Abstract
The practice of Nephrology in Nigeria dates back to the 1960s when the country gained independence from the UK. The University College Hospital (UCH) in Ibadan, as a college of the University of London, had the first recognised Nephrology unit. Several other units have been established over the years countrywide in federal, state and private institutions, although these units are mainly restricted to the urban parts of the country where an estimated 51.9% of the population now live. These units mainly have the capacity to carry out haemodialysis, with much fewer units having the capacity to carry out peritoneal dialysis and kidney transplantation. Haemodialysis has been consistently carried out in the country since 1982 with expanding capacity, and renal transplantation since March 2000. Peritoneal dialysis, however, despite being first performed in the early 1960s at UCH Ibadan, is done only in few centres and as acute intermittent peritoneal dialysis due to various challenges which are addressed in this chapter. The chapter also details a summary of the spectrum of kidney diseases, therapies and related research that are available in the country. The peculiarities and challenges faced by those engaged in the care of these patients are also outlined.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Nigeria
- Tropical nephrology
- Chronic glomerulonephritis
- Dialysis
- Kidney transplantation
- Paediatric nephrology
- HIV nephropathy
- Sickle cell nephropathy
- CAKUT
- Diaspora
- APOL-1
Area1 | 923,768 Km2 |
Population1 | 203.5 million (2018) |
Capital | Abuja |
Three most populated cities1 | 1. Lagos (13.5 million) 2.Kano (3.8 million) 3.Ibadan (3.4 million) |
Official language1 | English |
Gross Domestic Product (GDP)2 | 375.8 billion USD (2017) |
GDP per capita2 | 1968.6 USD (2017) |
Human Development Index (HDI)3 | 0.532 (2017) |
Official currency | Naira |
Total number of nephrologists | 188 |
National society of nephrology | Nephrology Association of Nigeria (NAN) |
Incidence of end-stage renal disease | 2018 – not available |
Prevalence of end-stage renal disease | 2018 – ~15 pmp |
Total number of patients on dialysis (all modalities) | 2017 – ~2000 2018 – ~3000 |
Number of patients on haemodialysis | 2017 – ~2000 2018 – ~3000 |
Number of patients on peritoneal dialysis | 2017 – <10 2018 – <10 |
Number of renal transplantations per year | 2017 – 117 2018 – 142 |
Introduction
Nigeria is situated in the West African sub-region with a total area of 923,768 Km2 and a current population of 203.5 million, making it the 32nd largest but the 7th most populous country in the world [1]. It is believed that one out of every five Black people in the world is a Nigerian. Nigeria is the most populous country in Africa and has the largest economy in the continent [2]. The economy is diverse but the largest revenue earner for the country is crude oil with the 10th largest reserves of crude oil in the world. The federal capital was moved to Abuja in 1984 from the coastal city of Lagos; however, Lagos remains the financial capital and the most populous city in the country.
Even though a democracy since its independence from Britain 59 years ago, Nigeria was bedevilled with a civil war and multiple military insurgences and regional conflicts for the first 39 years after its independence from the UK. This is partly responsible for the emigration of many of its professionals to many parts of the western world and the Middle East, such that there are possibly more nephrologists practicing outside the country than there are currently practicing in the country. Fortunately, however, it has had more than 20 consistent years of democracy to date and it is hoped that this will lead to sustained economic growth and development.
The population growth rate is 2.6%. The population is young with 42.5% and 3.3% of the country younger than 15 years and >65 years, respectively [1]. About 60.9% of this population are adjudged as being below the poverty line, although there is a marked disparity with its distribution around the country. While in the southwestern part of the country only 20% of the populations live below this poverty line, in some states in the northern part of the country, over 80% of the citizens live below the poverty line [3]. This skewed wealth distribution is also reflected in the distribution of Nephrology capacity around the country. While the southwest part of the country has as many as 62 dialysis units, the Northeast consisting of 6 states and a population of 19 million (by 2006 census) has only 10 dialysis units (Figs. 5.1 and 5.2). Regardless of the geopolitical zone, none of these units are located in the rural areas where 49.7% of the population resides.
Map of Nigeria with the numbers of dialysis centres in each of the six geopolitical zones, Lagos and Abuja
 North East states: Adamawa, Bauchi, Borno, Gombe, Taraba, Yobe
North East states: Adamawa, Bauchi, Borno, Gombe, Taraba, Yobe
 North West states: Jigawa, Kaduna, Kano, Katsina, Kebbi, Sokoto
North West states: Jigawa, Kaduna, Kano, Katsina, Kebbi, Sokoto
 North Central states: Benue, Kogi, Kwara, Nassarawa, Niger, Plateau
North Central states: Benue, Kogi, Kwara, Nassarawa, Niger, Plateau
 South East states: Abia, Anambra, Ebonyi, Enugu, Imo
South East states: Abia, Anambra, Ebonyi, Enugu, Imo
 South West states: Ekiti, Lagos, Ogun, Ondo, Osun, Oyo
South West states: Ekiti, Lagos, Ogun, Ondo, Osun, Oyo
 South South states: Akwa Ibom, Cross Rivers, Bayelsa, Delta, Edo, Rivers
South South states: Akwa Ibom, Cross Rivers, Bayelsa, Delta, Edo, Rivers
The disease pattern is reflective of a developing economy and features a double burden of both communicable and non-communicable diseases. While still battling with the scourge of malaria, tuberculosis and HIV, there is a rising prevalence of hypertension (now 28.9% of the adult population) and type 2 diabetes mellitus [4, 5]. These reflect strongly on the prevalence and aetiology of kidney diseases in the country. In addition, 20–30% of the population carry the sickle cell gene and 23–28% have the high-risk APOL1 genotype – two recognised genetic markers of non-diabetic chronic kidney disease [6,7,8].
Despite this double burden of disease, the allocation to health in the national budget is just 3.7% of the GDP. In addition, less than 5% of the population is covered by the National Health Insurance Scheme [9]. Consequently, most of the spending on health by individuals is out of pocket and, with the prevailing poverty index in the country, many resort to alternative health practitioners, faith healers, herbalists and complementary medicines in the pursuit of cures for their various ailments [10]. This partly explains why the number of patients with CKD receiving standard care is low and very few patients initiating dialysis are able to sustain long-term care (Table 5.1).
History of Nephrology in Nigeria
The practice of nephrology in Nigeria began with the establishment of the first medical school in the University College Hospital (UCH), Ibadan. This was one of the first teaching hospitals in the British Commonwealth and was at a time designated the 4th best hospital within the Commonwealth of Nations. The medical school was established first as a branch of the University College of London but with the inauguration of UCH Ibadan, the training of medical doctors took place wholly in Nigeria. The Nephrology unit in UCH was, therefore, the first-ever of such units in Nigeria under the headship of Professor Oladipo Akinkugbe, the first indigenous nephrologist who was trained in the UK. He is regarded as the doyen and father of nephrology in Nigeria and was recently awarded the International Society of Nephrology pioneers award for Africa.
The unit carried out the first peritoneal dialysis (PD) in the country in 1965 and along with other pioneers in the hospital published seminal works on tropical nephrology including the role of Plasmodium malariae in the aetiology of the nephrotic syndrome – the so-called quartan malaria nephropathy [11,12,13]. Ever since, several other units have been established in different parts of the country. The first haemodialysis (HD) unit in the country was established at the Lagos University Teaching Hospital in Lagos, under Professors Mabadeje and Odutola. This unit spurred on and helped with training staff for the over 180 other different dialysis units now in existent in different parts of the country. The first private dialysis unit was established in 1987 by Dr Okey Onuzo in Lagos. Renal transplantation was first carried out successfully at St Nicholas hospital in Lagos in March 2000. This unit remains the most active renal transplantation centre, but has been joined by 14 other centres in different parts of the country.
