of complications related to FMT-related transmission of enteropathogenic and/or shigatoxin-releasing E. coli.
Exclusive Enteral Nutrition
A promising form of nutritional intervention specific to CD is exclusive enteral nutrition (EEN). EEN is a nutritional intervention where patients are placed on a full-liquid mono-diet with a commercially available nutritional supplementation [24]. In pediatric CD patients, EEN has been shown to be more effective than steroids for induction of remission, but this has not yet been replicated in adult CD patients [25]. Presently, some centers use EEN in adults while they are tapered off steroids as they await elective surgery [26].
5-ASA Therapy
5-Aminosalicylate (5-ASA) moieties, which have a large role in the medical treatment of UC, are widely recognized to have a limited role in the treatment of CD. The indication for this class of medications is for the induction and maintenance of remission in mild-to-moderate UC. These medications are covered more fully in the Medical Therapy of UC chapter. The mechanism of action of 5-ASAs is as topical anti-inflammatory agents, which explains their efficacy in mucosal UC as opposed to CD, which is a full-thickness bowel disease.
Multiple well-designed double-blinded placebo-controlled RCTs of oral formations with varying dosages and meta-analyses have concluded that oral 5-ASAs lack efficacy for the induction of clinical remission for ileal, ileocolic, or colonic CD. In addition, as noted in the meta-analysis within the ECCO CD guidelines, oral 5-ASAs also lack efficacy for the maintenance of remission (RR 1.03, 95% CO 0.92. 1.16) [8].
Isolated Colonic Crohn’s
Nonetheless, the question remains if there is a role for 5-ASAs in isolated colonic CD. The largest trials of 5-ASAs for colonic disease were the National Cooperative Crohn’s Disease Study (NCCDS) and the European Cooperative Crohn’s Disease Study (ECCDS) [27, 28]. There were mixed results in the early clinical trials with mild-to-moderate disease, but these studies also lacked endoscopic or biochemical data [29]. Thus, a need exists to replace this older data with new studies which include modern assessments tools [30]. Some providers will use 5-ASAs in patients with mild colonic CD and assess response, in a treat-to-target manner with mucosal healing as the endpoint. 5-ASAs are not approved for CD in the USA but are approved in Europe, Canada, Australia, and Japan. Of note, the ACG and ECCO treatment guidelines also concluded that 5-ASAs lack efficacy for induction of remission in CD [6, 8].
Crohn’s Proctitis
Despite the overall lack of efficacy for the induction or maintenance of remission of CD, there may be a role for 5-ASA rectal formulations for patients with proctitis [31]. Proctitis may result in disabling fecal urgency, tenesmus, and agoraphobia. 5-ASA enemas and suppositories may have a role in palliating these symptoms as adjuncts to primary medical therapy. Mesalamine suppositories are typically prescribed at doses of 500–1000 mg per rectum at bedtime, with mesalamine enemas at 4 grams/60 cc enemas 1–2 times per day. These formulations are typically well-tolerated but often require prior authorization and/or may be non-formulary for many commercial insurance plans.
Side-Effects and Perioperative Management
5-ASA medications have an excellent safety profile and may be resumed postoperatively. The most common side-effects of these medications include gastrointestinal (GI) upset, headaches, and skin hypersensitivity to sun [29]. Rare side-effects include bone marrow suppression, fever, hemolytic anemia, hepatitis, hypersensitivity reactions, pancreatitis, pneumonitis, and rash. Patients who take sulfasalazine must also take folic acid (1 mg daily) because the medication depletes folic acid stores [29, 31].
Corticosteroids
Topical Corticosteroids
Budesonide is a synthetic glucocorticoid which is administered as an oral enteric-coated capsule which resists gastric degradation. Budesonide has high first-pass metabolism and very limited systemic absorption and is generally well-tolerated [32]. It comes in 3 mg capsule and is dosed up to 9 mg per day. Of note, budesonide is the mainstay of therapy for induction of remission in microscopic and collagenous colitis. In order to target small bowel proximal to the terminal ileum, the “open-capsule technique” may be chosen for administration; half of the daily dose (one full 3 mg capsule and half of one 3 mg capsule) is opened and sprinkled on food. The Multimatrix® (MMX®) formulation allows for controlled release for use in the colon [33].
A Cochrane meta-analysis found that budesonide was efficacious in the induction of clinical remission for CD patients, when compared with placebo [34]. This meta-analysis also stated that budesonide was not as effective as conventional steroids but was significantly safer. They also found a lack of efficacy for maintenance of remission. The ACG and ECCO guidelines recommend budesonide for the induction of remission in mild-to-moderate ileal or right-sided colonic disease [6, 8]. For maintenance of remission, the ACG guidelines suggest it not be used for more than 4 months, but the ECCO guidelines allow for maintenance therapy with budesonide [6, 8].
Side-Effects and Perioperative Management
Although well-tolerated and safer than traditional steroids, budesonide may have side effects (Table 46.3), especially when used for prolonged periods of time. When used for less than 1 year, the side-effect profile is similar to that of placebo with rare occurrences of the clinically important side effects typically associated with traditional glucocorticoids [35]. Given the excellent safety profile of budesonide with its limited systemic absorption, budesonide may be safely held immediately before and after surgery, stress-dose steroids are not needed, and resumption postoperatively may not be necessary.
Systemic Corticosteroids
Traditional corticosteroids are powerful systemic anti-inflammatory drugs which were first used by Truelove and Witt for the treatment of IBD in 1955 [36, 37]. Although they are extremely efficacious as anti-inflammatories, they have an unfavorable side-effect profile which limits their clinical utility to induction of remission in otherwise medically refractory disease. A meta-analysis limited to randomized controlled trials identified 2 trials including 267 patients using standard oral glucocorticoids to induce remission in active Crohn’s disease [38]. Overall, 79 of 132 patients (60%) assigned to oral glucocorticoids achieved remission compared with 42 of 135 (31%) prescribed placebo. Moreover, the number needed to treat to achieve remission in one patient with standard glucocorticoids was 3 (95% CI, 2–11), which is very low and associated with high efficacy. Both the ACG and ECCO guidelines recommend systemic steroids for induction of remission, but not for maintenance of remission [6, 8]. Steroids should not be used chronically as long-term use carries have a high risk of serious adverse events. The need for systemic steroids represents a “bad omen” or “tipping point” for patients with CD, as it is associated with a more complicated disease course. Steroid dependency is an indication for surgery.
For outpatient induction of remission, prednisone is typically prescribed at 40 mg by mouth daily and tapered by 5–10 mg per week; but this depends on what other medical or surgical options the patient, gastroenterologist, and colorectal surgeon are contemplating. Steroid conversion calculators and tables (Table 46.4) [37], widely available on the Internet, allow for conversion between enteral, parenteral, and various formulations.
Safety
Despite the substantial efficacy for induction of remission in CD, chronic corticosteroid treatment is among the most significant risk factors for postoperative infectious and/or wound complications. A summary of the toxicity of corticosteroid therapy is shown in Table 46.5 [37]. The side effects are organ-based and wide-ranging and for the most part dose- and duration-dependent. Cessation of steroid therapy will ameliorate some, but not all, of the risks of exposure to these medications. The side effects would not likely be considered acceptable, if not for the wide therapeutic effect across a wide range of human auto-inflammatory and autoimmune diseases. Many of these diseases lacked any efficacious therapy other than corticosteroids until recently. Chronic steroid use, loosely defined as more than several months, has largely fallen by the wayside as new biologic treatments with better short- and long-term safety profiles continue to be developed and marketed.
Stress-Dose Steroids and Tapering
Of note, several publications have examined the role of stress-dose steroids in the perioperative period for IBD [39,40,41,42]. In a series of steroid-dependent UC patients, only one patient developed postoperative adrenal insufficiency [39]. The authors concluded that stress-dosing was not beneficial, but all steroid-dependent patients should be monitored after surgery for symptoms of adrenal insufficiency. Two studies from Cedars Sinai had similarly questioned the utility of stress-dose steroids at the time of surgery for IBD [41, 42]. In the era of enhanced recovery, many patients receive 8 mg of intraoperative dexamethasone for postoperative nausea and vomiting prophylaxis which effectively replaces the need for stress-dose steroids [26]. For patients who received a short-term (1-2 weeks) of steroids preoperatively, it is our practice to simply stop them postoperatively, and for those on chronic steroids to continue post-operative corticosteroids at the same dose, or dose-equivalent, the patient was receiving preoperatively [43,44,45].
Chronic steroid therapy must not be stopped abruptly lest patients develop severe Addisonian crisis with circulatory collapse (Table 46.6). On the other hand, no evidence-based guidelines for steroid tapering exist [46]. When patients do present to surgery receiving corticosteroids, the rapidity with which they may be tapered depends on the chronicity of treatment. We typically reduce the dose by 50% every 5–7 days. Sometimes a slow taper with several additional weeks is required if the patient has been on steroids for a prolonged period to avoid withdrawal symptoms such as fatigue, lethargy, and depression. Testing for adrenal suppression in such cases is typically not needed; the patients can either be counseled that these uncomfortable symptoms will eventually pass, or their corticosteroid dose can be increased with a more prolonged tapering schedule. Readers are referred to the an excellent resource Glucocorticoid Therapy and Adrenal Suppression in the Internet book Endotext for further reading at www.endotext.org.
