Abstract
In this chapter, we will review studies of HER2 in osteosarcoma and discuss the controversies that have existed in this field. Our present understanding of HER2 in the context of osteosarcoma is that it is expressed on a subset of patient samples, but that expression is not prognostic. We will review the two trials that have been conducted in osteosarcoma which have targeted HER2. Use of an antibody, trastuzumab, did not suggest activity, but a smaller study using HER2-targeted CAR T cells suggested activity may be present. A trial of an antibody–drug conjugate targeting HER2 for recurrent osteosarcoma is under consideration. Trials targeting other surface proteins for the treatment of osteosarcoma have occurred or are in development. Indeed, this leads us to discuss in a broader fashion therapeutic approaches to targeting surface proteins. It is hoped that some of these approaches will lead to new effective therapies for patients with osteosarcoma.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The first studies of HER2 expression in osteosarcoma date back to the 1990s, recognizing a proportion of osteosarcoma samples express the protein. Early studies produced discordant results with the factors underlying variability in immunohistochemical staining in osteosarcoma not fully appreciated and genomic amplification of HER2, providing an alternative testing approach, not being present. The current understanding is expression is present on a subset of tumors from osteosarcoma patients, but this is not prognostic. Treating patients whose osteosarcoma samples express HER2 with trastuzumab did not demonstrate clinical activity, but a clinical trial utilizing HER2-directed CAR T cells suggested some clinical efficacy. The more recently developed approach for targeting low HER2-expressing malignancies is the use of antibody–drug conjugates, which will likely be pursued in clinical trials for osteosarcoma. Beyond HER2, antibody–drug conjugates that do not necessarily rely on the target protein being an oncogenic driver may be an alternative path forward for osteosarcoma treatment.
HER2 as an Oncogene in Osteosarcoma
HER2 Biology
HER2 was first described by multiple groups in the 1980s, which has led to its multiple names in the literature [1] . Like its homolog, EGFR, HER2 is a transmembrane tyrosine kinase receptor [2]. During fetal development, HER2 is widely expressed in tissues including placenta, liver, kidney, lung, and brain. Lower levels of expression are also seen in adult tissues: kidney, liver, skin, lung, jejunum, uterus, stomach, and colon. The HER2 null mouse is embryonic lethal due to complete absence of cardiac trabeculae [3]. There are four members of the family of epidermal growth factor receptor tyrosine kinases: ErbB1 (EGFR), ErbB2 (HER2), ErbB3 (HER3), and ErbB4 (HER4). All of these receptors need to dimerize to initiate the signaling cascade and frequently form heterodimers. HER2 is unique in that it is the only member of this family for which there is no known ligand. However, it has been shown to be the preferred partner for the other members to form heterodimers. HER2 overexpression has been shown to be tumorigenic. The transfection of NIH3T3 cells with HER2 transforms the cells and leads to tumor formation in mice. The tumorigenicity is associated with level of expression of HER2 within the transformed cells [4, 5]. Transgenic mice expressing HER2 under the control of a mouse mammary cell-specific promoter form mammary tumors consistent with adenocarcinomas at 4 months of age. Ultimately most of the mice develop lung metastases as well [6].
HER2 in Osteosarcoma Cell Lines
Unlike in breast cancer cells, in osteosarcoma cell lines, HER2 displays primarily cytoplasmic or mixed membranous and cytoplasmic staining. Compared to EGFR, HER2 demonstrated less intense staining by immunohistochemistry. The expression levels by immunohistochemistry correlate with the levels of messenger RNA detected by PCR and protein by Western blots. In primary osteosarcoma cell lines, despite the lack of detection of HER2 on the membrane by immunohistochemistry, flow cytometry reveals higher quantities of HER2 than EGFR on the surface [7].
Two other studies have corroborated the cell surface expression of HER2 by flow cytometry in osteosarcoma cell lines. Hassan et al. demonstrated in primary as well as established osteosarcoma cell lines that HER2 is detectable in greater quantities than EGFR [8]. Scotlandi et al. found that 62% of the primary and established osteosarcoma cell lines demonstrate HER2 expression by flow cytometry, albeit at lower levels than the breast and ovarian cancer cell lines used as positive controls. None of the osteosarcoma cell lines demonstrated amplification of the HER2 gene by fluorescence in situ hybridization [9]. Unlike the data in cell lines, the studies in patient samples have described conflicting results regarding whether HER2 is expressed in osteosarcoma and its role in defining prognosis.
