Abstract
The diagnosis of bladder pain syndrome/interstitial cystitis (BPS/IC) is substantially clinical, according to the ESSIC definition. After clinical suspicion, it is mandatory to exclude confusable diseases and identify phenotypical aspects of the disease. There are different severity grades, involved organs, possible allergies, and impact on quality of life. Some of these aspects can vary in the natural history of disease as well as after treatment. To facilitate a diagnostic pathway and follow-up, we suggest a standardized system. We elaborated a chart with 12 items, each considering a peculiar aspect/domain of the disease: micturition diary, Visual Analogue Scale (VAS), presence of pelvic/systemic pain, symptom prevalence (pain/LUTS), validated questionnaires, associated pathologies, allergies and intolerances, ESSIC classification, bladder anatomical capacity, and pelvic floor involvement. The grid is proposed to be a simple and immediate instrument to characterize the clinical picture and follow the variations over time.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bladder pain syndrome
- Interstitial cystitis
- Standardized evaluation system
- Diagnostic pathway
- Follow-up pathway
The most accepted definition of bladder pain syndrome (BPS) was given by the International Society for the Study of Interstitial Cystitis (ESSIC): chronic pelvic pain, pressure or discomfort of greater than 6 months duration perceived to be related to the urinary bladder accompanied by at least one other urinary symptom like persistent desire to void or urinary frequency [1]. The diagnosis is often achieved after exclusion of confusable diseases as the cause of the symptoms. There is no clinical evidence about the possible relationship between duration of symptoms and possible early spontaneous resolution of symptoms. While ESSIC definition uses a 6 months duration of symptoms, the American Urological Association Guideline indicates that 6 weeks is enough [2]. The 6th International Consultation on Incontinence does not give a specific recommendation and states that it is up to the discretion of the physician and patient as to the proper interval between symptom onset and evaluation and diagnosis of a chronic condition [3].
The scientific committee of the International Consultation on Incontinence indicated the term “bladder pain syndrome” for the disorder that has been commonly referred to as interstitial cystitis (IC), avoiding the term painful bladder syndrome. The term IC is used to indicate an inflammation involving the bladder walls.
The term bladder pain syndrome is in accordance with the taxonomy of the International Association for the Study of Pain (IASP) and focuses well on the actual symptom complex. Bladder pain syndrome, as previously stated, indicates the presence of persistent or recurrent pain perceived in the sovrapubic region, accompanied by at least one other symptom, such as pain worsening with bladder filling and daytime and/or nighttime urinary frequency. The diagnosis implies the absence of proven infection or other obvious local pathology. Bladder pain syndrome is often associated with negative cognitive, behavioral, sexual, or emotional consequences. The Consultation suggests that the presence of the characteristic Hunner lesions should be considered a distinct disease, with a clinical different response to local treatment; moreover there is lack of evidence that non-Hunner bladder may develop Hunner lesions. The Consultation suggests to consider the Hunner lesions in symptomatic patients as “interstitial cystitis,” thus indicating a true interstitial inflammation. To date, Hunner lesions may be considered as a distinct phenotype, but in the future, they may be classified as a separate disorder entirely, even though local symptoms may make it difficult to differentiate from bladder pain syndrome in the absence of endoscopy [3].
