Abstract
Parkinson’s disease (PD) is the second most common neurodegenerative disease and occurs with motor and non-motor symptoms. Among non-motor symptoms, cognitive decline is a highly prevalent symptom and strongly related to quality-of-life deterioration and functional disability. Patients experience cognitive impairment in a wide range of cognitive domains, including executive functions, attention, and memory. These cognitive symptoms progress until dementia occurs in PD; hence, treatment strategies for cognitive decline are needed. In this line, some studies have analyzed the effects of cognitive rehabilitation on cognition, functional outcome, and brain changes in PD patients.
The present chapter starts with an introductory section on the neuropathological process of the disease, the diagnostic criteria, the disease stages, and an overview of the available treatments for symptom relief. Then, the chapter focuses on the cognitive deficits in the disease and later describes the brain’s structural and functional neural correlates of these cognitive alterations. Later, an up to date of the effects of cognitive rehabilitation in PD is performed, with special emphasis on the efficacy on cognition, quality-of-life aspects, brain changes, and the longitudinal maintenance of these changes. Future directions on this matter are discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction to Parkinson’s Disease
Discovery, Incidence, and Cellular Explanation
Parkinson’s disease (PD) is the second most common neurodegenerative disease after Alzheimer’s disease, and its incidence is directly related to age (Hirsch, Jette, Frolkis, Steeves, & Pringsheim, 2016). PD was first described in 1817 by James Parkinson in a report entitled “An Essay on the Shaking Palsy.” Later, Jean-Marie Charcot made important contributions by defining the clinical features of “the shaking palsy” and proposed to change the name to “Parkinson’s disease” in honor of James Parkinson.
Most PD cases are idiopathic, but there is a small percentage of patients (3–5%) who have genetic factors (Klein & Westenberger, 2012). The causes of idiopathic PD are still unknown, but seem to be related to both genetic and environmental influences (Kalia & Lang, 2015). Exposure to pesticides and a head injury have been associated with an increased risk of developing PD, whereas exposure to both the factors triples the risk of PD diagnosis (Lee, Bordelon, Bronstein, & Ritz, 2012).
PD motor symptoms start with the neurodegeneration of the nigro-striatal pathway. The loss of dopaminergic neurons in the substantia nigra produces a reduction in the activation of the thalamo-cortical activity which triggers PD symptomatology (Del Tredici, Rub, De Vos, Bohl, & Braak, 2002). The neuropathological process of PD was described by Braak and colleagues in 2003 and was divided into six stages (Braak, Rüb, Gai, & Del Tredici, 2003). Stage 1 is characterized by early lesions in the olfactory bulb and the dorsal motor nucleus of the vagus nerve; stage 2 begins when the lesions appear in the lower raphe nuclei, locus coeruleus, and reticular nucleus; stage 3 includes the degeneration of the substantia nigra pars compacta and amygdala; the first cortical lesions appear in stage 4, located at the mesocortex; stage 5 is characterized by the atrophy of the secondary somatomotor areas and prefrontal cortex; finally, stage 6 of the disease involves cortical degeneration of the whole brain, including the primary somatosensory areas and premotor areas. These stages have been divided into the “presymptomatic phase” (from stage 1 to stage 3) and the “symptomatic phase” (from stage 4 to stage 6) (Braak, Ghebremedhin, Rüb, Bratzke, & Del Tredici, 2004).
Motor and Non-motor Symptoms
The first description of the disease made by James Parkinson in 1817 reported only the motor disturbances. The core motor symptoms that characterize the disease are rigidity, tremor, bradykinesia, and postural instability. In addition, freezing of gait (difficulty to initiate or continue walking) and flexed posture have been included in the cardinal motor symptoms of the disease (Xia & Mao, 2012).
At present, it is known that this neurodegenerative process produces a wide range of motor and non-motor symptoms in PD patients; hence, PD is considered a multiple system neurodegenerative disorder (Tolosa, Gaig, Santamaria, & Compta, 2009). Indeed, some non-motor symptoms have been suggested to appear even before motor symptoms, such as olfactory loss, cognitive impairment, sleep disturbances, mood disorders, dysautonomia, excessive sweating, and fatigue (Pont-Sunyer et al., 2015; Tolosa et al., 2009).
The first non-motor symptom to appear in PD is olfactory loss (Haehner et al., 2009), corresponding to stage 1 of the Braak staging scheme for PD (Braak et al., 2004). The prevalence of smell loss in PD ranges from 45% (Ansari & Johnson, 1975) to 90% (Doty, Deems, & Stellar, 1988). The high prevalence of this symptom makes it a good clinical biomarker for early diagnosis (Ross et al., 2008). Another common non-motor symptom in PD is REM sleep behavior disorder, as approximately 30% of PD patients suffer from sleep problems (Hu et al., 2015). In addition, 25% of patients also suffer from hallucinations, which are usually related to antiparkinsonian treatments (Fenelon, Mahieux, Huon, & Ziegler, 2000). Presence of visual hallucinations has also been associated with a higher risk of developing dementia (Ibarretxe-Bilbao et al., 2010). Mood disorders could appear from 2 to 10 years before motor symptoms (Pont-Sunyer et al., 2015), and the most common ones are apathy (Pagonabarraga, Kulisevsky, Strafella, & Krack, 2015) and depression (Aarsland, Påhlhagen, Ballard, Ehrt, & Svenningsson, 2012). Finally, dysautonomia is also a frequent non-motor symptom in PD. Symptoms of autonomic failure in patients with PD include constipation, urinary incontinence, and heat or cold intolerance (Goldstein, 2003). Finally, cognitive deterioration is an important non-motor symptom due to its prevalence among PD patients (Muslimovic, Post, Speelman, & Schmand, 2005), its relationship with quality of life (Leroi, McDonald, Pantula, & Harbishettar, 2012) and its progression to dementia (Hely, Reid, Adena, Halliday, & Morris, 2008).
Diagnosis
The most widely accepted clinical criteria for the diagnosis of PD are those introduced by the UK PD Society Brain Bank Diagnostic Criteria (Postuma et al., 2015). After the PD diagnosis, two tests are widely used to evaluate the evolution of the disease: The Unified PD Rating Scale (UPDRS) (Martinez-Martin et al., 1994) and the Hoehn and Yahr scale (Hoehn & Yahr, 1967). Both scales show a high correlation between them (Martinez-Martin et al., 1994). The UPDRS is composed of 42 items divided into four subscales: Mentation, Activities of Daily Living, Motor Section, and Treatment Complications. The Motor Section subscale of the UPDRS is the most widely used by researchers and clinicians. The Hoehn and Yahr scale measures motor dysfunction and was first divided into five stages (Hoehn & Yahr, 1967). Later, the modified Hoehn and Yahr scale included intermediate stages between them, describing a total of seven stages (Goetz et al., 2004) (see Table 7.1).
Treatments
The standard treatment for motor symptoms in PD is pharmacological treatment (Connolly & Lang, 2014). The most common pharmacological treatment is Levodopa, a drug that supplies the loss of dopamine in the disease. It is a very effective treatment, but it loses its efficacy as the disease progresses. Dopamine agonists are another common pharmacological treatment in PD, usually used as the initial treatment for young PD patients. Other treatments against PD motor symptoms are inhibitors of monoamine oxidase B (MAO-B), catechol-O-methyltransferase (COMT) inhibitors, and anticholinergics (Connolly & Lang, 2014).
When pharmacological treatments begin to lose efficacy, a surgical procedure is a common option that has been shown efficacy. The surgical intervention commonly used in PD is deep brain stimulation (DBS) (Okun, 2012).
These treatments (pharmacological and surgical) have shown to be effective against motor symptomatology; however, cognitive impairment and other non-motor symptoms are still present in the disease. Treatment strategies are needed to diminish these symptoms, but to date, no pharmacological treatments have demonstrated efficacy on the reduction of cognitive dysfunctions (Petersen et al., 2014). On the contrary, non-pharmacological therapies, such as cognitive rehabilitation, have demonstrated some efficacy against cognitive decline (Petersen et al., 2014), hence the importance of the cognitive rehabilitation approach in PD treatment.
Cognitive Impairment in PD
Cognitive impairment is a common non-motor symptom in PD. The percentage of PD patients with cognitive impairment ranges from 20 to 50% (Yarnall, Rochester, & Burn, 2013), and PD patients can develop cognitive impairment from the early stages of the disease (Muslimovic et al., 2005; Yarnall et al., 2014). These cognitive deficits deteriorate with the progression of the disease until dementia occurs (Hely et al., 2008).
