Abstract
A large number of studies explored the brainstem structures by using several reflex-recording techniques during ictal and interictal phases of migraine. Exteroceptive suppression of the temporalis muscle contraction, trigemino-cervical and trigemino-cervical-spinal reflexes, blink reflex, auditory evoked potentials, nociceptive flexion reflex, corneal reflex, and jaw-stretch reflex have been conducted with two main purposes: (1) to detect whether some neurophysiological parameters may represent a markers of migraine and (2) to investigate the pathophysiology of migraine.
With regard to the first point, the results of the basal assessment of brainstem reflexes are unsatisfactory, since all studies have shown almost normal or slightly abnormal findings in migraine patients and in patients with other forms of headache. On the other hand, much more homogeneous results have been obtained using protocols for the study of the habituation and recovery curves of such reflexes. These dynamic neurophysiologic studies confirm in migraineurs the phenomenon of “deficient habituation,” which is widely described during the interictal period for almost all sensory modalities. In this view, this phenomenon is considered a neurophysiologic biomarker of migraine.
In the same way, the study of brainstem reflexes may provide valuable insights in the debate about the pathogenesis of migraine and the role of CNS dysexcitability.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Migraine
- Habituation
- Exteroceptive suppression of the temporalis muscle contraction
- Trigemino-cervical reflex
- Blink reflex
- Auditory evoked potentials
- Nociceptive flexion reflex
- Jaw-stretch reflex
Brainstem structures play a critical role in the transmission of nociceptive impulses and in descending modulation of sensory transmission. Consequently, the study of brainstem reflexes may provide valuable insights into central pain processing mechanisms.
In this field, a large number of studies explored the brainstem by using reflex recording techniques (e.g., the trigeminofacial reflex, trigeminocervical reflexes, blink reflex, etc.).
Additionally, habituation and recovery curves to paired shocks, useful methods for investigating the excitability of the relevant sensitive, sensorial, nociceptive pathways in humans, were also widely evaluated for these reflexes. Since the trigeminal system and, more generally, the brainstem are key structures in the pathogenesis of migraine, the recovery curves of the aforementioned reflexes could provide valuable information about the status of the brainstem in this chronic pain disorder.
7.1 Exteroceptive Suppression of the Temporalis Muscle Contraction
Electrical stimulation of the infraorbital and mental nerves evokes a reflex that inhibits the voluntary contraction of the temporal and masseter muscles. A brainstem reflex mediates this inhibition, which is called “exteroceptive suppression.” On surface EMG recordings of jaw-closing muscles, the reflex appears as two suppression periods (SP1 and SP2) mediated by Aβ fibers: an early period, mediated by oligosynaptic pontine pathway, named SP1 response (ES1; 10–12 ms latency), and a late period, mediated by polysynaptic chain of interneurons of the lateral reticular formation, identified as SP2 response (ES2; 40–50 ms latency). The ES2 period is modulated via peripheral and central afferents (periaqueductal gray, nucleus raphe magnus, limbic cortex, orbitofrontal cortex). Consequently, the ES2 responses constitute a neurophysiologic correlate of the brainstem’s level of excitability [1].
Temporalis exteroceptive suppression (ES) has been widely studied in investigations of pain mechanisms, motor control, trigeminal nerve function, basal ganglia disorders, and brainstem lesions [2,3,4].
Furthermore, recording of the ES2 period of jaw-closing muscle activity is the only standardized method of studying the function of the brainstem inhibitory interneurons [2, 5].
Despite its usefulness in the assessment of pain mechanisms, only few studies investigated the ES2 duration in migraine at rest, with contradictory results.
Schoenen et al. reported reduced exteroceptive suppression of the temporalis muscle in patients with chronic tension-type headache but normal latency and duration of exteroceptive suppression in migraineurs [1].
In another study, the same author detected abnormal shortening of ES2 suppression period in patients with migraine [6].
Other authors observed low degree (the area of suppression was measured and divided by its duration) of exteroceptive suppression in 17 patients suffering from migraine without aura, while exteroceptive suppression in patients suffering from migraine with aura and cluster headache was the same as that in normative subjects [7].
The low degree of suppression might be supposed to reflect a deficiency in the endogenous pain control mechanism [8].
Unlike the previous studies, Zwart et al. observed that the durations of ES1 and ES2 periods were within normal limits in migraineurs [9].
Another study showed no statistical difference in a group of 28 migraineurs during interictal phase, considering onset latencies and duration of ES1 and ES2 periods, compared with controls. In this study, however, shorter duration of the ES2 period was evident during the attack period [10].
The mechanism governing this loss of muscle contraction control in migraineurs is still unclear. The authors of this study hypothesized that in migraine there may coexist an abnormality of control mechanisms of vascular and muscle contraction, and thus, the pain sensation of attacks might produce psychologic stress resulting in the loss of the suppressive function.
Only one study also assessed the recovery curve of the ES2 component of the temporalis muscle activity [11]. These authors reported that latencies, durations, and recovery curves of ES2 did not differ between control subjects, migraineurs, and patients with episodic and chronic tension-type headache.
In conclusion, controversial results have been reported regarding the different inhibitory and excitatory responses detected by means of exteroceptive suppression of the temporalis muscle in patients with migraine.
In many papers, there are significant abnormalities in the responses obtained during the attacks and in the intercritical phase. Scientific data pointed to the hyperactivity of contralateral aminoergic cortical-subcortical pathways, whose function is decreased between the migraine attacks [12]. Thus, unilateral trigeminal system hyperactivity has also been suggested [13, 14].
In this view, the ES2 period of exteroceptive suppression of the temporalis muscle, an anti-nociceptive reflex, may reflect a deficit in the endogenous pain control mechanisms in different types of headache. It has been suggested, however, that this response could be useful as a biologic marker in monitoring the time course of recovery from pain [15], and it is sensitive during the pain-free interval, so it can detect the persistent interictal abnormalities in migraine.
For these reasons, some authors hypothesized that the latency of ES2 period may be helpful in the differential diagnosis of peripheral and primary headache disorders and in particular to differentiate migraine and tension-type headache [16].
Moreover, it is conceivable that the exteroceptive suppression of the temporalis muscle may be used for evaluation of a drug’s effect. In fact, part of the 5HT effects in migraine is related to the inhibition of the trigeminal nuclear activity, and it is probable that part of the triptans effects is also mediated at this central site [17].
7.2 Trigeminocervical Reflexes
The trigeminocervical reflex (TCR) is obtained from the resting sternocleidomastoid muscle, using surface electromyographic recordings. Surface electrodes are positioned in a longitudinal direction over the muscles. Electrical stimuli are applied bilaterally to the supraorbital trigeminal branch near the point of nerve exit from the skull. The intensity is modified in order to result as strong but not painful. Several consecutive responses are averaged in each trace. The onset latency (ms), duration (ms), peak-to-peak amplitude (mV), and area (mV × ms) of the reflex responses are measured [18].