HER2 Is a Negative Prognostic Indicator in Osteosarcoma
Six studies have demonstrated that HER2 expression in osteosarcoma portends a poor outcome. Onda et al. in 1996 first described HER2 expression in osteosarcoma. They found that 42% of tissues demonstrated various levels of expression by immunoblotting , which was scored from 0 to 3+ (no staining, weak, moderate, and high, respectively). This was corroborated by immunohistochemistry, revealing a primarily membranous pattern of staining. Southern blot analysis did not reveal any amplification of the HER2 gene. Patients whose tumors expressed HER2 (1–3+) had a significantly worse response to preoperative chemotherapy and survival. In this series, patients who had no HER2 expression demonstrated a 1-year survival rate of 100% and 3-year survival rate of 84%. In contrast, those with weak to high expression of HER2 had significantly worse outcomes with 1- and 3-year survival rates of 61% and 14%, respectively [10].
Gorlick et al. evaluated 53 patients treated on the T12 protocol. This randomized trial found no survival benefit to dose intensification of the preoperative chemotherapy, allowing all the samples to be treated as a single cohort [11]. HER2 expression levels were evaluated by immunohistochemistry and scored according to the percentage of cells staining positive: 0 (no staining), 1+ (1–25%), 2+ (26–50%), 3+ (51–75%), and 4+ (76–100%). HER2 staining localized primarily to the cell membrane. Overexpression was defined as greater than 2+ staining. HER2 was overexpressed in 45.3% of the patients’ tumors, which was similar to the 42.6% detected from the initial biopsy specimens. Overexpression of HER2 was found to be correlated with decreased response to preoperative chemotherapy and event-free survival. At 5-years, patients whose tumors overexpressed HER2 had a 40% event-free survival compared to 78% for patients with low or undetectable levels of HER2 expression. The difference in event-free survival remained significant even when 13% of patients who presented with metastatic disease were excluded from the analysis (47% versus 79%) [12].
Zhou et al. reviewed HER2 expression from 25 patients treated at their institution from 1981 to 1996. They included in their analysis 25 primary tumor samples and 12 specimens from metastatic lung lesions. Immunohistochemistry was defined as positive if greater than 25% of tumor cells demonstrated immunoreactivity. Amplification was defined as positive if greater than 10% of the cells demonstrated more than two signals or if more than three cells showed a large number of signals by FISH probe for the HER2 gene. They found focal to diffuse cytoplasmic staining in 44% of the primary tumor samples and 58% of the pulmonary metastases. HER2 expression was not found to be correlated with response to chemotherapy. However, patients whose tumors stained positive for HER2 were found to have a significantly worse metastasis-free survival. To evaluate for amplification of the HER2 gene, FISH was performed on 12 samples. Increased signal consistent with amplification was observed in six of seven immunostain-positive samples and two of five immunostain-negative samples. In the two immunostain-negative samples which were found to have amplification of HER2, the immunohistochemistry revealed focal HER2 staining which did not meet the criteria for positive [13].
In 2004, Fellenberg et al. attempted to address some of these issues with immunohistochemistry by assessing HER2 expression at the level of mRNA by real-time reverse-transcription PCR (RT-PCR). To enrich the samples, they used laser microdissection to isolate osteosarcoma cells for analysis. They evaluated 17 pretreatment biopsies from a single institution using histologic response as their primary clinical endpoint. They found that HER2 mRNA could be detected in all the samples tested. HER2 expression was significantly elevated in patients who demonstrated a poor histologic response to preoperative chemotherapy. When they analyzed the samples for protein expression by immunohistochemistry, they found strong cytoplasmic staining in all the samples. There was no correlation between mRNA levels and protein expression of HER2 [14].
Ferrari et al. published a report on a cohort of 19 patients who presented with localized disease who subsequently experienced a pulmonary relapse. They examined HER2 expression by immunohistochemistry according to the percentage of cells staining positive on the membrane, 0–4+. The tumor was considered to be positive if it exhibited 2+ or greater staining. They found HER2 to be expressed in 32% of the primary tumors, and 53% of the patients had at least one nodule expressing HER2. The accordance rate, defined as the presence of the same expression pattern in the primary and metastatic samples, was 42%. Patients with HER2-positive primary tumors had a shorter recurrence-free interval of 17.2 months versus 31.8 months for patients with HER2-negative primary tumors. Likewise, patients with HER2-positive primary tumors were more likely to recur with multiple pulmonary metastases [15].
A large, single-institution, retrospective analysis of HER2 expression in osteosarcoma in 84 patients treated on two similar protocols was published by Scotlandi et al. in 2005. They examined pretreatment biopsy specimens, using two different antibodies, and for half of the specimens three different antibodies. They defined expression as having greater than 25% of the cells stain positive. They detected HER2 expression in 32% of the samples with a pattern of focal to diffuse cytoplasmic staining. Between the two antibodies tested, they found a concordance rate of 78%. For the samples tested with the third antibody, similar results were obtained with 28% of the samples positive for HER2 expression. Patients with HER2-negative tumors exhibited an event-free survival of greater than 60% compared to approximately 40% for those expressing HER2 [9]. This analysis demonstrated cytoplasmic staining for HER2 in osteosarcoma with a high rate of concordance using multiple antibodies.
