Abstract
Unilateral congenital cataracts are believed to result from localized ocular dysgenesis. Approximately 80–90% of unilateral cataracts are idiopathic. They are rarely associated with systemic anomalies and hence do not require systemic workup. Nuclear cataracts are common. Posterior capsule plaques are frequently encountered with unilateral congenital cataracts. Persistent fetal vasculature (PFV) poses special challenges in management. Early diagnosis and prompt treatment are critical for visually significant unilateral congenital cataracts owing to competition from the dominant normal eye. Preoperative counselling should stress the importance of full-time optical correction and amblyopia management. The visual outcomes are limited by early onset of deprivation amblyopia.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Unilateral congenital cataracts present unique challenges in diagnosis and management. The age at diagnosis can be delayed due to good vision in the unaffected eye. Most patients with unilateral cataract have deprivation amblyopia at the time of diagnosis owing to perpetual competition from the dominant normal eye. The critical period of visual development is shorter for unilateral compared to bilateral cataracts, making early diagnosis and management necessary. Amblyopia treatment plays a key role in the management of unilateral cataracts. Visual outcomes depend on the age at diagnosis, compliance to optical correction, and amblyopia management.
Epidemiology of Unilateral Congenital Cataracts
The overall prevalence of pediatric cataracts ranges from 0.01% to 0.15% [1], with unilateral cataracts being less common than bilateral cataracts. In a nationwide Danish study of 1027 congenital cataracts, 36% were unilateral cataracts compared to 64% bilateral cataracts [2]. In contrast, a collaborative study by 12 university medical centers in the United States reported that the prevalence of unilateral cataracts was 7.1 per 10,000 cases compared to 6.5 per 10,000 cases for bilateral cataracts [3].
Unilateral congenital cataracts are believed to be the result of localized ocular dysgenesis. Eighty to 90% of unilateral cataracts are idiopathic [2, 4]. The British Congenital Cataract Interest Group (BCCIG) found hereditary disease was associated with only 6% of unilateral cases, compared to 56% of bilateral cases [4]. Prenatal infections contributed to 2% of unilateral cases compared to 6% of bilateral cases [4]. Microphthalmos and persistent fetal vasculature were the most common associated ocular disorders for unilateral cataracts [4].
Morphology of Unilateral Congenital Cataracts
Nuclear Cataract
Nuclear cataract is the most frequently observed morphology found in pediatric unilateral cataracts. It accounted for 34% of unilateral cataracts across all major ethical groups in the Danish study [2]. This is similar to the findings reported by Infant Aphakia Treatment Study (IATS) where nuclear cataracts accounted for 54% of the cohort [5].
Cortical Cataract
Anterior and posterior cortical cataract, not involving the nucleus, were noted in 25% eyes in IATS [5].
Posterior Capsular Plaque
Posterior capsular plaque was observed in 88% eyes in IATS.; 7.2% had isolated posterior capsule plaque, and it was noted in all nuclear cataracts [5]. Plaques are also common in total cataracts [6] (Fig. 3.1).
Posterior Lenticonus
Posterior lenticonus was noted in 5–7% of unilateral pediatric cataracts [2, 5]. The progression of posterior lenticonus to cataract involving the cortex and nucleus is variable. During infancy, the cause of vision loss from posterior lenticonus may be due to anisometropia, posterior oil droplet-induced optical distortion [7], or amblyopia [8, 9] (Fig. 3.2).
Preexisting Posterior Capsule Defect (PCD)
PCD is believed to result from progression of posterior lenticonus. The prevalence of PCD varies from 2.2% to 6.75% [6, 10]. The cataract progresses rapidly once the PCD develops. In a classic case, PCD is hidden behind a total white cataract when viewed through an undilated, normal-sized pupil. Preoperative evaluation of such a cataract under maximum dilation is mandatory to unveil the important diagnostic signs such as well-demarcated thick defect margins, white dots on the posterior capsule (Fig. 3.3), and white dots in the anterior vitreous that move with the degenerated vitreous like a fish tail (fish-tail sign) [6].
