Abstract
Pediatric head and neck tumors are generally uncommon, representing 1–2 % of all head and neck tumors. Malignant tumors of head and neck account for about 25%, the most common including lymphomas, rhabdomyosarcoma, thyroid gland, salivary glands masses, nasopharyngeal carcinoma, and other rare tumors.
The clinical features of all these tumors differ according to the nature, site, and age at presentations.
There are different aspects of diagnosing head and neck tumors including the clinical evaluation and using the appropriate investigative tools according to the condition.
Modalities of treatment differ depending on tumor type, but generally, early detection reflects better prognosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The majority of head and neck masses in children are inflammatory in nature, but other etiologies include congenital, inflammatory, and neoplastic lesions.
Vascular anomalies of the head and neck region constitute more than 50% of vascular anomalies diagnosed in children and affect approximately 1 in 20 children. These lesions broadly fall into two categories—vascular tumors and vascular malformations. This is an important distinction because malformations and tumors show different growth characteristics. Infantile hemangioma is the most common and is considered a benign vascular tumor. It will rapidly enlarge, and then slowly regress over time. Vascular malformations are relatively uncommon, rarely regress, and will continue to enlarge and cause increased complications over time.
Neoplasms of the head and neck region account for approximately 5% of all childhood malignancies. The most common pediatric head and neck malignancies include lymphomas (60%), rhabdomyosarcomas (15%), thyroid malignancies (10%), nasopharyngeal carcinomas (NPCs), salivary gland malignancies, and neuroblastomas.
Persistent adenopathy raises more concerns, especially enlarged lymph nodes within the posterior triangle or supraclavicular space, nodes that are painless, firm, and not mobile.
2 Vascular Anomalies-Tumors
-
Vascular anomalies occur in the head and neck in approximately 4.5% of children [1].
-
They are classified into vascular tumors and vascular malformations (Table 59.1) [2].
-
The differentiation between the two types is essential as they show different growth characteristics [3].
2.1 Infantile Hemangioma
-
Has a distinct biologic tumorous entity characterized by rapid endothelial proliferation shortly after birth followed by slow regression over time.
-
Most common vascular anomaly seen in approximately 4–10% of infants [1].
-
Approximately 60% presents in the head and neck.
-
More common in whites, premature babies under 1000 g, and multiple gestations (2–3:1 girl/boy ratio).
-
Vascular endothelial growth factor (VEGF) and adrenergic receptor pathway are implicated in its development.
-
GLUT-1 has been identified as a specific marker for IH [4].
2.1.1 Clinical Features
-
Red macule at birth.
-
Rapid growth in the first 6 weeks after birth up until the first 8–12 months [5].
-
Involution occurs over 3–8 years.
-
Subglottic IH presents with stridor.
2.1.2 Treatment
-
The majority of IH need no treatment due to involution of the hemangioma over time.
-
Propranolol (beta blocker) has evolved to become the first-line treatment modality.
-
Many protocols for propranolol, most commonly dose is: 1–3 mg/kg/day divided three times a day.
-
Propranolol is most effective in the proliferative period. Therefore, mostly given for 6–12 months and then weaned off. If symptoms recur, it can be restarted again [6].
-
IH causing functional or cosmetic deformity (covering the eye, nasal tip, subglottic) should be treated early [2].
-
High dose steroids (prednisolone) is an effective treatment modality for IH. However, with higher side-effects in comparison to propranolol.
-
Prednisolone can be used as primary or adjuvant therapy in non-responders to propranolol [6].
-
Other modalities, including interferon and chemotherapy, are rarely used now.
-
Surgical interventions are still needed in up to 50% of cases, especially in the proliferating phase, where there is significant damage to surrounding tissues [7].

3 Vascular Anomalies-Malformations
3.1 Capillary Malformation
3.1.1 Clinical Features
-
Abnormally dilated capillaries in the superficial dermis are present at birth, and eventually change to a deep purple color with age and into adulthood.
-
Trigeminal nerve abnormalities lead to a risk of choroidal and intracranial vascular abnormalities called Sturge–Weber Syndrome [8]
3.1.2 Treatment
-
Pulsed-dye laser achieves significant lightening in 80% of patients.
-
Surgical excision in rare cases with skin grafting or advancement flaps [9].
