Abstract
Mindfulness-based Interventions (MBIs) are increasingly employed in healthcare settings for both healthcare professionals (HCPs) and patients, even though the evidence to support their effectiveness is equivocal. However, there is a general narrative within healthcare that mindfulness has the potential to impact on both well-being and clinical practice. In the following chapter, we first present a more fine-grained analysis of a number of meta-analyses on HCPs samples and explore whether the statistically significant effect sizes may be blinding us to the fact that the evidence base is very limited. We have also conducted a systematic review of meta-analyses of MBI’s among healthcare professionals. This review has three objectives; (1) to examine whether grouping different types of MBIs together is scientifically meaningful, (2) to assess whether there is evidence that they affect objective outcomes, and (3) to find out whether they are appropriate tools for healthcare professionals. The results of this review are outlined.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Mindfulness-based Interventions (MBIs) are increasingly employed in healthcare settings, even though the evidence to support their effectiveness is equivocal. The arguments in favour of mindfulness interventions emphasize that mindfulness, which involves reconnecting and enhancing meaning, has the potential to improve authentic awareness that arises through the paying of purposeful non-judgemental attention to the present moment (Connelly, 1999; Epstein, 1999; Kabat-Zinn & Hanh, 2009). Greater authentic awareness should enhance engagement (reduce feelings of burnout) and improve clinical practice.
The aforementioned seems to be supported by a number of meta-analyses. For example, meta-analyses of MBIs among healthcare professionals (HCPs) have concluded that; cognitive, behavioral, and mindfulness-based approaches are effective in reducing stress in medical students and practicing physicians (Regehr, Glancy, Pitts, & Le Blanc, 2014), MBIs have the potential to significantly ameliorate stress among HCPs (Burton, Burgess, Dean, Zoutsopoulou, & Hugh-Jones, 2017), and mindfulness-based interventions are effective in reducing distress and improving well-being (Spinelli, Wiserner, & Khoury, 2019). However, the aforementioned conclusions fail to present the major caveats of the MBIs research literature. A more fine-grained analysis of these meta-analyses indicates that the statistically significant effect sizes may be blinding us to the fact that the evidence base is very limited. In the following chapter, we conduct a systematic review of meta-analyses of MBI’s among healthcare professionals. Our review has three objectives; (1) to examine whether grouping MBIs together is scientifically meaningful, (2) to assess whether there is evidence that they affect employee wellbeing and clinical practice, and (3) to find out whether they are appropriate tools for healthcare professionals.
2 Systematic Review of the Literature
In this systematic review we searched PubMed, Web of Science, SCOPUS, ERIC, EBSCOhost and Cochrane databases for meta-analyses regarding mindfulness interventions and their impact on HCPs mental health and clinical practice from inception until April 2020. We used a combination of the key words mindfulness, systematic review, meta-analysis, stress, burnout, depression, anxiety, mood, mental-health and resilience to locate studies. In addition, we proceeded with hand searching the reference lists of all the papers included in the final list to identify any further meta-analysis for inclusion. Only studies published in English were included. Unpublished research was not included in this review. Studies were eligible if they included meta-analysis about mindfulness interventions for employees in the healthcare sector either exclusively or as part of wider study of different occupations. The definition of healthcare sector employee was broad and included nurses, physicians, psychologists, health care technicians, managers and other hospital employees. Mindfulness interventions were also broadly defined, thus in this review studies that included any type of mindfulness intervention, long and short term, practiced online, face to face, in the workplace or at home were included. In relation to outcomes we included all potential variables, for example stress, burnout, anxiety, and job engagement.
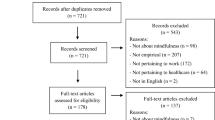
The returned data included 1598 studies (see Fig. 19.1). After removing duplicates, 890 studies remained. The search was conducted in three phases. During the first phase the data that were retrieved from the literature search were subjected to a screening process on the basis of their titles. At the end of this phase we identified and excluded 31 studies which were not reviews, 10 commentaries, 7 papers in languages other than English, 3 protocols, 2 retracted papers, 1 editorial, 1 erratum, 1 poster and 83 studies that were not related to mindfulness. At the second phase we reread the remaining titles and the abstract where necessary and we excluded 31 studies that did not include a mindfulness intervention review, 656 studies that were not about the workplace (most of them referred to mindfulness interventions for patients, students and adults outside of their workplace), 18 studies that did not include health care professionals, 3 studies that did not mention sample characteristics and 31 that did not include a meta-analysis. The first two phases resulted in 12 studies (see Table 19.1). For the third phase we read the full text of the papers. These 12 meta-analyses met the inclusion criteria and were subject to review and quality assessment.
