Abstract
Hairy cell leukemia (HCL) is a rare chronic B-cell neoplasm characterized by marked splenomegaly, progressive pancytopenia, and reactive marrow fibrosis. The annual incidence of HCL is estimated to be 0.3 cases per 100,000. Diagnosis is made by a review of peripheral blood smear, flow cytometry, and bone marrow biopsy. The hairy cells have a typical pattern of B-cell antigen expression (CD19, CD20) and coexpression of CD11c, CD25, and CD103. Recently, the BRAF-V600E mutation has been described as a disease-defining genetic event. Purine nucleoside analogs, cladribine and pentostatin, are the drugs of choice in the treatment of HCL. Recently, immunotoxin moxetumomab pasudotox has been approved by FDA for the treatment of patients with relapsed or refractory HCL. Vemurafenib, which inhibits the BRAF-V600E mutant, exhibits remarkable activity in multiply relapsed and refractory patients with classic HCL.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- BRAF
- Cladribine
- Dabrafenib
- Ibrutinib
- Immunotoxins
- Hairy cell leukemia
- HCL variant
- Moxetumomab pasudotox
- Pentostatin
- Rituximab
- Vemurafenib
1 Introduction


Hairy cell leukemia (HCL) is a rare type of chronic lymphoid leukemia originated from a mature B lymphocyte [1, 2]. The disease was first described by Bertha Bouroncle in 1958 [3]. HCL is characterized by progressive pancytopenia, splenomegaly, and infiltrations of the bone marrow, liver, and spleen. In addition to the classic form of HCL, the World Health Organization (WHO) now recognizes HCL variant (HCL-V) as a provisional entity distinct from classic HCL; it is regarded as an unclassifiable splenic B-cell leukemia/lymphoma, together with splenic diffuse red pulp small B-cell lymphoma (SDRPL) [4, 5]. However, the relationship between SDRPL and HCL-V remains unclear. HCL-V was first described in 1980 by Cawley et al. [6]. The disease is characterized by splenomegaly, lymphocytosis, and hypercellular bone marrow. In comparison to classic HCL, patients with HCL-V are often older, present with lymphocytosis, and are resistant to purine nucleoside analogs. Biologically, HCL-V is more closely related to splenic lymphomas and shares several overlapping clinical and morphological features with other disorders characterized by villous circulating cells. In the last three decades, tremendous progress in the biology and treatment of classic HCL and HCL-V has been made, which has resulted in an improvement in overall life expectancy and quality of life, mainly due to the introduction of purine nucleoside analogs, cladribine and pentostatin, as well as supportive care regimens. Thanks to the use of these drugs, classic HCL has evolved from a disease with poor prognosis to a highly treatable disorder and affords near-normal survival [7]. HCL-V has usually poorer prognosis than classic HCL.
2 Epidemiology
Hairy cell leukemia (HCL) is a rare mature B-cell malignancy with an incidence of 0.3 cases per 100,000 individuals and is four times more common in men than women [8]. It predominantly occurs in elderly patients with a median age of 49–51 years at initial diagnosis, but younger patients are also affected. These young patients with HCL have shorter responses to treatment and require more lines of therapy to maintain disease control while attaining similar long-term survival [9]. HCL-V is estimated to be 0.2 cases per 100,000 and the disease comprises 2% of all leukemias [8].
3 Molecular Biology and Pathogenesis
During recent years, many new discoveries have revolutionized the molecular understanding of HCL [10]. In 2011, Tiacci et al. discovered that classical HCL is characterized by a gain-of-function mutation of the BRAF serine/threonine protein kinase (V600E) [11, 12]. In the initial validation series, all HCL patients showed this particular mutation; however, a set of 195 B-cell lymphomas and leukemias did not harbor a mutated BRAF gene. The vast majority of BRAF-V600E mutations in HCL are heterozygous, but while homozygous mutations are rare, they have been suggested to be associated with a more aggressive disease course [13]. Recurrent deletions of the BRAF gene locus on chromosome 7q34 have been described in HCL and lead to loss of heterozygosity [14]. BRAF mutations, different from V600E, seem to be extremely rare in HCL and have been described in only two patients so far [15]. The incidence of BRAF mutations in nearly 100% HCL cases at diagnosis, i.e., encompassing the whole disease spectrum, their somatic nature, and presence in the entire tumor clone, as well as their high stability at relapse, strongly suggests that the pathogenesis of HCL critically depends on constitutively activated BRAF [11, 12, 16].
Chung et al. report that BRAF-V600E mutations are already present in hematopoietic stem cells (HSCs) or B-cell lymphoid progenitors of HCL patients and that these patients exhibit marked alterations in hematopoietic stem/progenitor cell (HSPC) frequencies [17]. Transplantation of BRAF-V600E-mutant HSCs from an HCL patient into immunodeficient mice resulted in stable engraftment of BRAF-V600E-mutant human hematopoietic cells, highlighting the functional self-renewal capacity of HCL HSCs. However, none of the transplanted mice developed a typical HCL, strongly suggesting that the development of a full HCL phenotype may require a permissive epigenetic background, likely restricted to a particular stage of B-cell differentiation, and/or the acquirement of further genetic lesions.
The BRAF-V600E mutation constitutively activates BRAF providing oncogenic signaling through the MEK-ERK cascade [11]. Both in vitro and in vivo studies have demonstrated that BRAF-dependent phospho-ERK activation is a critical signaling event in HCL. Moreover, in vitro treatment of primary purified HCL cells with BRAF and MEK inhibitors has resulted in the marked dephosphorylation of MEK/ERK, silencing of the RAF-MEK-ERK pathway transcriptional output, loss of the specific HCL gene expression profile signature, change of the characteristic morphology of the leukemic cells (from “hairy” to “smooth”), and eventual apoptosis [18].
Aberrant expression of cell cycle-related proteins such as cyclin D1 have been shown to be reversible using inhibitors of activated BRAF signaling, suggesting that expression is not a constitutive disease trait but elicited by MEK/ERK signaling and oncogenic BRAF mutations, respectively. This concept may have important consequences for minimal residual disease (MRD) assessment in the context of inhibitor treatment, as the marker profile (cyclin D1) could be dynamic, as well as for targeted drug treatment, which may be curtailed by the on-target effect of inhibitors.
In addition to the BRAF-V600E mutation, the most common genetic alteration in classical HCL was a loss in copy number for chromosome 7q. The minimally deleted region of this copy number alteration includes the wild-type locus of BRAF. This genetic lesion subdivides classical HCL into those with hemizygous versus those with heterozygous mutations of BRAF [12]. Whole exome sequencing study of relapsed and refractory HCL patients revealed known cancer-associated genes such as EZH2 and ARID1A, as well as novel inactivating mutations of the cell cycle inhibitor CDKN1B (p27). In a cohort of 81 mostly untreated HCL patients, the incidence of CDKN1B mutations was 16% [19]. While a clinical impact of CDKN1B mutations was not found, CDKN1B was found to be the second most commonly mutated gene in HCL. CDKN1B is a critical element in cell cycle control and a known tumor suppressor in different solid cancers [20].
