Abstract
This chapter discusses the pressing need for knowledge integration in the development of resilient healthcare human capital that will be able to embrace the implementation of forthcoming healthcare innovations. The chapter investigates the current challenges facing the UAE’s healthcare system and explores its preparedness—especially that of its human capital—for the government’s healthcare innovation strategy. Implementation of innovations will require a sophisticated approach of continuous improvement, carefully crafted change management procedures, and, above all, well-trained and competent human capital. The author suggests that outsourcing technologies and experts will not lead to sustainability of healthcare innovation. Professional research and development is pivotal for well-established and sustainable innovation because abrupt implementation of the technologies can lead to generation of fear and resistance among the employees.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Innovation benchmarking
- UAE Vision 2021
- Healthcare providers
- Emerging technologies
- Innovation
- Knowledge management
- Resilience
Since 2009, with the construction of worlds` tallest building Burj Khalifa, UAE has earned the reputation of being the world’s best destination for tourism. Since 2014, the UAE has been preparing for Expo 2020 and the government has announced its vision to become one of the top ten innovative countries in the world by the year 2021 (UAE Government portal, 2019). Out of the seven targeted categories for innovation, the health sector is one. Healthcare innovation strategy is meant to promote advanced technologies and to stimulate the growth of biotechnology and pharmaceutical industries and medical research. The government of the UAE has set the agenda, aiming at building a world-class healthcare system. The mandate is to achieve this objective by enhancing the healthcare system’s readiness to deal with epidemics and health-related risks. In the fiscal year 2017, a budget of AED 48.7 billion was allocated for innovation, out of which AED 4.2 billion (8.6%) was granted to healthcare innovation and protection of society (MOF, 2019).
According to global innovation index (GII) 2017, the UAE was ranked 35th among 127 countries, but in 2018 the ranking dropped to 38 (GII, 2017). However, among 129 participating nations, The UAE was ranked first in the Arab World and 36th globally in 2019, jumping two positions up from last year. This improvement in ranking is mainly due to high performance in the pillars of human capital and R&D (GII, 2019). As mentioned earlier, the government is aiming to be among the top ten innovative nations by 2021.
Upon close observation, it is noted that UAE healthcare has shown minimal progress toward the adoption and implementation of healthcare innovation since 2014. Although many conferences and seminars have taken place in the region, the practical implication of healthcare innovation strategies has moved at a slow pace. According to Dubai Health Authority (DHA) newsroom updates, (2018), “Dubai Health Authority (DHA) is working with private companies from across the world to implement cutting-edge technologies to provide patients with the very best standards of care”. The local authorities are still in the negotiation process with companies and international regulatory authorities to pave the way for cutting-edge technology in UAE healthcare, like robotic surgeries, using artificial intelligence for early detection and prevention of diseases (see DHA, 2019).
This chapter will explore the current challenges faced by the UAE healthcare system’s readiness and preparedness in terms of HRM policies and the readiness of Health Care Professionals (HCPs) to adopt and adapt to upcoming healthcare innovation strategies. These factors are discussed in detail to explore the area that is most challenging for healthcare innovation strategy in the UAE, namely, adoptability and adaptability of health innovations by HCPs. Recommendations are provided based on international best practices to accommodate the anticipated innovation strategies by HCPs.
Currently, this is an under-researched topic in this part of the world. Although, the UAE government and authorities are very much focused on the implementation of healthcare innovative strategies, there is limitation of research and data collection in this domain. Implementation of healthcare innovation strategies require a sophisticated approach of continuous improvement and carefully crafted change management procedures, which ultimately leads to resilience. If innovation strategies are imposed superficially, then desired outcomes cannot be achieved.
Methodology
For this exploratory research, which provides insights on and measures the level of preparedness for innovation strategy among the current UAE healthcare practitioners, a methodology of qualitative research is adopted, taking into account secondary data collected through extensive literature review. The author also looked into the current policies and strategies of health authorities (HAAD, DHA, DHCC and MOH) in the UAE to assess the resilience and preparedness of the policies for advances in the field of healthcare innovation. However, secondary data is analyzed to assess the readiness for healthcare innovation strategies so challenges and factors can be identified and discussed.
Secondary data is collected by systematic literature review of literature sources, published industry reports, peer-reviewed articles and information from the websites of the government and healthcare industry in the UAE. Utilization of secondary data is beneficial because it can be helpful for data analysis and reanalysis, in the process of inquiry and to combine information from various data sets (Johnston, 2017).
Initially, the plan was to conduct an online survey, which might have been included briefly in this study. The survey was meant for the evaluation of healthcare services delivered at tertiary care hospitals in Dubai, which are providing a complete range of services under one roof for the healthcare consumers. This primary data would have helped in the assessment of healthcare resilience and current quality of services. The respondents would have been doctors, nurses and healthcare administrators. However, due to legal aspects related to healthcare authorities in Dubai, this survey was called off.
Innovation
Once a forbidden word, used for accusation and humiliation (Heylin, 1637), innovation has recently become the catchword of this era. The word took its current form back in fifteenth century, arising from Latin roots. It is derived from a combination of two words, ‘in’ meaning into and ‘novare’ meaning introducing novelty. W. Rupert Maclaurin can be considered the first person to explicitly define innovation: “When an invention is introduced commercially as a new or improved product or process, it becomes an innovation” (Maclaurin, 1953). During the seventeenth and eighteenth centuries, innovators consciously and cautiously kept on denying their innovations to avoid the label of ‘evil character’ (Godin, 2012). An in-depth study of the history of this word revealed that it has been misunderstood as antisocial, renovation, invention, imitation and improvement.
The twentieth century brought not only better meanings to this word but also a better understanding of its role in the development of an economy. In 1967, the US Department of Commerce established that innovation is a “process by which an invention or idea is translated into the economy” (US Department of Commerce, 1967: 2). Europe recognized the urge for policies to stimulate technological innovation by stating “The health of the Western European countries very much depends on their international competitiveness. Such competitiveness increasingly requires a relative technical advance in certain science intensive industries” (OECD, 1966: 12).
The words ‘innovation’ and ‘emerging technologies’ have become the buzzwords of the twenty-first century but still there is lack of clear understanding of the effects of disruptive technologies on the outcomes of firms, employees and competition (Hang, Garnsey, & Ruan, 2015). There is extensive literature available for the development and advancement of emerging technologies, yet the adaptability and adoptability of these technologies on organizational and individual levels remain under-explored (Curado et al., 2018; Liu, Ying, & Wu, 2017).
In the 1970s, Quentin Skinner put forward the idea that “words are markers of our social understanding of the world, and that the emergence of new words is a marker of changes in society’s values” (Skinner, 1978, 1988). The word ‘innovation’ is an excessively used word these days and it is relevant to international competitiveness, the world economy, competitive advantage of a company, growth sustainability or out of the box creativity. In simple words, ‘innovation’ means doing things differently yet efficiently. In addition, “Innovation can be explained as a new idea, product, device or novelty. It is a mind-set, a way of thinking beyond the present and into the future” (Stenberg, 2017). To achieve sustainable economic growth and gain competitive advantage for both companies and nations, innovation is considered a central driver (Chen, 2017).
Baregheh, Rowley and Sambrook (2009) suggested a complete and multistage process definition of innovation: “Innovation is the multi-stage process whereby organizations transform ideas into new/improved products, service or processes, in order to advance, compete and differentiate themselves successfully in their marketplace”. Fri, Pehrsson and Søilen (2013) suggested, “Innovation is an activity which companies solves problems by combining knowledge”. However, Huebner and Fichtel (2015) argued that innovation is “a novel solution to an old problem”. To find a new solution to an old problem, individuals must stop practicing old strategies and must behave flexibly. Sardana (2016) explained, “Innovation was one key component to growth because it creates revenues which in turn creates profitability”. Hence, innovation plays a vital role in the sustainability of an economy. Länsisalmi, Kivimäki, Aalto and Ruoranen (2006) captured the three mainly significant yet distinctive characteristic of innovation, which are: (a) novelty, (b) a function element and (c) a proposed advantage.
