Abstract
This chapter reviews the benefits of corticosteroids (CS) and hyaluronic acid (HA) injections for the treatment of patients with knee osteoarthritis, and describes the outcomes associated with these interventions. CS provide significant, clinically meaningful pain reduction compared with saline-solution placebo at week 12. However, intra-articular CS, especially continuous intra-articular CS, may be associated with an increased risk of knee radiographic osteoarthritis progression. The available evidence reported for the clinical studies assessed demonstrates sustained and effective relief of knee osteoarthritis symptoms following a single injection of HA. In addition, an excellent biocompatibility profile is observed for HA as an intra-articular therapy for osteoarthritis, as reflected by the low rate of adverse effects associated with treatment. The co-injection of HA and CS provides a rapid improvement in pain relief, knee function, and range of motion, but does not differ significantly from that of HA alone in the long-term effect.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
3.1 Introduction
Knee osteoarthritis has become a pandemic condition in developed countries. Increasing in aging of population, incidence of obesity, and sport practice are the main factors contributing to its huge increased in last decades. It has been estimated that knee osteoarthritis affects 38–47% of the population older than 60 years [1]. Therefore, health and economic impact are relevant. For example, it has been estimated that the economic burden of treating a patient with knee osteoarthritis is up to $5700/year, higher than cost of treatment of conditions like hypertension [2]. In addition, it is an important cause of disability and early retirement, which has socioeconomic implications [1]. There is no treatment able to stop osteoarthritis progression. Osteoarthritis treatment includes conservative measures and surgical treatment. Conservative treatment includes weight loss, physical therapy, patient education, and non-steroidal drugs. Intra-articular injections are an important part of conservative treatment as well. However there are different options [i.e., corticosteroids (CS), hyaluronic acid (HA), platelet rich plasma (PRP), ozone, etc.]. Therefore, it is important to know its differences and indications to use the best option at each moment. In this chapter, we will focus in CS and HA injections. Other intra-articular therapies will be discussed in other chapters.
3.2 Corticosteroids (CS)
CS constitute the widest used intra-articular therapy for osteoarthritis treatment and many other orthopedic conditions [3]. Synthetic corticosteroids for intra-articular use are derivatives of prednisolone, an analogue of human cortisol. They are more potent than native cortisol, present in natural form in human body. There are three main types of corticosteroids for intra-articular use derived of methylprednisolone: triamcinolone and betamethasone [1, 4]. These three, as all non-soluble forms, have a depot effect, with prolonged action when injected intra-articularly [5].
They are similar in potency and usually provide a safety profile, with an average duration between 1 and 8 weeks [6]. Caution should be taken when injection is performed in diabetic patients, as hyperglucemic spurts can occur. As triamcinolone is less water-soluble, it has been proposed as a less risky alternative for these patients [4].
3.2.1 Mechanism of Action
Both triamcinolone and betamethasone contain esters. These characteristics require hydrolysis by cellular esterases to release the active principle. This is an advantage over non-ester preparation, as it last its duration [1].
The anti-inflammatory and immunosuppressive effects of corticosteroids are well known, either intra-articular or systemic. Once the main principle is released intra-articularly, they alter B- and T-cell function. They act at the nuclear steroid receptors, inhibiting the inflammatory cascade. This leads to inhibition of phospholipase A2, its derivatives (like leukotrienes and prostaglandins) and other inflammatory cytokines (like matrix metalloprotease, neutrophil superoxide) [7], while reducing vascular permeability, accumulation of inflammatory cells, and phagocytosis. This effect creates a new non-oxidative environment, allowing to prevent cartilage degradation [5].
It has been described an increase of relative viscosity of synovial fluid due to a higher hyaluronic acid concentration derived of intra-articular injections of corticosteroids [7].
3.2.2 Administration and Clinical Effects
CS injections are usually administered with local anesthetics, like lidocaine, mepivacaine, or bupivacaine [1]. To use one or other combination depends on practitioner preferences. In our daily practice, we prefer mepivacaine, as its onset of action takes 5–10 min and in duration of effect lasts for 3–4 h. When we use it as a complement of surgical treatment [i.e., total knee arthroplasty (TKA) periarticular injection] we prefer, to use it in combination with a bupivacaine plus epinephrine combo, as the effect last more hours, while diminishing bleeding [8].
Two main concerns have been proposed about the use of corticosteroids in combination with local anesthetics. The first one is related to precipitation/crystallization of the corticosteroid. In a study leaded by Benzon et al., analyzing dilution with anesthetics of different forms of corticosteroids with confocal microscopy, they did not find differences in crystals size or aggregation [9]. The second one is intra-articular administration with anesthetics. Although it has been reported that intra-articular continuous infusion of local anesthestics may lead to chondrolysis in experimental environment [10], there is no clinical evidence of this situation [11]. However, there is some evidence about chondral injury in repeated injections, with a cartilage loss of 0.7–3% [12].
