Abstract
Robotic surgery approval for clinical use by the FDA in 2000 has been applied to several surgical procedures in urology, cardiac surgery, and gynecology.
The minimally invasive surgical approach in colorectal surgery supports the use of the laparoscopic method compared with the open surgery; laparoscopy reduces rates of postoperative complications and shows significant reductions in length of stay while providing equivalent oncologic outcomes.
General surgery has adopted robotic assistance more frequently, and robotic colorectal surgery may be a way to overawe the limitations of laparoscopic surgery and current evidence recently demonstrated that it is a safe and feasible option in colorectal surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 History
The history of minimally invasive surgery began with the efforts of physicians to explore human cavities for diagnostic and therapeutic purposes with minimal surgical trauma.
As early as 1902, Kelling, a German surgeon from Dresden, reported the first endoscopic visualization of the peritoneal cavity by reporting the first actual laparoscopy performed in a canine model. Kelling made it by inserting a “Nitze cystoscope” in the peritoneal cavity of a living dog under anesthesia and examined the viscera [1].
Over the next several decades, laparoscopic surgery evolved and was finally introduced into general surgery in the 1980s; when the first laparoscopic appendectomy was performed in 1983 reported by Semm [2], years after that in 1987, the first laparoscopic cholecystectomy was performed [3].
Laparoscopic colorectal surgery was first described in 1991, in 20 patients for Jacobs, Verdeja, and Goldstein [4].
Endoscopic surgery continues to grow as an important tool used by almost all the surgical fields with multiple advantages from open surgery demonstrated by several trials on the coloproctology field as seen in the Clinical Outcomes of Surgical Therapy (COST) study, and the Conventional versus Laparoscopic-Assisted Surgery in Colorectal Cancer (CLASICC) trial; the Colon Cancer Laparoscopic or Open Resection (COLOR) trial, and the Barcelona trial have compared laparoscopic surgery with open surgery for colon cancer [5].
The laparoscopic advantages include improved postoperative recovery, reduced use of drugs and shorter length of stay, with similar rates of cancer recurrence complications and long-term survival.
Parallel to the time laparoscopic skills were developed, there where new technologies for minimally invasive surgery emerging. The most remarkable was the surgical robot. It was developed by Scott Fisher, PhD, at the National Aeronautics and Space Administration (NASA) Ames Research Center, and Joseph Rosen, MD (Department of Plastic Surgery, Stanford University, Palo Alto), in the mid-to-late 1980s, when they were working on telepresence [6].
The first non-laparoscopic device, the Unimation’s PUMA 560 system, was used in 1985 by Kwoh et al. to perform the first-documented robotic-assisted surgical procedure for a percutaneous brain biopsy [7].
The same system was used by Davies et al. to make a transurethral resection of the prostate (TURP) being a precursor of what would be named the PROBOT.
The ROBODOC system was the first robotic system to achieve a formal FDA approval and it was a machine designed to improve the precision of hip replacement surgery, with the first procedures being performed in 1992 [8].
The da Vinci robotic surgical system was introduced to the market in 1999. The da Vinci robotic system includes features to improve the laparoscopic deficits like a three-dimensional vision system, three arms, the EndoWrist technology. Originally created with three robotic arms, a fourth arm was added to the system in 2003, enhancing and upgrading the ability to manipulate and retract.
The “S” system released in 2006 included a high-definition vision and a multi-image display as the major complements to the already effective robot. And by the 2009, the “Si” system was launched with a dual console capacity for collaboration terms and for training and further enhancement of the visual system.
The final version of the system developed by Intuitive in 2014 is named “Xi” (Fig. 129.1) facilitating a multi-quadrant surgery, better optics systems, improvement in the process of arm positioning and port placement and the introduction of the Firefly imaging system that allows for direct visualization of tissue perfusion. Intuitive also added energy and stapling tools married to the armature.
These technologies together with laparoscopic surgery have become the predominant option for colon cancer; as an example, the proportion of laparoscopic colorectal cancer surgery in Korea increased from 42.6% to 64.7% until 2013.
The laparoscopic surgery has disadvantages such as tremors, the prolonged learning curve to achieve equivalent outcomes relative to open surgery, and the challenge in approaching the deep and narrow pelvis has been improved by the robotic system which provides exceptional ergonomics, EndoWrist technology, enhanced dexterity of movement, and a three-dimensional view [9].
In 2002, the first robotic colectomies were reported by Weber et al. for benign disease; Hashizume et al. reported the first colectomies for malignant disease; and in 2003, Guilianottie et al. reported the first proctectomy [10,11,12].