The trigeminocervical reflex, utilizing connections from the face to the neck motoneurones, is used for the examination of the brainstem interneuronal activity and its central control [18]. It may be supposed that different brainstem interneurons control the trigemino-trigeminal and the trigeminocervical reflexes.
Some authors used this neurophysiologic examination to assess brainstem interneurones function in migraine.
In one of the oldest studies assessing TCR [18], on the painful side of migraine patients, the mean onset reflex latency after ipsilateral and contralateral stimulation was strongly shortened. Conversely, there were no significant differences in the reflex duration, area, and amplitude between the painful and non-painful sides. No differences were also found between migraineurs and patients with tension-type headache [18]. The results of this study suggest a decreased activity of the brainstem inhibitory interneurons in migraine.
Other authors explored interictal and ictal phases of migraine. In particular, Nardone et al. [19] found that trigeminocervical responses are bilaterally abnormal in 17 out of 20 patients with migraine with aura (MA) and 15 out of 20 patients with migraine without aura (MO) during the headache attacks. In half of MA and MO patients, there were abnormal responses also during the interictal period. Moreover, in patients with normal trigeminocervical responses during the pain-free phase, the triptans were significantly more effective at relieving headache [19].
These findings were confirmed in another study by the same authors [20] and are consistent with the central role of the trigeminal system in the pathogenesis of migraine. The bilateral location of the abnormalities suggests a centrally located dysfunction. In particular, the trigeminocervical reflex is sensitive in disclosing a disordered brainstem activity and may be an index of neuronal activity in the human brainstem; moreover, its assessment may help as a valuable prognostic tool for predicting the efficacy of triptans therapy [20].
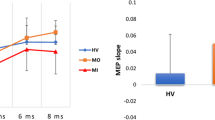
Partially in contrast with previous results, other authors [21] found no changes between controls and high-frequency episodic MO and MA patients in the mean values of trigemino-cervical-spinal reflexes (TCRSs) obtained at rest and during heterotopic painful stimulation (cold pressor test). Furthermore, the recovery curve of TCRs was significantly and markedly faster in migraine patients than in controls, while no differences were found in the basal trigemino-spinal reflexes (TSRs) [21]. The authors conclude that the interictal period of migraine is characterized by a hyperexcitability of the trigeminal pathways and by their anatomical and functional connections with the upper cervical cord neurons.
In conclusion, the trigemino-cervical and the trigemino-cervical-spinal reflexes may be useful for the evaluation of the impairment of the brainstem neuronal networks in migraine patients.
Overall, the more relevant findings of these studies demonstrated an abnormal hyperexcitability of trigeminal system during interictal phase, apparently not linked with supraspinal inhibitory modulation.
The “abnormality” of the supraspinal influences is probably more significant during the migraine attack and in the chronic migraine form than during the pain-free period.
TCR and TCRS studies are of little use in the diagnosis but are helpful for a better understanding of the common pain control mechanisms and the pathophysiology of migraine. In particular, the study of the recovery cycle of these reflexes appears to be a technique that can be used to make an accurate functional evaluation of the trigeminal pathways.
7.3 Blink Reflex
The mechanical or electrical stimulation of the supraorbital nerve elicits “blink reflex” responses and resembles the corneal reflex tested in clinical evaluation [22,23,24].
Usually, for the purpose of studying blink reflex, surface recording electrodes are located on the lower lateral side of the orbicularis oculi, reference electrodes are positioned on the lateral surface of the nose, and the ground electrode is located around the arm. The supraorbital nerve is stimulated with the cathode placed over the supraorbital foramen. Stimulation rate is 1 s−1. The shortest latency is taken into account and the EMG is not rectified.
Stimulation of the supraorbital nerve elicits two temporally separate responses of the orbicularis oculi, an early (R1) component, and two temporally separate contractile late responses ipsilateral and contralateral to the stimulation (R2 and R2′, respectively). R1 is an oligosynaptic reflex response and is evoked only on the side of stimulation via a pontine pathway [22,23,24]. On the other hand, unilateral stimulation elicits R2 bilateral response, which is presumably relayed through a more complex route (polysynaptic), including the pons and lateral medulla [25,26,27,28].
So, the blink reflex can be an objective and useful method for studying brainstem and the trigeminal system. Blink reflex recordings provide, consequently, a quantitative analysis for functions that involve the fifth and seventh cranial nerves, the dorsolateral pons, and the lateral medulla.
Several studies compared the latencies of R1, R2, and R2′ waves in migraine patients and control subjects (Table 7.1).
In the oldest study that evaluated blink reflex in 43 migraine patients, Bánk et al. [29] obtained the same R1 latencies in migraineurs and controls but R2 latency significantly prolonged in the migraine group. These findings indicate that trigeminal afferents and/or polysynaptic pathway in brainstem may be slightly functionally altered in migraine. The reasons for this delay are uncertain, especially in a headache-free interval.
This slight functional brainstem abnormality may underline or be the basis of migraine susceptibility. On the other hand, a peripheral abnormality of the trigeminal afferents could play a part in these pathophysiologic mechanisms. Sensory deficits of the face often can cause R2 latency alteration.
Other authors [30] reported that there was a statistically significant extension of bilateral R2 latencies in a 40-migraineur group compared with TTH patients and control groups. These confirm that brainstem and trigeminovascular connections play an important role in migraine pathogenesis and are functionally impaired in migraineurs (trigeminal system activation, sensitization of brainstem trigeminal nucleus, abnormal synaptic transmission, suppression of brainstem interneuron region) [30].
Unlike previous studies, Sand and Zwart [31] reported that mean R1 and R2 latencies were no different between various headache groups and that no group differences were found for the contralateral R2 response.
These findings were completely confirmed by Aktekin and colleagues [11] in episodic migraineurs. In this population, in fact, no differences were found also considering the facial side explored.
Some other researchers found normal R1 and R2 latencies, amplitudes, and areas obtained by ipsilateral and contralateral stimulations at any time intervals, during interictal phases of migraine as well as in episodic [32] and chronic migraine [33].
Other studies confirmed that there are no differences in all blink reflex components in migraine without aura, migraine with aura patients and controls and unilateral migraine patients did not differ from patients with bilateral pain [34, 35]. No significant differences were reported in another large group of migraine patients [36] and in medication overuse headache patients [37].
Avramidis et al. [38] reported similar results during interictal phase in 19 episodic migraineurs. In particular, latencies of all components are normal in all migraineurs. Conversely, during headache phase, significantly lower values of R2 and R2′ amplitude and size were found in the migraine group compared with the healthy control group. These findings were independent from stimulation site and were altered in the symptomatic side of headache. These authors described, furthermore, that sumatriptan administration was able to normalize R2′ amplitude and size.
