Abstract
After many decades of antibiotic therapy, resistance has emerged as one of the most important determinants of outcome in patients with serious infections. More than 700,000 healthcare-associated infections, many caused by antibiotic-resistant bacteria, occur annually in the US with almost half in critically ill patients. This review will address the burden of MDR infections in the ICU.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Infections
- Intensive Care Unit
- Complications
- Drug resistance, Multiple, Bacterial
- Prevention and control
- Antibacterial agents
2.1 Infections and Resistance: The Problem Dimension
After many decades of antibiotic therapy, resistance has emerged as one of the most important determinants of outcome in patients with serious infections. More than 700,000 healthcare-associated infections, many caused by antibiotic-resistant bacteria, occur annually in the US with almost half in critically ill patients [1]. Infections due to antibiotic-resistant microorganisms accounted for an estimated 33,110 attributable deaths and 874,541 disability-adjusted life years (DALYs) in Europe in 2015 [2]. The drug-resistance phenomenon already imposes a very heavy burden on healthcare with regard to mortality and health-care costs with infections caused by Gram-negative organisms often more prevalent than Gram-positive infections in many settings [3]. Moreover, some further studies prognosticate worrying trends, with an expected rising impact on global health through years, leading to more than ten million annual deaths worldwide in 2050 [3]. A majority of these deaths are, and will be, related to Gram-negative infections, particularly healthcare-acquired infections caused by extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant (MDR) Acinetobacter baumannii, and Pseudomonas aeruginosa. In Europe, the prevalence of Klebsiella pneumoniae carbapenemase (KPC)-producing Enterobacteriaceae is extremely high in some countries like Greece and Italy, and strains producing carbapenem-hydrolyzing oxacillinase-48 (OXA-48) and New Delhi metallo-betalactamase (NDM) are rapidly increasing [2]. The incidence of infections due to resistant Gram-negative pathogens has dramatically increased in the nosocomial setting [1,2,3,4,5]. In particular, Intensive Care Units (ICU) are often considered the epicenter of development, amplification, and dissemination of drug-resistant microorganisms [6]. Critically ill patients are particularly prone to infections because of exposure to multiple invasive procedures compromising the anatomical barriers’ defenses, impairment of protective mechanisms such as cough reflex or acid gastric ambient by sedative drugs or stress-ulcer prophylaxis and the frequent impairment of the immune response induced by trauma, surgery, and sepsis. Furthermore, the use of broad-spectrum antibiotics, that is closely related to the development and spread of drug-resistant microorganisms, is really frequent in ICU clinical practice, with studies reporting a 30–60% rate of inappropriate or incorrect antibiotic prescriptions. For these reasons, nosocomial infections caused by MDR microorganisms are common in ICUs, frequently even more than in other departments [1, 3].
A number of studies have been performed to assess the burden of infection in critical illness. The Intensive Care Over Nations (ICON) audit showed that more than one-third of the patients develop an infection during their ICU stay [7]. The Extended Prevalence of Infection in Intensive Care (EPIC) II study showed that 51% of patients were considered to be infected while in ICU. The infection was of respiratory origin in 64% of cases. Staphylococcus aureus (20.5%) was the most frequent organism isolated, despite the overall predominance of Gram-negative organisms as a group: 62.2% (E. coli, Enterobacter spp., Klebsiella spp., Pseudomonas spp., and Acinetobacter) [8]. Antibiotic resistance is a serious problem in all parts of the world, including Asia-Pacific, Latin America, Middle East, Europe, and North America. In Europe, the European Antimicrobial Resistance Surveillance Network (EARS-Net) has provided European reference data on antimicrobial resistance for public health purposes since the program began in 1999. Over the last years, the proportion of K. pneumoniae and E. coli with resistance to fluoroquinolones, third-generation cephalosporins, aminoglycosides, and a combined resistance to all three antibiotic groups has increased significantly [9].
The recent “European Antimicrobial Resistance One Health ministerial conference 2016” highlighted the substantial antimicrobial resistance problem in Europe and for several antimicrobial group–bacterium combinations [10]. In general, lower resistance percentages are reported by countries in the north and higher percentages by countries in the south and east of Europe [10].
2.2 Infections and Resistance: Definitions
A group of international experts, brought together by a joint initiative between the European Centre for Disease Control and Prevention (ECDC) and the United States Centre for Disease Control and Prevention (CDC), was tasked with creating a standardized international terminology to describe acquired resistance profiles in multidrug-resistant organisms [11]. MDROs have been divided into three categories depending on their resistance profile: 1. MDROs—nonsusceptible to at least 1 agent in 3 antimicrobial categories; 2. extensively drug-resistant (XDR) organisms—nonsusceptible to at least 1 agent in all but 2 or fewer antimicrobial categories; and 3. pan-drug-resistant (PDR) organisms—nonsusceptible to all agents in all antimicrobial categories. Moreover, a new, comprehensive recommendation on classification of infections caused by Gram-positive and emerging Gram-negative multidrug-resistant pathogens has been launched in 2012 in the consideration that E. faecium, S. aureus, K. pneumoniae, A. baumannii, P. aeruginosa, and Enterobacter spp. (ESKAPE) pathogens account for more than 80% of infectious episodes in the ICU. As this acronym seems to help to highlight the problem of MDR bacteria, some authors [12] claimed a change to “ESCAPE” is warranted (E. faecium, S. aureus, C. difficile, A. baumannii, P. aeruginosa, and Enterobacteriaceae) in order to highlight the importance of C. difficile and incorporate not only Enterobacter spp. but also other Enterobacteriaceae (or more modernly and widely Enterobacterales) because of the increasing levels of antibiotic resistance (including extended-spectrum β-lactamases, carbapenemases, and aminoglycoside resistance) and decreasing levels of fluoroquinolone susceptibility among these organisms.