The distribution of the dialysis and transplant units based on the six geopolitical zones in the country is outlined in Fig. 5.1. Although most of the units are in public hospitals, the most active ones are in private hospitals. Unfortunately, however, these units are restricted to the urban parts of the country where there is a concentration of personnel to run these units.
There has been a rapid increase in the numbers of nephrologists, dialysis nurses and technologists trained to run these units since the commencement of postgraduate training in Nigeria by the National Postgraduate Medical College of Nigeria in 1969 and the West African Postgraduate Medical College in 1976.
Renal Diseases in Nigeria
Kidney diseases are now very common and their prevalence has now assumed epidemic proportions globally. Though the true prevalence figure of end-stage renal disease (ESRD) in Nigeria is unknown, it is assumed to be high. However, several community and hospital studies have reported rates from 7.8% to 23.5% and an increase of 300% in the prevalence of CKD in the last three decades [14,15,16,17,18,19,20,21,22,23,24,25,26]. Awobusuyi et al. [23], in the largest community study involving ten urban communities in ten state capitals distributed among all the six geopolitical zones of the country, found a CKD crude prevalence of 23.47% (1896 out of 8077 participants). An analysis of all the available publications on prevalence of CKD from all geopolitical zones of Nigeria revealed that 20.4% of 14,253 screened participants had overt or covert CKD (Table 5.2). Advanced CKD and ESRD are also recognised to be quite common constituting about 8–23% of medical admissions in different tertiary hospitals [26, 27].
CKD is mainly a disease of the young and middle-aged (20–50 years) in Nigeria and this compares favourably with what is reported in other developing countries in Africa; however, it is in sharp contrast with the older age groups seen in the developed world [14, 26, 27]. A large proportion of CKD patients are males who are in the most economically productive age group [14, 26, 27]. The causes of CKD in Nigeria, though similar to what have been reported from different countries in sub-Saharan Africa, differ remarkably from that in the developed world [14, 26,27,28]. Hypertension and glomerulonephritis remain the most common causes of CKD with diabetic nephropathy being a distant third, though with the rising prevalence of diabetes mellitus, this is expected to increase [5, 26, 27, 29]. The traditional infectious causes of CKD still abound and HIV-associated nephropathy (HIVAN) remains a major contributor to the CKD burden [14, 26, 30]. Other important causes include obstructive uropathy, sickle cell nephropathy and chronic tubulointerstitial nephritis [27, 31].
The outcome of ESRD in Nigeria remains gloomy as majority of our patients cannot afford renal replacement therapy (RRT) and are thus placed on conservative management. Even those that are able to start RRT are unable to sustain RRT beyond a few sessions. Mortality is thus very high among patients presenting with ESRD with majority dying within the first year of presentation. This poor outlook has been attributed to a number of additional reasons including late presentation to healthcare facilities, associated co-morbidities, limited capacity for RRT, the exorbitant cost of managing patients, limited capacity of health workers particularly non-nephrologists in kidney disease prevention, and poor awareness of kidney disease as well as poor health-seeking attitude in the community [14, 26,27,28].
Acute kidney injury (AKI) in adults occurs mainly from prerenal and intrinsic renal causes and is principally community-acquired. The incidence established as a percentage of medical admissions is 3–5%, though figures as high as 19–24% of AKI have been reported following intensive care and surgical admissions (Table 5.3) [32,33,34,35,36,37,38,39,40,41,42]. The principal causes are gastroenteritis whether cholera related or not, nephrotoxins, sepsis from various infections, glomerulonephritis, malaria especially in non-immune visitors, obstructive uropathy in the elderly and drugs including radiocontrast agents. Pregnancy-related causes also abound and these include septic abortion, ante or postpartum haemorrhage and eclampsia among others [32,33,34,35,36, 38,39,40,41]. RRT modalities used in the management of AKI in Nigeria include acute or intermittent PD and acute HD. Continuous therapies are generally unavailable but are gradually being introduced in the last 5–10 years. Overall mortality varies remarkably between centres (18–45%) with differing patient populations but on the average hovers around 36% [32,33,34,35,36, 38,39,40,41].
Haemodialysis in Nigeria
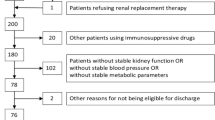
HD was first used in the management of ESRD at the Lagos University Teaching Hospital in 1981. Subsequently, the number of HD centres has grown remarkably and now stands at about 186 in the entire country (Figs. 5.1 and 5.2). It is the most commonly prescribed modality of RRT. Most of the patients (60–90%) are commenced on HD with very few patients (<1%) being initiated on PD and only about 1–2% being offered kidney transplantation [26, 27, 43]. The majority of ESRD patients are first offered HD, usually as an emergency lifesaving procedure, because many of them present with severe complications even at first visit. It is estimated that there are currently about 3000 patients accessing HD services yearly across the 186 units spanning the country. Many of these are, however, unable to sustain HD beyond a few sessions particularly in most of the public hospital run centres.
A review of HD publications use in the management of ESRD revealed that about 38.6% of the patients were unable to pay for any session of dialysis while 53.2% could only support it for less than 1 month. Only 0.6% of our ESRD patients are able to support the treatment for longer than 1 year (Table 5.3) [26,27,28, 31, 44, 45]. National Health Insurance Scheme (NHIS) now covers dialysis care for AKI, offering six sessions to enrollees with no support for chronic dialysis or transplantation. In addition, the relatively exorbitant cost of HD (about 100–200 US dollars per session) leads to withdrawal from dialysis care and eventual uremia and death. Even for those patients who are able to commence dialysis , adequacy is another major challenge as some may opt for once- or twice-weekly session on account of financial constraints. An audit of RRT in five public dialysis units in Lagos metropolis revealed financial constraints, 30.9% dialyse twice weekly, 43.6% once weekly even though the standard prescription is 4-hour sessions thrice weekly. This is at variance with the experience at St Nicholas hospital, a privately run unit, where 87% of the patients adhered to a twice-weekly scheduling, 10% to a thrice-weekly scheduling and just 3% to a once-weekly scheduling, a reflection of the different mix of patients seen in the unit differs from those in the publicly run units. This differential is also reflected in the various access routes employed by patients in these public units where 10% had AV fistulae as access, 81.8% temporary femoral catheters and just 7.3% long-term internal jugular catheters, as opposed to the SNH private unit where 10% had AV fistulae, 2% temporary catheters and 88% long-term internal jugular catheters in place. These statistics also consequently reflect on the outcomes of the patients managed in the public and private settings. While mortality is high in many of the public dialysis units with mortality at 1 year characteristically being in excess of 70% in contra-distinction to the mortality at the SNH unit which is just 5.3% in 1 year. This unit has a patient who has been on dialysis for over 20 years (as he has declined a kidney transplant being a Jehovah’s witness) along with 5.3% others on maintenance HD for more than 5 years. This is likely replicated in many of the units all around the country, but more likely in the privately run units that are more likely to manage patients with the capacity to sustain the costs involved.
Reuse of dialysers is not common but a few of the public units recycle patient-specific dialysers for up to five times in an attempt to limit costs. There is no applied ratio of nurses to HD patients but units generally have one nurse to 2–4 patients. Haemodiafiltration/haemofiltration are available in a few units particularly the privately run units but costs of running these limit their usage.
Incidence of the various viral infections, routinely screened for, varies but at the SNH unit in the year 2018 this was: HIV 4%, HCV 2.6% and HBsAg 2.6%. All units screen patients at presentation and most would repeat the screens after every 6 months if the patient remains on HD. Most units isolate viral positive patients when they are accepted for HD.
