Abstract
Tetralogy of Fallot is one of the most common congenital heart diseases with increasing numbers of patients surviving into adulthood due to advances in surgical and transcatheter techniques. Whereas children undergo surgical repair early, the pathophysiology has a lifetime of consequences, increasing the risk of right heart failure with variable timing and presentation throughout adulthood. Key sequelae of repair include pulmonary regurgitation, pulmonary stenosis, impaired right ventricular function, left ventricular dysfunction, arrhythmias, and conduction abnormalities—all of which contribute to morbidity and mortality later in life. These sequelae are managed using a combination of medical therapy, pacemaker and defibrillator devices, transcatheter and surgical valve replacement, and advanced heart failure therapies, including heart transplantation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tetralogy of Fallot
- Adult congenital heart disease
- Heart failure
- Right heart failure
- Pulmonary stenosis
- Pulmonary regurgitation
A 37-year-old woman with repaired Tetralogy of Fallot (ToF) was admitted for increased dyspnea on exertion. At age 22 months, she underwent ventricular septal defect (VSD) patch closure and right ventricular outflow tract (RVOT) transannular patch repair and felt well until age 18 years when she noted increased dyspnea on exertion and early fatigue with daily activities. Evaluation at the time revealed severe pulmonary regurgitation (PR), leading to recommendation to undergo surgical pulmonary valve replacement (PVR). This was pursued with successful valve implantation that was complicated by complete atrioventricular (AV) node block requiring placement of permanent pacemaker with atrial and ventricular epicardial leads. Her pacemaker was changed to a transvenous dual-chamber pacemaker at age 24 years.
4.1 What Are the Initial Thoughts?
The potential for lifelong heart failure (HF) for patients with congenital heart disease begins at birth. Symptoms and signs of HF depend on the complexity of the anatomic and physiologic disease—with more severe cases presenting at birth or shortly thereafter, necessitating urgent intervention. For those born with a failing right heart, all procedures, regardless of timing and type, should be considered palliative and not curative; despite repeated procedures, cumulative myocardial damage often occurs due to congenital pathophysiology, deranged hemodynamics, and the therapeutic procedures themselves.
4.2 What Is TOF?
Tetralogy of Fallot (ToF) is the most frequent cyanotic congenital heart disease with almost 33 cases per 100,000 live births [1]. The four fundamental features of ToF, first described in detail by Fallot in 1888, comprise of unrestrictive malalignment VSD, pulmonary outflow tract obstruction (which may vary and contribute to relative direction and degree of intra-cardiac shunting), overriding aorta, and right ventricular (RV) hypertrophy [2] (Fig. 4.1). Given the advancements in surgical techniques since Lillehei first began operating on patients in 1955, there more patients are surviving, and even thriving, well into adulthood [3, 4]. Because of these advancements, physicians of all fields will encounter these patients.
The four fundamental features of Tetralogy of Fallot (ToF). Tetralogy of Fallot is comprised of malalignment ventricular septal defect (VSD), right ventricle outflow tract (RVOT) obstruction, overriding aorta, and right ventricular (RV) hypertrophy. Adapted from American Heart Association, Heart.org
4.2.1 Anatomy and Physiology
Van Praagh et al. describes ToF as one basic abnormality—the inadequate development of the subpulmonary infundibulum (which may or may not involve the pulmonary valve itself) from which all pathophysiology results [2, 5]. The key to understanding the features of ToF is knowledge of RV anatomy: the inlet portion, the apical trabecular component, and the outflow. The embryology and anatomy of the RV is discussed in Chap. 1.
The hypoplastic infundibulum itself creates the obstruction within the pulmonary outflow tract. The VSD results because the displaced infundibulum no longer fills the area above the septal band and ventricular septum. The hypoplastic infundibulum, which contains the infundibular septum as its floor, does not develop normally in a rightward, posterior, and inferior direction. Consequently, the aortic valve, which attaches to the infundibular septum, is malaligned anteriorly and superiorly, and thus overrides the aorta. In this case, the pulmonary valve (if developed) is often thickened and stenotic. RV hypertrophy occurs in the postnatal period if the RV is exposed to both a significant pulmonary outflow tract obstruction and a large non-restrictive VSD as pulmonary vascular resistance begins to fall [2].