2.3 MDR Gram Positive
MDR Gram-positive are major human pathogens, causing both healthcare- and community-associated infections. Among them, methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus faecium (VRE), and drug-resistant Streptococcus pneumoniae have been designated as serious public threats by the CDC [13]. Indeed, MRSA and VRE are leading causes of healthcare-associated infections in the United States, with conservative estimates suggesting they cause >12,000 deaths per year. Similarly, infections due to drug-resistant S. pneumoniae, the main cause of bacterial pneumonia and meningitis in adults, are estimated to cause 19,000 excess admissions and 7000 deaths per year in the United States alone [13].
Infections due to MRSA accounted for an estimated 148,727 infections and 7049 deaths in Europe in 2015 [2].
Methicillin resistance is due to a modified penicillin-binding protein (PBP2a), which is not inhibited by any beta-lactam. MRSA phenotype is the most relevant from the clinical and the epidemiological points of view among staphylococci. In fact, MRSA infections have higher mortality and cause higher costs for the health system compared to methicillin-susceptible S. aureus (MSSA) [14]. MRSA is spread worldwide and prevalence is high in many countries, including Italy where it stands at about 40% [15].
Enterococci have a low virulence and are part of the intestinal flora but can provoke urinary tract infection (UTI), bacteremia, and endocarditis in vulnerable and immunocompromised patients; less frequently they are responsible, usually as copathogens, of intra-abdominal infections and surgical wound infections. Naturally resistant to cephalosporins, they can acquire genetic elements conferring resistance to penicillins, aminoglycosides, and glycopeptides (vancomycin-resistant enterococci, VRE). The European surveillance system EARS-Net indicates that the EU/EEA population-weighted mean percentage of resistance to vancomycin in E. faecium among European countries increased from 10.4% in 2014 to 14.9% in 2017 [9]. Risk factors for VRE infection include diabetes, renal failure, cancer, prolonged hospital stay, proximity to a colonized or infected patient, previous treatment with broad-spectrum antibiotics (particularly vancomycin and cephalosporins). Treatment of Clostridium difficile infection with metronidazole or oral vancomycin has also been reported to increase the risk of acquiring VRE [16]. Finally, it should be reminded that patients colonized by VRE have a higher risk of bacteremia in case they are exposed to vancomycin, are immunocompromised, have relevant comorbidities, live in long-term care facilities, or have a VRE infection in another site [17].
2.3.1 MRSA
Options for treating MRSA infections include the old drugs (vancomycin, teicoplanin, linezolid, daptomycin) and several new agents: the lipoglycopepetide dalbavancin and oritavancin, the new oxazolidinone tedizolid, the advanced-generation cephalosporins (ceftaroline and ceftobiprole), and the fluoroquinolone delafloxacin.
The most recent guidelines for the treatment of MRSA infections are those released by the Infectious Diseases Society of America (IDSA) in 2011 [18]. According to the guidelines, vancomycin, linezolid, and daptomycin have all the highest level of evidence and recommendation for the treatment of skin and SSTIs, only daptomycin is rated AI for the treatment of bacteremia and endocarditis on native valve, while linezolid is rated II for MRSA pneumonia (as vancomycin), but the results of the Zephyr study have not been considered. According to the latter, mortality at the end of the study was significantly lower with linezolid among patients with MRSA nosocomial pneumonia [19]. For bone and joint infections, all the three drugs are rated BII. In case MRSA is isolated and susceptibility pattern is available, the treatment should be based on vancomycin MIC. In case of MIC <1 mg/L, vancomycin is a valid option, in case of MIC ≥1 mg/L, daptomycin should be preferred in case of bacteremia or endocarditis and linezolid in case of pneumonia, central nervous system (CNS) infection or endophthalmitis. Empirical treatment should be based on the conditions of the patient, comorbidity, site of infection, and local epidemiology of resistance. In particular, MRSA etiology should be considered in presence of known colonization or previous MRSA infection or two or more of the following: previous stay in hospital or long-term care facility, previous antibiotic treatment, chronic renal failure in dialysis, age >60 years. If MRSA is unlikely, a beta-lactam should be preferred; otherwise an anti-MRSA drug should be selected according to local epidemiology of vancomycin MICs and site of infection. In case of severe sepsis or septic shock with renal impairment, the association of linezolid and daptomycin is an option, since vancomycin is slowly bactericidal and potentially nephrotoxic.
2.3.2 Potential Role for the New Antibiotics
Ceftaroline and ceftobiprole have anti-MRSA activity in addition to the spectrum of third-generation cephalosporins and might be useful in the treatment of pneumonia. Particularly, ceftobiprole is licensed for hospital-acquired pneumonia (excluding ventilator-associated cases). In fact, ceftobiprole has an anti-Pseudomonas activity close to that of ceftazidime, and in a randomized double-blind study, it showed cure rates comparable to those of ceftazidime plus linezolid in patients with HAP (excluding VAP) [20]. They share with the other cephalosporins a good safety profile, better than other anti-MRSA drugs.
Dalbavancin’s main peculiarity is the very long half-life allowing an intravenous administration every week or even 2 weeks. It’s licensed for complicated SSTIs and its good penetration in the bone suggests a role in the management of osteomyelitis [21]. Therefore, its potential use in the setting of ICUs seems to be very limited.
