Abstract
Advanced glycation end products (AGEs) play a major role in diabetic vascular complications, such as chronic kidney disease (CKD), by activating pro-oxidant and pro-inflammatory responses. Although traditionally AGEs have been associated with uncontrolled hyperglycemia of diabetes mellitus, there is increasing evidence that exogenous AGEs from diet have an important contribution to these processes. The reduction of dietary AGE intake has been demonstrated to prevent or diminish pro-oxidant and pro-inflammatory responses in several clinical trials. These trials have also demonstrated that dietary AGE restriction is simple, feasible, and safe to apply clinically, even in CKD patients. In this chapter, we will summarize the current data on the use of this intervention in clinical practice with particular emphasis on CKD patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Advanced glycation end products
- Chronic kidney disease
- Diabetes mellitus
- Oxidative stress
- Inflammation
- Carboxymethyllysine
- Pentosidine
- Methylglyoxal
- Diet
- Nutritional intervention
-
Advanced glycation end products (AGEs) can be produced endogenously or obtained exogenously from the diet.
-
AGEs have been associated with kidney damage and, thus, progression of chronic kidney disease.
-
Cooking methods where high heat and low moisture are used increase the formation of AGEs.
-
Interventions with a low dietary AGE have been shown to reduce circulating AGEs and markers of oxidative stress and inflammation.
-
Diets low in AGEs should be recommended for patients at high risk of CKD.
Introduction
Advanced glycation end products (AGEs) play a major role in diabetic vascular complications, such as chronic kidney disease (CKD), by activating pro-oxidant and pro-inflammatory responses [1, 2]. Although traditionally AGEs have been associated with uncontrolled hyperglycemia of diabetes mellitus, there is increasing evidence that exogenous AGEs from diet have an important contribution to these processes [3, 4]. The reduction of dietary AGE intake has been demonstrated to prevent or diminish pro-oxidant and pro-inflammatory responses in several clinical trials [5,6,7,8,9,10]. These trials have also demonstrated that dietary AGE restriction is simple, feasible, and safe to apply clinically, even in CKD patients. In this chapter, we will summarize the current data on the use of this intervention in clinical practice with particular emphasis on CKD patients.
What Are Advanced Glycation End Products (AGEs) and How Do They Cause Disease?
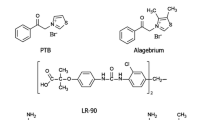
AGEs are a very large and heterogeneous group of compounds originating from the spontaneous reaction of reducing sugars with free amino groups in amino acids in the so-called Maillard or browning reaction. Although a lot of attention has been devoted to this reaction, we currently know that AGEs can be formed through many other reactions, such as oxidation of sugars, lipids, and amino acids that creates reactive aldehydes that in turn form AGEs. Carboxymethyllysine (CML), carboxyethyllysine (CEL), methylglyoxal-derivatives (MG), and pentosidine are some commonly measured and well-described AGEs in biological studies.
AGEs form continuously in the body through a variety of spontaneous reactions, which are markedly increased in conditions of hyperglycemia or elevated oxidative stress, such as in CKD; these are the endogenous AGEs. Of note, however, AGEs can also form outside of the body in any system as long as the required reagents are available. For example, we know they form spontaneously in food, especially when processed and cooked with heat; these are the exogenous AGEs [11, 12]. In a fraction of ingested food, AGEs will get absorbed and incorporated into the body AGE pool, where they are indistinguishable from their endogenous counterparts, both in structure and function [13].
AGEs, endogenous or exogenous, lead to tissue injury by at least two mechanisms: (1) by causing protein cross-linking, inducing direct modifications of protein structure and, therefore, function and (2) by activating pro-inflammatory and pro-oxidative cellular signaling pathways through receptor- and non-receptor-mediated mechanisms. For example, direct cross-linking of collagen may be responsible for arterial wall stiffness, and glycation of specific amino acids in a protein molecule could affect the binding of this protein to receptors.
AGE binding to the receptor of AGEs (RAGE) or Toll-like receptors (TLRs) 2 and 4 initiates intracellular signaling that leads to the activation of several pro-inflammatory and pro-oxidative stress responses [14]. In contrast, AGE binding and activation of the AGE receptor 1 (AGER1) initiate AGE breakdown and diminish the RAGE-mediated activation of nuclear factor-kappa B (NF-κB) [15].
Increased oxidative stress and inflammation are the underlying mechanisms of many chronic diseases, including diabetes, cardiovascular disease, and CKD. The kidneys are the major players in maintaining AGE homeostasis. AGE peptides undergo filtration followed by partial tubular reabsorption and possibly also secretion after tubular uptake from the peritubular blood flow [16]. AGEs undergo variable degrees of catabolism within the renal tubules. Not surprisingly, an elevation of AGEs is characteristic of any reduction in kidney function [17] and may play a role in facilitating the progression of any underlying kidney condition. Circulating AGE levels are markedly increased in CKD of any etiology, before and after the initiation of dialysis [1, 18]. This increase of AGEs in CKD may play a role in the high prevalence of endothelial dysfunction and subsequent cardiovascular disease in this population [19].