Erythropoietin-stimulating agents are generally available as are all other drugs used routinely in the care of patients with ESRD on dialysis. These are however often beyond the capacity of the patients to access them routinely as they often have to pay for these out-of-pocket. Consequently, uncontrolled hypertension, anaemia and poor control of mineral and bone disorder are not infrequent among these patients, contributing to the poor outcomes often encountered in these patients.
There are currently no Government regulations for the sector but the Nephrology Association of Nigeria (NAN) has developed guidelines , which are followed by its members staffing the various dialysis units.
Peritoneal Dialysis in Adult Nigerians
PD has been employed in the management of renal failure in Nigeria since 1967, when it was first used in patients with AKI secondary to post-abort sepsis [11]. Since then, several reports on the use of acute and intermittent PD in the country have been published [46, 47]. However, continuous ambulatory peritoneal dialysis (CAPD) is used infrequently [48].
Fewer than ten renal centres offer PD mainly in the form of acute or intermittent PD; none of them perform automated PD (APD). Only one centre performed CAPD but stopped because of daunting challenges, which included irregular supply of PD fluids and catheters and the exorbitant cost of these consumables; these consumables are not manufactured locally. In one earlier publication, PD consumables were a major challenge and frequently improvised [48]. Expectedly, peritonitis was a major setback and complicated 60–65% of acute PD [48, 49]. Several centres still practice acute PD, particularly in the management of AKI in adults and children, though it is more commonly used in the paediatric population [46, 47, 49]. In summary, PD practice is still largely suboptimal in Nigeria with CAPD being very irregular and APD virtually unavailable; there are thus less than ten patients on CAPD or APD in the whole country. If, however, the fore-mentioned challenges are surmounted, CAPD would contribute to the capacity to manage ESRD patients in the country.
Kidney Transplantation in Nigeria
Kidney transplantation became available in the country since 2000, first at St. Nicholas Hospital, a private facility in Lagos, and subsequently in two public facilities in 2002 [50]. Thereafter, 11 more facilities have been established (Table 5.4). By December 2018, about 550 patients have been transplanted within Nigeria with over 80% performed in two private-funded centres. Logistics, bureaucratic and funding challenges have impeded the development of the services in public-funded health institutions. Despite the availability of this service in Nigeria, quite a number of patients still travel abroad for transplantation [50, 51]. The total number of kidney transplants performed in Nigeria in all the units in 2017 was 117 and in 2018 142. All of these were living-related transplants and almost all were carried out by the two private units located in Lagos and Abuja.
Kidney transplantation in Nigeria received legal backing in 2014 by an act of the National Assembly [50]. This provided a legal framework for transplantation activities in Nigeria, although its implementation has been rather sporadic and inadequate. For example, only living donor kidney transplantation is available in the country, at the moment [50]. The majority of the organs are donated by genetically related individuals with a few from emotionally related persons. Kidney donation is usually reviewed by an independent committee, which provides ethical guidance. Pre-transplant investigations are mainly done within the centres, but there is limited availability of HLA typing and crossmatch services with only one centre, the Obafemi Awolowo University Teaching Hospital Complex, currently providing this service [52]. None provides flow cytometry crossmatch and testing for donor-specific antibodies. As a result, most centres still send their samples abroad with its attendant delays and increased cost of service.
Maintenance immunosuppressants are available and the majority of patients are on calcineurin inhibitor-based triple therapies. However, cost considerations limit the options available to patients with several patients opting for azathioprine rather than mycophenolate mofetil, for instance. Also, induction regimen is guided by HLA match and affordability. Measurement of drug levels for the calcineurin inhibitors is only available in a few centres. However, post-transplantation follow-up is available in many centres in Nigeria as there are nephrologists with locally and internationally acquired experience caring for kidney transplant patients. Although there is no countrywide transplant registry available, one publication that reviewed data from the various centres reported a 1-year graft and patient survival of 83.2% and 90.2%, respectively [53]. The 5-year graft and patient survival were 58.7% and 73.4% respectively. Post-transplant complications reported include acute rejection episodes, chronic allograft nephropathy, CMV infection , and malignancies especially Kaposi’s sarcoma.
Challenges of Renal Replacement Therapy
The challenges of RRT are mainly those of availability, affordability and accessibility, which are closely linked with the myriads of problems prevalent in a region bedevilled by widespread poverty, ineffective public policies, high unemployment, poor planning and mismanagement of available resources [54].
Funding remains a major challenge as most patients have to provide the cost of RRT from out of pocket in a country where the cost of a session of HD (which is 100–200 USD) is higher than the minimum wage of even the gainfully employed individuals. The implication of this is that the cost of an HD session is out of the reach for most of the population needing RRT [30]. Most patients are unable to afford more than a week of dialysis in government-owned facilities. Only a few private dialysis centres have affluent patients that are able to sustain for longer periods [26,27,28, 30]. Also, a few corporate patients have employers that provide healthcare support including dialysis.
The phenomenon termed “brain drain ” has contributed to the dearth of nephrology personnel in Nigeria. The quest for economic greener pastures has favoured an emigration to developed countries much to the detriment of the developing countries such as Nigeria where there is dire need for their skills and expertise. There are several Nigerian trained medical personnel practicing as Nephrologists round the globe and their numbers may actually be more than the numbers practicing in Nigeria.
Challenges to the applicability and usefulness of CAPD in the sub-region include non- availability of PD cyclers, PD fluids and catheters, which have to be imported. Others include high peritonitis rates, and more recently, dearth of skilled manpower in peritoneal dialysis [14, 26, 27, 43]. The challenges of kidney transplant in Nigeria include funding concerns, and paucity of laboratories able to perform tissue typing, drug levels and transplant kidney histology.
Paediatric Renal Diseases in Nigeria
Renal diseases in children are frequent and common reasons for hospitalisation (Table 5.5). From a prevalence of 1.1% of all paediatric admissions in the 1980–90s, kidney diseases now account for 3.8–8.9% of all paediatric admissions into public-funded tertiary hospitals [55,56,57,58]. The increase in the frequency of kidney diseases in hospitalised children may reflect a true increase, better recognition and/or as a result of refinement in the definitions of some these diseases to include milder forms. The changes in the definition of AKI and CKD to more sensitive ones are notable examples [59,60,61].
Nephrotic syndrome (NS) is the most commonly reported kidney disease in children. In most series, it accounted for 20–30% of all kidney diseases in children outside the neonatal period [57, 58, 62]. Its dramatic presentation with generalised oedema makes it easier to be recognised. Unlike in the period between 1970 and 2000 which was characterised by the predominance of steroid-resistant nephrotic syndrome, most recent reports of childhood nephrotic syndrome in Nigeria indicate that about 60–80% of children with idiopathic nephrotic syndrome have steroid-sensitive NS [13, 55, 63, 64]. The reason for the increased steroid responsiveness is not known, however, children are now developing nephrotic syndrome at a much younger age than in the past decades [63, 65, 66]. On the other hand, the frequency of acute glomerulonephritis is on the decline as would be expected with increase in the standard of living , access to antibiotics and health care [67, 68].
Following the adoption of AKI consensus definitions, which recognise milder forms, AKI is now reported among the top most common kidney diseases in children in Nigeria. Since 2012, AKI accounts for 20–30% of cases of kidney diseases among hospitalised children outside the neonatal period [58, 68]. In addition, congenital anomalies of the kidneys and urinary tract (CAKUT), with or without urinary tract infection, are also commonly reported in hospitalised children in Nigeria [58, 68]. Because most of the published studies focused on hospitalised children, it is likely that the frequency of CAKUT would be higher than currently reported as most cases of CAKUT seen only in outpatient settings are not included in these studies. Consistently, CKD accounts for less than 10% of kidney diseases [58, 68]. The near absence of symptoms until marked reduction in glomerular filtration rate (GFR) means that milder forms of CKD would be missed. Wilms tumour is the most common kidney tumour reported, accounting for 1.6–6.8% of cases of kidney disease [57, 68]. In one large tertiary hospital, Wilms tumour accounted for one-fifth of kidney diseases reported in hospitalised children [58].
