Abstract
With an ever-increasing elderly population, surgeons are faced with a challenging decision in both elective and emergency presentations with biliary disease. Optimizing the surgical approach in an elderly patient will offer the best outcome and the keys to this are assessment of comorbidities and presence or absence of stones in the common bile duct (CBD).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cholecystitis
- Gallbladder scoring system
- Conversion to open cholecystectomy
- Index surgery
- Surgical outcomes
- Elderly patient
1 Introduction
Cholecystitis is one of the most common emergency presentations to hospitals. In general, the incidence of biliary disease is 19% in women and 10% in men [1]. Left untreated, 25% of patients who had biliary colic develop biliary complications within the first year. These include acute cholecystitis, gallstone pancreatitis, and obstructive jaundice.
The prevalence of gallstones increases with age, rising from 20% in those in their 70s to 30% of 90-year olds. In nursing home patients >50% over the age of 80 and 80% over 90 have gallstones [2].
Globally, there is an ever-increasing aging population where those older than 60 will increase from 25 to 35% by 2050, a “silver tsunami” thus making the optimum management of symptomatic biliary disease increasingly important. This is further confounded by the increasing burden of dementia [3].
Many guidelines on the management of acute cholecystitis [4] exist but few deal with the elderly population [5]. The challenge of caring for elderly patients with cholecystitis is balancing the risk of comorbidities against the failure to perform emergency cholecystectomy.
Defining the term “elderly” can be problematic and the concept of the super elderly (>90 years of age) is being increasingly recognized. This chapter will focus on emergency cholecystectomy in the elderly (≥65 years), its indication, and outcomes.
2 Presentation and Triage
In general, elderly patients present with more advanced cholecystitis than younger patients. Right hypochondrium and epigastric pain is the only symptom definitively associated with cholecystitis in this age group [1]. Atypical pain or no pain has been reported in 12% and 5%, respectively [5]. In the elderly, symptoms may be less obvious and cholecystitis may only be identified during imaging, often performed for unexplained sepsis.
While a fever is reported in 50% of patients with cholecystitis, less than 10% will have a temperature of >38 °C. With calculous cholecystitis in the elderly, about 10% will have assorted choledocholithiasis.
In the elderly, cholangitis often presents as Charcot’s Triad and obtaining a clear history of rigors is essential to making the diagnosis. This is despite a suggestion from Rumsey and colleagues that Charcot’s Triad was of little specific clinical value [6]. Many studies evaluating cholangitis have reported fever rather than rigors as a cardinal symptom of Charcot’s Triad. If untreated, cholangitic patients, especially in the elderly, may progress to Reynold’s Pentad, with its associated confusion and hypotension [7, 8]. Morrow suggested there was a delay in diagnosis and surgery in 33% of elderly patients with cholecystitis [9]. A rising trend of CRP or an absolute value of 200 mg/L in elderly patients with right upper quadrant pain suggests fulminant cholecystitis and impending failure of a nonoperative approach.
To facilitate an optimal outcome and timely discharge to home, community, or institutional health care facility, an early diagnosis is important in facilitating a clear management path. The keys to making initial decisions are shown in Table 26.1.
3 What Is the Optimal Management of Acute Cholecystitis in the Elderly; Intervene or Observe?
Having made the diagnosis of cholecystitis, what is optimal care?
Elderly patients who present with cholecystitis tend to show less spontaneous resolution than younger patients, with increased risk of gangrenous cholecystitis, (as shown in US in Fig. 26.1), biliary peritonitis, and complex CBD disease with either stone in the CBD or fistulae. During the index admission, semi-urgent (emergency) laparoscopic cholecystectomy is preferred unless there are contraindications to surgery. Some but not all series in the elderly have shown high failure rates of nonoperative management [9, 10], anesthetic risk and surgical difficulty increase with age, with 50% of >70 years demonstrating frailty. The relative contraindications to proceeding with cholecystectomy are shown in Table 26.2.
Patients with gallstone ileus are not infrequent in the elderly and in general a laparoscopic or laparoscopic-assisted relief of small bowel obstruction is adequate.
Riall, in a US study of almost 30,000 patients, found that 25% of patients did not undergo cholecystectomy during the index admission [11]. Lack of definitive therapy was associated with a 27% subsequent cholecystectomy rate and a 38% gallstone-related readmission rate in the 2 years after discharge.
