Abstract
Acute severe asthma induces marked alterations in respiratory mechanics, characterized by a critical limitation of expiratory flow and a heterogeneous and reversible increase in airway resistance, resulting in dynamic hyperinflation and high intrinsic PEEP. These abnormalities increase the work of breathing and can lead to life-threatening respiratory failure, in which case mechanical ventilation is life-saving.
Clinicians should keep in mind these very important pathological alterations in respiratory mechanics when caring for ventilated asthmatics. In particular, a major concern is the risk of worsening lung hyperinflation and inducing or aggravating hemodynamic instability.
We focus on the practical management of patients with acute severe asthma. Particular attention must be paid to ventilator settings, monitoring of lung hyperinflation, the role of extrinsic PEEP, and administering inhaled bronchodilators. Controlled hypoventilation with permissive hypercapnia may reduce morbidity and mortality compared to conventional normocapnic ventilation. We also underline the importance of deep sedation to maintain patient–ventilator synchrony. Finally, the role of noninvasive positive pressure ventilation for the treatment of respiratory failure during severe asthma is discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
Asthma is the most frequent cause of hospitalization among children [1]. The pathologic hallmarks of asthma are airway inflammation, excessive mucus production, mucus plugging, and airway bronchospasm. These changes together may lead to severe airflow obstruction, increased work of breathing, and acute respiratory failure (ARF).
Treatment is essentially based on the administration of inhaled beta-agonists and systemic corticosteroids. Initial treatment is sometimes provided in the primary care setting or even at home. However, children with moderate-to-severe exacerbations require close observation for clinical deterioration, frequent treatments, and repeated evaluation. Thus, most children with moderate or severe asthma exacerbations should be managed in an Emergency Department (ED) setting, and children who fail to improve with initial treatment should be admitted to the PICU. The use of noninvasive positive pressure ventilation (NPPV) may help avoid the need for intubation by reducing the work of breathing until maximal therapeutic effects of pharmacotherapy take place.
6.2 Pathophysiology
Asthma is a chronic inflammatory lung disease characterized by symptoms of cough, wheezing, dyspnea, and chest tightness that occur in paroxysms usually related to specific triggering events [2]. The symptoms of asthma are due to airflow obstruction, which results from the cumulative effects of smooth muscle constriction around airways, airway wall edema, intraluminal mucus accumulation, inflammatory cell infiltration of the submucosa, and basement membrane thickening [2]. Airway narrowing is partially or completely reversible. Airway narrowing results in airflow obstruction in the distal airways, which causes increased airway resistance and development of long expiratory time constants in lung units. This leads to the development of air trapping and dynamic hyperinflation (i.e., lung volume above functional residual capacity), also known as auto-PEEP or intrinsic PEEP (PEEPi). The development of PEEPi and dynamic hyperinflation necessitates a further increase in the work of breathing since a greater negative force must be generated for inspiration to begin in the context of air trapping. Moreover, expansion of lung volume decreases lung compliance, further increasing the elastic work of breathing.
6.2.1 Asthma Evaluation
Approximately 80% of children with asthma develop symptoms, namely wheezing, dyspnea, and cough, before the age of five. Most acute asthma exacerbations have a slow onset over several days. Uncommonly, severe attacks may occur suddenly and with minimal warning, resulting in life-threatening exacerbations.
Precipitating factors include viral upper respiratory infections, exercise, exposure to cigarette smoke, indoor and outdoor allergens, cold air, and hot and humid air.
A history of intermittent or chronic symptoms typical of asthma plus the finding on physical examination of characteristic wheezing (present in association with symptoms and absent when symptoms resolve) strongly points to a diagnosis of asthma. Confirmation of the diagnosis of asthma is based on three key additional elements:
-
the demonstration of variable expiratory airflow obstruction on spirometry
-
the documentation of reversible obstruction
-
the exclusion of alternative diagnoses (see Table 6.1)
Airflow obstruction on spirometry is defined as FEV1 reduced to less than 80% predicted and an FEV1/FVC ratio of less than 85%. FEV1/FVC appears to be a more sensitive measure of impairment, whereas FEV1 is a more useful measure of risk for future exacerbations.
Documentation of reversible obstruction is very important. Thus, spirometry should be performed before and after administration of a bronchodilator to assess for reversibility (bronchodilator response [BDR]). Significant reversibility is indicated by an increase in FEV1 of ≥12% from baseline after administration of a short-acting bronchodilator in adults and by an increase in FEV1 of ≥8% in children. BDR is important even in children with a normal baseline FEV1 because many of these children will still have a BDR. A trial of asthma medication is warranted in patients with symptoms suggestive of asthma who have normal or near-normal spirometry or who are unable to perform spirometry due to age (i.e., children younger than 5 years of age) or other factors. Response to asthma medications is sufficient to make the diagnosis in these patients.
Other causes of wheezing in children must be excluded (see Table 6.1). Certain diseases are most commonly present in infancy, while others are seen more often in older children. The most common cause of acute wheezing in children <2 years of age is viral bronchiolitis, usually due to infection with respiratory syncytial virus (RSV). Foreign body aspiration should be suspected in any toddler or preschooler who presents with wheezing of sudden onset, even in the absence of a clear history of a choking episode.
Performing bronchoprovocation testing with methacholine, cold air, or exercise is advised when the clinical features are suggestive of asthma, but spirometry is normal and there is no response to asthma medications. For safety reasons, these tests should be conducted in a specialized facility with trained technicians and should not be performed if a patient has severe airflow limitation (i.e., FEV1 <50% predicted).
Measurements of peak expiratory flow using a peak flow-meter are more variable and effort dependent than spirometry. In addition, there is wide variability in the published predicted peak expiratory flow reference values. Thus, peak flow measurements alone should not be used to diagnose asthma. Peak flow measurements may be more useful in monitoring a patient's symptoms and response to therapy over time, although serial spirometry is preferred.
6.2.2 Exacerbations Treatment
Inhaled short-acting beta-agonists (SABAs), like salbutamol, are the mainstay of management of acute asthma exacerbation [3, 4]. SABAs relax airway smooth muscle, leading to a prompt increase in airflow. These drugs generally provide rapid relief of acute asthma symptoms with a time to onset of action of approximately 5–10 min, peak effect beginning within approximately 50 min, and duration of action of approximately 3–6 h. Inhaled SABAs are typically administered by a metered dose inhaler (MDI) through a valved holding chamber or by nebulization. For children less than 4, in order to increase effectiveness, it is recommended to connect the spacer to a facial mask (see Fig. 6.1). Inhaled SABAs are preferred because they have a shorter onset of action and fewer side effects than oral agents. A dry powder inhaler (DPI) SABA is also available for children ≥4 years of age. However, acute exacerbation could reduce inspiratory flow enough in this age group to reduce drug delivery when using a DPI. Thus, DPI SABAs are used for prophylactic treatment prior to exercise but are not useful in the acute setting.