Considering above-mentioned definitions, the word ‘innovation’ can be linked to creativity, profitability and sustainability. In recent times, innovation has become inevitable for sustainable survival. In the business world and for companies, the word ‘innovation’ is often used for something risky, costly and time consuming (Costello & Prohaska, 2013). Whether it is a country, an organization, an educational institute, the technology industry, transportation, manufacturing, retail, trade, construction, real state, agriculture, banks, pharmaceutical companies or health sciences, innovation plays an imperative role. These days, innovation has become a key ingredient and companies have to continuously deal with the creation of new products and services to manage global competitiveness (Farniha et al., 2016). To sum up, ‘innovation is novelty, profitability and sustainability’ (Fig. 11.1).
Healthcare Innovation and Global Trends
When it comes to healthcare, there is a need for further elaboration of the term ‘innovation’. ‘Healthcare innovation’ can be defined as “the introduction of a new concept, idea, service, process, or product aimed at improving treatment, diagnosis, education, outreach, prevention and research, and with the long term goals of improving quality, safety, outcomes, efficiency and costs” (Omachonu & Einspruch, 2010b).
Innovations and the emerging technologies of today will shape the future of the world tomorrow. Robot-assisted surgery (RAS) using 5G technology is a bright reality of the current era. Healthcare systems in the twenty-first century are experiencing certain challenges in the introduction of innovations and the implementation of emerging technologies and are aspiring to look for redesigned and modernized approaches. These challenges are not limited to the development and improvisation of new technologies but are more prevalent in the area of adoptability and adaptability of these technologies.
There is an enormous need to study and evaluate the influence of these emerging technologies on the human capital of the healthcare industry, to understand the perspectives to build corresponding HRM policies and to develop a competent workface to embrace the impact of forthcoming technologies and innovation in healthcare. Some common examples of today’s emerging technologies are found in the fields of nanotechnology, biotechnology, genetic technology, neurotechnology, machine learning and other advances in computing. The rapid development and availability of these technologies is associated with uncertainties in terms of, for example, risks and benefits and the effects of these technologies on the society (Nelson & Gorichanaz, 2019).
Grisot, Vassilakopoulou and Aanestad (2018) have discussed two case studies from Norwegian Healthcare and suggested a deeper need of ‘sociotechnical sensibility’ for the translation of emerging technologies and innovations into healthcare. So far, the widely adopted digitization in healthcare systems is Electronic Patient Record (ERP), which still is in the nascent stage, and did not happen without internal resistances and external pressures (Adler-Milstein et al., 2015). An Estonian firm is using blockchain for the management of ERP and providing services to healthcare entities (Angraal, Krumholz, & Schulz, 2017). Additionally, the latest products with digital information, nanotechnology, semiconductor and genetic engineering are transforming healthcare, creating previous statements and assumptions unacceptable and making unexpected predictions for innovation and development of presented procedures (Sahoo, Parveen, & Panda, 2007).
There is an increased demand on healthcare deliverance organizations all over the world (Starfield, 2000). Quality healthcare is the most important aspect through which individuals, especially patients, recognize the meaning of quality in their life. In some countries, healthcare industry is a part of the country’s national identity. It is appropriate to consider that it is time for a new explanation in every feature of the healthcare system, where every industry and stakeholders from governments to ventures to individuals are being involved in improving and developing healthcare through innovation. Globally, most of the healthcare industries are facing the same issues or challenges (Scott, 2006).
The distribution of innovation has become a foremost challenge in every industry, together with healthcare (Berwick, 2003). In recent times, there has been an increase in innovation in the healthcare industry. This is intended to improve life expectancy, quality of life, investigative treatment alternatives, in addition to the competence and cost efficiency of the healthcare structure (Varkey, Horne, & Bennet, 2008). Thus, using innovations in the progression using innovations in the progression of care deliverance (Varkey & Athyal, 2005), medications and surgical intercessions (Varkey et al., 2008). Healthcare has become the last of the foremost supply-driven industries (IOM, 2001).
In healthcare, abrupt introduction and implementation of the innovations may lead to permanent discomfort, disability and sometimes death (Länsisalmi et al., 2006). This, along with clinicians’ propensity to protect their patients’ independence and status, can endorse a culture of responsibility and confidentiality that restrain organizational learning and new production of innovations (Huntington, Gilliam, & Rosen, 2000). Moreover, innovative practices related to patient care in healthcare industries are traditionally examined carefully in an early developmental stage, so that the potential risks of harmful innovations can be avoided (Faulkner & Kent, 2001).
Since the advent of 21st century, the world has been experiencing fast-paced technological revolution. Patients have become an essential and active stakeholder in healthcare. They demand simplicity in getting information, easy access to their health records and better access to healthcare services, and they fix appointments according to their convenience and prefer to be equally involved. The arrival of innovative consumer technology is initiating even more challenges, or making the older technologies extinct. The technology encourages greater power to be given to the patient. Patients insist on transparency and simplicity of data and processes when it comes to healthcare treatments (Picker, 2000). Due to accessibility of evidence-based medicine, they want to receive the latest medicine or clinical treatment; of course, they also do not prefer to be in surgical waiting lists or eagerly request to get the option of going private irrespective of the cost incurred (Pfeffer & Sutton, 2006).
To fulfill the expectations of the patient, and to begin the evolution of healthcare to a demand-determined form, some of the world’s foremost and important hospitals are placing patient confidently at the midpoint of everything they do. For instance, Cleveland Clinic in Ohio established a clear mission to improve the experiences that a patient might be expected to receive, with a board-level Chief Experience Officer leading and handling the Office of the Patient Experience (Mangione et al., 2007). According to the hospital’s website, the mission is to “ensure care is consistently patient-centered by partnering with caregivers to exceed the expectations of patients and their families”. Cleveland Clinic, alongside a handful of other revolutionary hospitals, has always been an innovative and state-of-art technological user in patient care, and it will be interesting to see how many other hospitals are trying to attempt and make comparable preparations (McGlynn et al., 2003).
In general, from the development of a new medical device or enforcement of a new health policy, innovations are embedded in organizational networks (Lewis & Smith, 2014). Self-effort and persistence have a significant direct effect on innovation performance (Bandura, 1977; Mumtaz & Parahoo, 2019). Venkatesh, Morris, Davis and Davis (2003) have recommended the analytical use of ‘Unified Theory of Acceptance and Use of Technology’ (UTAUT), which is based on four precursors of the acceptance of information systems. These precursors are extracted from fourteen initial constructs from eight acceptance theories, namely, technology acceptance model (TAM), theory of reasoned action, theory of planned behavior (TPB), combined TAM and TPB model of PC utilization, diffusion of innovation, motivational model and social cognitive theory (Taherdoost, 2018).
Nowadays, life expectancy has improved and the average age of morbidity and mortality is declining (Blyth et al., 2019). This is due to the advances in understanding and recognizing the causes of diseases and resulting improvements in analytical techniques and cure. Average life expectancy in the OECD countries (Organisation for Economic Co-operation and Development) has now reached 80 years and continues to extend. People are living longer, even those with chronic diseases. This is an outcome of effective and efficient healthcare delivery.
Health Innovation Process and Its Stakeholders
Innovation in healthcare continues to be a powerful motivator in the exercise to control cost and steady healthcare quality. It is considered to be a significant element of a business in order to ensure productivity and competitive endurance (Christensen, 1997). The procedure of implementation of the innovation is equally multidimensional, apart from the industry itself, in which the innovative processes are being practiced. Implementation of healthcare innovation is multi-part and multi-dimensional involving many actors an factors, whereas progression of the innovation happens distinctly. The factors influencing the deployment of innovation into healthcare systems can be divided into three levels, namely, individual (micro), organizational (meso) and national (macro) (Kim & Von Glinow, 2017). Herzlinger (2006) has pointed out at the six force that can accelerate or inhabit efforts at innovation, namely, industry players; funding; public policy; technology; customers; and accountability.