The interpretation of these findings is that there is a temporary dysfunction of the bulbo-pontine interneurons only during the headache phase of migraine. In particular, the brainstem interneuron, which is part of the blink reflex arc, may be diffusely suppressed in migraine, only during the headache phase. Besides, blink reflex may be an objective laboratory method to monitor the effectiveness of specific drugs proposed for the treatment of migraine.
Other authors studied the blink reflex during migraine attacks.
Kaube et al. [39] studied 17 episodic migraine patients with unilateral migraine headache. The patients were studied within 6 h of attack’s onset. Blink reflexes were elicited in all patients using two different electrodes, a standard stimulating electrode (standard blink reflex) and a novel concentric stimulating “nociception-specific” electrode (“nociception-specific” blink reflex), during the acute migraine attack and after the treatment with intravenously lysine acetylsalicylate (1 g) or oral zolmitriptan (5 mg). The same protocols were used interictally. After “standard” stimulation, no differences were detected for the R1 and R2 onset latencies and areas under the curve (AUC) between the different time points and between the headache and non-headache side. “Nociception-specific” stimulation revealed, however, a significant shortening of R2 latency during the acute migraine attack compared with the headache-free interval. Drug treatment relief increased the onset latencies and reduced the AUC of R2 [39].
The authors of this study suggest a temporary sensitization of central trigeminal neurons during acute migraine attacks. In fact, the decrease of the onset latency and increase of the reflex integral (AUC) permit to hypothesize a facilitation of a spinal or medullary reflex. These findings are consistent with other experimental data [40].
These results are probably evident in this study and not in other similar studies because of a more selective stimulation (“nociception-specific”) that may lead to a higher and near-maximal saturation of the afferent pathway of the blink reflex and a reduced sensitivity toward more subtle changes in central thresholds and gain in sensory trigeminal transmission [41].
Another study confirmed these findings [42]. In this study, the comparison of R2 onset latencies during pain and during pain-free period within the groups of patients with migraine and sinusitis revealed a significant decrease of R2 latencies during the migraine attack compared to pain-free period but no differences between pain phase and pain-free period in the group of patients with sinusitis. These results are consistent with the facilitation of trigeminal nociception that seems specific for migraine rather than a consequence of peripheral pain, such as frontal sinusitis [42].
Other authors assessed the “nociception-specific” blink reflex interictally. Coppola et al. [43] reported no difference between migraineurs and healthy subjects for nociception-specific blink reflex (nBR) R2 responses in terms of stimulus intensity, pain threshold, onset latency, or AUC ipsilateral and contralateral.
Another study [44] showed that episodic migraine (EM) patients presented significantly decreased latencies and larger amplitudes and area-under-the-curve (AUC) values for the R2 component, whereas chronic migraine (CM) patients showed significantly prolonged latencies, smaller amplitudes, and AUC values for the R2 component. In the same study, the patients were assessed by means of pain-related evoked potentials (PREP) and both the EM and CM patients had decreased latencies of PREP responses with larger amplitude compared with the controls, which indicates facilitation at the cortical level. Additionally, the amplitude and AUC values of the R2 component exhibited a negative correlation, whereas the latency of the R2 component for the nBR showed a positive correlation with the frequency of headaches in migraineurs. This study provides electrophysiologic evidence that excitability of nociceptive-specific trigeminal pathways is different between EM and CM [44].
Other authors [37] assessing simultaneously nBR and PREP found “facilitation” of both trigeminal and somatic PREP, but not of nBR, indicating that the sensitization of nociceptive mechanisms mainly involved structures external to the trigeminal system and probably occurred at the supraspinal level [37].
In addition to the basal assessment of both “classical” and “nociception-specific” blink reflexes, many authors have compared the “recovery curve” and the habituation of blink reflex of migraineurs to non-migraine subjects.
Aktekin et al. reported similar R2 recovery curves in migraineurs and controls [11].
Coppola et al. confirmed these results [43] and described no difference of the nociceptive-BR R2 recovery curves between migraine patients outside of attacks and healthy volunteers.
De Marinis et al. [32] found R1 and R2 latencies, amplitudes, and areas similar in patients and control subject during basal assessment, but blink reflex habituation responses (R2 areas obtained at subsequent time intervals ranging between 10–5, 5–4, 4–3, and 3–2 s) markedly and statistically reduced in migraineurs with migraine attack within 72 h after neurophysiologic evaluation. In fact, in the comparison between groups, the R2 areas progressively decreased in control subjects, but remained high in migraine patients who experienced an attack within 72 h after testing. Also, the blink reflex habituation responses of the patients who had migraine attack after a longer time interval (from 4 to 15 days) were found reduced but did not differ significantly from those of controls. No correlations were found between blink reflex responses and age, duration of disease, and side of pain. These data are consistent with the activation of brainstem pathways involved in the blink reflex in the premonitory phase of migraine attacks, probably through mechanisms that involve dopaminergic function [32].
These findings confirmed the results of another contemporary study [45] that reported a significant defective habituation of blink reflex responses in patients during interictal period, fully reverted and “normalized” during a migraine attack [45].
Also Di Clemente et al. [46] found significant habituation deficit of BR-R2 response area in patients with migraine without aura during interictal phase. This lack of habituation shows a positive correlation in the same patients with a cortical habituation deficit, namely, the habituation of pattern-reversal visual evoked potentials.
These authors conclude that there is a wide neurobiologic dysfunction responsible for the habituation deficit in both cortex and brainstem [46].
The same authors investigated a nociceptive BR in 16 migraine patients without aura, 15 healthy subjects, and 14 healthy subjects with family history of migraine in their first-degree relatives [47]. The most significant habituation impairment was found in healthy subjects with a family history of migraine. The second one was found in migraine patients without aura, inversely correlated with the frequency of attacks. The authors interpreted that these results are the consequence of reduced serotoninergic transmission, leading to a decreased preactivation level, and are not due to trigeminal sensitization. Finally, an insufficient nociceptive-specific BR habituation is probably a presymptomatic neurophysiologic abnormality and, in this view, a marker of genetic predisposition for migraine [47].
In another study, De Marinis et al. [33] investigated the BR habituation in 35 patients with chronic migraine, outside and during a spontaneous attack, and control subjects. The habituation responses, delivered at time intervals of 10, 5, 4, 3, 2, and 1 s, were markedly reduced in patients studied outside an attack compared with those of the same patients studied during a migraine attack and of those of control subjects. There was a significant correlation between the decreased habituation of the blink reflex and a higher frequency of attacks. The decreased BR habituation outside an attack reveals abnormal excitability in chronic migraine, which normalizes during the attacks. The authors explain these data with central sensitization mechanisms that may also cause lower detection thresholds on the side affected by headache in patients during the attacks (allodynia). The blink reflex and its habituation may help shed light on the subtle neurophysiologic changes that occur in migraine patients between and during attacks [33].