Failure to perform a cholecystectomy on initial hospitalization was associated with a worse 2-year survival (hazard ratio 1.56, 95% CI 1.47–1.65). However, medical management with an interval cholecystectomy performed only for recurrent acute cholecystitis may be appropriate in selected patients especially where there are no CBD stones [10].
Patients presenting with acute cholecystitis had a 30% higher chance of being readmitted in comparison to those presenting with chronic cholecystitis. Similar findings are described by Giger et al. [12] Also, patients undergoing surgery on a weekend were associated with significantly increased readmission rates. Interestingly, the risk of readmission was reduced by around 15% when intraoperative cholangiogram was implemented, supported by the findings of Halawani et al. [13] following an analysis of the National Surgical Quality Improvement Program Database (NSQIP). Due to the potential seriousness of biliary complications, it begs the question of the current global approach to intraoperative cholangiography and single-stage bile duct clearance. A recent meta-analysis by Pan et al. found performance of intraoperative cholangiography to have superior outcomes in managing choledocholithiasis [14]. McIntyre, in a recent meta-analysis of factors associated with readmission, identified a readmission benchmark of 3.3% accounted for mostly by uncontrolled postoperative pain, nausea and vomiting, and surgical complications, particularly bile duct obstruction. Intraoperative cholangiography may reduce readmission rates [15].
4 Preoperative Preparation
Given the variable conversion rate from laparoscopic to open (ranging from 0 to 65%) [16], formal risk assessment should be done. P Possum, Apache II, and NELA scoring may assist [15, 17].
Predicting the risk of conversion is intuitive, but can be aided by preoperative imaging showing a grossly thickened GB wall or a shriveled gallbladder [18]. In addition, male patients with long-standing symptoms, previous ERCP for CBD stone clearance, previous cholecystostomy, and patients with multiple upper midline laparotomies are more likely to be converted.
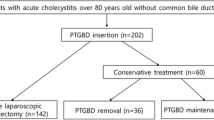
A postoperative high dependency bed should be organized and surgery should be performed on the next available OR list, following some prehabilitation, including a geriatric internal medicine review. Group and crossmatching of blood are generally not necessary. In the elderly, careful multimodality DVT prophylaxis should be used, with dose and risk-adjusted heparin given into the thigh rather than the abdomen. Care should be used in the super elderly with thromboembolic stockings as they may not be appropriate due to the delicate nature of the skin and potential presence of peripheral vascular disease. The operative decision tree is shown in Fig. 26.2.
Recently, the AAST scoring system has been validated and it has been suggested that it is superior to the 2013 Tokyo classification in part due to the greater number of grades of cholecystitis with the AAST classification [19]. The G10 10-point operative scoring system of cholecystitis severity has been validated as a good predictor of the need to convert (Table 26.3). This, or another grading system, should be used to document intraoperative findings [16].
5 Surgical Strategy at Cholecystectomy
The laparoscopic approach for the elderly patient will be similar to that utilized in younger patients, influenced by personal preference but in general, a 4 port approach, three 5 mm ports, and one 11 mm. Other options include; SILS, 3 mm mini ports, or use 3 ports. Certainly, if you are using two 10/11 mm ports with two 5 mm ports you should change your technique. The use of two 10/11 mm ports is not necessary and the GB can be removed through the umbilical port using a camera interchange with a 5 mm telescope. The laparoscopes used should be angled either at 30 or 45 degrees.
There should be a facility to do an operative cholangiogram, so positioning of the patient on the operating room (OR) table is checked before draping. Failure to diagnose and deal with CBD stones will result in increased complications, bile leaks, and recurrent cholangitis.
Obtaining adequate view of the CVS may not be possible and in this situation, there are a number of options (Fig. 26.3). A fundus first approach can be used but may be associated with more hemorrhage and risk of damage to the right hepatic radicles [20]. Rouviere’s sulcus or a line of safety similarly may not be clear, so a subtotal cholecystectomy can be undertaken and Purzner’s recent classification of this is shown in Fig. 26.4 [21, 22]. If a subtotal cholecystectomy is performed on the gallbladder (Fig. 26.5), then every attempt should be made to remove any residual gallstones. If a fenestrating subtotal cholecystectomy is performed, a drain should be placed as bile leaks occur in over 10%. The infundibular approach will increase the injury rate to the CBD.
Purzner’s classification of subtotal cholecystectomy [21] (Source: Toronto Video Atlas of Surgery www.tvasurg.ca) [22]
When performing a subtotal cholecystectomy an intraoperative cholangiogram (IOC) is generally not possible, so if there has not been preoperative visualization of the CBD a postoperative MRI should be considered.