There are some factors affecting CS injection effects. It has been observed that patients with joint effusion and those with low to mild grade of osteoarthritis are more prone to have a beneficial effect of injection [13, 14]. Other conditions such as obesity, sedentarism, and chronic medical comorbidities are risk factors for a poor response to CS [5, 15].
3.2.3 Response to Therapy and Side Effects
Related to response to therapy, there is no evidence about if the presence of effusion, significant synovitis, or Kellgren-Lawrence grade is in relation to response [16]. There is no evidence of cartilage loosening at short-term follow-up as well [17]. Patients should be advised about the possibility of having flares few hours after injection and within the first 2–3 days. As with previously mentioned conditions, flares have no relation with response [1]. Other local soft tissue events like fat necrosis, skin depigmentation, or cutaneous atrophy are rare, but the patient should be advised before injection [4].
3.3 Hyaluronic Acid (HA)
HA has become the other main alternative of intra-articular therapy for knee osteoarthritis [18]. It is present naturally at the body, either in connective tissues and synovial joints. In synovial joints, it provides viscoelastic properties to synovial fluid.
It is an essential component of proteoglycans, helping to trap water intra-articularly. This is an important function, to provide resistance to the cartilage against compressive forces by increasing the amount of water of the cartilage matrix. It can be avian-derived or, more frequently, produced in vitro by bacterial fermentation. Avian-derived formulations have the disadvantage of increased inflammatory reactions [19].
3.3.1 Mechanism of Action
HA of synovial fluid of osteoarthritic knees is lower in quantity and weight than in non-arthritic joints [19]. One of the mechanisms proposed for HA action is to restore the mean median weight of HA present at the knee [20]. Higher molecular weight HA has been reported to provide a better profile of proteoglycan synthesis, joint lubrication, and viscoelasticity in comparison with low-weight formulations [19]. In addition to previously mentioned mechanisms, HA works at osteoarthritis through several interrelated ways: increase viscosity of articular fluid, decrease oxidative stress, and inhibit phagocytosis [1]. HA can reduce pain by inhibiting joint nociceptors by blocking to stretching-activated mechanoreceptors. This block seems to be more effective in case of high-weight HA [19].
3.3.2 Side Effects
HA do not exit the joint, so systemic effects are inexistent [1]. However, there are some adverse local reactions in 2–4% of patients [21]. These adverse reactions include flares, granulomatous inflammation, and a higher risk of infection in comparison with corticosteroids [22, 23]. However, other works show no differences regarding to side events in HA administration in comparison with placebo [24].
3.3.3 Clinical Effects
HA administration has demonstrated to be an useful alternative to improve pain, stiffness, and physical function [25, 26]. Although there is no chondro-regenerative effect once osteoarthritis has begun, HA injections are able to delay need for total knee arthroplasty for up to 2–7 years, even in Kellgren-Lawrence grade IV knees [27, 28]. This improvement in pain and function is accompanied by a beneficial effect at metabolism of the articular cartilage, increasing water and proteoglycans content [29]. For thus, although there is no evidence of being chondro-regenerative, it is admitted that HA is chondroprotective and delay osteoarthritis progression.
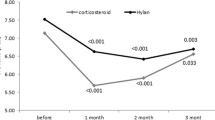
In fact, a Cochrane revision of 2006 comparing corticosteroids versus HA injections for knee osteoarthritis demonstrated that, although the effect of HA is lower to similar to corticosteroids in the first weeks, HA is more effective in pain relief after that period and effects remain more time in comparison with corticosteroids injections alone [30].
However, although evidence favoring HA effects is becoming higher, there are still some concerns about its use. There are authors that not see benefits of HA injections over corticosteroids. In fact, the American Academy of Orthopedic Surgeons (AAOS) guidelines for management of osteoarthritis of the knee do not recommend its use in symptomatic patients [31]. Fortunately, increasing evidence of beneficial effects of HA is becoming higher, and some discordant opinions have risen against AAOS guidelines in last years. In fact, adherence to AAOS guidelines is modest in real practice, demonstrating that intra-articular therapy is still highly variable [32, 33].
3.4 Authors’ Recommendations
We have seen along this chapter that evidence remains controversial in many aspects of intra-articular injections either with corticosteroids or hyaluronic acid. However, strong evidence is lacking for many therapies, and osteoarthritis of the knee is quiet frequent and probably will increase in the future. Although more studies are needed to evaluate intra-articular injections therapy, we would like to give some recommendations based on our daily practice. In our Department, all patients with osteoarthritis of the knee are encouraged to lose weight, strengthen quads, and do formal physical therapy. If it is not enough to control symptoms and osteoarthritis is diagnosed by X-rays, we start injection therapy in order to avoid or delay surgery as much as possible.
