Abstract
Nurse managers play a critical role in ensuring an appropriate number and mix of staff are available to ensure safe patient care is provided. When leadership decisions are effective, we see improved patient care outcomes, better staff performance, increased job satisfaction and staff retention. However, when decision making is less effective both patients and staff can be negatively impacted. The impact is particularly noticeable for patients who may experience increased adverse events, including greater risk of dying. Making evidence-based staffing decisions can be challenging for nurse managers given the complexity of today’s workplace and importantly, a lack of access to real-time data. Many factors impact on their decisions including nursing shortages; challenges to skills mix (human capital such as experience and qualifications); staff stress, burnout and fatigue; changes to the complexity of patient care needs; an aging workforce and communication inefficiencies. There are many workload measurement tools used internationally, but most are not based on real-time data showing patient acuity, bed occupancy rates and the quality and availability of staffing resources, all factors which are necessary to make cost-effective staffing decisions. Instead, nurse managers are left with many static and disparate reporting systems that do not meet managerial requirements for decision-making. This can result in increased workloads and stress for nurse managers, which also ultimately impact clinical staff. Hospitals need to develop and use software systems which will harness existing data, allowing nurse managers to extract, analyze and interpret data in a timely manner to support appropriate and safe nurse staffing decisions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning Objectives for the Chapter-
1.
Discuss the role of the nurse manager in the deployment and allocation of nursing resources to meet patient care needs.
-
2.
Examine the factors which impact nursing workload and analyze the advantages and disadvantages of current workload measurement tools used.
-
3.
Explain nursing sensitive outcomes and how these are measured in the healthcare system.
-
4.
Describe the complex factors that impact on managerial decision making and nursing workloads.
-
5.
Discuss the implications of staffing a ward with an insufficient number of nurses or poor skill mix.
-
6.
Discuss some of the administrative data which could be useful in nurse staffing decisions.
9.1 Introduction
Over the last decade there have been many changes impacting on nursing work including changes to patient mix and acuity, restructuring of services, bed shortages, cost containment measures and staff shortages (Kutney-Lee et al. 2013; Boudrias et al. 2019). These factors increase complexity in the workplace and are expected to have an impact on the workload of nurses, stress levels and overall job satisfaction. In addition, more sophisticated technologies are now used in health and there are ever-increasing consumer expectations (Duffield et al. 2019a). It has been the responsibility of nurse managers, as part of the administrative team leading the largest workforce in most health facilities, to guide their staff through these changes by maintaining adequate communication (Doleman 2017), appropriate staff allocation and skills mix (human capital), and to offer staff support and guidance as needed. The use of informatics by nursing management has been identified as an important part of the future of nursing, propelling the profession towards health systems transformation. This shift is expected to create a whole of systems approach that focuses on patient safety, use of evidence-based practice, collaboration amongst and between health professionals and improvement of patient health (Remus and Kennedy 2012; Barron McBride 2005). This chapter is focused on the administrative application of informatics in nursing. Current workforce trends, skills mix, workloads, patient outcomes, and current data limitations will be outlined.
9.2 The Nurse Manager Role
Nurse managers play a critical role in the delivery of health care services, by creating positive work environments and ensuring organizational obligations are met (Labrague et al. 2018). While managerial responsibilities may vary slightly across healthcare organizations, the nurse manager has one of the most demanding roles, ensuring standards of care are being met, ensuring successful deployment of a skilled and trained workforce and overseeing patient care (Scott and Timmons 2017). When leadership decision-making is effective, staff performance improves and this has been linked to quality of care, increased job satisfaction (Scott and Timmons 2017), and retention of the workforce. However, when nurse leaders fail or are unable to make appropriate staffing decisions, patient outcomes are negatively affected, reducing patient safety and in some cases, death can result (Department of Health 2010).
In recent times, there has been much debate about using generic non-clinical business managers rather than nurses with knowledge and expertise from both the clinical and management disciplines. There is a view that managing the complexity of the current healthcare environment, including the changes in patient demand, acuity and occupancy as well as unplanned admissions and staffing, and the impact these factors have on staffing decisions, can only be undertaken with knowledge and experience in the clinical setting (Duffield et al. 2019a). However, another view is that nurse managers cannot successfully reconcile the values and skills required of being a manager with those of a clinician, arguing that lay managers are necessary for effective decision-making, particularly where resources are concerned (Stanley 2016).
New Zealand adopted this latter view, introducing non-clinical managers in the 1990s. These managers had a background in business and managed finances, staffing and logistics of hospital wards. However, following implementation of these changes to nurse manager roles, there was an associated increase in adverse patient outcomes, including an increase in urinary tract infections, hospital-acquired pneumonia, deep venous thrombosis and sepsis (Carryer et al. 2010). The authors stated that managers with no nursing background were less likely to identify and understand the often-conflicting demands between hospital policies and patient outcomes. Clinical knowledge arising from having worked at the front line as a clinician was essential for ensuring services were aligned with patients’ care needs.
This view is supported by Duffield and colleagues (Duffield et al. 2019b) who recently identified that nurse managers believe they are engaged in clinically related activities despite not providing direct patient care. Using a self-report tool, they found that clinically focused activities, albeit undertaken in a different manner than a front-line clinical nurse, were not entirely lost from middle management roles. Examples of clinical activities in which nurse managers were involved included interdisciplinary collaboration and facilitating the patients’ journey through the health system, to name two. They concluded that this link to clinical knowledge and skills, as well as managerial expertise, are critical for ensuring safe and effective care is provided (Duffield et al. 2019b). This research supports the findings of the Francis inquiry conducted in the United Kingdom (Francis 2013), which found that when senior managers were more concerned with administrative tasks and meeting targets than addressing patient care issues, there were higher rates of errors in care, higher patient mortality rates and shortages of skilled nurses. Following this Inquiry it was suggested that nurse managers have greater involvement in the supervision of clinical staff and oversight of clinical care to minimize errors and adverse patient events.
Many managers however struggle to achieve this degree of involvement due to increased monitoring and reporting requirements by the organization (Scott and Timmons 2017; Rankin et al. 2016; Smiley et al. 2018). Hewko and colleagues (2015) identified that nurses managers intended to leave their job due to work overload, inability to ensure quality patient care, insufficient resources and a lack of recognition and empowerment. In addition, the rise in administrative demands has resulted in an increase in nurse managers’ stress levels, which has reduced their ability to lead front-line nurses effectively, also making these roles unattractive to the next generation of nurse leaders. Most importantly, nurse managers often have minimal data to be able to proactively match the demand for patients with the appropriate level of nurse staffing (Scott and Timmons 2017), and instead are left with many static and disparate reporting systems that do not meet managerial requirements for decision making (Rosow et al. 2003; Ghazisaeidi et al. 2015). This can result in increased workload and stress for managers and as a consequence, clinical staff.
9.2.1 Nursing Sensitive Outcomes
Over the last two decades a great deal of research has been undertaken in many countries to examine the link between nursing workload, staffing numbers, the mix of staff and the quality of nursing care (Ball et al. 2018; Aiken et al. 2014; Duffield et al. 2011a; Needleman et al. 2011). This work has been facilitated following the development, refinement and adoption of Nursing Sensitive Outcomes (NSOs), a measure of nursing’s contribution to patient safety.
Nursing Sensitive Outcomes are defined as adverse events which are considered sensitive to changes in nurse staffing (Kane et al. 2007a; Needleman et al. 2002). These NSOs include CNS complications, deep vein thrombosis (DVT), pressure injury, Gastro-intestinal (GI) bleeding, pneumonia, sepsis, shock/cardiac arrest, Urinary tract infection (UTI), failure to rescue, mortality, length of stay, physiologic/metabolic derangement, pulmonary failure and surgical wound infection (Needleman et al. 2001). Needleman et al. (2002) developed an algorithm to identify each of these outcomes from the hospital discharge database using coded medical records. Each algorithm specified inclusion and exclusion criteria for the specific adverse outcome so that only those patients who experienced a preventable adverse outcome, rather than one associated with the disease process, were identified. Algorithms were based on variables, such as diagnosis related groups (DRG) and major diagnostic categories (MDC), presence of a surgical procedure and age. They also developed an estimate of nursing care hours needed based on the diagnostic related group (nursing cost-weights).
Research shows that when there are not enough staff there are higher rates of negative outcomes for patients associated with insufficient nursing care being provided (Duffield et al. 2006). In the United States for example, patient death increased by 2% on a shift where a patient was exposed to staffing levels which were eight or more hours below the defined target staffing (Needleman et al. 2011). In seminal work, Aiken and colleagues conducted a study over 168 non-federal adult general hospitals and identified that with an additional patient per nurse, there was an increase of 7% in the rate of mortality within 30 days of admission and a likelihood of failure to rescue (Aiken et al. 2002). Lower levels of staffing are also associated with higher rates of drug administration errors, episodes of care left undone or missed nursing care (Ball et al. 2018; Griffiths et al. 2018).
Perhaps more important than the number of staff is the proportion of hours of care provided by registered nurses, as opposed to unregulated care givers. For example, Needleman and colleagues noted that when there is a higher number of hours of care provided by registered nurses there was a reduction in the rate of failure to rescue (Needleman et al. 2002). Australian work has found that increasing RN hours by 10% decreases the following adverse event rates by:
-
Central nervous system complications 45%
-
GI bleed 37%
-
UTI 34%
-
Failure to rescue 27%
-
Decubitus ulcers 19%
-
Sepsis 15% and
-
Pneumonia 11% (Roche et al. 2012).
These studies highlight the importance of understanding the elements which comprise nursing workload in order to determine an appropriate mix and number of staff to ensure the best outcomes for patients possible.