Conventional hemodialysis (HD) of three times a week for 4 hours each is not very effective at removing AGEs [18], while short daily dialysis, hemodiafiltration, and hemofiltration have been shown to be more effective [20, 21]. At least in one study , hemodiafiltration significantly lowered serum AGE levels as compared to high-flux HD by the end of the treatment period [22]. Circulating AGE levels are also increased in peritoneal dialysis (PD) patients, but lower than in HD patients, and the amount seems to vary depending on the type of PD solution [18, 23, 24]. Importantly, circulating AGE levels fall significantly following a successful kidney transplantation [25].
Evidence Linking AGEs and Kidney Disease
In Vitro Studies
AGEs, through their cross-link of proteins in the kidney extracellular matrix, lead to many abnormalities: altered matrix protein structure and function, aberrant cell-matrix interactions that change cellular adhesion, altered cell growth, and loss of the epithelial phenotype [26, 27].
In vitro incubation of AGEs with every cell type within the kidneys has been shown to initiate potential mechanisms of cell injury [28]. For example, binding of AGEs to mesangial cells increases production of matrix proteins while decreasing expression of major metalloproteinases that normally would degrade matrix proteins [29]. Incubation of human glomerular endothelial cells with AGEs increases expression of vascular endothelial growth factor that attracts inflammatory cells [30]. RAGE activation changes the endothelium surface from an anticoagulant to a procoagulant state by reducing thrombomodulin activity and increasing tissue factor expression [31]. AGEs also affect podocytes inducing podocyte apoptosis and reducing expression of nephrin [32], providing a direct link between AGEs and kidney damage.
Animal Studies
There is strong experimental animal data supporting a role for AGEs causing kidney damage in vivo. A classic study showed that intraperitoneal administration of AGEs for 4 weeks into mice induced a marked increase in glomerular extracellular matrix α1(IV) collagen, laminin β1, and transforming growth factor β (TGFβ) [33]. Moreover, these changes diminished with the coadministration of aminoguanidine, a known AGE inhibitor [33]. In another study , long-term administration of intravenous AGE-albumin to normal rats induced albuminuria and morphologic changes of diabetic nephropathy, including glomerular hypertrophy, mesangial matrix expansion, and basement membrane thickening [34]. Overexpression of RAGE in diabetic mice increased the signs of kidney disease, while blockade of RAGE by a soluble truncated form of RAGE prevented structural and functional characteristics of nephropathy in db/db mice [35, 36]. Anti-AGE strategies, such as the administration of aminoguanidine, benfotiamine, pyridoxamine, OPB-9195, and AGE breakers, have all been shown to ameliorate diabetic nephropathy in rats without influencing glycemic control [37, 38].
A direct connection between dietary AGEs and the development of kidney disease was demonstrated when diabetic nephropathy, highly prevalent in non-obese diabetic mice with type 1 diabetes and db/db mice with type 2 diabetes, fed with regular chow (rich in AGEs through pellet formation and sterilization), was almost completely abrogated in the same groups of mice randomized to a low-AGE diet (which was a purified diet that does not need to be sterilized) [39].
Human Data
Effects of Acute Oral AGE Loads
Recently, an interesting study performed in healthy volunteers tested the acute effect of a protein load (1 g/kg) either high or low on AGEs on noninvasive parameters of kidney function [40]. The study suggests that it is the AGE content, not the total protein load, that is responsible for the observed renal hemodynamic modifications (increased renal perfusion and renal oxygen consumption). Extrapolating results one may assume that decreasing dietary AGE content may ameliorate glomerular hyperfiltration and perhaps progressive CKD , but long-term studies are lacking.
In the past, acute oral AGE loads have been shown to have endothelial effects on both healthy subjects and diabetic patients. In one study, a single oral dose of a high-AGE beverage was administered to both healthy subjects and patients with diabetes [41]. Within 2 hours, serum AGE levels increased in association with transient impairment of flow-mediated vasodilatation , a noninvasive test of endothelial function. Pretreatment of the subjects with benfotiamine, an inhibitor of glycation, prevented the endothelial effects [42]. In another study, a single high-AGE solid meal given to patients with diabetes was also followed by marked impairment of flow-mediated vasodilatation, as compared with an isocaloric low-AGE meal [43]. All of these results support a mechanistic link between dietary AGEs and cardiovascular disease, since endothelial dysfunction is the earliest abnormality in atherosclerosis.