PRISMA 2009 flow diagram. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097. For more information, visit www.prisma-statement.org
3 Findings and Discussion
Overall, the meta-analyses reported statistically significant effect sizes, but with the caveat that there was relatively little evidence of follow-up studies to track the impact over time. The variability as to what actually constitutes a mindfulness intervention and the quality of studies included in the reviews is problematic. In the Regehr et al. (2014) meta-analysis, involving physicians and medical trainees, it is not clear what type of MBIs were employed as the authors report that all of the included studies examined interventions that incorporated components of cognitive-, behavioral-, and/or mindfulness based techniques. Additionally, the authors report that it is not clear if the reviewed MBIs are discernible from standard cognitive behavioural therapy. In the Burton et al. (2017) meta-analysis the MBIs included a wide range of approaches; smart phone mindfulness-based stress reduction applications, mindfulness-based stress reduction, an abbreviated mindfulness course, and mindfulness based cognitive attitude training workshops. Moreover, the authors reported a significant file drawer problem, in that only 44 non-significant studies would be needed to render the findings non-significant. Quality assessment of the papers in the Burton at al review, conducted as part of this review highlighted several methodological limitations, which draw the fidelity of the reported effects of the interventions into question. In the Spinelli et al. (2019) review there was considerable inconsistency in study measures and variations of intervention design, with moderate to high heterogeneity on some study outcomes.
Secondly, 75% of the studies reported that the majority of participants were women. The over-representation of women in MBI interventions has been noted in meta-analysis looking at the general working population (e.g., Heckenberg et al., 2018; Khoury et al., 2015). Additionally, it is likely that all participants represent a narrow range of people in terms of both socio-economic status and cultural variation. There is a broad movement in psychology that has detected biases when the vast majority of research is based on a single population demographic. This problem has been referred to as the bias of psychology research being dominated by WEIRD populations (Western, Educated, Industrialized, Rich, and Democratic), which account for 90% of psychology publications (Henrich, Heine, & Norenzayan, 2010).For example, when psychological studies have been conducted with non-WEIRD populations, researchers have discovered that presumed universal processes such as visual perception, spatial reasoning, and behavioral motivation related to fairness and cooperation have cultural variations (Henrich et al., 2010). Therefore, we are presently running the risk of overlooking the fact that the evidence pertaining to the effectiveness of MBIs is based on a very selective sample.
Thirdly, the majority of studies on mindfulness focus on outcome variables related to self-reported wellbeing. Apart from the problems associated with common method variance, the bigger problem is that research is not linking MBIs with healthcare practice. For example Spinelli et al. (2019) recommend linking MBIs with relevant skills, such as ambiguity tolerance, emotional intelligence, empathy, humility, leadership, resilience and diagnostic accuracy. In their review, physical health, cognitive performance, and clinical skills were not significantly affected by mindfulness training. Wellbeing should be the concern of healthcare organizations, but MBIs will not be taken seriously unless it can be demonstrated that they impact on clinical practice. Additionally, there is some evidence that MBIs benefit approach-coping versus avoidance coping in a sample of medical students, whereby MBIs (for approach coping) enables improved self-awareness and better emotional and behavioural self-regulation (Spinelli et al., 2019).
Fourthly, mindfulness requires significant levels of engagement and commitment. Is this method really the most appropriate for healthcare professionals? The Burton et al. (2017) review reported high attrition rates among studies, and this may simply reflect the fact that in healthcare such interventions are viewed as a burden or additional task. Support for this idea also comes from one of the few studies to explore intervention engagement through interviews and focus groups, reporting that the intervention was found to be enjoyable, but ongoing mindfulness practice outside of the intervention (advised to be between 10–40 min/day) would be difficult for health care professionals to implement and maintain (Foureur, Besley, Burton, Yu, & Crisp, 2013). Congruently, it was difficult to assess the context in which interventions were introduced. For example, it wasn’t clear to which extent have MBIs been introduced as a primary intervention or explicitly for employees with elevated stress levels (as secondary/tertiary intervention). Knowing which contexts are more suitable for MBIs would help to differentiate their ‘worth’.