We initially indicate CS injections. We administer a combination of high-volume low-concentration of CS and anesthetics. Our preferred CS is bethametasone, as it is a non-soluble particle, with depot effect. We use it with mepivacaine 2% in a fulfilled 10 cm3 syringe. Our preference is to inject it directly intra-articular through the anterolateral arthroscopic portal. If there is any periarticular pain or swelling (typically pes anserinus tendonitis), we inject it as well with a small dose of the combination. We have observed that combined injection of intra-articular and pes anserinus is very effective in terms of pain relief and increasing function, especially with stairs. Intra-articular effusion should be drained as well if present. We usually try one injection and wait at least 2–3 months to observe the effect [34]. If pain relief has been incomplete, we repeat the CS injection. We recommend not to exceed three injections in a year.
If it has not been effective, we try HA injection. Regarding to HA injection, we prefer bacterial fermentation origin HA. We use a high-weight HA, as there is some evidence of being more effective than low-weight HA for the treatment of knee osteoarthritis. As we have commented before, we usually perform a corticosteroid injection before HA injection. Sometimes we combine it at the same time, in a totally empiric way that seems to be backed by recent literature [35].
3.5 Conclusions
We have observed that combination of HA plus CS can be useful to obtain a good early pain relief (CS effect is quicker than HA) while avoiding some of adverse early effects of HA (mainly pain and articular effusion). If HA has been effective, we repeat it twice a year. We try HA injection in all patients before affording the possibility of TKA. However, it is not well established which patient will be more benefitted of HA injection. We have observed, accordingly to the literature, that response is better and more frequent in low to mild osteoarthritis. However, some patients with severe osteoarthritis experiment improvement with HA, many of them delaying or even avoiding surgery for years.
References
Levy DM, Petersen KA, Scalley Vaught M, Christian DR, Cole BJ. Injections for knee osteoarthritis: corticosteroids, viscosupplementation, platelet-rich plasma, and autologous stem cells. Arthroscopy. 2018;34:1730–43.
Maetzel A, Li LC, Pencharz J, Tomlinson G, Bombardier C, Community Hypertension and Arthritis Project Study Team. The economic burden associated with osteoarthritis, rheumatoid arthritis, and hypertension: a comparative study. Ann Rheum Dis. 2004;63:395–401.
Vaquero-Picado A, Barco R, Antuña SA. Lateral epicondylitis of the elbow. EFORT Open Rev. 2016;1:391–7.
MacMahon PJ, Eustace SJ, Kavanagh EC. Injectable corticosteroid and local anesthetic preparations: a review for radiologists. Radiology. 2009;252:647–61.
Yaftali NA, Weber K. Corticosteroids and hyaluronic acid injections. Clin Sports Med. 2019;38:1–15.
Wright JM, Cowper JJ, Page Thomas DP, Knight CG. The hydrolysis of cortisol 21-esters by a homogenate of inflamed rabbit synovium and by rheumatoid synovial fluid. Clin Exp Rheumatol. 1983;1:137–41.
Chatham WW, Kimberly RP. Treatment of lupus with corticosteroids. Lupus. 2001;10:140–7.
Rodriguez-Merchan EC, Vaquero-Picado A, Ruiz-Perez JS. Opioid-free total knee arthroplasty? Local infiltration analgesia plus multimodal blood-loss prevention make it possible. HSS J Musculoskelet J Hosp Spec Surg. 2019;15:17–9.
Benzon HT, Chew T-L, McCarthy RJ, Benzon HA, Walega DR. Comparison of the particle sizes of different steroids and the effect of dilution: a review of the relative neurotoxicities of the steroids. Anesthesiology. 2007;106:331–8.
Gomoll AH, Kang RW, Williams JM, Bach BR, Cole BJ. Chondrolysis after continuous intra-articular bupivacaine infusion: An experimental model investigating chondrotoxicity in the rabbit shoulder. Arthroscopy. 2006;22:813–9.
Piper SL, Kramer JD, Kim HT, Feeley BT. Effects of local anesthetics on articular cartilage. Am J Sports Med. 2011;39:2245–53.
Raynauld J-P, Buckland-Wright C, Ward R, Choquette D, Haraoui B, Martel-Pelletier J, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2003;48:370–7.
Weitoft T, Uddenfeldt P. Importance of synovial fluid aspiration when injecting intra-articular corticosteroids. Ann Rheum Dis. 2000;59:233–5.
McAlindon TE, Harkey MS, Ward RF, Hochberg MC, Driban JB. Intra-articular corticosteroid injections in the hip and knee: perhaps not as dangerous as they want you to believe? Radiology. 2020;2020:200050.
Matzkin EG, Curry EJ, Kong Q, Rogers MJ, Henry M, Smith EL. Efficacy and treatment response of intra-articular corticosteroid injections in patients with symptomatic knee osteoarthritis. J Am Acad Orthop Surg. 2017;25:703–14.
