Abstract
Current alternatives for xenograft use in correction of lower eyelid retraction are reviewed, together with strategies for patient evaluation, typical surgical techniques, and postoperative management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Retraction
- Xenograft
- Porcine
- Bovine
- Porous polyethylene
- Hyaluronic acid
- Polytetrafluoroethylene
- Lamella
- Paralytic
- Cicatricial
- Eyelid surgery
Introduction
Although the exact incidence of lower eyelid retraction is not known, it is a relatively common involutional malposition seen in the elderly, and is also frequently seen as a complication of facial, orbital, and lower eyelid surgery; facial trauma and burns; thyroid eye disease; facial neuropathy; and cicatrizing diseases of the conjunctiva. Associated symptoms may include redness, tearing, burning, and foreign body sensation, while clinical signs may include superficial keratitis and bacterial keratitis. Surgical treatment is aimed at improvement in the eyelid malposition with resolution of signs and symptoms when lubricating ointments and other medical therapies are ineffective.
Evaluation
Since lower eyelid position relative to the cornea is dependent on the direction of gaze and the orientation of the patient’s head, examination and photographic documentation for possible lower eyelid retraction should use a reproducible standard head orientation such as the Frankfort plane, the frontal plane, or natural head position [1], with the patient’s eyes in primary gaze. Measurements (in millimeters) are commonly made either relative to the limbus as inferior scleral show (ISS) or relative to the corneal light reflex as margin-reflex distance 2 ( MRD2). In any of the standard positions, the lower eyelid normally rests at the inferior limbus for younger patients. For older persons, horizontal laxity of the lower eyelid is associated with gradual descent [2], resulting in increased ISS and MRD2 measurements. Instead, pathological descent of the lower eyelid can be caused by facial trauma and burns; thyroid eye disease; facial neuropathy; cicatrizing diseases of the conjunctiva; and iatrogenically by facial, orbital, or lower eyelid surgery. Lower eyelid retraction can be identified by an ISS > 0 and/or an MRD2 > 6 and a classification scheme has been suggested by Bartley [3].
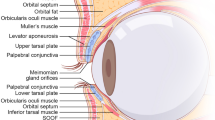
Standard oculoplastic examination will also disclose concomitant rotational malpositions of the lower eyelid, such as ectropion and entropion, laxity of the canthal tendons, orbicularis oculi weakness, and diseases of the skin, conjunctiva, and cornea. It is also important to measure resistance to passive lid movement (RPLM) . In the absence of pathology in the anterior, middle, or posterior lamellae of the eyelid, an examiner can passively move the typical lower eyelid upward approximately 1 cm with little resistance and without rotation of the globe. When present, RPLM can be documented on a severity scale (e.g., 0–3+) and the examination will usually reveal whether the restriction is primarily in the posterior, middle, or anterior lamella. Restriction in the posterior or middle lamellae will frequently require spacer graft correction, as well as repair of any horizontal laxity or anterior lamellar insufficiency (see following chapters). Spacer grafts in the posterior lamella have become accepted as an important part of surgical treatment for lower eyelid retraction [4].
Xenograft Options
For many reasons, autologous tissues have been generally preferred as spacer grafts for correction of lower eyelid retraction, and other chapters discuss the use of hard palate, auricular or nasal septal cartilage, dermis, and composite dermis-fat grafts. However, some patients will refuse harvest of autologous tissues, and sometimes, harvest of autologous tissues is inappropriate or not possible due to previous surgery or disease. Allografts from another nongenetically identical human (e.g., preserved sclera, human-derived acellular dermal matrix [cadaveric: Alloderm®, noncadaveric: Belladerm®]) may be considered, but xenografts from different species are commercially available and are often utilized. Also, in this category are a variety of bioengineered spacers manufactured for human reconstructive surgery.
Acellular cross-linked porcine collagen (Enduragen ®) is a flexible implant intended for reconstruction in the head and neck. It does not require hydration prior to use and provides a scaffold for fibroblast infiltration and vascularization. It is available in several sizes, with thickness of 0.5 mm and 1.0 mm. It does not require coverage with conjunctiva from the patient. Unlike human-derived acellular dermal matrix, it does not contain basement membrane and requires no special intraoperative orientation. Dailey et al. [5] have published the largest retrospective series using Enduragen®; they reported mean improvement in MRD2 of about 1 mm at 14 months among 160 eyelids, with few complications. Similar results were noted by McCord et al. [6] in 129 eyelids. A prospective, randomized comparative trial among Enduragen®, auricular cartilage, and Surgimend® (see below) for 42 retracted lower eyelids reported an average improvement in MRD2 of 2.3 mm at 6 months, with no significant difference between the three materials [7].