HER2 Is Not Prognostic in Osteosarcoma
Nine studies have reported that HER2 expression is not prognostic in osteosarcoma. In 2001, Maitra et al., using immunohistochemistry and FISH, examined 21 diagnostic biopsy specimens from a single institution. For immunohistochemistry analysis, they defined as positive only cell membrane staining, excluding cytoplasmic and nuclear staining, and graded according to a four-tier grading scheme: negative, low, medium, and high. They did not find HER2 overexpression by immunohistochemistry in any of the samples. Likewise, they did not detect any amplification of the HER2 gene by FISH [16].
Kilpatrick et al., in the same year, reported on a retrospective analysis from two centers between 1985 and 2000. They examined HER2 expression by immunohistochemistry comparing two different antibodies as well as decalcified versus non-decalcified specimens. Staining was scored from 0 to 3+. Positive was defined as 2+ or 3+: weak to moderate staining in more than 10% of cells or moderate to strong staining in more than 10% of cells. None of the osteosarcoma specimens demonstrated staining for HER2 on the cell membrane. Focal cytoplasmic staining in more than 10% of the cells was found in 83% and 98% of the samples, using the different antibodies. There was poor agreement between the antibodies in the extent of cytoplasmic staining. Neither antibody demonstrated a correlation with response to preoperative chemotherapy, metastasis, or survival [17].
Thomas et al. performed a retrospective analysis of osteosarcomas in a single institution from 33 patients. They graded the immunohistochemical staining according to a five-tier system: negative, cytoplasmic, low-positive membranous, medium-positive membranous, and high-positive membranous. None of the samples demonstrated staining for HER2 on the cell membrane. Forty-seven percent of the specimens demonstrated diffuse cytoplasmic staining. None of the samples had HER2 mRNA amplifiable by RT-PCR [18].
Anninga et al. evaluated 15 pretreatment biopsy specimens as well as 12 specimens including postchemotherapy resections or pulmonary, distant bone, or local relapse specimens. They evaluated the samples by quantitative real-time RT-PCR (qPCR) and by immunohistochemistry. Tumor samples were scored 0–3+ according to the level of membrane staining. Cytoplasmic staining was not considered positive. Of the 27 evaluable specimens, only one sample (from a pre-treatment biopsy) displayed membranous staining, which was scored as moderate. Focal cytoplasmic staining was detected in two other samples. None of the samples had overexpression of HER2 mRNA when compared to a HER2 overexpressing cell line. In the one sample with HER2 membranous staining, FISH did not reveal HER2 amplification [19].
A collaborative project involving four institutions evaluated HER2 expression in 22 samples from 20 patients. Immunohistochemistry was graded from 0 to 3+ according to level (>10% of cells) and intensity (mild, moderate, strong) of membranous staining. Scores of 0 and 1+ were considered to be negative. Four of the samples (18%) showed focal positivity for HER2 (1+ grading). None of the samples revealed amplification of HER2 by fluorescence in situ hybridization. When the authors interpreted 1+ staining as positive, univariate analysis did not reveal a statistically significant difference in survival in the two groups [20].
Somers et al. reviewed 34 samples from 18 patients in a single institution. They graded the immunostaining from 0 to 3+ according to the intensity of membrane staining. Cytoplasmic staining was graded as 0. They found that four osteosarcoma specimens from two patients displayed HER2 immunostaining. Two revealed cytoplasmic staining (0), and two cytoplasmic and membranous staining (1+). None of the samples were evaluated as having overexpression of HER2 by immunohistochemistry. None of the samples demonstrated HER2 gene amplification by FISH. In 39% of the tumors, aneuploidy (having multiple signals to the FISH probe) was detected in less than 10% of the cells. They also noted that four samples exhibited three nuclear signals in greater than 50% of the cells, which they state is suggestive for trisomy 17. None of the tumors with increased signal by FISH probe displayed expression for HER2 [21]. Since there was no concordance between the increased chromogenic signal and immunohistochemistry, the authors concluded that the increased signal should not be interpreted as amplification of the gene.