Traditionally, cognitive deficits in PD have been related to a dysexecutive syndrome, due to the deterioration of the circuitry that connects the frontal cortex with subcortical structures (Litvan, Mohr, Williams, Gomez, & Chase, 1991). Nowadays, studies have shown that widespread brain deterioration is present in PD patients with cognitive impairment (Mak, Su, Williams, & O’Brien, 2015). The incidence of cognitive deficits in PD in a newly diagnosed cohort was first presented in 2004, in a study that showed that 36% of PD patients experienced cognitive impairment classified as frontostriatal impairment, temporal impairment, or global deterioration (Foltynie, Brayne, Robbins, & Barker, 2004). Another study with newly diagnosed PD patients indicated that cognitive impairment was present in diverse cognitive domains, such as attention, language, executive functions, visuospatial ability, and memory, although performance in most of the domains was determined by memory and executive functions (Muslimovic et al., 2005). A later study identified a twofold increase in mild cognitive impairment (MCI) in PD patients compared to healthy controls, which affected a wide range of cognitive domains, while the largest effect size was noted for verbal memory (Aarsland et al., 2009). Interestingly, memory deficits in PD have been traditionally related to impairment in the retrieval process, but learning is also altered in the disease and may underlie retrieval failure (Chiaravalloti et al., 2014). Furthermore, cognitive deficits related to alterations in posterior brain areas, such as visuospatial or semantic fluency, have been found to play a relevant role in the dementing process in PD (Williams-Gray, Foltynie, Brayne, Robbins, & Barker, 2007).
Other complex cognitive functions have also been found to be impaired in PD. Decision-making ability, defined as the ability to modify choice behavior depending on reward contingencies (short or long delay), has been widely examined in PD patients using the Iowa Gambling Task (IGT). Studies using the IGT showed a dysfunctional decision-making pattern in PD patients compared to healthy subjects (Poletti, Cavedini, & Bonuccelli, 2011). Finally, social cognitive abilities have also been found to be impaired in PD. Specifically, recognition of emotions in facial expressions (Gray & Tickle-Degnen, 2010) and theory of mind, defined as the ability to understand and predict another’s beliefs or behavior, showed impairment in PD patients (Bodden et al., 2010).
Due to the importance and to the high prevalence of cognitive deficits in PD, an MCI classification has been proposed by the Movement Disorders Society, with specific guidelines for MCI diagnosis in PD (PD-MCI) (Litvan et al., 2012). The diagnosis of PD-MCI has been described as a stage between normal cognition and dementia, characterized by the presence of cognitive deficits not normal for a given age (Goldman & Litvan, 2011). The classification for PD-MCI could be performed with two types of cognitive assessments. The first type of assessment, also called by the authors “level I,” is based on an abbreviated assessment or a global cognitive scale such as the Montreal Cognitive Assessment (MoCA) . The “level II” type of assessment represents a comprehensive assessment and should include two tests per cognitive domain and evaluate five cognitive domains: attention and working memory, executive functions, language, memory, and visuospatial ability. The PD-MCI classification differentiates between single-domain MCI, which is diagnosed when only one cognitive domain is impaired, and multiple-domain MCI, when two or more cognitive domains are impaired. This subtype classification could help clinicians to adjust and adequate treatments for PD patients (Geurtsen et al., 2014; Litvan et al., 2012).
The presence of cognitive impairment in PD patients has been associated with an increased age at disease onset, longer disease duration, and severity of motor symptoms (Aarsland et al., 2010). Moreover, cognitive impairment has been shown to be related to reduced quality of life and functional disability in PD (Leroi et al., 2012; Rosenthal et al., 2010). Additionally, a relationship has been suggested between clinical symptoms and cognitive deficits in PD patients. For example, the presence of cognitive deficits in the disease has been associated with depressive symptoms (Gustafsson, Nordstrom, & Nordstrom, 2015). In addition, apathetic symptomatology is a common symptom in PD (Pagonabarraga et al., 2015) that has been linked to the development of cognitive deficits and the evolution to dementia in PD (Dujardin, Sockeel, Delliaux, Destée, & Defebvre, 2009).
Cerebral Correlates of Cognitive Impairment
Magnetic resonance imaging (MRI) studies have demonstrated structural (Duncan et al., 2016; Ibarretxe-Bilbao, Junque, Marti, & Tolosa, 2011) and functional (Cabeza & Nyberg, 2000; Christopher & Strafella, 2013) cerebral correlates of the impairment of different cognitive domains in PD.
Cognitive impairment in PD has been related to gray matter atrophy (Duncan et al., 2016; Melzer et al., 2012) especially in the frontal, temporal, and parietal cortex but also in the hippocampus, amygdala, and putamen (Duncan et al., 2016; Melzer et al., 2012). Specifically, executive dysfunction has been mostly associated with cortical deterioration in patients with PD (Hanna-Pladdy, 2007). Executive function has been correlated with frontal deterioration (Duncan et al., 2016), differentiating between the anterior cingulate cortex, which controls the initiative and inhibition; the orbitofrontal cortex, which has been related to decision-making; and the dorsolateral prefrontal cortex, which has been associated with problem-solving (Hanna-Pladdy, 2007). The brain correlates of decision-making measured with the IGT have also been analyzed, and results have shown a strong correlation with the lateral orbitofrontal cortex in PD (Kobayakawa, Tsuruya, & Kawamura, 2017). In addition, memory impairment in PD patients has been associated with a deterioration of the hippocampus (Bouchard et al., 2008; Bruck, Kurki, Kaasinen, Vahlberg, & Rinne, 2004; Carlesimo et al., 2012; Ibarretxe-Bilbao et al., 2008) and amygdala (Junqué et al., 2005). Semantic fluency has been related to frontal, temporal, and cerebellar brain areas in PD (Pereira et al., 2009). Visuospatial ability has been correlated mostly with the parietal and occipital lobes in patients with PD, and visuoperceptive ability has shown correlates with occipital, frontal, and subcortical areas in PD patients (Pereira et al., 2009). Furthermore, impaired facial emotion recognition in PD patients has been related to bilateral orbitofrontal cortex (Ibarretxe-Bilbao et al., 2009), and theory of mind deficit in PD has been associated with frontal and parietal lobes (Díez-Cirarda et al., 2015).
In addition, PD patients with cognitive impairment have shown widespread cerebral white matter deterioration (Duncan et al., 2016; Zheng et al., 2013; Matsui et al., 2007a, 2007b). Executive dysfunction in PD have been related to atrophy in the anterior white matter tracts (Melzer et al., 2013), as well as in tracts located in the parietal lobe (Matsui et al., 2007a). Memory impairment in PD patients has been related to anterior white matter deterioration (Melzer et al., 2013). Attention and working memory deficits have been associated with the anterior and posterior tracts (Melzer et al., 2013). Theory of mind deficit in PD has been related to frontal and parietal white matter deterioration (Díez-Cirarda et al., 2015).
Finally, functional MRI (fMRI) has also demonstrated that cognitive impairment in PD is related to functional brain deterioration, during resting state and during cognitive tasks inside the scanner (Christopher & Strafella, 2013; Olde Dubbelink et al., 2014). During resting state, PD patients with MCI usually showed reduced functional connectivity compared with PD patients without MCI and healthy subjects. Most of the connectivity alterations were found within the default-mode network (DMN) (Gorges et al., 2015), within the frontoparietal network (FPN) (Amboni et al., 2015), and within the dorsal attention network (DAN), but inter-network alterations were also identified between DMN-DAN and DAN-FPN (Baggio et al., 2015). Moreover, PD patients showed brain activation dysfunctions during cognitive fMRI tasks inside the scanner. For example, during a Wisconsin card sorting task that measures planning, execution, and cognitive flexibility, PD patients showed less deactivation in different areas of the DMN, and even reversed patterns of activation and deactivation compared to healthy controls (van Eimeren, Monchi, Ballanger, & Strafella, 2009). PD patients also showed decreased brain activation in frontal and occipital areas and decreased deactivation in the DMN during a recognition memory fMRI task (Ibarretxe-Bilbao et al., 2011). In addition, during a set-shifting task, PD patients showed decreased cortical activation in the caudate nucleus and increased activation in the dorsolateral prefrontal cortex (Monchi et al., 2004). During a working memory paradigm, PD patients with cognitive impairment showed reduced activation in the striatal and frontal lobes (Lewis, Dove, Robbins, Barker, & Owen, 2003). In 2012, the same results were found using the verbal two-back working memory task, and additionally, PD patients with MCI showed reduced activation in the right dorsal caudate nucleus, and the bilateral anterior cingulate cortex compared with PD patients without MCI (Ekman et al., 2012).