The diagnosis of BPS/IC is substantially clinical, according to the ESSIC definition [1]. After clinical suspicion, it is mandatory to exclude confusable diseases and identify phenotypical aspects of the disease. There are different severity grades, involved organs, possible allergies, and impact on quality of life. Some of these aspects can vary in the natural history of disease as well as after treatment. Patients affected by this disease have often stories that lasted for many years, carried out numerous tests and treatments. It is not always so easy to extrapolate the most important data from such complex stories. For male patients in whom bladder pain syndrome is mainly represented by chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) it is already available a clinical phenotyping system called UPOINTs, proposed by Shoskes for the tailored management of the pathology [4]. The system profiles patients in six qualitative clinical domains involved in the syndrome and indicates individual treatment targets. UPOINTs is an acronym standing for: Urinary, Psychosocial, Organ specific, Infection, Neurologic/Systemic, Tenderness and Sexual Dysfunction [5]. Traditional approach to manage CP/CPPS (i.e., monotherapy with alpha-blockers, antimuscarinics, phosphodiesterase type 5 inhibitors, and antibiotics) while working for some patents has failed in many patients diagnosed with this condition. Since no single management pathway is suitable for all patients, they should be managed according to their individual symptom pattern. This has led to the phenotypic multimodal approach using UPOINTs system. Although the validation of this approach is continuing, several studies confirmed the validity and applicability of the UPOINTs algorithm for the patient-tailored diagnosis and therapy of CP/CPPS [6]. Even if this approach has been extrapolated for IC/BPS by Nickel et al. [7], up-to-date there is no evidence about the validation of the UPOINTs method on BPS/IC.
To facilitate a diagnostic pathway and follow-up, we propose a standardized system dedicated to BPS/IC.
We elaborated a chart with 12 items, each considering a peculiar aspect/domain of the disease: voiding diary, Visual Analogue Scale (VAS), presence of pelvic/systemic pain, prevalence symptom (pain/LUTS), validated questionnaires, associated pathologies, allergies and intolerances, ESSIC classification, bladder anatomical capacity, and pelvic floor involvement (Fig. 6.1).
The first item (Fig. 6.1a) of the chart contains information from 3-days voiding diaries, including daytime frequency, nighttime frequency, and functional capacity. By definition such urinary symptoms are always present in these patients and improvement of these symptoms is a goal of the treatment [1]. The voiding diary highlights the urinary symptom that may have varying severity over time; sometimes a certain treatment acts more on urinary symptoms than on pain.
The second item (Fig. 6.1b) is represented by pain that represents the cardinal symptom of the pathology. We propose the use of the Visual Analogue Scale (VAS) to evaluate pain. The VAS allows to measure it and monitor changes during treatment.
The third box (Fig. 6.1c) analyzes the prevalence of pain with respect to lower urinary tract symptoms (LUTS). Sometimes the pain is exclusively pelvic and, in some cases, it involves other districts. Pain and LUTS can be variously represented in different cases. Sometimes pain symptoms prevail over LUTS, sometimes LUTS are the prevailing symptoms. Knowing this prevalence contributes in deciding proper treatment. Often, after treatment, this relationship changes. For example, pain may be reduced, but LUTS may remain: in this case LUTS treatment becomes a new goal.
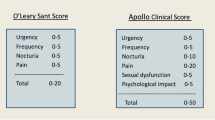
The second line (Fig. 6.1d,e,f) is dedicated to the different validated questionnaires for the pathology. They are important to quantify the impact on quality of life and to numerically express the results of therapy. We included the most relevant questionnaires: Pelvic Pain Urgency Frequency questionnaire (PUF) [8], O’Leary Saint Interstitial Cystitis (Symptom Index and Problem index) [9], Quality of Life questionnaire (QoL), Personal Global Impression of Improvement (PGI-I).
The third line (Fig. 6.1g,h,i) allows to investigate all the comorbidities (Table 6.1), the possible allergies and intolerances, often present in these patients. These data are important to put the suspicion on comorbidity in order to request the intervention of the right specialists for a specific case. This is useful to obtain a multidisciplinary management of the disease. For example, due to the diet-sensitive nature of BCS/IC, the finding of alimentary problems can recommend the intervention of a nutritionist specialist.
The first record of the last line (Fig. 6.1j) is dedicated to the ESSIC classification [1], i.e., to endoscopic and histological phenotyping (Table 6.2). Even if its role is controversial, it is the only phenotyping tool available to date. In this way, the grid allows to relate the phenotype to the different clinical aspects recorded in the previous items. The aim of this item may allow to address a tailored treatment on the basis of the endoscopic and histological phenotype.