A recent study [48] has confirmed that both migraine without aura and migraine with aura subjects showed a clear frequency-dependent deficit of habituation of the nBR-R2 responses when compared to healthy volunteers. However, migraine with aura subjects showed a less marked and/or non-homogeneous significant deficit of habituation of the nBR-R2 when compared to healthy controls. Furthermore, only in migraine without aura subjects, the mean frequency of migraine attacks correlates positively with the habituation rate of the nBR-R2. Based on these slight differences in terms of habituation deficit, the authors speculate a modulating role of the migraine aura susceptibility and excitability of the nociceptive trigeminal pathways [48].
Several authors also studied the effect of preceding conditioning stimuli on a blink reflex.
De Tommaso et al. [49] described a slight increase of blink reflex responses recovery after preconditioning stimulus observed in migraine patients.
Also Coppola et al. [43] reported that the inhibition of nBR obtained by means of supraorbital or peripheral (index finger) conditioning stimulation is normal in migraineurs interictally, which does exclude the previous hypothesized persistent sensitization in the trigeminal nociceptive system and demonstrate that descending brainstem pathways on medullary R2 interneurones are normal in migraine between attacks [43].
A more recent article [35] has reported that one-third of migraine patients did not have prepulse inhibition of R2 response after conditioning stimulation of the median nerve at wrist. These authors conclude that in migraine there is a loss of sensory modulation at the level of brainstem during and immediately after the attacks.
Other authors [50] reported that migraineurs did not have a significant change in nBR magnitude during a conditioning setting (noxious counterstimulus applied by inducing forearm ischemia), suggesting impaired conditioned pain modulation and, consequently, a deficient inhibition of trigeminal nociception.
In contrast to the evident lack of habituation found in the majority of studies assessing blink reflex responses in common migraine, this deficit is not present in genetic forms of migraine.
In fact, Hansen et al. [51] found that nociceptive BR habituation increased more in familial hemiplegic migraine (FHM-1 and FHM-2) subjects than in subjects with common migraine and controls. These results indirectly suggest that hyperexcitability of cortical neurons, previously demonstrated in the animal model of the FHM-1 and FHM-2 mutations in transgenic mice [52, 53], is not per se responsible for the habituation deficit in the common forms of migraine. Alternatively, in FHM, an increase in cortical inhibitory mechanism might compensate between attacks for the genetically determined increased neuronal excitability. All these results support the concept that various pathophysiologic aspects differ between FHM and common migraine, including cortical and brainstem responsiveness.
Lastly, several authors reported a clear effect (significant modification of blink reflex assessment’s findings) of different substances and pharmacologic and non-pharmacologic treatment of migraine [39, 54,55,56,57].
A recent paper [58] has reported an interesting different effect of ketogenic diet on cortical and brainstem habituation responses.
Also, low-frequency short-time stimulation of the greater occipital nerve seems not to modify nociceptive blink reflex responses [59].
In conclusion, most of the studies assessing blink reflex in migraine show substantial normality of the findings obtained from basal BR recordings in patients and, in many cases, significant and sudden variations of the response patterns only in the periictal phase.
In most of the studies that evaluated habituation and/or conditioning, larger differences are evident in terms of response patterns between migraine and non-migraine subjects. Such habituation anomalies, in almost all the studies, revert in the ictal phase.
The variability of the results in the study of blink reflex in migraine by many authors is a consequence of a series of factors: frequency of crises, proximity of the last crisis or of the next one, side predominance, stimulation modality, and prophylactic treatment.
Therefore, the blink reflex studies demonstrate the dynamic and sudden recurrent unbalance of excitability of all CNS systems (cortical, subcortical, brainstem, hypothalamus, and trigeminal structures).
This unbalance is more evident cyclically near or during a migraine attack, when the habituation deficit normalizes and sensitization of the pain pathways increases.
Finally, BR studies are a suitable tool for testing a drug’s efficacy.
7.4 Auditory Evoked Potentials
Auditory stimuli elicit small electrical potentials can be distinguished into short-, middle-, and long-latency auditory evoked potentials (AEPs), based on their generators in the auditory pathways. Short-latency AEPs originate in brainstem; conversely, middle- and long-latency AEPs originate in the auditory cortex.
For clinical and research studies, a set of five recording channels is recommended, including electrodes Fz, Cz, F3, and F4 of the international 10–20 system, referenced to the linked mastoid processes, but this is rarely conceivable in clinical practice, as many evoked potential recording devices offer no more than two recording channels. Averaging should be performed after an artifact rejection and should include at least 200 responses per condition.
AEPs are a sensitive measure of central nervous system dysfunction [60, 61], particularly of the brainstem. However, the studies of these potentials in migraine has yielded contradictory results [62,63,64] (Table 7.2).
Studies of short-latency AEPs, that is, brainstem auditory evoked responses (BAER), provide varying and heterogeneous results in migraine. Normal latencies [62,63,64,65,66]; increased latencies, especially for wave V [67, 68] mostly during the attacks [62, 65]; and interaural asymmetries [67], particularly in migraine with aura [69] were reported. An inverse correlation between discomfort to stimulations of low intensity (55 dB) and wave IV–V amplitude was found in another study [66].
The rare studies of cortical long-latency auditory evoked potentials showed no significant difference between migraineurs and controls with regard to N1, P2, and N2 component latency or amplitude [68].
Another recent study has confirmed no difference in terms of latency, amplitude, and interpeak of all auditory brainstem components between a group of vestibular migraine and control subjects. The same authors, however, found increased latencies of the frequency following response and lower discomfort thresholds in migraineurs compared to the control group [70].
Only few studies have explored the habituation of cortical AEPs.
The first one reported “potentiation” of N1-P2 amplitude only at high stimulus intensities in migraineurs, contrasting with physiologic habituation in healthy volunteers [71]. This result was not confirmed in another report [66], probably because of methodological differences.
In a successive study [72], the intensity dependence of auditory N1-P2 and habituation for each stimulation intensities was measured and potentiation was found in migraineurs, greater for high-intensity stimulations than for low-intensity stimulations, as opposed to the habituation or absence of amplitude change for all stimulation intensities in controls.
In addition to the study of habituation, another method of dynamic study of auditory evoked potentials consists of the study of sensory “gating.” Gating of sensory input is another characteristic of central processing of incoming information. A typical example of this phenomenon is the suppression of the cortical response to a test stimulus delivered after an identical preceding conditioning stimulus.
The middle-latency P50 component of the auditory evoked cortical potential is very sensitive to gating. Gating of the auditory P50 response was markedly reduced in migraine patients compared to healthy volunteers [73], which was considered an expression of reduced short-term habituation [74].