CDKN1B prevents the activation of cyclin E-CDK2 or cyclin D-CDK4 complexes and therefore regulates cell cycle progression in the G1 phase. Interestingly, BRAF-induced senescence in premalignant nevi is circumvented by deletion or mutation of CDKN2A in invasive melanoma. In BRAF-mutated hairy cell leukemia, CDKN1B loss may serve as a mechanism to escape oncogene-induced senescence [21]. In addition to CDKN1B, mutations cooperating with BRAF-V600E, recurrent, inactivating mutations in KMT2C (MLL3) were identified in 15% and 13% of classical HCL and HCL variant, respectively [12]. Another study described somatic mutations or deletions of the Krüppel-like factor 2 (KLF2) in 4 of 24 (16%) HCL patients examined, but KLF2 mutations are more frequent in other B-cell malignancies, such as SMZL (31%), and diffuse large B-cell lymphoma (26%). Although better descriptions of the genetic landscape of HCL have been obtained during recent years, the function of mutations cooperating with BRAF-V600E remains to be elucidated.
4 Differential Diagnosis
Historically, there were two different forms of HCL, the more common classical HCL (90%) and the less frequent HCL-V (10%). HCL-V is characterized by a more aggressive disease course and a poor response to purine analogs [22]. Most importantly, HCL-V cases are commonly negative for BRAF-V600E mutation. A small subset of patients with bona fide classical HCL but who also do not harbor any BRAF mutation has been reported but only in a single study [23]. However, these cases are often characterized by an IGHV4-34 immunoglobulin rearrangement, which is generally absent in classic HCL, and it is associated with a similar poor prognosis as HCL-V.
Almost 50% of HCL-V and IGHV4-34-expressing HCL cases were found to harbor activating mutations in the MAP2K1 gene encoding MEK1. All but one of the identified mutations (n = 15) have been described and are known to strongly increase phospho-ERK levels and, consequently, cell proliferation [24]. These findings underline the importance of constitutive MEK-ERK signaling even in this HCL-like disorder.
HCL cells typically show a distinctive immunophenotype coexpressing CD19, CD20, CD11c, CD25, CD103, and CD123. In contrast, HCL-V cells lack the expression of CD25 and CD123 [25]. Moreover, HCL cells strongly express CD200, which can also be used as another distinctive marker to differentiate HCL [26]. BRAF-V600E is now regarded as a specific oncogenic mutation occurring only in HCL [27]. Another distinctive feature of HCL is the expression of annexin A1, which is easily accessible by immunohistochemical staining [28]. In addition to HCL-V, the 2016 revision of the WHO classification of lymphoid neoplasms recognizes two provisional entities resembling HCL: splenic marginal zone lymphoma (SMZL), usually associated with NOTCH2 mutations, and splenic diffuse red pulp small B-cell lymphoma (SDRPBCL) whose genomic landscape has not been yet clarified. Table 12.1 summarizes the most important differential diagnosis of HCL and their characteristic markers.
Testing for BRAF-V600E mutation can be helpful as an additional marker in routine clinical practice if there is any diagnostic uncertainty. For relapsed and refractory patients, we strongly recommend evaluating BRAF mutation status, since this may serve as therapeutic target. The limited number of HCL cells present in the peripheral blood requires highly sensitive molecular assays to detect BRAF mutations (e.g., allele-specific polymerase chain reaction). Alternatively, BRAF-V600E mutation-specific antibodies can be used for immunohistochemical staining in bone marrow biopsies [5]. However, further validation of the diagnostic utility of these reagents in a larger number of cases is required.
5 Prognosis
Hairy cell leukemia belongs to the group of indolent lymphoid malignancies. Standard treatment with purine analogs induces complete remission in more than 80% of patients with classical hairy cell leukemia. If complete remission is achieved, the median time to next treatment is more than 10 years [29]. In case of a partial remission, patients have a significantly shorter treatment-free interval of only 3 years. If retreatment is necessary, and a subsequent complete remission can be achieved, patients with classical hairy cell leukemia enjoy again a very long treatment-free interval of more than 10 years [29]. However, the proportion of patients who achieve a CR decreases with each treatment round. Altogether, it has been shown that many classical hairy cell leukemia patients have an overall survival which is comparable with the normal population. Even younger patients with hairy cell leukemia, who tend to have shorter treatment-free intervals, seem to have a very good long-term outcome [9]. It is important to note that in contrast to classical HCL, it has been found that HCL-V and HCL with VH4-34 gene usage have a considerably poorer response and long-term outcome [30].
6 Treatment Response Evaluation and Disease Progression
Treatment response criteria are defined according the consensus guidelines and ESMO guidelines [1, 2]. Complete remission (CR) required morphologic absence of hairy cells on peripheral blood (PB) and bone marrow (BM) aspiration or biopsy specimens and normalization of organomegaly and peripheral blood counts. Patients in CR should have near normalization of peripheral blood counts including hemoglobin >11 g/dL, platelets >100,000/μL, and an absolute neutrophil count >1500/μL. It is recommended that an assessment for CR following cladribine should be performed 4–6 months after treatment, and at this time a BM biopsy should be performed to document a CR. A partial response (PR) is described as normalization of PB counts, with at least 50% reduction in organomegaly and bone marrow hairy cells and below 5% of circulating hairy cells. All other outcomes are considered as nonresponse. Patients with a CR demonstrate longer remission duration and longer survival than those achieving a PR [31]. Relapse is defined as deterioration in blood counts related to the detection of hairy cells in PB and/or BM and/or increasing splenomegaly. Progressive disease is defined by a 25% decrease in PB hematologic parameters that lasts for 2 months or more or an increase in the hairy cell infiltration of the BM [1]. In addition, 25% increase in either the size of the spleen or the liver based on the nadir measurements achieved following therapy is consistent with disease progression.