Immunomodulators
Thiopurines
Thiopurines (TPs) , namely 6-mercaptopurine (6MP) and azathioprine (AZA), along with methotrexate (MTX), are known as immunomodulators (IMM) [5, 6, 9]. TPs are purine analogs and thus antimetabolites, which inhibit DNA and have antiproliferative properties and proapoptotic action on activated T-lymphocytes [31]. The typical dose of AZA is 2 mg/kg daily, while 6MP is typically 1 mg/kg daily. AZA and 6MP are typically started at low doses (50 mg and 10 mg, respectively) with biweekly complete blood counts and liver function testing and given normal labs dose escalation every 2 weeks to the desired dose. Of note, the clinical effect of TP therapy takes several months, so patients are typically re-evaluated after 3 months of therapy [31].
TP Pharmacokinetics
AZA is a prodrug of 6MP , and both AZA and 6MP are prodrugs of 6-thioguanine (6TG). AZA and 6MP are converted by intracellular thiopurine methyltransferase (TPMT) to 6TG (Fig. 46.1) [47]. Clinical TPMT activity testing is critically important for patients prior to being placed on TG treatment [48]. While 80% of the population has normal TPMT metabolism, ~10% have hyperactive TPMT metabolic activity (“shunters”) which leads to the accumulation of toxic secondary metabolite, increasing the likelihood of drug side-effects such as hepatotoxicity [49]. Shunters, as the name implies, also shunt drug away from the normal metabolic pathway, resulting in less clinical activity. The shunting can be overcome by using allopurinol, which inhibits secondary metabolite production, and prescribing 25% of the usual TG dose [49].
In addition to the shunters, 10% of the population are heterozygous for TPMT and have intermediate (lower than average) metabolic activity, and 0.3% of the population are TPMT deficient (homozygous). The intermediate activity patients require a higher than average dose to acquire the desirous effect, while the deficient population will not be clinically responsive to TP treatment [48, 49].
Monotherapy
Current guidelines agree that TP are efficacious at the maintenance of remission of luminal CD obtained by other means and that they are not efficacious for the induction of remission in mild-to-moderate luminal CD [5, 6, 9]. This is mainly due to their onset of action; thus they may be started concomitantly with other medications for the induction of remission, which can then be weaned (in the case of steroids) while the TPs take effect. Thus, TPs have traditionally served a role as monotherapy for the maintenance of remission in CD as a steroid-sparing agent.
Specifically, when patients were unable to be weaned off steroids, TP therapy would provide an exit strategy from the steroid dependency in patients who were able to achieve but not maintain remission without continued steroids. In a meta-analysis of placebo-controlled randomized trial in steroid-dependent patients, AZA was shown to be superior to placebo (RR 1.19, 95% CI 1.05–1.34) for maintenance of remission as a steroid-sparing agent [5]. Combination therapy will be covered below in the section on biologics.
Relative contraindications include patients with neoplasia or hematologic comorbidities [49]. MTX is a relatively safe and more widely acceptable alternative in older patients and especially in young men. The EBV status in young males is important, as young men with +EBV status are at a very small but demonstrable risk of developing hepatocellular T-cell lymphoma, a universally-fatal condition, thus TGs are avoided in these at-risk patients. In addition, EBV naïve patients are at risks of developing hemaphagocystosis.
Side Effects and Perioperative Management
The side effects of TG therapy can be significant and are shown in Table 46.7. Idiosyncratic pancreatitis is the most common dose-independent side effect; hepatitis, which is dose-dependent and whose risk increases with ongoing therapy, is the most common overall. Many patients have GI side-effects from TG therapy; CBCs are used to assess for hematologic consequences. It is controversial whether long-term use has been associated with malignancy. The best available population-based cohort data comes from the CESAME – Cancer and Increased Risk Associated with Inflammatory Bowel Disease in France study group. They suggest risk is increased in IBD patients receiving TP therapy for hematologic neoplasia including leukemia and lymphoma, non-melanoma skin cancer, cervical cancer, and urinary tract cancer. The risk of colorectal adenocarcinoma may actually be lower due to control of intestinal inflammation [50,51,52]. TG therapy also have a number of drug-drug interactions to be aware of including ACE inhibitors, allopurinol, anticoagulants, sulfamethoxazole/trimethoprim, and other immunomodulators including MTX and cyclosporine A [49].
TP may be safely used in the perioperative period. Although therapeutic efficacy takes several months to be observed, the half-live of these medications is very short. In addition, TPs have not been shown to be associated with postoperative complications in IBD patients [53]. Thus, most surgeons hold TP therapy in the immediate postoperative period and allow the referring gastroenterologist to reassess the need for ongoing IMM therapy.
Methotrexate
The other drug in the immunomodulator class is MTX, which is also an antimetabolite, similar to the TGs. The discovery of MTX as a powerful inhibitor of cellular metabolism and mitosis was honored with a Nobel Prize in 1988, and the first trial demonstrating a benefit of MTX in CD was in 1989 [54, 55]. MTX has efficacy in the maintenance of remission of luminal CD obtained by other means and is not recommended for the induction of remission [5, 6, 9]. MTX inhibits TNF, MMPs, JAK 1/2, and IL-23 pathways [56]. It is typically prescribed at a dose of 25 mg subcutaneously (SC) or intramuscular (IM) weekly for active CD, and 15 mg PO/SC weekly for maintenance therapy, both with 5 mg of folic acid PO weekly.
Side-Effects and Perioperative Management
Similar to TPs, MTX may have dose-limiting toxicity (Table 46.8). For fertile young couples, pregnancy must be avoided as MTX is a known teratogenic agent and abortifacient, and abstinence and/or high-quality contraceptives should be used [57,58,59,60]. An effect of MTX on sperm counts and quality has also been described.
MTX inhibits dividing cells and thus may interfere with wound healing. However, it has a very short half-life. MTX does not appear to be associated with postoperative complications [61]. Thus, the perioperative management of MTX is the same as for TPs mentioned above; they may be safely discontinued prior to surgery and held in the postoperative period, and their ongoing therapeutics need to be reassessed by the GI team after recovery.
Biologic Therapy
Since the FDA approval of infliximab in 1998, biologic agents (summarized in Table 46.9) have revolutionized the treatment of CD. Rather than indiscriminate immunosuppression, biologic medications are monoclonal antibodies directed at particular proteins that drive the inflammatory cascade of IBD. They are approved to induce and maintain remission in moderate-to-severe CD. This is defined using clinical and endoscopic factors and typically includes a Crohn’s disease activity index (CDAI) >220, a Crohn’s disease endoscopic index of severity (CDEIS) >8, or a simple endoscopic score (SES-CD) >6. At present, there are three categories of biologic agents with six commonly used medications that are FDA-approved for this indication:
-
1.
Tumor Necrosis Factor inhibitor (TNFi) agents
-
Infliximab
-
Adalimumab
-
Certolizumab pegol
-
-
2.
Anti-integrin agents
-
Natalizumab
-
Vedolizumab
-
-
3.
Anti-interleukin agents
-
Ustekinumab
-
Selection of biologic therapy should be driven by patient and physician preference; but in reality, insurance approval and cost are often factors into which agent is ultimately chosen. A 2017 review of insurance policies regarding biologic use for IBD reported that 90% of policies are inconsistent with AGA guidelines [62].
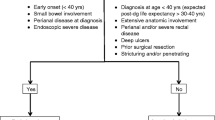
The positioning of biologic agents in the therapeutic algorithm is a matter of debate. Historically, a “step-up” strategy starting with 5-ASA compounds, IMM, and corticosteroids with escalation to biological therapy after failure to maintain remission has been employed. The top-down approach (early utilization of biologics) has been suggested for patients presenting with poor prognostic factors suggesting a complicated phenotype (Table 46.2). The goal of this approach is to optimally control disease and prevent complications such as fistula or stricture, where medical therapy is less or ineffective. Factors such as early age of diagnosis, stricturing or fistulizing disease, perianal or severe rectal disease, extensive involvement of the GI tract, deep ulcerations, prior surgical resection, or rapid onset should be considered for early biologic therapy. High-risk patients have shown benefit from the early use of TNFi’s for an overall risk reduction of surgery, hospitalization, loss of response, and the development of disease-related complications [63].
Before initiation of biologic therapy, routine assessment for tuberculosis (typically using QuantiFERON-TB Gold) and viral hepatitis and selective assessment for histoplasmosis and blastomycosis should be initiated. Patients should be vaccinated against pneumococcus, varicella, human papilloma virus, influenza vaccine, hepatitis A vaccine, and herpes zoster.