Paediatric Chronic Kidney Disease Epidemiology
The true burden of CKD in children in Nigeria is largely unknown. The absence of a national registry means reliance on reports from single centres to estimate the prevalence of CKD. Yearly incidence and prevalence of CKD in children in Nigeria is put between 3.0 to 11 and 12.5 to 48 cases per million children per year, respectively [69,70,71,72]. Although it does appear that CKD is less prevalent in children in Nigeria compared with children in the developed world, reliance on data from large urban hospitals means that the true burden of CKD in Nigeria is largely unknown, and most likely underreported [73, 74].
Chronic glomerulonephritis, either primary or secondary, is the leading cause of CKD in children. In a recent study of children in a southwest city, about 77% of the 53 children with ESRD had chronic glomerulonephritis; a third of which initially presented as nephrotic syndrome [71]. In another study involving 45 children with CKD defined as GFR <30 ml/min/1.73 m2, chronic glomerulonephritis was the cause of the CKD in 56% of the children [69]. The secondary causes of chronic glomerulonephritis include HIV, hepatitis B infection, and systemic lupus erythematosus [69, 70]. In one study, these secondary causes made up about a quarter of causes of CKD [70]. With a prevalence of sickle cell disease (SCD) of 1.5–3%, and an estimated 100,000 children born each year with sickle cell anaemia [75, 76], its contribution to CKD is expected to be higher than currently reported. In addition, as more children with SCD survive into adolescence, the prevalence of SCD-related chronic kidney disease is expected to increase.
CAKUT is the second most common causes of CKD in children. They accounted for 20–30% in most series [69, 71]. Posterior urethral valves (PUV) were the most common CAKUT reported, which partly explained the overrepresentation of males in most published studies [71, 72]. The predominance of chronic glomerulonephritis as the leading cause of CKD in children in Nigeria contrasts with the picture in most developed countries, where CAKUT, including aplasia, hypoplasia and dysplasia, are the leading causes [77, 78]. It is possible that with the high neonatal and under-5 mortality rates in Nigeria, mostly from prematurity, neonatal sepsis, pneumonia and malaria, younger children with undiagnosed CAKUT die before detection and are underrepresented in series of children with CKD, which feature mostly adolescents. It is not unusual in Nigeria for cases of PUV to be diagnosed in children older than 5 years [79, 80].
Management of children with CKD in Nigeria is largely suboptimal and frustrating to health workers and the affected families. The majority of children with ESRD in Nigeria do not get dialysis due to the family’s inability to pay for the care and the near-absence of any form of health insurance that provides coverage for dialysis [71, 72]. As with reimbursement for dialysis in adults, payment for RRT is out of pocket. Those that get dialysis do so infrequently and for only a few weeks or months at most, again, largely as a result of its costs [72, 81]. Chronic PD is not an established modality for ESRD both in children as well as in adults in Nigeria. Vascular access is mostly via acute femoral catheters; occasionally some children get tunnelled lines [82]. Not unexpected, management of anaemia, hypertension, fluid overload, metabolic acidosis, hyperkalemia, bone and mineral disease, and growth impairment is suboptimal.
As a result of suboptimal care, mortality from CKD is disproportionately high. Not uncommonly, mortality at 1 year after diagnosis of ESRD is in excess of 50% [71, 83].
Paediatric Haemodialysis in Nigeria
HD is generally not accessible to most African children [84]. This is largely due to the lack of facilities, lack of trained workforce and cost implications to the patient. In the few children who received HD with good outcome, the most common indication for HD was AKI [82]. Most children needing chronic HD receive it for only a short period because of the inability to pay for it [45]. Unavailability of size-appropriate dialysis consumables such as bloodlines and dialysers means that only bigger children get access to HD; for smaller children priming of the bloodlines is an option commonly used [82].
Peritoneal Dialysis in Children in Nigeria
PD , as a form of RRT, is a distant second option to HD for most persons needing dialysis in Nigeria. It is only available in large tertiary hospitals in urban centres of the country [85, 86]. When used, PD is administered manually rather than with automated cyclers in Nigeria [85, 86]. In some cases, nasogastric tubes and intercostal drains are used as improvised PD catheters [86]. In addition, it is not unusual for non-commercial PD fluids to be used because the cost of PD fluids is exorbitant [86]. These improvisations are needed because of the non-availability or exorbitant cost of the consumables and consequently PD in Nigeria is currently limited to children with AKI.
Paediatric Acute Kidney Injury and Critical Care Nephrology
AKI is a common kidney disease among children presenting to emergency hospital services in the country. In most recent studies, AKI ranks as high as nephrotic syndrome in terms of prevalence [58, 68]. Unlike in developed countries, most cases of AKI in children in Nigeria are community-acquired rather than hospital-acquired [87]. Sepsis is now commonly reported as the leading cause of AKI in the post-neonatal age group [88, 89]. Other common causes of AKI include primary kidney diseases and malaria [88, 90, 91]. The primary kidney diseases reported include nephrotic syndrome, posterior urethral valves and acute nephritic syndrome from post-streptococcal glomerulonephritis. Gastroenteritis as sole cause of AKI is less commonly encountered [88, 90]. Among the neonates, perinatal asphyxia and neonatal sepsis are the leading causes of AKI [91, 92].
AKI in children in Nigeria is characterised by the predominance of severe forms and high attendant mortality. In most series, children with stage 3 or RIFLE-F AKI made up more than 50% of the children with AKI [88, 90], and in-hospital mortality rate reached up to 30% [87, 89, 91]. The high mortality rate often stems from late presentation, predominance of more severe forms of AKI and poor availability of paediatric ICU services and dialysis [87, 93].
Approaches to Prevention of Kidney Diseases in Nigeria
With health insurance coverage clearly excluding chronic kidney care, most patients in Nigeria are unable to bear the cost of care. This makes prevention of CKD an imperative strategy. More so, awareness of kidney diseases in the general population is low [94]. There are no established prevention programs for CKD in Nigeria. However, many nephrologists have leveraged the opportunity presented by the annual World Kidney Day to raise awareness, educate and screen the population for kidney diseases. This has led to many prevention-related activities across the country [20, 21]. Kidney disease prevention activities in Nigeria can be categorised into programs aimed at:
-
Increasing awareness among the general population
-
Early detection and management of at-risk individuals
-
Timely referral for specialist care
Kidney disease awareness-raising activities have largely involved the use of mass media such as radio, television, online and print media. Face-to-face campaigns target places with large numbers of people such as markets, worship centres such as churches and mosques as well as schools, and densely populated work environments. Lately, social media platforms such as WhatsApp and Facebook are being used by kidney disease practitioners to raise awareness of kidney diseases. Given that CKD may be asymptomatic in the early phases, screening activities need to be sustained. However, large population screenings are not logistically possible in Nigeria as it involves enormous costs. It would be more appropriate to make the activities more efficient and cost-effective by embedding in the process a prescreening phase. This would involve an initial clinical history, blood pressure and anthropometric checks in which at-risk persons are identified for further screening with blood and urine testing [95]. It seems reasonable to offer this service as part of an integrated screening for prevention of both communicable and non-communicable diseases packages at primary and secondary care level. Nigeria’s three-tier health system has been designed to facilitate referrals from the primary to secondary to tertiary level of care and vice versa. However, due to a dearth of human resources for health and inadequate healthcare financing, this referral system has been suboptimal. In practice, primary care physicians refer patients with suspected or definite kidney diseases to specialists mostly practicing at tertiary centres.
