Abstract
Good nutrition is fundamental for health and well-being. Given the increasing levels of obesity in the United Kingdom, it is important that food and nutrition are taught from a young age. The school curriculum can ensure that pupils have the knowledge to make healthy choices, whilst the school environment can play a role in ensuring that pupils have the opportunities to make healthy choices. Food and nutrition in the school curriculum must be grounded in evidence-based guidelines that consider current nutrition information and how nutrition knowledge can be applied. The curriculum should include the fundamentals of energy balance and nutrient requirements; describe a balanced diet; consider public health, obesity and related co-morbidities; consider food journeys from farm to fork; and consider food safety and the application of nutrition knowledge. New areas for nutrition research, such as the role of the gut microbiome in health and disease, sustainability and global food security, can also be embedded into the curriculum to ensure that teaching is up to date and relevant. Using research to enhance the teaching of food and nutrition in schools, we can ensure that pupils have the knowledge they need to make healthy food choices to protect their health in the short and long terms.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Good food and nutrition are fundamental for health and well-being. An appropriate diet can provide energy, support growth, the immune system and cognitive development, and prevent obesity and non-communicable diseases such as diabetes and cardiovascular disease. Given that eating habits are shaped at a young age (De Costa, Moller, Frost, & Olse, 2017), it is important that children are given opportunities to learn and understand the role of food and nutrition in health. Schools are an important setting where children and young people can be informed about food and nutrition. However, it is important to ensure that the food and nutrition curriculum is based on evidence-based information and is kept up to date to reflect advances in the field. Therefore, this chapter aims to explore developments in nutrition research and how they can be used to help shape and strengthen the teaching of food and nutrition in schools.
The increase in the rates of overweight and obesity in the United Kingdom (UK) has been well documented (National Health Service (NHS), 2018; Organisation for Economic Co-operation and Development (OECD), 2017). Data from the UK National Child Measurement Programme showed that a quarter of children entering primary school are overweight or obese, rising to one third by the end of primary school (Public Health England (PHE), 2018). Schools have been identified as a key setting for interventions and education (World Health Organization (WHO), 2009) since they can offer a framework for educating pupils about nutrition and healthy eating and about the importance of physical activity, as well as facilitate the implementation of food standards (Story, Nanney, & Schwartz, 2009). Dietary habits learned in childhood are often continued into adulthood (Lien, Lytle, & Klepp, 2001), and therefore childhood is a crucial time for developing lifelong healthy eating patterns (Sadegholvad, Yeatman, Parrish, & Worlsey, 2017). Tull (2018) recommends that food education be taught in schools to develop food knowledge and preparation skills, understand the relationship between diet and health and develop independence and life skills. Furthermore, nutrition education has been shown to contribute to healthy eating in and out of school, and this may also help reduce the risk of childhood and adult obesity (Contento, 2012; Hayes, Contento, & Weekly, 2018), further emphasising the importance of teaching food and nutrition in schools.
The Teaching of Nutrition in the School Curriculum in England
There have been many changes to how food education is taught in schools since it was first introduced into the school curriculum (Rutland, 1997); subsequently, food and nutrition is now taught in different areas of the school curriculum. It is presented as a life skill in Personal, Social, Health and Economic Education (PSHE) and as an academic subject in Science. It is a compulsory part of the Design & Technology (D&T) National Curriculum for pupils aged 5–14 years, where under the heading Cooking and Nutrition, it is stated that ‘as part of their work with food, pupils should be taught how to cook and apply the principles of nutrition and healthy eating’ (Department for Education (DfE), 2013; Rutland, 2017) (see Table 15.1). Furthermore, the geography curriculum features food and farming, and physical education may also include reference to nutrition as a key part of overall health and well-being (Department of Education, 2014). There is currently a General Certificate of Secondary Education (GCSE) in Food Preparation and Nutrition, which according to Ballam (2018) was offered as an optional subject for pupils aged 14–16 years in 76% of secondary schools, though it was noted that the numbers of pupils taking this option were declining. However, the A level food qualification was not redeveloped in England and Wales, the last cohorts completing in 2018.
