Abstract
In total knee arthroplasty (TKA), arterial system is injured during surgery and misdiagnosis of this complication can be catastrophic. Its estimated incidence is of 0.08–0.5%. They suppose one of the worst complications in a TKA, with catastrophizing consequences, including compartment syndrome and amputation. Although it is decreasing with new diagnostic and therapeutical techniques, it has been communicated a mortality rate of 7% and amputation of up to 41%. There are four main clinical syndromes related to arterial complications in TKA needing vascular surgeon implication: acute ischemia, hemorrhage, ischemia with hemorrhage, and pseudoaneurysm formation. The most common location for vascular injuries in the context of a TKA is the popliteal artery. It can be injured by traction or direct trauma with surgical instruments. Superficial femoral artery can be injured as well, but in this case by tourniquet application, causing a dissection of intimal flap. It is paramount to check the vascular status of the limb after tourniquet deflation. If we are not aware of the possibility of these complications, diagnosis can be delayed with catastrophic consequences. Arteriography remains as the gold standard to detect arterial injuries. Endovascular techniques are preferred over open techniques for the treatment of arterial injuries. These techniques include diagnostic techniques (i.e., arteriography), contention techniques (i.e., endovascular balloon for stopping distal hemorrhage), and revascularization techniques (i.e., endovascular prosthesis, stent, coils).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
12.1 Introduction
Total knee arthroplasty (TKA) has raised as one of the most clinically successful and cost-effective medical procedures in the last century [1, 2]. It is a more and more common procedure, with an expected increasing in next decades, parallel to population aging. In the same way, although complications are less and less frequent in relative terms, they will increase in number as well.
Vascular complications in TKA are mainly classified in two groups: those affecting the venous system (like thromboembolism) and those affecting the arterial vessels (i.e., arterial injuries).
Veins can be affected preoperatively, during surgery or after surgery. Preoperative varicose veins determine slow flow and blood retention, favoring deep thromboembolism. They can be injured on superficial dissection during surgery, but are more frequently affected immediately after surgery, developing blood stasis and deep vein thrombosis (DVT). In contrast, arterial system is injured during surgery and misdiagnosis of this complication can be catastrophic. DVT exceeds the objective of this chapter, so we will focus on arterial injuries.
12.2 Definition and Epidemiology
Arterial injuries are defined as intraoperative vascular injury requiring surgical repair, bypass grafting, or stenting [2]. They suppose one of the worst complications in a TKA, with catastrophizing consequences, including compartment syndrome and amputation. Although it is decreasing with new diagnostic and therapeutical techniques, it has been communicated a mortality rate of 7% and amputation of up to 41% [3].
Fortunately, they are very infrequent, with an estimated incidence of 0.08–0.5% of cases [4,5,6]. Although percentage of injuries may stay stable along the time, increasing number of total knee replacements may lead to an increased absolute number of arterial injuries. In case of revision surgery, it has been reported a risk of 2.4 in comparison with primary surgery [7].
Some previous patient conditions have been related with vascular complications. These include peripheral vascular disease, weight loss, renal failure, coagulopathy, and metastatic cancer [8, 9].
There are four main clinical syndromes related to arterial complications in TKA needing vascular surgeon implication: acute ischemia, hemorrhage, ischemia with hemorrhage, and pseudoaneurysm formation [10].
The most common location for vascular injuries in the context of a TKA is the popliteal artery [4]. It can be injured by traction or direct trauma with surgical instruments. Superficial femoral artery can be injured as well, but in this case by tourniquet application, causing a dissection of intimal flap [11].
12.2.1 Acute Ischemia
Acute ischemia is usually due to occlusion of a main vessel. This occlusion can be due to thrombosis, embolization, or dissection of the vessel.
Thrombosis is the result of the classical Virchow’s triad: slow flow, endothelial damage, and hypercoagulability. Low blood flow is a consequence of tourniquet application or varicose veins [7]. Endothelial damage can be produced by microtears, stretching of vessels during manipulation or thermal damage by cement. These conditions in combination with hypercoagulability context (dehydration, blood loss, genetic conditions, etc.) can produce acute ischemia.
Another mechanism of acute ischemia is release of parietal calcifications in proximal arterial vessels that can occlude the vessel distally (i.e., at the site of tourniquet application).
12.2.2 Ischemia and Hemorrhage
This type of injury can be due to a partial/complete disruption of the vessel.