The evaluation of minimal residual disease (MRD) in HCL remains controversial and is generally not recommended in routine clinical practice. Preliminary studies indicate that the extent of MRD may predict the duration of remission. For quantitative evaluation of MRD, immunohistochemical staining of the BM core biopsy for CD20, DBA.44, VE-1, or CD79a may be useful. However, the level of disease involvement for MRD negativity is not yet established. Some authors indicate that risk of relapse is low if immunohistochemical staining reveals an MRD level below 1% and high if MRD is greater than 5% positive cells in the BM [32]. In another study, the PB-MRD panel consisted of 2 four-color tubes, including CD19, CD11c, CD25, CD22, and CD103 antigens, or 2 six-color tubes with the addition of CD123 and CD200 [33]. The sensitivity of this test was established as 0.01% and remained constant over the entire period of observation. This study has confirmed that patients with PB-MRD negativity at 6 months (0.01% cutoff) have a low probability of disease relapse. However, further studies are needed to establish the predictive value of PB flow cytometric monitoring for MRD relapse.
7 Treatment of Newly Diagnosed Patients with Classic HCL
Similarly to other indolent lymphoid malignancies, a “watch and wait” strategy is recommended in HCL patients asymptomatic at diagnosis. Approximately 10% of HCL patients do not require immediate therapy after diagnosis, and they should be monitored until treatment is indicated. Treatment should be initiated if symptomatic and/or progressive disease is recognized, especially cytopenia and/or symptomatic organomegaly [1]. According to current consensus guidelines, treatment should be initiated if one or more of the following hematologic parameters are met: hemoglobin less than 11 g/dL, platelet count less than 100 × 103/μL, or absolute neutrophil count less than 1000/μL [1, 2]. Symptomatic splenomegaly with or without cytopenias is also an indication for treatment.
Cladribine and pentostatin are the drugs of choice in the treatment of HCL [1, 2]. These agents have significantly improved the prognosis of patients with HCL as they typically induce very long-lasting remissions. Pentostatin was first used by Spiers et al. in 1984 for the treatment of two men with advanced but previously untreated HCL [34]. Quick clearance of hairy cells from the blood and regression of splenomegaly and lymphadenopathy were observed in both patients, as was correction of anemia, thrombocytopenia, and granulocytopenia. In 1990, the Piro group from Scripps Clinic, San Diego, reported 12 patients with HCL treated with cladribine (2-CDA, 2-chlorodeoxyadenosine) at a dose of 0.1 mg per kilogram of body weight per day, by continuous infusion for 7 days [35]. Eleven patients had CR with the normalization of PB and BM with disappearance of leukemic cells. The median duration of response was 15.5 months with the longest remission being 3.8 years and no relapse at the time of publication. Further studies confirmed these early reports. Both agents induce durable and unmaintained CR in more than 70% of patients, and the relapse rates were about 30–40% after 5–10 years of follow-up (Table 12.2) [29, 36,37,38,39,40,41,42,43,44,45,46].
Cladribine is most commonly administered as a continuous i.v. infusion at a dose of 0.09 mg/kg over a 5- to 7-day period or as a 2-h i.v. infusion at a dose of 0.12–0.14 mg/kg for 5–7 days [37, 47]. Administration of cladribine can result in severe neutropenia that can last weeks or longer. Cladribine is also not recommended for patients presenting with active infection requiring therapy for the underlying leukemia. Cladribine can be also given at a dose of 0.12–0.15 mg/kg in a 2-h infusion once a week for six doses. Weekly and daily administration induces similar OR and CR rates. In addition, randomized trials indicate no difference in the occurrence of adverse events, including infections and hematological toxicity, between the weekly and daily schedule [38, 48]. Cladribine given subcutaneously is as equally effective as the intravenous formulation but more convenient for patients [49].
Pentostatin is usually administered at a dose of 4 mg/m2 i.v. every second week, until CR with one or two consolidating injections [29, 40, 42, 43]. Pentostatin is more effective than interferon-α (IFN-α) in HCL patients, as confirmed in a large, multicenter, randomized trial [40]. Purine nucleoside analogs dramatically improved the prognosis for patients with HCL. Durable and unmaintained remission is observed in 76–98% of patients, with relapse rates of about 30–40% after 5–10 years of observation, and in many patients, overall OS is longer than 20 years [29, 43, 50].
Although no direct comparison between pentostatin and cladribine has been performed in any randomized trial, no significant difference has been found between the two with regard to their efficacy or safety. Both agents can be used as frontline treatment of HCL. Cladribine is most commonly used due to its simpler administration and its lower renal toxicity [51, 52]. However, pentostatin has been successfully administered to patients with an active infection due to the gradual administration of titrated doses of this drug. In addition, cladribine can induce remissions in patients resistant to pentostatin [53,54,55,56]. A summary description of larger clinical trials with purine analogs in classic HCL is given in Table 12.2.
Whether rituximab should be administered concurrently or sequentially with cladribine to obtain the maximum benefit in previously untreated patients remains unclear [57]. In a recent phase 2 study, cladribine 5.6 mg/m2 was given intravenously daily for 5 days, followed approximately 1 month later with rituximab 375 mg/m2 i.v. weekly for 8 weeks. In 59 patients with untreated HCL, the CR rate was 100%. With a median follow-up of 60 months, 5-year failure-free survival (FFS) was 95%. In addition, 94% of the patients achieved negative MRD. However, the combination of rituximab with a purine nucleoside analog as up-front therapy for classic HCL has not been prospectively compared to purine analog therapy alone.
IFN-α may still have a place in front-line treatment of HCL, but its use is currently limited. It can be used in pregnancy and in patients presenting with neutropenia below 0.2/μL, when the risk of infection due to nucleoside analog therapy is high [58, 59].
The indications for splenectomy are limited in the era of currently available drugs. Splenectomy can be considered in pregnancy when INF-α treatment fails [60, 61]. Moreover, splenectomy can be effective for patients with splenic rupture and in patients with disease refractory to available therapeutic agents.
8 Treatment of Relapsed and Refractory Patients with Classic HCL
Despite the high efficacy of purine analogs, several patients will relapse during the course of their disease. However, similarly to previously untreated patients, relapsed patients do not always require treatment at the time of diagnosis, and indications for subsequent lines of therapy are similar to those made at diagnosis. In relapsed patients, re-induction with cladribine or pentostatin again induces remissions. However, in many patients treated with purine analogs as a single agent, responses are usually shorter and some patients develop refractory disease. Patients who relapse within 2–3 years after the first course of treatment have worse prognosis and a lower likelihood of achieving second durable CR; in addition, some patients have disease refractory to purine analog therapy. The median duration of response to second-line cladribine monotherapy is around 3 years [42, 44].
In early relapse (before 12–18 months), rituximab may be given at a dose of 375 mg/m2 for four to eight doses as weekly IV infusions [62]. Response is seen usually in more than 50% of patients with refractory to or relapsing disease. Longer responses are achievable with sequential cladribine followed by rituximab [43, 57, 62]. In one study of the use of cladribine followed by rituximab for relapsed disease, the CR rate was found to be 100%, and the 5-year FFS and OS 100% among 14 participating patients [57]. Of this group, the median duration of response was found to be longer among the 12 patients who had received prior cladribine monotherapy, i.e., as second-line treatment with cladribine followed by rituximab, than two treatment-naïve patients, who received this course as first-line cladribine monotherapy (P = 0.004). Alternatively, rituximab can be administered concurrently with purine analogs; this combination is more active than rituximab alone but is also more toxic than sequential treatment.