6 Traps During Procedure
The OR ambiance must assist the surgeon, especially when approaching difficult or critical stages of dissection. The commonest traps are shown in Table 26.4. The decision to convert or abort should be proactive rather than reactive to secondary hemorrhage or visceral injury. A great device for a difficult and stuck GB is a laparoscopic peanut. This will facilitate tissue dissection and identification of the window between cystic duct and artery.
Many elderly patients undergo laparoscopic cholecystectomy as an emergency procedure and as such their incidence of CBD stones is >10%. Failure to detect and clear these will result in increased readmission and complications [15]. Preoperative MRI may help but access may be limited. Fluorescent cholangiography, which has some benefit in identifying the extrahepatic bile duct anatomy, does not detect CBD stones [23].
An intraoperative cholangiogram (IOC) is best done with a Reddick Olsen Forceps and a size 4 (or 3 if smaller) ureteric catheter via the cystic duct. There should be no side holes on the ureteric catheter and it should be primed with dilute contrast (Fig. 26.6). Once the control image has been identified, correct positioning of the image intensifier should capture the images in a continuous mode to allow the dilute contrast to outline the stones clearly in the CBD. If a CBD stone is discovered, a single procedure transcystic clearance is optimal. This should be done only if the operator is experienced. The success of a transcystic CBD clearance will be aided, where there is a large cystic duct, by using a “no-tip” Dormia basket and small choledochoscope. A CBD clearance should not be attempted if there is a small CBD, a large single stone, and a small cystic duct or multiple stones (>6) as the procedure is unlikely to be successful and risk damage to the CBD. Intraoperative ERCP will be increasingly used in the elderly as more centers take up its use [24].
7 Closure and Postoperative Care
If the patient has been converted to an open cholecystectomy using a Kocher incision, fascial closure should be done in small bites, utilizing a wound bundle, with antibiotic wash, wound protector, and consideration for onlay prophylactic mesh to reduce dehiscence and incisional hernia [25].
The elderly have less physiological reserve and a higher complication rate. If a drain has been used, especially in a difficult case, it is best left in for 48 h as occasionally bile leaks will not declare themselves until the second postoperative day. Matsui has clearly identified the pivotal importance of CBD stones and their effect of dramatically increasing the cumulative incidence of gallstone-related complications [26].
8 Conclusion
The fine art of decision before incision is particularly required when treating the elderly with cholecystitis. The elderly with cholecystitis are less likely to settle and do not have a great outcome with cholecystostomy. The procedure of choice is same admission cholecystectomy where possible and particular attention should be paid to identify and clear CBD stones if present before or during the index procedure, or with a postoperative ERCP (Fig. 26.7).
Gallstone-related complications in subgroup analysis according to a history of bile duct stones. (Source: Yoichi Matsui World J Surg (2019) 44:721–729) [26]
References
Festi D, Dormi A, Capodicasa S, et al. Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project). World J Gastroenterol. 2008;14:5282.
Ratner J. The prevalence of gallstone disease in very old institutionalized persons. JAMA. 1991;265:902.
Nishida Y, Otagiri N, Yoshifuku S, Misawa K, Ko K, Sasahara K, Kishimoto H, Mishima O, Tauchi K. Dementia in elderly patients undergoing early cholecystectomy for acute cholecystitis: a retrospective observational study. BMC Surg. 2019;19:71. https://doi.org/10.1186/s12893-019-0548-y.
Ansaloni L, Pisano M, Coccolini F, et al. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg. 2016;11:25. https://doi.org/10.1186/s13017-016-0082-5.
Pisano M, Ceresoli M, Cimbanassi S, et al. 2017 WSES and SICG guidelines on acute calcolous cholecystitis in elderly population. World J Emerg Surg. 2019;14:10. https://doi.org/10.1186/s13017-019-0224-7.
Rumsey S, Winders J, MacCormick A. Diagnostic accuracy of Charcot’s triad: a systematic review. ANZ J Surg. 2017;87:232–8.
Sokal A, Sauvanet A, Fantin B, de Lastours V. Acute cholangitis: diagnosis and management. J Visc Surg. 2019;156:515–25.
Reynolds B, Dargan E. Acute obstructive cholangitis: a distinct clinical syndrome. Ann Surg. 1959;150:299–303.
Morrow D. Acute cholecystitis in the elderly. Arch Surg. 1978;113:1149.
McGillicuddy E, Schuster K, Barre K, Suarez L, Hall M, Kaml G, Davis K, Longo W. Non-operative management of acute cholecystitis in the elderly. Br J Surg. 2012;99:1254–61.