9.3 Workloads
One of the most important tasks of a first-line nurse manger (the manager at the ward or unit level) is to assign patients to nurses for care. This allocation determines a significant portion, but not all, of a nurse’s workload. Nursing workload is usually described in terms of direct care activities (e.g. bathing, medication administration, patient interaction) and indirect nursing care (e.g. clerical work, interaction with team members), and these activities can be different depending on the specialty, ward area and patient acuity level. However, the nature and breadth of activities that comprise nursing has resulted in difficulties with defining the contribution that nursing makes to patients’ care and more importantly, the measurement of nursing workload. Much of what nurses do is invisible and difficult to quantify and allocate as workload (Lawler 1991). As discussed in Chaps. 2 and 3, now more than ever with shifting models of care delivery, nursing informatics needs to not only facilitate the measurement of nursing workload, but more importantly, make visible and measurable the nursing contribution. For example, it is hard to define and measure empathy and support towards patients and families, but perhaps more importantly, in a time frame that measures effectiveness and completion of the activity or intervention. This is in contrast to the production of goods, in which a set amount of time for task completion can be allocated.
Due to the lack of definition and difficulties in the measurement of workloads, it is currently impossible to determine whether a nurse is working harder than they need to or whether they could be more productive. This is important to note as excessive workloads are a major cause of stress for nurses and a cause of job dissatisfaction (Duffield et al. 2006; Lu et al. 2019), which contribute to a nurse deciding whether to remain in the job and/or the profession (Duffield et al. 2006). Additional negative effects of high workloads include:
-
Increased absenteeism,
-
Increased overtime,
-
Burnout,
-
Work related musculoskeletal disorders (MSD) and
-
An increased rate of injuries (Qureshi et al. 2018).
Research has shown that these negative impacts continue to fuel the turnover intentions of nurses (Lu et al. 2019). Unfortunately, as nurses continue to exit the workforce and workforce shortages persist, there is an increase in workload for those nurses remaining (MSSS and AAA 2015).
Nurses facilitate the provision of safe quality patient care through the use of observational skills, knowledge and understanding of interventions (Sensmeier 2016; Snavely 2016) that allows for early recognition and management of patient deterioration (Dalton et al. 2018) . Factors which increase nursing workload can impact on a nurse’s ability to provide the necessary oversight of patients. There is now a substantial body of research internationally, which demonstrates the strong link between nursing workload and patient mortality and morbidity.
9.4 Workload Measurement Tools
Since the early 1920s, the development of tools to measure nursing workload has been extensively researched. Determining workload is critical as it informs the decisions about allocation of patients to staff. Determining optimal staffing levels is difficult for managers due to limitations in data collection specifically related to staffing levels and the skills mix of nursing teams (National Quality Board 2016; Hurst 2003). Health care organizations across many countries have adopted different methods of managing and assigning nursing workloads. Mandated nurse to patient ratios are used for example in California (USA), and Victoria and Queensland in Australia. The United Kingdom uses a recommended national nurse staffing level; however these are not mandated (National Quality Board 2016; Ball 2010; Health Do 2018). In 2016, Wales introduced a Nurse Staffing Levels Act that recommends the nurse to patient ratio based on decisions of staffing (Welsh Government 2016). Ireland has introduced the Nursing Hours per Patient Day (NHPPD) model based on the Western Australia staffing model (Drennan et al. 2018).
There are many methods used around the world to measure staffing requirements. The most popular methods will be explained in greater detail below.
9.4.1 Patient Assessment and Information System (PAIS)
One of the earliest tools used to determine nursing workload in Australia was the Patient Assessment and Information System (PAIS) . Designed in the United States, this method was introduced into the health system in Victoria (Australia) in the early 1980s. Patients are assessed and classified into one of six groups depending on their level of dependency, that is, their need for nursing care, which in part determines nursing workload. An amount of time is then allocated for each dependency indicator, for example, how independent/dependent the patient is in being able to shower themselves. These numbers are added together to provide a total number of care hours required for each patient. The greater the number of indicators for each patient, the greater the workload and resources (nursing hours) required to care for that patient (Hovenga 1996).
Use of this measurement tool required nurses to enter data following their assessment/reassessment of patients. PAIS was sensitive to patients’ conditions and could be adjusted for each shift and indeed, on an as required basis, which accounted for patient variability and deterioration. This system is no longer in use, in part because there was a belief that nursing staff could ‘play the system’ and inflate patient scores. This resulted in an increase in care hours and as a result, increased staff numbers (Hovenga 1996).
9.4.2 Diagnostic Related Groups (DRG) Nurse Costing Models
Diagnostic Related Groups (DRGs) were developed as a method to determine resource allocation (all resources not just human resources) by categorizing patients based on their diagnosis and characteristics such as age and the presence of other illnesses which might increase resource requirements, for example diabetes (Queensland University of Technology 2001). The argument is that if patients can be categorized into clinically meaningful and homogenous groups, then resource allocation can be determined for each hospital based on the institution’s patient mix (casemix). Developed in the United States, this system is used extensively now throughout the world for example in Canada and in many European countries. In Australia there is agreement that all jurisdictions move to casemix-based activity funding in all hospitals (Heslop 2012).
The DRG classification is determined on discharge but its advantage is that it is derived from administrative data, the patient’s chart, and can be linked to other administrative data sets such as finance and payroll. The nursing resources required for each DRG, defined as nursing service weights, have been incorporated into each DRG (Diers and Bozzo 1997) and these are used to determine the number of nurses needed for a particular ward. However, the resources are determined across the DRG grouping post-discharge and so are not sensitive to an individual patient’s condition or changes to that condition during a shift or day. Nursing care is averaged out for a patient’s entire length of stay, which does not allow for days when these requirements may be greater or lesser than those estimated (Duffield et al. 2006). The nursing service weights have been criticized as underestimating the requirements for nursing care (Heslop 2012), but perhaps a more important criticism is that DRG determinations are derived from medical diagnoses and are not sensitive enough to variations, which can affect nursing care (O’Brien-Pallas et al. 1997).
9.4.3 Nursing Hours of Care per Patient Day (NHpPD)
Collecting data for the number of Nursing Hours per Patient Day (NHpPD) is easily achieved using administrative data sets. It is a simple calculation which divides the number of nursing hours allocated to each ward by the average number of patients on the ward (usually calculated at the midnight census) to determine the average number of hours of care each patient could potentially receive (Twigg and Duffield 2009).
There are several issues with this method. First of all, the basis on which the determination of hours of care patients required is not clear. Secondly, it isn’t really a method for determining workload but rather, a method of allocating paid nursing hours to a certain number of patients. It does not take into account patient complexity or specific care needs or changes to these over a shift or day (Twigg and Duffield 2009; Hodge et al. 2004). Nor does it take into account the ‘indirect’ aspects of nursing care—documentation , education of patients and their families to name just two (Hodge et al. 2004).
The exception to this is the model introduced in Western Australia (WA) in 2002 and currently being implemented in Ireland (Drennan et al. 2018). This method of staffing uses a ‘bottom up’ approach to classify wards into seven categories based on characteristics, such as patient complexity, patient turnover, emergency vs elective admissions and presence of a high dependency unit (Twigg et al. 2011). All wards in WA (emergency departments, ICU and CCU, high dependency and renal units have separate allocations) are then be classified according to these characteristics into one of seven bands of staffing (Department of Health 2019). These then prescribe the NHpPD allocated to the ward ranging from 3.0 (day surgery) to 7.5 h (high complexity, high intervention levels, tertiary pediatrics). Table 9.1 shows the ward categorization and the number of hours of nursing care required to care for patients on each ward in Western Australia and the characteristics which are considered. From this allocation of hours/patient the staffing numbers are determined for each ward. The nurse in charge of the ward can then determine how to allocate those hours of care by shift and day of the week to determine the number of nurses rostered on. Wards can apply to have their classification changed based on changes to the characteristics for example, an increase in emergency rather than elective patients over time (Department of Health 2019).
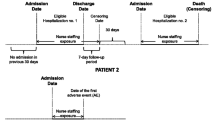
In 2016, the Department of Health in Ireland issued the Framework for Safe Nurse Staffing and Skill Mix in General and Specialist Medical and Surgical Care Settings in Adult Hospitals. Following publication of this document the WA NHpPD model of nurse staffing was introduced to three hospitals as pilot sites to test the impact that planned changes in nurse staffing and skill-mix have on patient, staff and organizational outcomes (Drennan et al. 2018). Administrative data were used to measure the association between the introduction of the staffing recommendations from the Framework and nursing sensitive outcome indicators related to patient care (Needleman et al. 2002). These included
-
mortality,
-
urinary tract infections,
-
pressure ulcers,
-
hospital acquired pneumonia,
-
deep vein thrombosis/pulmonary embolism,
-
upper gastro-intestinal bleeding,
-
central nervous system complications,
-
sepsis and shock/cardiac arrest,
-
wound infection,
-
pulmonary failure,
-
metabolic derangement and
-
length of stay (Needleman et al. 2002).
Cross-sectional data were used to measure staff outcomes including nurses’ perceptions of the working environment, job satisfaction, burnout, and missed care. At an organisational level, data were used to measure levels of staff turnover, absenteeism, agency and bank use by wards, and the extent to which actual and required staffing was in place on a day-to-day basis. The economic costs of implementing the NHpPD model were also examined and these included: the costs of changes to levels of staffing, agency and bank costs and the costs associated with nursing sensitive outcomes. The overall aim of the research was to measure the impact of the introduction of the Framework and to identify the extent to which key patient, staff and organisational outcomes changed as a consequence of the introduction of the NHpPD model of nurse staffing. At the time of writing this work is ongoing in the Emergency Departments.
9.4.4 Nurse to Patient Ratios (Ratios)
This method of determining the number of staff needed per ward/unit has gained wide-spread acceptance internationally, in part because of its simplicity. Wards are allocated staffing on the basis of a ratio, the number of patients nurses are to care for such as 1:3 = 1 nurse to 3 patients. California was the first state in the USA to mandate nurse to patient ratios across their hospitals and many other states and countries have since followed. Two States in Australia, Victoria and Queensland, have adopted this method of staffing. Ratios are established at the unit level and are meant to reflect patient acuity. The more acutely ill patients on the ward are, the fewer patients each nurse would be assigned. The issue with this method of determining staff numbers is that is it hard to determine the optimal ratio for each ward based on patient and staffing characteristics (Duffield et al. 2006).