Persistent Fetal Vasculature (PFV)
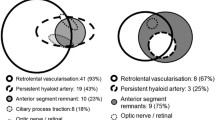
PFV contributes to 15–30% of unilateral congenital cataracts [2, 5]. PFV is typically unilateral, but bilateral PFV has been described in 10–15% of cases [11]. Persistence of some or significant portion of fetal vasculature leads to broad spectrum of clinical manifestations of PFV ranging from iridohyaloid vasculature, posterior fibrovascular sheath of the lens (retrolenticular membrane), persistent hyaloid artery, and Bergmeister papilla to severe retinal folds or detachment. PFV is often associated with microphthalmos [11]. The anterior segment vascular remnants are less common in unilateral compared to bilateral PFV [12].
The most common clinical presentation is a faint, small, vascular remnant within the Cloquet’s canal, attached to the posterior lens capsule. A less common presentation is the persistence of the entire hyaloid artery with varied amounts of perfusion from the optic nerve to the posterior lens surface. Rarely, it may also be attached to the optic nerve with its anterior end floating freely in the anterior vitreous [13]. Bergmeister papilla represents the remnant of the posterior portion of the hyaloid artery, causing primary congenital malformation of the optic nerve head. Figure 3.4 shows an eye with mature cataract with posterior fibrovascular sheath of lens with prominent ciliary processes.
Anterior Polar Cataract
Anterior polar cataract can be highly amblyogenic, not because it obscures the visual axis but because of induced refractive error, which is most often hyperopic anisometropia and astigmatism. They can be associated with reduced axial length [14].
Workup of Unilateral Congenital Cataracts
A thorough ocular exam of both eyes is recommended. The assessment should include age-appropriate visual acuity assessment; note the presence of strabismus, nystagmus, microcornea, intraocular pressure (IOP), refraction, and posterior segment evaluation with fully dilated pupils to look for PCD or PFV. B-scan ultrasonography should be performed if there is a poor view to the posterior segment. No systemic workup is typically recommended for a unilateral cataract.
Eyes with unilateral congenital cataract often have greater central corneal thickness, higher average keratometry values, and smaller corneal diameters. [15]
Outcomes of Pediatric Unilateral Cataracts
IATS is a landmark study in the management of congenital cataract in infants and young children. IATS randomized children 1–7 months of age at 12 sites across the United States to unilateral cataract surgery with or without intraocular lens (IOL) implantation [19]. The outcomes of this study are applicable to unilateral as well as bilateral congenital cataract surgery. Visual acuity, strabismus, stereopsis, and glaucoma outcomes were identical statistically between the IOL and contact lens (CL) group. The infants undergoing IOL implantation proved to have a more complicated course, including higher rates of additional intraocular surgery (72%) and adverse events such as lens proliferation into visual axis (40%), pupillary membrane (28%), corectopia (28%), glaucoma (19%), and glaucoma suspect (9%) [20]. At the end of 5-year follow-up, the study did not demonstrate any visual benefit of implanting an IOL at the time of unilateral cataract surgery in infants younger than 7 months of age [21]. About 50% of treated eyes in both groups had visual acuity of 20/200 or worse owing to deprivational amblyopia [23]. The data led the authors to conclude IOL implantation should be delayed in infants younger than 7 months at the time of surgery [19,20,21,22,23,24].
Young age at surgery is a risk factor for the development of glaucoma despite deferring cataract surgery for the first 4 weeks of life. There is 15–25% chance of developing glaucoma after congenital cataract surgery [23,24,25].
Early cataract extraction and successful optical rehabilitation are important to treat visual deprivation in children with congenital cataract to reduce the incidence of strabismus and nystagmus [18, 26]. The percentage of patients demonstrating strabismus over time increased from 24.6% at baseline to 70.4% by 12 months after cataract surgery. [27]
The same surgeons from IATS sites evaluated the outcomes of unilateral cataract surgery in 56 children aged 7–24 months operated in the same study period. Ninety-two percent received a primary IOL implantation in this group [26, 27]. The incidence of complications, reoperations, and glaucoma was low supporting the relatively safe use of IOLs in children older than 7 months of age [28]. The visual acuity was 20/40 or better only in 11% eyes in this cohort and 20/200 or worse in 44% eyes at 5 years of age owing to deprivation amblyopia [28].