Nephrology Practice in Nigeria
As stated earlier, renal care units were first established in the early 1960s and situated in the teaching hospitals in Ibadan (UCH), Lagos, Zaria, Ile-Ife and Enugu as part of internal medicine and paediatric services offered by these hospitals. The early specialists in these units, most of whom were trained abroad, were responsible for care of patients with renal diseases in addition to their responsibilities of care for patients with other non-communicable and communicable illnesses. At that time, PD and an attempt at HD using a coil dialysis machine were made at the University College Hospital, Ibadan. There was also a lot of research into the aetiology of nephrotic syndrome done at these early teaching hospitals including the association of steroid-resistant form of childhood nephrotic syndrome and Plasmodium malariae [12, 13].
The first dedicated HD unit was established at the Lagos University Teaching Hospital in 1981 and following this other units have been opened in almost every teaching hospital and federal tertiary hospital all over the country. Several state government hospitals also have established units.
Many of these units are bedevilled with various challenges faced by the public-funded institutions in Nigeria today, consequent on poor funding, poor administration of these units, inter-professional rivalry and rather frequent industrial disputes within these establishments. As a result of this, there are now many private renal care units that currently outnumber the public institutions in numbers and capacity. Generally, private units tend to be larger in capacity and attend to much larger numbers of patients than most public-funded units. Almost invariably, however, these renal units are situated in the urban centres and almost none in any of the rural areas where almost 50% of the population live. In addition, these private units are less likely to be involved in strikes and generally have better outcomes as they are more likely to see privately funded patients who have the capacity to sustain the costs associated with renal care by any of the various modalities. This would explain why the most active kidney transplant units in the country are in the private-funded hospitals and just two of these are responsible for over 80% of more than the 500 kidney transplants that have been carried out in the country till date. The costs involved in renal care in Nigeria are not covered by the National Health Insurance Scheme (NHIS) although advocacy by the NAN has led to a policy by government for the NHIS to cover the costs of the first six sessions of dialysis. With less than 5% of the population covered by the NHIS, most patients have to pay the costs for their care, out of pocket.
Majority of the nephrology specialists are engaged by the public institutions but many in their spare time also make their services available in many of the private institutions. Altogether there are over 180 nephrologists (over 150 adults and about 30 paediatric nephrologists) practicing in the country.
Currently, between 10 and 15 adult and paediatric nephrologists are certified each year by two postgraduate medical colleges through over a 6-year period. Each trainee passes through a similar three-stage examination process (Primary, Part 1 and Part 2 examinations) before certification as a nephrologist. Graduates of these training programs are appointable as consultant nephrologists. There are currently 188 consultant adult and paediatric nephrologists practicing in Nigeria, with the majority working in public hospitals where most of the nephrology and dialysis centres are located. There are estimated to be about 788 nurses and 295 renal technicians practicing in these units. The training for these nurses and technicians, after the initial training the pioneers of these professions received abroad, has also been done locally in the various units.
The NAN is the official professional body of nephrologists, renal nurses, renal technicians and other professionals involved in the care of the renal patient. It was established in 1987 in Ibadan, Oyo State, and currently boasts over 500 members. Yearly, it holds its scientific and general meeting with the venue rotated to different parts of the country with active nephrology practice. The themes and sub-themes of these meetings focus on relevant aspects of renal care in Nigeria. The Association accepts all physicians involved in the care of renal patients as ordinary members while nurse practitioners, nephrology nurses, dialysis technicians and dietitians are accepted as associate members. Through its members, the NAN is active in research and advocacy, and is in the process of setting up a national renal registry.
The Association is affiliated to both ISN and AFRAN. NAN has enjoyed an excellent collaboration with ISN that has led to significant development of capacities in most renal units across the country. Several nephrologists have benefitted from the Fellowship program of ISN and many centres have graduated from the Sister Renal Centre (SRC) relationship with several others still benefitting at different stages. NAN continues to benefit from the ISN Continuous Medical Education Committee with sponsorship of 3–4 resource persons to our annual scientific conference held in the second week of February every year. Many of our centres are also involved in the Educational Ambassador Program (EAP) and Library Enhancement Program (LEP). The attendance at the World Congress of Nephrology (WCNs) from Nigeria has improved remarkably in the last three decades. NAN now undertakes advocacy with the government and their agencies with a view to improving nephrology practice in the country, thereby engendering excellent outcomes to our patients as well as influencing policy decisions of the government.
There are job opportunities available around the country for all cadre of professionals engaged in the care of renal patients, more so in the northern parts of the country where the number of these specialists remains inadequate. The average starting salary for a young nephrologist would be in the region of $2000 per month. This relatively low pay when compared with similarly skilled professionals in the developed world is a major driver of the exodus of the Nigerian renal care professionals to various countries in the western world. An additional reason for the exodus is the suboptimal outcome of renal patients in the country, which is tied closely to poor funding.
Nephrology Practice by Nigerians in the Diaspora
Emigration , for a variety of reasons, has been an increasingly common practice among medical professionals from Nigeria [96]. The trend, part of a larger process colloquially known as the “Brain Drain” is largely believed to have started in the late 1980s and is considered to have reached levels where, by some accounts, majority of licensed physicians are either themselves considering emigration or know several colleagues who are [97].
The reasons for emigration vary according to the time of graduation. There are three common time frames for emigration: immediately following completion of pre-registration year and national youth service, during or when seeking middle-grade training or once established as a consultant. For earlier time points, movement seems to be a combination of training opportunities, family ties and socioeconomic opportunities. Movement of the established consultant seems more geared to socioeconomic opportunities. This may be reflected in the tendency of more mature practitioners to choose the Middle East as an emigration destination and the younger to seemingly favour the UK and the USA. The UK and USA are unarguably the two most desired countries for emigrant Nigerian physicians [97]. This is partly as a result of the convenience of the language and culture. English is the lingua franca (official language) in Nigeria. The UK is often the first relocation point for younger trainees even if they plan the USA to be their final destination. This may be due to historical ties to the UK existing since the colonial times (1914–1960). Another likely reason for the predilection to the UK is pre-existing family and social ties of would-be emigrants, easing the stress of the move and settling into a foreign and potentially hostile environment. Opportunities for progression in the UK in selected medical specialities such as Nephrology for the International Medical Graduate (IMGs) appear limited compared to those available in the USA potentially due to the relative size of the USA and varied perception of IMGs in the UK and the USA. This may explain the disproportionately high number of Nigerian IMGs registered with the General Medical Council versus only seven attaining certification in Nephrology in the UK. This is in contrast to the USA where there are 124 board-certified Nephrologists who received their initial medical degree from a Nigerian medical school. Other countries where Nigerian trained professionals are known to practice include the various countries in the Middle East, Australia, South Africa and Canada. Altogether, there are possibly more Nigerian nephrologists practicing outside the country than there are within.
Conclusion
In Nigeria, kidney diseases are very common in adults and children and the outcome of patients with ESRD is dismal because of suboptimal care. The suboptimal care is mainly driven by the inability of most families to meet the financial cost of care. Illiteracy, underdevelopment, dearth of personnel and infrastructure are additional major barriers mitigating against access to healthcare and RRT by the vast majority of the population domiciled largely in the rural areas. The true prevalence of CKD, though still largely speculative, is expected to rise markedly with the predicted increase in the prevalence of non-communicable diseases such as diabetes mellitus, and the continued scourge of infectious diseases. There is an ongoing concerted effort to develop a Nigerian renal registry and this is expected to assist in determining the true prevalence of ESRD and provide a firm basis for policies aimed at preventing and treating affected patients. Targeted screening of at-risk populations should be developed and aggressively implemented as well as measures to ensure sustainable financing of RRT. There is the need to develop effective monitoring systems that would ensure judicious utilisation of available resources while the health personnel need to be sufficiently motivated to mitigate the effects of brain drain.
