Abstract
Athero-embolic disease results from disruption of atheromatous plaque and subsequent migration of micro-fragments to distal vessels including the kidneys, resulting in an inflammatory response. The true incidence of renal athero-embolic disease is unknown, and it remains an underdiagnosed entity. Risk factors include male gender, age >60 years, white race, smoking history, diabetes mellitus, hypertension known atherosclerotic vascular disease, and femoral access route during cardiac catheterizations. Kidney injury follows an acute presentation or more commonly, a slow indolent course. Characteristic skin findings include the “purple toe” syndrome, livedo reticularis, and skin ulcerations. Typical findings on renal biopsy show the cholesterol emboli appearing as elongated, biconvex, needle-shaped clefts in the arteries or arterioles with inflammation surrounding the involved vessel. Treatment for this condition is mainly supportive. Given the increasing number of complex cardiovascular interventions for coronary artery disease and structural heart disease, recognizing athero-embolic disease risk factors prior to interventions and the occurrence of this entity after the procedure is key. Reducing athero-embolic disease risk prior to planned interventions should be part of a multidisciplinary cardionephrology assessment, given the limited therapeutic options that are available for this entity at this time.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Athero-embolic disease is a multisystemic disorder that is a result of the disruption of an atheromatous plaque and subsequent migration of plaque micro-fragments to distal vessels, resulting in an intense inflammatory response after lodging and disruption of blood flow. Also called cholesterol embolization syndrome, the disease is characterized by emboli that are rich in cholesterol crystals with multi-organ involvement. Renal involvement is seldom solitary and more often part of the systemic presentation of the condition [1, 2].
History
The earliest descriptions of athero-embolism come from mid-nineteenth century. Fenger and colleagues [3], when describing the autopsy of Icelandic sculptor Thorvaldsen, first reported this condition in the Danish literature in 1844. Panum [4] translated these findings into German in 1862. Further reporting was limited to autopsies. One of the first series by Flory [5] involving 267 subjects, described wedge-shaped, avascular areas supplied by involved vessels. Hollenhorst [6] described clinical findings of cholesterol embolization by describing his eponymous refractile plaques on retinal exam in 1961. Since then, other systemic findings like the “blue toe syndrome” have been described. Fine and colleagues [2] later reported antemortem diagnosis in 1987 in a review of 221 cases.
Pathogenesis and Risk Factors
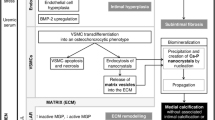
Cholesterol embolization requires the presence of a cholesterol-rich atheromatous plaque in a proximal vessel. Following an inciting event, or spontaneously, as was more common when first reported, the plaque erodes and exposes the underlying lipid-rich core, composed of calcium, lipids including cholesterol crystals, smooth muscle, platelets, fibrin, and mononuclear cells. The plaque debris embolizes to small-to-medium-dimensional vessels, resulting in local occlusion of blood flow. The presence of these emboli triggers a foreign body response, resulting in local acute inflammatory response at sites of said showers of emboli. The inflammatory infiltrate includes neutrophils and eosinophils in the walls of the involved vessels, resulting in local thrombus formation and occlusion of blood flow.
With Flory’s observations, the correlation between atherosclerotic aortic disease and the findings of cholesterol embolization was established. With increasing severity of atherosclerosis, he reported increased incidence of cholesterol embolization: none in cases where no aortic ulcerations were present (63 cases), 2 cases of arterial occlusions where mild to moderate aortic ulcerations were present (147 total cases, 1.3%), and 7 cases or 12.3% of arterial occlusions in 57 cases of severe plaque ulcerations were present. Summarized below are the associated risk factors in Table 16.1 [7, 8]. White race is likely identified as a risk factor due to underdiagnosis of cutaneous lesions of livedo and purple discoloration in blacks. The presence of diffuse aortic atherosclerosis is a strong predisposing factor [1, 5].
Triggers and Incidence
The precise incidence of athero-embolic renal disease is unknown, as the condition remains largely underdiagnosed. Prospective studies are mostly lacking. Among the earliest autopsy series, the phenotype of spontaneous athero-embolism predominated. Per Flory [5] in 1945, spontaneous athero-embolism accounted for about 3.4% of the described 267 cases. Unselected autopsy series such as by Kealy et al. from 1978 showed an incidence of 0.79% in males above 60 years [9]. Overall, the incidence ranged from 0.79% to 3.4%, markedly lower than the rates reported post cardiovascular intervention.