Antitumor Necrosis Factor Agents
The TNFi agents are infliximab, adalimumab, and certolizumab pegol. These medications successfully modulate the immune system by binding to tumor necrosis factor alpha (TNF-alpha) and inhibiting signal transduction and limiting inflammation. These agents are proven to induce remission and provide maintenance therapy in patients with moderate-to-severe CD and are supported by the AGA, ACG, and ECCO guidelines [5, 6, 8]. Several meta-analyses of RCTs support their use in those who failed therapy with steroids or other forms of immunosuppression [64,65,66]. TNFi’s- are particularly useful in the management of perianal or rectal disease, fistulizing CD , patients at high-risk for postoperative recurrence, and those with pyoderma. Response may be seen within the first few weeks after starting therapy, but maybe delayed up to 6 weeks after initiation.
Infliximab (IFX) is a chimeric mouse-human immunoglobulin (Ig) monoclonal antibody. This is typically administered with intravenous induction dosing at 5 mg/kg at weeks zero, two, and six followed by maintenance therapy every 8 weeks thereafter. IFX is the only agent with a phase 3 study demonstrating efficacy for the treatment of fistulizing disease, particularly perianal disease [67]. There are some data suggesting that infliximab is also associated with fewer hospitalizations, surgeries, and steroid use when compared with other TNFi agents for CD [68].
Adalimumab (ADA) is a fully human Ig monoclonal antibody given subcutaneously. This is started with induction dosing of 160 mg at week zero, followed by 80 mg at week 2, and then 40 mg every 2 weeks thereafter.
Certolizumab pegol is a PEG-ylated Fab fragment. This medication is self-administered subcutaneously at a dose of 400 mg at weeks 0, 2, and 4, followed by 400 mg every 4 weeks thereafter.
Adverse events with TNFi drugs include psoriasis , arthritis, hepatoxicity, rarely cytopenia, and an increased risk of melanoma and lymphoma formation [69]. Patents on combination therapy with immunomodulators may also have an increased risk of non-melanoma skin cancers and lymphoma [69]. Patients are also at risk for opportunistic infections.
Combination Therapy
The use of combination therapy with immunomodulators has been shown to increase TNFi serum concentrations while minimizing the risk of adverse drug reactions [70]. Unfortunately, combination therapy has also been associated with an increased risk of opportunistic infections [71, 72].
When starting IFX, combination therapy with a TP is generally recommended. The SONIC (Study Of Biologic and Immunomodulator Naïve Patients In Crohn’s Disease) trial compared IFX with AZA to each therapy alone in treatment naïve patients [70]. Combination therapy was more likely to result in mucosal healing [RR: 1.82; 95% CI: 1.01–3.26] and clinical remission at 26 weeks. The authors also found significantly lower rates of serious adverse events in those on combination therapy [RR: 0.56; 95% CI: 0.32–0.97]. No controlled trial has addressed whether to continue immunomodulators (IMM) when starting a TNFi after failure of IMM monotherapy. A post hoc subgroup meta-analysis of controlled trials of these types of patients showed no added benefit for the continued use of IMM with TNFi regarding 6 month remission [OR: 1.02; 95% CI: 0.80–1.31], induction of complete response [OR: 1.08; 95% CI: 0.79–1.4] or partial response [OR, 1.25; 95% CI, 0.84–1.88], maintenance therapy [OR: 1.53; 95% CI, 0.67–3.49], or fistula closure [OR: 1.10; 95% CI, 0.68–1.78] [73]. However, TNFi and other biologic agents are intrinsically antigenic, although the non-TNFi’s are less antigenic and combination therapy is most commonly used with the TNFi’s. The development of anti-drug antibodies (ADA) leading to loss of response is an important consideration; in the absence of direct evidence, an individualized approach to combination therapy seems appropriate [73].
The REACT [Early Combined Immunosuppression for the Management of Crohn’s Disease] trial showed that the early use of biologic therapy combined with IMMs as compared with a more conventional stepwise management was associated with significantly lower rates of complications including need for hospitalization, serious disease-related outcomes, or surgery in patients with early CD [63]. Of note, there was no significant difference between the two groups of patients in steroid-free remission, the trial’s primary outcome. The “Enhanced Algorithm for Crohn’s Treatment Incorporating Early Combination Therapy [REACT2]” is currently enrolling with a primary endpoint based on mucosal healing.
The DIAMOND [Deep Remission of Immunomodulator and Adalimumab Combination Therapy for Crohn’s Disease] trial is the only RCT that studied the use of combination therapy of adalimumab with thiopurines versus monotherapy for inducing remission [74]. Combination therapy was not superior for remission [RR: 0.95; 95% CI: 0.78–1.15]. While combination therapy was associated with endoscopic improvement at week 26 [RR: 1.32; 95% CI: 1.06–1.65], this benefit was lost at 1 year. There was no increase in adverse events associated with combination therapy [RR: 1.03; 95% CI: 0.60–1.78], but the dose of AZA used in this trial was lower than what is typically used in CD. Given the ability of immunomodulators to reduce the rate of ADA formation, long-term combination therapy in ADA may very well have a benefit outside of short-term clinical remission or maintenance.
Leukocyte-Trafficking Agents
Leukocyte-trafficking agents , or integrin receptor antagonists, prevent margination of leukocytes by blocking the surface integrins and preventing adhesion to endothelial cells. Natalizumab inhibits the α4 integrin, while vedolizumab blocks the α4β7 heterodimer and is gut selective.
Natalizumab is an infusional drug dosed at 300 mg every 4 weeks and is effective in the treatment of CD [75]. Because this medication is not specific to the GI tract, there is a rare but increased risk of progressive multifocal leukoencephalopathy (PML) resulting from infection with the John Cunningham (JC) virus [76]. This risk is reported to be as high as 1 in 100 who are antibody positive for JC virus, so patients should be surveilled for infection before starting treatment and at every 6 months after. Fear of this dreaded complication, combined with the demonstrated efficacy of novel biologics, has largely led to the abandonment of this medication for CD.
Vedolizumab is also an intravenous medication, with a 300 mg dose at 0, 2, and 6 weeks followed by maintenance every 8 weeks thereafter. The onset of action is quite slow, and initial response is typically seen within 12 weeks of starting the drug [77]. Vedolizumab has historically been used in those patients who have had an inadequate response, lost response, or could not tolerate anti-TNF, corticosteroids or IMM therapy. Failure of other therapies is not a requirement, however, and it can be positioned as first-line agent in patients with active disease. Vedolizumab has been shown to achieve clinical response, clinical remission, and steroid-free remission, and use is supported by the ACG and ECCO guidelines [6, 8, 77,78,79]. Because it is selective to the GI tract, there is no known risk for PML, unlike natalizumab. Patients who have received prior treatment with TNFi agents may require longer treatment to reach efficacy [80]. Those patients appear to have the same efficacy at 10 weeks that TNFi-naïve patients experience at 6 weeks. Prospective clinical trials comparing vedolizumab monotherapy with combination therapy has not been reported.
A recent network meta-analysis suggests that ADA or combination therapy with IFX and AZA is more effective than vedolizumab in inducing and maintaining remission in CD [81].
Interleukin-12 and -23 Antagonist
In 2016, the FDA-approved ustekinumab for use in moderate-to-severe CD. This drug targets the p40 subunit of interleukin-23 and interleukin-12. Induction should be given intravenously usually at 6 mg/kg followed by maintenance dosing of 90 mg subcutaneously every 8 weeks. The onset of action is usually seen within 6 weeks.
Ustekinumab is efficacious in treating patients with moderate-to-severe CD who have failed both conventional non-biologic therapy and TNFi medications but also can be positioned as a first-line agent [82]. Consistent with clinical trials, a large database study of patients undergoing treatment for psoriasis demonstrated an excellent safety profile without a significant increase in infections or malignancies [83]. There have been no trials directly comparing ustekinumab to integrin receptor antagonists or TNFi agents, and the choice of first biologic is at the discretion of the patient and provider. Ustekinumab may be less effective in patients who have failed TNFi therapy [84]. Both the ACG and ECCO guidelines support its use for both induction and maintenance of remission [6, 8].
Biosimilars
Biosimilar medications are highly structurally and clinically similar to an already FDA-approved originator product, and they undergo an accelerated and abbreviated FDA-approval pathway. These mediations should present no differences in efficacy or safety compared to their originator compounds and have the advantage of lower cost. Biosimilars were approved for the treatment of IBD in September 2013 in Europe and in April 2016 in the USA.
Biosimilar TNFi agents are effective treatments for patients with moderate-to-severe CD and can be used for de novo induction and maintenance therapy. The major advantage of biosimilar therapy is cost. Five agents have gained approval for infliximab and adalimumab, with many more expected in coming years:
-
Infliximab-abda
-
Infliximab-dyyb
-
Infliximab-qbtx
-
Adalimumab-atto
-
Adalimumab-adbm
While other generic small-molecule drugs are exact replicas, the same is not true for TNFi biosimilars. Exact replicas cannot be made of biologics because of their structural complexity and complicated manufacturing process. Their amino acid sequences remain the same, but they may differ in their glycosylation patterns. This influences a molecular solubility, stability, clearance, immunogenicity, and immune effector function [6, 55]. At present, there is not sufficient data to support the safety and efficacy of switching patients with stable disease from one biosimilar to another.