References
CIA. The World Factbook. Nigeria; 2019.
World Bank. Country Profile. Nigeria; 2018.
OPHI. Nigeria Country Briefing, Multidimensional Poverty Index Data Bank; 2017.
Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens. 2015;33(2):230–42. https://doi.org/10.1097/HJH.0000000000000413.
Adeloye D, Ige JO, Aderemi AV, Adeleye N, Amoo EO, Auta A, et al. Estimating the prevalence, hospitalisation and mortality from type 2 diabetes mellitus in Nigeria: a systematic review and meta-analysis. BMJ Open. 2017;7(5):e015424. https://doi.org/10.1136/bmjopen-2016-015424.
Tayo BO, Kramer H, Salako BL, Gottesman O, McKenzie CA, Ogunniyi A, et al. Genetic variation in APOL1 and MYH9 genes is associated with chronic kidney disease among Nigerians. Int Urol Nephrol. 2013;45(2):485–94. https://doi.org/10.1007/s11255-012-0263-4.
Ulasi II, Tzur S, Wasser WG, Shemer R, Kruzel E, Feigin E, et al. High population frequencies of APOL1 risk variants are associated with increased prevalence of non-diabetic chronic kidney disease in the Igbo people from South-Eastern Nigeria. Nephron Clin Pract. 2013;123(1–2):123–8. https://doi.org/10.1159/000353223.
Fleming AF, Storey J, Molineaux L, Iroko EA, Attai ED. Abnormal haemoglobins in the Sudan savanna of Nigeria. I. Prevalence of haemoglobins and relationships between sickle cell trait, malaria and survival. Ann Trop Med Parasitol. 1979;73(2):161–72. https://doi.org/10.1080/00034983.1979.11687243.
Hafez R. Nigeria health financing system assessment. 2018.
Chukwuneke FN, Ezeonu CT, Onyire BN, Ezeonu PO. Culture and biomedical care in Africa: the influence of culture on biomedical care in a traditional African society, Nigeria, West Africa. Niger J Med. 2012;21(3):331–3.
Akinkugbe OO, Abiose P. Peritoneal dialysis in acute renal failure, West Afr Med J 1967;16:165–168.
Hendrickse RG, Gilles HM. The nephrotic syndrome and other renal diseases in children in Western Nigeria. East Afr Med J. 1963;40:186–201.
Hendrickse RG, Adeniyi A, Edington GM, Glasgow EF, White RH, Houba V. Quartan malarial nephrotic syndrome. Collaborative clinicopathological study in Nigerian children. Lancet. 1972;1(7761):1143–9.
Arogundade FA, Barsoum RS. CKD prevention in Sub-Saharan Africa: a call for governmental, nongovernmental, and community support. Am J Kidney Dis. 2008;51(3):515–23. https://doi.org/10.1053/j.ajkd.2007.12.006.
Afolabi MO, Abioye-Kuteyi EA, Arogundade FA, Bello IS. Prevalence of chronic kidney disease in a Nigerian family practice population. S Afr Fam Pract. 2009;51(2):132–7.
Oluyombo R, Ayodele OE, Akinwusi PO, Okunola OO, Akinsola A, Arogundade FA, et al. A community study of the prevalence, risk factors and pattern of chronic kidney disease in Osun State, South West Nigeria. West Afr J Med. 2013;32(2):85–92.
Okoye OCA, Oviasu E, Ojogwu L. Prevalence of chronic kidney disease and its risk factors amongst adults in a rural population in Edo State, Nigeria. J US China Med Sci. 2011;8(8):471–81.
Ulasi II, Ijoma CK, Onodugo OD, Arodiwe EB, Ifebunandu NA, Okoye JU. Towards prevention of chronic kidney disease in Nigeria: a community-based study in Southeast Nigeria. Kidney Int Suppl. 2013;3:195–201.
Oluyombo R, Olamoyegun MA, Ayodele OE, Akinwusi PO, Akinsola A. Clustering of chronic kidney disease and cardiovascular risk factors in South-West Nigeria. J Nephropathol. 2017;6(3):196–203. https://doi.org/10.15171/jnp.2017.33.
Abene EE, Gimba ZM, Agaba PA, Uchendu DG, Olaniru OB, Ocheke IE, et al. Chronic kidney disease screening: results of the 2013 World Kidney Day activities conducted at the Jos University Teaching Hospital. Highl Med Res J. 2017;17(1):1–5.
Okwuonu CG, Chukwuonye II, Adejumo OA, Agaba EI, Ojogwu LI. Prevalence of chronic kidney disease and its risk factors among adults in a semi-urban community of South-East Nigeria. Niger Postgrad Med J. 2017;24(2):81–7. https://doi.org/10.4103/npmj.npmj_34_17.
Egbi OG, Okafor UH, Miebodei KE, Kasia BE, Kunle-Olowu OE, Unuigbe EI. Prevalence and correlates of chronic kidney disease among civil servants in Bayelsa state, Nigeria. Niger J Clin Pract. 2014;17(5):602–7. https://doi.org/10.4103/1119-3077.141426.
Awobusuyi JO, Bakare O, Dada A, Adamu U, Abasi-Ekong U, Effa E, et al. Indices of kidney damage in Nigeria: a survey of 8077 subjects in the six geopolitical zones of the country. Trop J Nephrol. 2015;10(2):95–105.
Nalado A, Abdu A, Adamu B, Aliyu MH, Arogundade FA, Sanusi AA, et al. Prevalence of chronic kidney disease markers in Kumbotso rural Northern Nigeria. Afr J Med Med Sci. 2016;45(1):61–5.
Oyebisi OO, Okunola OO, Jaiyesimi AE, Arogundade FA, Adelaja MA, Erohibe CE, et al. Prevalence and pattern of chronic kidney disease and its associated risk factors in a rural community in South Western Nigeria. West Afr J Med. 2018;35(2):109–16.
Arogundade FA, Sanusi AA, Hassan MO, Akinsola A. The pattern, clinical characteristics and outcome of ESRD in Ile-Ife, Nigeria: is there a change in trend? Afr Health Sci. 2011;11(4):594–601.
Ulasi II, Ijoma CK. The enormity of chronic kidney disease in Nigeria: the situation in a teaching hospital in South-East Nigeria. J Trop Med. 2010;2010:501957. https://doi.org/10.1155/2010/501957.
Arije A, Kadiri S, Akinkugbe OO. The viability of hemodialysis as a treatment option for renal failure in a developing economy. Afr J Med Med Sci. 2000;29(3–4):311–4.
King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414–31. https://doi.org/10.2337/diacare.21.9.1414.
Naicker S. Burden of end-stage renal disease in Sub-Saharan Africa. Clin Nephrol. 2010;74 Suppl 1:S13–6. https://doi.org/10.5414/cnp74s013.
Alebiosu CO, Ayodele OO, Abbas A, Olutoyin AI. Chronic renal failure at the Olabisi Onabanjo University Teaching Hospital, Sagamu, Nigeria. Afr Health Sci. 2006;6(3):132–8. https://doi.org/10.5555/afhs.2006.6.3.132.
Kadiri S, Ogunlesi A, Osinfade K, Akinkugbe OO. The causes and course of acute tubular necrosis in Nigerians. Afr J Med Med Sci. 1992;21(1):91–6.