Few treatment options are available for patients who progress following first-line therapy with a purine analog and/or rituximab. Interferon-α (IFN-α) may be an effective treatment option for selected patients with relapsed HCL. However, only PRs can be achieved in the majority of patients, and prolonged treatment is necessary to maintain remission [63,64,65]. Although IFN-α eliminates leukemic cells from the blood and reduces bone marrow fibrosis, continuous therapy is less convenient to the patient and decreases quality of life due to flu-like symptoms and fatigue. Patients experiencing side effects may lower their dose or temporarily discontinue the treatment (drug holiday) and resume IFN-α at the time of relapse.
The use of fludarabine or bendamustine combined with rituximab could be also considered in relapsed patients. Fludarabine given at a dose of 40 mg/m2 p.o. on 5 consecutive days in combination with an intravenous injection of rituximab 375 mg/m2 on day 1, every 28 days for 4 cycles, may be a therapeutic option in relapsed or refractory patients previously treated with cladribine [66]. After a median follow-up of 35 months, 5-year PFS was found to be 89% and OS 83%. The combination of bendamustine and rituximab has also activity in multiply relapsed/refractory HCL. Burotto et al. treated 12 patients with HCL with two or more prior therapies requiring treatment with rituximab 375 mg/m2 on days 1 and 15 and bendamustine 70–90 mg/m2 on days 1 and 2, for 6 cycles at 4-week intervals [67]. The overall response rate was 100%, including CR in seven patients. MRD was absent in six patients with CR, who remained in CR for 30–35 months of follow-up. The most common adverse events (AEs) were thrombocytopenia (83%), lymphopenia (75%), leukopenia (58%), and neutropenia (42%).
The anti-CD22 recombinant immunotoxin moxetumomab pasudotox (LUMOXITI™, Astra Zeneca) is now an important drug for the treatment of HCL, especially in patients where conventional therapies produce limited responses or treatment failure. Moxetumomab pasudotox is composed of the Fv fragment of an anti-CD22 monoclonal antibody fused to a 38-kDa fragment of Pseudomonas exotoxin A, PE38. The drug was investigated in a phase 1 trial in 26 patients with refractory/relapsed HCL [68]. Nineteen patients (73.1%) responded with a CR rate of 34.6% and a PR rate of 38.5%. Moxetumomab pasudotox produced inferior responses in splenectomized patients and in patients with massive splenomegaly. In an extension study, the combined 33-patient cohort displayed 88% OR, including 64% CR [69]. Importantly, CR duration was longer (42.1 months) in 11 MRD-negative patients than in 9 MRD-positive patients (13.5 months) (P < 0.001). Among MRD-negative CRs, ten patients had ongoing CR and nine were without MRD at the end of the study. Moxetumomab pasudotox is so far the only nonchemotherapy treatment that can eliminate MRD in a significant percentage of HCL patients. The results from the phase 1 study have been confirmed recently in a pivotal, multicenter, open-label trial performed in 80 relapsed/refractory patients [70]. The objective response rate was 75% and durable CR rate was 41%. Among patients who achieved a CR, 27 (85%) achieved MRD negativity as evaluated by immunohistochemistry. The most frequent AEs included peripheral edema (39%), nausea (35%), fatigue (34%), and headache (33%). Hemolytic uremic syndrome (7.5%) and capillary leak syndrome (5%) were also observed, but they were reversible and generally manageable with supportive care and treatment discontinuation. In 2018, moxetumomab pasudotox received FDA approval for the treatment of patients with relapsed or refractory HCL who had received at least two prior systemic therapies, including treatment with a purine nucleoside analog [71]. Patients refractory to purine analog therapy and moxetumomab pasudotox should be enrolled on clinical trials that use new agents whenever possible.
Splenectomy may be indicated in patients who have resistant massive symptomatic splenomegaly (>10 cm below the costal margin) and accompanying low-level bone marrow infiltration [52]. Another indication for splenectomy is progressive HCL refractory to nucleoside analogs and IFN-α. Chemotherapy should not be given until at least 6 months after splenectomy.
Allogeneic stem cell transplantation should be considered in heavily pretreated younger patients who have had multiple relapses and are refractory to purine analogs and rituximab [72,73,74].
9 Treatment of Hairy Cell Leukemia Variant
Potential treatment options for HCL-V patients include splenectomy, purine nucleoside analogs (cladribine, pentostatin), IFN-α, monoclonal antibodies and immunotoxins, and immunochemotherapy [24, 75]. The results of cladribine monotherapy in HCL-V are inferior to those achieved with cladribine in classic HCL, with a response rate of less than 55% and few examples of CR being reported [39, 76, 77]. However, some reports indicate that HCL-V patients had shorter time to next treatment than those with classical HCL but demonstrated similar OS [78]. Rituximab combined with cladribine is more effective in treating HCL-V than cladribine alone or rituximab alone. In a study performed by Kreitman et al., cladribine was given at a dose of 0.15 mg/kg on days 1–5, with eight weekly doses of 375 mg/m2 rituximab, beginning on day 1 [79]. Of 10 patients, 9 achieved a CR, including 8 (88%) with MRD negativity at 12–48 (median 27) months of follow-up. In other study, the efficacy of cladribine followed by four weekly doses of rituximab was also evaluated in seven patients with HCL-V [57]. CR rate was 86%, 5-year FFS 64%, and OS 51.4%. Cladribine followed by immediate rituximab seems also to be an effective first-line treatment in HCL-V. Visentin et al. reported three previously untreated elderly patients who were effectively treated with four cycles of this combination [80]. All patients achieved a CR with no evidence of MRD. After a median follow-up of 19 months, all three patients were still in CR. Similar results were recently reported by Letendre and Doll [81]. Complete responses were also observed in relapsed patients treated with moxetumomab pasudotox [70]. Novel agents like ibrutinib and trametinib are also considered for the treatment of this disease [82, 83]. Splenectomy is recommended in some patients as it may induce clinical responses, correct cytopenias, remove the bulk of the tumor, and improve responses to chemo- or immunochemotherapy. In addition, autologous and allogenic hematopoietic stem cell transplantation can be taken into account in relapsed/refractory cases.