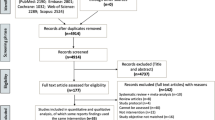
Although the updated National Curriculum for England requires all children and young people aged 5–14 years in maintained schools to study Cooking and Nutrition (Department for Education, 2014), how this is implemented varies from school to school. A recent British Nutrition Foundation (BNF) study found no evidence of change in the amount of cooking classes offered in schools since its introduction (Ballam, 2018). The Jamie Oliver Food Foundation, the British Nutrition Foundation (BNF), the Food Teachers Centre and the University of Sheffield published a report entitled ‘Food Education and Learning Landscape’ (FELL), which reviewed food education in schools (BNF, 2017). Their findings revealed large discrepancies in the quality of food education between schools, many of whom identified barriers such as resources, time and a lack of support. There were also concerns about the whole-school food environment that did not always allow children to be able to make good food choices. The report went on to recommend that schools should provide a healthy food environment and that more support should be available. In addition to this report, the British Nutrition Foundation (BNF) conducted a national survey in schools to investigate knowledge of food and nutrition in order to identify what young people know about cooking, healthy eating, food sources and physical activity (Ballam, 2017). Five thousand and forty young people aged 5–16 years participated in the study. Findings showed that in all age groups there was a clear lack of understanding as to where food originates. The findings revealed that 18% of children thought that fish fingers were made of chicken, and 10% of pupils aged 11–14 years did not know that potatoes and carrots grew underground. Amongst primary school children, there was also a lack of knowledge about the Public Health England’s Eatwell Guide (see Fig. 15.1). The survey revealed that the children got much of their nutrition information from the Internet, which is of variable quality, and hence there is a need to ensure that they are provided with up-to-date, evidence-based information through the school curriculum (Ballam, 2017).
Other research has shown that the majority of children in England do not consume the recommended amounts of fruit and vegetables; in 2016, 16% of children aged 5–15 years consumed five or more portions (Health Survey for England, 2016), and the average consumption was 3.1 portions per day. Schools that have engaged with programmes such as ‘Food for Life’ (Soil Association, 2019), which is a whole-school multicomponent intervention, have shown evidence for increased consumption of healthy food, with schools engaged with the ‘Food for Life’ programme in particular being found to be twice as likely to eat five or more portions of fruit and vegetables in comparison with other schools (Jones et al., 2017), again highlighting the importance of nutrition education for increasing healthy eating in and out of school.
The School Food Plan, published by the Department for Education in July 2013 (Dimbleby & Vincent, 2013), included a major review of school food in England and laid out actions to be implemented. These actions included adding cooking into the curriculum of children aged 4–14 years, introducing food-based standards for schools. Increasing the take up of good school food, establishing financial self-sufficient breakfast clubs, investigating extending free school meal entitlement (around the same time universal free school meals were offered to all pupils in reception year 1 & 2), training Head teachers and for Ofsted inspectors to consider behaviour and culture in the dining hall. The School Food Plan was never evaluated and in 2016 it came to an end, and a School Food Plan Alliance was established as a charity organisation independent of government funding (Scott, 2016).
The School Environment
The school environment also plays an important role in the development of healthy eating habits and may even compromise the pupil’s ability to make the healthiest food and drink choices. In August 2016, the UK government published Childhood Obesity: A Plan for Action (Her Majesty’s (HM) Government, 2016); as part of this report, plans were laid out for Ofsted to review levels of obesity, healthy eating and physical activity in schools (Ofsted, 2018). Their findings showed that some schools were constrained by their facilities, but 90% of schools that were visited had a full production kitchen (Ofsted, 2018).
Food served in schools in England is required to meet the School Food Standards (Dimbleby & Vincent, 2013) to ensure healthy balanced meals. The meals must provide fruit and vegetables, bread, cereals and/or potatoes and high-quality meat or fish. No more than two portions of deep fried, breaded or battered food can be served each week, and no chocolate crisps, sweets or drinks with added sugar can be sold in canteens or vending machines (School Food Plan, 2013). However, the take-up of school meals is low at 43% (Ofsted, 2018), and this includes the increase that occurred with the government’s introduction of free lunches for all infants (George, 2018). In older children, the decision to eat lunch at school may depend upon the facilities. Sometimes there are space restrictions and long queues, and the dining rooms can be described as dark and gloomy (Ofsted, 2018). Some pupils report school canteens as being noisy, unpleasant and with little food choice, and therefore they prefer to eat elsewhere (Wills et al., 2013). Older pupils may be more likely to leave the school premises at lunchtime and buy food and drink from local shops, supermarkets and fast-food takeaway outlets (Macdiarmid et al., 2015). Studies have shown that where children have permission to leave the school premises at lunchtime, at least 97% of them will purchase food and drink and that products bought outside of school can contribute up to 23% of pupil’s energy intakes (Sinclair & Winkler, 2008). Whilst pupils do recognise that food served in schools is usually healthier, it has been reported that healthy items sold in schools were expensive and it may be considered ‘uncool’ to be seen queueing for school food (Caraher et al., 2016).