A large randomized, non-inferiority phase 3 clinical trial of patients with CD compared IFX to the biosimilar infliximab-dyyb in biologic naïve patients [85]. Patients were randomly assigned to receive infliximab-dyyb then infliximab-dyyb, infliximab-dyyb then IFX, IFX then IFX, or IFX then infliximab-dyyb; the medication switch occurring at week 30. A total of 220 patients were enrolled, and response rates at week 6 were similar for infliximab-dyyb [69.4%, 95% CI 59.9–77.8] and IFX [74.3%, 95% CI 65.1–82.2], establishing non-inferiority. Adverse events were similar in each group. There is still a significant paucity of data around interchangeability, limiting adoption at this time despite cost savings.
Induction and Maintenance of Remission
Principles of Induction Therapy
Mild Disease
Mild disease limited to the terminal ileum may be managed with symptom control and dietary changes or by using budesonide. Mesalamine and antibiotics have not been associated with significant benefit. For mild disease involving the colon, 5-ASA compounds or steroids can be used. Mild disease with upper gastrointestinal involvement should be treated initially with steroids and immunomodulators; for those with clinical features suggestive of a more aggressive phenotype, consideration should be given for early biologic therapy.
Moderate Disease
Moderate ileal disease should be treated with budesonide or steroids. If indicated for complications of local sepsis, antibiotics can also be added. Alternative strategies can include steroids plus an immunomodulator, early biologic therapy, or surgery. The LIR!C trial demonstrated that early laparoscopic resection may be considered a reasonable, cost-effective alternative to upfront infliximab therapy in patients with limited (< 30 cm), inflammatory (non-stricturing/non-penetrating) ileocecal Crohn’s disease [86, 87].
Colonic disease should be treated with steroids or biologic therapy. In the setting of relapse, combination therapy with biologics and an IMM or an IMM with steroids (if relapses are infrequent) may be considered.
Severe Disease
Severe disease of the terminal ileum should be managed with biologic therapy with or without an IMM. Those with infrequent relapse may be treated with an IMM and steroids at the time of disease exacerbation. Early resection should also be considered. Colonic disease may be treated with steroids. Extensive upper gastrointestinal Crohn’s disease should be managed with steroids and IMM. For patients who have relapsed, biologic therapy with or without combination therapy is an option.
Principles of Maintenance Therapy
Target to Treat
Recently, there has been a paradigm shift in the medical management of patients with IBD. Classically, treatment has focused on controlling symptoms with escalation of therapy and a “step-up” approach as the disease progresses or therapies fail. This escalation of therapy appears suboptimal with respect prevention of disease progression. “Target to treat” is a shift toward to a more nuanced strategy, focusing on both control of symptoms and the objective signs of inflammation, that may occur before symptoms or complications develop. Inflammation can be assessed through blood and stool biomarkers such as fecal calprotectin and C-rective protein (CRP), cross-sectional imaging, and endoscopy. Goals of care are built on minimizing disease activity in the early stages of IBD to avoid progressive bowel damage such as fibrostenotic or penetrating disease.
The goals for target to treat are a combination of patient-reported and clinical outcomes as described by the “Selecting Therapeutic Targets in Inflammatory Bowel Disease” [STRIDE] International Organization for the Study of Inflammatory Bowel Diseases. These outcomes are defined as resolution of abdominal pain and diarrhea or altered bowel habit, endoscopic remission defined absent ulceration at endoscopy, or findings of inflammation on magnetic resonance enterography (MRE) or CT-enterography. The patient-reported endpoints should be assessed at a minimum of 3 month intervals during active disease, and the endoscopic endpoints should be assessed at 6–9 month intervals [88]. Other adjunctive measures include histological remission, and biomarker remission defined as a normal CRP and fecal calprotectin; mucosal healing is inversely associated with risk of relapse, surgery, hospitalization, and inability to wean steroids [88,89,90,91,92,93].
The “Effect of Tight Control Management on Crohn’s Disease” [CALM] was a phase 3 multicenter study comparing a “tight control strategy” to symptom-driven care [93]. In the tight control arm, treatment was escalated with a CDAI >150, fecal calprotectin >250, CRP > 5, and prednisone use within the previous week. In the standard care cohort, treatment was escalated if there was not a decrease in the CDAI >70 or 100 (at randomization or post-randomization, respectively), a CDAI >200, or steroid use within the previous week. Tight control was associated with superior endoscopic remission and a lower rate of Crohn’s disease-related hospitalizations when compared to symptom-driven care.
General Principles of Maintenance Therapy
If maintenance was initially achieved with steroids that have been successfully weaned, consideration may be given to no therapy with close observation typically by a 6-month follow-up endoscopic reassessment looking for inflammation. Additionally, isolated disease in the appropriate patient can also be managed by surgical resection followed by a surveillance colonoscopy 6 months post-resection.
IMM monotherapy may also be considered, but oral 5-ASA compounds have not been consistently shown to be effective in maintenance of remission. If induction was achieved with biologic agents, maintenance should be offered. However, combination therapy of biologics and IMM tend to have the best results. Annual endoscopy should be considered for those on biologic agents.
If patients experience a flair while taking a TNFi agent, drug concentrations and ADAs may be checked. Those with low drug level and low levels or absent ADAs may require higher dosing; those with high ADAs typically need to be switched to a different TNFi. Those with normal drug levels and no ADAs typically need to change to a new class of biologics for lack of response.
Therapeutic Drug Monitoring
Therapeutic drug monitoring (TDM) is the measurement of circulating levels of medications and ADA to inform therapy. The role of TDM in the management of transplant recipients has been well established; however, its role in patients with CD is emerging. While there is no definitive evidence to support routine TDM, there are clear theoretical advantages. Goals of care are based on maintaining medical remission while avoiding immunogenicity or loss of response. TDM would seemingly help in these endeavors as the trough concentrations of IMM and biologic therapy can vary. Factors effecting drug levels include disease severity, phenotype, degree of inflammation, combination therapy, patient sex, body mass index, and variability in drug clearance.
TDM can be done reactively following clinical evidence of active disease such as symptoms, endoscopic changes, elevation of CRP or fecal calprotectin, or proactively based on routine measurement done at set timepoints.
Patients usually become refractory to medical therapy for one of three reasons: lack of response, low drug concentrations, or development of ADAs. The AGA has clear guidelines for those on TNFi’s for maintenance therapy in the setting of disease recurrence (Fig. 46.2). Adequate trough levels are defined as ≥5μg/mL for IFX, ≥7.5μg/mL for ADA, and ≥20μg/mL for certolizumab pegol. However, there is no consensus of optimal trough concentrations, and those with perianal disease may require higher concentrations for efficacy:
-
If the drug level is normal, then the dose should be increased or the medication changed
-
If the drug level is absent or low, check ADAs:
-
If ADAs are absent or low assure compliance, then consider:
-
1.
Shorten the dosing interval
-
2.
Increase the dose
-
3.
Combination therapy with an immunomodulator
-
1.
-
If ADAs are high then switch medications
-
High serum trough levels have been shown to be associated with mucosal healing. A retrospective study of 145 patients over 5 years examined mucosal healing and associated this with trough levels of IFX and ADA at the same time points [94]. They found IFX levels >5μg/mL and ADA levels >7.1μg/mL identified patients with mucosal healing with 85% specificity. They also noted that higher levels of IFX and ADA beyond 8μg/mL and 12μg/mL, respectively, conferred no significant additional benefit [7].
A post hoc analysis of ACCENT I [A Crohn’s Disease Clinical Trial Evaluating Infliximab in a New Long-term Treatment Regimen I] evaluated the association between IFX trough concentrations and CRP at 14 weeks after induction treatment [95]. Patients with a durable sustained response had higher post-induction trough levels than patients without sustained response. Similarly, a study of 71 patients on ADA correlated high trough serum concentrations with remission [96].
Three large RCTs have been published on the role of TDM. Trough Concentration Adapted Infliximab [TAXIT] randomized 263 IBD patients on maintenance infliximab to dose adjustment for a target concentration of 3–7μg/mL versus empiric dosing [97]. All patients initially had a starting level of 3–7μg/mL and were dose adjusted if appropriate. The study found that those patients who required an increase in dosing to achieve target trough level had a higher rate of remission and a decrease in CRP. They also identified 67 patients who started at drug level >7μg/mL and were able to be dose reduced. This translated to a 28% reduction in cost. TDM did not affect levels of clinical remission at 1 year, but patients did experience fewer flares.
A more recent double-blind RCT known as “Study Investigating Tailored Treatment with Infliximab for Active Crohn’s Disease” [TAILORIX] included 122 biologic-naïve patients with active disease [98]. All patients underwent induction with combination therapy (immunomodulator plus IFX). At 14 weeks subjects were randomized to three groups: the control arm (dose increase 10 mg/kg based on clinical symptoms alone) or one of two dose intensification strategies based on clinical symptoms, biomarker analysis, and/or serum infliximab concentrations <3μg/mL. The authors found no benefit of TDM over symptom-guided management in achieving corticosteroid-free remission at 1 year. This study, however, was underpowered, and there was a very low threshold for dose escalation in the control arm.