Also in the postnatal period, the ductus arteriosus closes, and infants are solely reliant on the blood exiting the RV and flowing throughout the pulmonary vascular bed for systemic oxygenation. Thus, the degree of RVOT obstruction dictates the postnatal pathophysiology—the greater the obstruction, the less flow into the more distal pulmonary artery (PA). In infants born with significant obstruction (and/or if the pulmonary vascular resistance does not fall), there will be a net right-to-left shunt with flow of deoxygenated (blue) blood across the VSD, especially if it is large and unrestricted, into the systemic circulation, resulting in cyanosis [6].
4.3 What Are the Expected Physical Examination Findings in ToF?
In the post-operative adult, the physical exam directly correlates with the residual sequelae of the surgical intervention. A single S2 is due to the absence of functional pulmonary valve leaflets. A loud P2 may be due to a replaced pulmonic valve and/or pulmonary hypertension. A systolic ejection murmur can be heard if there is a residual outflow tract obstruction or abundant flow due to a regurgitant pulmonary valve. An early diastolic murmur denotes pulmonary regurgitation (PR) while flow due to tricuspid regurgitation (TR) or residual VSD can be heard throughout systole. A diminished or absent unilateral radial pulse and ipsilateral thoracotomy scar are key to the exam for patients who underwent subclavian artery-to-pulmonary artery anastomosis (classic Blalock-Taussig-Thomas {BTT} shunt) in early childhood [7].
4.3.1 Case Continued
On physical examination, the patient’s vital signs were normal, and she appeared comfortable. Well-healed sternotomy, abdominal, and deltopectoral scars were noted. The jugular venous pressure was elevated at 10 cm H2O, and her lungs were clear. Cardiovascular examination revealed an RV heave, normal S1, split S2 with loud P2, a grade II/VI systolic murmur at the left upper sternal border, and a grade II/IV diastolic murmur at the left lower sternal border. Peripheral pulses were normal.
4.4 What Is the Approach to ToF?
The goal for all surgical repair of ToF involves relief of RVOT muscular bundles and/or pulmonary valve annular obstruction, VSD closure, and main PA augmentation (and branches as needed).
Early surgical repair involved an anastomosis of the subclavian artery to the ipsilateral PA in order to augment pulmonary blood flow in those with severe RVOT obstruction (BTT shunt) [8]. The procedure then evolved into the modern approach using a modified BTT shunt with a polytetrafluroethylene interposition graft between the subclavian and pulmonary arteries, which may be taken down surgically later at the time of repair of the infundibulum and relief of the subpulmonary obstruction [8].
Earlier generations of patients may have undergone central shunt placement with anastomosis of the aorta to one of the branch pulmonary arteries in order to augment flow. Use of these shunts such as the Waterston (right PA to ascending thoracic aorta connection) and Potts (left PA to descending thoracic aorta anastomosis) has fallen out of favor as systemic to pulmonary flow is difficult to control, potentially leading to pulmonary overcirculation, iatrogenic ligation of nearby branch upper PA segments, or early shunt closure [9].
For those undergoing neonatal surgical repair with a narrowed infundibulum, the transannular approach to repair involves a full thickness incision along the infundibulum, effectively splaying it open to relieve the obstruction, followed by patch augmentation at the level of the pulmonic annulus, which fundamentally disrupts the valve architecture in order to provide this relief—sometimes with extension of the patch into the main PA—and VSD patch closure [6, 7, 10].
A valve-sparing technique has been advocated but still involves infundibulotomy or ventriculotomy to access the right ventricular outflow tract and resect obstructive muscle bundles [11]. Full relief of the infundibular obstruction may not result, cumulating in RV hypertrophy, fibrosis, recurrent RVOT obstruction, and a higher chance of reoperation [6, 10, 12].
The use of RV to PA conduit (cadaveric homograft or xenograft) may be necessary if the pulmonary arteries are diffusely small or if the location of the coronary arteries preclude infundibular repair [6]. PA reconstruction may also be required [12].
Non-surgical approaches including transcutaneous balloon valvuloplasty and stenting of the infundibulum have been used; the associated sequelae include residual RVOT obstruction, pulmonary regurgitation, tear within the infundibulum/main PA, and aneurysms and pseudoaneurysms within the outflow tract [13].
4.5 What Is the Pathophysiology of Right Heart Failure (RHF) in TOF?
ToF is an excellent model for RHF as the pathology begins before birth and has ramifications throughout life. In utero, the RV undergoes abnormal volume and pressure loading [14]. Concomitant poor development of pulmonary vasculature capacitance has significant long-term effects, and measurement of this value as a surrogate for RV afterload has noted implications for ventricular failure later on in life [15].