Whilst nutrient- and food-based standards exist for school dinners, no such standards exist for packed lunches. Ofsted (2018) reports that 44% of pupils in England have a packed lunch, and nutritional studies have found that packed lunches typically have lower nutrient profiles than school lunches (Stevens, Nicholas, Wood, & Newlson, 2013). Children who have packed lunches have also been found to consume higher sugar and salt intakes and lower fibre levels and generally eat a less healthy diet over the entire day (Evans, Mandl, Christian, & Cade, 2015). It has been suggested that there should be food-based standards for packed lunches, as well as recommendations to improve intakes of a few nutrients, namely vitamin C, iron and folate, which are often lacking in packed lunches (Evans & Cade, 2016).
Schools should support the development of a healthy food environment on the premises that extend beyond school lunches to include all food served in breakfast clubs, after-school clubs, tuck shops and vending machines, as well as snacks consumed at break times (Weichselbaum & Butriss, 2014). The whole-school approach recognises that children are more likely to adopt healthier behaviours if the taught curriculum is supported by the same message within the ethos and environment of the school and its local community (Denman, Moon, Parsons, & Stears, 2001; Department for Education & Skills (DfES), 2004; Robinson, 2006).
Nutrition Research to Strengthen the Teaching of Food and Nutrition in Schools
Given that nutrition is taught in schools in various parts of the curriculum and supported by the school environment, the question is how to ensure that the information is current and reflects the latest research findings. Food and nutrition, like all STEM (science, technology, engineering and math) subjects, relies on the scientific method to shape knowledge of the complex links between food, nutrients and health. Nutrition is a scientific subject, and rigorous methods are used for research investigations in this area. It could be argued that nutrition is a relatively new science. Up until the year 1900, nutrition research largely focused on energetics and calories (Hargrove, 2006; Holmes, 1985). However, in the years that followed, scientists started to comprehend that there were other components essential for a healthy diet, such as micronutrients, and that individual dietary components could play a role in the prevention or development of chronic disease. In the wake of both world wars, there was a greater understanding of the role of diet and the importance of appropriate rations for soldiers on the front line, as well as the general population, and subsequently nutrition research flourished (Huxley, Lloyd, Goldacre, & Neil, 2000). Thereafter, there was a move from focusing on single nutrients to focusing on overall diets in relation to chronic disease and the health of the nation, particularly since there seems to be a transition from traditional diet rich in wholegrains, fruits and vegetables to a more processed energy-dense diet (Popkin, Adair, & Ng, 2012). This nutrition transition has led to the ‘double burden of malnutrition’, which has been characterised by the World Health Organization (WHO) as the coexistence of under-nutrition, along with obesity, and diet-related non-communicable diseases, which can affect individuals and populations and people of all ages (WHO, 2018).
Public health nutrition has never been more important, with increases in the rates of obesity, cardiovascular disease and diabetes. Nutrition and food education can help contribute to public health policies for tackling diet-related disease (Tull, 2018) and inform health promotion and healthy eating initiatives. Given the role of food and nutrition in the health of people around the world and at all stages of the lifespan, a clear understanding of the fundamentals of good nutrition is needed. Arguably, the first concept that needs to be included in the school curriculum is the theory of energy balance, where energy intake, i.e. food and drinks consumed, is considered alongside energy expenditure, i.e. calories used for metabolic activities and physical exercise. Changes to this balance, such as greater energy intakes compared to energy expenditure, results in weight gain, and conversely, if energy intake is less than energy expenditure, then weight loss is expected. This energy balance equation is simple but also helps us understand how obesity may develop in the light of increasing food intakes and decreased levels of physical activity. However, more recently, researchers have suggested that the energy balance equation, whilst appearing straightforward, does not necessarily reflect the numerous factors that affect energy intake, such as hunger, social pressure, psychological factors, financial constraints and cultural influences, to name but a few (Hill, Wyatt, Reed, & Peters, 2003). Likewise, energy expenditure is influenced by physical activity, sedentary behaviours, dietary-induced thermogenesis (the increase in energy expenditure that occurs when food is consumed and metabolised) and even growth. Furthermore, this simplistic equation of energy balance does not explain how changes to one side of the equation may also impact the other side of the equation such that changes to energy intake may be accompanied by changes in the thermic effect of a meal or energy expenditures (Schoeller, 2009). Therefore, it has been suggested that the focus should be not just on what factors affect energy intake or energy expenditure but rather the gap between energy intake and energy expenditure.