HER2 gene amplification was evaluated by Willmore-Payne et al. using FISH as well as multiplex and monoplex PCR. They also performed immunohistochemistry on the samples, grading from 0 to 3+. Cytoplasmic staining was graded as 0. In the initial 21 cases evaluated by multiplex PCR and FISH, there was no evidence of HER2gene amplification. Of these cases, 11 demonstrated cytoplasmic staining for HER2 by immunohistochemistry, which were all graded as 0. No samples demonstrated membranous staining. Given the negative findings, they obtained an additional 35 paraffin blocks from 26 patients from another institution to perform monoplex PCR and FISH. Again, they were not able to detect any HER2 gene amplification. In these 26 patients, they detected 2 samples with cytoplasmic staining for HER2 by immunohistochemistry, and 1 sample with 1+ membranous staining [22].
Bakhshi et al. evaluated HER2 expression by immunohistochemistry in 63 patients. They delineated the pattern of staining as cytoplasmic versus membranous. They graded the samples according to the percentage of cells stained: 0, 0–10%; 1+, 11–30%; 2+, 31–50%; 3+, 51–100%. They observed HER2 staining (1+ and greater) in 47.6% of samples. All of the samples demonstrated cytoplasmic staining, and four samples demonstrated both cytoplasmic and membranous staining. Positive staining for HER2 was not correlated with metastatic disease at presentation [23].
The Children’s Oncology Group analyzed samples from a clinical trial of trastuzumab in osteosarcoma. They evaluated 191 samples from 149 patients for whom there were confirmed histologic diagnosis of osteosarcoma, adequate staining, and survival information. HER2 overexpression was evaluated by immunohistochemistry and graded according to the percentage of cells staining positive: negative (no staining), 1+ (0–25%), 2+ (26–50%), 3+ (51–75%), and 4 (>75%). Positive for HER2 overexpression was defined by a grade of 3+ or 4+. According to these criteria, the investigators found that HER2 was overexpressed in 13.4% of the samples evaluated. HER2 overexpression did not correlate with survival [24].
HER2 Is a Positive Prognostic Indicator in Osteosarcoma
Adding to the controversy over the relevance of HER2 in osteosarcoma, Akatsuka et al. published a report of 81 patients with localized disease from 2 centers. They evaluated initial biopsy specimens for HER2 expression by immunohistochemistry. The samples were graded from 0 to 3+ based on the percentage of cells staining positive: 0, negative; 1+, 1–30%; 2+, 31–75%; and 3+, 76–100%. The section with the highest degree of staining was used as representative, and overexpression was defined as tumors with 2+ or 3+ staining. They found that 63% of the tumors had overexpression of HER2. HER2 expression did not correlate with response to chemotherapy. Overexpression of HER2 was significantly correlated with event-free survival. At 5 years, the event-free survival of patients with overexpression of HER2 was 72% compared to 46% for patients without HER2 overexpression [25]. In a separate report, these authors also demonstrate that the rate of HER2 expression is lower in metachronous pulmonary metastases as compared to initial biopsy specimens [26].
Summary of HER2 Expression Studies
A summary of the results is provided in Table 5.1. A meta-analysis published in 2010 evaluated the association of HER2 overexpression with prognosis in osteosarcoma. Of the 28 evaluable reports, 23 were excluded. In the remaining five reports, the authors had difficulty with standardization of the cohorts as the reports as described above used different modalities to evaluate HER2 overexpression, different antibodies, and different criteria for the evaluation of immunohistochemistry staining. The authors conclude that HER2 positivity revealed a trend for a 1.26-fold higher risk of death, which was not statistically significant [27]. Another major confounder of the meta-analysis was the lack of standardization of the populations and the treatments across the studies.
In conclusion, interpreting HER2 expression in osteosarcoma is complicated by differences in the definition of positivity in the different studies. In most of the studies, HER2 was found to be expressed to some degree in 13%–98% of patient samples by immunohistochemistry. The HER2 gene in the majority of the studies is not amplified.
HER2 Targeted Therapies in Osteosarcoma
HER2 Directed Monoclonal Antibodies
Trastuzumab is a humanized, monoclonal antibody targeting HER2 that is FDA approved for HER2 overexpressing breast cancer as well as gastric cancer based on pivotal studies that showed improvement in outcomes for these patients [28, 29] . Other HER2-directed antibodies include pertuzumab and lapatinib. Due to prior preclinical studies showing HER2 expression in osteosarcoma along with its potential poor prognostic significance, trastuzumab was studied in a Phase 2 trial of patients with newly diagnosed metastatic osteosarcoma in combination with cytotoxic chemotherapy. Among 96 evaluable patients on study, 41 had tumors expressing HER2. All patients received the same chemotherapy backbone, and HER2-positive patients received trastuzumab concurrently with chemotherapy for 34 weeks. No difference in event-free (32% in each) or overall survival (59% in HER2 positive vs. 50% in HER2 negative) was seen between the two groups suggesting that the addition of trastuzumab to cytotoxic chemotherapy in HER2-positive patients did not provide additional clinical benefit [30]. However, trastuzumab has not been evaluated in a randomized trial in HER2-positive patients. Despite the failure of trastuzumab to improve outcomes in patients with osteosarcoma, HER2 remains as an antigen of interest, and other approaches to use this protein as a therapeutic target are being evaluated.