The Pediatric Crohn’s disease Adalimumab-Level-based Optimization Treatment [PAILOT] was a prospective study comparing proactive versus reactive TDM in pediatric patients [99]. The study included 78 biological-naïve children with CD who responded to adalimumab induction therapy and were then randomized to either proactive dose optimization (with a target of 5–10 mg/mL) or reactive testing. They found that clinical improvement was significantly higher in the proactive group versus reactive TDM group.
De-escalation
When contemplating de-escalation of therapy, strong consideration should be given not only to disease control but also to the overall disease characteristics, prior treatment history, tolerance to medications, and risk for adverse events. Some patients who are at lower risk for serious complications related to CD may benefit from de-escalation of medical therapy. This reduces the risk of immunosuppression and drug toxicity and can improve quality of life and provide for cost savings. De-escalation can mean moving from combination therapy to monotherapy or withdrawing medications completely. However, in the setting of subclinical inflammatory changes, de-escalation can increase the risk of flares, use of steroids, and hospitalizations and can lead to irreversible complications and surgery [100]. Patients discontinuing biologic therapy may develop drug resistance by producing ADAs, limiting future therapeutic options.
De-escalation of combination therapy can be considered in those with well-controlled disease with no prior Crohn’s-related resections or significant complications related to their disease course (Fig. 46.3) or after surgical resetting of the clock. Those with upper GI tract CD, repeated penetrating complications, surgeries, or escalated dosing of TNFi’s should not be considered for de-escalation. Once selected, patients have to be confirmed to be in deep remission defined by clinical symptoms, normal biomarkers, endoscopy with normal histology, or normal imaging of the small bowel for those with ileal disease. Surveillance after de-escalation includes clinical monitoring of inflammation every 12 weeks for a year with CRP and fecal calprotectin. Prior to de-escalation from biologics, consideration should be given to obtaining drug levels. If low, this suggests the biologic is probably not the source of remission and de-escalation is more likely to be successful.
If biomarkers start to rise, endoscopy or imaging should confirm recurrence, and other sources like infection should be ruled out. If recurrence of active Crohn’s is confirmed, the previously successful maintenance medication should be restarted. If needed, budesonide or steroids can be provided as a bridge.
Postoperative Prophylaxis
Off medical therapy, the rate of endoscopic disease approaches 90% at 3 years, while clinical recurrence may reach 60% [101]. The goal of postoperative prophylaxis is medical maintenance of remission, as we know 50% of those who undergoing ileocolic resection will require additional surgery within 10 years [102].
After ileocolic resection, all patients should undergo endoscopic surveillance at 6–12 months [103]. Only one RCT has been performed pertaining to the timing of prophylaxis [104]. The study randomized patients to routine AZA starting early at 8 weeks or to endoscopically guided therapy at 6–12 months. This study found no difference in the two groups; however, potential flaws included mismatched cohorts, high attrition, low accrual, and the use of non-biologic therapy.
Many factors have been associated with the risk of postoperative recurrence, and more aggressive initiation of medication is recommended in these patients. Risk factors for early recurrence include younger patients, male gender, tobacco abuse, penetrating or fistulizing disease, prior operative intervention, and short disease duration. A recent meta-analysis demonstrated a significantly increased risk of postoperative recurrence (OR, 1.7; 95% CI, 1.3–2.1; p < 0.001) based on the presence of histopathologically positive margins or presence of plexitis (OR, 2.3; 95% CI, 1.1–4.9; p = 0.02) [105].
Numerous RCTs have examined which agent should be utilized for postoperative prophylaxis. Probiotics, 5-ASA, and budesonide show no benefit over placebo [67, 106,107,108]. Antibiotics may reduce recurrence; but the best evidence to prevent postoperative disease is monotherapy with either biologics or IMM. Early and aggressive prophylaxis is particularly important in patients with risk factors for recurrence. Those patients who are low risk for recurrence (e.g., isolated short segment ileocolic disease present for a long duration in an elderly non-smoker) can be surveilled 6–12 months after surgery off therapy.
Conclusions
The last two decades have seen unprecedented advances in the medical management of CD. All current strategies for therapy focus on symptom management and control of inflammation to prevent or slow bowel damage. As we improve our understanding of the disease, so too does the capacity to provide new, innovative, safer, and more effective therapies. The approach to medical management over the recent years has shifted to more proactive utilization of medications with targeted assessment to verify efficacy prior to the development of complications. The armamentarium of drug options has expanded considerably. However, the efficacy of these medications remains limited, and surgical intervention is still commonly required to manage complications and to improve or restore patient quality of life.
References
Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis; a pathologic and clinical entity. Am J Med. 1952;13:583–90.
Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis: a pathologic and clinical entity. 1932. Mt Sinai J Med. 2000;67:263–8.
Mulder DJ, Noble AJ, Justinich CJ, Duffin JM. A tale of two diseases: the history of inflammatory bowel disease. J Crohns Colitis. 2014;8:341–8.
Ginzburg L. Regional enteritis: historical perspective (B. Crohn and L. Ginzburg). Gastroenterology. 1986;90:1310–1.
Terdiman JP, Gruss CB, Heidelbaugh JJ, Sultan S, Falck-Ytter YT, Practice AGAIC, Quality Management C. American Gastroenterological Association Institute guideline on the use of thiopurines, methotrexate, and anti-TNF-alpha biologic drugs for the induction and maintenance of remission in inflammatory Crohn’s disease. Gastroenterology. 2013;145:1459–63.
Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. ACG clinical guideline: management of Crohn’s disease in adults. Am J Gastroenterol. 2018;113:481–517.
Lichtenstein GR, Loftus EV Jr, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. Correction: ACG clinical guideline: management of Crohn’s disease in adults. Am J Gastroenterol. 2018;113:1101.
Torres J, Bonovas S, Doherty G, Kucharzik T, Gisbert JP, Raine T, Adamina M, Armuzzi A, Bachmann O, Bager P, Biancone L, Bokemeyer B, Bossuyt P, Burisch J, Collins P, El-Hussuna A, Ellul P, Frei-Lanter C, Furfaro F, Gingert C, Gionchetti P, Gomollon F, González-Lorenzo M, Gordon H, Hlavaty T, Juillerat P, Katsanos K, Kopylov U, Krustins E, Lytras T, Maaser C, Magro F, Kenneth Marshall J, Myrelid P, Pellino G, Rosa I, Sabino J, Savarino E, Spinelli A, Stassen L, Uzzan M, Vavricka S, Verstockt B, Warusavitarne J, Zmora O, Fiorino G, European Crohn’s and Colitis Organisation. ECCO guidelines on therapeutics in Crohn’s disease: medical treatment. J Crohns Colitis. 2019;14:4–22.
Gomollon F, Dignass A, Annese V, Tilg H, Van Assche G, Lindsay JO, Peyrin-Biroulet L, Cullen GJ, Daperno M, Kucharzik T, Rieder F, Almer S, Armuzzi A, Harbord M, Langhorst J, Sans M, Chowers Y, Fiorino G, Juillerat P, Mantzaris GJ, Rizzello F, Vavricka S, Gionchetti P, ECCO. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 1: diagnosis and medical management. J Crohns Colitis. 2017;11:3–25.
Uzzan M, Cosnes J, Amiot A, Gornet JM, Seksik P, Cotte E, Tiret E, Panis Y, Treton X. Long-term follow-up after ileorectal anastomosis for ulcerative colitis: a GETAID/GETAID Chirurgie multicenter retrospective cohort of 343 patients. Ann Surg. 2017;266:1029–34.
Khan KJ, Ullman TA, Ford AC, Abreu MT, Abadir A, Marshall JK, Talley NJ, Moayyedi P. Antibiotic therapy in inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol. 2011;106:661–73.
Townsend CM, Parker CE, MacDonald JK, Nguyen TM, Jairath V, Feagan BG, Khanna R. Antibiotics for induction and maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2019;2:CD012730.
Feagins LA, Holubar SD, Kane SV, Spechler SJ. Current strategies in the management of intra-abdominal abscesses in Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9:842–50.
Steinhart AH, Panaccione R, Targownik L, Bressler B, Khanna R, Marshall JK, Afif W, Bernstein CN, Bitton A, Borgaonkar M, Chauhan U, Halloran B, Jones J, Kennedy E, Leontiadis GI, Loftus EV Jr, Meddings J, Moayyedi P, Murthy S, Plamondon S, Rosenfeld G, Schwartz D, Seow CH, Williams C. Clinical practice guideline for the medical management of perianal fistulizing Crohn’s disease: the Toronto consensus. Inflamm Bowel Dis. 2019;25:1–13.
Alves C, Mendes D, Marques FB. Fluoroquinolones and the risk of tendon injury: a systematic review and meta-analysis. Eur J Clin Pharmacol. 2019;75:1431–43.