10 Novel Agents
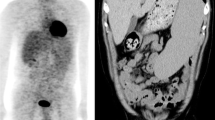
Recently, new targeted drugs are investigated in HCL, including vemurafenib and ibrutinib (Table 12.3). Vemurafenib (Zelboraf™, Roche) is the oral BRAF V600 inhibitor that has remarkable activity in multiply relapsed and refractory HCL patients with rapidly decreased splenomegaly, increased platelet counts, and normalization of hemoglobin and granulocyte counts [13, 84,85,86,87]. The safety and activity of vemurafenib were assessed in relapsed and refractory patients with classic HCL in two phase 2, multicenter studies in Italy and in the USA [86]. Vemurafenib was administered at a dose of 960 mg twice daily for a median of 16 weeks in the Italian study and 18 weeks in the US study, resulting in OR rates of 96% (CR 35%) in the Italian study and 100% (CR 42%) in the US study. Among the patients with CR, the median relapse-free survival (RFS) was 19 months, and the median treatment-free survival (TFS) was 25 months. Among those with PR, PFS was 6 months and TFS 18 months. Rash and arthralgia or arthritis were the most frequent AEs, and secondary cutaneous tumors was observed in 7 of 50 patients. Lower doses of vemurafenib are also effective in HCL. Dietrich et al. treated 21 heavily pretreated patients with vemurafenib starting at 240 mg BID and escalating to 720 or 960 mg in four patients [87]. CR was achieved in 40% (6/15) of evaluable patients, and median event-free survival (EFS) was 17 months. The response rate and kinetics of response were independent of vemurafenib dosage, and no significant difference in CR rate was found between lower and higher doses of vemurafenib. Vemurafenib is usually better tolerated than purine nucleoside analogs, and the risk of myelosuppression is relatively low. In addition, vemurafenib administration is associated with improvement in peripheral blood counts in infected patients. However, profound cytopenias and severe infections were also observed in HCL patients [88]. Other side effects noted with BRAF inhibitors include skeletal pain, photosensitivity, skin tumors, and renal toxicity. Secondary diffuse large B-cell lymphoma and well-differentiated squamous cell carcinoma were also observed in HCL patients treated with vemurafenib [89].
Vemurafenib combined with anti-CD20 monoclonal antibodies is even more effective than vemurafenib alone [90]. A phase 2 study by Tiaci et al. evaluated 31 patients who were either relapsed or refractory to purine analogs. Vemurafenib was administered at a dose of 960 mg twice daily for 8 weeks and rituximab at a dose of 375 mg/m2 on days 1 and 15. In addition, four doses of rituximab were given every 2 weeks after vemurafenib dosing. CRs were achieved in all 27 patients evaluable for efficacy. In addition, about two-thirds of the patients were found to be MRD negative in the BM by immunohistochemistry and flow cytometry. In the median follow-up period of 1.5 years, only 1 of 27 evaluable patients progressed. This chemotherapy-free regimen produces deep and durable responses in heavily pretreated patients with HCL and is superior to monotherapy with either vemurafenib or rituximab in the previous trials.
Dabrafenib, another BRAF inhibitor, is also promising and merits further evaluation in larger clinical trials [91, 92]. Combination therapy with BRAF and MEK inhibitors can be also more effective than vemurafenib alone and overcome vemurafenib resistance. A recent report presented interim analysis results of treatment with the combination of BRAF inhibitor dabrafenib and MEK inhibitor trametinib [93]. Treatment was used in 43 patients with heavily pretreated BRAF-V600E-mutated HCL that was refractory to first-line treatment with a purine analog or relapsed after two or more prior lines of treatment. This drug combination was well tolerated and demonstrated a high rate of durable responses. OR rate was 78% including 49% CR and 15% CR without MRD. Sixteen (50%) responses lasted 18 months or longer and 97.6% PFS and OS rates at 12 months.
Finally, Bruton’s tyrosine kinase pathway inhibitor ibrutinib is also being tested in patients with HCL and can induce a stable disease in most patients, including those with HCL-V [82, 94]. Consequently, multicenter phase 2 trials evaluating the role of ibrutinib in patients with relapsed HCL have been initiated (NCT01981512, NCT01841723). In the coming years, new agents will assist standard therapy for patients with HCL who may currently have suboptimal results after treatment with purine nucleoside analogs [95].
11 Treatment Complications and Supportive Care
Chemotherapy with purine analogs commonly leads to immune suppression and myelosuppression with cytopenias, as well as high risk of infections and bleeding, leading to hospitalization. In patients with febrile neutropenia, investigation for opportunistic, fungal, and viral infections is indicated, and treatment with broad-spectrum antibiotics and antifungal and antiviral drugs is recommended [2]. Patients treated with purine nucleoside analogs should receive prophylaxis for herpes simplex virus and varicella zoster virus, as well as prophylaxis against Pneumocystis jirovecii [2]. In patients with lymphopenia treated with cladribine or pentostatin, co-trimoxazole (960 mg three times per week) and aciclovir (200 mg three times per day) are recommended 1 week after purine analog administration. This prophylaxis should be given until the lymphocyte count increases to >1 × 109/L [2].
Granulocyte colony-stimulating factor may be considered for patients with severe neutropenia and life-threatening infection, but their role has not been proven. Annual influenza immunizations are also indicated as well as immunizations against Streptococcus pneumoniae. However, live viral vaccines are contraindicated. Transfused blood products should be irradiated to prevent transfusion-associated graft-versus-host disease.
12 Conclusions
Hairy cell leukemia is characterized by progressive pancytopenia, splenomegaly, and leukemic infiltrations of the bone marrow, liver, and spleen, The recent WHO classification distinguishes classic form of HCL and its HCL variant (HCL-V) as two distinct entities. Hairy cell leukemia usually has an indolent disease course. Most cases with classic HCL are BRAF-V600E-positive, but no cases of BRAF-V600E mutation have been described in HCL-V. The purine nucleoside analogs cladribine and pentostatin are effective drugs in the treatment of HCL; however, the disease mostly remains incurable, and new treatment options are needed for patients resistant to purine analog therapy. Rituximab is an active drug in HCL. The combination of rituximab with purine nucleoside analogs increases the occurrence and duration of response rates. Recently, the immunotoxin moxetumomab pasudotox received approval in the USA for the treatment of relapsed or refractory HCL patients who received at least two prior systemic therapies, including treatment with a purine nucleoside analog. Vemurafenib, an ATP-competitive BRAF inhibitor, is an active and well-tolerated drug in refractory or relapsed patients with classic HCL but not with HCL-V. Ibrutinib, an inhibitor of Bruton’s tyrosine kinase, has been shown to demonstrate antitumor activity in HCL patients, including HCL-V. The therapeutic algorithm for the treatment of patients with classic HCL is presented in Fig. 12.1.