Ipratropium bromide is an anticholinergic drug that provides bronchodilation. It is used as an adjunct to SABAs in the management of moderate-to-severe acute asthma exacerbations [3, 4]. It is administered by an MDI or by nebulization. It begins to work within 15–30 min with a maximum effect seen within 1–2 h. Inhaled anticholinergics appear safe with no apparent significant side effects. However, if they are used on their own, inhaled anticholinergics are less effective than SABAs.
Systemic glucocorticoids are indicated for children with moderate-to-severe asthma exacerbations and are also used in children with mild exacerbations who do not respond to inhaled beta-agonist therapy alone [3, 4]. The anti-inflammatory action of glucocorticoids effectively reduces the airway edema and bronchial secretions. Systemic glucocorticoids have a delayed onset of action compared to bronchodilators with a minimum onset time of 2 h with oral preparations. The use of inhaled glucocorticoids to treat children with acute asthma is an area of ongoing clinical research. Until more conclusive data are available. Thus, the routine use of inhaled glucocorticoids in addition to, or instead of, systemic glucocorticoids in the management of acute asthma exacerbation in children is not suggested.
The recommended doses of medications to treat children with acute asthma exacerbation are reviewed in Table 6.2.
6.3 Emergency Department Management
The initial severity of the exacerbation and level of treatment needed (i.e., mild, moderate, or severe) can be determined using an asthma exacerbation severity score such as the Pulmonary Index Score (PIS) (see Table 6.3). The severity of asthma exacerbation is somewhat loosely defined based upon presenting signs and symptoms and response to therapy. For example, a PIS of ≥12 or a peak flow rate <40% of the predicted value for age, sex, and height or personal best identify a severe asthma exacerbation.
The immediate goals of treatment of an acute asthma exacerbation include rapid reversal of airflow obstruction and correction of severe hypercapnia or hypoxemia, if present. Inhaled SABAs are the mainstay of management of acute asthma exacerbations (see Table 6.2). Ipratropium bromide is added in case of moderate or severe exacerbations. Systemic glucocorticoids are administrated if the signs and symptoms of airway obstruction are moderate to severe or fail to improve after the first treatment with inhaled beta-agonists. Administration of supplemental oxygen is indicated if oxygen saturation is ≤92% in room air.
Children with mild or moderate asthma exacerbation who have marked improvement in clinical parameters during the first 1–2 h of therapy may be discharged home. All patients seen for an acute asthma exacerbation should have an inhaled SABA available for the treatment of symptoms after discharge from the ED. Patients are typically advised treating with a SABA every 4 h during waking hours and up to every 4 h during sleep for the first 3 days after discharge from the ED. Children are treated with a short course of oral glucocorticoids if they received a dose of systemic glucocorticoids in the ED. Patients discharged from the ED should follow-up with their primary care provider or asthma specialist within 1 week after the ED visit. On the other hand, patients who were severely ill on arrival and who have little improvement after initial therapy with beta-agonists and systemic glucocorticoids require hospitalization. This includes patients who continue to have significant wheezing and retracting, poor aeration, or altered mental status, such as drowsiness or agitation. Additional factors that suggest a need for hospitalization include:
-
beta-agonist therapy more often than 4 h
-
requirement for supplemental oxygen an hour or more after initial therapy
-
a history of rapid progression of severity in past exacerbations
-
poor adherence with outpatient medication regimen
-
recent treatment with systemic glucocorticoids (includes current treatment with oral glucocorticoids at the time of presentation) or beta-agonist overuse
-
inadequate access to medical care, including lack of transportation back to the hospital if deterioration occurs
-
poor social support system at home with inability of the caregiver(s) to provide medical care and supervision at home
-
a history of severe exacerbations, including a prior need for pediatric intensive care unit (PICU) management with or without invasive or noninvasive ventilation
6.4 Intensive Care Unit Management
Children with acute severe asthma patients who require beta-agonist therapy treatment more often than every 2–4 h or who fail to improve with initial treatment in the emergency department should be admitted to the PICU. These patients are at risk for progressive air trapping and alveolar hyperinflation, which may lead to alveolar rupture (e.g., pneumothorax) and hemodynamic instability.
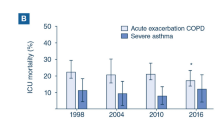
While overall mortality is low (i.e., 0.5%), patients with severe asthma who require mechanical ventilation have increased in-hospital mortality compared with patients who do not require mechanical ventilation. A mortality rate of 4% was found among children receiving mechanical ventilation [5]. In a separate study that reviewed asthma management in 1528 children who were treated in 11 PICUs, the mortality rate for ventilated asthmatic children was 2–3% [6].
ICU level management of these children entails the administration of glucocorticoids, aggressive bronchodilator therapy, and close monitoring.
These children are usually monitored with a cardiorespiratory monitor that displays a continuous electrocardiogram tracing, noninvasive blood pressure, oxygen saturation, and respiratory rate [7]. Additional monitoring includes frequent auscultation. Auscultation provides important information regarding aeration, optimal duration of exhalation (wheezing should terminate before the onset of the next inhalation), and the presence of pneumothorax or mucus plugging (indicated by asymmetric breath sounds) [7]. In addition to standard cardiorespiratory monitoring, mechanically ventilated patients may require arterial and central venous access for hemodynamic monitoring [8].
The fluid status must be carefully monitored. Many patients are hypovolemic on presentation due to poor intake of fluids and increased insensible fluid loss from the respiratory tract [7]. The risk of hypotension is furtherly increased in patients who are mechanically ventilated and who receive sedatives. Intravenous fluids should be administered to replace losses and optimize intravascular volume. However, overhydration should be avoided since it may result in pulmonary edema.
Mechanical ventilation is reserved for patients with continued progression toward respiratory failure despite maximal medical therapy. The decision to intubate should be made with great care since tracheal stimulation often worsens the asthma exacerbation and, in some cases, makes the situation worse. The best way to avoid intubation is to rapidly escalate the preintubation therapies, in particular in patients with a worsening trajectory indicated by increased work of breathing or CO2 retention.