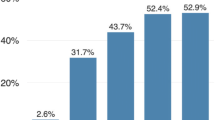
The six key sequelae of repaired ToF include pulmonary regurgitation, pulmonary stenosis, impaired RV function, LV dysfunction, arrhythmias, and conduction abnormalities; these contribute to the increasing morbidity and mortality seen in adulthood [16] (Fig. 4.2 and Table 4.1).
4.5.1 Pulmonary Regurgitation and Biventricular Dysfunction
Relief of RVOT obstruction often comes at the price of PR, resulting in adverse remodeling—as a compensatory measure to preserve stroke volume—due to volume, pressure, or mixed pressure/volume overload [1] (Fig. 4.3). Influential factors include: the duration of diastole, size of the orifice of regurgitation , the capacitance of the PAs, RV diastolic afterload, compliance of the RV, and the diastolic pressure gradient between the main PA and the RV [17, 18]. Alterations in pulmonary vascular resistance affect differential branch PA regurgitation with etiologies ranging from prior unilateral central shunt placement to external compression of the left lung by an enlarging heart [19].
Similar to LV adaptation to chronic volume loading in the setting of aortic valve regurgitation, the RV undergoes a pathophysiologic response to PR after ToF repair. First, there is a compensated stage during which end diastolic volume (EDV) increases, and eccentric and concentric hypertrophy occurs with maintenance of global systolic function and mass-to-volume ratio [20]. These mechanisms eventually fail (often years to decades later), leading to further ventricular dilation but with decreased mass-to-volume ratio (insufficient hypertrophy) and increased afterload with an associated decrease in global systolic function [17]. Eventually, these sequelae culminate in irreversible myocardial injury, characterized by increased wall stress, interstitial fibrosis, and dyssynchrony both within the RV and between the ventricles [1, 20]. This remodeling influences ventricular-ventricular interaction on the basis of mechanical and hemodynamic factors through septal geometry changes and chronically reduced left ventricular filling, respectively [21].
4.5.2 Pulmonary Stenosis
Residual obstruction in the RVOT , at or above the level of the pulmonary valve, or within the pulmonary vascular bed, can all result after ToF repair as a consequence of surgical intervention itself and/or be inherent within the patient’s anatomy. Pulmonary stenosis will result in additional RV pressure load. Animal models with surgically induced pressure overload demonstrate increases in contractile indices, systolic and diastolic reserves, and enhanced contractility via the Anrep effect [22]. This compensation may provide patients with an early protective effect on remodeling by preserving circumferential and radial myocardial strain while also negatively affecting LV intraventricular synchrony [23].
4.5.3 Arrhythmias and Conduction Abnormalities
In ToF, the His-Purkinje conduction pathway moves along the inferior aspect of the malalignment VSD, and therefore is often vulnerable to damage during surgery, resulting in classic postoperative right bundle branch block [24]. Atrial and ventricular arrhythmias late after repair are prevalent and correlated with a time-dependent risk of sudden cardiac death (SCD) [7]. Typical atrial flutter is the most common type of atrial arrhythmia in patients with repaired ToF [24]. SCD is the most common mode of death in ToF patients; the overall incidence ranges from 0.15% to 1.2% [25,26,27,28]. Risk scoring has been proposed for appropriate ICD shocks in primary prevention for patients with these variables: prior palliative shunt, inducible sustained ventricular tachycardia (VT), QRS duration ≥180 ms, ventriculotomy incision, nonsustained VT, and LV end-diastolic pressure ≥12 mmHg; a lower risk score confers a lower risk of annualized rate of appropriate shocks [29, 30].
4.6 What Diagnostic Work Up Would You Recommend?
As shown in Chap. 3, serial imaging studies are required to assess RV size and function. Color Doppler echocardiography provides visualization of regurgitation jets, and pulsed wave Doppler demonstration of diastolic flow reversal in the main or branch PAs, regurgitant fraction >40%, and jet pressure half-time of <100 ms are all indicative of severe regurgitation [31].