Another method suitable to assess physiologic CNS responses by means of AEPs is the intensity dependence of AEPs (IDAP), which assesses the amplitude increase of auditory evoked cortical responses with increasing stimulation intensities.
IDAP amplitude was found suddenly increased in migraine between attacks with increasing stimulus intensity [71], reflecting a pronounced intensity dependence of auditory evoked potentials (IDAP), which is likely to reflect reduced central serotonin neurotransmission [75].
The increased IDAP normalizes during the migraine attack [76], as well as during other dynamic changes of CNS excitability.
IDAP abnormalities correlate with personality profiles [77], and some authors interpret this finding with lower serotonergic transmission in migraine, but not in posttraumatic headache [77].
Two independent studies [78, 79] found evidence for a familial effect on IDAP in migraineurs, indicative of a genetic background; however, up to now no direct genetic link has been identified.
These hypotheses are fully confirmed in a recent multicentric study [80]. In this large study, in fact, the intensity dependence of auditory evoked cortical potentials is significantly increased during the interictal phase of migraine [80]. The underlying mechanism of these findings is still under debate and might involve lower preactivation levels of sensory cortices, due to thalamo-cortical dysrhythmia, and low serotonergic tone. Nevertheless, the peculiar abnormalities of both visual and auditory cortical potentials, together, have a high sensitivity and specificity to be considered as an endophenotypic biomarker of migraine.
The results of a previous study by Afra et al. [81], which do not report correlations between PR-VEP and IDAP amplitude-stimulus function slopes in patients with migraine, are partially against these hypothesis.
In conclusion, the studies of basal AEPs in migraine have produced divergent results. However, the dynamic assessment (habituation, gating, and IDAP) widely detects a deficit of habituation or potentiation, with evidence for a genetic-phenotypic correlation.
IDAP is not useful for diagnostic purposes, because of its limited repeatability in pathophysiologic studies [82]. This may be related to the fact that the major part of the IDAP increase in migraine could be due to the AEP habituation deficit at high-intensity stimulations [72].
Recent evidence, however, underlines that, if associated with other neurophysiologic methods, they can become more sensitive and specific in order to distinguish different types of headache [80].
On the other hand, IDAP is certainly suitable in longitudinal (to assess the same subjects at different time points) and pharmacologic studies [83].
7.5 Other Brainstem Reflexes: Nociceptive Flexion Reflex, Corneal Reflex, Jaw-Stretch Reflex, Others
7.5.1 Jaw-Stretch Reflex
Up to now, no study has explored jaw-stretch reflex in migraine.
7.5.2 Nociceptive Flexion Reflex
The stimulation of the sural nerve by means of a pair of surface electrodes, placed on the skin at the retro-malleolar site, evokes muscular response (RIII reflex—nociception flexion reflex) recorded electromyographically from the ipsilateral biceps femoris muscle (capitis brevis). The nociceptive flexion reflex (NFR) is a reliable and objective tool for exploring pain control systems in humans [84]. The threshold and amplitude of the RIII reflex are strictly linked to the threshold and amplitude of the concomitant pain evoked by the electrical stimulus, and the RIII reflex has been reported to be significantly inhibited by the activation of diffuse noxious inhibitory control (DNIC) [84,85,86].
In the older study assessing NFR [87], Sandrini et al. reported a decrease of RIII reflex threshold in severe and evolutive form of migraine and hypothesized, in this clinical condition, an impairment of the serotoninergic antinociceptive system.
In the same way, with an elegant and more recent study, the same authors [88] assessed, in migraine patients, the effects of heterotopic noxious conditioning stimulation (HNCS), in the form of the cold pressor test (CPT), on the NFR. The major finding of this study is that migraine patients showed no inhibition, but there was facilitation of the RIII reflex during the HNCS. The authors conclude that in migraine there is an impairment of supraspinal pain modulation systems that may contribute to the central sensitization.
Other authors [89] described significant fluctuations in the threshold of the nociceptive flexion reflex between the third week of active estrogen treatment and during the hormone-free interval. These fluctuations are more pronounced in women with migraine compared to non-migraineurs (without statistical significance). This “increased sensitivity,” mediated by estrogen withdrawal, was interpreted as the trigger of migraine attacks during the hormone-free interval.
7.5.3 Corneal Reflex
Electrical stimulation by means of a thin cotton thread connected to the cathode of a constant current stimulator, air puff, or direct touch to the cornea elicits a contraction of the orbicularis oculi muscle, defined corneal reflex (CR), similar to the blink reflex response. The muscular response is recorded from the orbicularis oculi using an electrode placed on each side of the inferior lid. In contrast to the BR, the CR has no early ipsilateral R1, but only a late bilateral R2 response [90]. The corneal reflex (CR) is a naturally protective brainstem reflex and allows the investigation of peripheral trigeminal nerve structures.
Few studies evaluated the corneal reflex in migraine.
One study [91] detected a reduction in the CR threshold and an increased sensitivity to tactile and painful stimulation in patients with migraine during the interictal phase, more marked on the symptomatic side. These findings were interpreted as an impairment of the afferent pathways and/or changes in excitability of the trigeminal pain pathway in migraine patients leading to cortical and subcortical hyperexcitability of sensory pathways.
Another study [92] reported no differences in baseline response areas under the curve (AUC) and latencies of the R2 components of CR between patients and controls, or any significant differences concerning the headache side and no significant influence of oral triptans. The authors conclude that there is no facilitation of the trigeminal system in the headache-free interval and that there is no effect of sumatriptan on this facilitation.
7.5.4 Others
Isolated studies used other less-validated methods in order to assess brainstem reflexes. In one of these studies, Duncko et al. [93] found that migraine is associated with a higher acoustic startle responsiveness that is already present in children at risk of developing the disorder.
7.6 Conclusions
Large varieties of neurophysiologic tools and different protocols have been used with the aim of studying the function of the brainstem in migraine.
None of the studies of the brainstem reflexes reveal completely repeatable and exhaustive results in terms of normality or alteration of the responses of migraineurs compared to those obtained from non-migraine subjects.
Therefore, none of these neurophysiologic methods have such a high sensitivity and specificity that they can be considered able to definitively differentiate migraine from other forms of primary or secondary headaches.
Results that are much more homogeneous have been obtained using protocols for the study of the habituation and recovery curves to paired shocks of such reflexes.
Since the brainstem plays a crucial role in the pathogenesis of migraine, the habituation and recovery of curves of brainstem reflexes could provide valuable information about the status of the brainstem in such disorder.