Observational Studies
There are several studies showing an association between levels of circulating AGEs and progression of CKD [43,44,45,47]. In a study in American Indians with type 2 diabetes, circulating AGEs (including CML and CEL) were inversely associated with glomerular filtration rate [44]. In a prospective cohort of individuals with CKD , MG was an independent risk factor for death, cardiovascular events, and/or end-stage kidney disease (ESKD) (which were the primary endpoints) [46]. Similarly, Semba et al.[45] showed that in a cohort of community-dwelling women from the Women’s Health and Aging Study, circulating CML and the soluble RAGE were independently associated with lower glomerular filtration rate. Finally, circulating levels of soluble RAGE were positively associated with CKD and ESKD [47].
Clinical Trials with Dietary AGE Restriction
CKD Patients Without Diabetes
Two clinical trials have tested the effects of an AGE-restricted diet in patients with CKD in the absence of diabetes. In one of the studies, a group of stage 3 CKD patients was randomly assigned to either a regular diet or an isocaloric diet containing 50% lower AGEs for a period of 4 weeks [7]. Patients on the low-AGE diet exhibited a significant decrease of extracellular and intracellular markers of inflammation and oxidative stress, including AGEs, tumor necrosis factor (TNFα), vascular cell adhesion molecule 1 (VCAM-1), and RAGE compared to the regular diet group [7]. In a second trial, a group of patients with ESKD without diabetes on maintenance PD was randomized to follow either a regular or a low-AGE diet for 4 weeks [6]. The low-AGE diet group showed a significant decrease in the levels of circulating AGEs and high-sensitivity C-reactive protein (hsCRP) [6].
In the above studies, patients with CKD without diabetes were instructed to lower the dietary intake of AGEs, while maintaining the same baseline caloric and nutrient content. This was achieved by receiving detailed instructions on how to prepare their food at home by a study dietitian who was in frequent telephone contact with them.
Patients with Diabetes without CKD
A few trials on the effect of dietary AGE restriction have been performed in patients with diabetes without overt kidney disease. The first study was published in 2002 [5]. This was a crossover study between low and regular AGE diets for a period of 6 weeks. Meals were prepared in the clinical research unit metabolic kitchen and patients picked them up twice a week during the duration of the study. Levels of circulating AGEs (both CML and MG) as well as markers of endothelial function and inflammation such as VCAM-1, hsCRP and TNFα markedly decreased in patients during the low-AGE diet intervention. Circulating AGE levels decreased by as much as 40% during the study despite similar degree of diabetic control. Of importance, before this study was published, high serum AGE levels in patients with diabetes were thought to result exclusively from hyperglycemia-induced endogenous overproduction. Therefore, the observed fall of serum AGE levels while maintaining overall unchanged glycemic control, probably attributed to the restricted AGE diet, was a novel finding.
In a more recent study , a group of patients with type 2 diabetes were randomized to follow either a regular or a low-AGE diet for 4 months [8]. Circulating markers of AGEs, inflammation, and oxidative stress also decreased following the low-AGE diet, but more importantly the AGE-restricted diet decreased the homeostatic model assessment index (HOMA), a marker of insulin resistance [8]. This reduction of HOMA, which implies improvement of insulin sensitivity, brings up an important hypothesis: AGEs seem to have an important role in modifying insulin resistance itself and, therefore, diabetes. If this effect of the low-AGE diet is further confirmed, it opens a big opportunity for a safe, inexpensive, and effective dietary modulation to prevent or improve diabetes and, therefore, future development of CKD.
A low-AGE diet has also been shown to increase AGER1 and sirtuin 1 (SIRT1), two protective markers that tend to be suppressed in conditions of high oxidative stress, such as diabetes and CKD [48]. The restoration of their levels by the low-AGE diet suggests the previous suppression is due to an environmental factor , most likely the high AGE-induced oxidative stress.
A third published clinical trial performed in Mexico also demonstrated that a low-AGE diet decreased markers of inflammation and oxidative stress in a group of patients with type 2 diabetes [10]. Recently, a randomized controlled trial by Lopez-Moreno et al. [49] tested the effects of a high saturated fat diet, high monounsaturated fat diet, and low-fat high-complex carbohydrate diet with or without omega-3 fatty acids in individuals with metabolic syndrome. The authors showed that those in the high monounsaturated fat diet reduced circulating AGEs and expression of genes associated with AGEs in peripheral blood mononuclear cells , such as the receptor for RAGE [49]. Although none of the patients with diabetes included in the studies above had CKD, these studies are very pertinent to this chapter since diabetes is a major risk factor for CKD in the USA.