Data suggest ventricular size and function predict major cardiac outcomes. Increases in RV volumes and reductions in biventricular ejection fraction by cardiac magnetic resonance imaging (MRI) correlate well with decreases in tricuspid and mitral annular plane systolic excursion (TAPSE and MAPSE respectively). Right and left ventricular peak longitudinal 2-dimensional strain imaging on echocardiography is suggestive of adverse ventricular-ventricular interaction and interrelation of biventricular function [32, 33]. Similarly, myocardial deformation parameters of ventricular longitudinal and circumferential strain as measured by cardiac MRI feature tracking—a technique that assesses strain function—are predictors of outcome of a combined endpoint of death, successful resuscitation, or ventricular tachycardia [34, 35].
RV end-diastolic volume (EDV) dilation (with Z-scores based on published normal values ≥ 7) along with right and/or left ventricular dysfunction as measured on cardiac MRI are predictive of death, sustained ventricular tachycardia, and worsening functional status [36]. A pre-operative indexed RV end-systolic volume (ESV) of >95 mL/m2, older age, lower RV ejection fraction, and lower LV ejection fraction are all associated with adverse outcomes, including death, HF, and sustained VT; an indexed RV ESV < 80 mL/m2 is predictive of RV volume and function normalization after PVR [37].
Echocardiography is useful to identify the level of stenosis as well as severity. Moderate stenosis of a native valve is associated with a peak velocity of 3–4 m/s (or 36–64 mmHg) while velocities above 4 m/s (or 64 mmHg) indicate severe stenosis [38]. If an RV-PA conduit is used as part of the original repair, leaflet fibrosis and calcification of the conduit can degrade valve function and/or obstruct blood flow at any location along the entire conduit length [39].
ECG and Holter monitoring can be utilized for surveillance of arrhythmias and have been useful for clinical decision-making, such as referral for electrophysiology study and/or placement of ICD [40]. For patients undergoing programmed ventricular stimulation following ToF repair, inducible monomorphic VT and polymorphic VT predict future clinical VT and SCD [27]. Lengthening of the QRS interval on ECG reflects mechanical asynchrony present within the RVOT (and not within the RV body itself) resulting from prior surgical repair and fibrosis at the surgical site [41].
4.6.1 Case Continued
Our patient’s electrocardiogram revealed sinus rhythm with a first-degree AV block, right bundle branch block, and left posterior fascicular block. Interrogation of the pacemaker device showed no arrhythmias. An echocardiogram showed normal LV size and systolic function, grade 1 diastolic dysfunction, moderately enlarged RV with moderately reduced systolic function, flattening of the interventricular septum, and a maximum instantaneous Doppler gradient of 53 mmHg across the RVOT, severe PR, and moderate TR with an estimated RV systolic pressure of 55 mmHg. Cardiac computerized tomography demonstrated unobstructed RVOT, no coaptation of pulmonary valve leaflets, a dilated RV with indexed RV EDV of 140 mL/m2 (53.6 ± 10.5 mL/m2) and indexed RV ESV of 80 mL/m2 (22 ± 7 mL/m2), a reduced RV ejection fraction of 42%, normal LV size with ejection fraction of 51%, normal sized main and branch PAs, and normal coronary artery course without stenosis.
4.7 What Are the Management Strategies for this Patient?
Patients often enjoy an asymptomatic period that lasts for several decades before manifesting signs of HF similar to their counterparts with acquired heart disease [42]. Archetypal HF symptoms such as exercise intolerance, dyspnea on exertion, volume overload, and fatigue may not be as overt in ToF patients [43].
Medical therapy often includes the same drug classes within the acquired LV HF armamentarium: diuretics; beta-blockers for myocardial preservation and arrhythmia management; and angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), aldosterone antagonists, and angiotensin receptor-neprilysin inhibitor (ARNi) for afterload reduction and prevention of adverse ventricular remodeling [44]. However, the evidence for HF drugs in ToF is lacking in randomized, double-blind placebo-controlled trials [45]. For ToF patients who develop pulmonary vascular disease, disease-targeting drug therapies have been used to decrease pulmonary vascular resistance and improve functional class [46]. Cardiac resynchronization therapy (CRT ) has been shown to improve LV ejection fraction with favorable trends in LV volumes in repaired ToF patients who met clinical criteria for upgrade or implantation of CRT pacemaker [47]. Electrophysiological studies and ablative therapies are also employed for arrhythmia management as needed [43]. Additionally, any modifiable HF risk factors, such as tobacco use, obesity, diabetes, or hypertension, should also be addressed [16].