Innovation in the healthcare industry comes with unique and exclusive challenges. The confrontations and challenges of implementation and penetration of innovations in the healthcare systems at multiple levels (i.e., government, organizational, human capital and consumer engagement) demand an ambidextrous approach. The implementation of innovations effectively depends on both the adoption of the technology and the modification of current processes and/or services to allow optimum adoptability and adaptability (Savory & Fortune, 2015). Any challenge to recognizing the progression of applying innovation in healthcare essentially starts with a thorough analysis of its challenges. Birkinshaw and Gupta (2013) recommend a multiple-level span to address critical innovation challenges through the development of innovation culture, building innovation capacity and involvement of top management. According to Omachonu and Einspruch (2010a, 2010b), there are five key stakeholders anticipating the innovation process in healthcare industries, and each one has its exclusive and purposeful requirements and expectations:: (1) physicians and other care providers, who are expected to enhance clinical results, improve diagnosis and ensure patient safety and proper handling of treatments; (2) patients, who expect to have better experience at a health facility, like less waiting time and prefer elimination of delays to the treatment so they can have improved physiological comfort; (3) organizations, who are required to develop swift internal operations, improve the cost effectiveness of treatments and enhance healthcare productivity thus achieving better quality and outcomes; (4) innovator companies, who are expected to increase profitability and provide enhanced results and (5) regulatory agencies, who are excepted to establish polices to reduce perceived risk and strengthen patient safety.
A systems approach to healthcare innovation has four general stages: identification, description, alteration and implementation (Asch, Terwiesch, Mahoney, & Rosin, 2014; Kaplan et al., 2013). In the 1980s, Fennell and Warnecke (1988) suggested that healthcare institutions may find the adaptation of a new technology beneficial due to the general competitive climate, to avoid malpractice suits, or to gain status. Christensen, Bohmer and Kenagy (2000) have expressed the pressing need to look into the enablers for the emerging disruptive innovations in the healthcare systems. During the last decade, technological innovations in healthcare have been accepted not only as a source of value generation but also as a source of profitability (Garber et al., 2014).
Meyer (2019) argued that the role of organization is pivotal for a detailed understanding of the emergence of envisioned futures. Omachonu and Einspruch (2010a) and Grose (2008) dispute the fact that massive savings can be realized by the additional and improved usage of emerging technologies like electronic record-keeping, utilizing software and automated workflows that can perceive inaccuracies and resolve matters in a speedy manner. The focus of healthcare research has shifted from molecular and tissue biology. The shift is towards health-related technologies to improve the patient care and in many countries, is being considered primarily under economy and commerce agenda (Tarkkala, Helén, & Snell, 2019).
Conceptual Model
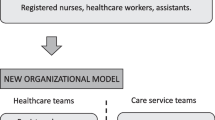
Based on the above discussion and literature review, a model is developed firstly to identify the active participants or actors or stakeholders of the healthcare innovation and then to comprehend the inter-relationship among them. Figure 11.2 shows this network of participants. Healthcare is complex as it involves a very wide variety of participants with variant levels of knowledge and authority. Successful establishment and integration of innovation in this field is possible only through the development of a strong communication network, which overcomes the gap among the actors (Proksch et al., 2019).
Healthcare is a unique enterprise, which involves multiple actors to complete a routine task on a daily basis. It will be interesting to delve into the multilevel challenges (i.e., government level, organizational level and HRM policies, human capital level and consumer engagement level) of implementation of innovations in healthcare, but this chapter will explore the human capital factor (micro level) alone. According to Fig. 11.2, initiation of implementation of innovation will start at the macro level, but it will trickle down to the micro level and result in fostering and implementation. As this research is conducted in the context of the UAE and its healthcare system, which is at the cusp of health innovation (Gulf News, 2019), the adoptability and adaptability of innovations by HCPs are of utmost importance.
Role of Human Capital in Healthcare Innovation
Human capital is the stock of skills that the labor force possesses which results in economic value (Goldin, 2016). Although an institutional role is played by the government to provide incentives and regulatory support for innovative strategies (Watkins, Papaioannou, Mugwagwa, & Kale, 2015), physicians and nurses are the frontliners of the healthcare industry. Organizational polices, culture and decisions can influence healthcare innovation strategies (Moullin, Sabater-Hernández, Fernandez-Llimos, & Benrimoj, 2015). With appropriate controls and leveraging of human capital in the healthcare industry, innovation strategies can be adopted faster (Prajogo & Oke, 2016) and lead to sustainable development (Cavicchi, 2017).
According to Munjal and Kundu (2017), the role of human capital in the implementation and adoption of innovation is complex and consists of multiple levels of analysis. This approach of authors, leads to opening of new arena of discussion that the role of human capital in the fostering of innovation itself is a multilevel process. An in-depth analysis of this one stakeholder, human capital, demands multifold research. Hence, this study will focus on the role of human capital in the implementation of innovation into the healthcare systems.
It is interesting to note that the term ‘human capital’ was not in use in the English language until almost half of the twentieth century. It was only in the late 1950s that the word came into practice and in the 1990s that it was extensively used in the literature (Goldin, 2016). During the early 1960s two scholars defined human capital as the set of knowledge, skills, competencies and abilities that are embodied in individuals and which individuals acquire over time, through training, education, work experience, healthcare and relocation (Becker, 1964; Schultz, 1961).
Health Care Professionals (HCP) are continuously facing the challenges of increasing costs and disease burden. Innovation has developed into more than just a cost-saving approach and strategy, and it is currently significant to the sustainability of the healthcare system. Hospitals are known and being categorized as service organizations; health authorities, groups of private hospitals and governments are concentrating on two under-utilized forces for accumulating significance to healthcare: obtaining innovation and creating more innovative procurement performance.
Meeting the challenges of new technology implementation will require experimentation, dialogue and continuous monitoring of the change (Schartinger et al., 2015). Many current researches have documented that health technology development often presents the challenge of poor value alignment between supply-side and demand-side (Greenhalgh, Fahy, & Shaw, 2018; Lehoux, Miller, Daudelin, & Denis, 2017; Markiewicz, Van Til, & IJzerman, 2014). Hence, it is crucial to involve medical experts as a stakeholder during the development of medical technologies (Anwar & Prasad, 2018), because acceptance and adaptability by the professional staff can be considered as the single most important determinant that will decide the fate of a new technology (Gheorghiu & Ratchford, 2015; Pols, 2012; Taylor et al., 2015; Wade, Eliott, & Hiller, 2014).
The worldwide scarcity of healthcare human capital such as healthcare providers and other essential practitioners promotes progress in the case of special treatments and requires fostering of innovative processes and technologies in healthcare. Under this situation, it is forecasted that the withdrawal and elimination of existing personnel within the next ten years will be intensified (Kivisaari et al., 2004; Warne & McAndrew, 2004). However, with the advancement in the technologies, automation of processes and improvisation of the procedures and practices in healthcare, human capital such as nurses and doctors are also facing difficulties in accepting, adopting and adapting to innovative technological systems.
As regards the present medical practices, quite a few researchers have pointed out that it is complicated to modify the performance of clinicians (Greco & Eisenberg, 1993) as well as of healthcare organizations (Shortell, Bennett, and Byck, 1995; Shortell et al., 2001). The acceptance and application of healthcare innovations is frequently regulated by the government and laws, in order to make changes over time (Faulkner & Kent, 2001).
Sustainable human resource management, described as the “adoption of HRM strategies and practices that enable the achievement of financial, social and ecological goals, with an impact inside and outside of the organization and over a long-term time horizon while controlling for unintended side effects and negative feedback” (Ehnert et al., 2016, p: 90). Lin, Qian, Li and Chen (2018) suggested that HRM practices must transcend the understanding of employees’ strengths and focus on enhancing employees’ capabilities and maintaining their wellness and prosperity. Many researchers have considered organizational culture as a key driver of innovation (e.g., Škerlavaj, Song, & Lee, 2010; Uzkurt, Kumar, Semih Kimzan, & Eminoğlu, 2013; Zhu & Engels, 2014). In addition, Hogan and Coote (2014) suggested that ‘Schein’s model’ explains cultural processes that support organizational innovation. Similarly, Kalyar and Rafi (2013) found a strong relationship between organizational learning culture and the innovativeness of a firm.