An Oral AGE Binder in CKD Patients with Diabetes
Two studies from the same group of investigators have been reported on the systemic effects of the use of sevelamer carbonate, proposed as an oral AGE binder, in CKD patients with diabetes [50]. Sevelamer is a nonselective anion binder, which is traditionally used as a phosphate binder, but may also bind other molecules, such as AGEs. The first study was a crossover study of 20 patients with diabetes and CKD comparing sevelamer carbonate versus calcium carbonate for 8 weeks, and the second study was a larger randomized study comparing sevelamer carbonate with calcium carbonate as parallel groups in 117 patients with type 2 diabetes and stages 2–4 CKD [51]. In both studies, attention was given to maintain dietary intake unchanged during the intervention period. The results in both studies were similar: sevelamer therapy, in contrast to calcium carbonate, reproduced all the findings observed with the low dietary AGE intervention described above, despite the unchanged dietary intake during the study period [50]. More specifically, the use of sevelamer was associated with reduced circulating levels of AGEs, 8-isoprostane, and TNFα, all of which were high and increased AGER1 and SIRT1, both of which were low. In vitro tests documented that sevelamer binds AGEs quite effectively, and presumably this was the explanation for the findings [50]. Of interest, in the second study, although the urinary albumin/creatinine ratio did not change in the overall group on sevelamer, subgroup analyses showed that the ratio was significantly decreased in subjects less than 65 years of age and in non-Caucasians [51]. Another randomized study from Japan looked at the effects of sevelamer versus calcium carbonate for 1 year in a group of 183 HD patients. Patients on sevelamer experienced decreased serum pentosidine levels and coronary artery calcium scores compared to those on calcium carbonate [42].
Healthy Subjects and Patients with the Metabolic Syndrome
A few studies done on healthy subjects [3, 7] and in patients with the metabolic syndrome [10, 51,52,54] have confirmed that the initiation of a low-AGE diet decreases circulating markers of AGEs, inflammation, oxidative stress, and more importantly, HOMA-IR index [10, 51,52,54].
How Does a Low-AGE Diet Work?
The exact mechanisms how dietary AGEs contribute to cardiovascular disease and CKD have not been precisely determined, but they may not just result from direct gastrointestinal absorption raising serum AGE levels that in turn induce elevated systemic oxidative stress and inflammation. In fact, only about 10% of dietary AGEs are absorbed [16]. However, it is also important to know that the amount of AGEs in foods far exceeds the amount of circulating AGEs and, thus, that 10% is a significant amount [16]. An action of unabsorbed dietary AGEs in the colon remains possible, including AGEs binding to RAGE or Toll-like receptors in the colon cells inducing a local inflammatory response with subsequent release of inflammatory mediators into the circulation or AGEs altering the microbiome profile in the gut leading to release of toxins into circulation. Yacoub et al. [55] assessed the effects of a low-AGE versus high-AGE diet for a month in peritoneal dialysis patients. They found that the dietary intervention altered the composition of the gut microbiota. Specifically, those in the AGE-restricted group had a reduction in the relative abundance of Prevotella copri and Bifidobacterium animalis and an increase in the relative abundance of Alistipes indistinctus, Clostridium citroniae, Clostridium hathewayi, and Ruminococcus gauvreauii. Recently, Snelson and Coughlan [13] reviewed the potential effects of AGEs on the gastrointestinal microbiome and metabolites produced by the microbiota. Interestingly, in experimental studies in rats, the use of heat-treated diets has been shown to decrease the cecal concentration of short-chain fatty acids, derived from the bacterial fermentation of carbohydrates and traditionally considered beneficial [13]. However, the long-term effects of these changes in the fecal microbiota and functional capacity of the microbiome in the context of CKD remain to be fully explored.
How to Implement and Recommend a Low-AGE Diet
Although the formation of AGEs is a complex process, dietary AGE intake is relatively easy to decrease. Additionally, a large database with the AGE content of common foods has been published and can be used to estimate dietary AGE intake as well as to give advice on how to reduce this intake [11, 12]. There are four main characteristics that affect the formation of AGEs in food: temperature, moisture, pH, and substrates for AGE formation (i.e., protein content) [11]. In terms of cooking foods, the basic concept of the low-AGE diet is that the same amount of a nutrient can provide very different amounts of oxidant substances depending on the cooking method. Unfortunately, there is no specific threshold temperature above which AGEs start to generate. Therefore, one can only make the general recommendation that the lower the temperature, the less the amount of AGEs generated. Cooking methods that use dry heat, such as broiling, searing, and frying, have been shown to have the highest content of AGEs [11]. Contrarily, methods that utilize a moisture-based heating process, such as poaching, stewing, steaming, and boiling, are lower in AGEs [11]. Thus, these methods should be preferred.