As well as studying energy balance and the amount of calories required in the diet, the sources of those calories need to be considered, and this can include the energy-yielding macronutrients carbohydrate, protein and fat. Recent discussions in the media have focused on individual macronutrients and, in particular, differences between carbohydrate and fat, with some parties recommending low-fat and high-carbohydrate diets whilst others favour high-fat and low-carbohydrate diets, and this has led to much confusion (Mozzaffarian, Rosenberg, & Uauy, 2018). Knowing who and which sources to trust is particularly important in this area since there is much misinformation on the Internet and social media, often posted by those with vested interests. It is probably too simplistic to divide food into such basic categories since carbohydrates include wholegrains and fibres, as well as simple sugars, and fats include saturated, monounsaturated, polyunsaturated and trans fats (trans fats are mostly created artificially and are found in manufactured food (Skeaff & Mann, 2017)); furthermore, many foods contain a mixture of macronutrients. For this reason, it may be better to focus on food models rather than on individual macronutrients in the context of a balanced diet. Pupils need to understand not only the caloric and nutritional value of food but also how together they can contribute to a balanced diet.
The ‘Eatwell Guide’ depicts how to achieve a balanced diet; it was introduced in 2016 (Public Health England (PHE), 2016; see Fig. 15.1) and replaced the old ‘Eatwell Plate’. The main changes in the ‘Eatwell Guide’ included the removal of the knife and fork because it was felt that they added little to the meaning of the model; the pictures of the food were drawn images rather than photographs; high fat, salt and sugar food were removed from the plate and were put outside the main image to help increase consumer understanding of the roles that these sorts of food and drinks play in the diet; fruit juices were removed from the fruit and vegetable segment; and some of the names of the segments were updated. The ‘Eatwell Guide’ now organises food into five main groups: (1) fruit and vegetables; (2) potatoes, bread, rice pasta and other starchy carbohydrates; (3) oils and spreads; (4) dairy and alternatives; and (5) beans, pulses, fish, eggs, meat and other proteins – recognising that there are foods other than meat that contribute to protein intake. There was also the addition of a hydration message, recommending that people drink 6–8 glasses of fluid every day, as well as details about energy requirements and the inclusion of a front of pack nutrition label. The ‘Eatwell Guide’ is said to apply to most people regardless of weight, dietary restrictions, preferences or ethnic origin. However, it is recognised to not apply to children under the age of two years who have different nutritional needs, and some people who may need to make adaptations based on their dietary requirements or medical needs.
Vitamins and minerals make crucial contributions to the diet and in most cases can be obtained easily if a variety of foods are consumed. It is worth informing pupils about the issues associated with too little of any nutrient but also the dangers of too much of any vitamin and mineral. If a varied diet is consumed, then typically there is no need for supplements; however there are some exceptions.
Women who are planning a pregnancy or who are pregnant should take daily a 400 mcg folic acid supplement up to the 12th week of pregnancy in order to prevent neural tube defects. Women who have a higher chance of having a pregnancy affected by neural tube defects need to take 5 mg of folic acid daily and should consult their GP (National Institute for Health and Care Excellence (NICE), 2018). However, not all pregnancies are planned, and women may be unaware that they need to be taking folic acid, so it has been suggested that flour should be fortified with folic acid. The UK government is currently launching a consultation on the amount of folic acid that should be added to help reduce the risk of complications (Department of Health and Social Care et al., 2019; Limb, 2018).
Other research has highlighted that some people need a vitamin D supplement to keep bones, teeth and muscles healthy. In spring and summer, most people get the vitamin D they need through sunlight on the skin and in the diet; however, in winter months, this may not be enough and a daily supplement should be considered (NHS, 2017). People who have little exposure to the sun should consider taking a supplement all year round (Scientific Advisory Committee on Nutrition (SACN), 2016). Children aged 1–4 years should also have up to 10 mcg daily of vitamin D, though children having more than 500 mL of infant formula milk a day will not need an additional supplement because the milk is already fortified with vitamin D.