9.4.5 Commercial Software Packages
There are several software packages which have been developed to plan care and the number of nurses needed. This involves nurses completing a care plan for each patient, which then forms the basis for the determination of their individual care hours. Each nursing activity is added to the system, which then calculates the staffing requirements. Patient acuity is indirectly measured on the basis of clinical hours required for care. However, consideration needs to be taken of patient co-morbidities, skills mix, complications, support staff and other specialty variations. In addition, some packages do not account for time nurses are undertaking indirect nursing duties (Duffield et al. 2006).
In summary, the methods of determining the number of nurses required to provide care for the patients on any given ward, and thus nursing workload, are varied. Some methods are based on the use of administrative data while others rely on nursing staff to provide additional documentation. None of the methods described take account of the mix of staff (registered nurses or unregulated workers) or skills mix (human capital—qualifications and experience of the staff member). While some methods endeavor to take account of the time nurses spend in indirect nursing activities (e.g. patient transfers in the WA NHpPD model) none adequately account for patient variability or patient deterioration, nor are they flexible enough to adjust staffing in the course of a shift or even a day (Duffield et al. 2006).
Probably the most critical skill for nurse managers, particularly first-line nurse managers, is to staff their wards with the appropriate number and mix of staff to ensure patients are safe and receive quality care and their nursing staff are not overworked (Scott and Timmons 2017). To do so requires real-time data to identify bed occupancy levels, patient care needs and resource allocation.
9.5 Challenges for Nurse Managers
Research has identified several complex factors that can impact on managerial decision-making regarding nurse staffing. These factors include nursing shortages, skills mix, stress, burnout and fatigue, changes to patient care needs, an aging workforce, decreased job satisfaction, and poor organizational communication. These areas will be discussed in the following sections.
9.5.1 Nursing Shortages and Workforce Trends
For many years research has documented insufficiencies in the supply and demand of nursing professionals (Marć et al. 2019). These shortages are set to impact countries across all levels of socioeconomic development. The World Health Organization estimates 9 million additional nurses and midwives will be needed by 2030 to ensure sustainability in the workforce. Shortages result from challenges with educational preparation, employment, retention, and workforce performance (World Health Organization 2018). As a consequence of these shortages many researchers and healthcare organizations are now focusing on retention of staff as a priority to ensure patient safety (Sermeus et al. 2011). As indicated earlier, ensuring patients receive safe quality care requires an adequate supply of nurses, particularly registered nurses. An imbalance between supply and demand of these human resources challenges nurse managers. As one of their main functions is to allocate enough nursing resources to meet patient care needs, doing so means they often have to rely on temporary nursing staff or less skilled workers to meet demands (Duffield et al. 2019a). The strain of staff allocation is further exacerbated by lack of real time data showing bed configuration, patient acuity and nursing resource requirements.
Nursing shortages also impact on the economic health of a country by increasing the costs associated with the provision of care (Snavely 2016). These costs are associated with the following:
-
1.
Higher patient re-admission rates (McHugh et al. 2013),
-
2.
Increase in infections including pneumonia, urinary tract infections (Scott 2009), surgical site infections (Cimiotti et al. 2012) and longer length of stay (Kane et al. 2007b), and
-
3.
High turnover of nurses (Snavely 2016).
9.5.2 Skills Mix
Skills mix on a ward or unit can also contribute to the individual nurses’ workload but also impacts on patient outcomes. Skills mix refers to the different levels of qualifications, level of nurse (registered or enrolled), experience levels and expertise of staff (Buchan and Dal Poz 2002). In recent times the healthcare system has seen the increased use of unregulated nursing support workers, also known as unlicensed assistive personnel in the USA, health care assistants in the UK, and assistants in nursing in Australia (Duffield et al. 2014). These roles account for approximately 25% of the health workforce in each of these three countries (Australian Bureau of Statistics 2013; Cavendish 2013; Squillace et al. 2007). Support workers usually undertake a range of activities including bathing, feeding, mobilizing and monitoring of patient vital signs (U.S Bureau of Labour Statistics 2013; National Health Service 2015; Blay and Roche 2020) usually under the direct supervision of an enrolled or registered nurse (Blay and Roche 2020). Support workers can be utilized in one of two ways, either a complementary or substitution model.
The complementary model involves the addition of nursing support workers to ward/unit staffing. This model has been identified as a potential strategy to decrease nursing workloads by increasing hours of care available resulting in increased patient contact, fewer tasks being delayed or not completed, better quality of patient care and improvements in nursing job satisfaction (Duffield et al. 2018). Australian research suggests that effective integration of support workers into ward staffing is associated with a higher rate of task completion for RNs (Roche et al. 2016). However, there is evidence that despite the addition of nursing support workers to the nursing team there is a negative impact on patients’ outcomes. Twigg and colleagues (Twigg et al. 2016) identified that for every 10% of time a patient spent on a ward with nursing support workers added to nurse staffing, there was a 1% increased chance of developing a hospital acquired urinary tract infection and a 2% chance of acquiring pneumonia. Likewise, Aiken and colleagues (2017) identified that increasing the percentage of assistive personnel resulted in an 11% increase in the chance of a preventable death and a decrease in the quality and safety of hospital care.
In contrast to this is the substitution model , whereby registered nurses are replaced with unregulated workers. While this maintains the number of hours of care available, it reduces the hours of care provided by registered nurses, which has been shown to have a negative impact on patient outcomes (Needleman et al. 2002, 2011; Twigg et al. 2011). In addition, some unregulated workers feel powerless in refusing to perform delegated activities, resulting in them undertaking activities outside of their scope of practice that they are not competent or trained to undertake. This may also result in an increase in negative patient outcomes (Blay and Roche 2020).
These negative patient outcomes identified with lower regulated nursing levels include:
-
shock and cardiac arrest,
-
upper gastrointestinal bleeding
-
failure to rescue
Through the substitution model there is also likely to be a greater burden on the remaining regulated nurses in terms of delegation to and supervision of unregulated staff (Butler et al. 2011). Hegney and colleagues (2019) identified that nurses were very dissatisfied with a poor mix of staff, which negatively impacted on their workloads. Nurses indicated they were working with too many inexperienced staff without the necessary skills, thereby increasing their workload.
Unfortunately, as nurses are the largest workforce in most if not all health care facilities, many hospitals and health care organizations try to contain costs by reducing the number of registered nurses or substituting professional nursing staff with less skilled nursing aids, licensed practical nurses and other assistive personal (Needleman 2017). Budgetary constraints can be challenging for nurse managers as they try to provide optimal staffing to meet patient needs, while trying to remain within budget (Hughes et al. 2015). Staffing decisions are made more difficult because of limited access to timely and accurate data showing bed occupancy and resource needs.
9.5.3 Stress, Burnout and Fatigue
Stress, burnout and fatigue have been identified as factors that impact on nurses’ workloads and their turnover intentions, resulting in some nurses leaving after only a few years in the profession (Snavely 2016). An estimated 30–50% of nurses leave their position in nursing or leave the profession altogether after the first three years (MacKusick and Minick 2010). It is estimated that in the twenty-first century a nurse’s career is five years or less with an estimated 2.5 million nurses not practicing (Goodare 2017).
Nurses experience one of the highest levels of occupational stress as a result of high workload demands, emotional strain, long working days, overtime, staff shortages, a lack of support and conflict between healthcare teams (Williams and Smith 2013; Rothmann et al. 2006). In recent years increased stress has also been associated with the advancement in technologies, increasing financial constraints on the health system and changes in workplace environments (Jennings 2007). The National Health Service conducted a review of the health and wellbeing of its staff and identified that one quarter of staff absences were due to stress, depression and anxiety (Fearon and Nicol 2011). This impacts on job satisfaction, productivity and performance and can compromise wellbeing, leading to nurses feeling inadequate and burned out (Najimi et al. 2012). Nurses who show changes in their psychological wellbeing are more inclined to resign from their position and leave the nursing profession (Drury et al. 2014). In addition, high levels of stress among nurses can result in a failure to recognize patient deterioration, leading to negative outcomes for patients including mortality (Stewart and Terry 2014).
Burnout is a psychological concept defined as complete emotional, physical and mental exhaustion caused from continual physical and psychological stress (Okwaraji and En 2014). Symptoms can also include depersonalization and a reduction in perceived accomplishments (Goodare 2017). Nurses are considered to be at high risk of burnout due to unpredictable and stressful working environments resulting from financial and managerial constraints, which impact on nurses’ ability to provide the quality of care they expect to deliver (Macken and Hyrkas 2014; Manzano García and Ayala Calvo 2012). Associated with burnout are the increased financial costs related to absenteeism, lost productivity, staff turnover and poor quality of care resulting in potential adverse events for patients. For example, in 2014 the average cost, in American dollars, of turnover per Full Time Equivalent (FTE) nurse is estimated at $48,790 in Australia, $20,561 in the USA, $26,652 in Canada and $23,71 in New Zealand. Akman and colleagues (2016) identified a direct link between job satisfaction and burnout. When job satisfaction was high burnout was low, and when job satisfaction was low burnout was high. High burnout negatively effects employees and impacts on the quality of care provided to patients (Gosseries et al. 2012). Interestingly, satisfaction with care is also lower in hospitals where nurses are dissatisfied and experience burnout. Research suggests that there is a link between nursing burnout and compassion fatigue (Foureur et al. 2013).