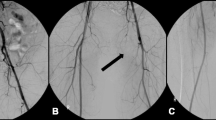
Since the advent of coronary and aortic interventions and increased use of anticoagulation and thrombolytic therapy, most reported cases are iatrogenic, accounting for three out of four cases. Among reported triggers are percutaneous vascular interventions – coronary and noncoronary angioplasty such as for renal artery stenosis, vessel incisions, and mechanical aortic trauma such as caused by radiological catheters, vessel clamping, or manipulation. Any of these can cause plaque disruption [7, 8, 10, 11]. In a prospective study by Keeley et al., more than 50% of 1000 percutaneous revascularization procedures observed were associated with scraping debris from the aorta. However, the presence of debris was not found to be associated with in-hospital ischemic complications [11].
Cardiovascular surgical procedures such as coronary artery bypass grafts, mitral valve surgery, carotid endarterectomy, aortofemoral bypass grafts have been implicated in the development of cholesterol emboli in up to 16% of cases. Noncoronary angiography such as carotid, aortic, thoraco-abdominal, or renal angiography makes up a small percentage of cases of iatrogenic cholesterol embolization [12]. It has also been reported to occur after transcatheter aortic valve replacement [13].
Early reports by Thurlbeck and Castleman following aortic surgery or older patients following interventions reported incidence as high as 77% [1]. Currently, angiography accounts for most cases of cholesterol embolization, accounting for 80% in some studies, with coronary angiography accounting for above 40% of those [14]. Discrepancies in these rates exist between different studies, frequently due to limited ability to research retrospective data [10, 15].
Anticoagulation (heparin, low-molecular-weight heparin, warfarin) and thrombolytic therapy have been implicated as well, possibly by destabilizing the ulcerated plaque [2, 7, 14, 16,17,18]. However, overall incidence of embolization due to anticoagulation alone remains low, at less than 1%, even with severe aortic plaques, as observed in one study [19]. More recently, there have been case reports of cholesterol embolism associated with the use of novel oral anticoagulants (NOACS) apixaban, dabigatran, edoxaban, and rivaroxaban [20].
Fine’s group reported the incidence of renal involvement in athero-embolic disease is about 50% in a male-predominant group of 221 patients with a mean age of 66 years [2]. Renal involvement varies, often due to the difficulty in diagnosing cholesterol embolization to the kidneys with clinical markers alone. Since most the affected patients tend to be elderly and rates of renal biopsy are lower in these patients, histological proof is often lacking. Additionally, it is hard to clinically tease out the role of contrast-induced acute kidney injury in these cases as the same subsets of patients are at highest risk for both insults. Often, additional signs or symptoms for peripheral embolization are lacking, as discussed below. Persistence of renal injury beyond the usual 2-week period can often point to cholesterol embolization rather than contrast-induced injury.
Role of Catheterization Access Routes
Coronary angiography via the femoral artery has been described as the most common precipitating factor in majority of patients with athero-embolic renal disease which may suggest an association regarding catheterization access route [21]. The risk of cholesterol embolization may be potentially increased with the femoral approach due to catheterization of the descending aorta. A prospective study by Kooiman using a regional database compared the risks of acute kidney injury (AKI) and nephropathy requiring dialysis (NRD) among patients treated with transradial percutaneous coronary intervention (PCI) versus transfemoral PCI. In the propensity-matched population consisting of 8857 procedures per group, transradial PCI was associated with lower adjusted odds ratio of acute kidney injury (OR, 0.74; 95% confidence intervals [0.58–0.96]) and bleeding (OR, 0.47; 95% confidence intervals [0.36–0.63]), but no difference in NRD was observed [22].
Similar findings were reported in the Acute Kidney Injury-Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox (AKI-MATRIX) study, a large, randomized, multicenter trial in patients with ST segment or non ST segment elevation myocardial infarction who underwent coronary angiography with or without PCI comparing incidence of AKI with radial versus femoral access. AKI was defined as either an absolute (>0.5 mg/dl) or a relative (>25%) increase from baseline in serum creatinine (sCr) levels during hospitalization. In this study, AKI occurred less in the radial approach compared with the femoral approach (15.4% vs 17.4%, (odds ratio [OR]: 0.87; 95% confidence interval [CI]: 0.77–0.98; p = 0.0181, [23]).
Potential reasons for decreased AKI in the radial approach include decreased risk of cholesterol embolization to the kidneys, decrease in episodes of hypotension due hemodynamically significant bleeding or vasovagal responses to femoral sheath removal, and a lower contrast volumes, although this difference was modest [22, 23]. In contrast, another prospective study by Fukumoto et al. did not find an increased risk of cholesterol embolization syndrome by the femoral approach [10].