2 From Laparoscopic to Robotic Surgery
The robotic approach has many advantages over laparoscopic surgery in the colorectal field. The most important advantage is to assist in the most technically challenging steps, that is, low rectal dissection, intracorporeal suturing in rectopexy, high vessel ligation, and intracorporeal anastomosis in hemicolectomies. In addition to the advantages mentioned, there is less tissue trauma and lower intraoperative blood loss. The colorectal surgeries that are performed with the use of robotic assistance that have the most benefit are: right hemicolectomy, rectal cancer surgery, and ventral mesh rectopexy [13].
There have been many studies describing the advantages of the robotic and laparoscopic surgery over the conventional open surgery, like the “Michigan Surgical Quality Collaborative Study” with total of 10,054 patients. Overall complications and surgical site infections were significantly favorable for the laparoscopic and robotic compared with the open approach. Anastomotic leaks were significantly fewer for the laparoscopic and robotic approaches compared with the open approach [14]. The American College of Surgeons National Surgical Quality Improvement Program has a large database that was used to compare laparoscopic and robotic approaches in 11,477 patients undergoing colorectal surgery including both the abdominal and pelvic surgery, showing that conversion rates in the pelvis were less for robotic surgery when compared to laparoscopic surgery. Hospital length of stay was significantly shorter for robotic abdominal cases than for laparoscopic abdominal and pelvic cases. There were no significant differences in surgical site infection (SSI), organ/space SSI, wound complications, anastomotic leak, sepsis/shock, or need for reoperation within 30 day [15]. Many other studies collectively conclude that robotic surgery is safe and efficacious, with equivalent oncological outcomes and complication rates, but operative times are significantly longer. Length of stay has been shown to be shorter with lower rates of conversion to open surgery for pelvic surgery. Although there are higher costs associated with robotic surgery, they could be offset by decreased length of stay [16,17,18].
3 Obesity and Robotic Surgery
According to the World Health Organization classification, normal BMI ranges are from 18.5 kg/m2 to 25 kg/m2, overweight ranges from 25 kg/m2 to 30 kg/m2, and obesity is classified as a BMI of 30 kg/m2 or more [19].
Obesity can affect adverse surgical outcomes because it is associated with high rates of comorbidities. It is often associated with abnormal cardiorespiratory and metabolic function and hemostasis, which may predispose to morbidity and mortality after surgery. Also, it has been associated with postoperative complications such as deep vein thrombosis, wound infections, dehiscence, incisional hernias, and anastomotic leaks [20].
The da Vinci robot (Intuitive Surgical, Sunnyvale, CA, USA®) offers numerous advantages when compared to laparoscopy, including several degrees of motion, three-dimensional (3D) imaging, and superior ergonomics that enable easy and precise intracorporeal suturing, improved visualization, tremor-less precision, and forms the basis for the emergence of robotic techniques.
Robotic rectal surgery for cancer in obese patients is equally effective as in nonobese patients. The robotic platform facilitates the obesity-related limitations of rectal surgery due to advantages in dexterity, visualization, and surgeon ergonomics [21, 22].
4 Intracorporeal Versus Extracorporeal Anastomosis for Minimally Invasive Right Colectomy
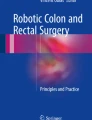
In the colorectal field, robotic surgery has been a revolutionary tool for the surgeon; talking about a right hemicolectomy (RHC), when performing a laparoscopic surgery, it has been difficult to make an intracorporeal ileocolic anastomosis, and for making an extracorporeal anastomosis using a laparoscopic approach, it is necessary to make additional mobilization of the colon to exteriorize the bowel through a mini-laparotomy incision. Some studies have shown benefits of the intracorporeal ileocolic anastomosis over the extracorporeal ileocolic anastomosis, such as faster return of bowel function, shorter length of stay, and reduced use of drugs [5]. It is safe, with no difference in rates of anastomotic leak, wound infection, or intra-abdominal abscess [23]. By taking advantage of the already-mentioned robotic surgery, cosmetic appearance and surgical outcomes going together with benefits such as wristed instruments may help overcome the difficulty of performing an intracorporeal anastomosis (Fig. 129.2).