Anterior PFV poses additional challenge owing to its association with microphthalmia and lifelong risk of developing glaucoma and retinal detachment [11, 29,30,31].
Case 1
A 6-day-old baby girl was urgently referred for absent red reflex in the left eye. She was otherwise healthy and born full term via vaginal delivery. No family history of childhood cataracts. On exam, her vision was blink to light in both eyes. Retinoscopy revealed a refraction of +4.00 +0.50 at 90 degrees in the right eye, but could not be performed on the left due to absent retinoscopic reflex. Corneal light reflexes were centered with Krimsky. Her anterior segment exam was unremarkable in the right and notable for symmetric corneal diameters and an opacity of the left lens. Eye pressures were 7 and 8 mmHg, respectively, with Tonopen. Fundus exam of the right eye was normal and not possible due to lens opacity in the left. B-scan was reassuringly unremarkable.
This girl underwent an uneventful surgery at 4 weeks of age and was left aphakic. She started CL correction and patching treatment on day 6 after the surgery. The visual acuity in the left eye was 20/125 with correction compared to 20/20 in the right eye at 5-year follow-up visit. She has 30–35 prism diopters of intermittent exotropia. She tolerates CL well at the time of writing, but she can be considered for secondary IOL placement if she becomes intolerant to contact lenses or desires functional vision without correction. She might subsequently need surgery for strabismus correction.
Comment
This fits into a classic presentation of unilateral congenital cataract. It is critical to diagnose unilateral cataracts early. The eye with unilateral cataract has deprivation amblyopia from day 1 after birth owing to competition from the healthy contralateral eye. The critical period for unilateral congenital cataract surgery is before 6 weeks of age, compared to 12–14 weeks for bilateral cataracts [16, 17]. Cataract surgery before 4 weeks is associated with greater prevalence of secondary membrane formation and glaucoma [16]. This child should be operated between 4 and 6 weeks of age, ideally at age 4 weeks.
It is important to counsel the family that cataract surgery is the beginning of treatment. Preoperative counseling should stress the importance of full-time optical correction and amblyopia management after surgery. Intraocular lens (IOL) implantation is not recommended in the first 7 months of life even in unilateral cataracts. IOL implantation can be offered in children older than 7 months at the time of surgery. When the child is left aphakic at the time of primary surgery, CL fitting should be performed within the first week after surgery. Extended wear silicone CL (Silsoft, Bausch and Lomb, Bridgewater, NJ) is preferred in this age group. It is important to remember that infants with aphakia are unable to accommodate and should be overcorrected by +2 or + 3 Diopters (D) to focus vision at a near viewing point. The families are advised to remove the CL at least once a week; however, it is recommended that the parents should try to manipulate CL every 2–3 days so that the parents as well as the child are used to the manipulation. The aphakic glasses are not a good option for optical correction in unilateral cataracts given the large amount of anisometropia. Amblyopia treatment should be initiated right after the CL fitting within the first week after surgery.
It is important to mention to the family that the eyes with unilateral congenital cataract are always left with some residual deprivation amblyopia despite early surgical intervention, full-time optical correction, and amblyopia management. The presence of strabismus or nystagmus in preoperative evaluation is an indicator of severe deprivation amblyopia and is more common in children who are diagnosed late [18].
Case 2
A 7-year-old girl was found to have unilateral cataract in her left eye at her annual physical exam. She presented to an outside ophthalmologist who gave her glasses correction for full-time use. She was recommended to undergo cataract surgery in the left eye at a follow-up visit 8 weeks later. The parents were conservative and wanted to pursue surgery only if it was really necessary, so they brought her for a second opinion. She was otherwise healthy except for asthma, for which she uses nebulizer as needed. There is no family history of childhood cataract.
On exam, her visual acuity was 20/20 in the right eye and 20/40 + 1 in the left with correction. Her current glasses were +0.75 D in the right eye and +1.25 D in the left eye. Her cycloplegic refraction showed more hyperopia: right eye, +3.25 D; left eye, +4.00 D. Sensorimotor exam did not demonstrate any strabismus or nystagmus. She had 60 arc seconds of stereoacuity. Anterior segment exam of the right eye was unremarkable; the left eye had a 2 mm posterior capsule plaque cataract, temporal to the central axis with a clear zone nasally, superiorly, and inferiorly allowing refraction and fundus examination. Fundus examination was unremarkable in both eyes.