In many patients who are progressing toward respiratory muscle fatigue, NPPV in conjunction with aggressive pharmacologic therapy can avoid the need for intubation by decreasing the work of breathing while awaiting the maximal therapeutic effects of pharmacotherapy.
6.4.1 Primary Preintubation Therapies in PICU
The goal of pharmacologic therapy for acute severe asthma exacerbations is to ensure adequate oxygenation and reduce bronchial obstruction with consequent mitigation of the work of breathing.
The primary preintubation therapies are supplemental oxygen, inhaled SABAs and anticholinergics, intravenous glucocorticoids (methylprednisolone 1–2 mg/kg per day with a maximum dose of 60 mg/day in children and 125 mg/day in adults) and systemic magnesium sulfate.
In the PICU setting, salbutamol should be delivered via nebulizer hourly or continuously (see Table 6.2) [9].
Evidence of benefit for inhaled ipratropium bromide has not been demonstrated in hospitalized patients and has not yet been specifically studied in the PICU population. However, one review found no serious adverse event associated with its use [10]. The dosing regimen can be extrapolated from the management of children with chronic lung disease (see Table 6.2).
Patients treated with magnesium sulfate (25–75 mg/kg intravenously with a maximum dose of 2 g over 20–30 min) should be monitored for hypotension [11].
For patients who fail to respond to inhaled bronchodilators, the transition to intravenous bronchodilators is suggested [12, 13]. Terbutaline is the intravenous bronchodilator most commonly used in the United States. On the contrary, intravenous salbutamol is not available in the United States. In countries where salbutamol is available, efficacy in patients with acute severe asthma has been demonstrated in randomized and observational studies [14, 15]. The dose is 0.5–5 μg/kg per minute. Beta2-agonist infusions may be associated with tachycardia, hypotension, hyperglycemia, hypokalemia, and arrhythmias. In general, the younger the age, the better the tachycardia is tolerated. SABAs have to be discontinued as soon as i.v. beta2-agonist therapy is started.
Subcutaneous or intramuscular epinephrine is an additional option if intravenous beta2-agonist is not available. Dosing for subcutaneous or intramuscular epinephrine is 0.01 mg/kg (0.01 mL/kg of 1:1000 solution [1 mg/mL]) every 20 min for up to three doses, maximum dose 0.5 mg.
Aminophylline is seldom used in PICUs for severe asthma exacerbations. It may be an option for the child with severe asthma exacerbations and impending respiratory failure who has not responded to intravenous salbutamol. Dosing of aminophylline is 6 mg/kg intravenous as loading dose, followed by continuous infusion. The starting infusion dose varies by patients age:
-
6 weeks to 6 months: 0.5 mg/kg/h
-
6–12 months: 0.6–0.7 mg/kg/h
-
1–9 years: 1 mg/kg/h
-
9–16 years: 0.8 mg/kg/h
Subsequently, the continuous infusion dosage is titrated on the plasma level. Therapeutic levels range between 10 and 20 μg/mL. Steady-state levels are checked 6–12 h following the bolus, then on a daily basis. If the patient's respiratory status does not improve and the 6-h theophylline level is below 15 μg/mL, the infusion is increased proportionately to a target level of 15 μg/mL. Toxicity develops with severe tachycardia, anxiety, persistent emesis, dysrhythmias, and seizures.
Clinical judgment dictates when patients should be weaned from intravenous bronchodilator therapy. Patients treated with intravenous salbutamol should have the medication reduced once clinical improvement is demonstrated and may be transitioned to continuous nebulized salbutamol with 1 h of overlapping therapy. Thereafter, they may be weaned to hourly nebulizer treatments as tolerated. If aminophylline is employed, it is generally continued until patients are consistently tolerating intermittent inhaled albuterol at a frequency of every 1–2 h.
There is sparse literature evaluating the use of high flow nasal cannula (HFNC) in children with severe asthma exacerbations. In a single-center retrospective study, investigators demonstrated the safety and feasibility of HFNC in these patients [16]. However, another study [17] suggests that HFNC in some subjects may delay NPPV support and potentially cause longer respiratory support, and longer PICU stay.
There are limited and conflicting data regarding the efficacy of Heliox (oxygen and helium mixture) in the treatment of children with acute severe asthma [18]. Oxygen and helium mixture increases laminar flow, as well as lowers viscosity, compared with nitrogen and oxygen mixture. Heliox is supplied in fixed gas mixtures 20% oxygen and 80% helium, so that additional oxygen should be blended and the oxygen concentration measured proximal to the patient. However, concentrations of oxygen more than 40% limit the beneficial effects of helium. Clinical improvement based upon PIS was reported in a small prospective study [19]. A subsequent review based only on small studies concluded that Heliox may have a role in the initial management of asthma in patients with more severe obstruction [20].
6.4.2 Noninvasive Positive Pressure Ventilation
NPPV involves the delivery of positive airway pressure through a noninvasive device, either as continuous pressure (continuous positive airway pressure, CPAP) or as mechanically assisted breaths (bilevel positive airway pressure [BiPAP]), without placement of an artificial airway.
NPPV may help to avoid endotracheal intubation in select patients who continue to have severe symptoms after intravenous bronchodilators or while awaiting the maximum therapeutic benefit of pharmacotherapy. NPPV may improve airflow obstruction in the distal airways by stenting open collapsing or narrowed airways, thereby allowing for more complete exhalation. Moreover, the application of expiratory positive airway pressure (EPAP) decreases the inspiratory effort necessary to begin inspiration. Additionally, inspiratory positive airway pressure (IPAP) further unloads the respiratory muscles [21].
NPPV has been used to treat children with respiratory failure from severe asthma exacerbations [21,22,23,24,25,26,27,28,29,30,31,32,33]. In several observational studies and case series, treatment with NPPV was associated with improved clinical parameters, decreasing respiratory rate, accessory muscle use, and dyspnea [26, 27, 29, 30, 33]. These results have been confirmed in a prospective study of 20 children (median age 4.8 years) admitted to the PICU with acute lower airway obstruction, randomly assigned to 2 h of NPPV followed by 2 h of standard therapy or to 2 h of standard therapy followed by 2 h of NPPV [28]. A reduction in PICU admissions when BiPAP was used in the pediatric emergency department setting was also reported [29]. Moreover, the safety, efficacy, and tolerability of BiPAP in children admitted to the PICU with severe asthma were evaluated in a randomized trial of standard therapy versus standard therapy plus NPPV for 24 h [32]. Rapid and significant improvements in clinical asthma scores were reported at each time point studied, although no significant differences between the two groups were seen for the other outcome measures. NPPV was well tolerated, and no major complications were reported [32]. Thus, evidence supporting the benefit of NPPV in children with acute severe asthma is accruing, although further trials are still needed [31].