A study was conducted by Trastulli et al. including 236 patients (robotic right colectomy with intracorporeal anastomosis = 102, laparoscopic right colectomy with extracorporeal anastomosis = 94, and laparoscopic right colectomy with intracorporeal anastomosis confectioning = 40). The three groups were comparable in their demographic and baseline characteristics. No significant differences were found in the conversion to open rates, intraoperative blood loss, 30-day morbidity and mortality, number of lymph nodes harvested and other pathological characteristics. Compared with the laparoscopic right colectomy with extracorporeal anastomosis, the robotic right colectomy with intracorporeal anastomosis required a longer operative time (P < 0.0001), but had better recovery outcomes , such as a shorter length of hospital stay (P < 0.0001). Compared with the laparoscopic, the robotic approach had a shorter time to first flatus (P < 0.0001), but offered no advantages in terms of the length of the hospital stay [24].
A case–control study in cancer patients by Morpurgo et al. compared robotic intracorporeal anastomosis (n = 48) with laparoscopic extracorporeal anastomosis (n = 48) and demonstrated earlier recovery of bowel function (day of first bowel movement 3 ± 1 days in the robotic group (RG) compared with 4.0 ± 1.2 days in the laparoscopic group; (p < 0.05), decreased hospital stay (robotic group: 7.5 ± 2.0 days vs. laparoscopic group: 9.0 ± 3.2 days; p < 0.05), lower incisional hernia rate (robotic group: 0 vs. laparoscopic group: 4), and lower anastomotic leak rate, and concluded that intracorporeal robotic anastomosis allows a faster recovery than laparoscopic surgery with extracorporeal anastomosis [25].
5 Left Colectomy and Low Anterior Resection
Robotic surgery improves the success of the intracorporeal anastomosis with low rates of leak and better access to the lower pelvis area, a robotic-assisted approach could potentially overcome the limitations of conventional laparoscopic rectal surgery and is particularly designed for procedures conducted in a small anatomical field in which precision is necessary.
Hand-sewn laparoscopic intracorporeal anastomosis is complex to perform and this procedure is more reliable by the robot, providing considerable benefits, especially in obese patients, with wide panniculus that require more force to manipulate and mobilize the short and heavy mesentery.
Recent literature shows that there was no difference between robotic and laparoscopic surgery regarding morbidity and anastomotic complications in left colon resection; some studies report that in left colectomy robotic surgery, patients had a significant shorter length of stay than the laparoscopic patient group (P = 0.003), with evidence of moderate heterogeneity, but the analysis included a total of 259 patients [24].
There are several techniques for robotic left colectomy:
-
Hybrid: accessing to multiple abdominal quadrants during robotic colorectal surgery procedures with laparoscopic splenic flexure take down
-
Single docking
-
Double docking
6 Near Future
The main technical limitation of robotic surgery is the decrease of tactile feedback but usually not rquired by the experienced robotic surgeon. The size of available robotic instruments could also become a limitation, making small fields almost impossible to be performed. The time to set up, and docking could be a minor technical limitation, it can be reduced to less than 5 minutes with practice [26].
Colon and rectal surgery stay in continuous development; robotic systems have multiple benefits, and many emerging areas have to be explored in the industry.
Robotic surgery has been shown to be useful for multiple platforms. These include single-port surgery, robotic natural orifice, transluminal endoscopic surgery, robotic transanal surgery, and endorobotics. Besides the Da Vinci platform, there have been many commercial biomedical companies making new technology in order to have more efficient and useful systems that surgeons can use for the benefit of patients [27].
7 Conclusions
Robotic surgery is constantly evolving and it provides several advantages over laparoscopic surgery in the colorectal field by advanced technologies including articulate instruments and motion scaling, especially when preforming an operation in the narrow pelvis space or in obese patients. There is evidence that proves that robotic colorectal surgery is safe and feasible and also has a place in surgical education using a dual console. The robotic surgery is a tool that can be used to create new approaches for helping patients.
References
Litynski GS. Laparoscopy—the early attempts: spotlighting Georg Kelling and Hans Christian Jacobaeus. JSLS. 1997;1(1):83–5.
Semm K. Endoscopic appendectomy. Endoscopy. 1983;15(02):59–64.
Blum C, Adams D. Who did the first laparoscopic cholecystectomy? J Minim Access Surg. 2011;7(3):165.
Jacobs M, Verdeja JC, Goldstein H. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1(3):144–50.
Cheng CL, Rezac C. The role of robotics in colorectal surgery. BMJ. 2018;360:j5304.
Satava RM. Surgical robotics: the early chronicles: a personal historical perspective. Surg Laparosc Endosc Percutan Tech. 2002;12(1):6–16.
Kwoh YS, Hou J, Jonckheere EA, Hayati S. A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng. 1988;35(2):153–60.