Fetal bovine acellular dermal matrix (Surgimend ®) is rich in types I and III collagen. It is available in one thickness that varies from 0.75 to 1.54 mm and must be prehydrated for approximately 5 minutes prior to implantation. It has been extensively studied in breast reconstruction, but few reports are available regarding its use in eyelids [8]. However, as noted above, Barmettler and Hai reported no significant difference in clinical results in a prospective, randomized trial among auricular cartilage, acellular porcine collagen, and bovine acellular dermal matrix [7].
Decellularized porcine-derived membrane (TarSys ®) derived from small intestine submucosa and consisting of collagen types I, III, and VI with glycosaminoglycan matrix similar to tarsus has been used for correction of lower eyelid retraction. It is manufactured in only one size (1 × 4 cm) and must be rehydrated for 20 minutes prior to implantation. The smoother side is preferred for epithelialization. Borrelli et al. [9] initially reported successful use of TarSys® for eyelid retraction in 2012, and Liao et al. [10] subsequently reported its successful use in 32 patients with TED, noting a mean improvement in MRD2 of 1.4 mm without significant complications. A recent case report documented florid inflammation in one patient following TarSys® implantation [11].
A bilayer matrix (Integra ®) is a more rigid option, consisting of a porous dermal replacement layer of bovine collagen and glycosaminoglycan to promote neodermal formation and an epidermal layer of polysiloxane to provide a moisture and bacterial barrier. It has been approved by FDA for burns and treatment of scar contracture; it was designed to precede epithelial autografting (immediately following removal of the polysiloxane layer at 14–21 days). However, it has been used successfully without secondary epithelial autograft in correction of lower eyelid retraction and cicatricial entropion [12].
Porous Polyethylene (Medpor ®) eyelid spacers are manufactured in one size (42 × 20 × 0.35 mm) but can be customized intraoperatively. They are typically placed using an infraciliary (subciliary) transcutaneous approach, secured to the inferior tarsal border and periosteum at the orbital rim, and have been shown to biointegrate [13]. Conjunctiva is necessary to cover the posterior surface of the spacer. A prospective study showed significant improvement in ISS, MRD2, lagophthalmos, and palbebral fissure size using porous polyethylene inserted preseptally via an infraciliary incision [14]. However, 15/32 patients had minor or major complications that required additional surgery and the authors recommended using the implant sparingly. Other authors have reported high incidence of eyelid contour deformities, malpositions, and exposure, and this implant is now used less frequently [15, 16].
Polytetrafluoroethylene (e-PTFE, Gore-Tex ®) was initially described for use in eyelid reconstruction by Karesh et al. [17, 18] and has been since used extensively for frontalis sling ptosis repair. Intraoperative perforation of the material with a 21-gauge needle may facilitate fibrovascular ingrowth. It is potentially more useful when placed in the middle lamella using a transcutaneous approach, since it typically extrudes if not covered completely by conjunctiva [19].
Hyaluronic acid gel injection for lower eyelid retraction was initially described by Goldberg et al. [20] as a temporary alternative to the surgical spacer grafting as discussed above. They noted an improvement in ISS of 1 mm lasting 3–6 months using hyaluronic acid (Restylane®) injected in the region of the orbital septum and lower lid retractors. A larger particle preparation (Perlane®) has also been described [21]. Similar results have been published by other authors [22], and the technique involves placement of multiple threadlike aliquots of gel posterior to the orbicularis oculi using a 30-gauge needle. Correction typically requires about 1 cc of gel injected per eyelid. The hyaluronic acid gels that are less hydrophilic (e.g., Restylane®, Perlane®, Belotero®) are preferred over those that are more hydrophilic (e.g., Juvéderm®) to avoid the possibility of prolonged superficial edema. Details of these injections will be further discussed in another chapter.
Surgical Techniques
Porous polyethylene and polytetrafluoroethylene implants each require complete coverage by conjunctiva to protect the globe from the implant, and are most successful when implanted via an infraciliary transcutaneous approach. The other xenografts can be successfully implanted via the transconjunctival approach, since conjunctiva will grow over their posterior surfaces in the early postoperative period. Both approaches may be combined with lateral canthal tightening procedures as indicated, and can be accomplished with a local anesthetic mixture such as 1% lidocaine with 1:100,000 epinephrine and 0.75% bupivacaine. Intravenous sedation may be useful in selected patients.
The transconjunctival approach is straightforward and can be performed with local anesthetic subconjunctival and subcutaneous infiltration and topical corneal anesthetic such as proparacaine 0.5%. The steps are as follows:
-
1.