As a matter of fact, the use of NPPV may be limited by several issues: (1) it requires patient cooperation, (2) it impairs ability to clear secretions from the respiratory tract, (3) it impairs ability to deliver medications to the respiratory tract, (4) it does not provide definitive control of the airway, (5) it may cause gastric distension with increased risk of aspiration, (6) it may cause heightened sense of air hunger upon initiation, and (7) patients may feel claustrophobic.
A trial of NPPV may be suggested in the following situations, provided that the child is alert, cooperative, and without increased airway secretions:
-
the child remains hypoxemic despite high flow oxygen and/or has documented hypercarbia;
-
the child is progressing toward respiratory muscle fatigue, but the maximum therapeutic effects of glucocorticoids and bronchodilators have not been reached.
In patients with moderately increased work of breathing or relatively mild–moderate degrees of hypoxemia or hypercarbia (PaCO2 of 45–50 mmHg) NPPV can begin as CPAP with a pressure of 5 cmH2O. However, in patients with significantly increased work of breathing and moderate or severe hypoxemia and/or hypercarbia (PaCO2 >50 mmHg). BiPAP provides a greater level of support and decreases more efficiently the work of breathing. The initial BiPAP settings should be relatively low and should be titrated to patient comfort, oxygenation, and ventilation. The inspiratory pressure may start at 8–10 cmH2O above the expiratory pressure and the expiratory pressure may be set at 5 cmH2O. These settings may be titrated up to an inspiratory pressure of 12–15 cmH2O above the expiratory pressure.
Bilevel positive airway pressure can be weaned to CPAP when the patient's work of breathing and respiratory rate is minimally elevated and the oxygen requirement is <50%. Subsequently, CPAP can be withdrawn when work of breathing and respiratory rate have normalized and the oxygen requirement is ≤40%.
Mild sedatives are sometimes used to facilitate the patient's tolerance of NPPV, but great care must be taken to avoid diminishing airway protective reflexes and respiratory drive [27].
6.4.3 The Decision to Intubate
Intubation should be approached cautiously in patients with severe asthma because manipulation of the airway can cause increased airflow obstruction due to exaggerated bronchial responsiveness. Thus, the clinician most experienced with airway management should perform the intubation preferably with a large-bore endotracheal tube to minimize airway resistance and enable suctioning. Clinicians must be prepared to manage acute deterioration due to pneumothorax and/or hypotension [34]. Mechanically, ventilated patients may require arterial and central venous access for hemodynamic monitoring, in addition to standard cardiorespiratory monitoring. Clinicians caring for children with acute severe asthma exacerbation who require mechanical ventilation may opt to give empiric fluid administration before intubation and sedation in anticipation of the hypotension that may be generated by sedative administration, dynamic hyperinflation, and the conversion to positive pressure ventilation. An extreme measure that can be taken if blood pressure fails to respond to volume resuscitation is to transiently disconnect the patient from the ventilator permitting complete evacuation of the lung and, in turn, appropriate venous return to the heart.
The decision to intubate a patient with severe asthma is made based upon clinical findings (e.g., inability to speak, confusion or somnolence, hypoxia despite supplemental oxygen or NPPV, moderate-to-severe hypercapnia). Care must be taken to control the airway before the patient suffers a respiratory arrest or a hypoxic insult.
Indications for intubation in patients with acute severe asthma include [35,36,37]:
-
Severe hypoxemia despite provision of high concentrations of oxygen or NPPV (PO2 <60 on >70% oxygen)
-
Severe and unremitting increased work of breathing (e.g., inability to speak)
-
Altered mental status
-
Respiratory or cardiac arrest
-
Hypercarbia alone is not an indication for intubation. However, intubation is warranted if a patient demonstrates a progressively rising arterial partial pressure of PaCO2 despite maximal medical therapy and/or NPPV and if hypercarbia causes significant respiratory acidosis or altered mental status.
6.4.4 Supportive Measures During Invasive Ventilation
Supportive measures for children with asthma who require invasive mechanical ventilation (IMV) include analgesia, sedation, and also muscle relaxation in more severe cases [38, 39]. The sedative agents that can be used for intubation include fentanyl, midazolam, ketamine, propofol, and etomidate. Morphine may generate histamine release and therefore is generally avoided. Additionally, neuromuscular blocking agents may be used to optimize intubating conditions. Once patients are intubated, sedation is also used to promote patient/ventilator synchrony and blunt tachypnea in order to reduce the risk of air trapping and barotrauma. Neuromuscular blockade may be employed as an adjunct to sedation to improve ventilator synynchrony [39].
Ketamine is often recommended as the induction agent of choice for the asthma patient requiring intubation (i.e., loading dose of 2 mg/kg is followed by an infusion of 20–60 μg/kg/min) because it has bronchodilatory as well as sedative effects [9, 27].
Propofol is a potent hypnotic/anesthetic agent that accomplishes global central nervous system depression via activation of gamma-aminobutyric acid (GABA) receptors, which is commonly used to facilitate intubation in patients with status asthmaticus [40]. Moreover, it is reported to have anti-inflammatory properties and to dilate central airways. Unfortunately, prolonged use of propofol (>48 h) is associated with propofol infusion syndrome that includes cardiac and renal failure, rhabdomyolysis, hepatomegaly, hyperkalemia, hypertriglyceridemia, and metabolic acidosis [41,42,43]. It occurs more commonly in children and in critically ill patients treated with glucocorticoids and catecholamines and is not recommended for continuous sedation in the PICU by the US Food and Drug Administration (FDA) [44, 45]. Nonetheless, there are numerous studies that have demonstrated the safe use of propofol for sedation in over 500 PICU patients, suggesting that propofol can be at doses <4 mg/kg/h for under 48 h in this population [46,47,48].
Fentanyl and midazolam in combination are commonly used in the PICU setting to accomplish sedation [49].