The fact that work attitude of medical and technical workers is different can act as a hindrance in finding solutions for medical-related problems and the adaptation of new technologies (Anwar & Prasad, 2018). The transitions approach for a new technology demands taking the interests and perspectives of stakeholders into account. It is interesting to note that healthcare professionals are underestimated as facilitators of technology; however, technology developers should consider them as a stakeholder of the emergent technology (Saborowski & Kollak, 2015). Jacobs et al. (2015) quantitatively proved that the perceptions of implementation climate (physicians’ perceptions) directly affect the implementation effectiveness in healthcare industry.
Various innovation progresses in healthcare have been set off by the healthcare stakeholders, such as patients themselves, patient support groups, healthcare organizations, medical doctors and physicians, and other healthcare experts (Omachonu & Einspruch, 2010a, 2010b). In some instances, the lead can be provided by the government in an attempt to moderate healthcare challenges faced during the transformation phase by the healthcare industries.
Distribution of innovations has become a foremost challenge in every industry, including healthcare (Berwick, 2003). The International Council of Nurses (ICN, 2018) has introduced a website intended as a platform for innovations in nursing and other human capital areas in healthcare industries. The ICN Innovations Database is a resource that is web-based and has been designed to smoothen the progress of spreading the usage of innovation in the human capital sector of healthcare globally.
The UAE healthcare industry is yet to find an innovative way to offer a seamless range of innovative technologies or innovative methods to its human capital and at the same time make it easier for patients to adapt to these innovations. This can lead the patient evolution among healthcare providers beginning from presentation of their problem to diagnosis to treatment and the end process of follow-up. Gaps in the permanence of healthcare providers threaten a patient’s comfort and well-being and initiate possible unfavorable events (Asahi, 2011).
Innovation and Healthcare Providers (HCP) Resilience
“Resilience is a key to enhancing quality of care, quality of caring, and sustainability of the health care workforce” (Epstein & Krasner, 2013, p. 301). Resilience is a concept that has been well accepted and practiced in other high-risk industries and has recently become a new approach in healthcare industry too. It is a key concept in human factors that deserves consideration in healthcare as well. As noted, organizational resilience is the main contributor for the drive of innovation.
It is important to recognize the internal process that innovation can bring to healthcare organizations such as a hospital, human capital and even patients. These organizations in general do not have the comfort of an enormous R&D department and so must depend on the unrefined talent and creativity of internal personnel and human capital of healthcare (Swan et al., 2016).
Resilience focuses on how and what HCPs can learn from successes and error avoidance rather than focusing on a basic reactive search for ‘causes’.
Resilience is the capacity to respond to stressful situations in a positive manner to achieve goals at minimal psychological and physical cost; resilient individuals “bounce back” after challenges while also growing stronger (Epstein & Krasner, 2013). Resilience is all about how individuals, teams and organizations monitor, adapt to and act on failures in high-risk situations; this is why it is an appropriate match for healthcare industry (Jeffcott, Ibrahim & Cameron, 2009).
To identify resilience in healthcare, especially in healthcare human capital, it is essential to first define the term in the healthcare context. Resilience has been conceptualized in diverse ways and is being used in a variety of disciplines. In healthcare treatment research, the word ‘resilience’ is often purposely connected to the professional and specialized challenges that human capital such as doctors, nurses and other healthcare personnel experience, and is observed as a personal ability that facilitates specialists, nurses, doctors and other healthcare personnel to deal with the demands of the workplace (Hart et al., 2014).
In terms of a more psychological approach, the expansion of psychological procedures to quantify resilience, in addition, reproduces a variety of definitions. The Connor-Davidson Resilience Scale (Connor 2003) consists of twenty-five items that review a variety of aspects that can influence resilience, which include self-esteem, adaptability, commitment, logic of control, and health and comedy. This instrument can be practical because considering what contributes toward resilience can facilitate the recognition of methods to develop it.
Another implementation is the Brief Resilience Scale (Smith et al., 2008), which is a technique to measure resilience particularly as an individual’s capability to recover from stress, as against measuring the aspects that possibly will contribute to resilience. Reciprocally, the definition stated from Hart et al. (2014) and the psychological conceptualizations of resilience were not successful in reproducing the complexity and difficulty of resilience and the broader frameworks that can influence it. Masten (2015) described resilience as the capability to completely and effectively adapt to demanding and tough circumstances or difficulties.
Discussion and Analysis of Findings
The federal health authority of the UAE is the Ministry of Health and Prevention (MoHP), which serves to provide comprehensive healthcare to all citizens and residents of the country. Since 2007, due to the subsequent establishment of individual emirate-based healthcare authorities by Abu Dhabi and Dubai, the MoHP has shifted its focus to the northern emirates of Sharjah, Ajman, Umm Al Quwain, Ras Al Khaimah and Fujairah (UAE Government portal, 2019).
Previously known as the General Authority of Health Services for the Emirate of Abu Dhabi, the Health Authority of Abu Dhabi (HAAD) was established to regulate both the public centers and private healthcare sector. HAAD is responsible for healthcare policies, laws, regulations, inspections and audits in the emirate of Abu Dhabi. This authority currently manages forty-six (46) primary healthcare centers, twelve (12) hospitals (community and general), four (4) specialized centers and three (3) dental centers in the public sector and more than eight hundred healthcare facilities in the private sector in Abu Dhabi (HAAD, 2019).
Dubai Health Authority (DHA) is aligned with ‘Dubai Strategic Plan 2015’ launched by H.H. Sheikh Mohammed bin Rashid Al Maktoum. As a direct translation of the objectives of the strategic plan, the authority is determined to deliver an accessible, effective and integrated healthcare system, protect public health and improve the quality of life in Dubai.
Currently, DHA oversees 38 hospitals, 4 fertility centers, 34 one-day-surgery centers, 1,624 specialized and general medical complexes, 82 dental treatment centers and laboratories, 868 pharmacies and 38 health examination and house nursing facilities. There are more than 36,055 licensed physicians serving the emirate of Dubai in both private and public sectors (DHA, 2019).
According to statistics released by Federal Statistics and Competitive Authority there are 36 government hospitals in the UAE, employing 6504 physicians and 16,547 nurses. However, the private sector has 79 hospitals, employing 10,165 physicians and 16,882 nurses. In the past few years, the UAE has launched a number of initiatives to promote innovation in the healthcare sector (http://fcsa.gov.ae).
Gaps in healthcare and challenges in implementing innovation and creating resilience are evidences that the human capital in healthcare system is not capable of responding with adequate output to meet the demand. Whether, or how, a system acts to fill such gaps in healthcare industry indicates its resilience. Manifestations of gap-filling adaptations, such as clinician programs and development of equipment plan, specify classes of interruption or demands and foundation of resilience that are at hand to help implement and accommodate demands for having innovation in healthcare and creating an atmosphere for human capital to adopt.
The UAE’s healthcare industry is at the cusp of health innovation. Automation, artificial intelligence and nanotechnology are being introduced in the UAE healthcare system (Gulf News, 2019). The local bodies are collaborating with international health authorities to institute cutting-edge technologies in the country. The government is playing a substantial role by filling the financial gap and providing platforms for further collaboration with global best practitioners. Similarly, the health authorities (HAAD, MOH and DHA) are taking initiatives for health innovation. As a part of DHA’s fifth Dubai Future Accelerators cycle, H.E. Humaid Al Qutami, Director General of the DHA, has discussed and brainstormed with four companies to discover the ways for the implementation of smart solutions in the health sector in Dubai (DHA, 2019).
In October 2018, H.E. Sheikh Abdulla Bin Mohamed Al Hamed, Chairman of the Department of Health—Abu Dhabi (DoH), said: “Through this year’s participation, DoH is aiming to contribute to the establishment of an innovation agenda for healthcare in Abu Dhabi by promoting entrepreneurship, invention and creative thinking. DOH is keen to attract top innovators and entrepreneurs from across the UAE to demonstrate their ideas and inventions to global investors who can provide the necessary support and funding to accelerate their development” (HAAD, 2019).