All nurses are at risk of developing compassion fatigue due to prolonged stressful situations and their inability to remove themselves from direct patient care. Compassion fatigue is noticed when a nurse shows declining empathy towards patients related to continual exposure to another’s suffering, both physical and emotional, as well as a lack of support from the workplace (Hegney et al. 2014). Unfortunately, research shows that when one reaches compassion fatigue it is hard to recover as the person is completely drained of all compassionate energy (Jenkins and Warren 2012; Coetzee and Klopper 2010). Compassion fatigue has been identified worldwide as a contributor to nursing shortages (Nolte et al. 2017; Harris and Griffin 2015; World Health Organization 2016). The symptoms of compassion fatigue include;
-
Sadness
-
Depression
-
Anxiety
-
Intrusive images
-
Flashbacks
-
Numbness
-
Avoidance and
-
Poor self-esteem (Hooper et al. 2010).
When nurses feel compassion fatigue the desire to leave the profession increases as does turnover intentions (Coetzee and Klopper 2010; Nolte et al. 2017; Harris and Griffin 2015; Sheppard 2016; Bohnenkamp 2016). Compassion fatigue also impacts patient care and safety resulting in an increase in patient dissatisfaction, and financial strain for the institution resulting from increased costly negative patient outcomes. It has been suggested that if organizations empower their nurses, they may potentially protect them from the development of compassion fatigue (Berger et al. 2015). In addition, workplaces that are supportive, nurturing, caring and compassionate towards staff are seen to combat compassion fatigue (Harris and Griffin 2015). Nurse managers need to consider the risk of stress, burnout and compassion fatigue when scheduling staff and allocating workloads in order to maintain staff health and wellbeing. This can be challenging due to the lack of real-time data available to assist with workload allocation, determination of patient care requirements and the number of nursing staff needed.
9.5.4 Changes to Patient Care Needs
In recent times, a variety of changes in patient characteristics has impacted nursing workload. One of the most significant is aging of the population, noticed in most developed countries. The United Nations reported that the world’s population aged 60 years and older will double over the next 30 years accounting for between 20–30% of the population in some countries (Giacalone et al. 2016; Vespa et al. 2018; McPake and Mahal 2017; Department of Economic and Social Affairs Population Division 2017). Patients above the age of 60 years usually have more than one diagnosis and multiple comorbidities. This increases the complexity of care required and results in greater consumption of resources, that is more nursing hours required to care for the patient (Snavely 2016; Duffield et al. 2015; Anderson 2014). In addition, many diseases that once resulted in death are now treatable, leading to an increased number of people living for many years with a chronic condition, increasing demands for care over time and as a consequence, more staff to meet those needs (Haddad and Toney-Butler 2019).
Patient churn is a factor which can significantly impact workloads at the unit level in hospitals (Duffield et al. 2019a). Patient churn is the excessive movement of patients due to admissions, transfers and discharges (Hughes et al. 2015; Blay et al. 2017). During times of churn a nurse’s workload increases beyond the work demands of direct patient care (Hughes et al. 2015). Blay et al. (2017) found that as a result of poor bed management policies resulting in patient churn, the amount of time needed to move medical-surgical patients between and within wards in one hospital site was equivalent to 11.3 Full-time Equivalent (FTE) nurses. These extra ward requirements are difficult for managers to plan for, as churn is unpredictable, resulting from a fluctuation occurring during a shift (Hughes et al. 2015). In addition, some hospitals still manage patient flow on paper, white boards and via phone calls, which does not allow precise and timely information to match bed availability and human resource requirements (nurses).
A study conducted by Duffield and colleagues (2019a) explored the impact of bed configuration changes on nursing workload. The study identified that there was a noticeable increase across most ward activities following planned changes to patient mix. Specifically, nurses noticed a substantial increase in workloads associated with transfers in and out of the ward, noting lengthy and repetitive contacts with bed management staff and staff on other wards or in different facilities. The addition of temporary staff also meant that many permanent nurses were left performing indirect care for patients that required knowledge of the ward, including discharge, liaison with doctors and communication with families. The ward had mandated nurse-to-patient ratios of 4 patients to 1 nurse. However, nurses stated that this ratio did not reflect the acuity of patients and resulted in some nurses being assigned four very sick patients. Nurses felt that the ward had become a difficult place in which to work. Further, the nurse staffing figures indicated that the planned staffing numbers did not accurately predict the impact of increased patient churn and changes to patient casemix (Duffield et al. 2019a).
Unfortunately, when patients are not discharged in a timely manner the result is system wide congestion. This results in poor quality of care including higher patient mortality rates, higher rates of readmission, greater exposure to error, decreased patient satisfaction, emergency blockage due to a lack of beds, increased length of stay, understaffing or overstaffing and strain on nursing and ancillary staff (Morley et al. 2018). As a consequence nurses increase their focus on improving bed capacity by speeding up discharges thereby increasing their workload, instead of focusing on their primary role of caring for patients (Ward et al. 2010). Interestingly, patients who are discharged early have a higher risk of being readmitted within 72 h of discharge, especially if they are discharged before they have adequately recovered (Anderson et al. 2011).
When workloads are high a nurse may ration care according to patient needs. Care rationing is used when a nurse needs to prioritize care according to resources and their capacity to undertake the work (Kalisch et al. 2009). In times of patient deterioration a nurse will assess, respond and intervene in a timely manner to prevent adverse events (Dalton et al. 2018). Patient deterioration may necessitate one-to-one patient care and at times, more than one nurse per patient, such as in a cardiac arrest. Unfortunately, this can also limit the time a nurse has with other patients allocated to them for the shift, resulting in missed or delayed nursing care (Kalisch et al. 2009; Duffield et al. 2011b). It is hard for nurse managers to anticipate staff workloads and staffing levels in the absence of timely and accurate data and this situation is compounded by ward instability (Duffield et al. 2015), difficult practice environments (Halpin et al. 2017), low staffing levels, inadequate time (Schubert et al. 2008) and violence towards healthcare professionals (Phillips 2016). Any of these factors can result in episodes of missed or delayed patient care, and it is unlikely that any staffing method could take account of these issues. This is where the role of experienced nurse managers becomes critical. Their expertise is essential in making effective staffing decisions, which can have life or death consequences for those in their care.
The ever-increasing expectations of patients and family members about treatment options and care they expect to receive while in hospital is also adding to the workload and stress levels of nurses. More than ever before nurses are being exposed to google doctor, terms like cyberchondriacs and the development of the e-patient. Many nurses have witnessed the increasing emphasis and influence that cyber reality has on healthcare, patients and their families (Holyoake and Searle 2015). There are benefits for patients searching the internet for healthcare related information including increased empowerment, knowledge, support, alleviation of anxiety (Power and Kirwan 2013) and taking more responsibility for their own health and wellbeing (Gee et al. 2012). The use of digital technologies by an older person may also have the added benefit of allowing them to remain in the community longer by supporting their own care needs (Georgsson 2018). However, the negative consequences of cyber reality can include misinformation, loss of professional authority and search anxiety. The loss of professional authority includes reduced confidence by the community in health professionals’ knowledge, and reduced effectiveness of health professionals’ intervention (Holyoake and Searle 2015), which can increase nursing workloads. This can also have a direct impact on patients as they may follow inaccurate and dangerous practices from untrustworthy sources (McMullan 2006), which can result in negative outcomes and even death.
Managers are meant to adjust nursing resources by reviewing shift-by-shift fluctuations in the number of patients but as the midnight census is used, it is difficult to take account of patient flow throughout shifts (Kane et al. 2007b; Unruh and Fottler 2006; Clements et al. 2008). This is critical as research shows that if managers allocate resources effectively the quality of care is improved and the consequences of nurse overload are reduced (Hughes et al. 2015). In contrast to this, when successful deployment of nursing personnel is not achieved, an increase in patient adverse events is noted, including an increase in mortality and morbidity and poor nursing outcomes such as job dissatisfaction, stress and burnout (Aiken et al. 2012, 2013), and increased turnover intentions. The difficulties with successful deployment of resources needs to be noted in terms of the limited data available for managers showing bed occupancy and patient acuity. Timeliness of data availability is also an issue.
9.5.5 Aging Workforce
As the generation of baby boomers is now reaching retirement age (Graham and Duffield 2010), the number of nurses leaving the profession in the next 15–20 years is set to increase (Snavely 2016). This has a direct impact on nursing care and patient outcomes due to the increase in less experienced and skilled nurses within the workforce (Collins-McNeil et al. 2012). Unfortunately, in the twenty-first century the ageing nursing workforce is a problem for most developed countries, as shown below;
-
The average age of nurses in Australia is 44 years of age with 2 in 5 nurses being over 50 (Australian Insitute of Health and Welfare 2016).
-
In the United States the average of nurses is higher, at 51 years of age (Smiley et al. 2018).
-
The labor force survey in the United Kingdom shows that 48.9% of registered nurses are 45 years or older (Royal College of Nursing 2017).
The greatest loss associated with the aging workforce is the loss of clinical expertise and intellectual capital that these nurses possess. These attributes are central to the education of new nurses, improvement in patient outcomes and the identification of improvements needed (Kirgan and Golembeski 2010; Glasper 2011). Unfortunately, as workloads increase this also has an impact on older nurses resulting in increased stress, poor health and injury (Gabrielle et al. 2008). Research suggests that nurse managers need to identify ways to retain older, more experienced and knowledgeable nurses, while trying to recruit younger nurses into the profession (Collins-McNeil et al. 2012; Kirgan and Golembeski 2010; Glasper 2011). One such strategy is for nurse managers to decrease workloads of older nurses to prevent stress and injury (Graham and Duffield 2010). This can be challenging for nurse managers due to the lack of real-time data showing bed occupancy, patient acuity and availability of nursing resources.
9.5.6 Communication
Poor communication within a healthcare organization has also been identified as a source of errors, job dissatisfaction and a contributor to nurse turnover intentions (Doleman 2017). Specifically, nurses have rated communication with supervisors, communication climate and media quality as the factors that most impact on job satisfaction and turnover intentions (Doleman 2017). Poor communication has been implicated in negative patient events leading to death or serious injury in patients. It is also the cause of patient dissatisfaction, lack of continuity of care and ineffective use of resources and worktime, all of which impact on the economics of a healthcare organization (Vermeir et al. 2015). Nurses often feel frustrated with information accessibility, hierarchical filtration, distortion and ease of access, all features of inefficient work environments (Yazici 2002). Agarwal and colleagues (2010) identified that communication inefficiencies cost the U.S healthcare system over $ 12 billion annually with a 500 bed hospital costing on average $4 million per year.