Dexmedetomidine, a selective alpha2-receptor agonist, is approved for use in the adult population and there are multiple reports of its safety and efficacy in the pediatric population [50]. Dosing is largely extrapolated from the adult literature. Patients are typically loaded with 0.5–1 μg/kg over 10–20 min, but some pediatric centers reduce or eliminate the loading dose in an effort to avoid hypotension and bradycardia. The infusion dose ranges from 0.2 to 0.7 μg/kg/h. However, the pediatric literature suggests that infusions can be safely given beyond the recommended limit of 24 h and at doses as high as 2 μg/kg/h. In addition to sedation for the ventilated patient, dexmedetomidine is also used to facilitate tolerance of NPPV [51].
Neuromuscular blockade may be employed as an adjunct to sedation in patients mechanically ventilated [39]. However, efforts should be made to discontinue the use of neuromuscular blocking agents as soon as feasible since their use in combination with glucocorticoids is associated with an increased risk of myopathy of critical illness [6, 52, 53].
6.4.5 Invasive Mechanical Ventilation
In children with severe asthma, the goals of IMV are [54]:
-
to relieve work of breathing and allow respiratory muscle rest
-
to ensure adequate oxygenation and adequate alveolar ventilation, considering that initial hypercarbia is tolerated until airway obstruction is reversed
-
to avoid or minimize dynamic hyperinflation and PEEPi, preventing barotrauma and hypotension.
The increase in dynamic hyperinflation, which can occur during IMV, can lead to very high intrapulmonary pressures with the risk of barotrauma. Barotrauma occurs when the alveolar pressure increases to a degree that disrupts the structural integrity of the alveolus leading to interstitial emphysema, pneumothorax, pneumoperitoneum, and subcutaneous emphysema [55]. Other clinical manifestations of pulmonary barotrauma include subpleural air cysts, bronchopleural fistula, tension lung cysts, and systemic gas embolism [56]. Dynamic hyperinflation may also compromise cardiac function by increasing pulmonary vascular resistance and impeding venous return to the heart. Successful mechanical ventilation in patients with asthma depends upon limiting the risk of hyperinflation and barotrauma.
The risk of hyperinflation is reduced by decreasing the minute volume and permitting adequate time for complete exhalation before the next inhalation begins. Reducing respiratory rate and inspiratory time increases the expiratory time, thereby decreasing the ratio of inspiratory to expiratory time (I:E ratio) [39]. To diminish the risk of hyperinflation and barotrauma, an initial PaCO2 higher than normal should be tolerated (i.e., permissive hypercapnia) [57,58,59,60]. Permissive hypercarbia is well tolerated by most children. A slow increase in PaCO2 allows the rise of serum bicarbonate level that balances serum pH [61]. However, those with concurrent chronic conditions, such as cyanotic heart disease, cardiomyopathy, or pulmonary hypertension, will probably not tolerate this strategy. Other potential contraindications to permissive hypercapnic ventilation include increased intracranial pressure, poor myocardial function, and coexistent metabolic acidosis (e.g., patients with renal disease).
After intubation, a deep sedation is usually maintained. Muscle relaxation may be employed as an adjunct to sedation. The ventilator is set in time-cycled modes, avoiding patient triggering. There is no evidence to support one mode of ventilation over another [8, 39]. In pressure-controlled ventilation, a peak pressure is ensured without, however, assuring the Vt in case of an increased airway resistance (e.g., in the event of bronchospasm or mucus plugging) and/or a reduction in the thoracic-pulmonary compliance (e.g., in the case of dynamic hyperinflation or pneumothorax). In volume-controlled ventilation, the Vt is always ensured without limiting the airways pressure in case of an increased airway resistance or a thoraco-pulmonary compliance reduction. On the other hand, pressure-controlled modes that guarantee a target Vt, such as the pressure-regulated volume control (PRVC), assures that the patient receives the target Vt at the lowest peak pressure [61].
Mechanical ventilators in volume-controlled mode display the peak pressure (Ppeak), which is the highest airway pressure measured during each respiratory cycle and reflects the sum of resistive pressure of airways plus elastic pressure of lungs plus total positive end-expiratory pressure (PEEPtot). The plateau pressure (Pplat) is measured at end-inspiration and represents the pressure in the small airways and alveoli after flow has ceased (see Fig. 6.2). To obtain a numeric value for intrinsic PEEP, the extrinsic PEEP is subtracted from airway pressure measured during a breath-hold at end-expiration. The difference between Ppeak and Pplat provides information about airway resistance and bronchodilatatory therapy efficacy [39]. Pressure-controlled ventilation does not allow the measurement of Ppeak.
Measurement of the end-inspiratory plateau pressure. Recordings of airway pressure and flow in a patient receiving controlled mechanical ventilation. The measurement of plateau pressure (Pplat) is obtained if airways are occluded at end-inspiration using the end-inspiratory hold function on the ventilator. An inspiratory hold (0.5–1 s) is applied at end-inspiration. During the period of zero flow, pressures in the alveoli and ventilator circuit equilibrate and the airway pressure displayed by the ventilator drops from the peak pressure to the plateau pressure
The tidal volume (TV) delivered should initially be 6–8 mL/kg [61]. The Ppeak and Pplat attained with these volumes should be noted and kept under 40 cmH2O and 30 cmH2O, respectively. Maintaining these limits helps to minimize dynamic hyperinflation and barotrauma [61]. The TV may need to be reduced if the plateau pressure limit exceeds 30 cm H2O [39]. Reducing the TV and RR, keeping the minute ventilation under 115 mL/kg per minute, may result in increased PaCO2.
In order to increase the expiratory time and prevent air trapping, it is paramount to obtain an I:E ratio between 1:3 and 1:5 [62]. Thus, respiratory rate (RR) and inspiratory time should be set slightly below physiologic values (see Table 6.4) [57]. For example, an RR between 8 and 12 per minute and Ti between 0.75 and 1 s should be set in patients older than 12 years.
Adequate oxygenation is usually achieved without difficulty in most patients with asthma since the airways, not the alveoli, are the primary targets of inflammation and bronchospasm. However, mucus plugging, atelectasis, hyperinflation, and ventilation/perfusion (V/Q) mismatch may contribute to hypoxemia. The fraction of inspired oxygen (FiO2) should be set at 1.0 upon intubation. FiO2 is then decreased as tolerated to concentrations of 0.5 or lower to maintain oxygen saturation >92% [61]. Use of an FiO2 of 1.0 for prolonged periods in patients with asthma predisposes them to resorption atelectasis and should therefore be avoided.