HER2-Specific Chimeric Antigen Receptor (CAR)-Modified T Cells
Chimeric antigen receptor-modified T cell (CAR T cell) is a form of adoptive cellular therapy that has been tremendously successful in some hematological malignancies leading to complete remission rates of greater than 80% [31]. A CD19 CAR (tisagenlecleucel) has recently been FDA approved for B-cell acute lymphoblastic leukemia. CARs directed toward antigens expressed in solid malignancies are also being developed and studied but face certain unique challenges. These include identification of an antigen that is ubiquitously expressed highly in a tumor but not in normal tissues, and immune suppressive microenvironment of many solid tumors including osteosarcoma and longevity/ persistence of CAR T cells in the host, specifically in the tumors, that would be required for sufficient activity. Researchers have continued to try to improvise CAR T-cell development to overcome some of these challenges by adding co-stimulatory molecules to first-generation CARs and other combinatorial approaches. In the case of osteosarcoma, although HER2 is not expressed ubiquitously or at very high levels, HER2 CAR T cells have been studied both in preclinical and in clinical settings as it was believed that these challenges of HER2 expression could be overcome by this adoptive therapy. Indeed, in osteosarcoma cell lines, treatment with HER2 CAR T cells induced immune responses by generation of IFN-ϒ and IL-2 with killing of target cells in HER2-specific manner. In vivo, HER2 CAR T cells led to tumor regression in tumors produced by a low HER2 expressing cell line LM7 [32]. Further, coculture with HER2 CAR T cells decreased the ability of osteosarcoma cells to form sarcospheres. This was also seen in osteosarcoma cells harvested from mouse tumors that were previously treated with HER2 CAR T cells. These data suggested that HER2 CAR T cells targeted tumor-initiating cells and could potentially be of benefit in preventing metastatic spread of the disease [33].
The first attempt to treat a patient with HER2 CAR T cells was eventful leading to fatal respiratory failure in a patient with colorectal cancer within a few minutes of infusion of cells [34]. The HER2 CAR vector was a third-generation CAR containing a single-chain variable fragment (scfv) derived from trastuzumab fused to CD8 hinge and transmembrane domains followed by CD28, 4-1BB, and CDzeta signaling domains. The cells were infused following a lympho-depleting conditioning regimen. Patient developed significant respiratory distress and pulmonary infiltrates within 15 minutes of infusion and eventually succumbed. The investigators believed that this patient had a severe cytokine storm in the lung due to reactivity with low levels of HER2 expression in lung parenchyma. Since then, three clinical trials have been completed using different HER2 CAR T constructs including one in HER2 expressing sarcomas [35,36,37]. In this study, of the 19 enrolled patients, 16 had metastatic or recurrent osteosarcoma. This HER2 CAR T cell used a different antibody clone called FRP5 which had lower HER2 affinity than trastuzumab in a second-generation CAR design. No dose-limiting toxicities were observed in this study after cells were infused without any prior lympho-depleting therapy. HER2 CAR T cells persisted for at least 6 weeks in seven of the nine evaluable patients who received greater than 106 cells/m2. Of the 16 osteosarcoma patients, 2 were not evaluable, 10 had progressive disease, 3 patients had stable disease for ≥12 weeks and subsequently underwent tumor removal and remain in remission, and 1 patient had partial response for 9 months after second infusion. The median overall survival for all 19 patients was 10.3 months (range 5.1–29.1 months). This study concluded that HER2 CAR T-cell therapy was feasible in patients with sarcoma, cells can persist for 6 weeks or longer without significant toxicities, and there was a preliminary signal of efficacy thus providing a rationale for future studies of HER2 CAR T cells with other immunomodulatory approaches in osteosarcoma [37].
Trastuzumab Deruxtecan (DS-8201)
An alternative approach to target surface proteins on cancer cells is via antibody–drug conjugates (ADCs). ADCs comprise of an antibody to a surface protein of interest such as HER2, a linker and a payload cytotoxic agent. The goal of an ADC is to be able to deliver large doses of the cytotoxic agent specifically to the malignant cells that express the antigen without exposure to normal tissues, which would not be tolerable if administered systemically. DS-8201 is one such ADC where the humanized monoclonal HER2 antibody is linked to a topoisomerase 1 inhibitor payload called DXd via a self-immolative enzymatically cleaved linker. No specific preclinical data currently exist with DS-8201 in osteosarcoma, but in other preclinical studies with adult cancer cell lines, DS-8201 showed activity against both low and high HER2-expressing cell lines [38]. A phase 1 trial of DS-8201 was recently completed in adults with advanced breast and gastric tumors. No maximum tolerated dose was reached. The most common grade 3 events were lymphopenia, neutropenia, and anemia. Three serious adverse events were reported which included febrile neutropenia, cholangitis, and intestinal perforation. Of the 23 evaluable patients, 6 had low HER2-expressing tumors. Forty-three percent (10 of 23) of the patients had an objective response, and 91% (21/ 23) achieved disease control [39]. A phase 2 clinical trial is currently under development in adolescents with recurrent HER2-positive osteosarcoma.