Bamgboye EL, Mabayoje MO, Odutola TA, Mabadeje AF. Acute renal failure at the Lagos University Teaching Hospital: a 10-year review. Ren Fail. 1993;15(1):77–80.
Arogundade FA, Sanusi AA, Okunola OO, Soyinka FO, Ojo OE, Akinsola A. Acute renal failure (ARF) in developing countries: which factors actually influence survival. Cent Afr J Med. 2007;53(5–8):34–9.
Emem-Chioma PC, Alasia DD, Wokoma FS. Clinical outcomes of dialysis-treated acute kidney injury patients at the University of Port Harcourt teaching hospital, Nigeria. ISRN Nephrol. 2013;2013:540526. https://doi.org/10.5402/2013/540526.
Okunola OO, Ayodele OE, Adekanle AD. Acute kidney injury requiring hemodialysis in the tropics. Saudi J Kidney Dis Transpl. 2012;23(6):1315–9. https://doi.org/10.4103/1319-2442.103587.
Oluseyi A, Ayodeji A, Ayodeji F. Aetiologies and short-term outcomes of acute kidney injury in a tertiary centre in Southwest Nigeria. Ethiop J Health Sci. 2016;26(1):37–44. https://doi.org/10.4314/ejhs.v26i1.8.
Makusidi AM, Liman HM, Yakubu A, Hassan M, Isah MD, Chijioke A. Hemodialysis among pregnancy related acute kidney injury patients: a single center experience in North-Western Nigeria. Indian J Nephrol. 2016;26(5):340–2. https://doi.org/10.4103/0971-4065.171224.
Bello BT, Busari AA, Amira CO, Raji YR, Braimoh RW. Acute kidney injury in Lagos: pattern, outcomes, and predictors of in-hospital mortality. Niger J Clin Pract. 2017;20(2):194–9. https://doi.org/10.4103/1119-3077.183258.
Awowole IO, Omitinde OS, Arogundade FA, Bola-Oyebamiji SB, Adeniyi OA. Pregnancy-related acute kidney injury requiring dialysis as an indicator of severe adverse maternal morbidity at a tertiary center in Southwest Nigeria. Eur J Obstet Gynecol Reprod Biol. 2018;225:205–9. https://doi.org/10.1016/j.ejogrb.2018.04.041.
Okunola OO, Arogundade FA, Sanusi AA, Akinsola A. Acute renal failure in the intensive care unit: aetiological and predisposing factors and outcome. West Afr J Med. 2009;28(4):240–4.
Raji YR, Ajayi SO, Ademola AF, Lawal TA, Ayandipo OO, Adigun T, et al. Acute kidney injury among adult patients undergoing major surgery in a tertiary hospital in Nigeria. Clin Kidney J. 2018;11(4):443–9. https://doi.org/10.1093/ckj/sfx144.
Arogundade FA, Ishola DA Jr, Sanusi AA, Akinsola A. An analysis of the effectiveness and benefits of peritoneal dialysis and haemodialysis using Nigerian made PD fluids. Afr J Med Med Sci. 2005;34(3):227–33.
Oluyombo R, Okunola OO, Olanrewaju TO, Soje MO, Obajolowo OO, Ayorinde MA. Challenges of hemodialysis in a new renal care center: call for sustainability and improved outcome. Int J Nephrol Renovasc Dis. 2014;7:347–52. https://doi.org/10.2147/IJNRD.S65835.
Bello BT, Raji YR, Sanusi I, Braimoh RW, Amira OC, Mabayoje OM. Challenges of providing maintenance hemodialysis in a resource poor country: experience from a single teaching hospital in Lagos, Southwest Nigeria. Hemodial Int. 2013;17(3):427–33. https://doi.org/10.1111/hdi.12024.
Akinsola A, Arije A. Peritoneal dialysis in Nigerian patients with a short history of advanced renal failure. West Afr J Med. 1987;6:205–9.
Ojogwu LI. Peritoneal dialysis in the management of hypertensive acute oliguric renal failure. Trop Geogr Med. 1983;35(4):385–8.
Akinsola A, Adelekun A, Arogundade FA. Continuous ambulatory peritoneal dialysis (CAPD) practice in OAUTHC Ile-Ife., Nigeria, a preliminary experience. Dial Transplant. 2000;29(12):774–82.
Arogundade FA, Olatunde LO, Ishola DA Jr, Bappa A, Sanusi AA, Akinsola A. PD (peritoneal dialysis) peritonitis: still a major limiting factor in peritoneal dialysis management today. Afr J Nephrol. 2004;8:52–6.
Ulasi II, Ijoma CK. Organ transplantation in Nigeria. Transplantation. 2016;100(4):695–7. https://doi.org/10.1097/TP.0000000000001149.
Okafor UH. Kidney transplant in Nigeria: a single centre experience. Pan Afr Med J. 2016;25:112. https://doi.org/10.11604/pamj.2016.25.112.7930.
Bolarinwa RA, Oyekunle AA, Arogundade FA, Sanusi AA, Salawu L, Togun RA, et al. Preliminary report of HLA (DNA) typing of Nigerians using sequence-specific primer technique. Niger Postgrad Med J. 2014;21(4):285–9.
Arogundade FA. Kidney transplantation in a low-resource setting: Nigeria experience. Kidney Int Suppl (2011). 2013;3(2):241–5. https://doi.org/10.1038/kisup.2013.23.
Bamgboye EL. Barriers to a functional renal transplant program in developing countries. Ethn Dis. 2009;19(1 Suppl 1):S1-56–59.
Eke FU, Eke NN. Renal disorders in children: a Nigerian study. Pediatr Nephrol. 1994;8(3):383–6.
Etuk IS, Anah MU, Ochighs SO, Eyong M. Pattern of paediatric renal disease in inpatients in Calabar, Nigeria. Trop Dr. 2006;36(4):256. https://doi.org/10.1258/004947506778604968.
Michael IO, Gabriel OE. Pattern of renal diseases in children in Midwestern Zone of Nigeria. Saudi J Kidney Dis Transpl. 2003;14(4):539–44.
Ladapo TA, Esezobor CI, Lesi FE. Pediatric kidney diseases in an African country: prevalence, spectrum and outcome. Saudi J Kidney Dis Transpl. 2014;25(5):1110–6.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;(2):1–138.
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl. 2012;2:139–274.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative w. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–12. https://doi.org/10.1186/cc2872.
Ugwu GI, Nwajei G, Chinemelu U. Pattern of renal diseases among children in the Niger Delta Region, Nigeria. Arab J Nephrol Transplant. 2014;7(1):49–50.
Ladapo TA, Esezobor CI, Lesi FE. High steroid sensitivity among children with nephrotic syndrome in Southwestern Nigeria. Int J Nephrol. 2014;2014:350640. https://doi.org/10.1155/2014/350640.
Anochie I, Eke F, Okpere A. Childhood nephrotic syndrome: change in pattern and response to steroids. J Natl Med Assoc. 2006;98(12):1977–81.
Ibadin MO, Abiodun PO. Epidemiology and clinicopathologic characteristics of childhood nephrotic syndrome in Benin-City, Nigeria. J Pak Med Assoc. 1998;48(8):235–8.
Okoro BA, Okafor HU, Nnoli LU. Childhood nephrotic syndrome in Enugu, Nigeria. West Afr J Med. 2000;19(2):137–41.
Adedoyin OT, Adesiyun OA, Mark F, Adeniyi A. Childhood renal disorders in Ilorin, North Central Nigeria. Niger Postgrad Med J. 2012;19(2):88–91.
Anigilaje EA, Adesina TC. The pattern and outcomes of childhood renal diseases at University of Abuja Teaching Hospital, Abuja, Nigeria: a 4 year retrospective review. Niger Postgrad Med J. 2019;26(1):53–60. https://doi.org/10.4103/npmj.npmj_174_18.