Atelectasis that results from mucus plugging can usually be treated with judicious application of extrinsic PEEP (e.g., 3–5 cmH2O), as well as regular removal of secretions from the endotracheal tube [63].
Mechanical ventilation in severe asthma patients should require qualitative and quantitative monitoring of dynamic hyperinflation. The flow/time curve allows a relatively easy assessment of air trapping (see Fig. 6.3). PEEPi should be measured to quantify the extent of dynamic hyperinflation (see Fig. 6.4) [64]. In adult patients, it is recommended to keep a Pplat less than 30 cmH2O and a PEEPi less than 10 cmH2O to minimize the risk of complications due to dynamic hyperinflation [61]. Whether these measures are valid in children is unknown.
Flow time curve suggesting the presence of dynamic hyperinflation. Recordings of flow time curve in a patient receiving mechanical ventilation. Arrow A shows expiratory flow returning to 0 before the next breath begins. This condition suggests the absence of dynamic hyperinflation. Arrow B shows expiratory flow not returning to 0 before the next breath begins. This condition suggests the presence of dynamic hyperinflation
Measurement of intrinsic PEEP. Recordings of airway pressure (Paw), flow, and volume in a patient receiving controlled mechanical ventilation. After the third breath, the airway was occluded at end-expiration using the end-expiratory hold function on the ventilator. During the period of zero flow, pressures in the alveoli and ventilator circuit equilibrate and the plateau pressure reflects intrinsic PEEP
6.4.6 Adjunctive Therapies
In extreme cases, airflow obstruction is so severe that sufficient ventilation cannot be achieved despite intensive bronchodilator therapy, intravenous glucocorticoids, ventilatory support, sedation, and paralysis. In such cases, adjunctive therapies, such as inhalational anesthetics or extracorporeal membrane oxygenation (ECMO), may be successful as rescue measures. However, the routine use of these therapies cannot be recommended on the basis of existing clinical studies. They remain heroic rescue maneuvers for the extremely refractory patient.
The inhalational anesthetics, halothane, isoflurane, and sevoflurane, are potent bronchodilators. The positive effects of isoflurane for status asthmaticus have been described in a few case series [65,66,67,68]. Their mechanism of action is unknown, but it probably includes direct smooth muscle relaxation, reduction of vagal tone, and synergy with catecholamines. However, the use of alogenates could be difficult in many PICUs. In fact, the ventilator used to deliver these agents must have a scavenger system to prevent staff exposure to anesthetic agents. Then, not all pediatric intensivists are anesthesiologists and some of them could lack familiarity with anesthesia machines and inhalational anesthetics [65,66,67,68]. Furthermore, another limitation to the use of inhalational anesthetics includes the abrupt return of bronchoconstriction after discontinuation of the drug. That is why the majority of PICUs never use volatile agents [69].
6.5 Weaning from Mechanical Ventilation
Positive response to therapy is indicated by [61]:
-
decreased wheezing in the expiratory phase of respiration
-
improvement of arterial blood gas measurements (i.e., PaO2, PaCO2, and pH) and decreased FiO2 necessary to maintain a valid PaO2
-
decrease in the amount of peak inspiratory pressure necessary to deliver the desired Vt.
In these conditions, the patient could be put in spontaneous modes that allow the patient to determine the RR, the inspiratory and expiratory times, and partially the Vt (summation effect of negative pleural pressure generated by the patient and positive pressure delivered by the ventilator). Moreover, spontaneous modes permit to lighten the sedation and to facilitate a gradual weaning from ventilatory support (i.e., reducing gradually the inspiratory pressure) [6]. For this purpose, pressure ventilation modes are always used and Pressure Support Ventilation (PSV) is the most frequently used mode. It is particularly important to adjust inspiratory trigger at a very sensitive level, which means that the ventilator should be set at the maximum sensitivity of the trigger that does not determine auto-triggering. The expiratory trigger should be set to allow a Te long enough to enable the lungs to empty. PEEP should be set to a value of about 5 cmH2O to facilitate activation of inspiratory mechanical assistance. The extrinsic PEEP can offset the adverse effects of PEEPi, because it reduces the effort necessary to trigger inspiration during patient-initiated breaths. Thus, the amount of PEEPi must be measured accurately to avoid administering excess extrinsic PEEP and exacerbating air-trapping. However, airflow obstruction is inhomogeneous, so levels of PEEPi are likely to vary from airway to airway. Thus, as a general rule, extrinsic PEEP is usually set up to, but not exceeding, 80% of the measured PEEPi in order to prevent regions of worsening dynamic hyperinflation [39, 61, 70, 71]. Thus, before shifting to PSV and decreasing the sedation, the amount of PEEPi should be measured accurately (see Fig. 6.4).
A trial of extubation can be performed when the patient is comfortably achieving a normal or near-normal PaCO2 with minimal pressures settings (e.g., external PEEP and pressure support of 5 cmH2O each) and a peripheral oxygen saturation (SpO2) more than 95% with a FiO2 of 0.4 or less. Once the patient demonstrates readiness for extubation, sedation should be held and he should be extubated when he demonstrates appropriate strength and wakefulness. Following extubation, patients should be observed in the ICU for at least 24 h to monitor for respiratory embarrassment, including tachypnea, dyspnea, increased work of breathing, hypoxia, and atelectasis.
6.5.1 Criteria for Discharge from the PICU
Criteria for transitioning patients from the pediatric PICU to the general pediatric ward undoubtedly vary among institutions and are largely a matter of clinical judgment. However, several general criteria are useful to consider when making this decision, including:
-
successful weaning from invasive or noninvasive positive pressure ventilation
-
successful cessation of intravenous bronchodilators
-
requirement of aerosolized bronchodilators at a frequency that can be safely delivered on the general pediatric ward
-
oxygen requirement within the range of what can be safely and locally appropriate to deliver on the general pediatric ward
-
minimal increased work of breathing.
Patients who have required an ICU admission for an asthma exacerbation are at risk for having another life-threatening or fatal asthma exacerbation. Thus, they should be closely followed by an asthma specialist in the outpatient setting.
References
Mannino DM, Homa DM, Akinbami LJ, et al. Surveillance for asthma—United States, 1980–1999. MMWR Surveill Summ. 2002;51:1.
British Thoracic Society Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. Thorax. 2008;63(Suppl 4):iv1.