Place a traction suture at the lower eyelid margin. This can be accomplished with a suture passed in the coronal plane in the gray line without bolsters (see Fig. 12.1a, b) or as a mattress suture through the skin using a bolster.
-
2.
With the eyelid everted using the traction suture, create a transconjunctival incision 1 mm inferior to the inferior tarsal border and develop a dissection plane anterior to the conjunctiva and capsulopalpebral fascia, but posterior to the orbital fat. Release any scar that prevents upward mobilization of the eyelid, taking care to avoid perforation through the lower eyelid skin.
-
3.
Measure the newly created posterior lamellar defect horizontally and vertically with the eyelid held in a mildly overcorrected position. The typical width will be 20–30 mm, and the typical height will be 7–9 mm.
-
4.
If necessary, hydrate the selected xenograft implant, and trim it to size according to your measurements. The orientation does not matter for acellular cross-linked porcine collagen (Enduragen®) or for fetal bovine acellular dermal matrix (Surgimend®). However, for decellularized porcine-derived membrane (TarSys®), the smooth side should be positioned toward the globe, while for the bilayer matrix (Integra®), the clear polysiloxane layer is placed toward the globe (Fig. 12.2).
-
5.
Secure the superior edge of the xenograft to the inferior border of the tarsus with partial thickness, buried, interrupted, or running 6-0 absorbable suture to avoid corneal irritation (Fig. 12.3). Polyglactin 910 is preferred over chromic or plain gut to provide longer-term fixation.
-
6.
Fixate the inferior edge of the xenograft to the superior edge of the retractors with buried interrupted absorbable sutures.
-
7.
A lateral canthoplasty with tarsal strip or other canthal tightening procedure can be accomplished concomitantly if horizontal laxity is present.
-
8.
The traction suture can be temporarily secured to the forehead with steri-strips and benzoin as a Frost suture, if desired (Fig. 12.4). For recalcitrant, recurrent cicatrix, longer-term upward postoperative traction can be obtained with suture passage through the upper eyelid margin and fixation to the forehead (Fig. 12.5). Using 2 mattress sutures allows for a wider, more stable eyelid traction by distributing tension, and the 5-0 polypropylene is nonreactive for up to a month.
Traction sutures: (a) The suture needles can be placed through the eyelid margin gray line, and help place the eyelid on vertical traction when dissecting transcutaneously, (b) This double-pass technique for Frost traction sutures has several advantages – intraoperatively, it allows for a wider, more stable eyelid traction, and postoperatively, there is minimal damage to the gray line if pulled out inadvertently, and 5-0 polypropylene is nonreactive for up to a month
The infraciliary, transcutaneous approach is also straightforward, although it requires more attention to the anatomy, particularly for eyelids with extensive scarring. It can be performed with local anesthetic subconjunctival and subcutaneous infiltration, often with intravenous sedation. The steps are as follows:
-
1.
Mark the intended infraciliary incision. It can be modified slightly depending on the type of planned traction suture.
-
2.
Place a traction suture at the lower eyelid margin. This can be accomplished with a suture passed in the coronal plane in the gray line without bolsters (Fig. 12.1a) or as a mattress suture through the skin using a bolster. The eyelid is then pulled upward (Fig. 12.1b).
-
3.
Create the infraciliary incision and dissect inferiorly in the subcutaneous plane, minimizing injury to the pretarsal orbicularis oculi muscle. At approximately 5 mm inferior to the eyelid margin, transition to a dissection plane posterior to the preseptal orbicularis muscle. The orbital septum is typically visible as an avascular, white plane, and with further inferior dissection, fat can be discerned deep to the orbital septum.
-
4.
For porous polyethylene implants, a pocket is created anterior to the septum inferiorly to the orbital rim. The implant is trimmed and the medial and lateral edges bent to avoid anterior winging. It may be soaked in antibiotic solution, and contact with the skin should be avoided. For more rigid support of the lower eyelid, the inferior edge of the implant is secured to the arcus marginalis periosteum at the inferior orbital rim. When less rigidity is required, an incision can be created in the orbital septum just above the orbital rim, permitting the implant to slide posteriorly and inferiorly into the orbit to retain eyelid motility.
-
5.
In either case, the superior edge of the implant is sutured to the inferior tarsal border with absorbable sutures. Polyglactin 910 is preferred over chromic or plain gut to provide longer-term fixation.
-
6.