Cowley G. Introducing “Robodoc.” A robot finds his calling—in the operating room. Newsweek. 1992;120(21):86.
Cheong C, Kim NK. Minimally invasive surgery for rectal cancer: current status and future perspectives. Indian J Surg Oncol. 2017;8(4):591–9.
Weber PA, Merola S, Wasielewski A, Ballantyne GH. Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum. 2002;45(12):1689–94; discussion 1695–1696.
Hashizume M, Shimada M, Tomikawa M, Ikeda Y, Takahashi I, Abe R, et al. Early experiences of endoscopic procedures in general surgery assisted by a computer-enhanced surgical system. Surg Endosc. 2002;16(8):1187–91.
Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138(7):777–84.
Sivathondan P, Jayne D. The role of robotics in colorectal surgery. Ann Royal Coll Surg Engl. 2018;100(Supplement 7):42–53.
Batool F, Collins SD, Albright J, Ferraro J, Wu J, Krapohl GL, et al. A regional and national database comparison of colorectal outcomes. JSLS. 2018;22(4):e2018.00031.
Bhama AR, Obias V, Welch KB, Vandewarker JF, Cleary RK. A comparison of laparoscopic and robotic colorectal surgery outcomes using the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database. Surg Endosc. 2016;30(4):1576–84.
Tam MS, Kaoutzanis C, Mullard AJ, Regenbogen SE, Franz MG, Hendren S, et al. A population-based study comparing laparoscopic and robotic outcomes in colorectal surgery. Surg Endosc. 2016;30(2):455–63.
Tyler JA, Fox JP, Desai MM, Perry WB, Glasgow SC. Outcomes and costs associated with robotic colectomy in the minimally invasive era. Dis Colon Rectum. 2013;56(4):458–66.
Halabi WJ, Kang CY, Jafari MD, Nguyen VQ, Carmichael JC, Mills S, et al. Robotic-assisted colorectal surgery in the United States: a nationwide analysis of trends and outcomes. World J Surg. 2013;37(12):2782–90.
Ri M, Aikou S, Seto Y. Obesity as a surgical risk factor. Ann Gastroenterol Surg. 2018;2(1):13–21.
Harr JN, Luka S, Kankaria A, Juo Y-Y, Agarwal S, Obias V. Robotic-assisted colorectal surgery in obese patients: a case-matched series. Surg Endosc. 2017;31(7):2813–9.
Bayraktar O, Aytaç E, Özben V, Atasoy D, Bilgin İA, Erenler Bayraktar İ, et al. Does robot overcome obesity-related limitations of minimally invasive rectal surgery for cancer? Surg Laparosc Endosc Percutan Tech. 2018;28(1):e8–e11.
Gorgun E, Ozben V, Costedio M, Stocchi L, Kalady M, Remzi F. Robotic versus conventional laparoscopic rectal cancer surgery in obese patients. Colorectal Dis. 2016;18(11):1063–71.
Lee KH, Ho J, Akmal Y, Nelson R, Pigazzi A. Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc. 2013;27(6):1986–90.
Trastulli S, Coratti A, Guarino S, Piagnerelli R, Annecchiarico M, Coratti F, et al. Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicentre study. Surg Endosc. 2015;29(6):1512–21.
Morpurgo E, Contardo T, Molaro R, Zerbinati A, Orsini C, D’Annibale A. Robotic-assisted Intracorporeal anastomosis versus extracorporeal anastomosis in laparoscopic right hemicolectomy for cancer: a case control study. J Laparoendosc Adv Surg Tech. 2013;23(5):414–7.
Kim KC, editor. Robotics in general surgery [Internet]. New York, NY: Springer New York; 2014. [citado el 10 de diciembre de 2018]. Disponible en: http://springerlink.bibliotecabuap.elogim.com/10.1007/978–1-4614–8739–5
Toh JWT, Phan K, Kim S-H. Robotic colorectal surgery: more than a fantastic toy? Innov Surg Sci. 2018;3(1):65–8.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Davila, E.P., Hartmann, C., Rodríguez, C.E., Ali, A. (2021). Robotic Colorectal Surgery: General Considerations. In: Gharagozloo, F., Patel, V.R., Giulianotti, P.C., Poston, R., Gruessner, R., Meyer, M. (eds) Robotic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-53594-0_129
Download citation
DOI: https://doi.org/10.1007/978-3-030-53594-0_129
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53593-3
Online ISBN: 978-3-030-53594-0
eBook Packages: MedicineMedicine (R0)