The Ministry of Health (MOH) is also diligently taking steps toward the translation of health innovation. The ministry has launched a platform for idea management, known as ‘Afkari’. This world-class idea management hub is meant to empower HCPs and to welcome their ideas for active participation for health innovation. Furthermore, MOH has collaborated with the international health authorities to develop and launch ‘Leadership and innovation in healthcare’ training program to fulfill the gap of knowledge among healthcare workers (MOHAP, 2019).
The findings of an intensive literature review show that the UAE health system is challenged by shortage of physicians and nurses, especially nationals with high turnover rate and low retention of expat HCP, skill-mix imbalance with weak knowledge base, and limited cognitive flexibility with inadequate investment in human resources (Hannawi & Salmi, 2014). Three of the above-mentioned challenges can have a strong negative impact on the UAE health innovation agenda.
Challenges of Implementation of Health Innovation in the UAE
High Turnover Rate and Low Retention
UAE nationals constitute 19% of total physicians and 8% of nurses, whereas more than eighty five percent (85%) of the clinical workforce is expatriate. The high turnover rate of expatriate nurses occurs because of unfavorable UAE immigration policies. Limited education and training capacities, low salaries, and lack of financial and non-financial incentives were identified as further reasons (Koornneef et al., 2015). As noted by Pereira and Malik (2015), increased mobility of the human capital can result in drop of expenditure toward training and skill enhancement of the human capital.
Skill-Mix Imbalance and Weak Knowledge
Career development activities are uncoordinated and there are no systematic performance appraisal; the continuing education programs are episodic and often unplanned (Hannawi & Salmi, 2014). Recently, the UAE has changed the selection criteria for nurses. According to the new regulation, a nurse holding a diploma will not be licensed after January 2020. Only holders of bachelor’s degree (BSN) will be able to perform patient care. This announcement resulted in a chaotic situation because many of the nurses working in the UAE healthcare industry are only diploma holders and now at the verge of losing their jobs (https://gulfnews.com/uae/uae-hundreds-of-indian-nurses-risk-losing-jobs-1.67129926).
Cognitive Flexibility
Huebner and Fichtel (2015) argued that innovation is “a novel solution to an old problem”. To find a new solution to an old problem, individuals must stop practicing old strategies and must behave flexibly. The practice of following protocol and performing tasks conservatively is routine in healthcare, which results in resistance to change and acceptance of innovations (Mørk, 2009; Mørk, Hoholm, Ellingsen, Edwin, & Aanestad, 2010).
Developing Resilience in the UAE’s HCPs
Southwick et al. (2014) state that “determinants of resilience include a host of biological, psychological, social and cultural factors that interact with one another to determine how one responds to stressful experiences”. According to Schumpeter (2010), radical innovations demand creative destruction of existing practices, technologies and processes. Innovation, almost always, certainly results in disruption, which will consequently create stress, conflict and instability. However, these tensions can be taken positively as a precondition for learning and development (Hoholm, 2011). Learning at organizational level is characterized as an ongoing and continuous cycle of action and reflection (Sujan, 2017).
As discussed earlier, the UAE healthcare industry is at the cusp of innovation. At the macro and meso levels, so far the efforts for the initiation of innovation strategy are effectively moving in the right direction. But at the micro level, especially physicians and nurses seem to be in need of developing skills to effectively and efficiently participate in this wave of health innovation in the UAE.
Resilience is a dynamic capability which can be acquired deliberately (Lengnick-Hall, 2011). To establish this required capability, the UAE’s HCPs should go through intensive training programs to acquire knowledge about health innovation. Milestad and Hadatsch (2003) have acknowledged that resilience can be built through the integration of knowledge.
The knowledge of the subject can be helpful in the removal of resistance and fear of the unknown. With adequate knowledge, HCPs can respond well to the uncertainty created by innovation. Personal resilience characteristics can be listed as optimism, flexibility and adaptability, initiative, tolerance, organizational skills, being a team worker, keeping within professional boundaries, assertiveness, humor and a sense of self-worth (Matheson et al., 2016; Jones 2019). To establish the required capability to foster and absorb innovation, HCP scan build and enhance resilience through knowledge and training. Thus, the UAE’s HCPs should go through a tailored training program to accept the disruptive changes and be prepared to foster the incoming wave of health innovation in the country.
Unified Theory of Acceptance and Use of Technology
As healthcare is embracing innovations and emerging technologies at large, the capability and resilience of HCPs can be enhanced by using Unified Theory of Acceptance and Use of Technology (UTAUT). This theory is intended toward users who are reluctant to adopt a new technology. According to Venkatesh et al. (2003), in this era of technology and innovation, recent advancements in Information Technology (IT) acceptance research have resulted in the development and availability of multiple competing models which have exhibited variant sets of acceptance determinants/factors. The authors have reviewed and empirically compared eight (8) models that are based on: (i) the theory of reasoned action; (ii) the technology acceptance model; (iii) the motivational model; (iv) the theory of planned behavior, (v) a model combining the technology acceptance model and the theory of planned behavior; (vi) the model of PC utilization, (vii) the innovation diffusion theory and (viii) the social cognitive theory.
The Unified Theory of Acceptance and Use of Technology (UTAUT) is comprised of four core determinants of intention and usage in addition to the four moderators of key relationships. UTAUT was tested over a period of six months in four organizations and the results were encouraging. It was established that the UTAUT surpassed the performance of the eight individual models. Hence, it was accomplished that the UTAUT provides a useful tool for managers and decision makers who are required to assess the probability of success of implementation of a new technology in their organization.
UTAUT is a beneficial tool to identify the drivers of acceptance of the technology, in order to proactively design interventions for the sustainable development of human capital in their organizations, like training and marketing. Utilization of this theory can be beneficial in future researches to improve the usage and acceptance of technological innovations in healthcare.
Healthcare Innovation Training Program for the UAE’s HCPs
The emerging technologies are abruptly challenging the status quo and are demanding updated policies and procedures for not only personnel management but also for proper selection of human capital to sustain in the future. According to Liu et al. (2017), high-commitment human resource management (HCHRM) system has a direct and positive correlation to the HR capability and ambidextrous technological innovation. However, they argued that HRM capabilities can affect knowledge management, both directly and indirectly. HRM policies and practices can stimulate creativity and innovative behaviors of employees (Pastor et al., 2010; Ishak, Eze, & Ling, 2010).
It has been noted that medical schools provide intense training and knowledge about the health of the human body. The core subjects taught are basic sciences like physiology, anatomy and biochemistry and advance subjects includes medicine, surgery, obstetrics and pediatrics. To complement the high-pace technological advancements in healthcare and to be able to effectively participate in the agenda of health innovation for better patient outcomes, HCPs are suggested to undergo focused training programs. This will provide them with the ability to understand the expectations, develop resilience and leverage the cost and time effectiveness of current and future innovations.
Below is the suggested outline of ‘Healthcare Innovation Training Program’ for UAE-based health professionals, and may be beyond. These identified areas are usually lacking in medical education. In addition, most medical professionals go through only health sciences during their medical education, thus lacking the capability to incorporate such knowledge in the daily practices. In addition, with such educational activities, HCPs will be able to participate in the innovation strategy by contributing their ideas to make the translation at a better pace, as seen in Fig. 11.3.
The suggested training modules will act as a guide toward the fostering of innovative systems, processes and procedures. The research was based on the identification of multilevel challenges; this is why it is recommended that while conducting these trainings, certain levels should be kept in consideration. This tailored program for the UAE’s HCPs will be effective only if conducted with the involvement and mutual collaboration of qualified physicians and industry experts.
Recommendations
-
Training programs are required for the UAE’s HCPs for better understanding of health innovation, as well as to establish the capability to incorporate innovation in daily practice. A detailed program comprised of seven modules has been suggested in this study. The HCPs play a pivotal role in the translation of innovation. Thus, these modules will not only provide required knowledge to them but can also be helpful in developing the strategies and policies.
-
Also, it is suggested that health authorities should reward technology-based entrepreneurial activities that closely overlap with the challenges of health systems.
-
Policy-makers should translate system-level demand signals into innovation development opportunities since it is imperative to foster innovations.