3.2 Venous Malformations (VM)
-
VMs represent the third most common vascular mass in the head and neck after IH and LM.
-
These lesions are structural anomalies that have a normal growth rate (grow with the child) and normal rates of endothelial turnover.
-
VMs typically present as compressible masses, often with overlying blue or purplish skin staining. On the mucous membranes, these will be soft purple blebs.
-
VMs can present at any site but are more common in the muscle and mucous membranes [10].
-
Lesions occur in isolation or part of capillary venous malformation.
-
Grow with the child and can expand at puberty, after trauma or subtotal excision.
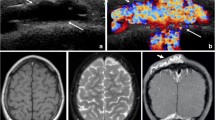
3.2.1 Diagnosis
-
Ultrasound: is useful for superficial sites.
-
MRI: VM will appear isointense on T1-weighted sequences and hyperintense on T2-weighted sequences
3.2.2 Treatment
-
Observation: however, most VM will require treatment at some point.
-
Treatment modalities: sclerotherapy, surgery, and laser therapy.
-
Most VMs will require a multimodality approach to treatment.
-
The location, size, and relation to adjacent structures will guide which modality treatment is adopted.
-
Sclerotherapy works successfully and results in a significant reduction of the VM.
-
Many sclerotherapy agents have been used.
-
On average, 1–4 sclerotherapy sessions over a period of 3–12 months is needed.
-
Sclerotherapy complications: swelling, ulceration, peripheral nerve palsy, deep vein thrombosis, and muscle contracture.
-
Small well-confined VM with clear borders can be cured by simple surgical excision.
-
VM with poorly defined borders which can invade normal tissue can be extremely difficult to be excised completely. This type of surgery carries a high risk of bleeding and injury to surrounding structures (e.g., parotid VM).
-
Nd:YAG laser has been in the management of VM, typically for airway lesions [11].

3.3 Lymphatic Malformations (LM)
-
Known previously as cystic hygroma or lymphangioma.
-
Consists of many dilated lymphatic channels lined by single epithelial layer, forming swellings of differing size.
-
75% involves the head and neck due to its abundant lymphatics [12].
-
Commonly linked to VM and called venolymphatic malformation (VLM).
-
Classified into: macrocystic (>2 cm), microcystic <2 cm), and mixed.
-
4 different types have been described (Serres satging):
-
Type I: Unilateral infrahyoid
-
Type II: Unilateral suprahyoid
-
Type III: Unilateral infra- and suprahyoid
-
Type IV: Bilateral suprahyoid
-
-
Type III and IV are more complex and difficult to treat, requiring frequent treatments.
3.3.1 Clinical Features
-
Presents at birth or can develop during childhood.
-
Sudden swelling can be linked to respiratory infection or minor trauma due to internal hemorrhage.
-
On examination: similar to VM, however, less compressible and intertwine with normal tissue leading to cosmetic and functional deformity.
-
Macroglossia. Tongue covered in vesicles.
-
Can lead to airway obstruction, a tracheostomy may be necessary.
-
3.3.2 Treatment
-
LM treatment is usually complex and depends on the cosmetic and functional deformity.
-
The primary goal of treatment is to improve functionality by reducing its size.
-
The secondary goal of treatment is the complete eradication of the disease.
-
Conservative management mainly with respiratory infections and trauma. This is achieved with antibiotics and steroids.
-
Sclerotherapy: ideal for macrocytic type I. However, it may have a role for microcystic lesions.
-
Sclerotherapy injections for type I are normally intralesional and done under radiologic guidance leading to an inflammatory response. In microcystic lesion, sclerotic agent is injected submucosally.
-
Surgery: total excision of type I and subtotal excision of type II.
-
Partial glossectomy may be needed for macroglossia or even surface lasering of tongue vesicles if they are present.
-
An immunosuppressant, sirolimus has recently been used for their antilymphangiogenic properties in treating LM [13].
-
Psychological support for patients who experience facial disfigurement.
3.4 Arteriovenous Malformation (AVM)
-
Fast-flow lesions.
-
Relatively uncommon in head and neck, except in cranial cavity where they are 20x more common than slow-flow lesions.
-
Presents in childhood commonly or adolescence [14].
3.4.1 Clinical Features
-
Warm and pulsatile swelling.