This girl likely had congenital or developmental unilateral cataract but was diagnosed late at age 7 years. Given the presence of cataract and anisometropia, she had deprivation amblyopia in the left eye that had become established over the years, though it was mild. Her vision was 20/40 with correction in the left eye, but she had good stereopsis with no strabismus. Given that she had established deprivation amblyopia, she may not significantly benefit from cataract surgery. The cataract was not associated with strabismus and allowed refraction and fundus evaluation, which indicated that it was not visually significant. The decision was made to just monitor her closely for cataract progression. She did patching treatment for 6 months (2 to 4 hours per day), but it did not improve her vision. Her cataract and vision have remained stable for 1.5 years without surgical intervention until the last follow-up visit (Fig. 3.5).
Comment
This case illustrates that visually insignificant unilateral cataracts that are not progressive can be monitored safely. They can be treated with pupillary dilation, refractive correction, and patching in early stages to promote visual development.
Early diagnosis and prompt treatment are important factors for optimizing visual outcomes for visually significant unilateral congenital cataracts. The compliance and cost of optical correction with contact lenses stay a challenge in unilateral congenital cataracts operated in the first 7 months of life. IOL implantation is a safe option in older children. The amblyopia management plays a key role in improving visual prognosis. The visual outcomes are limited by early onset deprivation amblyopia in unilateral congenital cataracts.
References
Foster A, Gilbert C, Rahi J. Epidemiology of cataract in childhood: a global perspective. J Cataract Refract Surg. 1997;23:601–4.
Haargaard B, Wohlfahrt J, Fledelius HC, et al. A nationwide Danish study of 1027 cases of congenital/infantile cataracts: etiological and clinical classifications. Ophthalmology. 2004;111:2292–8.
SanGiovanni JP, Chew EY, Reed GF, et al. Infantile cataract in the collaborative perinatal project: prevalence and risk factors. Arch Ophthalmol. 2002;120:1559–65.
Rahi JS, Dezateux C. Congenital and infantile cataract in the United Kingdom: underlying or associated factors: British Congenital Cataract Interest Group. Invest Ophthalmol Vis Sci. 2000;41:2108–14.
Wilson ME, Trivedi RH, Morrison DG, et al. The Infant Aphakia Treatment Study: evaluation of cataract morphology in eyes with monocular cataracts. J AAPOS. 2011;15:421–6.
Vasavada AR, Praveen MR, Nath V, et al. Diagnosis and management of congenital cataract with preexisting posterior capsular defect. J Cataract Refract Surg. 2004;30:403–8.
Cheng KP, Hiles DA, Biglan AW, Pettapiece MC. Management of posterior lenticonus. J Pediatr Ophthalmol Strabismus. 1991;28:143–9.
Kushner BJ. Functional amblyopia associated with abnormalities of the optic nerve. Arch Ophthalmol. 1984;102:683–5.
Bradford GM, Kutschker PJ, Scott WE. Results of amblyopia therapy in eyes with unilateral structural abnormalities. Ophthalmology. 1992;99:1616–21.
Wilson ME, Trivedi RH. Intraocular lens implantation in pediatric eyes with posterior lentiglobus. Trans Am Ophthalmol Soc. 2006;104:176–82.
Goldberg M. Persistent fetal vasculature (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV Edward Jackson Memorial Lecture. Am J Ophthalmol. 1997;124:587–626.
Solebo AL, Russell-Eggitt I, Cumberland P, Rahi JS. Congenital cataract associated with persistent fetal vasculature: findings from IoLunder2. Eye. 2016;30:1204–9.
Hittner HM, Hirsch NJ, Rudolph HJ. Assessment of gestational age by examination of the anterior vascular capsule of the lens. J Pediatr. 1977;91:455–8.
Rasul A, Kessel L. Prevalence of anterior polar cataracts in children and risk factors for amblyopia. Acta Ophthalmol. 2018; https://doi.org/10.1111/aos.13966.