For polytetrafluoroethylene, the superior septum can be opened transversely and the orbital fat teased away from the capsulopalpebral fascia, located posterior to the fat. The capsulopalpebral fascia is loosely adherent to the palpebral conjunctiva and must be disinserted from the tarsus superiorly and carefully dissected away from the conjunctiva so that it is recessed inferiorly. Assuming that the conjunctiva itself is not scarred, release of these layers should provide upward mobilization of the lower eyelid. The polytetrafluoroethylene spacer may be soaked in antibiotic solution, and contact with the skin should be avoided. It can then be customized to reduce the surgical defect between the intended location of the tarsus and the capsulopalpebral fascia and is secured to each with absorbable sutures. Polyglactin 910 is preferred over chromic or plain gut to provide longer-term fixation.
-
7.
Closure is then accomplished in two layers, with meticulous repair of the orbicularis muscle using polyglactin 910, and reapproximation of the skin with suture as desired. Lateral canthoplasty with a tarsal strip or other canthal tightening procedure can be accomplished concomitantly, if indicated.
-
8.
The traction suture can be temporarily secure to the forehead with steri-strips and benzoin as a Frost suture, if desired (Figs. 12.4 and 12.5).
Postoperative Care
Postsurgical wound care is similar to other eyelid surgeries. The patient is told to expect swelling and bruising for the first 1–2 weeks, and to apply cold compresses for the first 2 days while awake. Topical ophthalmic antibiotic ointment can be prescribed for use on skin sutures. Topical ophthalmic antibiotic-steroid combination eyedrops can be prescribed for use with conjunctival incisions. Systemic narcotics are usually not necessary.
Initial follow-up can be scheduled for 1 week postoperatively to check on eyelid position, consider removal of Frost sutures if used, and to examine the cornea for possible epithelial injury. Patients are instructed to call for an earlier appointment if persistent foreign body sensation is noted after the first day. The polysiloxane layer of the Integra® graft is usually well tolerated, but corneal abrasions from it or from sutures used with any of the xenografts are possible, and should be treated aggressively to prevent infectious keratitis. Prudent, earlier follow-up may be appropriate, especially for patients with corneal sensory neuropathy or pre-existing epitheliopathy.
For patients with Integra® grafts, follow-up between 3 and 8 weeks should be planned for removal of the polysiloxane layer in the office using topical anesthesia (Fig. 12.6). For all graft types, close follow-up during the first 6 months is advisable to manage complications and to evaluate surgical efficacy. Patients with negative vector orbit, such as proptosis from thyroid eye disease, may often require additional considerations for optimal correction, such as decompression of the orbit, orbital rim implants to decrease negative vector, or implants with more rigidity to vertically support the lower eyelid upwards (Figs. 12.7 and 12.8).
Patient with thyroid eye disease who underwent retraction repair with Enduragen® implants: (a) Preoperative lower eyelid retraction and several millimeters of inferior scleral show, (b) 1 week postoperatively, with edge of Enduragen® implant visible below tarsus, (c) 2 months postoperatively with improved lower eyelid position
Risks and Informed Consent
In addition to the general risks associated with eyelid surgery such as bleeding, infection, asymmetry, scarring, eyelash loss, pain, ectropion, suture problems, persistent malposition, need for further surgery, ocular injury, diplopia, and blindness, there are specific risks inherent in the use of xenografts. These include risk of disease transmission (not yet reported in the literature), late xenograft extrusion or failure, reduced lower eyelid mobility in downgaze, and inflammatory reactions. Late graft extrusion through the skin has been most commonly observed with porous polyethylene implants in up to 13% of patients [14].
Informed consent discussion with the patient regarding the risks, potential benefits, and alternatives to the use of xenografts is appropriate as part of the preoperative evaluation and surgical planning. Completion of a written or online record of informed consent is always necessary to document the discussion and the patient’s agreement to surgery. In rare cases, personal or religious beliefs may limit its use.
Summary/Conclusion
Xenografts can be useful in the surgical management of symptomatic lower eyelid retraction, carry the advantage of no donor site morbidity, and may be considered for use in selected patients. Surgical implantation techniques are similar to those used for correction of lower eyelid retraction with autologous human implants, with adequate scar release of paramount importance. Hyaluronic acid gel can be used for selected patients as a temporary, minimally invasive alternative administered in an office or clinic setting. Details for this technique are considered in the following chapter.
References
Naini FB. The Frankfort plane and head positioning in facial aesthetic analysis-the perpetuation of a myth. JAMA Facial Plast Surg. 2013;15:333–4.
Shore JW. Changes in lower eyelid resting position, movement, and tone with age. Am J Ophthalmol. 1985;99:415–23.
Bartley GB. The differential diagnosis and classification of eyelid retraction. Ophthalmology. 1996;103:106–13.