Butterworth AD, Thomas AG, Akobeng AK. Probiotics for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2008:CD006634.
Jonkers D, Penders J, Masclee A, Pierik M. Probiotics in the management of inflammatory bowel disease: a systematic review of intervention studies in adult patients. Drugs. 2012;72:803–23.
Derwa Y, Gracie DJ, Hamlin PJ, Ford AC. Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease. Aliment Pharmacol Ther. 2017;46:389–400.
Limketkai BN, Iheozor-Ejiofor Z, Gjuladin-Hellon T, Parian A, Matarese LE, Bracewell K, MacDonald JK, Gordon M, Mullin GE. Dietary interventions for induction and maintenance of remission in inflammatory bowel disease. Cochrane Database Syst Rev. 2019;2:CD012839.
Sokol H, Landman C, Seksik P, Berard L, Montil M, Nion-Larmurier I, Bourrier A, Le Gall G, Lalande V, De Rougemont A, Kirchgesner J, Daguenel A, Cachanado M, Rousseau A, Drouet E, Rosenzwajg M, Hagege H, Dray X, Klatzman D, Marteau P, Saint-Antoine IBDN, Beaugerie L, Simon T. Fecal microbiota transplantation to maintain remission in Crohn’s disease: a pilot randomized controlled study. Microbiome. 2020;8:12.
Paramsothy S, Paramsothy R, Rubin DT, Kamm MA, Kaakoush NO, Mitchell HM, Castano-Rodriguez N. Faecal microbiota transplantation for inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis. 2017;11:1180–99.
Imdad A, Nicholson MR, Tanner-Smith EE, Zackular JP, Gomez-Duarte OG, Beaulieu DB, Acra S. Fecal transplantation for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2018;11:CD012774.
Chen T, Zhou Q, Zhang D, Jiang F, Wu J, Zhou JY, Zheng X, Chen YG. Effect of faecal microbiota transplantation for treatment of Clostridium difficile infection in patients with inflammatory bowel disease: a systematic review and meta-analysis of cohort studies. J Crohns Colitis. 2018;12:710–7.
Swaminath A, Feathers A, Ananthakrishnan AN, Falzon L, Li FS. Systematic review with meta-analysis: enteral nutrition therapy for the induction of remission in paediatric Crohn’s disease. Aliment Pharmacol Ther. 2017;46:645–56.
Narula N, Dhillon A, Zhang D, Sherlock ME, Tondeur M, Zachos M. Enteral nutritional therapy for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2018;4:CD000542.
Liska D, Bora Cengiz T, Novello M, Aiello A, Stocchi L, Hull TL, Steele SR, Delaney CP, Holubar SD. Do patients with inflammatory bowel disease benefit from an enhanced recovery pathway? Inflamm Bowel Dis. 2020;26:476–83.
Summers RW, Switz DM, Sessions JT Jr, Becktel JM, Best WR, Kern F Jr, Singleton JW. National Cooperative Crohn’s Disease Study: results of drug treatment. Gastroenterology. 1979;77:847–69.
Malchow H, Ewe K, Brandes JW, Goebell H, Ehms H, Sommer H, Jesdinsky H. European Cooperative Crohn’s Disease Study (ECCDS): results of drug treatment. Gastroenterology. 1984;86:249–66.
Ma C, Dutton SJ, Cipriano LE, Singh S, Parker CE, Nguyen TM, Guizzetti L, Gregor JC, Chande N, Hindryckx P, Feagan BG, Jairath V. Systematic review with meta-analysis: prevalence, risk factors and costs of aminosalicylate use in Crohn’s disease. Aliment Pharmacol Ther. 2018;48:114–26.
Mansfield J, MacDougall L. Editorial: aminosalicylates in Crohn’s disease-prevalence, risks, costs and time to re-assess? Aliment Pharmacol Ther. 2018;48:487–8.
Girardin M, Manz M, Manser C, Biedermann L, Wanner R, Frei P, Safroneeva E, Mottet C, Rogler G, Schoepfer AM. First-line therapies in inflammatory bowel disease. Digestion. 2012;86 Suppl 1:6–10.
O’Donnell S, O’Morain CA. Therapeutic benefits of budesonide in gastroenterology. Ther Adv Chronic Dis. 2010;1(4):177–86.
Nardelli S, Pisani LF, Tontini GE, Vecchi M, Pastorelli L. MMX((R)) technology and its applications in gastrointestinal diseases. Therap Adv Gastroenterol. 2017;10:545–52.
Kuenzig ME, Rezaie A, Kaplan GG, Otley AR, Steinhart AH, Griffiths AM, Benchimol EI, Seow CH. Budesonide for the induction and maintenance of remission in Crohn’s disease: systematic review and meta-analysis for the Cochrane collaboration. J Can Assoc Gastroenterol. 2018;1:159–73.
Lichtenstein GR, Bengtsson B, Hapten-White L, Rutgeerts P. Oral budesonide for maintenance of remission of Crohn’s disease: a pooled safety analysis. Aliment Pharmacol Ther. 2009;29:643–53.
Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955;2:1041–8.
Nicolaides NC, Pavlaki AN, Maria Alexandra MA, Chrousos GP. Glucocorticoid therapy and adrenal suppression. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, Hershman JM, Kaltsas G, Koch C, Kopp P, Korbonits M, McLachlan R, Morley JE, New M, Perreault L, Purnell J, Rebar R, Singer F, Trence DL, Vinik A, Wilson DP, editors. Endotext. South Dartmouth: MDText.com, Inc; 2000.
Ford AC, Bernstein CN, Khan KJ, Abreu MT, Marshall JK, Talley NJ, Moayyedi P. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106:590–9; quiz 600.
Aytac E, Londono JM, Erem HH, Vogel JD, Costedio MM. Impact of stress dose steroids on the outcomes of restorative proctocolectomy in patients with ulcerative colitis. Dis Colon Rectum. 2013;56:1253–8.
Ritter KA, Burke JP, Stocchi L, Aiello A, Holubar S, Ashburn JH, Lipman JM, Shawki S, Hull T. Postoperative steroid taper is associated with pelvic sepsis after ileal pouch-anal anastomosis. Inflamm Bowel Dis. 2019;25:1383–9.
Zaghiyan K, Melmed G, Murrell Z, Fleshner P. Are high-dose perioperative steroids necessary in patients undergoing colorectal surgery treated with steroid therapy within the past 12 months? Am Surg. 2011;77:1295–9.
Zaghiyan K, Melmed G, Murrell Z, Fleshner P. Safety and feasibility of using low-dose perioperative intravenous steroids in inflammatory bowel disease patients undergoing major colorectal surgery: a pilot study. Surgery. 2012;152:158–63.
Chilkoti GT, Singh A, Mohta M, Saxena AK. Perioperative “stress dose” of corticosteroid: pharmacological and clinical perspective. J Anaesthesiol Clin Pharmacol. 2019;35:147–52.
Freudzon L. Perioperative steroid therapy: where’s the evidence? Curr Opin Anaesthesiol. 2018;31:39–42.
Urmson K. Stress dose steroids: the dogma persists. Can J Anaesth. 2020;67:276–7.
Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R, Brown JP, Cohen A, Kim H. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol. 2013;9:30.
Bean RH. The treatment of chronic ulcerative colitis with 6-mercaptopurine. Med J Aust. 1962;49(2):592–3.
Sanderson J, Ansari A, Marinaki T, Duley J. Thiopurine methyltransferase: should it be measured before commencing thiopurine drug therapy? Ann Clin Biochem. 2004;41:294–302.
Chouchana L, Narjoz C, Beaune P, Loriot MA, Roblin X. Review article: the benefits of pharmacogenetics for improving thiopurine therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2012;35:15–36.
Ferraro S, Leonardi L, Convertino I, Blandizzi C, Tuccori M. Is there a risk of lymphoma associated with anti-tumor necrosis factor drugs in patients with inflammatory bowel disease? A systematic review of observational studies. Front Pharmacol. 2019;10:247.
Bourrier A, Carrat F, Colombel JF, Bouvier AM, Abitbol V, Marteau P, Cosnes J, Simon T, Peyrin-Biroulet L, Beaugerie L, CESAME Study Group. Excess risk of urinary tract cancers in patients receiving thiopurines for inflammatory bowel disease: a prospective observational cohort study. Aliment Pharmacol Ther. 2016;43:252–61.
Lopez A, Mounier M, Bouvier AM, Carrat F, Maynadie M, Beaugerie L, Peyrin-Biroulet L, CESAME Study Group. Increased risk of acute myeloid leukemias and myelodysplastic syndromes in patients who received thiopurine treatment for inflammatory bowel disease. Clin Gastroenterol Hepatol. 2014;12:1324–9.
Landerholm K, Kalman D, Wallon C, Myrelid P. Immunomodulators: friends or enemies in surgery for Crohn’s disease? Curr Drug Targets. 2019;20:1384–98.
Hitchings GH Jr. Nobel lecture in physiology or medicine--1988. Selective inhibitors of dihydrofolate reductase. In Vitro Cell Dev Biol. 1989;25:303–10.