Lougheed MD, Lemiere C, Ducharme FM, et al. Canadian Thoracic Society 2012 guideline update: diagnosis and management of asthma in preschoolers, children and adults. Can Respir J. 2012;19:127.
The Global Initiative for Asthma (GINA). Resources include Pocket Guide for Asthma Management and Prevention, and GINA report, Global strategy for asthma management and prevention. www.ginasthma.org. Accessed 13 Jul 2015.
Rampa S, Allareddy V, Asad R, et al. Outcomes of invasive mechanical ventilation in children and adolescents hospitalized due to status asthmaticus in United States: a population based study. J Asthma. 2015;52:423.
Roberts JS, Bratton SL, Brogan TV. Acute severe asthma: differences in therapies and outcomes among pediatric intensive care units. Crit Care Med. 2002;30:581.
Quinonez RA, Garber MD, Schroeder AR, et al. Choosing wisely in pediatric hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8:479.
Kneyber MCJ, de Luca D, Calderini E, Jarreau PH, Javouhey E, Lopez-Herce J, Hammer J, Macrae D, Markhorst DG, Medina A, Pons-Odena M, Racca F, Wolf G, Biban P, Brierley J, Rimensberger PC, and on behalf of the section Respiratory Failure of the European Society for Paediatric and Neonatal Intensive Care (2017). Recommendations for mechanical ventilation of critically ill children from the Paediatric Mechanical Ventilation Consensus Conference (PEMVECC). Intensive Care Med. 2017;43:1764–80.
Nievas IF, Anand KJ. Severe acute asthma exacerbation in children: a stepwise approach for escalating therapy in a pediatric intensive care unit. J Pediatr Pharmacol Ther. 2013;18:88.
Vézina K, Chauhan BF, Ducharme FM. Inhaled anticholinergics and short-acting beta(2)-agonists versus short-acting beta2-agonists alone for children with acute asthma in hospital. Cochrane Database Syst Rev. 2014;7:CD010283.
From the Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA). 2014. http://www.ginasthma.org/. Accessed 7 Nov 2014.
Stephanopoulos DE, Monge R, Schell KH, et al. Continuous intravenous terbutaline for pediatric status asthmaticus. Crit Care Med. 1998;26:1744.
Wheeler DS, Jacobs BR, Kenreigh CA, et al. Theophylline versus terbutaline in treating critically ill children with status asthmaticus: a prospective, randomized, controlled trial. Pediatr Crit Care Med. 2005;6:142.
Browne GJ, Penna AS, Phung X, Soo M. Randomised trial of intravenous salbutamol in early management of acute severe asthma in children. Lancet. 1997;349:301.
Bohn D, Kalloghlian A, Jenkins J, et al. Intravenous salbutamol in the treatment of status asthmaticus in children. Crit Care Med. 1984;12:892.
Baudin F, Buisson A, Vanel B, Massenavette B, Pouyau R, Javouhey E. Nasal high flow in management of children with status asthmaticus: a retrospective observational study. Ann Intensive Care. 2017;7(1):55.
Pilar J, Modesto I, Alapont V, Lopez-Fernandez YM, Lopez-Macias O, Garcia-Urabayen D, Amores-Hernandez I. High-flow nasal cannula therapy versus non-invasive ventilation in children with severe acute asthma exacerbation: an observational cohort study. Med Intensiva. 2017;41(7):418.
Carroll CL. Heliox for children with acute asthma: has the sun set on this therapy? Pediatr Crit Care Med. 2010;11:428.
Kim IK, Phrampus E, Venkataraman S, et al. Helium/oxygen-driven albuterol nebulization in the treatment of children with moderate to severe asthma exacerbations: a randomized, controlled trial. Pediatrics. 2005;116:1127.
Rodrigo GJ, Castro-Rodriguez JA. Heliox-driven β2-agonists nebulization for children and adults with acute asthma: a systematic review with meta-analysis. Ann Allergy Asthma Immunol. 2014;112:29.
Najaf-Zadeh A, Leclerc F. Noninvasive positive pressure ventilation for acute respiratory failure in children: a concise review. Ann Intensive Care. 2011;1:15.
Fortenberry JD, Del Toro J, Jefferson LS, et al. Management of pediatric acute hypoxemic respiratory insufficiency with bilevel positive pressure (BiPAP) nasal mask ventilation. Chest. 1995;108:1059.
Padman R, Lawless ST, Kettrick RG. Noninvasive ventilation via bilevel positive airway pressure support in pediatric practice. Crit Care Med. 1998;26:169.
Bernet V, Hug MI, Frey B. Predictive factors for the success of noninvasive mask ventilation in infants and children with acute respiratory failure. Pediatr Crit Care Med. 2005;6:660.
Essouri S, Chevret L, Durand P, et al. Noninvasive positive pressure ventilation: five years of experience in a pediatric intensive care unit. Pediatr Crit Care Med. 2006;7:329.
Carroll CL, Schramm CM. Noninvasive positive pressure ventilation for the treatment of status asthmaticus in children. Ann Allergy Asthma Immunol. 2006;96:454.
Akingbola OA, Simakajornboon N, Hadley EF Jr, Hopkins RL. Noninvasive positive-pressure ventilation in pediatric status asthmaticus. Pediatr Crit Care Med. 2002;3:181.
Thill PJ, McGuire JK, Baden HP, et al. Noninvasive positive-pressure ventilation in children with lower airway obstruction. Pediatr Crit Care Med. 2004;5:337.
Beers SL, Abramo TJ, Bracken A, Wiebe RA. Bilevel positive airway pressure in the treatment of status asthmaticus in pediatrics. Am J Emerg Med. 2007;25:6.
Mayordomo-Colunga J, Medina A, Rey C, et al. Non-invasive ventilation in pediatric status asthmaticus: a prospective observational study. Pediatr Pulmonol. 2011;46:949.
Korang SK, Feinberg J, Wetterslev J, Jakobsen JC. Non-invasive positive pressure ventilation for acute asthma in children. Cochrane Database Syst Rev. 2016;9:CD012067.
Basnet S, Mander G, Andoh J, et al. Safety, efficacy, and tolerability of early initiation of noninvasive positive pressure ventilation in pediatric patients admitted with status asthmaticus: a pilot study. Pediatr Crit Care Med. 2012;13:393.