Arden NK, Reading IC, Jordan KM, Thomas L, Platten H, Hassan A, et al. A randomised controlled trial of tidal irrigation vs corticosteroid injection in knee osteoarthritis: the KIVIS study. Osteoarthr Cartil. 2008;16:733–9.
Klocke R, Levasseur K, Kitas GD, Smith JP, Hirsch G. Cartilage turnover and intra-articular corticosteroid injections in knee osteoarthritis. Rheumatol Int. 2018;38:455–9.
Rodriguez-Merchan EC. Intra-articular injections of hyaluronic acid and other drugs in the knee joint. HSS J. 2013;9:180–2.
Watterson JR, Esdaile JM. Viscosupplementation: Therapeutic mechanisms and clinical potential in osteoarthritis of the knee. J Am Acad Orthop Surg. 2000;8:277–84.
Sun S-F, Hsu C-W, Sun H-P, Chou Y-J, Li H-J, Wang J-L. The effect of three weekly intra-articular injections of hyaluronate on pain, function, and balance in patients with unilateral ankle arthritis. J Bone Joint Surg Am. 2011;93:1720–6.
Adams ME, Lussier AJ, Peyron JG. A risk-benefit assessment of injections of hyaluronan and its derivatives in the treatment of osteoarthritis of the knee. Drug Saf. 2000;23:115–30.
Septic knee arthritis after intra-articular hyaluronate injection. Two case reports. n.d. https://www.ncbi.nlm.nih.gov/pubmed/?term=Albert+C%2C+Brocq+O%2C+Gerard+D%2C+Roux+C%2C+Euller-Ziegler+L.+Septic+knee+arthritis+after+intra-articular+hyaluronate+in-+jection.+Two+case+reports. Accessed February 28, 2020.
Ong KL, Runa M, Xiao Z, Ngai W, Lau E, Altman RD. Severe acute localized reactions following intra-articular hyaluronic acid injections in knee osteoarthritis. Cartilage. 2020;2020:1947603520905113.
Concoff A, Sancheti P, Niazi F, Shaw P, Rosen J. The efficacy of multiple versus single hyaluronic acid injections: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2017;18:542.
DeCaria JE, Montero-Odasso M, Wolfe D, Chesworth BM, Petrella RJ. The effect of intra-articular hyaluronic acid treatment on gait velocity in older knee osteoarthritis patients: a randomized, controlled study. Arch Gerontol Geriatr. 2012;55:310–5.
Rutjes AWS, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S. Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis. Ann Intern Med. 2012;157:180–91.
Waddell DD, Bricker DC. Total knee replacement delayed with Hylan G-F 20 use in patients with grade IV osteoarthritis. J Manag Care Pharm. 2007;13:113–21.
Waddell DD, Joseph B. Delayed total knee replacement with Hylan G-F 20. J Knee Surg. 2016;29:159–68.
Shah RP, Stambough JB, Fenty M, Mauck RL, Kelly JD, Reddy R, et al. T1rho magnetic resonance imaging at 3T detects knee cartilage changes after viscosupplementation. Orthopedics. 2015;38:e604–10.
Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;2:CD005328.
Jevsevar DS. Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg. 2013;21:571–6.
Meiyappan KP, Cote MP, Bozic KJ, Halawi MJ. Adherence to the American Academy of Orthopaedic Surgeons clinical practice guidelines for nonoperative management of knee osteoarthritis. J Arthroplast. 2020;35:347–52.
Carlson VR, Ong AC, Orozco FR, Hernandez VH, Lutz RW, Post ZD. Compliance with the AAOS guidelines for treatment of osteoarthritis of the knee: a survey of the American Association of Hip and Knee Surgeons. J Am Acad Orthop Surg. 2018;26:103–7.
Saltychev M, Mattie R, McCormick Z, Laimi K. The magnitude and duration of the effect of intra-articular corticosteroid injections on pain severity in knee osteoarthritis - a systematic review and meta-analysis. Am J Phys Med Rehabil 2020.
Smith C, Patel R, Vannabouathong C, Sales B, Rabinovich A, McCormack R, et al. Combined intra-articular injection of corticosteroid and hyaluronic acid reduces pain compared to hyaluronic acid alone in the treatment of knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2019;27:1974–83.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Vaquero-Picado, A., Rodríguez-Merchán, E.C. (2020). Intra-articular Injections of Corticosteroids and Hyaluronic Acid in Knee Osteoarthritis. In: Rodríguez-Merchán, E., Gómez-Cardero, P. (eds) Comprehensive Treatment of Knee Osteoarthritis. Springer, Cham. https://doi.org/10.1007/978-3-030-44492-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-44492-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-44491-4
Online ISBN: 978-3-030-44492-1
eBook Packages: MedicineMedicine (R0)