-
The public should contribute to the articulation of system-level needs and challenges of health innovation.
-
Funding provided by the government should also be used for further collection of data and researches by healthcare innovation policy-makers, for which purpose UTAUT can be a helpful tool.
Limitations and Scope for Future Research
The challenges faced during this research includes the scarcity of the literature on the role of human capital in this region in all fields and specifically for healthcare sector. Health innovation in the UAE is in a state of infancy; hence, collection of primary data and further investigations are essential and the need of the hour. Due to local health regulatory policies, primary data collection through surveys, interviews and focus groups was not accomplished. There is a scarcity of both qualitative and quantitative data in the domain of healthcare innovation in the UAE. This calls for further exploratory researches to determine the readiness of HCPs for the forthcoming innovations in healthcare. Lastly, time is a crucial factor to study innovations and technologies, because these are dynamic, apace, fast evolving and can be disruptive. This characteristic demands agile and continuous research, expeditious adoption and rapid implementation.
Conclusion
Due to continuous support from the UAE government, the healthcare industry is at the cusp of medical innovation but is facing many challenges, which if not addressed in timely manner might result in delays of expected outcomes. The UAE government and healthcare authorities are enthusiastic about implementing healthcare innovation strategies, but there are limitations and weaknesses on the human capital capability. While these strategies are being implemented by the government, training and development of HCPs as well as of consumers must be provided on high priority. Moreover, outsourcing technologies and experts will not lead to sustainability of healthcare innovation. The current workforce must undergo training to embrace the impact of upcoming innovations. Professional research and development is pivotal for well-established and sustainable innovation in the health industry. By overcoming these challenges, the UAE’s healthcare sector will become resilient for innovation and cutting-edge advances in healthcare.
References
Adler‐Milstein, J., Everson, J., & Lee, S. Y. D. (2015). EHR adoption and hospital performance: Time‐related effects. Health services research, 50(6), 1751–1771.
Angraal, S., Krumholz, H. M., & Schulz, W. L. (2017). Blockchain technology: Applications in health care. Circulation: Cardiovascular Quality and Outcomes, 10(9), e003800.
Anwar, S., & Prasad, R. (2018). Framework for future telemedicine planning and infrastructure using 5G technology. Wireless Personal Communications, 100(1), 193–208.
Asch, D. A., Terwiesch, C., Mahoney, K. B., & Rosin, R. (2014). Insourcing health care innovation. The New England Journal of Medicine, 370, 1775.
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191.
Baregheh, A., Rowley, J., & Sambrook, S. (2009). Towards a multidisciplinary definition of innovation. Management Decision, 47(8), 1323–1339.
Becker, G. S. (1964). Human capital: A theoretical and empirical analysis, with special reference to education. New York: NBER.
Berwick, D. M. (2003). Disseminating innovations in health care. Jama, 289(15), 1969–1975.
Birkinshaw, J., & Gupta, K. (2013). Clarifying the distinctive contribution of ambidexterity to the field of organization studies. Academy of Management Perspectives, 27(4), 287–298.
Blyth, F. M., Briggs, A. M., Schneider, C. H., Hoy, D. G., & March, L. M. (2019). The global burden of musculoskeletal pain—where to from here?. American journal of public health, 109(1), 35–40.
Cavicchi, C. (2017). Healthcare sustainability and the role of intellectual capital: Evidence from an Italian regional health service. Journal of Intellectual Capital, 18(3), 544–563.
Chen, J. (2017). Towards new and multiple perspectives on innovation. International Journal of Innovation Studies, 1(1), 1–4.
Christensen, C. M., Bohmer, R., & Kenagy, J. (2000). Will disruptive innovations cure health care? Harvard Business Review, 78(5), 102–112.
Christensen, C. M. (2013). The innovator’s dilemma: When new technologies cause great firms to fail. Harvard Business Review Press.
Costello, T., & Prohaska, B. (2013). Innovation. IT Professional, 15(3), 62–64.
Curado, C. (2018). Human resource management contribution to innovation in small and medium-sized enterprises: A mixed methods approach. Creativity and Innovation Management, 27(1), 79–90.
Curado, C., Muñoz-Pascual, L., & Galende, J. (2018). Antecedents to innovation performance in SMEs: A mixed methods approach. Journal of Business Research, 89, 206–215.
Department of Health - Abu Dhabi, HAAD. (2019). Retrieved from https://www.haad.ae/haad/
DHA, Department of Health Authority. (2019). Retrieved from https://www.dha.gov.ae/en/pages/dhahome.aspx
Ehnert, I., Parsa, S., Roper, I., Wagner, M., & Muller-Camen, M. (2016). Reporting on sustainability and HRM: A comparative study of sustainability reporting practices by the world’s largest companies. The International Journal of Human Resource Management, 27(1), 88–108.
Epstein, R. M., & Krasner, M. S. (2013). Physician resilience: What it means, why it matters, and how to promote it. Academic Medicine, 88(3), 301–303.
Farinha, L., Ferreira, J., & Gouveia, B. (2016). Networks of innovation and competitiveness: A triple helix case study. Journal of the Knowledge Economy, 7(1), 259–275.
Faulkner, A., & Kent, J. (2001). Innovation and regulation in human implant technologies: Developing comparative approaches. Social Science & Medicine, 53(7), 895–913.
Fennell, M. L., & Warnecke, R. B. (1988). Definition and diffusion of the innovation. In The diffusion of medical innovations (pp. 171–192). Boston, MA: Springer.
Fri, W., Pehrsson, T., & Søilen, K. (2013). How phases of cluster development are associated with innovation - the case of China. International Journal of Innovation Science, 5(1), 31–44. Retrieved from http://reports.weforum.org/global-agenda-council-2012/councils/emerging-technologies/
Garber, S., Gates, S. M., Keeler, E. B., Vaiana, M. E., Mulcahy, A. W., Lau, C., & Kellermann, A. L. (2014). Redirecting innovation in US health care: Options to decrease spending and increase value. Rand health quarterly, 4(1).
Gheorghiu, B., & Ratchford, F. (2015). Scaling up the use of remote patient monitoring in Canada. Studies in Health Technology and Informatics, 209, 23–26.
Global Innovation Index, GII. (2017). Retrieved from https://www.insead.edu/sites/default/files/assets/dept/globalindices/docs/GII-2017-report.pdf
Global Innovation Index, GII. (2019). Retrieved from https://www.globalinnovationindex.org/gii-2019-report
Godin, B. (2012). καινοτομία: An old word for a new world, or the de-contestation of a political and contested concept. In Challenging the innovation paradigm (pp. 51–74). New York: Routledge.
Goldin, C. (2016). Human capital. In Handbook of cliometrics (pp. 55–86). Heidelberg: Springer.
Greenhalgh, T., Fahy, N., & Shaw, S. (2018). The bright elusive butterfly of value in health technology development: Comment on “providing value to new health technology: The early contribution of entrepreneurs, investors, and regulatory agencies”. International Journal of Health Policy and Management, 7(1), 81.
Grisot, M., Vassilakopoulou, P., & Aanestad, M. (2018). Dealing with tensions in technology enabled healthcare innovation: Two cases from the Norwegian healthcare sector. In Controversies in healthcare innovation (pp. 109–132). London: Palgrave Macmillan.
Greco, P. J., & Eisenberg, J. M. (1993). Changing physicians’ practices.
Grose, T. K. (2008). Life support systems. Prism Magazine.org, pp. 35–39.
Gulf News. (2019). Retrieved from https://gulfnews.com/uae/uae-hundreds-of-indian-nurses-risk-losing-jobs-1.67129926
Hang, C. C., Garnsey, E., & Ruan, Y. (2015). Opportunities for disruption. Technovation, 39, 83–93.
Hannawi, S., & Salmi, I. A. (2014). Health workforce in the United Arab Emirates: Analytic point of view. The International journal of health planning and management, 29(4), 332–341.
Hart, P. L., Brannan, J. D., & De Chesnay, M. (2014). Resilience in nurses: An integrative review. Journal of nursing management, 22(6), 720–734.