Riall T, Zhang D, Townsend C, Kuo Y, Goodwin J. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg. 2010;210:668–77.
Giger U, Michel J, Vonlanthen R, Becker K, Kocher T, Krähenbühl L. Laparoscopic cholecystectomy in acute cholecystitis: indication, technique, risk and outcome. Langenbecks Arch Surg. 2004;390:373–80.
Halawani H, Tamim H, Khalifeh F, Mailhac A, Taher A, Hoballah J, Jamali F. Outcomes of laparoscopic vs open common bile duct exploration: analysis of the NSQIP database. J Am Coll Surg. 2017;224:833–840.e2.
Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, Zhang B, Cai X. The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis. Ann Surg. 2018;268:247–53.
McIntyre C, Johnston A, Foley D, Lawler J, Bucholc M, Flanagan L, Sugrue M. Readmission to hospital following laparoscopic cholecystectomy: a meta-analysis. Anaesthesiol Intensive Ther. 2020;52:47. https://doi.org/10.5114/ait.2020.92967.
Sugrue M, Coccolini F, Bucholc M, Johnston A. Intra-operative gallbladder scoring predicts conversion of laparoscopic to open cholecystectomy: a WSES prospective collaborative study. World J Emerg Surg. 2019;14:12. https://doi.org/10.1186/s13017-019-0230-9.
In: Data.nela.org.uk. https://data.nela.org.uk/riskcalculator/. Accessed 6 Apr 2020.
Sugrue M, Sahebally S, Ansaloni L, Zielinski M. Grading operative findings at laparoscopic cholecystectomy—a new scoring system. World J Emerg Surg. 2015;10:14. https://doi.org/10.1186/s13017-015-0005-x.
Hernandez M, Murphy B, Aho J, Haddad N, Saleem H, Zeb M, Morris D, Jenkins D, Zielinski M. Validation of the AAST EGS acute cholecystitis grade and comparison with the Tokyo guidelines. Surgery. 2018;163:739–46.
van de Graaf F, van den Bos J, Stassen L, Lange J. Lacunar implementation of the critical view of safety technique for laparoscopic cholecystectomy: results of a nationwide survey. Surgery. 2018;164:31–9.
Purzner R, Ho K, Al-Sukhni E, Jayaraman S. Safe laparoscopic subtotal cholecystectomy in the face of severe inflammation in the cystohepatic triangle: a retrospective review and proposed management strategy for the difficult gallbladder. Can J Surg. 2019;62:402–11.
TVASurg difficult choles module—classification system. 2020. Pie.med.utoronto.ca. http://pie.med.utoronto.ca/tvasurg/tvasurg_content/assets/masterFolders/PB_difficultCholecystectomyModule/module/content/classification/index.html. Accessed 10 Aug 2020.
Dip F, LoMenzo E, Sarotto L, et al. Randomized trial of near-infrared Incisionless fluorescent cholangiography. Ann Surg. 2019;270:992–9.
Mohseni S, Ivarsson J, Ahl R, et al. Simultaneous common bile duct clearance and laparoscopic cholecystectomy: experience of a one-stage approach. Eur J Trauma Emerg Surg. 2018;45:337–42.
Sugrue M, Johnston A, Zeeshan S, Loughlin P, Bucholc M, Watson A. The role of prophylactic mesh placement to prevent incisional hernia in laparotomy. Is it time to change practice? Anaesthesiol Intensive Ther. 2019;51:323–9.
Matsui Y, Hirooka S, Sakaguchi T, Kotsuka M, Yamaki S, Yamamoto T, Kosaka H, Satoi S, Sekimoto M. Bile duct stones predict a requirement for cholecystectomy in older patients. World J Surg. 2019;44:721–9. Free Access article distributed under the terms of Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/).
Funding
EU INTERREG funding for Centre for Personalised Medicine.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sugrue, M., Huan, H., Skelly, B., Watson, A. (2021). Emergency Cholecystectomy in the Elderly. In: Latifi, R., Catena, F., Coccolini, F. (eds) Emergency General Surgery in Geriatrics . Hot Topics in Acute Care Surgery and Trauma. Springer, Cham. https://doi.org/10.1007/978-3-030-62215-2_26
Download citation
DOI: https://doi.org/10.1007/978-3-030-62215-2_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-62214-5
Online ISBN: 978-3-030-62215-2
eBook Packages: MedicineMedicine (R0)