Tedizolid, licensed for SSTIs, has a good penetration in the epithelial lining fluid and has a potential role in the management of pneumonia. It seems to have a better safety profile compared to linezolid, particularly concerning bone marrow suppression [22]. Since such toxicity is more frequent after 10–14 days of treatment, which is generally considered an adequate duration of treatment for pneumonia, the cheaper linezolid is likely to remain the preferred option in the majority of cases; however, tedizolid might be appealing in patients that already have a significant reduction of blood cells.
Delafloxacin is a new fluoroquinolone with enhanced activity against Gram-positive bacteria. Licensed for SSTIs, it’s being tested for pneumonia. Due to its peculiar chemical structure and mechanism of action with multiple bacterial targets, it’s thought to be less prone to the selection of resistance [23].
2.3.3 VRE
Aminopenicillins are preferred over all other agents when enterococci are susceptible and patients can tolerate them. In case of endocarditis on native or prosthetic valve, an aminoglycoside or ceftriaxone should be added. Daptomycin and linezolid have demonstrated clinical efficacy against VREs. In case of UTI of the upper urinary tract or associated with bacteremia, daptomycin or linezolid is recommended. Quinupristin/Dalfopristin (Q/D) is reserved for selected cases of infection due to Enterococcus faecium resistant to vancomycin. In case of bacteremia or endocarditis due to vancomycin- and ampicillin-resistant strains, daptomycin and linezolid are preferable to Q/D, and none of the two has been demonstrated to be more effective in retrospective studies. Some authors suggest higher than standard doses of daptomycin, e.g., 10–12 mg/kg, should be considered in severe bloodstream infections due to VRE, to obtain a bactericidal effect; another possible strategy to enhance efficacy of daptomycin and prevent selection of resistance seems to be the combination with a beta-lactam, such as ampicillin, ceftriaxone, and, probably better, ceftaroline [24]. In case VRE strains are not highly resistant to aminoglycosides, these can be associated with daptomycin, linezolid, or Q/D, while in case of strains highly resistant to aminoglycoside (HLR), tigecycline, doxycyclyne, or rifampin can be an alternative as partner drug. In selected cases, daptomycin can represent an alternative to aminoglycosides for its rapid bactericidal activity, and the association with linezolid can be an option [25, 26]. Synergistic combinations are often warranted in complex infections of high inoculum and biofilms, while monotherapies are generally appropriate for uncomplicated infections. Although active against resistant enterococci, the pharmacokinetics, efficacy, and safety of tigecycline and quinupristin/dalfopristin can be problematical for severe infections. Recently, approved agents such as tedizolid and oritavancin have good in vitro activity against VRE, but clinical studies are lacking [27].
2.4 MDR Gram Negative
Evidence suggests that the prevalence of MDR Gram-negative bacteria is increasing worldwide [1,2,3,4]. Numerous risk factors can increase the likelihood of infection with resistant organisms, including: (1) prior antimicrobial therapy, especially with a broad-spectrum agent, in the preceding 90 days; (2) current hospitalization for 5 days; (3) a high prevalence of resistant organisms in a hospital environment; (4) immunosuppressive therapy; and (5) specific risk factors such as hospitalization for 2 days in the preceding 90 days, residence in a nursing home or long-term care facility, chronic dialysis within the preceding 30 days, home wound care or intravenous infusion therapy, and a family member with a resistant pathogen.
2.4.1 ESBL-Producing Enterobacteriaceae
Resistance to third-generation cephalosporins among Enterobacteriaceae is generally mediated by the production of extended-spectrum beta-lactamase (ESBL). Therapeutic options are limited by the typically multiresistant phenotype of ESBL-producing Enterobacteriaceae and conditioned by the site and the severity of the infection. A timely and appropriate treatment is essential to reduce the mortality of these infections. Carbapenems represent the first choice in case of severe infections: meropenem 1–2 g IV tid and imipenem 1 g IV tid, in extended or continuous infusion after a loading dose. Ertapenem 1 g IV qd is a valid alternative because it has no activity against Pseudomonas spp and Acinetobacter spp, and therefore it does not apply selective pressure on nonfermenting Gram-negative bacteria and because it can be administered once daily [28]. However, data on clinical efficacy are more limited compared to imipenem and meropenem, and it is advisable to adopt it in case of not severe infections. Doripenem 500 mg IV tid in extended infusion has similar characteristics to meropenem and could represent an alternative, but data about its use against ESBL-producing bacteria are still scarce.
Piperacillin/tazobactam 4.5 g IV tid or qid in extended or continuous infusion is a valid option when the microorganism is reported to be susceptible. The association with an aminoglycoside, if active, could offer an advantage. The extended infusion in 4 h, after a loading dose in 30 min, seems to guarantee a better pharmacodynamic profile against microorganisms with a MIC up to 16 mg/L [29]. However, recent results from a randomized clinical trial suggest that treatment with meropenem is associated with lower mortality compared to piperacillin/tazobactam, in patients with bacteremia due to ceftriaxone-resistant K.pneumoniae [30].
Ceftolozane/tazobactam, the combination of a new cephalosporine with an old beta-lactamase inhibitor, has been licensed for intra-abdominal and urinary tract infections and, more recently, pneumonia (HAP and VAP). This drug showed in vitro activity comparable to that of meropenem against E.coli and slightly inferior (but still superior to that of piperacillin/tazobactam and cephalosporins) against K.pneumoniae [31]. A wider use of this drug might be considered to spare carbapenems that have a high impact on the selection of resistant strains, such as carbapenemase-producing Gram-negative bacteria.