Kozarek RA, Patterson DJ, Gelfand MD, Botoman VA, Ball TJ, Wilske KR. Methotrexate induces clinical and histologic remission in patients with refractory inflammatory bowel disease. Ann Intern Med. 1989;110:353–6.
Bedoui Y, Guillot X, Selambarom J, Guiraud P, Giry C, Jaffar-Bandjee MC, Ralandison S, Gasque P. Methotrexate an old drug with new tricks. Int J Mol Sci. 2019;20(20):5023.
Tandon P, Govardhanam V, Leung K, Maxwell C, Huang V. Systematic review with meta-analysis: risk of adverse pregnancy-related outcomes in inflammatory bowel disease. Aliment Pharmacol Ther. 2020;51:320–33.
Restellini S, Biedermann L, Hruz P, Mottet C, Moens A, Ferrante M, Schoepfer AM. Update on the management of inflammatory bowel disease during pregnancy and breastfeeding. Digestion. 2020;101 Suppl 1:27–42.
Mahadevan U, Robinson C, Bernasko N, Boland B, Chambers C, Dubinsky M, Friedman S, Kane S, Manthey J, Sauberan J, Stone J, Jain R. Inflammatory bowel disease in pregnancy clinical care pathway: a report from the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology. 2019;156:1508–24.
Gaidos JKJ, Kane SV. Sexuality, fertility, and pregnancy in Crohn’s disease. Gastroenterol Clin North Am. 2017;46:531–46.
Afzali A, Park CJ, Zhu K, Hu JK, Sharma P, Sinanan MN, Lee SD. Preoperative use of methotrexate and the risk of early postoperative complications in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:1887–95.
Yadav A, Foromera J, Feuerstein I, Falchuk KR, Feuerstein JD. Variations in health insurance policies regarding biologic therapy use in inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:853–7.
Khanna R, Bressler B, Levesque BG, Zou G, Stitt LW, Greenberg GR, Panaccione R, Bitton A, Pare P, Vermeire S, D’Haens G, MacIntosh D, Sandborn WJ, Donner A, Vandervoort MK, Morris JC, Feagan BG, Investigators RS. Early combined immunosuppression for the management of Crohn’s disease (REACT): a cluster randomised controlled trial. Lancet. 2015;386:1825–34.
Stidham RW, Lee TC, Higgins PD, Deshpande AR, Sussman DA, Singal AG, Elmunzer BJ, Saini SD, Vijan S, Waljee AK. Systematic review with network meta-analysis: the efficacy of anti-TNF agents for the treatment of Crohn’s disease. Aliment Pharmacol Ther. 2014;39:1349–62.
Cholapranee A, Hazlewood GS, Kaplan GG, Peyrin-Biroulet L, Ananthakrishnan AN. Systematic review with meta-analysis: comparative efficacy of biologics for induction and maintenance of mucosal healing in Crohn’s disease and ulcerative colitis controlled trials. Aliment Pharmacol Ther. 2017;45:1291–302.
Present DH, Rutgeerts P, Targan S, Hanauer SB, Mayer L, van Hogezand RA, Podolsky DK, Sands BE, Braakman T, DeWoody KL, Schaible TF, van Deventer SJ. Infliximab for the treatment of fistulas in patients with Crohn’s disease. N Engl J Med. 1999;340:1398–405.
Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106:644–59, quiz 60.
Singh S, Heien HC, Sangaralingham LR, Schilz SR, Kappelman MD, Shah ND, Loftus EV Jr. Comparative effectiveness and safety of anti-tumor necrosis factor agents in biologic-naive patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2016;14:1120–9 e6.
Targownik LE, Bernstein CN. Infectious and malignant complications of TNF inhibitor therapy in IBD. Am J Gastroenterol. 2013;108:1835–42, quiz 43.
Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, Lichtiger S, D’Haens G, Diamond RH, Broussard DL, Tang KL, van der Woude CJ, Rutgeerts P, SONIC Study Group. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383–95.
Cheifetz AS. Management of active Crohn disease. JAMA. 2013;309:2150–8.
Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012;380:1590–605.
Jones JL, Kaplan GG, Peyrin-Biroulet L, Baidoo L, Devlin S, Melmed GY, Tanyingoh D, Raffals L, Irving P, Kozuch P, Sparrow M, Velayos F, Bressler B, Cheifetz A, Colombel JF, Siegel CA. Effects of concomitant immunomodulator therapy on efficacy and safety of anti-tumor necrosis factor therapy for Crohn’s disease: a meta-analysis of placebo-controlled trials. Clin Gastroenterol Hepatol. 2015;13:2233–40.e1–2; quiz e177–8.
Matsumoto T, Motoya S, Watanabe K, Hisamatsu T, Nakase H, Yoshimura N, Ishida T, Kato S, Nakagawa T, Esaki M, Nagahori M, Matsui T, Naito Y, Kanai T, Suzuki Y, Nojima M, Watanabe M, Hibi T, DIAMOND Study Group. Adalimumab monotherapy and a combination with azathioprine for Crohn’s disease: a prospective, randomized trial. J Crohns Colitis. 2016;10:1259–66.
Sandborn WJ, Colombel JF, Enns R, Feagan BG, Hanauer SB, Lawrance IC, Panaccione R, Sanders M, Schreiber S, Targan S, van Deventer S, Goldblum R, Despain D, Hogge GS, Rutgeerts P, International Efficacy of natalizumab as Active Crohn’s Therapy Trial Group, Evaluation of Natalizumab as Continuous Therapy Trial Group. Natalizumab induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2005;353:1912–25.
Van Assche G, Van Ranst M, Sciot R, Dubois B, Vermeire S, Noman M, Verbeeck J, Geboes K, Robberecht W, Rutgeerts P. Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn’s disease. N Engl J Med. 2005;353:362–8.
Sandborn WJ, Feagan BG, Rutgeerts P, Hanauer S, Colombel JF, Sands BE, Lukas M, Fedorak RN, Lee S, Bressler B, Fox I, Rosario M, Sankoh S, Xu J, Stephens K, Milch C, Parikh A, Group GS. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013;369:711–21.
Chandar AK, Singh S, Murad MH, Peyrin-Biroulet L, Loftus EV Jr. Efficacy and safety of natalizumab and vedolizumab for the management of Crohn’s disease: a systematic review and meta-analysis. Inflamm Bowel Dis. 2015;21:1695–708.
Lin L, Liu X, Wang D, Zheng C. Efficacy and safety of antiintegrin antibody for inflammatory bowel disease: a systematic review and meta-analysis. Medicine (Baltimore). 2015;94:e556.
Sands BE, Feagan BG, Rutgeerts P, Colombel JF, Sandborn WJ, Sy R, D’Haens G, Ben-Horin S, Xu J, Rosario M, Fox I, Parikh A, Milch C, Hanauer S. Effects of vedolizumab induction therapy for patients with Crohn’s disease in whom tumor necrosis factor antagonist treatment failed. Gastroenterology. 2014;147:618–27.e3.
Hazlewood GS, Rezaie A, Borman M, Panaccione R, Ghosh S, Seow CH, Kuenzig E, Tomlinson G, Siegel CA, Melmed GY, Kaplan GG. Comparative effectiveness of immunosuppressants and biologics for inducing and maintaining remission in Crohn’s disease: a network meta-analysis. Gastroenterology. 2015;148:344–54.e5; quiz e14–5.
Feagan BG, Sandborn WJ, Gasink C, Jacobstein D, Lang Y, Friedman JR, Blank MA, Johanns J, Gao LL, Miao Y, Adedokun OJ, Sands BE, Hanauer SB, Vermeire S, Targan S, Ghosh S, de Villiers WJ, Colombel JF, Tulassay Z, Seidler U, Salzberg BA, Desreumaux P, Lee SD, Loftus EV Jr, Dieleman LA, Katz S, Rutgeerts P, Group U-I-US. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375:1946–60.
Papp K, Gottlieb AB, Naldi L, Pariser D, Ho V, Goyal K, Fakharzadeh S, Chevrier M, Calabro S, Langholff W, Krueger G. Safety surveillance for ustekinumab and other psoriasis treatments from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Drugs Dermatol. 2015;14:706–14.
Sandborn WJ, Gasink C, Gao LL, Blank MA, Johanns J, Guzzo C, Sands BE, Hanauer SB, Targan S, Rutgeerts P, Ghosh S, de Villiers WJ, Panaccione R, Greenberg G, Schreiber S, Lichtiger S, Feagan BG, Group CS. Ustekinumab induction and maintenance therapy in refractory Crohn’s disease. N Engl J Med. 2012;367:1519–28.
Ye BD, Pesegova M, Alexeeva O, Osipenko M, Lahat A, Dorofeyev A, Fishman S, Levchenko O, Cheon JH, Scribano ML, Mateescu RB, Lee KM, Eun CS, Lee SJ, Lee SY, Kim H, Schreiber S, Fowler H, Cheung R, Kim YH. Efficacy and safety of biosimilar CT-P13 compared with originator infliximab in patients with active Crohn’s disease: an international, randomised, double-blind, phase 3 non-inferiority study. Lancet. 2019;393:1699–707.