An acidic pH has also been shown to limit the formation of AGEs, whereas alkaline pH favors the Schiff base formation, one of the first reactions for AGE formation. Thus, the use of acidic foods, such as citrus foods or vinegars, as condiments can be recommended (i.e., marinade made with vinegar for high-protein foods, such as meats, is an easy way to incorporate into cooking). These culinary techniques have long been featured in the Mediterranean, Asian, and other cuisines throughout the world to create palatable, easily prepared meals, with an added benefit of limiting AGE formation.
The content of dietary protein is also a determinant of AGE formation, as it is the substrate of the amine group. Dietary protein intake is a cornerstone of the medical nutrition therapy in kidney diseases. While a low-protein diet is recommended in moderate-to-late stages of CKD, once patients transition into dialysis, dietary protein intake is recommended to increase. Unfortunately, to date, there are no studies that have assessed the effect of different amounts of dietary protein in nondialysis and dialysis-dependent CKD on circulating AGEs and AGE-mediated effects.
The immediate critique to a dietary intervention that relies on changing culinary technique is that patients will not follow it. The argument is often made that stewed chicken would be less tasty than fried chicken and, therefore, people will abandon this diet very easily. Based on our studies, however, consumers can be educated as to how to use low-AGE-generating cooking methods such as poaching, steaming, stewing, and boiling. Additionally, the use of herbs, condiments (free of sodium and potassium), and spices should be encouraged, as some may have intrinsic antiglycation activity. In addition, as mentioned above, the use of marinades based on citrus fruits and vinegars may also reduce the amount of AGEs formed. These recommendations would make the low-AGE diet appealing and flavorful.
Currently, no official recommendations exist which point out the acceptable range or identify the upper limit on dietary AGE intake. We have previously proposed that half of the current mean AGE intake, or about 7500 kU per day, is a realistic goal [11]. Studies have shown that dietary AGE reduction of this magnitude is feasible and can significantly alter levels of circulating AGEs, while at the same time reducing levels of markers of oxidative stress and inflammation and enhancing insulin sensitivity in patients with diabetes [5,6,7,8,9].
We propose a multipronged strategy, which is a food-first approach:
-
1.
Decrease the intake of foods rich in AGEs (based on existing databases), taking into consideration cooking methods, moisture, pH, and protein [11, 18].
-
2.
Increase the intake of fresh food, naturally high in polyphenols and antioxidants to counter the already high oxidative stress and inflammatory states in CKD.
-
3.
Incorporate the use of herbs, spices, and condiments (with no sodium or potassium added) to improve the taste of food and which may also have antiglycation effect (curcumin, cinnamon, parsley, thyme, and clove) [56].
-
4.
Although not a dietary intervention, avoid the use of cigarette as it is high in AGEs [56]. Additionally, supplementation with benfotiamine (a derivative of vitamin B1– thiamine) [43] and pyridoxamine (a form of vitamin B6) [57] has been shown in experimental and clinical studies to reduce AGE formation. We must state clearly, however, that we have tested only the AGE-restricted diet and we are assuming that the simultaneous application of points 2 through 4 will have beneficial and synergistic effects.
Conclusion
Dietary AGEs, abundantly present in the food commonly consumed in a typical American diet, contribute significantly to the body pool of AGEs, which in turn is at least partly responsible for the elevated oxidative stress and inflammation observed in patients with diabetes and CKD. A final proof of a therapeutic role for the low-AGE diet will require large, prospective, and randomized clinical trials, which indeed may never take place. In the meantime, however, we believe that a careful analysis of the current data makes it reasonable and prudent to advise the limitation of dietary AGEs in CKD patients. This is particularly important since consumption of lower-AGE foods and preparation methods can easily be integrated into dietary patterns that are consistent with current recommendations designed to promote public health and prevent cardiovascular disease, cancer, diabetes, and obesity.
References
Gugliucci A, Menini T. The axis AGE-RAGE-soluble RAGE and oxidative stress in chronic kidney disease. Adv Exp Med Biol. 2014;824:191–208.
Chilelli NC, Burlina S, Lapolla A. AGEs, rather than hyperglycemia, are responsible for microvascular complications in diabetes: a “glycoxidation-centric” point of view. Nutr Metab Cardiovasc Dis. 2013;23(10):913–9.
Uribarri J, Cai W, Peppa M, Goodman S, Ferrucci L, Striker G, et al. Circulating glycotoxins and dietary advanced glycation endproducts: two links to inflammatory response, oxidative stress, and aging. J Gerontol A Biol Sci Med Sci. 2007;62(4):427–33.
Vlassara H, Uribarri J. Advanced glycation end products (AGE) and diabetes: cause, effect, or both? Curr Diab Rep. 2014;14(1):453.
Vlassara H, Cai W, Crandall J, Goldberg T, Oberstein R, Dardaine V, et al. Inflammatory mediators are induced by dietary glycotoxins, a major risk factor for diabetic angiopathy. Proc Natl Acad Sci U S A. 2002;99(24):15596–601.