Tigecycline’s spectrum of activity includes Gram-negative producing ESBL and carbapenemase. It’s bacteriostatic, it does not reach adequate serum levels, but concentrates in the sites of infection, though not in the CNS and the urine. The slightly higher mortality among patients treated with tigecycline compared to those treated with other agents (difference of 1%) [32] suggests to limit the use of tigecycline to the registered indications (intra-abdominal infections, skin and soft-tissue infections), and in case it’s used against multiresistant Gram-negative bacteria, the association with other agents, such as colistin, fosfomycin, and carbapenems, as well as higher doses, such as 100 or 200 mg bid in large volumes to prevent nausea and vomit [33, 34], are advisable.
Intravenous fosfomycin, at a dose of 12–24 g per day, may be an option in nonsevere infections, particularly in the setting of urinary tract infections, preferably in association with other agents, such as an aminoglycoside.
2.4.2 AmpC-Producing Enterobacteriaceae
Ampicillinase C (AmpC) production is another mechanism of resistance to cephalosporins used by Enterobacteriaceae. This enzyme is naturally present in Enterobacter cloacae, and aerogenes, Citrobacter freundii, and Serratia marcescens and it’s spreading through plasmids to other bacteria, such as E. coli, K. pneumoniae, Salmonella enterica, and Proteus mirabilis. Differently by ESBL, AmpC is less active against fourth-generation cephalosporins such as cefepime, which is often active against AmpC-producers, but are not inhibited, or much less, by beta-lactamase inhibitors, namely, clavulanic acid, sulbactam, and tazobactam. The efficacy of fourth-generation cephalosporins on AmpC-producers, however, can be impaired in case of severe infections with high bacterial mass, due to inoculum effect. In case of severe infection, therefore, a carbapenem is preferable [35].
2.4.2.1 Carbapenem-Resistant Gram Negative
The increased use of carbapenems due to the spread of ESBL applied a selective pressure that induced an increase in carbapenem-resistance among nonfermenting Gram-negative, such as P. aeruginosa and A. baumannii, and more recently among Enterobacteriaceae. The main concern is at the moment the spread of carbapenem-resistance in K. pneumoniae [2, 9]. Most common carbapenemase types include KPC (K. pneumoniae carbapenemase), more common among K. pneumoniae and less frequently detected in other Enterobacteriaceae and P. aeruginosa, OXA (oxacillinase), more common in A. baumannii and also found in Klebsiella spp and MBL (metallo-beta-lactamase), found in Enterobacteriaceae and nonfermenting Gram-negative [36]. Among these, KPC showed the capability of spreading very fast and it currently represents one of the main therapeutic challenges.
2.4.3 XDR P. aeruginosa
XDR P. aeruginosa is resistant to carbapenems, all beta-lactams, fluoroquinolones, and often aminoglycosides. These strains are colistin-only susceptible (COS). Colistin is an old molecule necessarily rescued, although the experience about its use in clinical practice is quite scarce and out of date. It is usually used at the dose of two to three million units IV tid, possibly after a loading dose of nine million units, in an adult >75 kg. Administration once daily (nine million in 4 h) or twice a day (4.5 million bid) is recommended on the basis of pharmacokinetic data, but the risk of bacterial regrowth between too distant doses suggests caution. The scarce concentrations in the sites of infection and the relatively high MICs, even among strains still susceptible, strongly suggest the use of colistin in association with other drugs. Laboratory and clinical data suggest rifampin 600 mg IV or oral is a possible partner. However, the choice of the best combination of drugs should be based on synergy tests that the laboratory should perform in case of XDR clinical isolates. Other possible partners include injectable fosfomycin 3–6 g IV qid, aminoglycosides, for instance, amikacin 1 g IV qd, and in case of intermediate susceptibility or low-level resistance, carbapenems, in two- or three-drug combinations [33, 35]. These approaches are experimental and consequently require a strong collaboration between clinicians and microbiologists so that each case can contribute to the general debate.
The new compound Ceftolozane/tazobactam has been demonstrated to have a good activity against P. aeruginosa, including MDR and XDR strains, and should always be tested on these strains [31]. Real-life experience suggests ceftolozane/tazobactam can be effective in the treatment of serious infections due to Pseudomonas aeruginosa, including pneumonia, in this case at a dose double than standard [37].
Cefiderocol, a new siderophore cephalosporin, is promisingly active against carbapenem-resistant Gram negative, including Enterobacteriaceae, A. baumannii, P. aeruginosa, and S. maltophilia [38].
2.4.4 XDR A. baumannii
Usually, infections due to A. baumannii affect patients admitted in ICUs in epidemic clusters. Colonization is much more common than infection and it’s important to reserve treatment only to well-defined infections. This is quite simple for bacteremia, but much less for VAP.
The phenotype of resistance of XDR A. baumannii is close to that of P. aeruginosa, with the relevant difference that more than 50% of the strains show relatively low MICs of tigecycline (2 mg/L). Also in case of XDR A. baumannii infection, monotherapy with colistin, and even worse, with tigecycline, is not recommended and an association of at least two drugs, for instance, colistin and tigecycline, is advisable. Amikacin, which is often reported to be active, often results to be antagonistic when combined with colistin [33].
Cefiderocol, due to its high in vitro activity, might have a significant impact in the management of A.baumannii infections [38].