Herzlinger, R.E. (2006). Why innovation in health care is so hard. Harvard Business Review, 84(5), p. 58
Heylin, P. (1637), A brief and moderate answer, to the seditious and scandalous challenges of Henry Burton, late of Friday-Streete in the two sermons, by him preached on the fifth of November. 1636. and in the apologie prefixt before them. By Peter Heylin London: Printed by Ric. Hodgkinsonne; and are to be sold by Daniel Frere, dwelling in little-Brittan, at the signe of the red-Bull.
Hoholm, T. (2011). Constructing Ethnography. In The Contrary Forces of Innovation (pp. 38–53). Palgrave Macmillan, London.
Hogan, S. J., & Coote, L. V. (2014). Organizational culture, innovation, and performance: A test of Schein’s model. Journal of Business Research, 67(8), 1609–1621.
Huebner, F., & Fichtel, C. (2015). Innovation and behavioral flexibility in wild redfronted lemurs (Eulemur rufifrons). Animal Cognition, 18(3), 777–787.
Huntington, J., Gilliam, S., & Rosen, R. (2000). Organizational development for clinical governance. British Medical Journal, 16, 679–682.
ICN (2018). https://2018.icnvoicetolead.com/
Institute of Medicine. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press.
Ishak, N. B., Eze, U. C., & Ling, L. S. (2010). Integrating knowledge management and human resource management for sustainable performance. Journal of Organizational Knowledge Management, 2010, 1–13.
Jacobs, S. R., Weiner, B. J., Reeve, B. B., Hofmann, D. A., Christian, M., & Weinberger, M. (2015). Determining the predictors of innovation implementation in healthcare: A quantitative analysis of implementation effectiveness. BMC Health Services Research, 15(1), 6.
Jeffcott, S. A., Ibrahim, J. E., & Cameron, P. A. (2009). Resilience in healthcare and clinical handover. BMJ Quality & Safety, 18(4), 256–260.
Johnston, M. P. (2017). Secondary data analysis: A method of which the time has come. Qualitative and Quantitative Methods in Libraries, 3(3), 619–626.
Jones, S. M. (2019). Resilience of primary healthcare professionals working in challenging environments: A focus group study. The British Journal of General Practice, 66(648), e507–e515.
Kalyar, M. N., & Rafi, N. (2013). ‘Organizational learning culture’: An ingenious device for promoting firm's innovativeness. The Service Industries Journal, 33(12), 1135–1147.
Kaplan, G., Bo-Linn, G., Carayon, P., Pronovost, P., Rouse, W., Reid, P., et al. (2013). Bringing a systems approach to healthcare. Washington, DC: Institute of Medicine and National Academy of Engineering.
Kim, K., & Von Glinow, M. A. (2017). Managing non-traditional human capital in international assignments: A qualitative analysis of the talent and innovation gaps. In Human capital and innovation (pp. 91–129). London: Palgrave Macmillan.
Kivisaari, S., Saranummi, N., & Väyrynen, E. (2004). Knowledge-intensive service activities in health care innovation: Case pirkanmaa. VTT Technical Research Centre of Finland.
Kivisaari, S., Saari, E., Lehto, J., Kokkinen, L., & Saranummi, N. (2013). System innovations in the making: Hybrid actors and the challenge of up-scaling. Technology Analysis & Strategic Management, 25(2), 187–201.
Connor., K. M. (2003). “Davidson JR.” Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety 18 (2003): 76–82.
Koornneef, E., Robben, P., Hajat, C., & Ali, A. (2015). The development, implementation and evaluation of clinical practice guidelines in Gulf Cooperation Council (GCC) countries: A systematic review of literature. Journal of evaluation in clinical practice, 21(6), 1006–1013.
Länsisalmi, H., Kivimäki, M., Aalto, P., & Ruoranen, R. (2006). Innovation in healthcare: A systematic review of recent research. Nursing Science Quarterly, 19(1), 66–72.
Lehoux, P., Miller, F. A., Daudelin, G., & Denis, J. L. (2017). Providing value to new health technology: The early contribution of entrepreneurs, investors, and regulatory agencies. International Journal of Health Policy and Management, 6(9), 509.
Lehoux, P., Miller, F. A., Daudelin, G., & Urbach, D. R. (2015). How venture capitalists decide which new medical technologies come to exist. Science and Public Policy, 43(3), 375–385.
Lengnick-Hall, C. A., Beck, T. E., & Lengnick-Hall, M. L. (2011). Developing a capacity for organizational resilience through strategic human resource management. Human Resource Management Review, 21(3), 243–255.
Lewis, M. W., & Smith, W. K. (2014). Paradox as a metatheoretical perspective: Sharpening the focus and widening the scope. The Journal of Applied Behavioral Science, 50(2), 127–149.
Lin, X. S., Qian, J., Li, M., & Chen, Z. X. (2018). How does growth need strength influence employee outcomes? The roles of hope, leadership, and cultural value. The International Journal of Human Resource Management, 29(17), 2524–2551.
Liu, Y., Ying, Y., & Wu, X. (2017). Catch-up through collaborative innovation: Evidence from China. Thunderbird International Business Review, 59(4), 533–545.
Maclaurin, W. R. (1953). The sequence from invention to innovation and its relation to economic growth. Quarterly Journal of Economics, 67(1), 97–111.
Mangione-Smith, R., DeCristofaro, A. H., Setodji, C. M., Keesey, J., Klein, D. J., Adams, J. L., ... & McGlynn, E. A. (2007). The quality of ambulatory care delivered to children in the United States. New England Journal of Medicine, 357(15), 1515–1523.
Markiewicz, K., Van Til, J. A., & IJzerman, M. J. (2014). Medical devices early assessment methods: Systematic literature review. International Journal of Technology Assessment in Health Care, 30(2), 137–146.
Martin, B. R. (1995). Foresight in science and technology. Technology Analysis & Strategic Management, 7(2), 139–168.
Masten, A. S. (2015). Pathways to integrated resilience science. Psychological Inquiry, 26(2), 187–196.
Matheson, C., Robertson, H. D., Elliott, A. M., Iversen, L., & Murchie, P. (2016). Resilience of primary healthcare professionals working in challenging environments: A focus group study. The British Journal of General Practice, 66(648), e507–e515.
McGlynn, E. A., Asch, S. M., Adams, J., Keesey, J., Hicks, J., DeCristofaro, A., & Kerr, E. A. (2003). The quality of health care delivered to adults in the United States. New England journal of medicine, 348(26), 2635–2645.
Meyer, U. (2019). The emergence of an envisioned future. Sensemaking in the case of “Industrie 4.0” in Germany. Futures, 109, 130–141.
Milestad, R., & Hadatsch, S. (2003). Organic farming and social-ecological resilience: The alpine valleys of Sölktäler, Austria. Conservation Ecology, 8(1).
MOF, Ministry of Finance. (2019). Retrieved from https://www.mof.gov.ae/en/pages/default.aspx
MOHAP, Ministry of Health and Prevention. (2019). Retrieved from https://www.mohap.gov.ae/en/Pages/default.aspx
Mørk, B. E. (2009). Changing practices: A practice-based study of cross-disciplinary technology development in hospitals.
Mørk, B. E., Hoholm, T., Ellingsen, G., Edwin, B., & Aanestad, M. (2010). Challenging expertise: On power relations within and across communities of practice in medical innovation. Management Learning, 41(5), 575–592.
Moullin, J. C., Sabater-Hernández, D., Fernandez-Llimos, F., & Benrimoj, S. I. (2015). A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Research Policy and Systems, 13(1), 16.
Mumtaz, S., & Parahoo, S. K. (2019). Promoting employee innovation performance: Examining the role of self-efficacy and growth need strength. International Journal of Productivity and Performance Management. https://doi.org/10.1108/IJPPM-12-2017-0330
Munjal, S., & Kundu, S. (2017). Exploring the connection between human capital and innovation in the globalising world. In Human capital and innovation (pp. 1–11). London: Palgrave Macmillan.