Congruently, it may be that problems like psychological distress need an organizational solution that focuses on job-person fit rather than an individual approach that uses mindfulness to have a ‘ripple effect’ on quality and safety in a healthcare setting. Contemplative interventions are defined as practices originally rooted in Buddhist traditions and comprise a variety of cognitive-behavioural activities intended to produce sustained alterations in basic cognitive and affective processes, including the regulation of attention, affect, and distress, to support personal insight and well-being (Davidson et al., 2012). Slemp et al. (2019) in a meta-analysis of 119 studies assessing contemplative interventions in the general workforce found that the weakest effects were observed in health care, with regard to the impact of contemplative interventions on general psychological distress (Cohen’s d = 0.21, 0.04, 0.38, k = 18). Encouraging healthcare professionals to be more mindful is desirable and the benefits seem obvious. But we need to be careful as to whether we are really advocating practices that dovetail with the tendency of physicians (in particular) to solve problems individually rather than advocating solutions that prompt people to reflect on team and work practices that challenge quality and safety.
4 Where Do We Go from Here with Mindfulness?
Systematic reviews and meta-analysis are an important step in the hierarchy of evidence, but they become less useful when they communicate mixed messages—such as evidence that MBIs can work but with caveats that significantly undermine the evidence presented. Reading the conclusions of methodologically sound meta-analyses about MBIs can mask the fact that the interventions reviewed can include a varied mix/combination of the following; mindfulness meditation, focused concentration, open awareness, body/internal focus, nature/external focus, yoga, tai chi, and qigong. Therefore, we should acknowledge that there is not yet enough evidence as to the effectiveness of MBIs in healthcare. This does not mean that an organization should not use them, but simply recognize that their use of these approaches entails an evaluation of them in parallel.
The basic idea of mindfulness, to be more aware of our surroundings, should be one that has the potential to improve both quality of care and patient safety. However, attempts to ‘crow-bar’ it into daily practice in a healthcare setting are more likely to increase the work demands of an already exhausted workforce. There has to be the recognition that it is likely to be viewed as either alien or a luxury by healthcare professionals whose daily experiences involve heavy patient loads, work-arounds and little time for self-care (i.e., breaks, food). Randomized controlled trials of MBIs are only useful to the extent that the ‘medicine’ being evaluated is meaningful and applicable. Since the majority of interventions utilize cognitive and movement based aspects, and because there is substantial variation within each of these categories (e.g., mindfulness meditation, focused concentration, open awareness, body/internal focus, nature/external focus, yoga, tai chi, qigong), it may be useful for future studies to identify the beneficial outcomes associated with specific techniques, or the most appropriate target audiences for each technique (Dharmawardene et al., 2016).
Finally, it’s important not to ‘throw the baby out with the bathwater’. For example, approaches such as Mindful Practice (Krasner et al., 2009) which enable clinicians to apply qualities such as attentive observation, critical curiosity, beginner’s mind, and presence to their practice of medicine are more likely to have face validity with healthcare workers. Mindfulness was adopted as a strategy on the basis that it had great potential to ameliorate stress and burnout, but its assimilation into the culture of medicine is dependent on its ability to demonstrate an impact on patient experience, claims reports, rehospitalisation rates and higher levels of psychological safety in among medical teams.
Key messages for researchers |
The evidence concerning the efficacy of mindfulness based interventions among HCPs is limited and based largely on the experience of women participants in western populations There is a significant lack of follow-up studies concerning the impact of mindfulness based interventions The majority of outcomes that have been measured concern self-reported well-being measures, this needs to be supported by studies that demonstrate the impact of mindfulness based interventions on clinical outcomes |
Key messages for healthcare delivery |
The use of piloting prior to the use of mindfulness based interventions, and the use of exit interviews following implementation is strongly advised Mindfulness based interventions need to be assessed for feasibility and acceptability before being employed in healthcare settings Mindfulness based interventions should be part of a comprehensive approach that includes a combination of individual and organizational approaches |
References
Bartlett, L., Martin, A., Neil, A. L., Memish, K., Otahal, P., Kilpatrick, M., et al. (2019). A systematic review and meta-analysis of workplace mindfulness training randomized controlled trials. Journal of Occupational Health Psychology, 24(1), 108–126. https://doi.org/10.1037/ocp0000146
Burton, A., Burgess, C., Dean, S., Zoutsopoulou, G. Z., & Hugh-Jones, S. (2017). How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress & Health, 33, 3–13.