2.4.5 KPC-Producing K. pneumoniae and Other Carbapenemase-Producing Enterobacteriaceae (CRE)
KPC-producing K. pneumoniae (KPC-KP) is currently spreading as an epidemic in many Countries, mostly in ICUs, but also in Neurorehabilitation, Internal Medicine, and Surgery wards due to the pathway of patients transferred from one ward to another and spreading the microorganism within the hospital. These outbreaks are also relevant for the mortality that seems to be higher than that caused by nonfermenting XDR Gram-negative. Risk factors for KPC-KP colonization include prolonged hospital stay and concomitant broad-spectrum antibiotic treatment. KPC-KP infections mainly affect vulnerable patients and often induce septic shock.
The strategy to treat KPC-KP infection has been traditionally based on (a) higher doses, for instance, meropenem 2 g tid, tigecycline 100 mg bid, colistin nine million units as loading dose followed by 4.5 million units bid, (b) optimized administration, e.g., loading dose followed by extended infusion of carbapenems, and (c) combination therapy. In fact, combination therapy has demonstrated superiority in terms of mortality versus monotherapy [34, 39]. However, the wide use of carbapenems is among the reasons of the spread of MDR bugs and should be used in the treatment of CRE, in combination with other drugs, only when precise MICs are available and relatively low. Rapid and standardized tests aimed at studying the synergistic activity of different combinations of antibiotics are urgently needed.
Recently introduced, Ceftazidime/avibactam, the association of an old third-generation cephalosporin with a new beta-lactamase inhibitor, can now be considered as first-line treatment for severe infections caused by these microorganisms, preferably in combination with a companion drug, such as an aminoglycoside, to increase bactericidal activity and prevent selection of resistance [40]. Although the best administration strategy has not yet been established, at least in most severe infections, a loading dose followed by extended or continuous infusion is probably advisable. In less severe, nonbacteremic infections, ceftazidime/avibactam can possibly be spared using tigecycline in the setting of abdominal infections, fosfomycin and aminoglycosides for UTIs. The association of gentamicin with colistin is generally not advisable because of the high risk of nephrotoxicity.
Unfortunately, avibactam is not active against MBL, such as NDM enzymes. In such a case, aztreonam should be considered, since it is generally resistant to MBL, preferably in association with avibactam, or perhaps another beta-lactamase inhibitor, to protect it against other beta-lactamase, that often these strains produce in addition to MBL [41]. Again, a loading dose followed by extended or continuous infusion is probably the best administration strategy. A coformulation with avibactam will probably be available in the next future. Meanwhile, the combination with ceftazidime/avibactam is the only option.
Cefiderocol showed a very promising in vitro activity against CRE, with very low resistance rates [42].
Other drugs, such as plazomicin, a new aminoglycoside, eravacycline, and combinations of carbapenems with other beta-lactamase inhibitors, namely, meropenem/vaborbactam and imipenem/relebactam, are about to be available and might contribute significantly to the management of these infections.
2.5 Empiric Therapy
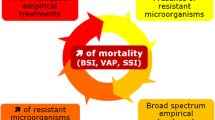
The fundamental principle of antimicrobial therapy in these patients is the timeliness of the beginning of optimal initial antibiotic treatment (IAT) [34]. However, the increasing prevalence of MDR Gram-negative bacteria increases the chances of failure of the IAT, while an extended use of broad-spectrum antimicrobials may lead to further spread of resistance.
Waiting for the results of cultures, recommendations for the initial management of patients with suspected Gram-negative infections include [6]: (1) careful assessment of the infectious state in terms of clinical severity and probability of Gram-negative MDR bacteria etiology; (2) assessment of previous bacterial colonization or of treatments that may have increased the likelihood of resistant organisms; (3) knowledge of local epidemiology; (4) early administration of an empirical antimicrobial therapy based on these considerations with subsequent adjustment based on the results from the microbiological laboratory. Depending on the suspected microorganism, an appropriate empirical IAT may include the combination of a broad-spectrum or anti-Pseudomonas cephalosporin plus an aminoglycoside, a beta-lactamase inhibitor combined with an aminoglycoside or a carbapenem. Although antibiotic-combination therapy regimens can lead to increased costs and adverse effects of drugs, the rationale for their use, at least at an early stage, is based on the possibility to take advantage of possible drug synergism, prevention (or delay) of drug resistance and widening of antimicrobial coverage when the risk of MDR organisms is high by using drugs with different mechanisms of action.
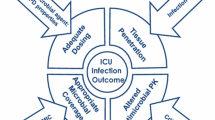
Standard dosing regimens are often not adequate for critically ill patients due to some differences in pharmacokinetic/pharmacodynamic parameters characterizing ICU patients: an (a) increased volume of distribution and (b) increased renal clearance of antibiotics [43]. Initial antibiotic doses should therefore address the increased volume of distribution of antibiotics such that a large loading dose is required independent of subsequent clearances. If not, time to achieve adequate bacterial killing activity is delayed due to underdosing, which predisposes to the emergence of newly resistant bacterial strains.
Once the results of the laboratory are available, the treatment regimen can be adapted and, possibly, de-escalated to the narrowest spectrum of activity. Notably, de-escalation of initial empirical therapy seems to be associated with lower mortality among patients’ sepsis and septic shock [44].