Residual obstructive or regurgitant lesions may require catheter-based or surgical interventions. PVR often improves symptoms in those with combined pulmonary stenosis and regurgitation rather than regurgitation alone and is reasonable in patients with symptoms and/or evidence of RV and/or LV dysfunction [48] (Fig. 4.4). PVR can be performed surgically or percutaneously; transcatheter PVR (TPVR) can be placed valve-in-valve (Medtronic Melody or Edwards SAPIEN valves) within existing RVOT conduits or previously placed surgical valves [49, 50]. Branch PA balloon dilation and stenting may be used for relief of stenosis while collaterals causing pulmonary vascular overcirculation or hemoptysis may require catheter-based coiling or vascular plug deployment [49]. Residual VSD(s), RVOT obstruction(s), PA stenosis, significant aortic regurgitation, RVOT aneurysm, and enlarged aortic root with diameter ≥ 55 mm also may require surgical intervention [51].
Referral for pulmonary valve replacement after ToF repair. ToF tetralogy of fallot, RV right ventricular, LV left ventricular, RVEDV right ventricular end diastolic volume, RVESP right ventricular end systolic volume, RVSP right ventricular systolic pressure, RVOT right ventricle outflow tract, CPET cardiopulmonary exercise testing. Adapted from Stout et al., JACC 2019;73:e81–e192
4.8 What Are the Options for Advanced Therapies?
Advanced HF therapies have been employed in repaired ToF patients, including inotrope and vasopressor therapy, ventricular assist device (VAD), and heart transplantation [52, 53].
VAD placement for a subpulmonic RV is technically challenging given the anterior position of the RV, and its use is limited [54]. Data for the use of a subaortic LV VAD is also limited, though mortality is similar to those without congenital heart disease [55,56,57]. RV dysfunction often precludes LV VAD therapy. Cardiac transplantation may also be used in severe HF, but patients often have longer wait-list times and congenital heart disease-specific factors that may affect transplant candidacy, such as allo-sensitization, pulmonary hypertension, surgical challenges (e.g. adhesions, collateral vessels, PA reconstruction), and liver dysfunction [52, 58, 59]. Palliative care may be appropriate for those who are not candidates for advanced HF therapies [52] as discussed in Chap. 12.
4.9 What Is the Prognosis?
The utility of cardiopulmonary exercise testing (CPET) has been highlighted as a tool in the management of patients with HF. CPET provides insight into cardiac physiology as well as the response of pulmonary and musculoskeletal systems to the metabolic demands of exercise; use of peak VO2 (peak oxygen consumption) and VE/VCO2 slope (minute ventilation-carbon dioxide output relationship, a measurement of ventilation-perfusion matching) has been described in risk stratification for patients with repaired ToF [60]. Multiple factors associated with repaired ToF influence myocardial reserve, including pulmonary and tricuspid valve regurgitation, RV-LV interactions, wall motion abnormalities due to surgical patches within the RVOT and ventricular septum, conduction abnormalities, neurohormonal imbalances, and myocardial architectural damage. In turn, these factors affect the hemodynamic disturbances seen during exercise as noted by changes in submaximal and maximal CPET measurements [61].
Use of HF tools, such as the Seattle Heart Failure Model, for risk stratification in adults with congenital heart disease can help identify populations at high-risk for death and cardiovascular hospitalization [62]. Biomarker measurements may also be helpful as elevated levels of N-terminal pro-B-type natriuretic peptide (NT-proBNP), high-sensitivity troponin T, and growth-differentiation factor 15 have been associated with cardiovascular events [63, 64].
4.9.1 Case Conclusion
On the basis of the findings above, the patient underwent TPVR with a bovine pericardium bioprosthetic valve with a valve-in-valve approach. Her post-procedural course was uncomplicated, and on clinic follow up, her symptoms had resolved.
Clinical Pearls
-
Heart failure in repaired ToF manifests as volume overload, atrial and ventricular arrhythmias, and decreased exercise tolerance.
-
ToF results from infundibular septum hypoplasia, and surgical repair focuses on relieving RVOT obstruction, often at the expense of pulmonary regurgitation.
-
Exam findings directly correspond to the sequelae of surgical repair, including single S2, murmurs of pulmonary stenosis and/or regurgitation, diminished or absent radial pulse due to prior BTT shunt, and residual VSD murmur.
-
Electrocardiogram and echocardiogram are important diagnostic tools in patients with acute HF symptoms. Cross-sectional imaging, such as CT and MRI, is utilized for interventional planning. CPET can be used for prognostication. Invasive assessment of hemodynamics may be of particular utility when RHF is longstanding or concomitant liver impairment is suspected, given the propensity towards low systemic vascular resistance in these cases.