Chiesa, A., & Serretti, A. (2009). Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. The Journal of Alternative and Complementary Medicine, 15(5), 593–600. https://doi.org/10.1089/acm.2008.0495
Connelly, J. (1999). Being in the present moment: developing the capacity for mindfulness in medicine. Academic Medicine, 74, 420–424.
Davidson, R. J., Dunne, J., Eccles, J. S., Engle, A., Greenberg, M., Jennings, P., et al. (2012). Contemplative practices and mental training: Prospects for American education. Child Development Perspectives, 6(2), 146–153.
de Vibe, M., Solhaug, I., Rosenvinge, J. H., Tyssen, R., Hanley, A., & Garland, E. (2018). Six-year positive effects of a mindfulness-based intervention on mindfulness, coping and well-being in medical and psychology students: results from a randomized controlled trial. PLoS One, 13, e0196053.
Dharmawardene, M., Givens, J., Wachholtz, A., Makowski, S., & Tjia, J. (2016). A systematic review and meta-analysis of meditative interventions for informal caregivers and health professionals. BMJ Supportive & Palliative Care, 6(2), 160–169. https://doi.org/10.1136/bmjspcare-2014-000819
Epstein, R. M. (1999). Mindful practice. Journal of the American Medical Association, 282, 833–839.
Kabat-Zinn, J., & Hanh, T. N. (2009). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness (15th ed.). New York: Delta.
Foureur, M., Besley, K., Burton, G., Yu, N., & Crisp, J. (2013). Enhancing the resilience of nurses and midwives: Pilot of a mindfulness based program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemporary Nurse, 45, 114–125. https://doi.org/10.5172/conu.2013.45.1.114
Heckenberg, R. A., Eddy, P., Kent, S., & Wright, B. (2018). Do workplace-based mindfulness meditation programs improve physiological indices of stress? A systematic review and meta-analysis. Journal of Psychosomatic Research, 114, 62–71.
Henrich, J., Heine, S. J., & Norenzayan, A. (2010). Most people are not WEIRD. Nature, 466(7302), 29–29.
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78, 519–528.
Krasner, M., Epstein, R., Beckman, H., Suchman, A., Mooney, C., & Quill, T. (2009). Association of an educational program in mindful communication with burnout, empathy and attitudes among primary care physicians. Journal of the American Medical Association, 302, 1284–1293.
Lomas, T., Medina, J. C., Ivtzan, I., Rupprecht, S., & Eiroa-Orosa, F. J. (2019). Mindfulness-based interventions in the workplace: An inclusive systematic review and meta-analysis of their impact upon wellbeing. The Journal of Positive Psychology, 14(5), 625–640.
Petrie, K., Crawford, J., Baker, S. T. E., Dean, K., Robinson, J., Veness, B. G., et al. (2019). Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta-analysis. The Lancet Psychiatry, 6(3), 225–234. https://doi.org/10.1016/S2215-0366(18)30509-1
Regehr, C., Glancy, D., Pitts, A., & Le Blanc, V. (2014). Interventions to reduce the consequences of stress in physicians: A review and meta-analysis. Journal of Nervous and Mental Disease, 202, 353–359.
Scheepers, R. A., Emke, H., Esptein, R. M., & Lombarts, K. M. J. H. (2019). The impact of mindfulness-based interventions on doctors’ well-being and performance: A systematic review. Medical Education, 54, 138–149.
Slemp, G. R., Jach, H. K., Chia, A., Loton, D., & Kern, M. L. (2019). Contemplative interventions and employee distress: A meta-analysis. Stress & Health, 35, 227–225.
Spinelli, C., Wiserner, M., & Khoury, B. (2019). Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials. Journal of Psychosomatic Research, 120, 29–38.
Virgili, M. (2015). Mindfulness-based interventions reduce psychological distress in working adults: A meta-analysis of intervention studies. Mindfulness, 6, 326. https://doi.org/10.1007/s12671-013-0264-0
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Montgomery, A., Georganta, K., Gilbeth, A., Subramaniam, Y., Morgan, K. (2020). Mindfulness as a Way to Improve Well-Being in Healthcare Professionals: Separating the Wheat from the Chaff. In: Montgomery, A., van der Doef, M., Panagopoulou, E., Leiter, M.P. (eds) Connecting Healthcare Worker Well-Being, Patient Safety and Organisational Change. Aligning Perspectives on Health, Safety and Well-Being. Springer, Cham. https://doi.org/10.1007/978-3-030-60998-6_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-60998-6_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-60997-9
Online ISBN: 978-3-030-60998-6
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)