Effective organizational communication is needed for quality and safety for patient care and also, operational effectiveness (Agarwal et al. 2010). Effective communication relies on management’s ability to maintain the communication flow within an organization. Research suggests that by restructuring and improving communication systems, distortion of information will reduce (Doleman 2017; Duffield et al. 2011b), which may also have the benefit of reducing the mean length of stay, maintaining high patient satisfaction levels (Friedman and Berger 2004) and supporting the sustainability of the workforce.
9.6 Implications of Incorrect Staffing
Nurse managers are challenged in their attempts to allocate staff resources successfully by a variety of factors that impact on nursing workloads. They often struggle to make evidence-based decisions due to limited access to critical real-time data at the point of delivery. These limitations can impact on nursing resource allocations, workloads and the optimization of patient outcomes (Hussey et al. 2015).
The current workload models show limited evidence for the reliability of measuring workloads and staffing requirements. Fasoli and colleagues (2011) and Fasoli and Haddock (2010) concluded that many systems are not accurate enough for resource allocation or decision-making. The problem in Australia lies in the limited information collected by government funded agencies about nursing in the hospital and the characteristics of patients that create the demand for nursing resources. In the United States of America, the utilization of patient data for quality assurance has been undertaken since the early 1990s (Rosser and Kleiner 1995). However, the data and the outcomes measured are linked to medical management rather than nursing care. Unfortunately, data available on the patient, nurse, organization and outcomes are not routinely extracted to quantify their effect on costs, patient safety and quality of care (Duffield et al. 2006).
In addition, most workload measurement tools use some degree of professional judgement to measure the demand for nursing care and each makes an underlying assumption about what constitutes adequate safe care or quality staffing (Griffiths et al. 2020). Further, each method provides a basis for nurse staffing, but fails to provide insight into the most appropriate mix of staff, and fails to take into consideration casemix variability (patient mix); all aspects which are required for the provision of adequate and safe care. There are also implications for full time nurses that are often left working hours around those that are part time and casual. This loss of control over practice and work life has been identified internationally as a key issue for nurses and a challenge for nurse managers when making decisions about the allocation of nursing resources (Duffield et al. 2006; Aiken et al. 2001; Duffield and O’Brien-Pallas 2002).
The current method of measuring and allocating nursing resources can also have an impact on the quality of patient care if insufficient or inadequate information is available on which to base decision-making. For example, current workload measures assume that patient volume is static and due to the lack of real time data on patient movement, renders workload associated with patient churn invisible. As a result, shifts that have high patient turnover or churn show an increase in patient mortality related to an increase in nursing workloads (Hughes et al. 2015; Blay et al. 2017). Similar results were identified In the United Kingdom, where a 9% increase in the risk of death in one trust hospital was noted due to inadequate staffing levels (Griffiths et al. 2018). They also identified that the relationship between registered nurse staffing and mortality appeared to be linear with no clear threshold effect, highlighting the difficulties for managers assessing optimal staffing levels to meet patient care needs. Further, in a study conducted in Finland, an increase in negative patient outcomes including mortality was noted when workloads were above optimal levels (Fagerström et al. 2018; Junttila et al. 2016).
In addition, the costs of negative outcomes due to increased hospital stay and additional resource demands need to be considered as the average cost of a patient stay in 2013–2014 in an acute care setting was $1839 per day in Australia (Independent Hosptial Pricing Authority n.d.). These costs increase pressure on the already tight healthcare budget in most countries. Based on data limitations, fragmentation of services, poor coordination of care and a lack of real time information at the point of care continue to impede the provision of quality and safe patient care (Agency Healthcare Research and Quality 2014).
9.7 The Future
Over the years, safety concerns linked to staffing, nurses’ workloads and patient outcomes have been noted, in part due to the lack of real time data available on which nurse managers can make decisions. These limitations in data availability provide a continual challenge for nurse managers in measuring the complex and dynamic workload of nurses. They need access to real-time data on aspects such as bed occupancy, patient acuity and the characteristics and availability of nursing resources (Duffield et al. 2019a).
Unfortunately, the static nature of performance reporting systems is caused by lack of consensus on key measures, lack of consistency in data sources, poor quality of available data and lack of support from IT (Ghazisaeidi et al. 2015). This results in inconsistent and poor-quality reports which are time consuming to develop, but which in many instances, do not allow managers to identify or monitor ward performance, therefore hindering decision-making. As nurse managers are in a critical position responsible for the utilization of information to ensure positive patient outcomes (Hart 2010) and nurse staffing sustainability, they require interactive tools to transmit, organize, analyze and display performance data in real time (Ghazisaeidi et al. 2015). Nurse managers should be able to advocate for appropriate systems, known more commonly as performance dashboards, to be installed (Ghazisaeidi et al. 2015), which will allow them to create an environment that will promote quality patient care (Strudwick et al. 2019a).
A performance dashboard is a layered information system that has the capacity to allow managers to measure, monitor and manage ward performance effectively (Ghazisaeidi et al. 2015). By having these systems in place managers are able to focus on other activities which promote patient safety and the corrective actions needed to improve care provision (Ghazisaeidi et al. 2015; Duffield et al. 2006). The successful implementation of a performance dashboard can support evidence-based nursing care by allowing support for clinical judgement and client values based on proven outcomes (Nursing Informatics Awareness Task Force 2007). In addition, the availability of accurate and timely data will allow nurse managers to successfully allocate nursing resources based on patient care needs. This will allow nurse managers to successfully manage and progress patients through the health facility while facilitating effective clinical leadership of front-line nurses, which drives safe and quality patient care (Wise and Duffield 2019).
A study conducted in Queensland (Australia) provides an example of the administrative data required for the creation of a successful hospital performance dashboard. In the study, administrative data were collected over a two-year period to explore the impact that bed configuration changes and patient mix have on a nurses’ workload. The administrative data collected examined ward activity, acuity indicators, resource intensity and nurse staffing requirements. See Table 9.2 for a summary of some data elements which can be readily accessed from administrative datasets. Results from the study determined that the bed configuration changes resulted in an increase in patient transfers, greater variability in casemix and an increase in nursing workloads. The study concluded that nurse managers should be supported with the necessary skills to access and utilize available administrative data, allowing for expert decisions to be made regarding the complex and often hidden aspects of nursing workloads (Duffield et al. 2019a). By harnessing administrative data, organizations will have the ability to measure and act on key indicators and events in real-time.
In another example also in Queensland, a digital reporting and monitoring dashboard system was implemented into community child health services to inform service improvements, guide strategic planning and support implementation of strategic priorities. This dashboard collected information on service activity, workforce, consumer feedback and socio-demographic data, and was accessible to all child health services and programs. The data allowed for baseline establishment prior to interventions to improve service delivery. Each team accessing the dashboard identified areas of improvements based on information reported in the dashboard. As a result of the implementation of the dashboard child health services were able to make informed decisions about clinical service, utilization of resources and future planning (Kennedy and Tracey 2018). In addition, Rosow et al.’s (2003) seminal work identified the benefits of performance dashboards as
-
Increased performance and reduced costs and time.
-
Process improvement optimizing patient placement,
-
Increasing staff efficiency,
-
Improving bed utilization, occupancy and patient flow,
-
Optimizing utilization of materials,
-
Predicative capacity management which reduced overcrowding, operating delays,
-
Increased staff satisfaction,
-
Better treatment of patients
-
On-demand historical, real-time and predicative reports,
-
Alerts warning and recommendations, ability to share information throughout the hospital
-
Timely data driven decision making regarding staffing levels,
-
Improved crisis management
Collectively these integrated applications directly benefit health care providers, insurers, and most importantly, patients. Improvements in the workflow of service co-ordination is also noted (Hussey et al. 2015) as nurse managers will have real-time data showing patients’ diagnoses, patient acuity, census data, patient rooms, admission dates and estimated discharge and requirement of specialty staff (Punnakitikashem et al. 2013).
9.7.1 Challenges
There are several requirements that must be met before dashboards can be utilized for quality improvement (Weggelaar-Jansen et al. 2018). These include the efficiency and effectiveness of information presented to the user; content needs to align with needs; there must be an ability to customize visualization and display timely and complete data for users; and the system must be capable of inter-connectivity and performance indicator development (Ghazisaeidi et al. 2015; Weggelaar-Jansen et al. 2018). Unfortunately, these issues have been identified in the literature as areas that hospitals and health care facilities fail to manage appropriately.
Regardless of the dashboard system used, the output will only be as good as the data being entered into the system. Support will need to be provided to clinicians to ensure the input of quality data. This also requires managerial and staff commitment as an essential component for successful implementation and use (Taylor et al. 2015). Staff training is also important, as is staff understanding of expected benefits and uses. Research continues to identify that nurse managers are underprepared for their roles, particularly in the use of data (Collins et al. 2017; Westra and Delaney 2008; Strudwick et al. 2019b; Moore et al. 2016). Therefore, educational institutions and employers must strengthen efforts to improve the knowledge and skills of individuals to be able to undertake these roles successfully. The importance of this cannot be underestimated as the need for health practitioners to engage and use technology successfully now and into the future escalates (Hussey et al. 2015).
Importantly, staff will become cynical if there are limited perceived benefits of system implementation. Tools must be tested for reliability in each new setting where implementation occurs (van Oostveen et al. 2016). If this is not undertaken, engagement may be impacted, especially if important aspects of care are omitted because they are deemed to be less important (Brennan and Daly 2015). While the use of dashboards has been developed to unite disparate data sources into meaningful readily available reports, the satisfaction with such deployment has been modest (Kennedy and Tracey 2018; Lachev and Price 2018; Lytvyak et al. 2018). The challenges include incomplete or out of date data, limited system access and usability. These challenges need to be addressed to facilitate successful infiltration of dashboards in the future. Despite the importance for quality patient care and staffing costs there is little available research that pays attention to the impact that these tools and systems can have in facilitating nurse staffing decisions (Griffiths et al. 2020).