HER2 is one of the many antigens that are expressed on cell surface in osteosarcoma. Others include but are not limited to disialoganglioside 2 (GD2) and B7-H3 (CD276). ADC provides a unique approach to target any or many of these. However, the success of these ADCs will depend on the specificity of the target, a linker that can easily deliver and detach the drug at its cellular target as well as the potency of the cytotoxic agent being used.
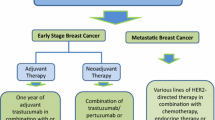
Targeting Surface Proteins
Numerous approaches are being taken to target HER2 as already described but trials targeting other surface receptors have also been conducted. As one example, the Children’s Oncology Group completed a phase 2 trial in recurrent osteosarcoma of an antibody–drug conjugate, glembatumumab vedotin, which targets the surface protein GPNMB. This leads one to consider how one should think about these targeting approaches. In targeting surface proteins , there have been several approaches utilized as depicted in Fig. 5.1. A simplified way of thinking about these approaches is considering the potency of the therapeutic agents with antibody–drug conjugates having less ability to kill protein-expressing cells as compared to the CAR T cells. This indeed may be the basis of the difference in activity observed with trastuzumab versus CAR T cells. Indeed the drug conjugates achieve some of their therapeutic index by requiring proliferation for cellular cytotoxicity by the drug component of the molecule, which is typically a micro-tubule inhibitor, topoisomerase inhibitor, or DNA damaging agent. This allows some minimization of toxicity on host cells that express the protein target. As an overly broad generalization, antibody–drug conjugates have had limited toxicity, and as such the ideal surface protein target would be expressed in all or nearly all osteosarcoma samples. Certainly, if it is expressed in a subset of patients, it would be critical for the protein expression to be on the patients who do not have disease eradication with standard treatment. If the surface protein expression is highly restricted to osteosarcoma and not essential normal tissues, as has been the case for cancer–testis antigens in the context of other malignancies, a cellular therapy approach may be more efficacious. Regardless of the targeting approach, a key consideration in the success or failure of these approaches, as illustrated by resistance to CD19 CAR T cells, is the ability of the cancer cells to survive despite down-regulation of the surface protein. Unfortunately, none of these studies have been undertaken for HER2 or other surface protein targets in osteosarcoma. Perhaps, CRISPR screening and dependency maps, which have been created to a limited extent for osteosarcoma, may help in defining what targets may be relevant.
Conclusion
HER2 is expressed in a subset of osteosarcoma samples and continues to be explored as a potential therapeutic target. Our knowledge of both the surfaceome of osteosarcoma and how to target these proteins continues to expand at a rapid pace. We remain hopeful that these approaches will overcome the stalled progress in improving the outcomes of patients with osteosarcoma.