Oestreicher JH, Pang NK, Liao W. Treatment of lower eyelid retraction by retractor release and posterior lamellar grafting: an analysis of 659 eyelids in 400 patients. Ophthalmic Plast Reconstr Surg. 2008;24:207–12.
Dailey RA, Marx DP, Ahn ES. Porcine dermal collagen in lower eyelid retraction repair. Ophthalmic Plast Reconstr Surg. 2015;31:233–41.
McCord C, Nahai FR, Codner MA, et al. Use of porcine acellular dermal matrix (Enduragen) grafts in eyelids: a review of 69 patients and 129 eyelids. Plast Reconstr Surg. 2008;122:1206–13.
Barmettler A, Heo M. A prospective, randomized comparison of lower eyelid retraction repair with autologous auricular cartilage, bovine acellular dermal matrix (Surgimend), and porcine acellular dermal matrix (Enduragen) spacer grafts. Ophthalmic Plast Reconstr Surg. 2018;34:266–73.
Sun J, Liu X, Zhang Y, et al. Bovine acellular dermal matrix for levator lengthening in thyroid-related upper-eyelid retraction. Med Sci Monit. 2018;24:2728–34.
Borrelli M, Unterlauft J, Kleinsasser N, et al. Decellularized porcine derived membrane (Tarsys) for correction of lower eyelid retraction. Orbit. 2012;31:187–9.
Liao SL, Wei YH. Correction of lower lid retraction using tarSys bioengineered grafts for graves ophthalmopathy. Am J Ophthalmol. 2013;156(2):387–92.
Mancera N, Schneider A, Margo CE, et al. Inflammatory reaction to decellularized porcine-derived xenograft for lower eyelid retraction. Ophthalmic Plast Reconstr Surg. 2019;35:e95–7.
Burkat CN, Hawes MJ, Willoughby B, Fante, RG. Silicone scaffold support using the bilayer dermal regeneration matrix template (Integra) for correction of complex or recurrent lower eyelid retraction. Presented at the Fall 2019 Meeting of the American Society of Ophthalmic Plastic and Reconstructive Surgery, San Francisco, California.
Mavrikakis I, Francis N, Poitelea C, et al. Medpor lower eyelid spacer: does it biointegrate? Orbit. 2009;28(1):58–62.
Tan J, Olver J, Dickinson AJ. The use of porous polyethylene (Medpor) lower eyelid spacers in lid heightening and stabilization. Br J Ophthalmol. 2004;88:1197–200.
de Jong-Hesse Y, Paridaens DA. Correction of lower eyelid retraction with a porous polyethylene (Medpor) lower eyelid spacer. Klin Monatsbl Augenheilkd. 2006;223:577–82.
Wong JF, Soparkar CN, Patrinely JR. Correction of lower eyelid retraction with high density porous polyethylene: the Medpor lower eyelid spacer. Orbit. 2001;20:217–25.
Karesh JW, Fabrega MA, Rodrigues MM, Glaros DS. Polytetrafluoroethylene as an interpositional graft material for the correction of lower eyelid retraction. Ophthalmology. 1989;96:419–23.
Karesh JW. Polytetrafluoroethylene as a graft material in ophthalmic plastic and reconstructive surgery. An experimental and clinical study. Ophthalmic Plast Reconstr Surg. 1987;3:179–85.
Lee YJ, Khwarg SI. Polytetrafluoroethylene as a spacer graft for the correction of lower eyelid retraction. Korean J Ophthalmol. 2005;19:247–51.
Goldberg RA, Lee S, Jayasundera T, et al. Treatment of lower eyelid retraction by expansion of the lower eyelid with hyaluronic acid gel. Ophthalmic Plast Reconstr Surg. 2007;23:343–8.
Peckinpaugh JL, Reddy HS, Tower RN. Large particle hyaluronic acid gel for the treatment of lower eyelid retraction associated with radiation-induced lipoatrophy. Ophthalmic Plast Reconstr Surg. 2010;26:377–9.
Zamani M, Thyagarajan S, Olver JM. Functional use of hyaluronic acid gel in lower eyelid retraction. Arch Ophthalmol. 2008;126:1157–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fante, R.G. (2020). Lower Eyelid Retraction: Middle/Posterior Lamellar Correction Using Xenografts. In: Hartstein, M.E., Burkat, C.N., Ramesh, S., Holds, J.B. (eds) Avoiding and Managing Complications in Cosmetic Oculofacial Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-51152-4_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-51152-4_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-51151-7
Online ISBN: 978-3-030-51152-4
eBook Packages: MedicineMedicine (R0)