9.8 Conclusion
This chapter highlights the challenges faced by nurse managers in terms of measuring nurses’ complex and dynamic workload at the ward level (Duffield et al. 2015; Douglas 2010). Without the use of real time data at the point of care, the mismatch between the supply of nursing resources and patient needs will continue with consequences for patients, staff and the health care system as a whole (Douglas 2010; Tierney et al. 2013). As reported in Chaps. 2 and 14, artificial intelligence (AI) and machine learning (ML) increasingly are being considered useful for decision support in health and social care delivery. Hospitals rarely use the extensive administrative data they collect about patients and staff on each ward to make evidence-based staffing decisions. To harness existing data, software must be employed that allows data to be extracted, analyzed and interpreted for visualization in a timely manner to support staffing decision making (Leary et al. 2016). Evidence-based staffing decisions need to incorporate both comparative and longitudinal trends offered by quantitative administrative data, with the perspective of expert nurses who have the knowledge to contextualize the data and provide a full picture of nursing workload at the ward level.
9.9 Review Questions
-
1.
Can you list some of the challenges that nurse managers face in allocating enough resources to meet patent care requirements and consider how these challenges are overcome in your practice?
-
2.
Can you list some of the nursing sensitive outcomes mentioned in this chapter and consider how they are captured in existing healthcare systems in your practice?
-
3.
Can you recall the different types of workload measurement systems listed in this chapter, select one of them and explain why you consider it to be your preferred choice to implement in practice?
9.9.1 Answers
-
1.
The challenges faced by nurse managers include,
Nursing shortages and workforce trends,
Skills mix.
Stress, burnout and fatigue.
Changes to patient care needs.
Aging workforce.
Communication.
-
2.
Needleman and colleagues (2001) identifies the following Nursing Sensitive Outcomes;
Mortality,
Failure to Rescue (FTR),
Shock/ Cardiac Arrest,
Deep Vein Thrombosis,
Central Nervous System Complications,
Decubitus Ulcer,
Gastrointestinal Bleeding,
Pneumonia,
Sepsis.
Urinary Tract Infection,
Length of Stay,
Physiologic/Metabolic Derangement,
Pulmonary Failure.
Surgical Wound Infection.
-
3.
In this chapter, five workload measurement systems are listed
The patient assessment and information system (PAIS),
The Diagnostic Related Grouping (DRG) Nurse Cost Model,
The Nurse Hours of Care per day,
Nursing to patient ratios and mandated ratios, and
Commercial software packages.
References
Agarwal R, Sands DZ, Díaz Schneider J. Quantifying the economic impact of communication inefficiencies in US hospitals. J Healthc Manag. 2010;55(4):265.
Agency Healthcare Research and Quality. Care coordination measurement atlas. California 2014. Contract No.: 14-0037-EF.
Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, et al. Nurses’ reports on hospital care in five countries. Health Aff. 2001;20(3):43–53.
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. J Am Med Assoc. 2002;288(16):1987–93.
Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. Br Med J. 2012;344:20.
Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Sermeus W, Consortium Rc. Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud. 2013;50(2):143–53.
Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383(9931):1824–30.
Aiken LH, Sloane D, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, et al. Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual Saf. 2017;26(7):559–68.
Akman O, Ozturk C, Bektas M, Ayar D, Armstrong MA. Job satisfaction and burnout among paediatric nurses. J Nurs Manag. 2016;24(7):923–33.
Anderson A. The impact of the Affordable Care Act on the health care workforce, vol. 2887: The Heritage Foundation; 2014. p. 1–20.
Anderson D, Price C, Golden B, Jank W, Wasil E. Examining the discharge practices of surgeons at a large medical center. Health Care Manag Sci. 2011;14(4):338–47.
Australian Bureau of Statistics. April 2013-Doctors and Nurses Canberra, Australia Australian Bureau of Statistics; 2013.
Australian Insitute of Health and Welfare. Nursing and midwifery workforce 2015: Australia Australian Insitute of Health and Welfare; 2016.
Ball J. Guidance on safe nurse staffing levels in the UK: RCN; 2010.
Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, Rafferty AM, et al. Post-operative mortality, missed care and nurse staffing in nine countries: a cross-sectional study. Int J Nurs Stud. 2018;78:10–5.
Barron McBride A. Actually achieving our preferred future. Reflect Nurs Leadersh. 2005;31(4):22–3.
Berger J, Polivka B, Smoot EA, Owens H. Compassion fatigue in pediatric nurses. J Pediatr Nurs. 2015;30(6):e11–e7.
Blay N, Roche M. A systematic review of activities undertaken by the unregulated nursing assistant. J Adv Nurs. 2020;76:1538–51.
Blay N, Roche MA, Duffield C, Gallagher R. Intrahospital transfers and the impact on nursing workload. J Clin Nurs. 2017;26(23–24):4822–9.
Bohnenkamp S. Decreasing moral distress: what do we need to do to keep our nurses at the bedside? Medsurg Nurs. 2016;25(6):378.
Boudrias V, Trépanier S-G, Foucreault A, Peterson C, Fernet C. Investigating the role of psychological need satisfaction as a moderator in the relationship between job demands and turnover intention among nurses. Empl Relat. 2019;
Brennan CW, Daly BJ. Methodological challenges of validating a clinical decision-making tool in the practice environment. West J Nurs Res. 2015;37(4):536–45.
Buchan J, Dal Poz MR. Skill mix in the health care workforce: reviewing the evidence. Bull World Health Organ. 2002;80:575–80.
Butler M, Collins R, Drennan J, Halligan P, O’Mathúna DP, Schultz TJ, et al. Hospital nurse staffing models and patient and staff-related outcomes. Cochrane Database Syst Rev. 2011;(7)
Carryer JB, Diers D, McCloskey B, Wilson D. Effects of health policy reforms on nursing resources and patient outcomes in New Zealand. Policy Polit Nurs Pract. 2010;11(4):275–85.
Cavendish C. The Cavendish review: an independent review into healthcare assistants and support workers in the NHS and social care settings. London: Department of Health; 2013.
Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care–associated infection. Am J Infect Control. 2012;40(6):486–90.
Clements A, Halton K, Graves N, Pettitt A, Morton A, Looke D, et al. Overcrowding and understaffing in modern health-care systems: key determinants in meticillin-resistant Staphylococcus aureus transmission. Lancet Infect Dis. 2008;8(7):427–34.
Coetzee SK, Klopper HC. Compassion fatigue within nursing practice: a concept analysis. Nurs Health Sci. 2010;12(2):235–43.
Collins S, Yen P-Y, Phillips A, Kennedy MK. Nursing informatics competency assessment for the nurse leader: the Delphi study. J Nurs Adm. 2017;47(4):212–8.
Collins-McNeil J, Sharpe D, Benbow D. Aging workforce: retaining valuable nurses. Nurs Manag. 2012;43(3):50–4.
Dalton M, Harrison J, Malin A, Leavey C. Factors that influence nurses’ assessment of patient acuity and response to acute deterioration. Br J Nurs. 2018;27(4):212–8.
Department of Economic and Social Affairs Population Division. World population aging 2017: New York United Nations; 2017.
Department of Health. Equity and excellence: liberating the NHS. London: Department of Health; 2010.
Department of Health. NHpPD application manual: guiding principles Western Australia: Department of Health; 2019.
Diers D, Bozzo J. Nursing resource definition in DRGs. Nurs Econ. 1997;15(3):124–32.
Doleman G. The impact of communication satisfaction on paediatric nurses’ job satisfaction and intention to stay [doctoral dissertation]: Edith Cowan University; 2017.
Douglas K. Ratios – if it were only that easy. Nurs Econ. 2010;28(2):119–26.
Drennan J, Duffield C, Scott AP, Ball J, Brady NM, Murphy A, et al. A protocol to measure the impact of intentional changes to nurse staffing and skill-mix in medical and surgical wards. J Adv Nurs. 2018;74(12):2912–21.
Drury V, Craigie M, Francis K, Aoun S, Hegney DG. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in A ustralia: Phase 2 results. J Nurs Manag. 2014;22(4):519–31.
Duffield C, O’Brien-Pallas L. The nursing workforce in Canada and Australia: two sides of the same coin. Aust Health Rev. 2002;25(2):136–44.
Duffield C, Roche M, Merrick ET. Methods of measuring nursing workload in Australia. Collegian. 2006;13(1):16–22.
Duffield C, Roche MA, Blay N, Thoms D, Stasa H. The consequences of executive turnover in Australian hospitals. J Res Nurs. 2011a;16(6):503–14.
Duffield C, Diers D, O’Brien-Pallas L, Aisbett C, Roche M, King M, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl Nurs Res. 2011b;24(4):244–55.
Duffield CM, Twigg DE, Pugh JD, Evans G, Dimitrelis S, Roche MA. The use of unregulated staff: time for regulation? Policy Polit Nurs Pract. 2014;15(1–2):42–8.
Duffield CM, Roche MA, Dimitrelis S, Homer C, Buchan J. Instability in patient and nurse characteristics, unit complexity and patient and system outcomes. J Adv Nurs. 2015;71(6):1288–98.
Duffield C, Roche M, Twigg D, Williams A, Rowbotham S, Clarke S. Adding unregulated nursing support workers to ward staffing: exploration of a natural experiment. J Clin Nurs. 2018;27(19–20):3768–79.
Duffield C, Roche MA, Wise S, Debono D. Harnessing ward-level administrative data and expert knowledge to improve staffing decisions: a multi-method case study. J Adv Nurs. 2019a;76(1):287–96.