-
If untreated for a long time, skin necrosis and destruction of facial bones can take place.
3.4.2 Diagnosis
-
Doppler ultrasound used to confirm arteriovenous shunting.
-
MRI/ angiography.
3.4.3 Treatment
-
No treatment for most cases if asymptomatic.
-
Selective embolization can be used pre-operatively.
-
Subtotal excision means that recurrence is very likely as new vascular channels will develop over time.
-
Total excision is the only cure; however, it is a very extensive surgery [11].
4 Benign Tumors
4.1 Teratoma
-
Occurs approximately in 1 in 4000 births.
-
Said to be derived from pluripotent cells.
-
7–9% of cases are localized to the head and neck area.
4.1.1 Clinical Features
-
Most cases occur in sacrococcygeal region, ovaries, testes, anterior mediastinum, and retroperitoneum.
-
Malignant transformation is rare in the head and neck.
-
Presents as a massive benign neck mass at birth.
-
Despite being benign, morbidity and mortality are high.
4.1.2 Treatment
-
Surgical resection.
-
Careful monitoring of tumor markers—alpha fetoprotein and beta human chorionic gonadotrophin—in the blood is highly suggested [11].

4.2 Juvenile Nasopharyngeal Angiofibroma
5 Malignant Tumors
-
25% of pediatric malignancies will involve the head at some stage.
-
Estimated that 5% originate in the head and neck area.
-
The most common presentation of a malignancy in the head and neck region in childhood is the asymptomatic mass.
-
The best predictors of malignancy in cervical lymphadenopathy are the size of the node, the number of sites involved, and the age of the patient.
-
Squamous cell carcinoma is extremely rare in children [14].
-
The most common lesions are lymphomas and sarcomas in children, as shown in the following Table 59.2 [15]:
5.1 Hodgkin’s Lymphoma
-
A malignant neoplasm of lymphoreticular system
-
Occurs mostly in adolescents
-
Distinguished from non-Hodgkin’s lymphoma by the presence of Reed–Sternberg cells
5.1.1 Clinical Features
-
Progressive enlargement of cervical and supraclavicular lymph nodes.
-
Enlargement of liver, spleen, and abdominal lymph nodes as the disease spreads.
-
Neutropenia, thrombocytopenia, and anemia in peripheral blood film.
-
Constitutional symptoms (B symptoms)—fever, night sweats and weight loss in 25–30%.
5.1.2 Diagnosis
-
FNA has a limited role.
-
Excision biopsy is the gold standard.
5.1.3 Treatment
-
Chemotherapy or radiotherapy depending on stage [16].
5.2 Non-Hodgkin’s Lymphoma
-
A mixed group of solid malignant neoplasms of lymphoreticular system.
-
Affects ages 2–12 years mostly.
5.2.1 Clinical Features
-
Presents commonly as cervical lymphadenopathy but can affect extra-nodal sites.
-
Lesions are common in head and neck, nasopharynx, orbit, and skull base.
-
May present as asymmetrical tonsillar enlargement.
5.2.2 Diagnosis
-
FNA has limited role.
-
Excision biopsy is the gold standard.
5.2.3 Treatment
Chemotherapy or radiotherapy depending on stage [17].
5.3 Rhabdomyosarcoma
-
Second most common malignancy in pediatric.
-
30–40% of cases occur in head and neck.
-
>50% of cases are in <5 years of age.
-
Prognosis has improved with multimodality treatments.
-
Classified into two types: embryonal and alveolar [18].
-
Embryonal affects approximately 80% and has a better prognosis than alveolar type.
5.3.1 Clinical Features
-
Most common sites are the orbit (most common), nasopharynx, middle ear and mastoid, and sinonasal cavities.
-
Typically presents as rapidly enlarging mass in a child under the age of 12 years old.
-
Presentation depends on the site involved.
-
Nodal involvement is estimated between 3% and 36%.
5.3.2 Diagnosis
-
Biopsy, MRI, and CT are required.
-
Multiple modalities are utilized in staging: chest CT, abdominal ultrasound, bone marrow aspiration, and lumbar puncture [19].
5.3.3 Treatment
-
Follows guidelines of Inter Group Rhabdomyosarcoma (IRS) (Table 59.3).