References
Grever MR, Abdel-Wahab O, Andritsos LA, et al. Consensus guidelines for the diagnosis and management of patients with classic hairy cell leukemia. Blood. 2017;129:553–60.
Robak T, Matutes E, Catovsky D, Zinzani PL, Buske C, ESMO Guidelines Committee. Hairy cell leukaemia: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v100–7.
Bouroncle BA, Wiseman BK, Doan CA. Leukemic reticuloendotheliosis. Blood. 1958;13:609–30.
Wang X, Spielberger R, Huang Q. Hairy cell leukemia variant, a new entity of the WHO 2008. J Clin Oncol. 2011;29(36):e864–6.
Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90.
Cawley JC, Burns GF, Hayhoe FG. A chronic lymphoproliferative disorder with distinctive features: a distinct variant of hairy-cell leukaemia. Leuk Res. 1980;4:547–59.
Chandran R, Gardiner SK, Smith SD, Spurgeon SE. Improved survival in hairy cell leukaemia over three decades: a SEER database analysis of prognostic factors. Br J Haematol. 2013;163:407–9.
Teras LR, DeSantis CE, Cerhan JR, Morton LM, Jemal A, Flowers CR. 2016 US lymphoid malignancy statistics by World Health Organization subtypes. CA Cancer J Clin. 2016;66:443. https://doi.org/10.3322/caac.21357.
Getta BM, Woo KM, Devlin S, et al. Treatment outcomes and secondary cancer incidence in young patients with hairy cell leukaemia. Br J Haematol. 2016;175:402–9.
Roider T, Falini B, Dietrich S. Recent advances in understanding and managing hairy cell leukemia. F1000 Res. 2018;7. pii: F1000 Faculty Rev-509.
Tiacci E, Schiavoni G, Forconi F, et al. Simple genetic diagnosis of hairy cell leukemia by sensitive detection of the BRAF-V600E mutation. Blood. 2012;119:192–5.
Tiacci E, Trifonov V, Schiavoni G, et al. BRAF mutations in hairy-cell leukemia. N Engl J Med. 2011;364:2305–15.
Samuel J, Macip S, Dyer MJ. Efficacy of vemurafenib in hairy-cell leukemia. N Engl J Med. 2014;370:286–8.
Durham BH, Getta B, Dietrich S, et al. Genomic analysis of hairy cell leukemia identifies novel recurrent genetic alterations. Blood. 2017;130:1644–8.
Tschernitz S, Flossbach L, Bonengel M, Roth S, Rosenwald A, Geissinger E. Alternative BRAF mutations in BRAF V600E-negative hairy cell leukaemias. Br J Haematol. 2014;165:529–33.
Tiacci E, Pettirossi V, Schiavoni G, Falini B. Genomics of hairy cell leukemia. J Clin Oncol. 2017;35:1002–10.
Chung SS, Kim E, Park JH, et al. Hematopoietic stem cell origin of BRAFV600E mutations in hairy cell leukemia. Sci Transl Med. 2014;6:238ra71.
Falini B, Martelli MP, Tiacci E. BRAF V600E mutation in hairy cell leukemia: from bench to bedside. Blood. 2016;128:1918–27.
Andrulis M, Penzel R, Weichert W, von Deimling A, Capper D. Application of a BRAF V600E mutation-specific antibody for the diagnosis of hairy cell leukemia. Am J Surg Pathol. 2012;36:1796–800.
Uppal G, Ly V, Wang ZX, et al. The utility of BRAF V600E mutation-specific antibody VE1 for the diagnosis of hairy cell leukemia. Am J Clin Pathol. 2015;143:120–5.
Dietrich S, Hüllein J, Lee SC, et al. Recurrent CDKN1B (p27) mutations in hairy cell leukemia. Blood. 2015;126:1005–8.
Tiacci E, Schiavoni G, Martelli MP, et al. Constant activation of the RAF-MEK-ERK pathway as a diagnostic and therapeutic target in hairy cell leukemia. Haematologica. 2013;98:635–9.
Pettirossi V, Santi A, Imperi E, et al. BRAF inhibitors reverse the unique molecular signature and phenotype of hairy cell leukemia and exert potent antileukemic activity. Blood. 2015;125:1207–16.
Robak T. Hairy-cell leukemia variant: recent view on diagnosis, biology and treatment. Cancer Treat Rev. 2011;37:3–10.
Xi L, Arons E, Navarro W, et al. Both variant and IGHV4-34-expressing hairy cell leukemia lack the BRAF V600E mutation. Blood. 2012;119:3330–2.
Waterfall JJ, Arons E, Walker RL, et al. High prevalence of MAP2K1 mutations in variant and IGHV4-34-expressing hairy-cell leukemias. Nat Genet. 2014;46:8–10.
Sandes AF, de Lourdes Chauffaille M, Oliveira CR, et al. CD200 has an important role in the differential diagnosis of mature B-cell neoplasms by multiparameter flow cytometry. Cytometry B Clin Cytom. 2014;86:98–105.
Pillai V, Pozdnyakova O, Charest K, Li B, Shahsafaei A, Dorfman DM. CD200 flow cytometric assessment and semiquantitative immunohistochemical staining distinguishes hairy cell leukemia from hairy cell leukemia-variant and other B-cell lymphoproliferative disorders. Am J Clin Pathol. 2013;140:536–43.
Else M, Dearden CE, Matutes E, et al. Long-term follow-up of 233 patients with hairy cell leukaemia, treated initially with pentostatin or cladribine, at a median of 16 years from diagnosis. Br J Haematol. 2009;145:733–40.
Arons E, Suntum T, Stetler-Stevenson M, Kreitman RJ. VH4-34+ hairy cell leukemia, a new variant with poor prognosis despite standard therapy. Blood. 2009;114:4687–95.
Goodman GR, Burian C, Koziol JA, Saven A. Extended follow-up of patients with hairy cell leukemia after treatment with cladribine. J Clin Oncol. 2003;21:891–6.
Mhawech-Fauceglia P, Oberholzer M, Aschenafi S, et al. Potential predictive patterns of minimal residual disease detected by immunohistochemistry on bone marrow biopsy specimens during a long-term follow-up in patients treated with cladribine for hairy cell leukemia. Arch Pathol Lab Med. 2006;130:374–7.
Ortiz-Maldonado V, Villamor N, Baumann T, et al. Is there a role for minimal residual disease monitoring in the management of patients with hairy-cell leukaemia? Br J Haematol. 2018;183:127–9.
Spiers AS, Parekh SL, Bishop MB. Hairy cell leukaemia: induction of complete remission with pentostatin (2′-deoxycoformycin). J Clin Oncol. 1984;2:1336–42.
Piro LD, Carrera CJ, Carson DA, Beutler E. Lasting remissions in hairy cell leukemia induced by a single infusion of 2-chlorodeoxyadenosine. N Engl J Med. 1990;322:1117–21.