Uribarri J, Peppa M, Cai W, Goldberg T, Lu M, He C, et al. Restriction of dietary glycotoxins reduces excessive advanced glycation end products in renal failure patients. J Am Soc Nephrol. 2003;14(3):728–31.
Vlassara H, Cai W, Goodman S, Pyzik R, Yong A, Chen X, et al. Protection against loss of innate defenses in adulthood by low advanced glycation end products (AGE) intake: role of the antiinflammatory AGE receptor-1. J Clin Endocrinol Metab. 2009;94(11):4483–91.
Uribarri J, Cai W, Ramdas M, Goodman S, Pyzik R, Chen X, et al. Restriction of advanced glycation end products improves insulin resistance in human type 2 diabetes: potential role of AGER1 and SIRT1. Diabetes Care. 2011;34(7):1610–6.
Birlouez-Aragon I, Saavedra G, Tessier FJ, Galinier A, Ait-Ameur L, Lacoste F, et al. A diet based on high-heat-treated foods promotes risk factors for diabetes mellitus and cardiovascular diseases. Am J Clin Nutr. 2010;91(5):1220–6.
Luevano-Contreras C, Garay-Sevilla ME, Wrobel K, Malacara JM, Wrobel K. Dietary advanced glycation end products restriction diminishes inflammation markers and oxidative stress in patients with type 2 diabetes mellitus. J Clin Biochem Nutr. 2013;52(1):22–6.
Goldberg T, Cai W, Peppa M, Dardaine V, Baliga BS, Uribarri J, et al. Advanced glycoxidation end products in commonly consumed foods. J Am Diet Assoc. 2004;104(8):1287–91.
Uribarri J, Woodruff S, Goodman S, Cai W, Chen X, Pyzik R, et al. Advanced glycation end products in foods and a practical guide to their reduction in the diet. J Am Diet Assoc. 2010;110(6):911–16.e12.
Snelson M, Coughlan MT. Dietary advanced glycation end products: digestion, metabolism and modulation of gut microbial ecology. Nutrients. 2019;11(2)
Monden M, Koyama H, Otsuka Y, Morioka T, Mori K, Shoji T, et al. Receptor for advanced glycation end products regulates adipocyte hypertrophy and insulin sensitivity in mice: involvement of Toll-like receptor 2. Diabetes. 2013;62(2):478–89.
Cai W, Ramdas M, Zhu L, Chen X, Striker GE, Vlassara H. Oral advanced glycation endproducts (AGEs) promote insulin resistance and diabetes by depleting the antioxidant defenses AGE receptor-1 and sirtuin 1. Proc Natl Acad Sci U S A. 2012;109(39):15888–93.
He C, Sabol J, Mitsuhashi T, Vlassara H. Dietary glycotoxins: inhibition of reactive products by aminoguanidine facilitates renal clearance and reduces tissue sequestration. Diabetes. 1999;48(6):1308–15.
Vlassara H, Uribarri J, Cai W, Striker G. Advanced glycation end product homeostasis: exogenous oxidants and innate defenses. Ann N Y Acad Sci. 2008;1126:46–52.
Peppa M, Uribarri J, Cai W, Lu M, Vlassara H. Glycoxidation and inflammation in renal failure patients. Am J Kidney Dis. 2004;43(4):690–5.
Linden E, Cai W, He JC, Xue C, Li Z, Winston J, et al. Endothelial dysfunction in patients with chronic kidney disease results from advanced glycation end products (AGE)-mediated inhibition of endothelial nitric oxide synthase through RAGE activation. Clin J Am Soc Nephrol. 2008;3(3):691–8.
Fagugli RM, Vanholder R, De Smet R, Selvi A, Antolini F, Lameire N, et al. Advanced glycation end products: specific fluorescence changes of pentosidine-like compounds during short daily hemodialysis. Int J Artif Organs. 2001;24(5):256–62.
Gerdemann A, Wagner Z, Solf A, Bahner U, Heidland A, Vienken J, et al. Plasma levels of advanced glycation end products during haemodialysis, haemodiafiltration and haemofiltration: potential importance of dialysate quality. Nephrol Dial Transplant. 2002;17(6):1045–9.
Lin CL, Huang CC, Yu CC, Yang HY, Chuang FR, Yang CW. Reduction of advanced glycation end product levels by on-line hemodiafiltration in long-term hemodialysis patients. Am J Kidney Dis. 2003;42(3):524–31.
Friedlander MA, Wu YC, Schulak JA, Monnier VM, Hricik DE. Influence of dialysis modality on plasma and tissue concentrations of pentosidine in patients with end-stage renal disease. Am J Kidney Dis. 1995;25(3):445–51.