Clinical Features
Clinical symptoms and signs of embolization syndrome vary depending on the location of originating plaque, frequency and recurrence of showering plaques, and burden of atherosclerotic disease. Patients can range from being clinically asymptomatic to having multi-organ involvement as detailed in Table 16.2 [1, 2, 5, 24].
The involvement of the kidneys, when overt, follows an acute presentation or more commonly a slow and indolent course often from recurrent showers of embolization. The acute presentation usually occurs within a week of the inciting event and results in fulminant involvement from large burden of emboli. It is responsible for about a third of renal athero-embolic disease [7]. The subacute presentation involves a stepwise worsening of renal function and is the most common presentation. After a rise in serum creatinine within a few weeks after the triggering event, renal function partially stabilizes before ensuing slow worsening. Renal involvement can result in accelerated hypertension. Lye et al. [16] reported severe hypertension in 48% of the diagnosed cases of renal embolization. Purported mechanisms include renal ischemia and renin-angiotensin activation. Multi-organ features usually accompany renal involvement. Skin involvement is most common among involved organs, with some authors reporting from 30% to 90% incidence in proven cases of embolization (Table 16.3). Typical lesions include the “purple toe” syndrome, characterized by the sudden appearance of a cyanotic toe, with preserved peripheral pulses. This is often complicated by ulceration requiring digital amputation. Livedo reticularis can be noted on the peripheries or the lumbar region, characterized by a lacy blue rash, resulting from emboli to the dermal vessels. Gastrointestinal (GI) involvement is reported in up to a third of cases and can cause abdominal pain from mucosal ulceration or mesenteric ischemia, depending on the location of the emboli. Blood loss can be occult to overt, presenting as melena or bloody diarrhea, depending on the site and location of ulceration, while transaminitis reflects emboli to the liver. Repeated emboli can cause fibrosis of involved GI tract. Retinal involvement takes the form of visible, refractile plaques named Hollenhorst plaques [6]. Diagnosis depends on the quality of exam, index of suspicion, and correlation with vascular interventions. Reported incidence range from 6% to 25%, depending on source [2, 14, 16, 17]. Other central nervous system manifestations can range from confusion, focal neurological deficits causing TIA, or amaurosis fugax to cerebral infarction. Emboli to muscles can cause myositis. Virtually any organ can be involved.
Laboratory Features
Lab findings are nonspecific but can lend to the diagnosis if clinical suspicion is high. Presence of anemia, thrombocytopenia, and leukocytosis can be seen along with elevation in serum inflammatory markers such as CRP or ESR. Urinalysis can show microscopic hematuria, non-nephrotic range proteinuria, and pyuria. Eosinophilia can be transiently present. Kasinath et al. [25] reported presence of eosinophilia in about 80% of cases of athero-embolic renal disease. Persistent eosinophilia can be related to recurrent showers of athero-emboli. Other case series have reported incidence of eosinophilia ranging from as low as 17% [14, 17]. Low complement levels were reported by Lye et al. in 39% of their studied patients [16]; however subsequent groups have noted normal levels [17]. Similarly, organ-specific laboratory findings might implicate a wider involvement than suggested clinically. Elevated creatinine phosphokinase (CK) levels suggest myositis. Raised amylase or lipase levels suggest pancreatic involvement. High serum cholesterol levels are a risk factor for athero-embolism, and a few studies report higher serum cholesterol levels in patients with athero-embolic renal disease [21].
Diagnosis
Athero-embolic renal disease is difficult to diagnose due to the many and varied presentations and organ involvement. It can mimic other conditions and without a significant index of suspicion, can be missed clinically. Histologic diagnosis is often limited to postmortem findings, as renal biopsies are rare in the elderly population that are at highest risk for athero-embolic disease in general. Per literature review, different groups have had varying experience with rates of histological and clinical diagnosis (Table 16.3).
For the confirmation of the diagnosis, biopsy of the skin lesion or involved organ may be required. Typically this means a skin, kidney, or muscle biopsy. Skin biopsy is considered the safest and highest-yielding choice when skin lesions are noted. Cholesterol emboli appear as elongated, biconvex, needle-shaped clefts in the vessels with inflammation surrounding the involved vessel in all involved organs (Fig. 16.1). Arteriosclerotic lesions and hyalinosis of the glomeruli or tubules can be noted, especially in the setting of ischemic nephropathy from repeated embolic showers. Renal parenchyma might show wedge-shaped infarcts in the cortical areas in areas involved by obstructed vessels (Fig. 16.2).