Overall, interictally migraineurs with and without aura show a time-dependent amplitude increase of evoked potentials and reflexes to repeated stereotyped stimuli compared to normal subjects. This phenomenon was called “deficient habituation” or “lack of habituation” and was seen only during the interictal period for almost all sensory modalities. In this view, this phenomenon is considered a neurophysiologic biomarker of migraine.
Nevertheless, the habituation is a dynamic phenomenon, as it changes when incoming an attack, during the attack and when episodic migraine evolves to chronic migraine. Chronic migraine is a complication of migraine where sensitization makes its appearance and change profoundly the response pattern to incoming inputs.
The interictal dysexcitability may be of subcortical (thalamo-cortical) origin or correspond to a primary cortical dysfunction (impaired inhibition due to disrupted excitatory glutamatergic neurotransmission), or can represent the result of coexistence of both phenomena and can occur in variable degrees depending on patients and on the migraine phases (time from the previous or the next attack and frequency of migraine) [94].
As a result, neurophysiologic methods have had and continue to have considerable importance in the study of the pathophysiologic mechanisms underlying migraine, in particular of the neurobiologic mechanisms modulating the processing of information at different levels, above all with regard to the cyclical and sudden variations of excitability of the CNS in critical phase.
The incomplete repeatability of the different study methods, anyway, does not exclude that these methods may be useful in longitudinal studies, that is, in the same subjects during ictal and interictal phase or at different timings of the illness natural history.
Finally, the different ways of studying brainstem reflexes represent an interesting tool useful to test a drug’s efficacy.
References
Schoenen J, Jamart B, Gerard P, Lenarduzzi P, Delwaide PJ. Exteroceptive suppression of temporalis muscle activity in chronic headache. Neurology. 1987;37(12):1834–6.
Cruccu G, Ongerboer de Visser BW. The jaw reflexes. The International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol Suppl. 1999;52:243–7.
Berardelli A, Cruccu G, Kimura J, Ongerboer de Visser BW, Valls-Sole J. The orbicularis oculi reflexes. The International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol Suppl. 1999;52:249–53.
Kimura J. Electrodiagnosis in diseases of nerve and muscle : principles and practice. 2nd ed. Philadelphia, PA: Davis; 1989.
Schoenen J. Wolff award 1992. Exteroceptive suppression of temporalis muscle activity in patients with chronic headache and in normal volunteers: methodology, clinical and pathophysiological relevance. Headache. 1993;33(1):3–17.
Wang W, Schoenen J. Reduction of temporalis exteroceptive suppression by peripheral electrical stimulation in migraine and tension-type headaches. Pain. 1994;59(3):327–34.
Nakashima K, Takahashi K. Exteroceptive suppression of the masseter, temporalis and trapezius muscles produced by mental nerve stimulation in patients with chronic headaches. Cephalalgia. 1991;11(1):23–8.
Schoenen J. Clinical neurophysiology of headache. Neurol Clin. 1997;15(1):85–105.
Zwart JA, Sand T. Exteroceptive suppression of temporalis muscle activity: a blind study of tension-type headache, migraine, and cervicogenic headache. Headache. 1995;35(6):338–43.
Tataroglu C, Kanik A, Sahin G, Ozge A, Yalcinkaya D, Idiman F. Exteroceptive suppression patterns of masseter and temporalis muscles in central and peripheral headache disorders. Cephalalgia. 2002;22(6):444–52.
Aktekin B, Yaltkaya K, Ozkaynak S, Oguz Y. Recovery cycle of the blink reflex and exteroceptive suppression of temporalis muscle activity in migraine and tension-type headache. Headache. 2001;41(2):142–9.
Weiller C, May A, Limmroth V, et al. Brain stem activation in spontaneous human migraine attacks. Nat Med. 1995;1(7):658–60.
Lance JW, Lambert GA, Goadsby PJ, Zagami AS. 5-Hydroxytryptamine and its putative aetiological involvement in migraine. Cephalalgia. 1989;9(Suppl 9):7–13.
Paulus W, Raubuchl O, Straube A, Schoenen J. Exteroceptive suppression of temporalis muscle activity in various types of headache. Headache. 1992;32(1):41–4.
Keidel M, Rieschke P, Juptner M, Diener HC. Pathological jaw opening reflex after whiplash injury. Nervenarzt. 1994;65(4):241–9.
Rossi P, Vollono C, Valeriani M, Sandrini G. The contribution of clinical neurophysiology to the comprehension of the tension-type headache mechanisms. Clin Neurophysiol. 2011;122(6):1075–85.
Goadsby PJ, Hoskin KL. Serotonin inhibits trigeminal nucleus activity evoked by craniovascular stimulation through a 5HT1B/1D receptor: a central action in migraine? Ann Neurol. 1998;43(6):711–8.
Sartucci F, Rossi A, Rossi B. Trigemino cervical reflex in man. Electromyogr Clin Neurophysiol. 1986;26(2):123–9.
Nardone R, Tezzon F. Short latency trigemino-sternocleidomastoid response in patients with migraine. J Neurol. 2003;250(6):725–32.
Nardone R, Ausserer H, Bratti A, et al. Trigemino-cervical reflex abnormalities in patients with migraine and cluster headache. Headache. 2008;48(4):578–85.
Serrao M, Perrotta A, Bartolo M, et al. Enhanced trigemino-cervical-spinal reflex recovery cycle in pain-free migraineurs. Headache. 2005;45(8):1061–8.
Kugelberg E. Facial reflexes. Brain. 1952;75(3):385–96.
Kimura J, Powers JM, Van Allen MW. Reflex response of orbicularis oculi muscle to supraorbital nerve stimulation. Study in normal subjects and in peripheral facial paresis. Arch Neurol. 1969;21(2):193–9.
Shahani BT, Young RR. Human orbicularis oculi reflexes. Neurology. 1972;22(2):149–54.
Csecsei G. Facial afferent fibers in the blink reflex of man. Brain Res. 1979;161(2):347–50.
Hiraoka M, Shimamura M. Neural mechanisms of the corneal blinking reflex in cats. Brain Res. 1977;125(2):265–75.
Kimura J, Lyon LW. Orbicularis oculi reflex in the Wallenberg syndrome: alteration of the late reflex by lesions of the spinal tract and nucleus of the trigeminal nerve. J Neurol Neurosurg Psychiatry. 1972;35(2):228–33.
Kimura J. Electrodiagnosis in diseases of nerve and muscle: principles and practice. Philadelphia, PA: Davis; 1983.
Bank J, Bense E, Kiraly C. The blink reflex in migraine. Cephalalgia. 1992;12(5):289–92.
Yildirim G, Sayin R, Cogen EE, Odabas FO, Tombul T. Randomised, controlled blink reflex in patients with migraine and tension type headache. J Pak Med Assoc. 2011;61(10):978–82.