Nutrition requirements do change during the lifespan, and it is important to understand how nutrition can help maintain good health at different stages since an individual’s need for nutrients and energy changes over time and may be different for particular population groups (Langley-Evans, 2015). At any stage of the lifespan, there will be varying influences on nutritional status and food habits or constraints on dietary intake, including income, religion, vegetarianism, age, gender and lifestyle. Different factors will influence our nutritional intake from birth when breastfeeding is recommended, through weaning growth, adolescence, adulthood and ageing in the later years. Knowledge of the changes in nutritional requirements can ensure that appropriate advice is given.
Pupils should also be aware of the origins of food since evidence from the BNF shows that this is currently not the case (Ballam, 2017). An understanding of the fact that food comes from plants or animals and needs to be grown, farmed or caught is important and that food is changed as it makes the journey from farm to fork to make it safe and edible, for example the journey from wheat to flour to bread (Food a fact of life, 2018). Practical food growing not only can help teach pupils where food comes from but also reinforce teaching about healthy diet and create environmental awareness (Porritt, 2009). Food preservation and food safety also need to be considered to ensure that the food supply is safe, considers animal welfare and avoids the risk of food poisoning in the home and businesses.
Developing Areas of Research
Nutrition is an evolving science subject, and as such there have been major developments in the last decade. Recently, the gut microbiome has been identified as a key regulator of health and disease, and consequently there has been increased interest in the gut flora, otherwise known as the gut microbiome. The gut microbiome is the complex community of trillions of cells and microorganisms, including bacteria that live in our digestive tracts. The gut microbiota may be affected by diet, genetics, medication use, and stress (Lockyer, 2017). Intestinal microbes can influence absorption, metabolism and the storage of ingested nutrients and have important effects on the host’s physiology (Gentile & Weir, 2018). For example, the microorganisms in the gut may be crucial for digestive function and play an important role in regulating the immune system, even appetite and energy metabolism (Valdes, Walter, & Spector, 2018). It would appear that we are only beginning to understand the role of the microbiome, as well as diet and host interactions (Mozzaffarian et al., 2018) and what food and supplements can help improve and maintain the microbiome. Probiotics are food and supplements that contain live bacteria, such as yoghurt or fermented food, and can now be bought from any supermarket. Probiotics are microorganisms that provide a health benefit to the host (Hill et al., 2014). The bacteria strains used vary widely, but well-studied and popular strains are from the genus Lactobacillus. There is some evidence that some probiotics can improve digestive health and may help prevent infections such as travellers’ diarrhoea, but not everybody responds to probiotics in the same way, so further research is required to clarify the probiotics that will affect specific health outcomes and help identify the people who will respond positively to probiotics (Sanders, Merenstein, Merrifield, & Hutkins, 2018). Alternatively, prebiotics are non-digestible foods or food ingredients that can stimulate growth of bacterial species that are already in the gut. Research is working towards identifying particular prebiotics that can help improve and maintain a balanced gut microbiota to enhance health and well-being (Gibson, Probert, Van Loo, Rastall, & Roberfroid, 2004). We are only beginning to understand the way the gut may affect our brains, moods, hormones and metabolism, but it is apparent that a healthy varied diet that includes plenty of plant-based foods and fibre is important for a healthy microbiome.
Issues such as climate change, biodiversity, land use and soil condition all help shape the food system, as does access to clean water. The long-term consequences of food production, distribution and consumption all need to be considered to ensure that it is sustainable (Mason & Lang, 2017). The Food and Agricultural Organization (FAO) of the United Nations (FAO, 2010) have described sustainable diets as ‘protective and respectful of biodiversity and ecosystems, culturally acceptable, accessible, economically fair and affordable; nutritionally adequate, safe and healthy while optimizing natural and human resources’. In their review of climate change and nutrition, Sustain (2013) concluded that benefits could come from reducing the amount of meat and dairy consumed and replacing it with food with lower greenhouse gas footprints; reducing intakes of sugary food, tea and coffee, and chocolate; reducing food waste and composting what food waste cannot be avoided, reducing the air freighting of food; avoiding bottled water; buying local, seasonal and fair trade products. The British Dietetic Association (2018) have also recently published a position statement on sustainable food where they highlighted that meat and dairy products are the leading contributors to greenhouse gas emissions and could be replaced with more plant-based proteins such as beans and pulses. They also commented that insects have been a much-discussed source of protein, but it may be some time before they are incorporated into many peoples’ diet. Ultimately, though, solutions to global food issues will be dependent upon partnerships with governments and industrial corporations, as well as the will of individuals (Food & Agricultural Organisation, 2017).