Renal cholesterol crystal emboli. Intraglomerular cholesterol crystals (arrows, a, b); cholesterol crystals in a renal arteriole (c); crystals in an arcuate artery with a pseudovasculitis inflammatory reaction (arrow, d); crystals in an arcuate artery and encasement of a crystal by a giant cell (arrow, e); and organized occlusive crystals in a renal arteriole (f). (Adapted with permission from Scolari and Ravani [24])
Cholesterol crystal emboli in dermal arterioles. Low-power view of cholesterol crystals (arrow, a) and high-power view showing clusters of cholesterol crystals (b–d). (Adapted with permission from Scolari and Ravani [24])
Treatment
There is no specific therapy for renal athero-embolic disease. Treatment is mainly supportive. All patients should be aggressively treated for secondary prevention of cardiovascular disease including institution of statins, aspirin, blood pressure control, smoking cessation, and glycemic control in diabetics.
Some case reports have noted halting and reversal of progressive renal dysfunction after treatment with statins [26, 27]. Other observational studies note improvement in renal function with low- or high-dose corticosteroids [28, 29]. In a retrospective study of 51 patients by Nakayama et al., patients were divided into two groups according to whether or not they had received steroids. At 4 weeks, more patients who received low-dose corticosteroids showed improvement in renal function. However, on long-term follow-up, there was no significant difference in the change of GFR between diagnosis and last follow-up between the two groups [30].
Prognosis
Prognosis for renal athero-embolic disease is generally poor probably reflecting the severity of underlying vascular disease. In a prospective study by Scolari et al. of 354 subjects with athero-embolic renal disease, 116 patients (33%) required dialysis, and 102 patients (28%) died during an average follow-up of 2 years [21]. Lye and colleagues reported 40% of 129 patients required dialysis and had a 1-year mortality rate of 64% [16]. Belenfant and co-workers reported 41 of 67 patients (61%) developed renal failure needing dialysis, of which 16 (39%) recovered renal function. In this study, the 1-year mortality rate was lower at 13%, probably due to a more aggressive therapeutic approach [17]. In a case series of 52 histologically proven cases, Thadani et al. found that patients with renal failure due to athero-embolism alone, as opposed to multiple renal insults, were more likely to recover renal function (24% versus 3%) [14]. Predictors of the need for long-term dialysis include preexisting chronic kidney disease and longstanding hypertension. Factors associated with higher risk of death include diabetes, heart failure, baseline level of renal function, acute or subacute renal failure, and presence of extrarenal manifestations [21].
Conclusions and Future Directions
Renal athero-embolic disease remains to be an underdiagnosed entity. Risk factors include male, age > 60 years old, white race, smoking, hypertension, diabetes mellitus, and known atherosclerotic disease. Majority of cases are seen after coronary angiography. Renal dysfunction can follow an acute, subacute, or chronic course. Increased vigilance and identification of this condition is warranted especially in patients undergoing angiography or other cardiac procedures. Prospective trials regarding prevention and treatment are needed to limit the significant morbidity and mortality associated with this syndrome.
References
Thurlbeck WM, Castleman B. Atheromatous emboli to the kidneys after aortic surgery. N Engl J Med. 1957;257(10):442–72.
Fine MJ, Kapoor W, Falanga B. Cholesterol crystal embolization: a review of 221 cases in the English literature. Angiology. 1987;38(10):769–84.
Fenger CE. J. J. Beretning af Obductionen over Albert Thorvaldsen (autopsy report of Albert Thorvaldsen). Ugeskr Laeger. 1844;X(14–15):215–8.
Panum P. Experimentell Beitrage zur Lehre von der Embolie. Virchows Arch Pathol Anat. 1862;25:308–10.
Flory C. Arterial occlusions produced by emboli from eroded aortic atheromatous plaques. Am J Path. 1945;21(3):549–65.
Hollenhorst R. Significance of bright plaques in the retinal arterioles. JAMA. 1961;178(1):23–9.
Scolari F, Tardanico R, Zani R, Pola A, Viola BF, Movilli E, Maiorca R. Cholesterol crystal embolism: a recognizable cause of renal disease. Am J Kidney Dis. 2000;36(6):1089–109.
Modi K, Rao V. Atheroembolic renal disease. J Am Soc Nephrol. 2001;12(8):1781–7.
Kealy W. Atheroembolism. J Clin Pathol. 1978;31(10):984–9.
Fukumoto Y, Tsutsui H, Tsuchihashi M, Masumoto A, Takeshita A. The incidence and risk factors of cholesterol embolization syndrome, a complication of cardiac catheterization: a prospective study. J Am Coll Cardiol. 2003;42(2):211–6.
Keeley EC, Grines CL. Scraping of aortic debris by coronary guiding catheters: a prospective evaluation of 1,000 cases. J Am Coll Cardiol. 1998;32(7):1861–5.