References
Schechter AL, Stern DF, Vaidyanathan L, Decker SJ, Drebin JA, Greene MI et al (1984) The neu oncogene: an erb-B-related gene encoding a 185,000-Mr tumour antigen. Nature 312(5994):513–516
Coussens L, Yang-Feng TL, Liao YC, Chen E, Gray A, McGrath J et al (1985) Tyrosine kinase receptor with extensive homology to EGF receptor shares chromosomal location with neu oncogene. Science 230(4730):1132–1139
Lee KF, Simon H, Chen H, Bates B, Hung MC, Hauser C (1995) Requirement for neuregulin receptor erbB2 in neural and cardiac development. Nature 378(6555):394–398
Di Fiore PP, Pierce JH, Kraus MH, Segatto O, King CR, Aaronson SA (1987) erbB-2 is a potent oncogene when overexpressed in NIH/3T3 cells. Science 237(4811):178–182
Hudziak RM, Schlessinger J, Ullrich A (1987) Increased expression of the putative growth factor receptor p185HER2 causes transformation and tumorigenesis of NIH 3T3 cells. Proc Natl Acad Sci U S A 84(20):7159–7163
Guy CT, Webster MA, Schaller M, Parsons TJ, Cardiff RD, Muller WJ (1992) Expression of the neu protooncogene in the mammary epithelium of transgenic mice induces metastatic disease. Proc Natl Acad Sci U S A 89(22):10578–10582
Hughes DP, Thomas DG, Giordano TJ, Baker LH, McDonagh KT (2004) Cell surface expression of epidermal growth factor receptor and Her-2 with nuclear expression of Her-4 in primary osteosarcoma. Cancer Res 64(6):2047–2053
Hassan SE, Bekarev M, Kim MY, Lin J, Piperdi S, Gorlick R et al (2012) Cell surface receptor expression patterns in osteosarcoma. Cancer 118(3):740–749
Scotlandi K, Manara MC, Hattinger CM, Benini S, Perdichizzi S, Pasello M et al (2005) Prognostic and therapeutic relevance of HER2 expression in osteosarcoma and Ewing’s sarcoma. Eur J Cancer 41(9):1349–1361
Onda M, Matsuda S, Higaki S, Iijima T, Fukushima J, Yokokura A et al (1996) ErbB-2 expression is correlated with poor prognosis for patients with osteosarcoma. Cancer 77(1):71–78
Meyers PA, Gorlick R, Heller G, Casper E, Lane J, Huvos AG et al (1998) Intensification of preoperative chemotherapy for osteogenic sarcoma: results of the Memorial Sloan-Kettering (T12) protocol. J Clin Oncol 16(7):2452–2458
Gorlick R, Huvos AG, Heller G, Aledo A, Beardsley GP, Healey JH et al (1999) Expression of HER2/erbB-2 correlates with survival in osteosarcoma. J Clin Oncol 17(9):2781–2788
Zhou H, Randall RL, Brothman AR, Maxwell T, Coffin CM, Goldsby RE (2003) Her-2/neu expression in osteosarcoma increases risk of lung metastasis and can be associated with gene amplification. J Pediatr Hematol Oncol 25(1):27–32
Fellenberg J, Krauthoff A, Pollandt K, Delling G, Parsch D (2004) Evaluation of the predictive value of Her-2/neu gene expression on osteosarcoma therapy in laser-microdissected paraffin-embedded tissue. Lab Investig 84(1):113–121
Ferrari S, Bertoni F, Zanella L, Setola E, Bacchini P, Alberghini M et al (2004) Evaluation of P-glycoprotein, HER-2/ErbB-2, p53, and Bcl-2 in primary tumor and metachronous lung metastases in patients with high-grade osteosarcoma. Cancer 100(9):1936–1942
Maitra A, Wanzer D, Weinberg AG, Ashfaq R (2001) Amplification of the HER-2/neu oncogene is uncommon in pediatric osteosarcomas. Cancer 92(3):677–683
Kilpatrick SE, Geisinger KR, King TS, Sciarrotta J, Ward WG, Gold SH et al (2001) Clinicopathologic analysis of HER-2/neu immunoexpression among various histologic subtypes and grades of osteosarcoma. Mod Pathol 14(12):1277–1283
Thomas DG, Giordano TJ, Sanders D, Biermann JS, Baker L (2002) Absence of HER2/neu gene expression in osteosarcoma and skeletal Ewing’s sarcoma. Clin Cancer Res 8(3):788–793
Anninga JK, van de Vijver MJ, Cleton-Jansen AM, Kristel PM, Taminiau AH, Nooij M et al (2004) Overexpression of the HER-2 oncogene does not play a role in high-grade osteosarcomas. Eur J Cancer 40(7):963–970
Tsai JY, Aviv H, Benevenia J, Chang VT, Patterson F, Aisner S et al (2004) HER-2/neu and p53 in osteosarcoma: an immunohistochemical and fluorescence in situ hybridization analysis. Cancer Investig 22(1):16–24
Somers GR, Ho M, Zielenska M, Squire JA, Thorner PS (2005) HER2 amplification and overexpression is not present in pediatric osteosarcoma: a tissue microarray study. Pediatr Dev Pathol 8(5):525–532
Willmore-Payne C, Holden JA, Zhou H, Gupta D, Hirschowitz S, Wittwer CT et al (2006) Evaluation of Her-2/neu gene status in osteosarcoma by fluorescence in situ hybridization and multiplex and monoplex polymerase chain reactions. Arch Pathol Lab Med 130(5):691–698