Sand T, Zwart JA. The blink reflex in chronic tension-type headache, migraine, and cervicogenic headache. Cephalalgia. 1994;14(6):447–50; discussion 394–5.
De Marinis M, Pujia A, Natale L, D'Arcangelo E, Accornero N. Decreased habituation of the R2 component of the blink reflex in migraine patients. Clin Neurophysiol. 2003;114(5):889–93.
De Marinis M, Pujia A, Colaizzo E, Accornero N. The blink reflex in “chronic migraine”. Clin Neurophysiol. 2007;118(2):457–63.
Sand T, Moll-Nilsen B, Zwart JA. Blink reflex R2 amplitudes in cervicogenic headache, chronic tension-type headache and migraine. Cephalalgia. 2006;26(10):1186–91.
Uygunoglu U, Gunduz A, Ertem HD, et al. Deficient prepulse inhibition of blink reflex in migraine and its relation to allodynia. Neurophysiol Clin. 2017;47(1):63–8.
Brooks JB, Fragoso YD. The blink reflex test does not show abnormalities in a large group of patients with chronic migraine. Arq Neuropsiquiatr. 2013;71(11):862–5.
Ayzenberg I, Obermann M, Nyhuis P, et al. Central sensitization of the trigeminal and somatic nociceptive systems in medication overuse headache mainly involves cerebral supraspinal structures. Cephalalgia. 2006;26(9):1106–14.
Avramidis TG, Podikoglou DG, Anastasopoulos IE, Koutroumanidis MA, Papadimitriou AL. Blink reflex in migraine and tension-type headache. Headache. 1998;38(9):691–6.
Kaube H, Katsarava Z, Przywara S, Drepper J, Ellrich J, Diener HC. Acute migraine headache: possible sensitization of neurons in the spinal trigeminal nucleus? Neurology. 2002;58(8):1234–8.
Steffens H, Schomburg ED. Convergence in segmental reflex pathways from nociceptive and non-nociceptive afferents to alpha-motoneurones in the cat. J Physiol. 1993;466:191–211.
Kaube H, Katsarava Z, Kaufer T, Diener H, Ellrich J. A new method to increase nociception specificity of the human blink reflex. Clin Neurophysiol. 2000;111(3):413–6.
Katsarava Z, Lehnerdt G, Duda B, Ellrich J, Diener HC, Kaube H. Sensitization of trigeminal nociception specific for migraine but not pain of sinusitis. Neurology. 2002;59(9):1450–3.
Coppola G, Di Clemente L, Fumal A, et al. Inhibition of the nociceptive R2 blink reflex after supraorbital or index finger stimulation is normal in migraine without aura between attacks. Cephalalgia. 2007;27(7):803–8.
Sohn JH, Kim CH, Choi HC. Differences in central facilitation between episodic and chronic migraineurs in nociceptive-specific trigeminal pathways. J Headache Pain. 2016;17:35.
Katsarava Z, Giffin N, Diener HC, Kaube H. Abnormal habituation of ‘nociceptive’ blink reflex in migraine—evidence for increased excitability of trigeminal nociception. Cephalalgia. 2003;23(8):814–9.
Di Clemente L, Coppola G, Magis D, Fumal A, De Pasqua V, Schoenen J. Nociceptive blink reflex and visual evoked potential habituations are correlated in migraine. Headache. 2005;45(10):1388–93.
Di Clemente L, Coppola G, Magis D, et al. Interictal habituation deficit of the nociceptive blink reflex: an endophenotypic marker for presymptomatic migraine? Brain. 2007;130(Pt 3):765–70.
Perrotta A, Anastasio MG, De Icco R, et al. Frequency-dependent habituation deficit of the nociceptive blink reflex in aura with migraine headache. Can migraine aura modulate trigeminal excitability? Headache. 2017;57(6):887–98.
de Tommaso M, Murasecco D, Libro G, et al. Modulation of trigeminal reflex excitability in migraine: effects of attention and habituation on the blink reflex. Int J Psychophysiol. 2002;44(3):239–49.
Williams AE, Miller MM, Bartley EJ, McCabe KM, Kerr KL, Rhudy JL. Impairment of inhibition of trigeminal nociception via conditioned pain modulation in persons with migraine headaches. Pain Med. 2019;20(8):1600–10.
Hansen JM, Bolla M, Magis D, et al. Habituation of evoked responses is greater in patients with familial hemiplegic migraine than in controls: a contrast with the common forms of migraine. Eur J Neurol. 2011;18(3):478–85.
Pietrobon D. Familial hemiplegic migraine. Neurotherapeutics. 2007;4(2):274–84.
Tottene A, Conti R, Fabbro A, et al. Enhanced excitatory transmission at cortical synapses as the basis for facilitated spreading depression in ca(v)2.1 knockin migraine mice. Neuron. 2009;61(5):762–73.
de Tommaso M, Guido M, Libro G, Sciruicchio V, Puca F. Zolmitriptan reverses blink reflex changes induced during the migraine attack in humans. Neurosci Lett. 2000;289(1):57–60.
Katsarava Z, Limmroth V, Baykal O, Akguen D, Diener HC, Kaube H. Differences of anti-nociceptive mechanisms of migraine drugs on the trigeminal pain processing during and outside acute migraine attacks. Cephalalgia. 2004;24(8):657–62.
de Tommaso M, Delussi M. Nociceptive blink reflex habituation biofeedback in migraine. Funct Neurol. 2017;32(3):123–30.
Watson DH, Drummond PD. Cervical referral of head pain in migraineurs: effects on the nociceptive blink reflex. Headache. 2014;54(6):1035–45.
Di Lorenzo C, Coppola G, Bracaglia M, et al. A ketogenic diet normalizes interictal cortical but not subcortical responsivity in migraineurs. BMC Neurol. 2019;19(1):136.
Jurgens TP, Busch V, Opatz O, Schulte-Mattler WJ, May A. Low-frequency short-time nociceptive stimulation of the greater occipital nerve does not modulate the trigeminal system. Cephalalgia. 2008;28(8):842–6.
Chiappa KH. Evoked potentials in clinical medicine. 2nd ed. New York, NY: Raven Press; 1990.
Sand T. Clinical correlates of brain-stem auditory evoked potential variables in multiple sclerosis. Relation to click polarity. Electroencephalogr Clin Neurophysiol. 1991;80(4):292–7.
Podoshin L, Ben-David J, Pratt H, et al. Auditory brainstem evoked potentials in patients with migraine. Headache. 1987;27(1):27–9.
Battistella PA, Suppiej A, Casara G, et al. Brainstem auditory evoked potentials (BAEPs) in childhood migraine. Headache. 1988;28(3):204–6.
Benna P, Bianco C, Costa P, Piazza D, Bergamasco B. Visual evoked potentials and brainstem auditory evoked potentials in migraine and transient ischemic attacks. Cephalalgia. 1985;5(Suppl 2):53–8.