Nelson, J., & Gorichanaz, T. (2019). Trust as an ethical value in emerging technology governance: The case of drone regulation. Technology in Society, 59, 101131.
OECD. (1966). Government and technical innovation. Paris: OECD.
Omachonu, V. K., & Einspruch, N. G. (2010a). Innovation: implications for goods and services. International Journal of Innovation and Technology Management, 7(02), 109–127.
Omachonu, V. K., & Einspruch, N. G. (2010b). Innovation in healthcare delivery systems: A conceptual framework. The Innovation Journal: The Public Sector Innovation Journal, 15(1), 1–20.
Pereira, V., & Malik, A. (2015). Human capital in the Indian IT/BPO industry (1st ed.). London: Palgrave Macmillan.
Pfeffer, J., & Sutton, R. I. (2006). Evidence-based management. Harvard business review, 84(1), 62.
Picker Institute. (2000). Eye on Patients. A Report by the Picker Institute for the American Hospital Association. Boston, Mass.: Picker Institute.
Pols, J. (2012). Care at a distance. On the closeness of technology. Amsterdam: Amsterdam University Press.
Porter, A. L., Roessner, J. D., Jin, X. Y., & Newman, N. C. (2002). Measuring national ‘emerging technology’ capabilities. Science and Public Policy, 29(3), 189–200.
Prajogo, D. I., & Oke, A. (2016). Human capital, service innovation advantage, and business performance: The moderating roles of dynamic and competitive environments. International Journal of Operations & Production Management, 36(9), 974–994.
Prieto Pastor, I. M., Perez Santana, M. P., & Martín Sierra, C. (2010). Managing knowledge through human resource practices: Empirical examination on the Spanish automotive industry. The International Journal of Human Resource Management, 21(13), 2452–2467.
Proksch, D., Busch-Casler, J., Haberstroh, M. M., & Pinkwart, A. (2019). National health innovation systems: Clustering the OECD countries by innovative output in healthcare using a multi indicator approach. Research Policy, 48(1), 169–179.
Rotolo, D., Hicks, D., & Martin, B. R. (2015). What is an emerging technology? Research Policy, 44(10), 1827–1843.
Saborowski, M., & Kollak, I. (2015). “How do you care for technology?” – Care professionals’ experiences with assistive technology in care of the elderly. Technological Forecasting and Social Change, 93, 133–140.
Sahoo, S. K., Parveen, S., & Panda, J. J. (2007). The present and future of nanotechnology in human health care. Nanomedicine: Nanotechnology, Biology and Medicine, 3(1), 20–31.
Sardana, G. D. (2016). Innovation and growth. Broadway, NY: American Management Association.
Savory, C., & Fortune, J. (2015). From translational research to open technology innovation systems. Journal of Health Organization and Management, 29(2), 200–220.
Schartinger, D., Miles, I., Saritas, O., Amanatidou, E., Giesecke, S., Heller-Schuh, B., et al. (2015). Personal health systems technologies: Critical issues in service innovation and diffusion. Technology Innovation Management Review, 5(2), 46.
Schumpeter, J. A. (2010). Capitalism, socialism and democracy.
Schultz, T. W. (1961). Investment in human capital. The American Economic Review, 1, 1–17.
Scott, M. K. (2006). Health care in the express lane: The emergence of retail clinics. Oakland: California HealthCare Foundation.
Shimbun, A. (2011). What Went Wrong: Fukushima Flashback a Month After Crisis Started. Apr 12, 2011.
Shortell, S. M., O’Brien, J. L., Carman, J. M., Foster, R. W., Hughes, E. F., Boerstler, H., & O’Connor, E. J. (1995). Assessing the impact of continuous quality improvement/total quality management: Concept versus implementation. Health services research, 30(2), 377.
Shortell, S. M., Zazzali, J. L., Burns, L. R., Alexander, J. A., Gillies, R. R., Budetti, P. P., ... & Zuckerman, H. S. (2001). Implementing evidence-based medicine: The role of market pressures, compensation incentives, and culture in physician organizations. Medical care, I62–I78.
Škerlavaj, M., Song, J. H., & Lee, Y. (2010). Organizational learning culture, innovative culture and innovations in south Korean firms. Expert Systems with Applications, 37(9), 6390–6403.
Skinner, Q. (1978). The foundations of modern political thought, 2 volumes. Cambridge: Cambridge University Press.
Skinner, Q. (1988). Language and social change. In J. Tully (Ed.), Meaning and context (pp. 119–132). Princeton University Press: Princeton.
Small, H., Boyack, K. W., & Klavans, R. (2014). Identifying emerging topics in science and technology. Research Policy, 43(8), 1450–1467.
Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International journal of behavioral medicine, 15(3), 194–200.
Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European journal of psychotraumatology, 5(1), 25338.
Starfield, B. (2000). Is US health really the best in the world?. Jama, 284(4), 483–485.
Stenberg, A. (2017). What does innovation mean - a term without a clear definition. Halmstad: Halmstad University.
Sujan, M. (2017). High Reliability Organisations: Making Care Safer through Reliability and Resilience. In Improving Healthcare (pp. 101–114). Routledge.
Swan, J., Newell, S., & Nicolini, D. (Eds.). (2016). Mobilizing knowledge in health care: Challenges for management and organization. Oxford University Press.
Taherdoost, H. (2018). A review of technology acceptance and adoption models and theories. Procedia manufacturing, 22, 960–967.
Tarkkala, H., Helén, I., & Snell, K. (2019). From health to wealth: The future of personalized medicine in the making. Futures, 109, 142–152.
Taylor, J., Coates, E., Brewster, L., Mountain, G., Wessels, B., & Hawley, M. S. (2015). Examining the use of telehealth in community nursing: Identifying the factors affecting frontline staff acceptance and telehealth adoption. Journal of Advanced Nursing, 71(2), 326–337.
The social work careers magazine. (2019). Retrieved from https://www.socialworker.com/feature-articles/technology-articles/social-work-tech-notes-social-work-and-future-technology-what-can-be-automated-will-be/
UAE Government portal. (2019). Retrieved from https://www.government.ae/en#/
US Department of Commerce. (1967). Technological innovation: Its environment and management. Washington: USGPO.
Uzkurt, C., Kumar, R., Semih Kimzan, H., & Eminoğlu, G. (2013). Role of innovation in the relationship between organizational culture and firm performance: A study of the banking sector in Turkey. European Journal of Innovation Management, 16(1), 92–117.
Varkey, P., & Athyal, V. P. (2005). Service delivery innovations at Mayo Clinic. Minnesota Medical, 88, 39–42.
Varkey, P., Horne, A., & Bennet, K. E. (2008). Innovation in health care: A primer. American Journal of Medical Quality, 23, 382–388.
Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. D. (2003). User acceptance of information technology: Toward a unified view. MIS Quarterly, 3, 425–478.
Wade, V. A., Eliott, J. A., & Hiller, J. E. (2014). Clinician acceptance is the key factor for sustainable telehealth services. Qualitative Health Research, 24(5), 682–694.
Warne, T., & McAndrew, S. (2004). The mental health assistant practitioner: An oxymoron?. Journal of Psychiatric and Mental Health Nursing, 11(2), 179–184.
Watkins, A., Papaioannou, T., Mugwagwa, J., & Kale, D. (2015). National innovation systems and the intermediary role of industry associations in building institutional capacities for innovation in developing countries: A critical review of the literature. Research Policy, 44(8), 1407–1418.
Zhu, C., & Engels, N. (2014). Organizational culture and instructional innovations in higher education: Perceptions and reactions of teachers and students. Educational Management Administration & Leadership, 42(1), 136–158.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Qureshi, W. (2020). The Role of Human Capital in the Implementation of Healthcare Innovation in the UAE. In: Pereira, V., Neal, M., Temouri, Y., Qureshi, W. (eds) Human Capital in the Middle East. Palgrave Studies in Global Human Capital Management. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-42211-0_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-42211-0_11
Published:
Publisher Name: Palgrave Macmillan, Cham
Print ISBN: 978-3-030-42210-3
Online ISBN: 978-3-030-42211-0
eBook Packages: Business and ManagementBusiness and Management (R0)