Progression of Cognitive Impairment
The cognitive deficits present in patients with PD deteriorate with the progression of the disease, until dementia occurs after 10–20 years (Hely et al., 2008; Williams-Gray et al., 2013). One study followed newly diagnosed PD patients over time and found that after 20 years, dementia was present in 83% of patients (Hely et al., 2008). The incidence of dementia in PD has been found to be six times higher than the incidence in healthy people (Emre, 2003). With the progression of the disease, cognitive deterioration is accompanied by grey matter deterioration (Ramírez-Ruiz et al., 2005), white matter degeneration (Zhang, Wu, Tosun, Foster, & Schuff, 2016), and functional brain alterations (Huang et al., 2007; Segura et al., 2013). When dementia occurs in PD patients, cortical degeneration has been extended to frontal, temporal, parietal, and occipital areas (Mak et al., 2015).
There are some factors that can influence cognitive performance and its progression. Among those factors, cognitive reserve has been largely studied. Cognitive reserve could be defined as “the amount of damage that can be sustained before reaching a threshold for clinical expression” and is determined by life-time educational experiences that protect against dementia (Stern, 2002). Cognitive reserve in PD has been related to premorbid intelligence and the amount of years of education (Armstrong et al., 2012). The neuroprotective effects of cognitive reserve have been suggested in PD; however, this relationship needs to be analyzed deeply (Hindle, Martyr, & Clare, 2014).
Cognitive Rehabilitation in PD
Due to the importance of cognitive deterioration in the progression of PD, intervention strategies are needed to treat cognitive decline. Among treatments against cognitive impairment, cognitive rehabilitation has proven to be the most effective in improving cognition (Petersen et al., 2014). Cognitive rehabilitation can be defined as a behavioral treatment for cognitive impairment based on the restoration, compensation, and optimization of the cognitive functions that targets cognitive skills, but also daily functioning (Bahar-Fuchs, Clare, & Woods, 2013; Wykes & Spaulding, 2011). This section will focus on the efficacy of cognitive rehabilitation programs in producing cognitive, functional, and cerebral changes in patients with PD. Finally, the longitudinal maintenance of these changes over time in PD will be analyzed.
Cognitive and Functional Changes After Cognitive Rehabilitation
The efficacy of cognitive rehabilitation programs on improving cognition has been demonstrated in PD through several randomized controlled studies (Cerasa et al., 2014; Edwards et al., 2013; París et al., 2011; Pena et al., 2014; Petrelli et al., 2014; Sammer, Reuter, Hullmann, Kaps, & Vaitl, 2006; Zimmermann et al., 2014). Table 7.2 shows a summary of cognitive rehabilitation studies in PD that meet the following criteria: (1) They were randomized controlled trials; (2) the experimental group attended a cognitive rehabilitation program; and (3) the experimental group attended only the cognitive rehabilitation program and not a combination of therapies (e.g., cognitive training + motor training).
Among these studies, there is considerable variability across cognitive rehabilitation protocol characteristics, including (1) the number of cognitive domains trained; (2) the duration of the rehabilitation (from 4 to 13 weeks); (3) the frequency of the sessions (1–3 sessions per week); (4) the duration of the sessions (30–90 min per session); (5) the format (group-based or individual); and (6) the modality (paper/pencil or computer-based exercises) (Hindle, Petrelli, Clare, & Kalbe, 2013; Leung, 2015). Despite these differences, all studies demonstrated that the overall cognition in PD patients was increased after attending the cognitive rehabilitation program compared to the control group (Leung, 2015). According to the meta-analysis by Leung et al. (Leung, 2015), the cognitive domains that have shown greater improvements after cognitive training are executive functions, working memory, processing speed, and memory. Nevertheless, attention and visuospatial abilities have also shown significant improvements in PD (Leung, 2015). In addition, verbal fluency (París et al., 2011) and theory of mind (Pena et al., 2014) have also shown improvement after rehabilitation.
Traditionally, the main target of cognitive treatments has usually been cognitive improvement; however, a promising finding in PD is that cognitive rehabilitation programs not only improve cognitive functions but also could have an impact on functional outcome (Walton, Naismith, Lampit, Mowszowski, & Lewis, 2017). That is, benefits from cognitive treatments can be transferred to other variables that have not been trained directly during the cognitive program. Depressive symptomatology is one of the clinical symptoms that has been usually evaluated in the studies on the efficacy of cognitive programs in PD. The overall results point to a reduction of the symptoms of depression after treatment, as reported in a meta-analysis (Leung, 2015). These results should be taken with caution, because the PD patients had not been diagnosed with depression in any of the studies, and a ceiling effect could be present in the data. Moreover, among the five randomized controlled trials that evaluated the change in depressive symptomatology after rehabilitation, only two studies found significant differences (Pena et al., 2014; Petrelli et al., 2015), while the rest of the studies did not find any significant changes (Cerasa et al., 2014; Edwards et al., 2013; París et al., 2011).
PD patients usually present with functional disability, which is usually related to cognitive decline (Leroi et al., 2012; Rosenthal et al., 2010). Functional disability is defined by the World Health Organization (WHO) as a limitation that lasts in time and causes a disability in activity, always produced by a disease. Interestingly, a cognitive rehabilitation study demonstrated that functional disability measured with the short version of the World Health Organization Disability Assessment Schedule II (WHO-DAS II) could be reduced after training in PD patients (Pena et al., 2014). In contrast, another randomized controlled trial included the Parkinson’s Disease Questionnaire (PDQ-39) to assess the change in the quality of life of the PD patients who attended the cognitive rehabilitation program, but no significant changes were found (París et al., 2011). These authors attributed the absence of change in PDQ-39 to the short duration of the treatment (1 month) (París et al., 2011), and in fact, the study that identified significant changes in functional disability applied a longer cognitive rehabilitation program that lasted 3 months (Pena et al., 2014). Therefore, the duration of treatment could be relevant in terms of its impact on PD patients’ quality of life.
Moreover, studies in PD have also combined cognitive rehabilitation with other trainings such as physical exercise or motor training and also found positive results (Hindle et al., 2013). Specifically, one study investigated the efficacy of the combination of therapies: (1) cognitive training with individual sessions focused on different cognitive functions; (2) transfer training focused on daily routines; and (3) motor training (Reuter, Mehnert, Sammer, Oechsner, & Engelhardt, 2012). PD patients who attended cognitive training combined with transfer and motor training showed higher significant improvements, including quality-of-life improvements (measured with the PDQ-39) than those PD patients who only attended cognitive training or cognitive training combined with transfer training (Reuter et al., 2012). Further research needs to be done towards the understanding of the cognitive improvements and the transfer effects to clinical aspects after cognitive treatment in PD.
Furthermore, detecting variables that predict the efficacy of cognitive treatments is an important objective in order to understand the cognitive rehabilitation process and could guide researchers to develop more effective programs and clinicians to personalize treatments for patients. Only two studies have investigated the predictor outcomes of the efficacy of cognitive treatments in PD (Edwards, Delahunt, & Mahncke, 2009; Zimmermann et al., 2014). These PD studies found that lower age at diagnosis and longer disease duration were predictors of a higher degree of cognitive improvements after rehabilitation (Edwards et al., 2009). However, higher scores in working memory and flexibility at baseline were related to a lower degree of improvements after training (Zimmermann et al., 2014).
Additionally, the treatment of cognitive symptoms and functional aspects of PD patients can also be completed in parallel with the training of their caregivers (París et al., 2011; Reuter et al., 2012). Most of the people who take care of PD patients are informal caregivers, usually family members. The primary care provider plays a relevant role in the quality of life of the PD patient, and vice versa. Indeed, the symptoms of PD patients can influence the caregiver, and there is a risk of developing caregiver burden (Leroi et al., 2012; Martínez-Martín et al., 2007). Some studies in PD have focused on the treatment of caregivers (A’Campo, Wekking, Spliethoff-Kamminga, Le Cessie, & Roos, 2010; Secker & Brown, 2005), and the treatment of caregivers has also been included in cognitive rehabilitation trials for the benefit of both PD patients and caregivers (Reuter et al., 2012). The intervention with the primary care provider usually includes modules focused on providing information about the disease and care management, giving support on cognitive rehabilitation of the PD patient and also dealing with individual problems related to the role of a caregiver and the psychological aspects involved (A’campo, Spliethoff-Kamminga, et al., 2010; Reuter et al., 2012). Following a combined caregiver educational program and a cognitive rehabilitation program for PD patients, results showed that caregivers felt more calm, self-assured, and capable of managing daily situations and helping PD patients with cognitive tasks. PD patients were also more relaxed and trustful with their caregivers (Reuter et al., 2012). These findings highlight the importance of including caregiver training in future cognitive rehabilitation studies in PD.