Yamada T, Dickins QS, Arensdorf K, Corbett J, Kimura J. Basilar migraine: polarity-dependent alteration of brainstem auditory evoked potential. Neurology. 1986;36(9):1256–60.
Sand T, Vingen JV. Visual, long-latency auditory and brainstem auditory evoked potentials in migraine: relation to pattern size, stimulus intensity, sound and light discomfort thresholds and pre-attack state. Cephalalgia. 2000;20(9):804–20.
Bussone G, Sinatra MG, Boiardi A, La Mantia L, Frediani F, Cocchini F. Brainstem auditory evoked potentials in migraine patients in basal conditions and after chronic flunarizine treatment. Cephalalgia. 1985;5(Suppl 2):177–80.
Drake ME, Pakalnis A, Hietter SA, Padamadan H. Visual and auditory evoked potentials in migraine. Electromyogr Clin Neurophysiol. 1990;30(2):77–81.
Schlake HP, Grotemeyer KH, Hofferberth B, Husstedt IW, Wiesner S. Brainstem auditory evoked potentials in migraine—evidence of increased side differences during the pain-free interval. Headache. 1990;30(3):129–32.
Takeuti AA, Favero ML, Zaia EH, Gananca FF. Auditory brainstem function in women with vestibular migraine: a controlled study. BMC Neurol. 2019;19(1):144.
Wang W, Timsit-Berthier M, Schoenen J. Intensity dependence of auditory evoked potentials is pronounced in migraine: an indication of cortical potentiation and low serotonergic neurotransmission? Neurology. 1996;46(5):1404–9.
Ambrosini A, Rossi P, De Pasqua V, Pierelli F, Schoenen J. Lack of habituation causes high intensity dependence of auditory evoked cortical potentials in migraine. Brain. 2003;126(Pt 9):2009–15.
Ambrosini A, De Pasqua V, Afra J, Sandor PS, Schoenen J. Reduced gating of middle-latency auditory evoked potentials (P50) in migraine patients: another indication of abnormal sensory processing? Neurosci Lett. 2001;306(1–2):132–4.
Siniatchkin M, Kropp P, Gerber WD. What kind of habituation is impaired in migraine patients? Cephalalgia. 2003;23(7):511–8.
Hegerl U, Juckel G. Intensity dependence of auditory evoked potentials as an indicator of central serotonergic neurotransmission: a new hypothesis. Biol Psychiatry. 1993;33(3):173–87.
Judit A, Sandor PS, Schoenen J. Habituation of visual and intensity dependence of auditory evoked cortical potentials tends to normalize just before and during the migraine attack. Cephalalgia. 2000;20(8):714–9.
Wang W, Wang YH, Fu XM, Sun ZM, Schoenen J. Auditory evoked potentials and multiple personality measures in migraine and post-traumatic headaches. Pain. 1999;79(2–3):235–42.
Sandor PS, Afra J, Ambrosini A, Schoenen J. Prophylactic treatment of migraine with beta-blockers and riboflavin: differential effects on the intensity dependence of auditory evoked cortical potentials. Headache. 2000;40(1):30–5.
Siniatchkin M, Kropp P, Neumann M, Gerber W, Stephani U. Intensity dependence of auditory evoked cortical potentials in migraine families. Pain. 2000;85(1–2):247–54.
Ambrosini A, Kisialiou A, Coppola G, et al. Visual and auditory cortical evoked potentials in interictal episodic migraine: an audit on 624 patients from three centres. Cephalalgia. 2017;37(12):1126–34.
Afra J, Proietti Cecchini A, Sandor PS, Schoenen J. Comparison of visual and auditory evoked cortical potentials in migraine patients between attacks. Clin Neurophysiol. 2000;111(6):1124–9.
Sandor PS, Roon KI, Ferrari MD, van Dijk JG, Schoenen J. Repeatability of the intensity dependence of cortical auditory evoked potentials in the assessment of cortical information processing. Cephalalgia. 1999;19(10):873–9.
Roon KI, Sandor PS, Schoonman GG, et al. Auditory evoked potentials in the assessment of central nervous system effects of antimigraine drugs. Cephalalgia. 1999;19(10):880–5.
Skljarevski V, Ramadan NM. The nociceptive flexion reflex in humans – review article. Pain. 2002;96(1–2):3–8.
Willer JC, Bouhassira D, Le Bars D. Neurophysiological bases of the counterirritation phenomenon:diffuse control inhibitors induced by nociceptive stimulation. Neurophysiol Clin. 1999;29(5):379–400.
Willer JC, Roby A, Le Bars D. Psychophysical and electrophysiological approaches to the pain-relieving effects of heterotopic nociceptive stimuli. Brain. 1984;107(Pt 4):1095–112.
Sandrini G, Martignoni E, Micieli G, Alfonsi E, Sances G, Nappi G. Pain reflexes in the clinical assessment of migraine syndromes. Funct Neurol. 1986;1(4):423–9.
Sandrini G, Rossi P, Milanov I, Serrao M, Cecchini AP, Nappi G. Abnormal modulatory influence of diffuse noxious inhibitory controls in migraine and chronic tension-type headache patients. Cephalalgia. 2006;26(7):782–9.
De Icco R, Cucinella L, De Paoli I, et al. Modulation of nociceptive threshold by combined hormonal contraceptives in women with oestrogen-withdrawal migraine attacks: a pilot study. J Headache Pain. 2016;17(1):70.
Thatcher DB, Van Allen MW. Corneal reflex latency. Neurology. 1971;21(7):735–7.
Sandrini G, Proietti Cecchini A, Milanov I, Tassorelli C, Buzzi MG, Nappi G. Electrophysiological evidence for trigeminal neuron sensitization in patients with migraine. Neurosci Lett. 2002;317(3):135–8.
Busch V, Kaube S, Schulte-Mattler W, Kaube H, May A. Sumatriptan and corneal reflexes in headache-free migraine patients: a randomized and placebo-controlled crossover study. Cephalalgia. 2007;27(2):165–72.
Duncko R, Cui L, Hille J, Grillon C, Merikangas KR. Startle reactivity in children at risk for migraine. Clin Neurophysiol. 2008;119(12):2733–7.
Magis D, Lisicki M, Coppola G. Highlights in migraine electrophysiology: are controversies just reflecting disease heterogeneity? Curr Opin Neurol. 2016;29(3):320–30.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Vollono, C. (2021). Brainstem Reflexes. In: Coppola, G., Chen, WT. (eds) Neurophysiology of the Migraine Brain. Headache. Springer, Cham. https://doi.org/10.1007/978-3-030-56538-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-56538-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-56537-4
Online ISBN: 978-3-030-56538-1
eBook Packages: MedicineMedicine (R0)