The second record of the last line (Fig. 6.1k) evaluates bladder capacity under anesthesia. This data is obtained from cystoscopy with hydrodistention at 80cmH2O filling pressure, which is considered important in the evaluation of disease. In this regard, it is important to identify patients with a significant reduction in anatomical bladder capacity that typically respond purely to standard treatments. In some cases, a significant reduction is an indication to perform a bladder augmentation surgery.
The last record (Fig. 6.1l) is dedicated to the involvement of pelvic floor. Many patients exhibit hypertonia and vaginal trigger points with varying grades of severity. These data can be useful to start a correct pelvic floor rehabilitation. In the event of significant anomalies noticed in this area, it will be advisable to request the intervention of a physiatrist.
The grid was created to be a simple and rapid tool to characterize the clinical picture and follow variations over time. Following each item of the chart, it is easy to collect all necessary information about the disease and have a global view of the clinical condition. The use of the grid during follow-up made it very easy to highlight changes in any item.
Another interesting aspect is the possibility to identify a relationship between ESSIC phenotype, clinical manifestations, and response to different therapies. For example, it may be useful to understand why some patients respond to bladder instillations and others to oral therapy alone, or the impact of rehabilitative treatment.
By this grid we suggest a standardized method to the clinical approach, collecting useful information for clinical classification and management of the disease. In our opinion, the grid could represent a methodological guidance in the approach to the pathology.
References
van de Merwe JP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M, Daha LK, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008;53(1):60–7.
Hanno PM, Burks DA, Clemens JQ, Dmochowski RR, Erickson D, Fitzgerald MP, Forrest JB, Gordon B, Gray M, Mayer RD, Newman D, Nyberg L Jr, Payne CK, Wesselmann U, Faraday MM, Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011;185(6):2162–70.
Incontinence, 6th Edition 2017, 6th International Consultation on Incontinence, Tokyo September 2016.
Shoskes DA, Nickel JC. Classification and treatment of men with chronic prostatitis/chronic pelvic pain syndrome using the UPOINT system. World J Urol. 2013;31(4):755–60. https://doi.org/10.1007/s00345-013-1075-6. Epub 2013 Apr 16
Magri V, Wagenlehner F, Perletti G, Schneider S, Marras E, Naber KG, Weidner W. Use of the UPOINT chronic prostatitis/chronic pelvic pain syndrome classification in European patient cohorts: sexual function domain improves correlations. J Urol. 2010;184(6):2339–45.
Shoskes DA, Nickel JC, Rackley RR, Pontari MA. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009;12(2):177–83.
Nickel JC, Shoskes D, Irvine-Bird K. Clinical phenotyping of women with interstitial cystitis/painful bladder syndrome (IC/PBS): a key to classification and potentially improved management. J Urol. 2009;182:155–60.
Brewer ME, White WM, Klein FA, Klein LM, Waters WB. Validity of pelvic pain, urgency, and frequency questionnaire in patients with interstitial cystitis/painful bladder syndrome. Urology. 2007;70(4):646–9.
Lubeck DP, Whitmore K, Sant GR, Alvarez-Horine S, Lai C. Psychometric validation of the O'leary-Sant interstitial cystitis symptom index in a clinical trial of pentosan polysulfate sodium. Urology. 2001;57(6 Suppl 1):62–6.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Giammò, A., Ammirati, E. (2021). Bladder Pain Syndrome/Interstitial Cystitis (BPS/IC): A New Standardized Evaluation System. In: Giammò, A., Biroli, A. (eds) Chronic Pelvic Pain and Pelvic Dysfunctions. Urodynamics, Neurourology and Pelvic Floor Dysfunctions. Springer, Cham. https://doi.org/10.1007/978-3-030-56387-5_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-56387-5_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-56386-8
Online ISBN: 978-3-030-56387-5
eBook Packages: MedicineMedicine (R0)