Abstract
Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) represent a spectrum of severe, immune-mediated, mucocutaneous disease secondary to exposure to drugs or infection. SJS/TEN has up to a 35% mortality rate. Ocular sequelae are the most significant chronic complications of SJS/TEN in survivors. These chronic sequelae can be prevented or lessened by appropriate management in the acute phase of the disease. Visual prognosis and long-term health of the ocular surface lies in the presence and degree of acute eye and eyelid involvement. Amniotic membrane transplantation (AMT), when done correctly in the acute phase, has been shown to decrease chronic ocular surface disease from SJS/TEN. AMT involves the use of amniotic membrane, the innermost layer of the placenta, which consists of a thick basement membrane and an avascular mesenchymal layer. The exact mechanism by which AMT is beneficial is not fully understood, but amnion has antimicrobial and immunomodulatory properties and promotes epithelialization. This procedure can either be done at bedside or in the operating room. Patients who are in a burn intensive care unit and sedated may not need additional anesthesia, and the procedure can be done at bedside. Adults who are awake and alert can oftentimes have the procedure performed at bedside with local anesthetic only. Children who are awake and alert will need general anesthesia requiring an operating room setting. Since the last edition of this book, we have developed a new sutureless method which allows bedside application in virtually all patients with no general anesthesia required. This new sutureless method is also described below. The commercial source of amnion in the USA, Bio-Tissue, now has 10 × 5 cm amnion sheets available. However, if unavailable, three of the smaller 3.5 cm2 amnion pieces can be sutured together to create a single 3.5 × 10.5 cm piece.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Amniotic membrane
- Stevens
- Johnson syndrome
- Toxic epidermal necrolysis
- Ocular surface disease
- Ocular surface reconstruction
Indications
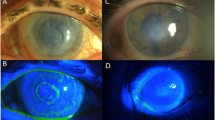
Ocular surface epithelial defects, pseudomembrane formation, or any eyelid margin defects during the first week after onset of SJS/TEN should be considered for AMT.
Essential Steps
-
1.
Fashion a custom-made symblepharon ring with IV tubing or use a ready-made symblepharon ring (Fig. 7.1)
-
2.
Upper and lower eyelashes trimmed
-
3.
Amniotic membrane (AM) laid over the eye with the basement membrane side up
-
4.
AM secured to the upper eyelid with or without bolsters
-
5.
AM deposited into upper fornix
-
6.
Symblepharon ring inserted
-
7.
AM deposited into lower fornix
-
8.
Symblepharon ring adjusted
-
9.
AM secured to lower eyelid with or without bolsters
-
10.
Excess AM trimmed
Amniotic membrane (AM) transplantation. utilizing a single 5 × 10 cm sheet. (a) Creation of symblepharon ring with intravenous tubing. (b) Placement of AM over upper eyelid. (c) Anchoring of AM using 6-0 polypropylene mattress sutures and bolsters. (d) Unfolding of AM over the ocular surface. (e) Placement of the custom-made symblepharon ring in the fornices. The ring is already pushed into the upper fornix and is being gently deposited into the lower fornix. (f) Anchoring of AM to lower eyelid. Permissions from: Elsevier Limited. Article: Ma KN, Thanos A, Chodosh J, Shah AS, Mantagos IS. A Novel Technique for Amniotic Membrane Transplantation in Patients with Acute Stevens-Johnson Syndrome. Ocular Surface Jan;14(1):31–6. https://doi.org/10.1016/j.jtos.2015.07.002. Epub 2015 Sep 24. Figure on Page 33
Complications
Very few complications reported. Those reported include:
-
Microbial infection (it is difficult to make any direct relationship between AMT and infection)
-
Hemorrhage beneath the amnion
-
Detachment of the membrane
Template Operative Dictation
Preoperative diagnosis:
(Stevens–Johnson syndrome/toxic epidermal necrolysis) with (right/left/bilateral) ocular involvement
Procedure:
Amniotic membrane transplantation (OD/OS/OU)
Postoperative diagnosis:
Same
Indication:
This ____-year-old (male/female) was admitted for management of SJS/TEN . Ophthalmic examination warrants placement of AMT. After a detailed review of risks and benefits, the patient (or legal surrogate if patient sedated) elected to undergo the procedure.
Description of the procedure (sutured):
The patient was identified in the holding area, and the (right/left/both) eye(s) was/were marked with a marking pen (or if done at bedside, indicate so). The patient was brought into the OR on an eye stretcher in the supine position. The patient was prepped in the usual sterile ophthalmic fashion. Non-adhesive drapes were used to protect the skin. After proper time-out was performed verifying correct patient, procedure, site, positioning, and special equipment prior to starting the case, local anesthesia was administered (if general anesthesia used, indicate so).