Vongsanim S, Fan S, Davenport A. Comparison of skin autofluorescence, a marker of tissue advanced glycation end-products in peritoneal dialysis patients using standard and biocompatible glucose containing peritoneal dialysates. Nephrology (Carlton). 2019;24(8):835–40.
Slowik-Zylka D, Safranow K, Dziedziejko V, Ciechanowski K, Chlubek D. Association of plasma pentosidine concentrations with renal function in kidney graft recipients. Clin Transpl. 2010;24(6):839–47.
Uribarri J, Tuttle KR. Advanced glycation end products and nephrotoxicity of high-protein diets. Clin J Am Soc Nephrol. 2006;1(6):1293–9.
Daroux M, Prevost G, Maillard-Lefebvre H, Gaxatte C, D’Agati VD, Schmidt AM, et al. Advanced glycation end-products: implications for diabetic and non-diabetic nephropathies. Diabetes Metab. 2010;36(1):1–10.
Zhou G, Li C, Cai L. Advanced glycation end-products induce connective tissue growth factor-mediated renal fibrosis predominantly through transforming growth factor beta-independent pathway. Am J Pathol. 2004;165(6):2033–43.
McLennan SV, Kelly DJ, Schache M, Waltham M, Dy V, Langham RG, et al. Advanced glycation end products decrease mesangial cell MMP-7: a role in matrix accumulation in diabetic nephropathy? Kidney Int. 2007;72(4):481–8.
Pala L, Cresci B, Manuelli C, Maggi E, Yamaguchi YF, Cappugi P, et al. Vascular endothelial growth factor receptor-2 and low affinity VEGF binding sites on human glomerular endothelial cells: biological effects and advanced glycosilation end products modulation. Microvasc Res. 2005;70(3):179–88.
Cerami C, Founds H, Nicholl I, Mitsuhashi T, Giordano D, Vanpatten S, et al. Tobacco smoke is a source of toxic reactive glycation products. Proc Natl Acad Sci U S A. 1997;94(25):13915–20.
Chuang PY, Yu Q, Fang W, Uribarri J, He JC. Advanced glycation endproducts induce podocyte apoptosis by activation of the FOXO4 transcription factor. Kidney Int. 2007;72(8):965–76.
Yang CW, Vlassara H, Peten EP, He CJ, Striker GE, Striker LJ. Advanced glycation end products up-regulate gene expression found in diabetic glomerular disease. Proc Natl Acad Sci U S A. 1994;91(20):9436–40.
Horie K, Miyata T, Maeda K, Miyata S, Sugiyama S, Sakai H, et al. Immunohistochemical colocalization of glycoxidation products and lipid peroxidation products in diabetic renal glomerular lesions. Implication for glycoxidative stress in the pathogenesis of diabetic nephropathy. J Clin Invest. 1997;100(12):2995–3004.
Yamamoto Y, Kato I, Doi T, Yonekura H, Ohashi S, Takeuchi M, et al. Development and prevention of advanced diabetic nephropathy in RAGE-overexpressing mice. J Clin Invest. 2001;108(2):261–8.
Wendt TM, Tanji N, Guo J, Kislinger TR, Qu W, Lu Y, et al. RAGE drives the development of glomerulosclerosis and implicates podocyte activation in the pathogenesis of diabetic nephropathy. Am J Pathol. 2003;162(4):1123–37.
Soulis T, Cooper ME, Sastra S, Thallas V, Panagiotopoulos S, Bjerrum OJ, et al. Relative contributions of advanced glycation and nitric oxide synthase inhibition to aminoguanidine-mediated renoprotection in diabetic rats. Diabetologia. 1997;40(10):1141–51.
Peppa M, Brem H, Cai W, Zhang JG, Basgen J, Li Z, et al. Prevention and reversal of diabetic nephropathy in db/db mice treated with alagebrium (ALT-711). Am J Nephrol. 2006;26(5):430–6.
Zheng F, He C, Cai W, Hattori M, Steffes M, Vlassara H. Prevention of diabetic nephropathy in mice by a diet low in glycoxidation products. Diabetes Metab Res Rev. 2002;18(3):224–37.
Normand G, Lemoine S, Villien M, Le Bars D, Merida I, Irace Z, et al. AGE content of a protein load is responsible for renal performances: a pilot study. Diabetes Care. 2018;41(6):1292–4.
Uribarri J, Stirban A, Sander D, Cai W, Negrean M, Buenting CE, et al. Single oral challenge by advanced glycation end products acutely impairs endothelial function in diabetic and nondiabetic subjects. Diabetes Care. 2007;30(10):2579–82.
Kakuta T, Tanaka R, Hyodo T, Suzuki H, Kanai G, Nagaoka M, et al. Effect of sevelamer and calcium-based phosphate binders on coronary artery calcification and accumulation of circulating advanced glycation end products in hemodialysis patients. Am J Kidney Dis. 2011;57(3):422–31.