Cerebral Changes After Cognitive Rehabilitation
Little is known about the neurobiological effects of cognitive rehabilitation programs on PD. To date, the literature is scarce about the presence of cerebral changes associated with cognitive treatments assessed with structural and functional MRI techniques in PD. Only three studies have found functional cerebral changes in PD patients after attending cognitive training (Cerasa et al., 2014; Díez-Cirarda et al., 2017; Nombela et al., 2011) (see Table 7.3).
The first study in PD that assessed brain changes after training did not apply a traditional cognitive rehabilitation program, but PD patients trained individually with Sudoku exercises at home for 6 months (Nombela et al., 2011). After the intervention, PD patients showed increased performance in the Stroop test that was accompanied by reduced brain activation during a modified Stroop task inside the scanner. This reduced activation was similar to the brain activation pattern of healthy subjects. Hence, the authors concluded that an over-activation was present in PD patients at baseline, which was reduced after Sudoku training (Nombela et al., 2011).
A second study assessed functional brain changes during a resting-state fMRI acquisition after an attention rehabilitation program in PD patients (Cerasa et al., 2014). The attention rehabilitation was group-based and consisted of computer-assisted tasks that trained attention and information processing during 6 weeks. The control group attended a placebo intervention. This study found improvements in attention and processing speed tasks and increased brain activation in the left dorsolateral prefrontal cortex and the superior parietal cortex in PD patients who attended attention rehabilitation compared to the active control group (Cerasa et al., 2014). Both the brain areas have been associated with attention, executive functioning, and working memory (Duncan et al., 2016; Hanna-Pladdy, 2007).
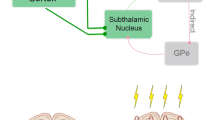
Recently, another study in PD assessed the functional and structural brain changes after cognitive rehabilitation using the REHACOP program (Díez-Cirarda et al., 2017). Functional brain changes were analyzed during resting-state and during a memory fMRI paradigm. The memory fMRI paradigm comprised a learning task (a list of words) and a subsequent recognition task (which involved discriminating previous words from a longer list of words). The REHACOP is a 3-month integrative cognitive intervention with paper/pencil exercises that trains different cognitive functions: attention, memory, language, executive functions, and social cognition. The control group attended occupational therapy. After treatment, PD patients attending cognitive rehabilitation compared to the active control group had improved processing speed, memory, and theory of mind (Pena et al., 2014) and showed increased brain connectivity during resting-state fMRI between frontal and temporal regions (see Fig. 7.1) and increased brain activation during a memory paradigm in frontal and temporal lobes (Díez-Cirarda et al., 2017).
In summary, these three studies showed that PD patients can present functional brain changes related to cognitive improvements after cognitive rehabilitation. These studies suggest that the brain changes in PD could be detected during both resting state and during a cognitive paradigm and have been mostly located in the prefrontal cortex and inter-network changes between the dorsolateral prefrontal cortex and other brain regions.
Furthermore, the ultimate goal of cognitive treatments is to ensure that benefits are maintained over long periods of time, but little is known about the maintenance of cognitive improvements over time in PD patients (Walton et al., 2017). One study in PD showed the persistence of some cognitive improvements over 6 months after cognitive training (Sinforiani, Banchieri, Zucchella, Pacchetti, & Sandrini, 2004). On the contrary, another study in PD found that only cognitive training combined with transfer training and physical activity maintained cognitive improvements after 6 months follow-up (Reuter et al., 2012). A later study in PD assessed the long-term effects of cognitive rehabilitation for a longer period of time and found that cognitive improvements persisted after 12 months, concluding that cognitive treatment could prevent cognitive decline (Petrelli et al., 2015). Finally, a posterior study found that both cognitive and functional brain changes could be maintained after 18 months from posttreatment (Díez-Cirarda et al., 2018).
The studies discussed above demonstrate that patients with PD can improve with regard to cognitive functions, reduce clinical symptomatology, and present functional cerebral changes after attending a cognitive rehabilitation program. Additionally, these neuropsychological changes can be maintained over time. More research needs to be done to replicate and support these findings. These studies found the existence of brain plasticity in patients with this pathology, despite the neurodegenerative process, and support the efficacy of cognitive rehabilitation treatments in PD patients. These findings show that cognitive rehabilitation programs have an impact on PD patients’ cognition and functionality, which can be reflected in changes in functional imaging.
Future Directions
Great steps have been taken towards understanding the efficacy of cognitive rehabilitation programs in PD; however, further research is needed in this field. Future directions should focus on two main aspects, among others. First, the methodology used to assess the efficacy of cognitive rehabilitation programs should be unified, and second, more research needs to be done into developing the most effective cognitive rehabilitation programs for PD patients.
The Consolidated Standards of Reporting Trials (CONSORT) guidelines for randomized controlled trials should be followed and implemented in all the studies related to the efficacy of cognitive rehabilitation programs. The CONSORT Statement (http://www.consort-statement.org/) is focused on the improvement of health research reports and, consequently, on the improvement of research quality.
One of the main points that should be addressed in future studies is identifying the characteristics that make an integrative cognitive rehabilitation program the most suitable and the most effective one against cognitive impairment. A review of the field of cognitive rehabilitation programs concluded that better results may be obtained in group-based format compared to individual format (Walton et al., 2017). However, while most of the rehabilitation studies in PD are group-based, this question has not been directly addressed. In addition, a recent meta-analysis compared the efficacy of standardized with tailored (individualized) cognitive interventions, but found that there were insufficient studies for a formal comparison (Lawrence, Gasson, Bucks, Troeung, & Loftu, 2017). Furthermore, other variables are also to be defined, such as the most appropriate number of sessions, their frequency, and the duration of the treatment. Finally, the number of cognitive domains trained may also influence the results.
Very little is known about the longitudinal maintenance of cognitive changes after rehabilitation. Future studies should include follow-up periods in order to replicate previous findings and assess whether the improvements after training could be maintained over time. Furthermore, it would be interesting to examine the maintenance of these changes in PD patients with and without booster sessions.
Cognitive rehabilitation studies in PD usually include extensive neuropsychological evaluations. Transfer effects to clinical characteristics have been found in cognitive rehabilitation studies in PD, and therefore, future studies should also include clinical and functionality scales in pre- and posttreatment neuropsychological assessments. Additionally, promising findings have been noted regarding brain changes after treatment in PD, which support the efficacy of cognitive rehabilitation programs in the disease. However, to date, few studies have been published with brain changes assessment after cognitive interventions. In order to replicate previous studies, future studies should include the fMRI acquisition, as part of the protocol assessment to evaluate brain changes after treatment. Moreover, very few studies have been found that examined the predictors of change after treatment in PD, and this should be addressed in future trials. Predictors of efficacy could help to understand the cognitive rehabilitation process and could guide researchers to develop more effective programs and for clinicians to personalize treatments for patients. In fact, one possible hypothesis is that the existence of brain changes could be a predictor of the efficacy of cognitive rehabilitation programs and an indicator of the probable maintenance of the cognitive improvements over time.
Several randomized controlled trials have been published in the field of cognitive rehabilitation programs in PD patients; however, all of them highlighted the small sample size as a limitation, which makes it difficult to generalize the findings. It would be interesting to perform an international multicenter clinical trial with a large sample size to evaluate the efficacy of cognitive training programs in PD.
Finally, most of the randomized controlled trials in PD have been performed with PD patients at the early Hoehn and Yahr stages of the disease. Future studies should also include PD patients at more advanced stages to evaluate whether cognitive treatments could also benefit these patients. Interestingly, a study protocol was recently published addressing the efficacy of a cognitive rehabilitation in PD patients with dementia, but the results are pending (Hindle et al., 2016).
In conclusion, studies have demonstrated cognitive rehabilitation programs to be effective on improving cognitive functions and may also improve functional disability and produce brain changes in patients with PD. Further research should be performed in the field, to the goal of reaching generalized conclusions and including cognitive rehabilitation in the standard of care of PD patients.