12.2.3 Hemorrhage
Hemorrhage is due to direct vascular injury to the vessel wall, usually with Hohmann retractors on posterior tibial plateau or oscillating saw during posterior tibial and femoral cuts.
12.2.4 Pseudoaneurysm
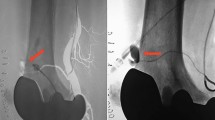
This type of injury is due to injury of the vessel’s wall, leading to a widen extravascular compartment where the blood is retained (Fig. 12.1). It usually requires delayed treatment, but with narrow surveillance, because pseudoaneurysm’s wall is very thin and can broke leading to a massive hemorrhage.
Six days after the implantation of a semi-constrained prosthesis (CCK, constrained condylar knee) due to severe preoperative deformity, a pseudoaneurysm was suspected. A computed tomography (CT) angiogram and a digital subtraction arteriography were performed, which demonstrated the existence of a pseudoaneurysm in a superior lateral geniculate artery. The arterial embolization which was carried out immediately afterwards using a helical microcoil (arrow) succeeded in occluding the pseudoaneurysm. Note the helical microcoil (arrow) which can be seen as a metallic spot above the knee prosthesis
12.3 Clinical Course
Diagnosis of vascular complications is usually clinical and special tests are utilized to confirm the diagnosis. There are five classical signs of ischemia (in this order of apparition): pain, pallor, pulseless, paresthesias, and paralysis.
In case of hemorrhage, hemarthrosis and bleeding through the surgical wound are the main symptoms. Localized edema, swelling, pulsatile mass, palpable thrill, or neurological compression are typical of arteriovenous fistula and pseudoaneurysms [7, 10, 12].
12.4 Diagnosis
If TKA is performed with tourniquet, all these conditions will be detected after tourniquet release. Classically, tourniquet release was after implantation and before wound closure, to detect any bleeding and practice surgical hemostasis. Actual blood saving protocols recommend to deflate the tourniquet after skin closure and wound bandage. This may difficult diagnosis in first minutes in comparison when the tourniquet is deflated before skin closure. In addition, most patients are operated under spinal anesthesia, so they will not complain of pain immediately. It is paramount to check the vascular status of the limb after tourniquet deflation. If we are not aware of the possibility of these complications, diagnosis can be delayed with catastrophic consequences. In fact, hemorrhage diagnosis can be delayed for hours until it becomes obvious [4, 12]. The best way to avoid misdiagnosis is periodical clinical checking after tourniquet release.
Once diagnosis has been suspected, several radiological tests can confirm the problem. Doppler is present in most surgical recovery units today. Absent of pulse in tibial or peroneal arteries should put us on the way of a possible ischemic injury. It can be useful to detect bleeding vessels and to check distal filling after reperfusion.
AngioCT is considered today the best test to detect any bleeding or stop in blood circulation in any part of the body. However, knee prosthesis can artifact radiological images and diagnosis can be sometimes difficult. Recent advantages in subtraction of implants image have increased sensitivity and specificity of this test.
Arteriography remains as the gold standard to detect vascular injuries. Although it has a sensitivity and specificity close to 100%, it is time-consuming and, at this moment, it is only indicated and performed by vascular surgeon or radiologist for addressing the injury intraoperatively.
12.5 Treatment
12.5.1 General Treatment
Endovascular techniques are preferred over open techniques for the treatment of vascular injuries. These techniques include diagnostic techniques (i.e., arteriography), contention techniques (i.e., endovascular balloon for stopping distal hemorrhage), and revascularization techniques (i.e., endovascular prosthesis, stent, coils).
Most frequent endovascular therapeutic techniques are: (1) thrombectomy with Fogarty catheter; (2) angioplasty with ballon and/or stent; (3) coil embolization (typically for pseudoaneurysms); (4) pharmacomechanical thrombolysis; (5) endoprosthesis [7, 10].
Endovascular addressing of vascular injuries proportionates a high rate of success, avoiding huge medial wound associated to open revascularization and its consequences (scarring, stiffness, infection, etc.) [12]. It also avoids contralateral saphenous harvest. Although open revascularization is a good option with similar rates of limb salvage in comparison with endovascular strategies, associated morbidity is quiet high in open procedures [5].