Stirban A, Negrean M, Stratmann B, Gawlowski T, Horstmann T, Gotting C, et al. Benfotiamine prevents macro- and microvascular endothelial dysfunction and oxidative stress following a meal rich in advanced glycation end products in individuals with type 2 diabetes. Diabetes Care. 2006;29(9):2064–71.
Saulnier PJ, Wheelock KM, Howell S, Weil EJ, Tanamas SK, Knowler WC, et al. Advanced glycation end products predict loss of renal function and correlate with lesions of diabetic kidney disease in American Indians with type 2 diabetes. Diabetes. 2016;65(12):3744–53.
Semba RD, Ferrucci L, Fink JC, Sun K, Beck J, Dalal M, et al. Advanced glycation end products and their circulating receptors and level of kidney function in older community-dwelling women. Am J Kidney Dis. 2009;53(1):51–8.
Tezuka Y, Nakaya I, Nakayama K, Nakayama M, Yahata M, Soma J. Methylglyoxal as a prognostic factor in patients with chronic kidney disease. Nephrology (Carlton). 2019;24(9):943–50.
Rebholz CM, Astor BC, Grams ME, Halushka MK, Lazo M, Hoogeveen RC, et al. Association of plasma levels of soluble receptor for advanced glycation end products and risk of kidney disease: the Atherosclerosis Risk in Communities study. Nephrol Dial Transplant. 2015;30(1):77–83.
Uribarri J, Cai W, Pyzik R, Goodman S, Chen X, Zhu L, et al. Suppression of native defense mechanisms, SIRT1 and PPARgamma, by dietary glycoxidants precedes disease in adult humans; relevance to lifestyle-engendered chronic diseases. Amino Acids. 2014;46(2):301–9.
Lopez-Moreno J, Quintana-Navarro GM, Camargo A, Jimenez-Lucena R, Delgado-Lista J, Marin C, et al. Dietary fat quantity and quality modifies advanced glycation end products metabolism in patients with metabolic syndrome. Mol Nutr Food Res. 2017;61(8)
Vlassara H, Uribarri J, Cai WJ, Goodman S, Pyzik R, Post J, et al. Effects of sevelamer on HbA1c, inflammation, and advanced glycation end products in diabetic kidney disease. Clin J Am Soc Nephrol. 2012;7(6):934–42.
Yubero-Serrano EM, Woodward M, Poretsky L, Vlassara H, Striker GE, Group AG-lS. Effects of sevelamer carbonate on advanced glycation end products and antioxidant/pro-oxidant status in patients with diabetic kidney disease. Clin J Am Soc Nephrol. 2015;10(5):759–66.
Vlassara H, Cai W, Tripp E, Pyzik R, Yee K, Goldberg L, et al. Oral AGE restriction ameliorates insulin resistance in obese individuals with the metabolic syndrome: a randomised controlled trial. Diabetologia. 2016;59(10):2181–92.
Luevano-Contreras C, Gomez-Ojeda A, Macias-Cervantes MH, Garay-Sevilla ME. Dietary advanced glycation end products and cardiometabolic risk. Curr Diab Rep. 2017;17(8):63.
Kim Y, Keogh JB, Clifton PM. Effects of two different dietary patterns on inflammatory markers, advanced glycation end products and lipids in subjects without type 2 diabetes: a randomised crossover study. Nutrients. 2017;9(4)
Yacoub R, Nugent M, Cai W, Nadkarni GN, Chaves LD, Abyad S, et al. Advanced glycation end products dietary restriction effects on bacterial gut microbiota in peritoneal dialysis patients; a randomized open label controlled trial. PLoS One. 2017;12(9):e0184789.
Nagai R, Shirakawa J, Ohno R, Moroishi N, Nagai M. Inhibition of AGEs formation by natural products. Amino Acids. 2014;46(2):261–6.
Williams ME, Bolton WK, Khalifah RG, Degenhardt TP, Schotzinger RJ, McGill JB. Effects of pyridoxamine in combined phase 2 studies of patients with type 1 and type 2 diabetes and overt nephropathy. Am J Nephrol. 2007;27(6):605–14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Biruete, A., Uribarri, J. (2020). Advanced Glycation End Products. In: Burrowes, J., Kovesdy, C., Byham-Gray, L. (eds) Nutrition in Kidney Disease. Nutrition and Health. Humana, Cham. https://doi.org/10.1007/978-3-030-44858-5_29
Download citation
DOI: https://doi.org/10.1007/978-3-030-44858-5_29
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-44857-8
Online ISBN: 978-3-030-44858-5
eBook Packages: MedicineMedicine (R0)