-
The majority are at stage II at presentation and complete surgical excision is difficult to achieve.
-
Multimodality treatment is used:
-
Surgical resection
-
Chemotherapy
-
Radiotherapy
-
5.4 Thyroid Malignancy
-
More common in adolescents than pediatrics.
-
Has a female predominance 4:1.
-
Close association with previous radiation history.
-
Slow growing tumors and associated with prolonged survival rate.
-
45% are differentiated papillary carcinomas.
-
45% mixed papillary/follicular types.
-
10% follicular lesions.
-
Medullary thyroid carcinoma (MTC) is rare (only 10% of thyroid malignancies in children) and must be suspected in children with multiple endocrine neoplasia (MEN) types IIa and IIb.
-
Anaplastic and undifferentiated tumors are extremely rare in children and adolescents [20].
5.4.1 Clinical Features
-
Solitary asymptomatic mass in the anterior or lateral neck is the most common presentation.
-
It is estimated that 74% will have nodal metastases and 25% distant metastases at time of presentation.
5.4.2 Diagnosis
-
Ultrasound scan, usually in conjunction with an ultrasound-guided FNAC.
-
Thyroid function tests and plasma thyroglobulin levels.
-
Plasma calcitonin when suspecting medullary carcinoma.
5.4.3 Treatment
-
Complete surgical excision is the ideal approach.
-
Possible complications for total thyroidectomy include injury to recurrent laryngeal nerve, hypocalcemia, and airway compromise if both recurrent laryngeal nerves have been injured.
-
Following surgery, a whole-body radioiodine scan is performed, and ablative radioiodine treatment is given if necessary [21].
-
Plasma thyroglobulin can then be used as a tumor marker and suppressive levothyroxine should be given.
-
Radiotherapy is rarely indicated in differentiated thyroid carcinoma in childhood [22].
5.5 Neuroblastoma
-
Commonest malignancy in children under the age of 1.
-
90% of cases present before 10 years of age.
-
Arise from undifferentiated sympathetic nervous system cells of neural crest origin.
5.5.1 Clinical Features
-
Predominantly found in adrenal gland and sympathetic chain.
-
May present as a primary neck mass arising from the cervical sympathetic trunk associated Horner’s syndrome.
-
Metastases to regional lymph nodes is common (~35%) [23].
5.5.2 Treatment
-
Surgery can be curative for localized lesions with 90% survival rate in children with resectable disease.
-
Radiation and chemotherapy are chosen for metastatic lesions [24].
5.6 Nasopharyngeal Carcinoma (NPS)
-
1–2% of pediatric malignancies in the USA and Europe.
-
10–20 % of pediatric malignancies in Africa.
-
Originates from epithelium and associated with EBV.
-
Undifferentiated NPS is most common in children.
-
5-year survival is similar to adults (30–60%).
5.6.1 Clinical Features
-
Children will often have metastatic disease in their neck.
-
Unilateral otitis media.
-
Rhinorrhea.
-
Nasal obstruction.
-
Cranial nerve palsies and facial pain suggest skull-base involvement.
5.6.2 Diagnosis
-
Delayed diagnosis is very common.
-
Flexible nasopharyngoscopy.
-
Biopsy.
-
CT and MRI imaging.
-
Staging.
5.6.3 Treatment
-
Dependent on type, location, and extent of spread.
-
Chemoradiation.
-
Surgery [25].
Take Home Messages
-
The pediatric head and neck malignancies differ from adults; hence a different approach is required.
-
Squamous cell carcinomas are extremely rare in children.
-
Hemangiomas; propranolol have evolved to become the first-line treatment modality in the proliferative period.
-
Sirolimus has recently been used for their antilymphangiogenic properties in treating LM.
References
Greene AK, Kim S, Rogers GF, Fishman SJ, Olsen BR, Mulliken JB. Risk of vascular anomalies with Down syndrome. Pediatrics. 2008;121(1):e135–40.
Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69(3):412–22.
Fin MD, Glowacki J, Mulliken JB. Congenital vascular lesions: clinical application of a new classification. J Pediatr Surg. 1983;18:894.
North PE, Waner M, Mizeracki A, Mihm MC Jr. GLUT1: a newly discovered immunohistochemical marker for juvenile hemangiomas. Hum Pathol. 2000;31(1):11–22.