Kun L, Szigeti A, Bausz M, et al. Preoperative biometry data of eyes with unilateral congenital cataract. J Cataract Refract Surg. 2018;44:1198–202.
Birch EE, Cheng C, Stager DR Jr, et al. The critical period for surgical treatment of dense congenital bilateral cataracts. J AAPOS. 2009;13:67–71.
Birch EE, Stager DR. The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci. 1996;37:1532–8.
Felius J, Busettini C, Lynn MJ, Infant Aphakia Treatment Study Group, et al. Nystagmus and related fixation instabilities following extraction of unilateral infantile cataract in the Infant Aphakia Treatment Study (IATS). Invest Ophthalmol Vis Sci. 2014;55:5332–7.
The Infant Aphakia Treatment Study Group. The Infant Aphakia Treatment Study: design and clinical measures at enrollment. Arch Ophthalmol. 2010;128:21–7.
Plager DA, Lynn MJ, Buckley EG, Infant Aphakia Treatment Study Group, et al. Complications in the first 5 years following cataract surgery in infants with and without intraocular lens implantation in the Infant Aphakia Treatment Study. Am J Ophthalmol. 2014;158:892–8.
Lambert SR, Lynn MJ, Hartmann EE, The Infant Aphakia Treatment Study Group. Comparison of contact lens and intraocular lens correction of monocular Aphakia during infancy. A randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol. 2014;132:676–82.
Freedman SF, Lynn MJ, Beck AD, Infant Aphakia Treatment Study Group, et al. Glaucoma-related adverse events in the first 5 years after unilateral cataract removal in the Infant Aphakia Treatment Study. JAMA Ophthalmol. 2015;133:907–14.
Rabiah PK. Frequency and predictors of glaucoma after pediatric cataract surgery. Am J Ophthalmol. 2004;137:30–7.
Nihalani BR. Congenital cataract lessons learned from Infant Aphakia Treatment Study. Adv Ophthalmol Optom. 2016;1:211–29.
Wong IB, Sukthankar VD, Cortina-Borja M, et al. Incidence of early onset glaucoma after infant cataract extraction with and without intraocular lens implantation. Br J Ophthalmol. 2009;93:1200–3.
Bothun ED, Lynn MJ, Christiansen SP, Infant Aphakia Treatment Study, et al. Sensorimotor outcomes by age 5 years after monocular cataract surgery in the Infant Aphakia Treatment Study (IATS). J AAPOS. 2016;20:49–53.
Bothun ED, Cleveland J, Lynn MJ, et al. One-year strabismus outcomes in the Infant Aphakia Treatment Study. Ophthalmology. 2013;120:1227–31.
Bothun ED, Wilson ME, Traboulsi EI, et al. Outcomes of unilateral cataracts in infants and toddlers 7 to 24 months of age. Toddler Aphakia and Pseudophakia Study Group (TAPS). Ophthalmology. 2019;126(8):1189–95.
Mittra RA, Huynh LT, Ruttum MS, et al. Visual outcomes following lensectomy and vitrectomy for combined anterior and posterior persistent hyperplastic primary vitreous. Arch Ophthalmol. 1998;116:1190–4.
Vasavada AR, Vasavada SA, Bobrova N, Praveen MR, Shah SK, Vasavada VA, Pardo AJV, Raj SM, Trivedi RH. Outcomes of pediatric cataract surgery in anterior persistent fetal vasculature. J Cataract Refract Surg. 2012;38:849–57.
Warren N, Trivedi RH, Wilson ME. Persistent fetal vasculature with elongated ciliary processes in children. Am J Ophthalmol. 2019;198:25–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
The authors have no financial disclosure or proprietary interest that is relevant to the manuscript.
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cheung, C.S.Y., Nihalani, B.R. (2020). Unilateral Congenital Cataracts. In: Kraus, C. (eds) Pediatric Cataract Surgery and IOL Implantation. Springer, Cham. https://doi.org/10.1007/978-3-030-38938-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-38938-3_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-38937-6
Online ISBN: 978-3-030-38938-3
eBook Packages: MedicineMedicine (R0)