Back in 2014, a group of nutrition scientists were asked to predict what the most important nutrition trends in 2020 would be (Hackman et al., 2014). Their list included the microbiome, global food security, energy metabolism, ageing, cancer, inflammation and bioengineering, but also nutrition education. They reported that nutrition education needed to identify methods to make healthy choices more appealing and encourage healthy behaviours. They also recognised the importance of social media platforms in disseminating nutrition messages. Social media can bring members of the public in direct contact with health experts, but there are plenty of opportunities for misinformation. Ensuring that nutrition information is accurate and evidence based will be a challenge now and in the future.
Conclusion
Clearly there is a need for investment in food and nutrition education to give pupils knowledge about healthy, safe and sustainable diet. New developments in nutrition research should inform the curriculum and help strengthen the teaching of food and nutrition in schools to give pupils the skills they need to make informed choices regarding food and diet that will protect their health and the health of their families in both the short and long terms.
References
Ballam, R. (2017). British Nutrition Foundation health eating week 2017. Nutrition Bulletin, 42, 351–355.
Ballam, R. (2018). Where next for food education. Nutrition Bulletin, 43, 7–9.
British Dietetic Association. (2018). Policy statement sustainable diets. Retrieved July 22, 2019, from https://www.bda.uk.com/improvinghealth/healthprofessionals/policy_statements/policy_statement_sustainable_food.pdf
British Nutrition Foundation. (2017). Food education learning landscape. Retrieved July 22, 2019, from https://www.nutrition.org.uk/foodinschools/curriculum/foodeducationlearninglandscape.html
Caraher, M., Lloyd, S., Mansfield, M., Alp, C., Brewster, Z., & Gresham, J. (2016). Secondary schools pupils’ food choices around schools in a London borough: Fast food and walls of chips. Appetite, 103, 208–210.
Contento, I. R. (2012). Improving the diets and eating patterns of children and adolescents: How can nutrition education help? Adolescent Medicine, 23, 471–492.
De Costa, P., Moller, P., Frost, B. M., & Olse, A. (2017). Changing children’s eating behaviour – A review of experimental research. Appetite, 113, 327–357.
Denman, S., Moon, A., Parsons, C., & Stears, D. (2001). The health promoting school, research and practices. London, UK: Routledge.
Department for Education. (2013). National curriculum in England: Design and technology programmes of study Published 11 September 2013. Retrieved July 22, 2019, from https://www.gov.uk/government/publications/national-curriculum-in-england-design-and-technology-programmes-of-study/national-curriculum-in-england-design-and-technology-programmes-of-study
Department for Education. (2014). National curriculum. Retrieved July 22, 2019, from https://www.gov.uk/government/collections/national-curriculum
Department of for Education and Skills. (2004). Healthy living blue print for schools. London, UK: DfES.
Department of Health and Social Care, the Welsh Government, the Scottish Government, and the Department of Health (Northern Ireland). (2019). Open consultation adding folic acid to flour. Retrieved July 22, 2019, from https://www.gov.uk/government/consultations/adding-folic-acid-to-flour
Dimbleby, H., & Vincent, J. (2013). School food plan. Retrieved July 22, 2019, from http://www.schoolfoodplan.com/
Evans, C. E. L., & Cade, J. E. (2016). A cross-sectional assessment of food and nutrient based standards applied to British school children’s packed lunches. Public Health Nutrition, 20, 565–570.
Evans, C. E. L., Mandl, V., Christian, M. S., & Cade, J. E. (2015). Impact of school lunch type on nutritional quality of English children’s diets. Public Health Nutrition, 19, 36–45.
Food & Agricultural Organisation. (2010). Sustainable diets and biodiversity: Directions and solutions for policy research and action. In Proceedings of the International Scientific Symposium Biodiversity and sustainable diets united against hunger 3–5 Nov 2010 FAO Headquarters, Rome.
Food & Agricultural Organisation. (2017). The future of food and agriculture: Trends and challenges. Rome, Italy: FAO.
Food a fact of life. (2018). Retrieved July 22, 2019, from http://www.foodafactoflife.org.uk/Sheet.aspx?siteId=0§ionId=63&contentId=146
Gentile, C. L., & Weir, T. L. (2018). The gut microbiota at the intersection of diet and human health. Science, 362, 776–780.
George, M. (2018). Free infant lunches policy double take-up of school meals. TES, Retrieved January 24, 2018, from https://www.tes.com/news/free-infant-lunches-policy-doubled-take-school-meals
Gibson, G. R., Probert, H. M., Van Loo, J., Rastall, R. A., & Roberfroid, M. B. (2004). Dietary modulation of the human colonic microbiota: Updating the concept of prebiotics. Nutrition Research Reviews, 17, 259–275.