In the era of fast, automated nucleic acid amplification tests, the Microbiology lab is able to detect genes encoding for resistance mechanisms, e.g., carbapenemases, well before phenotypic susceptibility testing is available. On the basis of this information, the clinician can adjust therapy: for instance, supposing an Enterobacteriacea is isolated from blood culture and no genes for carbapenemases are detected, a carbapenem or ceftolozane/tazobactam, eventually in combination with an aminoglycoside, can be chosen; in case gene for KPC is detected, ceftazidime/avibactam, eventually in combination with an aminoglycoside, is probably the best option; in case gene for MBL is detected, ceftazidime/avibactam plus aztreonam is probably the most effective regime.
2.6 Duration of Therapy
The optimal duration of antibiotic therapy remains controversial but has significantly decreased over the past two decades, since an excessively long duration is recognized as one of the main reasons of inappropriateness in antibiotic therapy. In ventilator pneumonia, a shorter treatment course of 7–8 days has been validated, even though for some specific pathogens or clinical situations a longer treatment course may still be recommended [1]. For complicated intra-abdominal infection, a treatment course of 4 days may also be acceptable when septic shock is not present [45]. Serial biomarkers such as procalcitonin can also help to accurately identify patients appropriate for shorter courses of antibiotics [46].
2.7 Role of Additional Therapies in Gram-Negative MDR/XDR Bacteria Septic Shock
Early identification of the causing agent, appropriate antibiotic therapy, and prompt volemic resuscitation in shocked patients are the cornerstones for the treatment of sepsis caused by MDR germs. However, given the increasing clinical and therapeutic burdens caused by antibiotic resistance and the high prevalence of immune suppression in patients with MDR infection, many experts and opinion makers consider the use of additional therapies reasonable in critically ill patients [6]. The use of adjunctive therapies for restoring immune function seems to be very promising but, unfortunately, sound evidence is not yet available. Waiting for the results of the ongoing trials, in patients with sepsis by MDR/XDR infections the capability of immune response should be carefully monitored by appropriate biomarkers. New emerging drugs focused on modifying the inflammatory response are currently being investigated for the treatment of septic shock. Immunomodulatory therapy for sepsis includes inflammatory cytokines, cellular receptors, nuclear transcription factors, coagulation activators, and apoptosis regulators. There are various therapies based on monoclonal antibodies that block inflammatory mediators and receptors, agents that block or eliminate bacterial products, modulators of immune function and immunostimulatory molecules. They have shown promising results in animal tests and are currently at various stages of clinical evaluation. This is an approach based on the more modern concept of “precision” or “personalized” medicine. An example of “personalized medicine in sepsis management” is the potential benefit of beta blockers infusion in the subset of patients with tachycardia [47, 48].
2.8 Prevention and Control of MDR Infections in the ICU
Infection control measures, pivotal for reducing the spread of Gram-negative MDR organisms in hospitals, include the implementation of specific guidelines for the early detection of resistant organisms (e.g., screening for rectal colonization), educational programs for hand hygiene and monitoring of hand hygiene protocols application, timely alert systems, and strict isolation procedures when resistant microorganisms are isolated [6, 33]. Since microorganism resistance patterns may vary from center to center, effective surveillance is important to continuously evaluate the state of bacterial resistance in specific departments. Antimicrobial stewardship programs should be implemented to ensure the appropriate use of antibiotics. A recent meta-analysis evaluated the relative effectiveness of strategies for the prevention of Gram-negative MDR bacteria infections in ICU patients [3]. Forty-two studies (5 randomized controlled trials and 37 observational studies) and 62,068 patients were included in the analysis. The meta-analysis showed that a multifaceted strategy consisting of standard care, antimicrobial stewardship, accurate environmental cleansing, and source control actions was the most effective intervention to prevent the acquisition of MDR Gram-negative germs.
2.9 Antimicrobial Stewardship
Institution of an antimicrobial stewardship program (AMS) seems to be an effective strategy and is strongly recommended in ICUs with a high prevalence of MDR bacteria with the aim of fighting drug resistances, improving patient outcomes, and reducing health-care costs [49]. Key issues of AMS programs are halting antibiotics in patients without infection and selection of the appropriate drug for empirical therapy that, as general rules, depends on clinical conditions of the patient, source of infection, local antimicrobial susceptibility patterns, patient microbiological history, and previous therapy. Moreover, use of adequate dosages, early de-escalation of empirical broad-spectrum antibiotics focusing the treatment on the isolated microorganism, switching to monotherapy whenever possible, and a short course of therapy are also fundamental elements of AMS in critically ill patients. An AMS program in ICUs should include also full-time Infectious Disease physicians and clinical pharmacists with infectious disease training in reducing antimicrobial use.
A close relationship with the Microbiology Laboratory is mandatory in case of severe infections due to MDR microorganisms: all the phases of processing have to be fastened and results promptly communicated and tailored strategies such as additional susceptibility tests, synergy testing, and bactericidal activity of the serum must be considered.
Also, prospective audit and feedback of antimicrobial prescriptions, therapeutic drug monitoring, formulary restrictions, use of local antibiograms, and partnership with infection prevention services, when available, are important parts of the package.
References
Kollef M, Bassetti M, Francois B, et al. The intensive care medicine research agenda on multidrug-resistant bacteria, antibiotics, and stewardship. Intensive Care Med. 2017;43:1187–97.
Cassini A, Högberg LD, Plachouras D, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis. 2019;19(1):56–66. Epub 2018 Nov 5. https://doi.org/10.1016/S1473-3099(18)30605-4.
Bassetti M, Righi E. New antibiotics and antimicrobial combination therapy for the treatment of gram-negative bacterial infections. Curr Opin Crit Care. 2015;21:402–11.