References
A’campo, L., Spliethoff-Kamminga, N., Macht, M., Roos, R., & EduPark Consortium. (2010). Caregiver education in Parkinson’s disease: Formative evaluation of a standardized program in seven European countries. Quality of Life Research, 19(1), 55–64. https://doi.org/10.1007/s11136-009-9559-y
A’Campo, L., Wekking, E., Spliethoff-Kamminga, N., Le Cessie, S., & Roos, R. (2010). The benefits of a standardized patient education program for patients with Parkinson’s disease and their caregivers. Parkinsonism & Related Disorders, 16(2), 89–95. https://doi.org/10.1016/j.parkreldis.2009.07.009
Aarsland, D., Bronnick, K., Larsen, J. P., Tysnes, O. B., Alves, G., & Norwegian ParkWest Study Group. (2009). Cognitive impairment in incident, untreated Parkinson disease: The Norwegian ParkWest study. Neurology, 72(13), 1121–1126. https://doi.org/10.1212/01.wnl.0000338632.00552.cb
Aarsland, D., Bronnick, K., Williams-Gray, C., Weintraub, D., Marder, K., Kulisevsky, J., … Emre, M. (2010). Mild cognitive impairment in Parkinson disease: A multicenter pooled analysis. Neurology, 75(12), 1062–1069. https://doi.org/10.1212/WNL.0b013e3181f39d0e
Aarsland, D., Påhlhagen, S., Ballard, C. G., Ehrt, U., & Svenningsson, P. (2012). Depression in Parkinson disease—Epidemiology, mechanisms and management. Nature Reviews Neurology, 8(1), 35–47. https://doi.org/10.1038/nrneurol.2011.189
Amboni, M., Tessitore, A., Esposito, F., Santangelo, G., Picillo, M., Vitale, C., … Corbo, D. (2015). Resting-state functional connectivity associated with mild cognitive impairment in Parkinson’s disease. Journal of Neurology, 262(2), 425–434. https://doi.org/10.1007/s00415-014-7591-5
Ansari, K., & Johnson, A. (1975). Olfactory function in patients with Parkinson’s disease. Journal of Chronic Diseases, 28(9), 493–497. https://doi.org/10.1016/0021-9681(75)90058-2
Armstrong, M. J., Naglie, G., Duff-Canning, S., Meaney, C., Gill, D., Eslinger, P. J., … Marras, C. (2012). Roles of education and IQ in cognitive reserve in Parkinson’s disease-mild cognitive impairment. Dementia and Geriatric Cognitive Disorders Extra, 2(1), 343–352. https://doi.org/10.1159/000341782
Baggio, H., Segura, B., Sala-Llonch, R., Marti, M., Valldeoriola, F., Compta, Y., … Junque, C. (2015). Cognitive impairment and resting-state network connectivity in Parkinson’s disease. Human Brain Mapping, 36(1), 199–212. https://doi.org/10.1002/hbm.22622
Bahar-Fuchs, A., Clare, L., & Woods, B. (2013). Cognitive training and cognitive rehabilitation for persons with mild to moderate dementia of the Alzheimer’s or vascular type: A review. Alzheimers Research & Therapy, 5(4), 35. https://doi.org/10.1186/alzrt189
Bodden, M. E., Mollenhauer, B., Trenkwalder, C., Cabanel, N., Eggert, K. M., Unger, M. M., … Kalbe, E. (2010). Affective and cognitive theory of mind in patients with Parkinson’s disease. Parkinsonism & Related Disorders, 16(7), 466–470. https://doi.org/10.1016/j.parkreldis.2010.04.014
Bouchard, T. P., Malykhin, N., Martin, W. W., Hanstock, C. C., Emery, D. J., Fisher, N. J., & Camicioli, R. M. (2008). Age and dementia-associated atrophy predominates in the hippocampal head and amygdala in Parkinson’s disease. Neurobiology of Aging, 29(7), 1027–1039. https://doi.org/10.1016/j.neurobiolaging.2007.02.002
Braak, H., Ghebremedhin, E., Rüb, U., Bratzke, H., & Del Tredici, K. (2004). Stages in the development of Parkinson’s disease-related pathology. Cell and Tissue Research, 318(1), 121–134. https://doi.org/10.1007/s00441-004-0956-9
Braak, H., Rüb, U., Gai, W., & Del Tredici, K. (2003). Idiopathic Parkinson’s disease: Possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. Journal of Neural Transmission, 110(5), 517–536. https://doi.org/10.1007/s00702-002-0808-2
Bruck, A., Kurki, T., Kaasinen, V., Vahlberg, T., & Rinne, J. O. (2004). Hippocampal and prefrontal atrophy in patients with early non-demented Parkinson’s disease is related to cognitive impairment. Journal of Neurology, Neurosurgery, and Psychiatry, 75(10), 1467–1469. https://doi.org/10.1136/jnnp.2003.031237
Cabeza, R., & Nyberg, L. (2000). Imaging cognition II: An empirical review of 275 PET and fMRI studies. Journal of Cognitive Neuroscience, 12(1), 1–47. https://doi.org/10.1007/s10072-014-1666-z
Carlesimo, G. A., Piras, F., Assogna, F., Pontieri, F. E., Caltagirone, C., & Spalletta, G. (2012). Hippocampal abnormalities and memory deficits in Parkinson disease: A multimodal imaging study. Neurology, 78(24), 1939–1945. https://doi.org/10.1212/WNL.0b013e318259e1c5
Cerasa, A., Gioia, M. C., Salsone, M., Donzuso, G., Chiriaco, C., Realmuto, S., , . . . D’amelio, M. (2014). Neurofunctional correlates of attention rehabilitation in Parkinson’s disease: An explorative study. Neurological Sciences, 35(8), 1173–1180. https://doi.org/10.1007/s10072-014-1666-z
Chiaravalloti, N., Ibarretxe-Bilbao, N., DeLuca, J., Rusu, O., Pena, J., García-Gorostiaga, I., & Ojeda, N. (2014). The source of the memory impairment in Parkinson’s disease: Acquisition versus retrieval. Movement Disorders, 29(6), 765–771. https://doi.org/10.1002/mds.25842
Christopher, L., & Strafella, A. P. (2013). Neuroimaging of brain changes associated with cognitive impairment in Parkinson’s disease. Journal of Neuropsychology, 7(2), 225–240. https://doi.org/10.1111/jnp.12015
Connolly, B. S., & Lang, A. E. (2014). Pharmacological treatment of Parkinson disease: A review. JAMA, 311(16), 1670–1683. https://doi.org/10.1001/jama.2014.3654
Del Tredici, K., Rub, U., De Vos, R. A., Bohl, J. R., & Braak, H. (2002). Where does Parkinson disease pathology begin in the brain? Journal of Neuropathology and Experimental Neurology, 61(5), 413–426. https://doi.org/10.1093/jnen/61.5.413
Díez-Cirarda, M., Ojeda, N., Peña, J., Cabrera-Zubizarreta, A., Gómez-Beldarrain, M. Á., Gómez-Esteban, J. C., & Ibarretxe-Bilbao, N. (2015). Neuroanatomical correlates of theory of mind deficit in Parkinson’s disease: A multimodal imaging study. PLoS One, 10(11), e0142234. https://doi.org/10.1371/journal.pone.0142234