Agrawal A, Ziccardi MR, Witzke C, Palacios I, Rangaswami J. Cholesterol embolization syndrome: an under-recognized entity in cardiovascular interventions. J Interv Cardiol. 2018;31:407–15.
Devy L, Brunet-Possenti F. Cholesterol embolization after transcatheter aortic-valve replacement. N Engl J Med. 2016;375:11.
Thadani R, Camargo C, Xavier R, Fang L, Bazari H. Atheroembolic renal failure after invasive procedures. Natural history based on 52 histologically proven cases. Medicine. 1995;74(6):350–8.
Nasser T, Mohler E, Wilensky R, Hathaway D. Peripheral vascular complications following coronary interventional procedures. Clin Cardiol. 1995;18(11):609–14.
Lye WC, Cheah JS, Sinnjah R. Renal cholesterol embolic disease. Case report and review of the literature. Am J Nephrol. 1993;13(6):489–93.
Belenfant X, Meyrier A, Jacquot C. Supportive treatment improves survival in multivisceral cholesterol crystal embolism. Am J Kidney Dis. 1999;33(5):840–50.
Gupta BK, Spinowitz BS, Charytan C, Wahl SJ. Cholesterol crystal embolization- associated renal failure after therapy with recombinant tissue-type plasminogen activator. Am J Kidney Dis. 1993;21:659–62.
Tunick PA, Nayar AC, Goodkin GM, Mirchandani S, Francescone S, Rosenzweig BP, Freedberg RS, Katz ES, Applebaum RM, Kronzon I. Effect of treatment on the incidence of stroke and other emboli in 519 patients with severe thoracic aortic plaque. Am J Cardiol. 2002;90(12):1320–5.
AHG M-H, CRGM D-G, Schut NH. Cholesterol embolisms as possible adverse drug reaction of direct oral anticoagulants. Neth J Med. 2018;76(3):125–8.
Scolari F, Ravani P, Gaggi R, Santostefano M, Rollino C, Stabellini N, Colla L, Viola BF, Maiorca P, Venturelli C, Bonardelli S, Faggiano P, Barrett BJ. The challenge of diagnosing atheroembolic renal disease, clinical features and prognostic factors. Circulation. 2007;116(3):298–304.
Kooiman J, Seth M, Dixon S, et al. Risk of acute kidney injury after percutaneous coronary interventions using radial versus femoral access. Insights from the blue cross blue shield of Michigan Cardiovascular Consortium. Circ Cardiovasc Interv. 2014;7:190–8.
Ando G, Cortese B, Russo F, et al. Acute kidney injury after radial or femoral access for invasive acute coronary syndrome management, AKI-MATRIX. J Am Coll Cardiol. 2017;69:2592–603.
Scolari F, Ravani P. Atheroembolic renal disease. Lancet. 2010;375(9726):1650–60.
Kasinath BS, Coewin HL, Bidani AK. Eosinophilia in the diagnosis of atheroembolic renal disease. Am J Nephrol. 1987;7:173–7.
Woolfson RG, Lachmann H. Improvement in renal cholesterol emboli syndrome after simvastatin. Lancet. 1998;351(9112):1331–2.
Yonemura K, Ikegaya N, Fujigaki Y, Suzuki H, Togawa A, Hishida A. Potential therapeutic effect of simvastatin on progressive renal failure and nephrotic-range proteinuria caused by renal cholesterol embolism. Am J Med Sci. 2001;322(1):50–2.
Sharma A, Hada R, Agrawal RK, Baral A. Favorable outcome in atheroembolic renal disease with pulse steroid therapy. Indian J Nephrol. 2012;22(6):473–6.
Mann SJ, Sos TA. Treatment of atheroembolization with corticosteroids. Am J Hypertens. 2001;14(8 Pt 1):831–4.
Nakayama M, Isumaru K, Nagata M, Ikeda H, Nishida K, Hasegawa W, Ohta Y, Tsuchihashi T, Urabe K. The effect of low-dose corticosteroids on short- and long-term renal outcome in patients with cholesterol crystal embolism. Ren Fail. 2011;33(3):298–30624.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Punj, S., Tuazon, J. (2020). Renal Athero-embolic Disease: An Underdiagnosed Entity in Cardiac Catheterization. In: Rangaswami, J., Lerma, E., McCullough, P. (eds) Kidney Disease in the Cardiac Catheterization Laboratory . Springer, Cham. https://doi.org/10.1007/978-3-030-45414-2_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-45414-2_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45413-5
Online ISBN: 978-3-030-45414-2
eBook Packages: MedicineMedicine (R0)