Teerawattanapong N, Kengkla K, Dilokthornsakul P, et al. Prevention and control of multidrug-resistant gram-negative bacteria in adult intensive care units: a systematic review and network meta-analysis. Clin Infect Dis. 2017;64:S51–60.
Hawkey PM, Warren RE, Livermore DM, et al. Treatment of infections caused by multidrug-resistant gram-negative bacteria: report of the British Society for Antimicrobial Chemotherapy/Healthcare Infection Society/British Infection Association Joint Working Party. J Antimicrob Chemother. 2018;73:iii2–iii78.
Tosi M, Roat E, De Biasi S, Munari S, et al. Multidrug resistant bacteria in critically ill patients: a step further antibiotic therapy. J Emerg Crit Care Med. 2018;2:103.
Vincent JL, Marshall JC, Amendys-Silva SA, et al. Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med. 2014;2:380–6.
Vincent J, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302:2323–9.
European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). Stockholm: ECDC; 2010. p. 2017.
http://www.consilium.europa.eu/en/press/press-releases/2016/06/17-epsco-conclusions-antimicrobial-resistance/. Visited April 2019.
Magiorakos A-P, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
Peterson LR. Bad bugs, no drugs: no escape revisited. Clin Infect Dis. 2009;49:992–3.
Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States. http://www.cdc.gov/drugresistance/threat-report-2013/index.html. Visited April 2019.
Maragakis LL, Perencevich EN, Cosgrove SE. Clinical and economic burden of antimicrobial resistance. Expert Rev Anti Infect Ther. 2008;6:751–63.
Malacarne P, Boccalatte D, Acquarolo A, et al. Epidemiology of nosocomial infection in 125 Italian intensive care units. Minerva Anestesiol. 2010;76:13–23.
Al-Nassir WN, Sethi AK, Li Y, et al. Both oral metronidazole and oral vancomycin promote persistent overgrowth of vancomycin resistant enterococci during treatment of Clostridium difficile-associated disease. Antimicrob Agents Chemother. 2008;52:2403–6.
Salgado CD. The risk of developing a vancomycin-resistant Enterococcus bloodstream infection for colonized patients. Am J Infect Control. 2008;36:S175.e5–8.
Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285–92.
Wunderink RG, Niederman MS, Kollef MH, Shorr AF, Kunkel MJ, Baruch A, McGee WT, Reisman A, Chastre J. Linezolid in methicillin-resistant Staphylococcus aureus nosocomial pneumonia: a randomized, controlled study. Clin Infect Dis. 2012;54(5):621–9. Epub 2012 Jan 12. https://doi.org/10.1093/cid/cir895.
Awad SS, Rodriguez AH, Chuang YC, Marjanek Z, Pareigis AJ, Reis G, Scheeren TW, Sánchez AS, Zhou X, Saulay M, Engelhardt M. A phase 3 randomized double-blind comparison of ceftobiprole medocaril versus ceftazidime plus linezolid for the treatment of hospital-acquired pneumonia. Clin Infect Dis. 2014;59(1):51–61. Epub 2014 Apr 9. https://doi.org/10.1093/cid/ciu219.
Dunne MW, Puttagunta S, Sprenger CR, Rubino C, Wart S, Baldassarre J. Extended-duration dosing and distribution of Dalbavancin into bone and articular tissue. Antimicrob Agents Chemother. 2015;59(4):1849–55. Prepublished online 2015 Jan 5. Published online 2015 Mar 11. https://doi.org/10.1128/AAC.04550-14.
Lodise TP, Fang E, Minassian SL, Prokocimer PG. Platelet profile in patients with acute bacterial skin and skin structure infections receiving tedizolid or linezolid: findings from the phase 3 ESTABLISH clinical trials. Antimicrob Agents Chemother. 2014;58(12):7198–204. https://doi.org/10.1128/AAC.03509-14.
Tulkens PM, Van Bambeke F, Zinner SH. Profile of a novel anionic Fluoroquinolone-Delafloxacin. Clin Infect Dis. 2019;68(Supplement_3):S213–22. https://doi.org/10.1093/cid/ciy1079.
Munita JM, Murray BE, Arias CA. Daptomycin for the treatment of bacteraemia due to vancomycin-resistant enterococci. Int J Antimicrob Agents. 2014;44(5):387–95. Epub 2014 Sep 2. https://doi.org/10.1016/j.ijantimicag.2014.08.002.
Yadav G, Thakuria B, Madan M, Agwan V, Pandey A. Linezolid and vancomycin resistant enterococci: a therapeutic problem. J Clin Diagn Res. 2017;11:GC07–11.
Rivera AM, Boucher HW. Current concepts in antimicrobial therapy against select gram-positive organisms: methicillin-resistant Staphylococcus aureus, penicillin-resistant pneumococci, and vancomycin-resistant enterococci. Mayo Clin Proc. 2011;86:1230–43.
Mercuro NJ, Davis SL, Zervos MJ, Herc ES. Combatting resistant enterococcal infections: a pharmacotherapy review. Expert Opin Pharmacother. 2018;19:979–92.
Mody RM, Erwin DP, Summers AM, et al. Ertapenem susceptibility of extended spectrum beta-lactamase-producing organisms. Ann Clin Microbiol Antimicrob. 2007;6:6.
Kaufman SE, Donnell RW, Hickey WS. Rationale and evidence for extended infusion of piperacillin-tazobactam. Am J Health Syst Pharm. 2011;68:1521–6.