Anochie I, Eke F. Chronic renal failure in children: a report from Port Harcourt, Nigeria (1985–2000). Pediatr Nephrol. 2003;18(7):692–5. https://doi.org/10.1007/s00467-003-1150-0.
Olowu WA, Adefehinti O, Aladekomo TA. Epidemiology and clinicopathologic outcome of pediatric chronic kidney disease in Nigeria, a single center study. Arab J Nephrol Transplant. 2013;6(2):105–13.
Asinobi AO, Ademola AD, Ogunkunle OO, Mott SA. Paediatric end-stage renal disease in a tertiary hospital in South West Nigeria. BMC Nephrol. 2014;15:25. https://doi.org/10.1186/1471-2369-15-25.
Odetunde OI, Okafor HU, Uwaezuoke SN, Ezeonwu BU, Adiele KD, Ukoha OM. Chronic kidney disease in children as seen in a tertiary hospital in Enugu, South-East, Nigeria. Niger J Clin Pract. 2014;17(2):196–200. https://doi.org/10.4103/1119-3077.127553.
Ardissino G, Dacco V, Testa S, Bonaudo R, Claris-Appiani A, Taioli E, et al. Epidemiology of chronic renal failure in children: data from the ItalKid project. Pediatrics. 2003;111(4 Pt 1):e382–7.
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ. Epidemiology of chronic kidney disease in children. Pediatr Nephrol. 2012;27(3):363–73. https://doi.org/10.1007/s00467-011-1939-1.
Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN. Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med. 2013;10(7):e1001484. https://doi.org/10.1371/journal.pmed.1001484.
Adedoyin OT, Adesiyun OO, Adegboye OA, Bello OA, Fatoye OP. Sickle cell nephropathy in children seen in an African Hospital – case report. Niger Postgrad Med J. 2012;19(2):119–22.
Wong CJ, Moxey-Mims M, Jerry-Fluker J, Warady BA, Furth SL. CKiD (CKD in children) prospective cohort study: a review of current findings. Am J Kidney Dis. 2012;60(6):1002–11. https://doi.org/10.1053/j.ajkd.2012.07.018.
Lewis MA, Shaw J, Sinha MD, Adalat S, Hussain F, Castledine C, et al. UK Renal Registry 12th Annual Report (December 2009): chapter 14: demography of the UK paediatric renal replacement therapy population in 2008. Nephron Clin Pract. 2010;115(Suppl 1):c279–88. https://doi.org/10.1159/000301237.
Orumuah AJ, Oduagbon OE. Presentation, management, and outcome of posterior urethral valves in a Nigerian tertiary hospital. Afr J Paediatr Surg. 2015;12(1):18–22. https://doi.org/10.4103/0189-6725.150937.
Ikuerowo SO, Balogun BO, Akintomide TE, Ikuerowo AO, Akinola RA, Gbelee HO, et al. Clinical and radiological characteristics of Nigerian boys with posterior urethral valves. Pediatr Surg Int. 2008;24(7):825–9. https://doi.org/10.1007/s00383-008-2163-3.
Olowu WA. Renal failure in Nigerian children: factors limiting access to dialysis. Pediatr Nephrol. 2003;18(12):1249–54. https://doi.org/10.1007/s00467-003-1255-5.
Asinobi AO, Ademola AD, Alao MA. Haemodialysis for paediatric acute kidney injury in a low resource setting: experience from a tertiary hospital in South West Nigeria. Clin Kidney J. 2016;9(1):63–8. https://doi.org/10.1093/ckj/sfv112.
Odetunde OI, Okafor HU, Uwaezuoke SN, Ezeonwu BU, Ukoha OM. Renal replacement therapy in children in the developing world: challenges and outcome in a tertiary hospital in Southeast Nigeria. ScientificWorldJournal. 2014;2014:903151. https://doi.org/10.1155/2014/903151.
Ashuntantang G, Osafo C, Olowu WA, Arogundade F, Niang A, Porter J, et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in Sub-Saharan Africa: a systematic review. Lancet Glob Health. 2017;5(4):e408–17. https://doi.org/10.1016/S2214-109X(17)30057-8.
Ademola AD, Asinobi AO, Ogunkunle OO, Yusuf BN, Ojo OE. Peritoneal dialysis in childhood acute kidney injury: experience in Southwest Nigeria. Perit Dial Int. 2012;32(3):267–72. https://doi.org/10.3747/pdi.2011.00275.
Esezobor CI, Ladapo TA, Lesi FE. Peritoneal dialysis for children with acute kidney injury in Lagos, Nigeria: experience with adaptations. Perit Dial Int. 2014;34(5):534–8. https://doi.org/10.3747/pdi.2013.00097.
Olowu WA. Acute kidney injury in children in Nigeria. Clin Nephrol. 2015;83(7 Suppl 1):70–4.
Ademola AD, Asinobi AO, Ekpe-Adewuyi E, Ayede AI, Ajayi SO, Raji YR, et al. Acute kidney injury among paediatric emergency room admissions in a tertiary hospital in South West Nigeria: a cohort study. Clin Kidney J. 2018:1–6. https://doi.org/10.1093/ckj/sfy120.
Esezobor CI, Ladapo TA, Lesi FE. Clinical profile and hospital outcome of children with severe acute kidney injury in a developing country. J Trop Pediatr. 2015;61(1):54–60. https://doi.org/10.1093/tropej/fmu066.
Esezobor CI, Ladapo TA, Osinaike B, Lesi FE. Paediatric acute kidney injury in a tertiary hospital in Nigeria: prevalence, causes and mortality rate. PLoS One. 2012;7(12):e51229. https://doi.org/10.1371/journal.pone.0051229.
Anochie IC, Eke FU. Acute renal failure in Nigerian children: Port Harcourt experience. Pediatr Nephrol. 2005;20(11):1610–4. https://doi.org/10.1007/s00467-005-1984-8.
Airede A, Bello M, Weerasinghe HD. Acute renal failure in the newborn: incidence and outcome. J Paediatr Child Health. 1997;33(3):246–9.
Olowu WA, Adelusola KA. Pediatric acute renal failure in Southwestern Nigeria. Kidney Int. 2004;66(4):1541–8. https://doi.org/10.1111/j.1523-1755.2004.00918.x.
Oluyombo R, Ayodele OE, Akinwusi PO, Okunola OO, Gbadegesin BA, Soje MO, et al. Awareness, knowledge and perception of chronic kidney disease in a rural community of South-West Nigeria. Niger J Clin Pract. 2016;19(2):161–9. https://doi.org/10.4103/1119-3077.175960.
Perico N, Remuzzi G. Prevention programs for chronic kidney disease in low-income countries. Intern Emerg Med. 2016;11(3):385–9. https://doi.org/10.1007/s11739-016-1425-7.
Burch VC, McKinley D, van Wyk J, Kiguli-Walube S, Cameron D, Cilliers FJ, et al. Career intentions of medical students trained in six Sub-Saharan African countries. Educ Health (Abingdon). 2011;24(3):614.
NOIPolls. 2018. https://www.noi-polls.com/documents/Emigration_of_Medical_Doctors_Survey_Report.pdf. Accessed 28 May 2019.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Arogundade, F.A. et al. (2021). Nephrology in Nigeria. In: Moura-Neto, J.A., Divino-Filho, J.C., Ronco, C. (eds) Nephrology Worldwide. Springer, Cham. https://doi.org/10.1007/978-3-030-56890-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-56890-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-56889-4
Online ISBN: 978-3-030-56890-0
eBook Packages: MedicineMedicine (R0)