-
Diuretics and antiarrhythmics may be given in the acute presentation of HF. Standard HF guideline-directed medical therapy is often used for afterload reduction and prevention of adverse remodeling, though compelling data supporting long-term use are lacking. Pulmonary vasodilators are utilized in concomitant pulmonary hypertension management. Ablative therapies may be beneficial in specific instances of tachyarrhythmia; pacemakers and ICDs may be useful to treat bradyarrhythmias and to reduce incidence of sudden cardiac death.
-
Advanced therapies, including inotrope infusion, mechanical circulatory support, and heart transplantation are generally offered for refractory heart failure.
-
Diagnostic evaluation and therapeutic strategies for patients with RHF associated with congenital heart disease should be reviewed in conjunction with expert clinicians in the management of congenital heart disease.
References
Valente AM, Geva T. How to image repaired tetralogy of Fallot. Circ Cardiovasc Imaging. 2017;10:e004270.
Van Praagh R. The first Stella van Praagh memorial lecture: the history and anatomy of tetralogy of Fallot. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2009;12:19–38.
Lillehei CW, Cohen M, Warden HE, Varco RL. The direct-vision intracardiac correction of congenital anomalies by controlled cross circulation; results in thirty-two patients with ventricular septal defects, tetralogy of Fallot, and atrioventricularis communis defects. Surgery. 1955;38:11–29.
Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115:163–72.
Van Praagh R, Van Praagh S, Nebesar RA, Muster AJ, Sinha SN, Paul MH. Tetralogy of Fallot: underdevelopment of the pulmonary infundibulum and its sequelae. Am J Cardiol. 1970;26:25–33.
Sharkey AM, Sharma A. Tetralogy of Fallot: anatomic variants and their impact on surgical management. Semin Cardiothorac Vasc Anesth. 2012;16:88–96.
Downing TE, Kim YY. Tetralogy of Fallot: general principles of management. Cardiol Clin. 2015;33:531–41, vii-viii.
Gladman G, McCrindle BW, Williams WG, Freedom RM, Benson LN. The modified Blalock-Taussig shunt: clinical impact and morbidity in Fallot’s tetralogy in the current era. J Thorac Cardiovasc Surg. 1997;114:25–30.
Dorobantu DM, Pandey R, Sharabiani MT, et al. Indications and results of systemic to pulmonary shunts: results from a national database. Eur J Cardiothorac Surg. 2016;49:1553–63.
McKenzie ED, Maskatia SA, Mery C. Surgical management of tetralogy of Fallot: in defense of the infundibulum. Semin Thorac Cardiovasc Surg. 2013;25:206–12.
Bacha E. Valve-sparing options in tetralogy of Fallot surgery. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2012;15:24–6.
Karl TR, Stocker C. Tetralogy of Fallot and its variants. Pediatr Crit Care Med. 2016;17:S330–6.
Hoffman JIE. At what age should tetralogy of Fallot be corrected? Cardiol Young. 2017;27:625–9.
Hirji A, Bernasconi A, McCrindle BW, et al. Outcomes of prenatally diagnosed tetralogy of Fallot: implications for valve-sparing repair versus transannular patch. Can J Cardiol. 2010;26:e1–6.
Dupont M, Mullens W, Skouri HN, et al. Prognostic role of pulmonary arterial capacitance in advanced heart failure. Circ Heart Fail. 2012;5:778–85.
Wald RM, Valente AM, Marelli A. Heart failure in adult congenital heart disease: emerging concepts with a focus on tetralogy of Fallot. Trends Cardiovasc Med. 2015;25:422–32.
Geva T. Indications and timing of pulmonary valve replacement after tetralogy of Fallot repair. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2006;9:11–22.
Redington AN. Physiopathology of right ventricular failure. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2006;9:3–10.
Kang IS, Redington AN, Benson LN, et al. Differential regurgitation in branch pulmonary arteries after repair of tetralogy of Fallot: a phase-contrast cine magnetic resonance study. Circulation. 2003;107:2938–43.
Geva T. Repaired tetralogy of Fallot: the roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support. J Cardiovasc Magn Reson. 2011;13:9.