Díez-Cirarda, M., Ojeda, N., Peña, J., Cabrera-Zubizarreta, A., Lucas-Jiménez, O., Gómez-Esteban, J. C., … Ibarretxe-Bilbao, N. (2017). Increased brain connectivity and activation after cognitive rehabilitation in Parkinson’s disease: A randomized controlled trial. Brain Imaging and Behavior, 11(6), 1640–1651. https://doi.org/10.1007/s11682-016-9639-x
Díez-Cirarda, M., Ojeda, N., Peña, J., Cabrera-Zubizarreta, A., Lucas-Jiménez, O., Gómez-Esteban, J. C., … Ibarretxe-Bilbao, N. (2018). Long-term effects of cognitive rehabilitation on brain, functional outcome and cognition in Parkinson’s disease. European Journal of Neurology, 25(1), 5–12. https://doi.org/10.1111/ene.13472
Doty, R. L., Deems, D. A., & Stellar, S. (1988). Olfactory dysfunction in Parkinsonism: A general deficit unrelated to neurologic signs, disease stage, or disease duration. Neurology, 38(8), 1237–1244. https://doi.org/10.1212/wnl.38.8.1237
Dujardin, K., Sockeel, P., Delliaux, M., Destée, A., & Defebvre, L. (2009). Apathy may herald cognitive decline and dementia in Parkinson’s disease. Movement Disorders, 24(16), 2391–2397. https://doi.org/10.1002/mds.22843
Duncan, G. W., Firbank, M. J., Yarnall, A. J., Khoo, T. K., Brooks, D. J., Barker, R. A., … O’Brien, J. T. (2016). Gray and white matter imaging: A biomarker for cognitive impairment in early Parkinson’s disease? Movement Disorders, 31(1), 103–110. https://doi.org/10.1002/mds.26312
Edwards, J. D., Delahunt, P. B., & Mahncke, H. W. (2009). Cognitive speed of processing training delays driving cessation. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64(12), 1262–1267. https://doi.org/10.1093/gerona/glp131
Edwards, J. D., Hauser, R. A., O’Connor, M. L., Valdes, E. G., Zesiewicz, T. A., & Uc, E. Y. (2013). Randomized trial of cognitive speed of processing training in Parkinson disease. Neurology, 81(15), 1284–1290. https://doi.org/10.1212/WNL.0b013e3182a823ba
Ekman, U., Eriksson, J., Forsgren, L., Mo, S. J., Riklund, K., & Nyberg, L. (2012). Functional brain activity and presynaptic dopamine uptake in patients with Parkinson’s disease and mild cognitive impairment: A cross-sectional study. The Lancet Neurology, 11(8), 679–687. https://doi.org/10.1016/S1474-4422(12)70138-2
Emre, M. (2003). Dementia associated with Parkinson’s disease. The Lancet Neurology, 2(4), 229–237. https://doi.org/10.1016/S1474-4422(03)00351-X
Fenelon, G., Mahieux, F., Huon, R., & Ziegler, M. (2000). Hallucinations in Parkinson’s disease: Prevalence, phenomenology and risk factors. Brain: A Journal of Neurology, 123(4), 733–745. https://doi.org/10.1093/brain/123.4.733
Foltynie, T., Brayne, C. E., Robbins, T. W., & Barker, R. A. (2004). The cognitive ability of an incident cohort of Parkinson’s patients in the UK. The CamPaIGN study. Brain : A Journal of Neurology, 127(3), 550–560. https://doi.org/10.1093/brain/awh067
Geurtsen, G. J., Hoogland, J., Goldman, J. G., Schmand, B. A., Tröster, A. I., Burn, D. J., & Litvan, I. (2014). Parkinson’s disease mild cognitive impairment: Application and validation of the criteria. Journal of Parkinson’s Disease, 4(2), 131–137. https://doi.org/10.3233/JPD-130304
Goetz, C. G., Poewe, W., Rascol, O., Sampaio, C., Stebbins, G. T., Counsell, C., … Wenning, G. K. (2004). Movement disorder society task force report on the Hoehn and Yahr staging scale: Status and recommendations the movement disorder society task force on rating scales for Parkinson’s disease. Movement Disorders, 19(9), 1020–1028. https://doi.org/10.1002/mds.20213
Goldman, J. G., & Litvan, I. (2011). Mild cognitive impairment in Parkinson’s disease. Minerva Medica, 102(6), 441–459.
Goldstein, D. S. (2003). Dysautonomia in Parkinson’s disease: Neurocardiological abnormalities. The Lancet Neurology, 2(11), 669–676. https://doi.org/10.1002/cphy.c130026
Gorges, M., Müller, H., Lulé, D., Pinkhardt, E. H., Ludolph, A. C., Kassubek, J., & LANDSCAPE Consortium. (2015). To rise and to fall: Functional connectivity in cognitively normal and cognitively impaired patients with Parkinson’s disease. Neurobiology of Aging, 36(4), 1727–1735. https://doi.org/10.1016/j.neurobiolaging.2014.12.026
Gray, H. M., & Tickle-Degnen, L. (2010). A meta-analysis of performance on emotion recognition tasks in Parkinson’s disease. Neurophysiology, 24(2), 176–191. https://doi.org/10.1037/a0018104
Gustafsson, H., Nordstrom, A., & Nordstrom, P. (2015). Depression and subsequent risk of Parkinson disease: A nationwide cohort study. Neurology, 84(24), 2422–2429. https://doi.org/10.1212/WNL.0000000000001684
Haehner, A., Boesveldt, S., Berendse, H., Mackay-Sim, A., Fleischmann, J., Silburn, P. A., … Reichmann, H. (2009). Prevalence of smell loss in Parkinson’s disease–a multicenter study. Parkinsonism & Related Disorders, 15(7), 490–494. https://doi.org/10.1016/j.parkreldis.2008.12.005
Hanna-Pladdy, B. (2007). Dysexecutive syndromes in neurologic disease. Journal of Neurologic Physical Therapy: JNPT, 31(3), 119–127. https://doi.org/10.1097/NPT.0b013e31814a63c2
Hely, M. A., Reid, W. G., Adena, M. A., Halliday, G. M., & Morris, J. G. (2008). The Sydney multicenter study of Parkinson’s disease: The inevitability of dementia at 20 years. Movement Disorders, 23(6), 837–844. https://doi.org/10.1002/mds.21956
Hindle, J. V., Martyr, A., & Clare, L. (2014). Cognitive reserve in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism & Related Disorders, 20(1), 1–7. https://doi.org/10.1016/j.parkreldis.2013.08.010
Hindle, J. V., Petrelli, A., Clare, L., & Kalbe, E. (2013). Nonpharmacological enhancement of cognitive function in Parkinson’s disease: A systematic review. Movement Disorders, 28(8), 1034–1049. https://doi.org/10.1002/mds.25377
Hindle, J. V., Watermeyer, T. J., Roberts, J., Martyr, A., Lloyd-Williams, H., Brand, A., … Clare, L. (2016). Cognitive rehabiliation for Parkinson’s disease dementia: A study protocol for a pilot randomised controlled trial. Trials, 17(1), 152. https://doi.org/10.1186/s13063-016-1253-0
Hirsch, L., Jette, N., Frolkis, A., Steeves, T., & Pringsheim, T. (2016). The incidence of Parkinson’s disease: A systematic review and meta-analysis. Neuroepidemiology, 46(4), 292–300. https://doi.org/10.1159/000445751
Hoehn, M. M., & Yahr, M. D. (1967). Parkinsonism: Onset, progression and mortality. Neurology, 17(5), 427–442.