The distance between the superior and inferior orbital rims was measured at ___cm and used to estimate the diameter of the symblepharon ring to be constructed. Sterile intravenous tubing was cut so that one edge was oblique and the other edge blunt. The oblique edge was threaded into the blunt opening.
Attention was then turned to the patient’s (right/left) eye. The eyelashes were trimmed short. A _5 × 10_cm piece of amniotic membrane (Bio-Tissue, serial number __; exp. date __/__/__) was removed from its sterile packaging and placed over the eye with the basement membrane side up. Styrofoam bolsters made from the suture packaging (or plastic if IV tubing was used instead) were used to secure the amniotic membrane to the upper eyelid with 6-0 Prolene sutures in a partial thickness fashion about _2–3_ mm superior to the lash line.
An eyelid retractor was then used to lift the upper lid, allowing deposition of the amniotic membrane into the upper fornix. The previously fashioned symblepharon ring was then inserted into the upper fornix. The lower eyelid was then retracted to allow deposition of the amniotic membrane into the lower fornix. The membrane extending over the eyelid inferiorly was then sutured to the lower eyelid in the same manner as described above. Care was taken to spread the membrane over the entire ocular surface. Excess membrane was trimmed with Westcott scissors.
Description of the procedure (sutureless):
The patient was identified at bedside, and the (right/left/both) eye(s) was/were marked with a marking pen. The patient was prepped in the usual sterile ophthalmic fashion. Non-adhesive drapes were used to protect the skin (this is a substerile procedure and draping is at discretion of the surgeon). After a time-out was performed verifying correct patient, procedure, site, positioning, and special equipment prior to starting the case, topical anesthetic was administered.
The distance between the superior and inferior orbital rims was measured at ___cm and used to estimate the diameter of the symblepharon ring to be constructed. Sterile intravenous tubing was cut so that one edge was oblique and the other edge blunt. The oblique edge was threaded into the blunt opening (Fig. 7.2).
Sutureless amniotic membrane transplantation. (a) Upper and lower eyelashes are trimmed. (b) Cyanoacrylate glue is used to secure the amniotic membrane (AM) sheet (5 × 10 cm) to the upper eyelid. Care is taken to ensure glue is placed at least 4 mm above the eyelid margin. (c) AM is held across the upper eyelid for 30 seconds to ensure adhesion. (d) Desmarres lid retractor is used to retract the upper eyelid to allow the symblepharon ring to be placed in the superior fornix. (e) The symblepharon ring is then tucked into the inferior fornix. (f) The inferior margin of the AM is secured to the lower eyelid with cyanoacrylate glue. The patient should be able to close the eye without any lagophthalmos caused by the symblepharon ring. Permissions from: Elsevier Limited. Article: Shanbhag SS, Chodosh J, Saeed HN. Sutureless amniotic membrane transplantation with cyanoacrylate glue for acute Stevens-Johnson syndrome/toxic epidermal necrolysis. Ocular Surface. 2019 Jul;17(3):560–564. https://doi.org/10.1016/j.jtos.2019.03.001. Epub 2019 Mar 11
Attention was then turned to the patient’s (right/left) eye. The eyelashes were trimmed short. A 5 × 10 cm piece of amniotic membrane (Bio-Tissue, serial number; exp. date __/__/__) was removed from its sterile packaging and placed over the eye with the basement membrane side up. Cyanoacrylate glue was then applied 4 mm above the eyelid margin to secure the amniotic membrane to the upper eyelid.
An eyelid retractor was then used to lift the upper eyelid, allowing deposition of the amniotic membrane into the upper fornix. The previously fashioned symblepharon ring was then inserted into the upper fornix. The lower eyelid was then retracted to allow deposition of the amniotic membrane into the lower fornix. The membrane extending over the eyelid inferiorly was then glued in the same manner as described above, 4 mm away from the eyelid margin. Care was taken to spread the membrane over the entire ocular surface. Excess membrane was trimmed with Westcott scissors.
If procedure was performed bilaterally – Attention was then turned to the patient’s (left/right) eye, and the same exact procedure was then performed using another _ 5 × 10 _cm piece of amniotic membrane (Bio-Tissue, serial number __; exp. date __/__/__).
The drapes were removed and (antibiotic/steroid) ointment was placed on the eye(s). The patient tolerated the procedure well (and was transferred to the recovery room in stable condition—if done in operating room).
Additional Resource
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Saeed, H.N., Mantagos, I.S., Chodosh, J. (2021). Amniotic Membrane Transplantation in Stevens–Johnson Syndrome. In: Rosenberg, E.D., Nattis, A.S., Nattis, R.J. (eds) Operative Dictations in Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-030-53058-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-53058-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53057-0
Online ISBN: 978-3-030-53058-7
eBook Packages: MedicineMedicine (R0)