Needleman J, Sykes J, Schroeder S, Singer L. Noninvasive positive pressure ventilation in the treatment of pediatric status asthmaticus. Pediatr Asthma Allergy Immunol. 2004;17:272.
American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 10. 5 Near-fatal asthma. Circulation. 2005;112(Suppl 24):139.
Newth CJ, Meert KL, Clark AE, et al. Fatal and near-fatal asthma in children: the critical care perspective. J Pediatr. 2012;161:214.
Bratton SL, Odetola FO, McCollegan J, et al. Regional variation in ICU care for pediatric patients with asthma. J Pediatr. 2005;147:355.
Carroll CL, Smith SR, Collins MS, et al. Endotracheal intubation and pediatric status asthmaticus: site of original care affects treatment. Pediatr Crit Care Med. 2007;8:91.
Wetzel RC. Pressure-support ventilation in children with severe asthma. Crit Care Med. 1996;24:1603.
Rotta AT. Asthma. In: Fuhrman BP, Zimmerman JJ, editors. Pediatric critical care. 3rd ed. Philadelphia: Mosby; 2006. p. 589.
Marik PE. Propofol: therapeutic indications and side-effects. Curr Pharm Des. 2004;10:3639.
Burburan SM, Xisto DG, Rocco PR. Anaesthetic management in asthma. Minerva Anestesiol. 2007;73:357.
Wong JM. Propofol infusion syndrome. Am J Ther. 2010;17:487.
Vasile B, Rasulo F, Candiani A, Latronico N. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med. 2003;29:1417.
Hauser GJ, Bell KG. Prolonged propofol infusions in critically ill children: are we ready for a large controlled study?∗. Pediatr Crit Care Med. 2014;15:176.
Chidambaran V, Costandi A, D’Mello A. Propofol: a review of its role in pediatric anesthesia and sedation. CNS Drugs. 2015;29:543.
Koriyama H, Duff JP, Guerra GG, et al. Is propofol a friend or a foe of the pediatric intensivist? Description of propofol use in a PICU. Pediatr Crit Care Med. 2014;e66:15.
Cornfield DN, Tegtmeyer K, Nelson MD, et al. Continuous propofol infusion in 142 critically ill children. Pediatrics. 2002;110:1177.
Svensson ML, Lindberg L. The use of propofol sedation in a paediatric intensive care unit. Nurs Crit Care. 2012;17:198.
Nett S, Emeriaud G, Jarvis JD, et al. Site-level variance for adverse tracheal intubation-associated events across 15 North American PICUs: a report from the national emergency airway registry for children. Pediatr Crit Care Med. 2014;15:306.
Buck ML. Dexmedetomidine use in pediatric intensive care and procedural sedation. J Pediatr Pharmacol Ther. 2010;15:17.
Takasaki Y, Kido T, Semba K. Dexmedetomidine facilitates induction of noninvasive positive pressure ventilation for acute respiratory failure in patients with severe asthma. J Anesth. 2009;23:147.
Douglass JA, Tuxen DV, Horne M, et al. Myopathy in severe asthma. Am Rev Respir Dis. 1992;146:517.
Barohn RJ, Jackson CE, Rogers SJ, et al. Prolonged paralysis due to nondepolarizing neuromuscular blocking agents and corticosteroids. Muscle Nerve. 1994;17:647.
Bohn D, Kissoon N. Acute asthma. Pediatr Crit Care Med. 2001;2:151.
Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144:1447.
Morris WP, Butler BD, Tonnesen AS, Allen SJ. Continuous venous air embolism in patients receiving positive end-expiratory pressure. Am Rev Respir Dis. 1993;147:1034.
Cox RG, Barker GA, Bohn DJ. Efficacy, results, and complications of mechanical ventilation in children with status asthmaticus. Pediatr Pulmonol. 1991;11:120.
Picado C, Montserrat JM, Roca J, et al. Mechanical ventilation in severe exacerbation of asthma. Study of 26 cases with six deaths. Eur J Respir Dis. 1983;64:102.
Bellomo R, McLaughlin P, Tai E, Parkin G. Asthma requiring mechanical ventilation. A low morbidity approach. Chest. 1994;105:891.
DeNicola LK, Monem GF, Gayle MO, Kissoon N. Treatment of critical status asthmaticus in children. Pediatr Clin North Am. 1994;41:1293.
Schwarz AJ, Lubinsky PS. Acute severe asthma. In: Levin DL, Morriss FC, editors. Essentials of pediatric intensive care. 2nd ed. New York: Churchill Livingstone; 1997. p. 130.
Venkataraman ST. Mechanical ventilation and respiratory care. In: Fuhrman BP, Zimmerman JJ, editors. Pediatric critical care. Philadelphia: Mosby; 2006. p. 692.
Maxwell GM. The problem of mucus plugging in children with asthma. J Asthma. 1985;22:131.
Papiris S, Kotanidou A, Malagari K, Roussos C. Clinical review: severe asthma. Crit Care. 2002;6:30.
Shankar V, Churchwell KB, Deshpande JK. Isoflurane therapy for severe refractory status asthmaticus in children. Intensive Care Med. 2006;32:927.
Koninckx M, Buysse C, de Hoog M. Management of status asthmaticus in children. Paediatr Respir Rev. 2013;14:78.
Mikkelsen ME, Woo YJ, Sager JS, et al. Outcomes using extracorporeal life support for adult respiratory failure due to status asthmaticus. ASAIO J. 2009;55:47.
Carroll CL. Just a lot of hot air? Volatile anesthetics in children with status asthmaticus. Pediatr Crit Care Med. 2013;14:433.
Char DS, Ibsen LM, Ramamoorthy C, Bratton SL. Volatile anesthetic rescue therapy in children with acute asthma: innovative but costly or just costly? Pediatr Crit Care Med. 2013;14:343.
Marini JJ. Should PEEP be used in airflow obstruction? Am Rev Respir Dis. 1989;140:1.
Stewart TE, Slutsky AS. Occult, occult auto-PEEP in status asthmaticus. Crit Care Med. 1996;24:379.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Racca, F., Montagnini, L. (2020). Acute Asthma Exacerbations in Children: From Emergency Room to Intensive Care Unit Management. In: Chiumello, D. (eds) Practical Trends in Anesthesia and Intensive Care 2019. Springer, Cham. https://doi.org/10.1007/978-3-030-43873-9_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-43873-9_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43872-2
Online ISBN: 978-3-030-43873-9
eBook Packages: MedicineMedicine (R0)