Mulliken JB, Fishman SJ, Burrows PE. Vascular anomalies. Curr Probl Surg. 2000;37(8):517–84.
Frongia G, Byeon J-O, Arnold R, Mehrabi A, Günther P. Cardiac diagnostics before oral propranolol therapy in infantile hemangioma: retrospective evaluation of 234 infants. World J Pediatr. 2018;14(3):254–8. https://doi.org/10.1007/s12519-018-0137-7.
Archauer BM, Celikoz B, Vanderkam VM. Intralesional bare fiber laser treatment of hemangioma of infancy. Plast Reconstr Surg. 1998;101:1212–7.
Shirley MD, Tang H, Gallione CJ, Baugher JD, Frelin LP, Cohen B, North PE, Marchuk DA, Comi AM, Pevsner J. Sturge-Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. N Engl J Med. 2013;368(21):1971–9.
Lee JW, Chung HY. Capillary malformations (Portwine stains) of the head and neck: natural history, investigations, laser, and surgical management. Otolaryngol Clin North Am. 2018;51(1):197–211.
Boon LM, Mulliken JB, Enjolras O, Vikkula M. Glomuvenous malformation (glomangioma) and venous malformation: distinct clinicopathologic and genetic entities. Arch Dermatol. 2004;140(8):971–6.
Graham JM, Scadding GK, Bull P. Pediatric ENT. Berlin: Springer-Verlag; 2008.
Kaur N, Gupta A, Amratash M, Singh N. Giant cystic hygroma of the neck with spontaneous rupture. J Indian Assoc Pediatr Surg. 2007;12:154.
Hammill AM, Wentzel MS, Gupta A, Nelson S, Lucky A, Elluru R, Dasgupta R, Azizkhan RG, Adams DM. Sirolimus for the treatment of complicated vascular anomalies in children. Pediatr Blood Cancer. 2011;57:1018–24.
Albright JT, Topham AK, Reilly JS. Pediatric head and neck malignancies: US incidence and trends over 2 decades. Arch Otolaryngol Head Neck Surg. 2002;128:655–9.
Isaacson PG. The revised European American lymphoma REAL classification. Clin Oncol (R Coll Radiol). 1995;7(6):347–8.
Hudson MM, Donaldson SS. Hodgkin’s disease. Pediatr Clin North Am. 1997;44:891–906.
Patte C. Non-Hodgkin’s lymphoma. Eur J Cancer. 1998;34:359–62.
Parham DM, Barr FB. Classification of rhabdomyosarcoma and its molecular basis. Anat Pathol. 2013;20(6):387–97.
Pappo AS, Shapiro DN, Crist WM. Rhabdomyosarcoma: biology and treatment. Pediatr Clin North Am. 1997;44:953–72.
Newman KD, Black T, Heller G, et al. Differentiated thyroid cancer: determinants of disease progression in patients <21 years of age at diagnosis. A report from the Surgical Discipline Committee of the Children’s Cancer Group. Ann Surg. 1998;227:533–41.
Segal K, Shvero J, Stern Y, et al. Surgery of thyroid cancer in children and adolescents. Head Neck. 1998;20:293–7.
Jocham A, Joppich I, Hecker W, et al. Thyroid carcinoma in childhood: management and follow up of 11 cases. Eur J Pediatr. 1994;153:17–22.
Haase GM. Head and neck neuroblastoma. Sem Pediatr Surg. 1994;3:194–202.
Weinstein JL, Katzenstein HM, Cohn SL. Advances in the diagnosis and treatment of neuroblastoma. Oncologist. 2003;8:278–92.
Mertens R, Granzen B, Lassay L, et al. Nasopharyngeal carcinoma in childhood and adolescence. Cancer. 1997;80:951–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Abdulkader, F., Mukhtar, N.E.E. (2021). Pediatric Head and Neck Vascular Anomalies and Tumors. In: Al-Qahtani, A., Haidar, H., Larem, A. (eds) Textbook of Clinical Otolaryngology. Springer, Cham. https://doi.org/10.1007/978-3-030-54088-3_59
Download citation
DOI: https://doi.org/10.1007/978-3-030-54088-3_59
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-54087-6
Online ISBN: 978-3-030-54088-3
eBook Packages: MedicineMedicine (R0)