Duffield C, Gardner G, Doubrovsky A, Wise S. Manager, clinician or both? Nurse managers’ engagement in clinical care activities. J Nurs Manag. 2019b;27(7):1538–45.
Fagerström L, Kinnunen M, Saarela J. Nursing workload, patient safety incidents and mortality: an observational study from Finland. BMJ Open. 2018;8(4)
Fasoli DR, Haddock KS. Results of an integrative review of patient classi cation systems. Annu Rev Nurs Res. 2010;28(1):295–316.
Fasoli DR, Fincke BG, Haddock KS. Going beyond patient classification systems to create an evidence-based staffing methodology. J Nurs Adm. 2011;41(10):434–9.
Fearon C, Nicol M. Strategies to assist prevention of burnout in nursing staff. Nurs Stand. 2011;26(14)
Foureur M, Besley K, Burton G, Yu N, Crisp J. Enhancing the resilience of nurses and midwives: Pilot of a mindfulnessbased program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp Nurse. 2013;45(1):114–25.
Francis R. Report of the Mid Staffordshire NHS Foundation Trust public inquiry: executive summary: The Stationery Office; 2013.
Friedman DM, Berger DL. Improving team structure and communication: a key to hospital efficiency. Arch Surg. 2004;139(11):1194–8.
Gabrielle S, Jackson D, Mannix J. Adjusting to personal and organisational change: views and experiences of female nurses aged 40–60 years. Collegian. 2008;15(3):85–91.
Gee PM, Greenwood DA, Kim KK, Perez SL, Staggers N, DeVon HA. Exploration of the e-patient phenomenon in nursing informatics. Nurs Outlook. 2012;60(4):e9–e16.
Georgsson M. An aging population, larger chronic disease burden, and reliance on digital self-management tools require contributions from nurse informaticians. Online J Nurs Inform. 2018;22:3.
Ghazisaeidi M, Safdari R, Torabi M, Mirzaee M, Farzi J, Goodini A. Development of performance dashboards in healthcare sector: key practical issues. Acta Informatica Medica. 2015;23(5):317.
Giacalone D, Wendin K, Kremer S, Frøst MB, Bredie WL, Olsson V, et al. Health and quality of life in an aging population – food and beyond. Food Qual Prefer. 2016;47:166–70.
Glasper A. Can older nurses still provide care? Br J Nurs. 2011;20(18):1206–7.
Goodare P. Literature review: why do we continue to lose our nurses? Aust J Adv Nurs. 2017;34(4):50.
Gosseries O, Demertzi A, Ledoux D, Bruno M-A, Vanhaudenhuyse A, Thibaut A, et al. Burnout in healthcare workers managing chronic patients with disorders of consciousness. Brain Inj. 2012;26(12):1493–9.
Graham EM, Duffield C. An ageing nursing workforce. Aust Health Rev. 2010;34(1):44–8.
Griffiths P, Ball J, Bloor K, Böhning D, Briggs J, Dall’Ora C, et al. Nurse staffing levels, missed vital signs observations and mortality in hospital wards: retrospective longitudinal observational study. NIHR Journals Library. 2018;
Griffiths P, Saville C, Ball J, Jones J, Pattison N, Monks T, et al. Nursing workload, nurse staffing methodologies and tools: a systematic scoping review and discussion. Int J Nurs Stud. 2020;103:103487.
Haddad LM, Toney-Butler TJ. Nursing shortage. StatPearls [Internet]: StatPearls Publishing; 2019.
Halpin Y, Terry LM, Curzio J. A longitudinal, mixed methods investigation of newly qualified nurses’ workplace stressors and stress experiences during transition. J Adv Nurs. 2017;73(11):2577–86.
Harris C, Griffin MTQ. Nursing on empty: compassion fatigue signs, symptoms, and system interventions. J Christ Nurs. 2015;32(2):80–7.
Hart MD. A Delphi study to determine baseline informatics competencies for nurse managers. CIN: Computers, Informatics, Nursing. 2010;28(6):364–70.
Health Do. Framework for safe nurse staffing and skill mix in general and specialist medical and surgical care settings in Ireland 2018: London Department of Health; 2018.
Hegney DG, Craigie M, Hemsworth D, Osseiran-Moisson R, Aoun S, Francis K, et al. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: study 1 results. J Nurs Manag. 2014;22(4):506–18.
Hegney DG, Rees CS, Osseiran-Moisson R, Breen L, Eley R, Windsor C, et al. Perceptions of nursing workloads and contributing factors, and their impact on implicit care rationing: a Queensland, Australia study. J Nurs Manag. 2019;27(2):371–80.
Heslop L. Status of costing hospital nursing work within Australian casemix activity-based funding policy. Int J Nurs Pract. 2012;18(1):2–6.
Hewko SJ, Brown P, Fraser KD, Wong CA, Cummings GG. Factors influencing nurse managers’ intent to stay or leave: a quantitative analysis. J Nurs Manag. 2015;23(8):1058–66.
Hodge MB, Romano PS, Harvey D, Samuels SJ, Olson VA, Sauvé MJ, et al. Licensed caregiver characteristics and staffing in California acute care hospital units. J Nurs Adm. 2004;34(3):125–33.
Holyoake D-D, Searle K. Cyberchondria: emerging themes for children’s nurses in the Internet age. Nurs Child Young People. 2015;27(5):34.
Hooper C, Craig J, Janvrin DR, Wetsel MA, Reimels E. Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. J Emerg Nurs. 2010;36(5):420–7.
Hovenga E. Patient Assessment and Information System (PAIS). 1996.
Hughes RG, Bobay KL, Jolly NA, Suby C. Comparison of nurse staffing based on changes in unit-level workload associated with patient churn. J Nurs Manag. 2015;23(3):390–400.
Hurst K. Selecting and applying methods for estimating the size and mix of nursing teams: a systematic review of the literature commissioned by the Department of Health: Nuffield Institute for Health; 2003.
Hussey P, Adams E, Shaffer FA. Nursing informatics and leadership, an essential competency for a global priority: eHealth. Nurse Lead. 2015;13(5):52–7.
Independent Hosptial Pricing Authority. National hosptial cost data collection: Australian public hospitals cost report 2013–2014 Round 18. Australia: Independent Hosptial Pricing Authority; n.d.
Jenkins B, Warren NA. Concept analysis: compassion fatigue and effects upon critical care nurses. Crit Care Nurs Q. 2012;35(4):388–95.
Jennings BM. Turbulance. Hughes R, ed. Rockville, MD: Agency for Helathcare Research and Quality; 2007.
Junttila JK, Koivu A, Fagerström L, Haatainen K, Nykänen P. Hospital mortality and optimality of nursing workload: a study on the predictive validity of the RAFAELA Nursing Intensity and Staffing system. Int J Nurs Stud. 2016;60:46–53.
Kalisch BJ, Landstrom GL, Hinshaw AS. Missed nursing care: a concept analysis. J Adv Nurs. 2009;65(7):1509–17.
Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007a:1195–204.
Kane RL, Shamliyan T, Mueller C, Duval S, Wilt TJ. Nurse staffing and quality of patient care. Evid Rep Technol Assess (Full Rep). 2007b;151(1):115.
Kennedy C, Tracey F. An integrated approach to sustainability and delivery of improved health outcomes for Children’s Health Queensland community based services and programs. Int J Integr Care (IJIC). 2018;18
Kirgan M, Golembeski S. Retaining an aging workforce by giving voice to older and experienced nurses. Nurse Lead. 2010;8(1):34–6.
Kutney-Lee A, Wu ES, Sloane DM, Aiken LH. Changes in hospital nurse work environments and nurse job outcomes: an analysis of panel data. Int J Nurs Stud. 2013;50(2):195–201.
Labrague LJ, McEnroe-Petitte DM, Leocadio MC, Van Bogaert P, Cummings GG. Stress and ways of coping among nurse managers: an integrative review. J Clin Nurs. 2018;27(7–8):1346–59.
Lachev T, Price E. Applied Microsoft Power BI: bring your data to life! Prologika Press; 2018.
Lawler J. Behind the screens: Nursing, somology, and the problem of the body. Melbourne: Churchill Livingstone; 1991.
Leary A, Cook R, Jones S, Smith J, Gough M, Maxwell E, et al. Mining routinely collected acute data to reveal non-linear relationships between nurse staffing levels and outcomes. BMJ Open. 2016;6(12):e011177.
Lu H, Zhao Y, While A. Job satisfaction among hospital nurses: a literature review. Int J Nurs Stud. 2019;94:24–31.
Lytvyak E, Dieleman L, Halloran B, Huang V, Kroeker K, Peerani F, et al. A130 tableau dashboard as a quality improvement and strategic driving tool in the IBD outpatient setting: early experience from IBD Centre of excellence at the University of Alberta hospital. J Can Assoc Gastroenterol. 2018;1(suppl_1):225–6.
Macken L, Hyrkas K. Retention, fatigue, burnout and job satisfaction: new aspects and challenges. J Nurs Manag. 2014;22(5):541.
MacKusick CI, Minick P. Why are nurses leaving? Findings from an initial qualitative study on nursing attrition. Medsurg Nurs. 2010;19:6.
Manzano García G, Ayala Calvo JC. Emotional exhaustion of nursing staff: influence of emotional annoyance and resilience. Int Nurs Rev. 2012;59(1):101–7.
Marć M, Bartosiewicz A, Burzyńska J, Chmiel Z, Januszewicz P. A nursing shortage – a prospect of global and local policies. Int Nurs Rev. 2019;66(1):9–16.
McHugh MD, Berez J, Small DS. Hospitals with higher nurse staffing had lower odds of readmissions penalties than hospitals with lower staffing. Health Aff. 2013;32(10):1740–7.
McMullan M. Patients using the Internet to obtain health information: how this affects the patient – health professional relationship. Patient Educ Couns. 2006;63(1–2):24–8.
McPake B, Mahal A. Addressing the needs of an aging population in the health system: the Australian case. Health Syst Reform. 2017;3(3):236–47.