Saven A, Burian C, Kozioł JA, Piro LD. Long-term follow-up of patients with hairy cell leukemia after cladribine treatment. Blood. 1998;92:1918–26.
Cheson BD, Sorensen JM, Vena DA. Treatment of hairy cell leukemia with 2-chlorodeoxyadenosine via the group protocol mechanism of the National Cancer Institute: a report of 979 patients. J Clin Oncol. 1998;16:3007–15.
Robak T, Jamroziak K, Gora-Tybor J, et al. Cladribine in a weekly versus daily schedule for untreated active hairy cell leukemia: final report from the Polish Adult Leukemia Group (PALG) of a prospective, randomized, multicenter trial. Blood. 2007;109:3672–5.
Robak T, Błasińska-Morawiec M, Błoński J, et al. 2-chlorodeoxyadenosine: (cladribine) in the treatment of hairy cell leukemia and hairy cell leukemia variant 7-year experience in Poland. Eur J Haematol. 1999;62:49–56.
Grever M, Kopecky K, Foucar MK, et al. Randomized comparison of pentostatin versus interferon alfa-2a in previously untreated patients with hairy cell leukemia: an intergroup study. J Clin Oncol. 1995;13:974–82.
Maloisel F, Benboubker L, Gardembas M, et al. Long-term outcome with pentostatin treatment in hairy cell leukemia patients. A French retrospective study of 238 patients. Leukemia. 2003;17:45–51.
Flinn IW, Kopecky KJ, Foucar MK, et al. Long-term follow-up of remission duration, mortality and second malignancies in hairy cell leukemia patients treated with pentostatin. Blood. 2000;96:2981–6.
Else M, Dearden CE, Catovsky D. Long-term follow-up after purine analogue therapy in hairy cell leukaemia. Best Pract Res Clin Haematol. 2015;28:217–29.
Zinzani PL, Pellegrini C, Stefoni V, et al. Hairy cell leukemia: evaluation of the long-term outcome in 121 patients. Cancer. 2010;116:4788–92.
Inbar M, Herishanu Y, Goldschmidt N, et al. Hairy cell leukemia: retrospective analysis of demographic data and outcome of 203 patients from 12 medical centers in Israel. Anticancer Res. 2018;38:6423–9.
Forconi F, Cencini E, Zaja F, et al. Analysis of toxicity and efficacy of subcutaneous cladribine at reduced or standard doses (five versus seven consecutive days) in patients with hairy cell leukemia (HCL) in the ICGHCL2004 protocol by the Italian Cooperative Group on HCL. Blood. 2010;116:Abstravt 701.
Robak T, Blasinska-Morawiec M, Krykowski E, et al. 2-chlorodeoxyadenosine (2-CdA) in 2-hour versus 24-hour intravenous infusion in the treatment of patients with hairy cell leukemia. Leuk Lymphoma. 1996;22:107–11.
Zenhäusern R, Schmitz SF, Solenthaler M, et al. Randomized trial of daily versus weekly administration of 2-chlorodeoxyadenosine in patients with hairy cell leukemia: a multicenter phase III trial (SAKK 32/98). Leuk Lymphoma. 2009;50:1501–11.
von Rohr A, Schmitz SF, Tichelli A, et al. Treatment of hairy cell leukemia with cladribine (2-chlorodeoxyadenosine) by subcutaneous bolus injection: a phase II study. Ann Oncol. 2002;13:1641–9.
Sigal DS, Sharpe R, Burian C, Saven A. Very long-term eradication of minimal residual disease in patients with hairy cell leukemia after a single course of cladribine. Blood. 2010;115:1893–6.
Cornet E, Delmer A, Feugier P, et al. Recommendations of the SFH (French Society of Haematology) for the diagnosis, treatment and follow-up of hairy cell leukaemia. Ann Hematol. 2014;93:1977–83.
Jones G, Parry-Jones N, Wilkins B, Else M, Catovsky D. Revised guidelines for the diagnosis and management of hairy cell leukaemia and hairy cell leukaemia variant. Br J Haematol. 2012;156:186–95.
Piro LD, Ellison DJ, Saven A. The Scripps clinic experience with 2-chlorodeoxyadenosine in the treatment of hairy cell leukemia. Leuk Lymphoma. 1994;14(Suppl 1):121–5.
Saven A, Piro LD. Complete remissions in hairy cell leukemia with 2-chlorodeoxyadenosine after failure with 2′-deoxycoformycin. Ann Intern Med. 1993;119:278–83.
Dearden CE, Matutes E, Hilditch BL, Swansbury GJ, Catovsky D. Long-term follow-up of patients with hairy cell leukaemia after treatment with pentostatin or cladribine. Br J Haematol. 1999;106:515–9.
Estey EH, Kurzrock R, Kantarjian HM, et al. Treatment of hairy cell leukemia with 2-chlorodeoxyadenosine (2-CdA). Blood. 1992;79:882–7.
Chihara D, Kantarjian H, O’Brien S, et al. Long-term durable remission by cladribine followed by rituximab in patients with hairy cell leukaemia: update of a phase II trial. Br J Haematol. 2016;174:760–6.
Baer MR, Ozer H, Foon KA. Interferon-alpha therapy during pregnancy in chronic myelogenous leukaemia and hairy cell leukaemia. Br J Haematol. 1992;81:167–9.
Habermann TM, Rai K. Historical treatments of in hairy cell leukemia, splenectomy and interferon: past and current uses. Leuk Lymphoma. 2011;52:18–20.
Adeniji BA, Fallas M, Incerpi M, et al. Laparoscopic splenectomy for hairy cell leukemia in pregnancy. Case Report Med. 2010;2010. pii: 136823.
Stiles GM, Stanco LM, Saven A, et al. Splenectomy for hairy cell leukemia in pregnancy. J Perinatol. 1998;18:200–1.
Leclerc M, Suarez F, Noël MP, et al. Rituximab therapy for hairy cell leukemia: a retrospective study of 41 cases. Ann Hematol. 2015;94:89–95.
Seymour JF, Estey EH, Keating MJ, Kurzrock R. Response to interferon-α in patients with hairy cell leukemia relapsing after treatment with 2-chlorodeoxyadenosine. Leukemia. 1995;9:929–32.
Hoffman MA. Interferon-alpha is a very effective salvage therapy for patients with hairy cell leukemia relapsing after cladribine: a report of three cases. Med Oncol. 2011;28:1537–41.
Silva WFD, Teixeira LLC, Rocha V, Buccheri V. Current role of interferon in hairy cell leukemia therapy: a timely decision. Hematol Transfus Cell Ther. 2019;41:88–90.