Harris PNA, Tambyah PA, Lye DC, et al. Effect of Piperacillin-Tazobactam vs Meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: a randomized clinical trial. JAMA. 2018;320(10):984–94.
Sader HS, Farrell DJ, Castanheira M. Antimicrobial activity of ceftolozane/tazobactam tested against Pseudomonas aeruginosa and Enterobacteriaceae with various resistance patterns isolated in European hospitals (2011-12). J Antimicrob Chemother. 2014;69(10):2713–22.
Tasina E, Haidich AB, Kokkali S, Arvanitidou M. Efficacy and safety of tigecycline for the treatment of infectious diseases: a meta-analysis. Lancet Infect Dis. 2011;11:834–44.
Cerceo E, Deitelzweig SB, Sherman BM, Amin AN. Multidrug-resistant gram-negative bacterial infections in the hospital setting: overview, implications for clinical practice, and emerging treatment options. Microb Drug Res. 2016;22:412–31.
Cunha BA. Pharmacokinetic considerations regarding tigecycline for multidrug-resistant (MDR) Klebsiella pneumoniae or MDR Acinetobacter baumannii urosepsis. J Clin Microbiol. 2009;47:1613.
Bassetti M, Carnelutti A, Peghin M. Patient specific risk stratification for antimicrobial resistance and possible treatment strategies in gram-negative bacterial infections. Expert Rev Anti Infect Ther. 2017;15:55–65.
Miriagou V, Cornaglia G, Edelstein M, et al. Acquired carbapenemases in gram-negative bacterial pathogens: detection and surveillance issues. Clin Microbiol Infect. 2010;16:112–22.
Bassetti M, Castaldo N, Cattelan A. Ceftolozane/tazobactam for the treatment of serious Pseudomonas aeruginosa infections: a multicentre nationwide clinical experience. Int J Antimicrob Agents. 2019;53(4):408–15.
Zhanel GG, Golden AR, Zelenitsky S, et al. Cefiderocol: a siderophore cephalosporin with activity against carbapenem-resistant and multidrug-resistant gram-negative bacilli. Drugs. 2019;79(3):271–89.
Tumbarello M, Trecarichi EM, De Rosa FG, Giannella M, Giacobbe DR, Bassetti M, Losito AR, Bartoletti M, Del Bono V, Corcione S, Maiuro G, Tedeschi S, Celani L, Cardellino CS, Spanu T, Marchese A, Ambretti S, Cauda R, Viscoli C, Viale P, ISGRI-SITA (Italian Study Group on Resistant Infections of the Società Italiana Terapia Antinfettiva). Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrob Chemother. 2015;70(7):2133–43. Epub 2015 Apr 21. https://doi.org/10.1093/jac/dkv086.
Tumbarello M, Trecarichi EM, Corona A, et al. Efficacy of Ceftazidime-Avibactam salvage therapy in patients with infections caused by Klebsiella pneumoniae Carbapenemase-producing K. pneumoniae. Clin Infect Dis. 2019 Jan 18;68(3):355–64.
Emeraud C, Escaut L, Boucly A, et al. Aztreonam plus Clavulanate, Tazobactam or Avibactam for treatment of infections caused by Metallo-β-lactamase-producing gram-negative bacteria. Antimicrob Agents Chemother. 2019;63(5):e00010–9.
Hackel MA, Tsuji M, Yamano Y, Echols R, Karlowsky JA, Sahm DF. In vitro activity of the siderophore cephalosporin, cefiderocol, against carbapenem-nonsusceptible and multidrug-resistant isolates of gram-negative bacilli collected worldwide in 2014 to 2016. Antimicrob Agents Chemother. 2018;62:e01968–17. https://doi.org/10.1128/AAC.01968-17.
Roberts JA, Taccone FS, Lipman J. Understanding PK/PD. Intensive Care Med. 2016;42:1797–800.
Garnacho-Montero J, Gutiérrez-Pizarraya A, Escoresca-Ortega A, Corcia-Palomo Y, Fernández-Delgado E, Herrera-Melero I, Ortiz-Leyba C, Márquez-Vácaro JA. De-escalation of empirical therapy is associated with lower mortality in patients with severe sepsis and septic shock. Intensive Care Med. 2014;40(1):32–40. Epub 2013 Sep 12. https://doi.org/10.1007/s00134-013-3077-7.
Sawyer RG, Claridge JA, Nathens AB, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372:1996–2005.
De Jong E, van Oers JA, Beishuizen A, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016;16:819–27. https://doi.org/10.1016/S1473-3099(16)00053-0.
Busani S, Roat E, Serafini G, et al. The role of adjunctive therapies in septic shock by gram negative MDR/XDR infections. Can J Infect Dis Med Microbiol. 2017;2017:2808203.
Rello J, Valenzuela-Sanchez F, Ruiz-Rodriguez M, Moyano S. Sepsis: a review of advances in management. Adv Ther. 2017;34:2393–411.
Karanika S, Paudel S, Grigoras C, et al. Systematic review and meta-analysis of clinical and economic outcomes from the implementation of hospital-based antimicrobial stewardship programs. Antimicrob Agents Chemother. 2016;60:4840–52.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tagliaferri, E., Menichetti, F., Biancofiore, G. (2020). MDR Infections in the ICU. In: Chiumello, D. (eds) Practical Trends in Anesthesia and Intensive Care 2019. Springer, Cham. https://doi.org/10.1007/978-3-030-43873-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-43873-9_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43872-2
Online ISBN: 978-3-030-43873-9
eBook Packages: MedicineMedicine (R0)