Bakhshi S, Gupta A, Sharma MC, Khan SA, Rastogi S (2009) Her-2/neu, p-53, and their coexpression in osteosarcoma. J Pediatr Hematol Oncol 31(4):245–251
Gorlick S, Barkauskas DA, Krailo M, Piperdi S, Sowers R, Gill J et al (2014) HER-2 expression is not prognostic in osteosarcoma; a Children’s Oncology Group prospective biology study. Pediatr Blood Cancer 61(9):1558–1564
Akatsuka T, Wada T, Kokai Y, Kawaguchi S, Isu K, Yamashiro K et al (2002) ErbB2 expression is correlated with increased survival of patients with osteosarcoma. Cancer 94(5):1397–1404
Akatsuka T, Wada T, Kokai Y, Sawada N, Yamawaki S, Ishii S (2001) Loss of ErbB2 expression in pulmonary metastatic lesions in osteosarcoma. Oncology 60(4):361–366
Li YG, Geng X (2010) A meta-analysis on the association of HER-2 overexpression with prognosis in human osteosarcoma. Eur J Cancer Care (Engl) 19(3):313–316
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344(11):783–792
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A et al (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376(9742):687–697
Ebb D, Meyers P, Grier H, Bernstein M, Gorlick R, Lipshultz SE et al (2012) Phase II trial of trastuzumab in combination with cytotoxic chemotherapy for treatment of metastatic osteosarcoma with human epidermal growth factor receptor 2 overexpression: a report from the children’s oncology group. J Clin Oncol 30(20):2545–2551
Park JH, Geyer MB, Brentjens RJ (2016) CD19-targeted CAR T-cell therapeutics for hematologic malignancies: interpreting clinical outcomes to date. Blood 127(26):3312–3320
Ahmed N, Salsman VS, Yvon E, Louis CU, Perlaky L, Wels WS et al (2009) Immunotherapy for osteosarcoma: genetic modification of T cells overcomes low levels of tumor antigen expression. Mol Ther 17(10):1779–1787
Rainusso N, Brawley VS, Ghazi A, Hicks MJ, Gottschalk S, Rosen JM et al (2012) Immunotherapy targeting HER2 with genetically modified T cells eliminates tumor-initiating cells in osteosarcoma. Cancer Gene Ther 19(3):212–217
Morgan RA, Yang JC, Kitano M, Dudley ME, Laurencot CM, Rosenberg SA (2010) Case report of a serious adverse event following the administration of T cells transduced with a chimeric antigen receptor recognizing ERBB2. Mol Ther 18(4):843–851
Feng K, Liu Y, Guo Y, Qiu J, Wu Z, Dai H et al (2018) Phase I study of chimeric antigen receptor modified T cells in treating HER2-positive advanced biliary tract cancers and pancreatic cancers. Protein Cell 9(10):838–847
Ahmed N, Brawley V, Hegde M, Bielamowicz K, Kalra M, Landi D et al (2017) HER2-specific chimeric antigen receptor-modified virus-specific T cells for progressive glioblastoma: a phase 1 dose-escalation trial. JAMA Oncol 3(8):1094–1101
Ahmed N, Brawley VS, Hegde M, Robertson C, Ghazi A, Gerken C et al (2015) Human epidermal growth factor receptor 2 (HER2) -specific chimeric antigen receptor-modified T cells for the immunotherapy of HER2-positive sarcoma. J Clin Oncol 33(15):1688–1696
Takegawa N, Nonagase Y, Yonesaka K, Sakai K, Maenishi O, Ogitani Y et al (2017) DS-8201a, a new HER2-targeting antibody-drug conjugate incorporating a novel DNA topoisomerase I inhibitor, overcomes HER2-positive gastric cancer T-DM1 resistance. Int J Cancer 141(8):1682–1689
Doi T, Shitara K, Naito Y, Shimomura A, Fujiwara Y, Yonemori K et al (2017) Safety, pharmacokinetics, and antitumour activity of trastuzumab deruxtecan (DS-8201), a HER2-targeting antibody-drug conjugate, in patients with advanced breast and gastric or gastro-oesophageal tumours: a phase 1 dose-escalation study. Lancet Oncol 18(11):1512–1522
Abdou AG, Kandil M, Asaad NY, Dawoud MM, Shahin AA, Abd Eldayem AF (2016) The prognostic role of Ezrin and HER2/neu expression in osteosarcoma. Appl Immunohistochem Mol Morphol 24(5):355–363
Ma Q, Zhou Y, Ma B, Chen X, Wen Y, Liu Y et al (2012) The clinical value of CXCR4, HER2 and CD44 in human osteosarcoma: a pilot study. Oncol Lett 3(4):797–801
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gill, J., Hingorani, P., Roth, M., Gorlick, R. (2020). HER2-Targeted Therapy in Osteosarcoma. In: Kleinerman, E.S., Gorlick, R. (eds) Current Advances in Osteosarcoma . Advances in Experimental Medicine and Biology, vol 1257. Springer, Cham. https://doi.org/10.1007/978-3-030-43032-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-43032-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43031-3
Online ISBN: 978-3-030-43032-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)