Hu, Y., Yu, S. Y., Zuo, L. J., Cao, C. J., Wang, F., Chen, Z. J., … Zhang, W. (2015). Parkinson disease with REM sleep behavior disorder: Features, alpha-synuclein, and inflammation. Neurology, 84(9), 888–894. https://doi.org/10.1212/WNL.0000000000001308
Huang, C., Tang, C., Feigin, A., Lesser, M., Ma, Y., Pourfar, M., … Eidelberg, D. (2007). Changes in network activity with the progression of Parkinson’s disease. Brain, 130(7), 1834–1846. https://doi.org/10.1093/brain/awm086
Ibarretxe-Bilbao, N., Junque, C., Marti, M. J., & Tolosa, E. (2011). Brain structural MRI correlates of cognitive dysfunctions in Parkinson’s disease. Journal of the Neurological Sciences, 310(1), 70–74. https://doi.org/10.1016/j.jns.2011.07.054
Ibarretxe-Bilbao, N., Junque, C., Tolosa, E., Marti, M., Valldeoriola, F., Bargallo, N., & Zarei, M. (2009). Neuroanatomical correlates of impaired decision-making and facial emotion recognition in early Parkinson’s disease. European Journal of Neuroscience, 30(6), 1162–1171. https://doi.org/10.1111/j.1460-9568.2009.06892.x
Ibarretxe-Bilbao, N., Ramirez-Ruiz, B., Junque, C., Marti, M. J., Valldeoriola, F., Bargallo, N., … Tolosa, E. (2010). Differential progression of brain atrophy in Parkinson’s disease with and without visual hallucinations. Journal of Neurology, Neurosurgery, and Psychiatry, 81(6), 650–657. https://doi.org/10.1136/jnnp.2009.179655
Ibarretxe-Bilbao, N., Ramirez-Ruiz, B., Tolosa, E., Martí, M. J., Valldeoriola, F., Bargallo, N., & Junque, C. (2008). Hippocampal head atrophy predominance in Parkinson’s disease with hallucinations and with dementia. Journal of Neurology, 255(9), 1324–1331. https://doi.org/10.1007/s00415-008-0885-8
Ibarretxe-Bilbao, N., Zarei, M., Junque, C., Marti, M. J., Segura, B., Vendrell, P., … Tolosa, E. (2011). Dysfunctions of cerebral networks precede recognition memory deficits in early Parkinson’s disease. NeuroImage, 57(2), 589–597. https://doi.org/10.1016/j.neuroimage.2011.04.049
Junqué, C., Ramírez-Ruiz, B., Tolosa, E., Summerfield, C., Martí, M., Pastor, P., … Mercader, J. M. (2005). Amygdalar and hippocampal MRI volumetric reductions in Parkinson’s disease with dementia. Movement Disorders, 20(5), 540–544. https://doi.org/10.1002/mds.20371
Kalia, L. V., & Lang, A. E. (2015). Parkinson’s disease. The Lancet, 386(9996), 896–912. https://doi.org/10.1016/S0140-6736(14)61393-3
Klein, C., & Westenberger, A. (2012). Genetics of Parkinson’s disease. Cold Spring Harbor Perspectives in Medicine, 2(1), a008888. https://doi.org/10.1101/cshperspect.a008888
Kobayakawa, M., Tsuruya, N., & Kawamura, M. (2017). Decision-making performance in Parkinson’s disease correlates with lateral orbitofrontal volume. Journal of the Neurological Sciences, 372, 232–238. https://doi.org/10.1016/j.jns.2016.11.046
Lawrence, B., Gasson, N., Bucks, R. S., Troeung, L., & Loftu, A. M. (2017). Cognitive training and noninvasive brain stimulation for cognition in Parkinson’s disease: A meta-analysis. Neurorehabilitation and Neural Repair, 31(7), 597–608. https://doi.org/10.1177/1545968317712468
Lee, P. C., Bordelon, Y., Bronstein, J., & Ritz, B. (2012). Traumatic brain injury, paraquat exposure, and their relationship to parkinson disease. Neurology, 79(20), 2061–2066. https://doi.org/10.1212/WNL.0b013e3182749f28
Leroi, I., McDonald, K., Pantula, H., & Harbishettar, V. (2012). Cognitive impairment in Parkinson disease: Impact on quality of life, disability, and caregiver burden. Journal of Geriatric Psychiatry and Neurology, 25(4), 208–214. https://doi.org/10.1177/0891988712464823
Leung, I. H. (2015). Cognitive training in Parkinson disease. Neurology, 85, 1–9. https://doi.org/10.1212/WNL.0000000000002145
Lewis, S. J., Dove, A., Robbins, T. W., Barker, R. A., & Owen, A. M. (2003). Cognitive impairments in early Parkinson’s disease are accompanied by reductions in activity in frontostriatal neural circuitry. The Journal of Neuroscience : The Official Journal of the Society for Neuroscience, 23(15), 6351–6356.
Litvan, I., Goldman, J. G., Tröster, A. I., Schmand, B. A., Weintraub, D., Petersen, R. C., … Williams-Gray, C. H. (2012). Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement disorder society task force guidelines. Movement Disorders, 27(3), 349–356. https://doi.org/10.1002/mds.24893
Litvan, I., Mohr, E., Williams, J., Gomez, C., & Chase, T. N. (1991). Differential memory and executive functions in demented patients with Parkinson’s and Alzheimer’s disease. Journal of Neurology, Neurosurgery, and Psychiatry, 54(1), 25–29. https://doi.org/10.1136/jnnp.54.1.25
Mak, E., Su, L., Williams, G. B., & O’Brien, J. T. (2015). Neuroimaging correlates of cognitive impairment and dementia in Parkinson’s disease. Parkinsonism & Related Disorders, 21(8), 862–870. https://doi.org/10.1016/j.parkreldis.2015.05.013
Martínez-Martín, P., Forjaz, M. J., Frades-Payo, B., Rusiñol, A. B., Fernández-García, J. M., Benito-León, J., … Catalán, M. J. (2007). Caregiver burden in Parkinson’s disease. Movement Disorders, 22(7), 924–931. https://doi.org/10.1002/mds.21355
Martinez-Martin, P., Gil-Nagel, A., Gracia, L. M., Gómez, J. B., Martínez-Sarriés, J., & Bermejo, F. (1994). Unified Parkinson’s disease rating scale characteristics and structure. Movement Disorders, 9(1), 76–83. https://doi.org/10.1002/mds.870090112
Matsui, H., Nishinaka, K., Oda, M., Niikawa, H., Komatsu, K., Kubori, T., & Udaka, F. (2007a). Wisconsin card sorting test in Parkinson’s disease: Diffusion tensor imaging. Acta Neurologica Scandinavica, 116(2), 108–112.
Matsui, H., Nishinaka, K., Oda, M., Niikawa, H., Kubori, T., & Udaka, F. (2007b). Dementia in Parkinson’s disease: Diffusion tensor imaging. Acta Neurologica Scandinavica, 116(3), 177–181. https://doi.org/10.1111/j.1600-0404.2007.00838.x
Melzer, T. R., Watts, R., MacAskill, M. R., Pitcher, T. L., Livingston, L., Keenan, R. J., … Anderson, T. J. (2012). Grey matter atrophy in cognitively impaired Parkinson’s disease. Journal of Neurology, Neurosurgery, and Psychiatry, 83(2), 188–194. https://doi.org/10.1136/jnnp-2011-300828
Melzer, T. R., Watts, R., MacAskill, M. R., Pitcher, T. L., Livingston, L., Keenan, R. J., … Anderson, T. J. (2013). White matter microstructure deteriorates across cognitive stages in Parkinson disease. Neurology, 80(20), 1841–1849. https://doi.org/10.1212/WNL.0b013e3182929f62
Monchi, O., Petrides, M., Doyon, J., Postuma, R. B., Worsley, K., & Dagher, A. (2004). Neural bases of set-shifting deficits in Parkinson’s disease. The Journal of Neuroscience, 24(3), 702–710. https://doi.org/10.1523/JNEUROSCI.4860-03.2004
Muslimovic, D., Post, B., Speelman, J. D., & Schmand, B. (2005). Cognitive profile of patients with newly diagnosed parkinson disease. Neurology, 65(8), 1239–1245. https://doi.org/10.1212/01.wnl.0000180516.69442.95
Nombela, C., Bustillo, P. J., Castell, P. F., Sanchez, L., Medina, V., & Herrero, M. T. (2011). Cognitive rehabilitation in Parkinson’s disease: Evidence from neuroimaging. Frontiers in Neurology, 2, 82. https://doi.org/10.3389/fneur.2011.00082
Okun, M. S. (2012). Deep-brain stimulation for Parkinson’s disease. New England Journal of Medicine, 367(16), 1529–1538. https://doi.org/10.1056/NEJMct1208070
Olde Dubbelink, K. T., Schoonheim, M. M., Deijen, J. B., Twisk, J. W., Barkhof, F., & Berendse, H. W. (2014). Functional connectivity and cognitive decline over 3 years in Parkinson disease. Neurology, 83(22), 2046–2053. https://doi.org/10.1212/WNL.0000000000001020
Pagonabarraga, J., Kulisevsky, J., Strafella, A. P., & Krack, P. (2015). Apathy in Parkinson’s disease: Clinical features, neural substrates, diagnosis, and treatment. The Lancet Neurology, 14(5), 518–531. https://doi.org/10.1016/S1474-4422(15)00019-8
París, A. P., Saleta, H. G., de la Cruz Crespo Maraver, M., Silvestre, E., Freixa, M. G., Torrellas, C. P., … Bartolomé, M. V. P. (2011). Blind randomized controlled study of the efficacy of cognitive training in Parkinson’s disease. Movement Disorders, 26(7), 1251–1258. https://doi.org/10.1002/mds.23688
Pena, J., Ibarretxe-Bilbao, N., Garcia-Gorostiaga, I., Gomez-Beldarrain, M. A., Diez-Cirarda, M., & Ojeda, N. (2014). Improving functional disability and cognition in parkinson disease: Randomized controlled trial. Neurology, 83(23), 2167–2174. https://doi.org/10.1212/WNL.0000000000001043
Pereira, J. B., Junqué, C., Martí, M., Ramirez-Ruiz, B., Bargalló, N., & Tolosa, E. (2009). Neuroanatomical substrate of visuospatial and visuoperceptual impairment in Parkinson’s disease. Movement Disorders, 24(8), 1193–1199. https://doi.org/10.1002/mds.22560
Pereira, J. B., Junque, C., Marti, M. J., Ramirez-Ruiz, B., Bartres-Faz, D., & Tolosa, E. (2009). Structural brain correlates of verbal fluency in Parkinson’s disease. Neuroreport, 20(8), 741–744. https://doi.org/10.1097/WNR.0b013e328329370b
Petersen, R., Caracciolo, B., Brayne, C., Gauthier, S., Jelic, V., & Fratiglioni, L. (2014). Mild cognitive impairment: A concept in evolution. Journal of Internal Medicine, 275(3), 214–228. https://doi.org/10.1111/joim.12190
Petrelli, A., Kaesberg, S., Barbe, M., Timmermann, L., Rosen, J., Fink, G., … Kalbe, E. (2015). Cognitive training in Parkinson's disease reduces cognitive decline in the long term. European Journal of Neurology, 22(4), 640–647. https://doi.org/10.1111/ene.12621
Petrelli, A., Kaesberg, S., Barbe, M. T., Timmermann, L., Fink, G. R., Kessler, J., & Kalbe, E. (2014). Effects of cognitive training in Parkinsons disease: A randomized controlled trial. Parkinsonism & Related Disorders, 20(11), 1196–1202. https://doi.org/10.1016/j.parkreldis.2014.08.023
Poletti, M., Cavedini, P., & Bonuccelli, U. (2011). Iowa gambling task in Parkinson’s disease. Journal of Clinical and Experimental Neuropsychology, 33(4), 395–409. https://doi.org/10.1016/j.neuropsychologia.2016.07.032
Pont-Sunyer, C., Hotter, A., Gaig, C., Seppi, K., Compta, Y., Katzenschlager, R., … Bayés, A. (2015). The onset of nonmotor symptoms in Parkinson’s disease (the ONSET PD study). Movement Disorders, 30(2), 229–237. https://doi.org/10.1002/mds.26077
Postuma, R. B., Berg, D., Stern, M., Poewe, W., Olanow, C. W., Oertel, W., … Halliday, G. (2015). MDS clinical diagnostic criteria for Parkinson’s disease. Movement Disorders, 30(12), 1591–1601.