Hackman, R. M., Bharat, B., Aggarwal, R. S., Applebaum, R. W., deVere White, M. A., Dubick, M. A., et al. (2014). Forecasting nutrition research in 2020. Journal of the American College of Nutrition, 33, 340–346.
Hargrove, J. L. (2006). History of the calorie. Journal of Nutrition, 136, 2957–2961.
Hayes, D., Contento, I. R., & Weekly, C. (2018). Position of the Academy of Nutrition and Dietetics, Society for Nutrition Education and Behavior, and School Nutrition Association: Comprehensive nutrition programs and services in schools. Journal of Nutrition Education and Behavior, 50, 433–439.e1.
Health Survey for England. (2016). Retrieved July 22, 2019 from http://healthsurvey.hscic.gov.uk/data-visualisation/data-visualisation/explore-the-trends/fruit-vegetables.aspx
Hill, C., Guarner, F., Reid, G., Gibson, G., Merenstein, D. J., Pot, B., et al. (2014). Expert consensus document. The International Scientific Association for probiotics and prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature Reviews Gastroenterology & Hepatology, 11, 506–514.
Hill, J. O., Wyatt, H. R., Reed, G. W., & Peters, J. C. (2003). Obesity and the environment: Where do we go from here? Science, 299, 853–855.
HM Government. (2016). Childhood obesity: A plan for action. Retrieved July 22, 2019, from https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action
Holmes, F. L. (1985). Lavoisier and the chemistry of life. London, UK: University of Wisconsin Press Ltd.
Huxley, R. R., Lloyd, B. B., Goldacre, M., & Neil, H. A. (2000). Nutrition research in World War 2: The Oxford nutrition survey and its research potential 50 years later. British Journal of Nutrition, 84, 247–251.
Jones, M., Pitt, H., Oxford, L., Bray, I., Kimberlle, R., & Orme, J. (2017). Association between food for life, a whole setting healthy and sustainable food programme, and primary school children’s consumption of fruit and vegetables: A cross-sectional study in England. International Journal of Environmental Research and Public Health, 14, 639.
Langley-Evans, S. (2015). Nutrition a lifespan approach. Oxford, UK: Wiley-Blackwell.
Lien, N., Lytle, L. A., & Klepp, K. I. (2001). Stability in consumption of fruit, vegetables and sugary foods in a cohort from age 14 to age 21. Preventative Medicine, 33, 217–226.
Limb, M. (2018). Flour to be fortified with folic acid within weeks, says reports. British Medical Journal, 363, k4348.
Lockyer, S. (2017). Are probiotics useful for the average consumer? Nutrition Bulletin, 42, 42–48.
Macdiarmid, J., Wills, W. J., Masson, L. F., Craig, L. C. A., Bromley, C., & McNeill, G. (2015). Food and drinks purchasing habits out of school at lunchtime: A national survey of secondary school pupils in Scotland. International Journal of Behavioral Nutrition and Physical Activity, 12, 98. https://doi.org/10.1186/s12966-015-0259-4.
Mason, P., & Lang, T. C. (2017). Nutrition and the environment and sustainable diets. In J. Mann & A. S. Truswell (Eds.), Essentials of human nutrition. Oxford, UK: Oxford University Press.
Mozzaffarian, D., Rosenberg, I., & Uauy, R. (2018). History of modern nutrition science – Implications for current research, dietary guidelines and food policy. British Medical Journal, 361, k2392.
National Health Service. (2017). Vitamin D. Retrieved July 22, 2019 from https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
National Institute for Health and Clinical Excellence. (2018). Folic Acid. Retrieved July 22, 2019 from https://bnf.nice.org.uk/drug/folic-acid.html
National Health Service (2018). Statistics on obesity, physical activity and diet. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2018
Ofsted. (2018). Obesity, healthy eating and physical activity in primary schools. Retrieved July 22, 2019 from www.gov.uk/government/organsiations/Ofsted
Organisation for Economic Co-operation and Development. (2017). Obesity Update. Retrieved July 22, 2019 from www.oecd.org/health/obesity-update.htm
Popkin, B. M., Adair, L. S., & Ng, S. W. (2012). Global nutrition transition and the pandemic of obesity in developing countries. Nutrition Reviews, 170, 3–21.
Porritt, J. (2009). Growing up green. Sustainable Development UK, Spring 2009.