Ponsioen CY, de Groof EJ, Eshuis EJ, Gardenbroek TJ, PMM B, Hart A, Warusavitarne J, Buskens CJ, van Bodegraven AA, Brink MA, ECJ C, van Wagensveld BA, MCM R, Crolla R, Noomen CG, APJ H, Mallant RC, Boom M, Marsman WA, Stockmann HB, Mol B, de Groof AJ, Stokkers PC, D’Haens GR, Bemelman WA, LIR!C Study Group. Laparoscopic ileocaecal resection versus infliximab for terminal ileitis in Crohn’s disease: a randomised controlled, open-label, multicentre trial. Lancet Gastroenterol Hepatol. 2017;2:785–92.
de Groof EJ, Stevens TW, Eshuis EJ, Gardenbroek TJ, Bosmans JE, van Dongen JM, Mol B, Buskens CJ, Stokkers PCF, Hart A, D’Haens GR, Bemelman WA, Ponsioen CY, LIR!C Study Group. Cost-effectiveness of laparoscopic ileocaecal resection versus infliximab treatment of terminal ileitis in Crohn’s disease: the LIR!C trial. Gut. 2019;68:1774–80.
Peyrin-Biroulet L, Sandborn W, Sands BE, Reinisch W, Bemelman W, Bryant RV, D’Haens G, Dotan I, Dubinsky M, Feagan B, Fiorino G, Gearry R, Krishnareddy S, Lakatos PL, Loftus EV Jr, Marteau P, Munkholm P, Murdoch TB, Ordas I, Panaccione R, Riddell RH, Ruel J, Rubin DT, Samaan M, Siegel CA, Silverberg MS, Stoker J, Schreiber S, Travis S, Van Assche G, Danese S, Panes J, Bouguen G, O’Donnell S, Pariente B, Winer S, Hanauer S, Colombel JF. Selecting therapeutic targets in inflammatory bowel disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015;110:1324–38.
Baert F, Moortgat L, Van Assche G, Caenepeel P, Vergauwe P, De Vos M, Stokkers P, Hommes D, Rutgeerts P, Vermeire S, D’Haens G, Belgian Inflammatory Bowel Disease Research Group, North-Holland Gut Club. Mucosal healing predicts sustained clinical remission in patients with early-stage Crohn’s disease. Gastroenterology. 2010;138:463–8; quiz e10–1.
De Cruz P, Kamm MA, Prideaux L, Allen PB, Moore G. Mucosal healing in Crohn’s disease: a systematic review. Inflamm Bowel Dis. 2013;19:429–44.
Neurath MF, Travis SP. Mucosal healing in inflammatory bowel diseases: a systematic review. Gut. 2012;61:1619–35.
Rutgeerts P, Diamond RH, Bala M, Olson A, Lichtenstein GR, Bao W, Patel K, Wolf DC, Safdi M, Colombel JF, Lashner B, Hanauer SB. Scheduled maintenance treatment with infliximab is superior to episodic treatment for the healing of mucosal ulceration associated with Crohn’s disease. Gastrointest Endosc. 2006;63:433–42; quiz 64.
Schnitzler F, Fidder H, Ferrante M, Noman M, Arijs I, Van Assche G, Hoffman I, Van Steen K, Vermeire S, Rutgeerts P. Mucosal healing predicts long-term outcome of maintenance therapy with infliximab in Crohn’s disease. Inflamm Bowel Dis. 2009;15:1295–301.
Ungar B, Levy I, Yavne Y, Yavzori M, Picard O, Fudim E, Loebstein R, Chowers Y, Eliakim R, Kopylov U, Ben-Horin S. Optimizing anti-TNF-alpha therapy: serum levels of infliximab and adalimumab are associated with mucosal healing in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2016;14:550–7.e2.
Cornillie F, Hanauer SB, Diamond RH, Wang J, Tang KL, Xu Z, Rutgeerts P, Vermeire S. Postinduction serum infliximab trough level and decrease of C-reactive protein level are associated with durable sustained response to infliximab: a retrospective analysis of the ACCENT I trial. Gut. 2014;63:1721–7.
Mazor Y, Almog R, Kopylov U, Ben Hur D, Blatt A, Dahan A, Waterman M, Ben-Horin S, Chowers Y. Adalimumab drug and antibody levels as predictors of clinical and laboratory response in patients with Crohn’s disease. Aliment Pharmacol Ther. 2014;40:620–8.
Vande Casteele N, Ferrante M, Van Assche G, Ballet V, Compernolle G, Van Steen K, Simoens S, Rutgeerts P, Gils A, Vermeire S. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology. 2015;148:1320–9.e3.
D’Haens G, Vermeire S, Lambrecht G, Baert F, Bossuyt P, Pariente B, Buisson A, Bouhnik Y, Filippi J, Vander Woude J, Van Hootegem P, Moreau J, Louis E, Franchimont D, De Vos M, Mana F, Peyrin-Biroulet L, Brixi H, Allez M, Caenepeel P, Aubourg A, Oldenburg B, Pierik M, Gils A, Chevret S, Laharie D, GETAID. Increasing infliximab dose based on symptoms, biomarkers, and serum drug concentrations does not increase clinical, endoscopic, and corticosteroid-free remission in patients with active luminal Crohn’s disease. Gastroenterology. 2018;154:1343–51.e1.
Assa A, Matar M, Turner D, Broide E, Weiss B, Ledder O, Guz-Mark A, Rinawi F, Cohen S, Topf-Olivestone C, Shaoul R, Yerushalmi B, Shamir R. Proactive monitoring of adalimumab trough concentration associated with increased clinical remission in children with Crohn’s disease compared with reactive monitoring. Gastroenterology. 2019;157:985–96.e2.
Torres J, Boyapati RK, Kennedy NA, Louis E, Colombel JF, Satsangi J. Systematic review of effects of withdrawal of immunomodulators or biologic agents from patients with inflammatory bowel disease. Gastroenterology. 2015;149:1716–30.
Olaison G, Smedh K, Sjodahl R. Natural course of Crohn’s disease after ileocolic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut. 1992;33:331–5.
Bernell O, Lapidus A, Hellers G. Risk factors for surgery and recurrence in 907 patients with primary ileocaecal Crohn’s disease. Br J Surg. 2000;87:1697–701.
Nguyen GC, Loftus EV Jr, Hirano I, Falck-Ytter Y, Singh S, Sultan S, Committee AGAICG. American Gastroenterological Association Institute guideline on the management of Crohn’s disease after surgical resection. Gastroenterology. 2017;152:271–5.
Ferrante M, Papamichael K, Duricova D, D’Haens G, Vermeire S, Archavlis E, Rutgeerts P, Bortlik M, Mantzaris G, Van Assche G, International Organization for Study of Inflammatory Bowel Diseases. Systematic versus endoscopy-driven treatment with azathioprine to prevent postoperative ileal Crohn’s disease recurrence. J Crohns Colitis. 2015;9:617–24.
Ryan JM, Rogers AC, O’Toole A, Burke JP. Meta-analysis of histological margin positivity in the prediction of recurrence after Crohn’s resection. Dis Colon Rectum. 2019;62:882–92.
Prantera C, Scribano ML, Falasco G, Andreoli A, Luzi C. Ineffectiveness of probiotics in preventing recurrence after curative resection for Crohn’s disease: a randomised controlled trial with Lactobacillus GG. Gut. 2002;51:405–9.
Ewe K, Bottger T, Buhr HJ, Ecker KW, Otto HF. Low-dose budesonide treatment for prevention of postoperative recurrence of Crohn’s disease: a multicentre randomized placebo-controlled trial. German Budesonide Study Group. Eur J Gastroenterol Hepatol. 1999;11:277–82.
Hellers G, Cortot A, Jewell D, Leijonmarck CE, Lofberg R, Malchow H, Nilsson LG, Pallone F, Pena S, Persson T, Prantera C, Rutgeerts P. Oral budesonide for prevention of postsurgical recurrence in Crohn’s disease. The IOIBD Budesonide Study Group. Gastroenterology. 1999;116:294–300.
Mottet C, Schoepfer AM, Juillerat P, Cosnes J, Froehlich F, Kessler-Brondolo V, Seibold F, Rogler G, Vavricka SR, Michetti P. Experts opinion on the practical use of azathioprine and 6-mercaptopurine in inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(11):2733–47.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Smith, R.K., Holubar, S.D. (2022). Medical Therapy for Crohn’s Disease. In: Steele, S.R., Hull, T.L., Hyman, N., Maykel, J.A., Read, T.E., Whitlow, C.B. (eds) The ASCRS Textbook of Colon and Rectal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-66049-9_46
Download citation
DOI: https://doi.org/10.1007/978-3-030-66049-9_46
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-66048-2
Online ISBN: 978-3-030-66049-9
eBook Packages: MedicineMedicine (R0)