Moore LW, Sublett C, Leahy C. Nurse managers’ insights regarding their role highlight the need for practice changes. Appl Nurs Res. 2016;30:98–103.
Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One. 2018;13(8):e0203316.
MSSS H, AAA C. The nursing shortage impact on job outcome (the case in Sri Lanka). J Competitiveness. 2015;7(3)
Najimi A, Goudarzi AM, Sharifirad G. Causes of job stress in nurses: a cross-sectional study. Iran J Nurs Midwifery Res. 2012;17(4):301.
National Health Service. National Health Service careers: Healthcare assistant 2015.
National Quality Board. Supporting NHS providers to deliver the right staff, with the right skills, in the right place at the right time: safe, sustainable and productive staffing: National Quality Board (NQB); 2016.
Needleman J. Nursing skill mix and patient outcomes: BMJ Publishing Group Ltd; 2017.
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse staffing and patient outcomes in hospitals: Harvard School of Public Health Boston; 2001.
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715–22.
Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037–45.
Nolte AG, Downing C, Temane A, Hastings-Tolsma M. Compassion fatigue in nurses: a metasynthesis. J Clin Nurs. 2017;26(23–24):4364–78.
HIMSS Nursing Informatics Awareness Task Force. An emerging giant: nursing informatics. Nurs Manag. 2007;38(3):38–42.
O’Brien-Pallas L, Irvine D, Peereboom E, Murray M. Measuring nursing workload: understanding the variability. Nurs Econ. 1997;15(4):171–83.
Okwaraji F, En A. Burnout and psychological distress among nurses in a Nigerian tertiary health institution. Afr Health Sci. 2014;14(1):237–45.
van Oostveen CJ, Ubbink DT, Mens MA, Pompe EA, Vermeulen H. Pre-implementation studies of a workforce planning tool for nurse staffing and human resource management in university hospitals. J Nurs Manag. 2016;24(2):184–91.
Phillips JP. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374(17):1661–9.
Power A, Kirwan G. Cyberpsychology and new media: a thematic reader: Psychology Press; 2013.
Punnakitikashem P, Rosenberber JM, Buckley-Behan DF. A stochastic programming approach for integrated nurse staffing and assignment. Lie Transactions. 2013;45(10):1059–76.
Queensland University of Technology. Business planning framework: nursing resources: Brisbane Queensland Health; 2001.
Qureshi SM, Purdy N, Neumann WP, editors. Simulating the impact of patient acuity and nurse-patient ratio on nurse workload and care quality. Congress of the international ergonomics association: Springer; 2018.
Rankin J, McGuire C, Matthews L, Russell M, Ray D, Research LBC, et al. Facilitators and barriers to the increased supervisory role of senior charge nurses: a qualitative study. J Nurs Manag. 2016;24(3):366–75.
Remus S, Kennedy MA. Innovation in transformative nursing leadership: nursing informatics competencies and roles. Can J Nurs Leadersh. 2012;25(4):14–26.
Roche M, Duffield C, Aisbett C, Diers D, Stasa H. Nursing work directions in Australia: does evidence drive the policy? Collegian. 2012;19(4):231–8.
Roche MA, Duffield C, Friedman S, Dimitrelis S, Rowbotham S. Regulated and unregulated nurses in the acute hospital setting: tasks performed, delayed or not completed. J Clin Nurs. 2016;25(1–2):153–62.
Rosow E, Adam J, Coulombe K, Race K, Anderson R. Virtual instrumentation and real-time executive dashboards: solutions for health care systems. Nurs Adm Q. 2003;27(1):58–76.
Rosser LH, Kleiner BH. Using management information systems to enhance health care quality assurance. J Manag Med. 1995;9:27–36.
Rothmann S, Van Der Colff J, Rothmann J. Occupational stress of nurses in South Africa. Curationis. 2006;29(2):22–33.
Royal College of Nursing. The UK nursing labour market review 2018. London: Royal College of Nursing; 2017.
Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care. 2008;20(4):227–37.
Scott RD. The direct medical costs of healthcare-associated infections in US hospitals and the benefits of prevention; 2009.
Scott A, Timmons S. Tensions within management roles in healthcare organisations. Nurs Manag. 2017;24(1):31–7.
Sensmeier J. Make the most of health IT. Nurs Manag. 2016;47(12):32–5.
Sermeus W, Aiken LH, Van den Heede K, Rafferty AM, Griffiths P, Moreno-Casbas MT, et al. Nurse forecasting in Europe (RN4CAST): rationale, design and methodology. BMC Nurs. 2011;10(1):6.
Sheppard K. Compassion fatigue: are you at risk. Am Nurse Today. 2016;11(1):53–5.
Smiley RA, Lauer P, Bienemy C, Berg JG, Shireman E, Reneau KA, et al. The 2017 national nursing workforce survey. J Nurs Regul. 2018;9(3 Supplement)
Snavely TM. A brief economic analysis of the looming nursing shortage in the United States. Nurs Econ. 2016;34(2):98–101.
Squillace MR, Rosenoff E, Remsburg RE, Bercovitz A, Branden L. An introduction to the national nursing assistant survey. 2007.
Stanley D. Leadership and management. Chichester, UK: John Wiley & Sons; 2016.
Stewart W, Terry L. Reducing burnout in nurses and care workers in secure settings. Nurs Stand. 2014;28(34):37–45.
Strudwick G, Nagle L, Kassam I, Pahwa M, Sequeira L. Informatics competencies for nurse leaders: a scoping review. J Nurs Adm. 2019a;49(6):323–30.
Strudwick G, Booth RG, Bjarnadottir RI, Rossetti SC, Friesen M, Sequeira L, et al. The role of nurse managers in the adoption of health information technology: findings from a qualitative study. J Nurs Adm. 2019b;49(11):549–55.
Taylor B, Yankey N, Robinson C, Annis A, Haddock KS, Alt-White A, et al. Evaluating the Veterans Health Administration’s Staffing Methodology model: a reliable approach. Nurs Econ. 2015;33(1):36.
Tierney SJ, Seymour-Route P, Crawford S. Weighted staffing plans for better prediction of staffing needs. J Nurs Adm. 2013;43(9):461–7.
Twigg D, Duffield C. A review of workload measures: a context for a new staffing methodology in Western Australia. Int J Nurs Stud. 2009;46(1):132–40.
Twigg D, Duffield C, Bremner A, Rapley P, Finn J. The impact of the nursing hours per patient day (NHPPD) staffing method on patient outcomes: a retrospective analysis of patient and staffing data. Int J Nurs Stud. 2011;48(5):540–8.
Twigg DE, Myers H, Duffield C, Pugh JD, Gelder L, Roche M. The impact of adding assistants in nursing to acute care hospital ward nurse staffing on adverse patient outcomes: an analysis of administrative health data. Int J Nurs Stud. 2016;63:189–200.
U.S Bureau of Labour Statistics. Occuaptional outlook handbook United States: U.S Bureau of Labour Statistics; 2013.
Unruh LY, Fottler MD. Patient turnover and nursing staff adequacy. Health Serv Res. 2006;41(2):599–612.
Vermeir P, Vandijck D, Degroote S, Peleman R, Verhaeghe R, Mortier E, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015;69(11):1257–67.
Vespa J, Armstrong DM, Medina L. Demographic turning points for the United States: population projections for 2020 to 2060: US Department of Commerce, Economics and Statistics Administration, US …; 2018.
Ward L, Fenton K, Maher L. The high impact actions for nursing and midwifery 8: ready to go – no delays…last in our series. Nurs Times. 2010;106(34):16–7.
Weggelaar-Jansen AMJ, Broekharst DS, De Bruijne M. Developing a hospital-wide quality and safety dashboard: a qualitative research study. BMJ Qual Saf. 2018;27(12):1000–7.
Welsh Government. Nurse Staffing Levels Act 2016. Cardiff: Welsh Government; 2016.
Westra BL, Delaney CW. Informatics competencies for nursing and healthcare leaders. AMIA annual symposium proceedings: American Medical Informatics Association; 2008.
Williams J, Smith AP. Stress, job satisfaction and mental health of NHS nurses. Contemporary Ergonomics and Human Factors 2013. 95: ROUTLEDGE in association with GSE Research; 2013. p. 95–102.
Wise S, Duffield C. Has the search for better leadership come at the expense of management? Int J Nurs Stud. 2019;97:A1–2.
World Health Organization. Global strategy on human resources for health: workforce 2030. Geneva, Switzerland: WHO; 2016.
World Health Organization. Global health workforce statistics: Geneva World Health Organisation; 2018.
Yazici HJ. The role of communication in organizational change: an empirical investigation. Inf Manag. 2002;39:539–52.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
9.1 Electronic Supplementary Material
Data 1
Educational Template (PPTX 49 kb)
Glossary
- CQI
-
Continuous Quality Improvement
- DRG
-
Diagnosis Related Groups
- Failure to rescue FR
-
As a safety and quality measure, failure to rescue has been defined as the inability to prevent death after the development of a complication.
- MDC
-
Major Diagnostic Categories
- MIS
-
Management Information System
- NHpPD
-
Nursing Hours per Patient Day
- NSO
-
Nursing Sensitive Outcomes—a measure of nursing’s contribution to patient safety.
- NWMS
-
Nursing Workload Management System, which measure direct, indirect, and nonclinical patient care hours by patient acuity
- PAIS
-
Patient Assessment and Information System
- Patient churn
-
The excessive movement of patients due to admissions, transfers and discharges
- PCS
-
Patient Classification System, also used interchangeably with NWMS
- TQM
-
Total Quality Improvement
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Doleman, G., Duffield, C. (2021). Administrative Applications. In: Hussey, P., Kennedy, M.A. (eds) Introduction to Nursing Informatics. Health Informatics. Springer, Cham. https://doi.org/10.1007/978-3-030-58740-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-58740-6_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-58739-0
Online ISBN: 978-3-030-58740-6
eBook Packages: MedicineMedicine (R0)