Public Health England. (2016). The Eatwell guide: How does it differ to the Eatwell plate and why? Retrieved July 22, 2019 from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/528201/Eatwell_guide_whats_changed_and_why.pdf
Public Health England. (2018). National child measurement programme (NCMP): Trends in child BMI, 26 July 2018. Retrieved July 22, 2019 from https://www.gov.uk/government/publications/national-child-measurement-programme-ncmp-trends-in-child-bmi
Robinson, S. (2006). Healthy eating for primary schools. London, UK: Paul Chapman Publishing.
Rutland, M. (1997). Food in the national curriculum. In M. Rutland (Ed.), Teaching food technology in secondary schools. London, UK: David Fulton Publishers.
Rutland, M. (2017). Food in the school curriculum: A discussion of alternative approaches. In M. J. de Vries (Ed.), Handbook of technology education. London, UK: Springer International.
Sadegholvad, S., Yeatman, H., Parrish, A. M., & Worlsey, A. (2017). What should be taught in secondary schools’ nutrition and food systems education? Views from prominent food related professionals in Australia. Nutrients, 9, 1207.
Sanders, M. E., Merenstein, D., Merrifield, C. A., & Hutkins, R. (2018). Probiotics for human use. Nutrition Bulletin, 43, 212–225.
Schoeller, D. A. (2009). The energy balance equation: Looking back and looking forward are two very different views. Nutrition Reviews, 67, 249–254.
School Food Plan. (2013). School food standards. Retrieved July 22, 2019 from http://www.schoolfoodplan.com/actions/school-food-standards/
Scientific Advisory Committee on Nutrition. (2016). Vitamin D and Health. Retrieved July 22, 2019 from https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report
Scott, S. (2016). What happened to the school food plan, Schools Week. Retrieved July 22, 2019 from https://schoolsweek.co.uk/what-happened-to-the-school-food-plan/
Sinclair, S., & Winkler, J. T. (2008). The school fringe: What pupils buy and eat from shops surrounding secondary schools. London, UK: Nutrition Policy Unit, London Metropolitan University.
Skeaff, C. M., & Mann, J. (2017). Lipids. In J. Mann & A. S. Truswell (Eds.), Essentials of human nutrition. Oxford, UK: Oxford University Press.
Soil Association. (2019). Food for life. Retrieved July 22, 2019 from https://www.foodforlife.org.uk/
Stevens, L., Nicholas, J., Wood, L., & Newlson, M. (2013). School lunches v. packed lunches: A comparison of secondary schools in England following the introduction of compulsory school food standards. Public Health Nutrition, 16, 1037–1042.
Story, M., Nanney, M. S., & Schwartz, M. B. (2009). Schools and obesity prevention: Creating school environments and policies to promote healthy eating and physical activity. Milbank Quarterly, 87, 71–100.
Sustain. (2013). The sustain guide to good food: How to make our food and farming system for the future. London, UK: Sustain.
Tull, A. (2018). Food and cooking skills education: Why teach people how to cook? Abingdon: Routledge, ProQuest Ebook Central, http://ebookcentral.proquest.com/lib/roehampton-ebooks/detail.action?docID=5257637.
Valdes, A. M., Walter, J., & Spector, T. D. (2018). Role for the gut microbiota in nutrition and health. British Medical Journal, 361, k2179.
Weichselbaum, E., & Butriss, J. L. (2014). Diet, nutrition and school children: An update. Nutrition Bulletin, 39, 9–73.
Wills, W. J., McDiarmid, J. I., Masson, L. F., Bromely, C., Craig, L., & McNeill, G. (2013). Children’s food and drink purchasing behaviour “Beyond the school gate”: The development of a survey module. Nutrition, 2013, 501450.
World Health Organisation. (2009). Interventions on diet and physical activity: What works. Retrieved from July 22, 2019, from https://www.who.int/dietphysicalactivity/whatworks/enl
World Health Organisation. (2018). Double burden of malnutrition. Retrieved from July 11, 2019, from https://www.who.int/nutrition/double-burden-malnutrition/en/
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Reeves, S. (2020). Current Research in Nutrition in the School Curriculum in England. In: Rutland, M., Turner, A. (eds) Food Education and Food Technology in School Curricula. Contemporary Issues in Technology Education. Springer, Cham. https://doi.org/10.1007/978-3-030-39339-7_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-39339-7_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-39338-0
Online ISBN: 978-3-030-39339-7
eBook Packages: EducationEducation (R0)