Ramírez-Ruiz, B., Martí, M. J., Tolosa, E., Bartrés-Faz, D., Summerfield, C., Salgado-Pineda, P., … Junqué, C. (2005). Longitudinal evaluation of cerebral morphological changes in Parkinson’s disease with and without dementia. Journal of Neurology, 252(11), 1345–1352. https://doi.org/10.1007/s00415-005-0864-2
Reuter, I., Mehnert, S., Sammer, G., Oechsner, M., & Engelhardt, M. (2012). Efficacy of a multimodal cognitive rehabilitation including psychomotor and endurance training in Parkinson’s disease. Journal of Aging Research, 2012, 235765. https://doi.org/10.1155/2012/235765
Rosenthal, E., Brennan, L., Xie, S., Hurtig, H., Milber, J., Weintraub, D., … Siderowf, A. (2010). Association between cognition and function in patients with Parkinson disease with and without dementia. Movement Disorders, 25(9), 1170–1176. https://doi.org/10.1002/mds.23073
Ross, G. W., Petrovitch, H., Abbott, R. D., Tanner, C. M., Popper, J., Masaki, K., … White, L. R. (2008). Association of olfactory dysfunction with risk for future Parkinson’s disease. Annals of Neurology, 63(2), 167–173. https://doi.org/10.1002/ana.21291
Sammer, G., Reuter, I., Hullmann, K., Kaps, M., & Vaitl, D. (2006). Training of executive functions in Parkinson’s disease. Journal of the Neurological Sciences, 248(1), 115–119. https://doi.org/10.1016/j.jns.2006.05.028
Secker, D. L., & Brown, R. G. (2005). Cognitive behavioural therapy (CBT) for carers of patients with Parkinson’s disease: A preliminary randomised controlled trial. Journal of Neurology, Neurosurgery, and Psychiatry, 76(4), 491–497. https://doi.org/10.1136/jnnp.2004.042291
Segura, B., Ibarretxe-Bilbao, N., Sala-Llonch, R., Baggio, H. C., Marti, M. J., Valldeoriola, F., … Junque, C. (2013). Progressive changes in a recognition memory network in Parkinson’s disease. Journal of Neurology, Neurosurgery, and Psychiatry, 84(4), 370–378. https://doi.org/10.1136/jnnp-2012-302822
Sinforiani, E., Banchieri, L., Zucchella, C., Pacchetti, C., & Sandrini, G. (2004). Cognitive rehabilitation in Parkinson’s disease. Archives of Gerontology and Geriatrics, 38, 387–391. https://doi.org/10.1016/j.archger.2004.04.049
Stern, Y. (2002). What is cognitive reserve? Theory and research application of the reserve concept. Journal of the International Neuropsychological Society, 8(3), 448–460. https://doi.org/10.1017/S1355617701020240
Tolosa, E., Gaig, C., Santamaria, J., & Compta, Y. (2009). Diagnosis and the premotor phase of Parkinson disease. Neurology, 72(7 Suppl), S12–S20. https://doi.org/10.1212/WNL.0b013e318198db11
van Eimeren, T., Monchi, O., Ballanger, B., & Strafella, A. P. (2009). Dysfunction of the default mode network in Parkinson disease: A functional magnetic resonance imaging study. Archives of Neurology, 66(7), 877–883. https://doi.org/10.1001/archneurol.2009.97
Walton, C. C., Naismith, S. L., Lampit, A., Mowszowski, L., & Lewis, S. J. (2017). Cognitive training in Parkinson’s disease: A theoretical perspective. Neurorehabilitation and Neural Repair, 31(3), 207–216. https://doi.org/10.1177/1545968316680489
Williams-Gray, C. H., Foltynie, T., Brayne, C. E., Robbins, T. W., & Barker, R. A. (2007). Evolution of cognitive dysfunction in an incident Parkinson’s disease cohort. Brain: A Journal of Neurology, 130(7), 1787–1798. https://doi.org/10.1093/brain/awm111
Williams-Gray, C. H., Mason, S. L., Evans, J. R., Foltynie, T., Brayne, C., Robbins, T. W., & Barker, R. A. (2013). The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. Journal of Neurology, Neurosurgery, and Psychiatry, 84(11), 1258–1264. https://doi.org/10.1136/jnnp-2013-305277
Wykes, T., & Spaulding, W. D. (2011). Thinking about the future cognitive remediation therapy--What works and could we do better? Schizophrenia Bulletin, 37(Suppl 2), S80–S90. https://doi.org/10.1093/schbul/sbr064
Xia, R., & Mao, Z. (2012). Progression of motor symptoms in Parkinson’s disease. Neuroscience Bulletin, 28(1), 39–48. https://doi.org/10.1007/s12264-012-1050-z
Yarnall, A. J., Breen, D. P., Duncan, G. W., Khoo, T. K., Coleman, S. Y., Firbank, M. J., … ICICLE-PD Study Group. (2014). Characterizing mild cognitive impairment in incident Parkinson disease: The ICICLE-PD study. Neurology, 82(4), 308–316. https://doi.org/10.1212/WNL.0000000000000066
Yarnall, A. J., Rochester, L., & Burn, D. J. (2013). Mild cognitive impairment in Parkinson’s disease. Age and Ageing, 42(5), 567–576. https://doi.org/10.1093/ageing/aft085
Zhang, Y., Wu, I., Tosun, D., Foster, E., & Schuff, N. (2016). Progression of regional microstructural degeneration in Parkinson’s disease: A multicenter diffusion tensor imaging study. PLoS One, 11(10), e0165540. https://doi.org/10.1371/journal.pone.0165540
Zheng, Z., Shemmassian, S., Wijekoon, C., Kim, W., Bookheimer, S. Y., & Pouratian, N. (2013). DTI correlates of distinct cognitive impairments in Parkinson’s disease. Human Brain Mapping, 35(4), 1325–1333. https://doi.org/10.1002/hbm.22256
Zimmermann, R., Gschwandtner, U., Benz, N., Hatz, F., Schindler, C., Taub, E., & Fuhr, P. (2014). Cognitive training in Parkinson disease: Cognition-specific vs nonspecific computer training. Neurology, 82(14), 1219–1226. https://doi.org/10.1212/WNL.0000000000000287
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Díez-Cirarda, M., Ibarretxe-Bilbao, N., Peña, J., Ojeda, N. (2020). Parkinson’s Disease. In: DeLuca, J., Chiaravalloti, N.D., Weber, E. (eds) Cognitive Rehabilitation and Neuroimaging. Springer, Cham. https://doi.org/10.1007/978-3-030-48382-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-48382-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-48381-4
Online ISBN: 978-3-030-48382-1
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)