Gerrie AS, Zypchen LN, Connors JM. Fludarabine and rituximab for relapsed or refractory hairy cell leukemia. Blood. 2012;119:1988–91.
Burotto M, Stetler-Stevenson M, Arons E, et al. Bendamustine and rituximab in relapsed and refractory hairy cell leukemia. Clin Cancer Res. 2013;19:6313–21.
Kreitman RJ, Tallman MS, Robak T, et al. Phase I trial of anti-CD22 recombinant immunotoxin moxetumomab pasudotox (CAT-8015 or HA22) in patients with hairy cell leukemia. J Clin Oncol. 2012;30:1822–8.
Kreitman RJ, Tallman MS, Robak T, et al. Minimal residual hairy cell leukemia eradication with moxetumomab pasudotox: phase 1 results and long-term follow-up. Blood. 2018;131:2331–4.
Kreitman RJ, Dearden C, Zinzani PL, et al. Moxetumomab pasudotox in relapsed/refractory hairy cell leukemia. Leukemia. 2018;32:1768–77.
Dhillon S. Moxetumomab pasudotox: first global approval. Drugs. 2018;78:1763–7.
Cheever MA, Fefer A, Greenberg PD, et al. Treatment of hairy-cell leukemia with chemoradiotherapy and identical-twin bone-marrow transplantation. N Engl J Med. 1982;307:479–81.
Zinzani PL, Bonifazi F, Pellegrini C, et al. Hairy cell leukemia: allogeneic transplantation could be an optimal option in selected patients. Clin Lymphoma Myeloma Leuk. 2012;12:287–9.
Kiyasu J, Shiratsuchi M, Ohtsuka R, et al. Achievement of complete remission of refractory hairy cell leukemia by rituximab progressing after allogeneic hematopoietic stem cell transplantation. Int J Hematol. 2009;89:403–5.
Robak T. Management of hairy cell leukemia variant. Leuk Lymphoma. 2011;52(Suppl 2):53–6.
Matutes E, Wotherspoon A, Catovsky D. The variant form of hairy-cell leukaemia. Best Pract Res Clin Haematol. 2003;16:41–56.
Tetreault SA, Robbins BA, Saven A. Treatment of hairy cell leukemia-variant with cladribine. Leuk Lymphoma. 1999;35:347–54.
Getta B, Woo KM, Devlin S, et al. Hairy cell leukemia variant has similar survival to classical disease despite poorer responses to initial therapy: a 30-year experience from Memorial Sloan Kettering Cancer Center. Blood. 2015;126:Abstract 1476.
Kreitman RJ, Wilson W, Calvo KR, et al. Cladribine with immediate rituximab for the treatment of patients with variant hairy cell leukemia. Clin Cancer Res. 2013;19:6873–81.
Visentin A, Imbergamo S, Frezzato F, et al. Bendamustine plus rituximab is an effective first-line treatment in hairy cell leukemia variant: a report of three cases. Oncotarget. 2017;8:110727–31.
Letendre P, Doll D. Novel therapeutics in the treatment of hairy cell leukemia variant. Leuk Res. 2018;75:58–60.
Bohn JP, Wanner D, Steurer M. Ibrutinib for relapsed refractory hairy cell leukemia variant. Leuk Lymphoma. 2017;58:1224–6.
Andritsos LA, Grieselhuber NR, Anghelina M, et al. Trametinib for the treatment of IGHV4-34, MAP2K1-mutant variant hairy cell leukemia. Leuk Lymphoma. 2018;59:1008–11.
Dietrich S, Zenz T. BRAF inhibitor therapy in HCL. Best Pract Res Clin Haematol. 2015;28:246–52.
Dietrich S, Glimm H, Andrulis M, et al. BRAF inhibition in refractory hairy-cell leukemia. N Engl J Med. 2012;366:2038–40.
Tiacci E, Park JH, De Carolis L, et al. Targeting mutant BRAF in relapsed or refractory hairy-cell leukemia. N Engl J Med. 2015;373:1733–47.
Dietrich S, Pircher A, Endris V, et al. BRAF inhibition in hairy cell leukemia with low-dose vemurafenib. Blood. 2016;127:2847–55.
Shenoi DP, Andritsos LA, Blachly JS, et al. Classic hairy cell leukemia complicated by pancytopenia and severe infection: a report of 3 cases treated with vemurafenib. Blood Adv. 2019;3:116–8.
Bhangoo MS, Saven A. Secondary malignancies after treatment with single-agent vemurafenib in two patients with refractory hairy cell leukemia. Leuk Lymphoma. 2018;15:1–3. https://doi.org/10.1080/10428194.2018.1519809.
Tiacci E, Carolis LD, Zaja F, et al. The chemotherapy-free combination of vemurafenib and rituximab produces deep and durable responses in relapsed or refractory hairy cell leukemia (HCL) patients. Blood. 2017;130:Abstract 409.
Blachly JS, Lozanski G, Lucas DM, Grever MR, Kendra K, Andritsos LA. Cotreatment of hairy cell leukemia and melanoma with the BRAF inhibitor dabrafenib. J Natl Compr Cancer Netw. 2015;13:9–13.
Vergote V, Dierickx D, Janssens A, et al. Rapid and complete hematological response of refractory hairy cell leukemia to the BRAF inhibitor dabrafenib. Ann Hematol. 2014;93:2087–9.
Kreitman RJ, Moreau P, Hutchings M, et al. Treatment with combination of dabrafenib and trametinib in patients with recurrent/refractory BRAF V600E-mutated hairy cell leukemia (HCL). Blood. 2018;132:Abstract 391.
Jones JA, Andritsos LA, Lucas DM. Preliminary safety and efficacy of the Bruton’s tyrosine kinase (BTK) inhibitor ibrutinib (IBR) in patients (pts) with hairy cell leukemia (HCL). J Clin Oncol. 2014;32(15 Suppl):Abstract 7063.
Robak T, Wolska A, Robak P. Potential breakthroughs with investigational drugs for hairy cell leukemia. Expert Opin Investig Drugs. 2015;24:1419–31.
Kreitman RJ, Stetler-Stevenson M, Margulies I, et al. Phase II trial of recombinant immunotoxin RFB4(dsFv)-PE38 (BL22) in patients with hairy cell leukemia. J Clin Oncol. 2009;27:2983–90.
Conflicts of Interest
No potential conflicts of interest were disclosed.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Robak, T., Dietrich, S. (2021). Hairy Cell Leukemia. In: Dreyling, M., Ladetto, M. (eds) Indolent Lymphomas . Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-55989-2_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-55989-2_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-55988-5
Online ISBN: 978-3-030-55989-2
eBook Packages: MedicineMedicine (R0)