12.5.2 Acute Ischemia or Ischemia and Hemorrhage
Usually, ischemia is diagnosed sometime after tourniquet release. Once it is diagnosed, vascular surgeon (or radiologist) should be localized. Usually an arteriography is performed to detect the cause of ischemia (thrombosis, intimal flap, dissection, or transection) and adequate treatment is performed in consequence [7]. Endovascular treatment can be an option for most cases of thrombosis, intimal flap, dissection, or partial transection. They can be treated with endovascular prosthesis or stent. When endovascular treatment is unaffordable and in complete transection, open revascularization (direct repair or bypass) is indicated.
12.5.3 Hemorrhage
Hemorrhage should be managed initially with tourniquet inflation. If it is diagnosticated intraoperatively (less commonly with recent blood saving protocols), it can be packaged until further evaluation by the vascular surgeon [7]. It is the only injury that it is still better managed with open procedures.
12.5.4 Pseudoaneurysm
This entity is usually diagnosed and treated later (few days or weeks after index surgery). Endovascular techniques are of election for its treatment [7]. Endovascular prosthesis, coils, or stents are used to exclude the pseudoaneurysm of the circulation (Fig. 12.1).
12.6 Conclusion
Most frequent endovascular therapeutic techniques for treating arterial injuries in TKA are: Thrombectomy with Fogarty catheter; angioplasty with ballon and/or stent; coil embolization (typically for pseudoaneurysms); pharmacomechanical thrombolysis; and endoprosthesis. Endovascular addressing of arterial injuries proportionates a high rate of success, avoiding huge medial wound associated to open revascularization and its consequences (scarring, stiffness, infection, etc.). It also avoids contralateral saphenous harvest. Although open revascularization is a good option with similar rates of limb salvage in comparison with endovascular strategies, associated morbidity is quiet high in open procedures.
References
Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–21.
Healy WL, Della Valle CJ, Iorio R, Berend KR, Cushner FD, Dalury DF, et al. Complications of total knee arthroplasty: standardized list and definitions of the knee society. Clin Orthop. 2013;471:215–20.
Kumar SN, Chapman JA, Rawlins I. Vascular injuries in total knee arthroplasty. A review of the problem with special reference to the possible effects of the tourniquet. J Arthroplast. 1998;13:211–6.
Calligaro KD, Dougherty MJ, Ryan S, Booth RE. Acute arterial complications associated with total hip and knee arthroplasty. J Vasc Surg. 2003;38:1170–7.
Abularrage CJ, Weiswasser JM, Dezee KJ, Slidell MB, Henderson WG, Sidawy AN. Predictors of lower extremity arterial injury after total knee or total hip arthroplasty. J Vasc Surg. 2008;47:803–7.
Ko LJM, DeHart ML, Yoo JU, Huff TW. Popliteal artery injury associated with total knee arthroplasty: trends, costs and risk factors. J Arthroplast. 2014;29:1181–4.
Troutman DA, Dougherty MJ, Spivack AI, Calligaro KD. Updated strategies to treat acute arterial complications associated with total knee and hip arthroplasty. J Vasc Surg. 2013;58:1037–42.
Parvizi J, Pulido L, Slenker N, Macgibeny M, Purtill JJ, Rothman RH. Vascular injuries after total joint arthroplasty. J Arthroplast. 2008;23:1115–21.
Papadopoulos DV, Koulouvaris P, Lykissas MG, Giannoulis D, Georgios A, Mavrodontidis A. Popliteal artery damage during total knee arthroplasty. Arthroplasty Today. 2015;1:53–7.
Li Z, Xiang S, Bian Y-Y, Feng B, Zeng R, Weng X-S. Diagnosis and treatment of arterial occlusion after knee arthroplasty: the sooner, the better. Orthop Surg. 2019;11:366–72.
Daniels SP, Sneag DB, Berkowitz JL, Trost D, Endo Y. Pseudoaneurysm after total knee arthroplasty: imaging findings in 7 patients. Skelet Radiol. 2019;48:699–706.
Agarwala S, Menon A, Gupta M, Kulkarni A, Kapadia F, Padate B, et al. Multidimensional management of a vascular injury following total knee arthroplasty: a rare case report. J Clin Orthop Trauma. 2019;10:991–4.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Vaquero-Picado, A., Rodríguez-Merchán, E.C. (2020). Arterial Injuries in Total Knee Arthroplasty. In: Rodríguez-Merchán, E., Gómez-Cardero, P. (eds) Comprehensive Treatment of Knee Osteoarthritis. Springer, Cham. https://doi.org/10.1007/978-3-030-44492-1_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-44492-1_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-44491-4
Online ISBN: 978-3-030-44492-1
eBook Packages: MedicineMedicine (R0)