Dragulescu A, Friedberg MK, Grosse-Wortmann L, Redington A, Mertens L. Effect of chronic right ventricular volume overload on ventricular interaction in patients after tetralogy of Fallot repair. J Am Soc Echocardiogr. 2014;27:896–902.
Yerebakan C, Klopsch C, Niefeldt S, et al. Acute and chronic response of the right ventricle to surgically induced pressure and volume overload—an analysis of pressure-volume relations. Interact Cardiovasc Thorac Surg. 2010;10:519–25.
Latus H, Hachmann P, Gummel K, et al. Impact of residual right ventricular outflow tract obstruction on biventricular strain and synchrony in patients after repair of tetralogy of Fallot: a cardiac magnetic resonance feature tracking study. Eur J Cardiothorac Surg. 2015;48:83–90.
Le Gloan L, Guerin P, Mercier LA, et al. Clinical assessment of arrhythmias in tetralogy of Fallot. Expert Rev Cardiovasc Ther. 2010;8:189–97.
Gatzoulis MA, Balaji S, Webber SA, et al. Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of Fallot: a multicentre study. Lancet. 2000;356:975–81.
Harrison DA, Siu SC, Hussain F, MacLoghlin CJ, Webb GD, Harris L. Sustained atrial arrhythmias in adults late after repair of tetralogy of Fallot. Am J Cardiol. 2001;87:584–8.
Khairy P, Landzberg MJ, Gatzoulis MA, et al. Value of programmed ventricular stimulation after tetralogy of Fallot repair: a multicenter study. Circulation. 2004;109:1994–2000.
Silka MJ, Hardy BG, Menashe VD, Morris CD. A population-based prospective evaluation of risk of sudden cardiac death after operation for common congenital heart defects. J Am Coll Cardiol. 1998;32:245–51.
Khairy P, Dore A, Poirier N, et al. Risk stratification in surgically repaired tetralogy of Fallot. Expert Rev Cardiovasc Ther. 2009;7:755–62.
Khairy P, Harris L, Landzberg MJ, et al. Implantable cardioverter-defibrillators in tetralogy of Fallot. Circulation. 2008;117:363–70.
Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30:303–71.
Kempny A, Diller GP, Orwat S, et al. Right ventricular-left ventricular interaction in adults with tetralogy of Fallot: a combined cardiac magnetic resonance and echocardiographic speckle tracking study. Int J Cardiol. 2012;154:259–64.
Diller GP, Kempny A, Liodakis E, et al. Left ventricular longitudinal function predicts life-threatening ventricular arrhythmia and death in adults with repaired tetralogy of Fallot. Circulation. 2012;125:2440–6.
Orwat S, Diller GP, Kempny A, et al. Myocardial deformation parameters predict outcome in patients with repaired tetralogy of Fallot. Heart. 2016;102:209–15.
Moon TJ, Choueiter N, Geva T, Valente AM, Gauvreau K, Harrild DM. Relation of biventricular strain and dyssynchrony in repaired tetralogy of Fallot measured by cardiac magnetic resonance to death and sustained ventricular tachycardia. Am J Cardiol. 2015;115:676–80.
Knauth AL, Gauvreau K, Powell AJ, et al. Ventricular size and function assessed by cardiac MRI predict major adverse clinical outcomes late after tetralogy of Fallot repair. Heart. 2008;94:211–6.
Bokma JP, Winter MM, Oosterhof T, et al. Preoperative thresholds for mid-to-late haemodynamic and clinical outcomes after pulmonary valve replacement in tetralogy of Fallot. Eur Heart J. 2016;37:829–35.
Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr. 2009;10:1–25.
Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:e57–185.
Czosek RJ, Anderson J, Khoury PR, Knilans TK, Spar DS, Marino BS. Utility of ambulatory monitoring in patients with congenital heart disease. Am J Cardiol. 2013;111:723–30.
Uebing A, Gibson DG, Babu-Narayan SV, et al. Right ventricular mechanics and QRS duration in patients with repaired tetralogy of Fallot: implications of infundibular disease. Circulation. 2007;116:1532–9.
Alshawabkeh LI, Opotowsky AR. Burden of heart failure in adults with congenital heart disease. Curr Heart Fail Rep. 2016;13:247–54.
Sabanayagam A, Cavus O, Williams J, Bradley E. Management of heart failure in adult congenital heart disease. Heart Fail Clin. 2018;14:569–77.
Book WM, Shaddy RE. Medical therapy in adults with congenital heart disease. Heart Fail Clin. 2014;10:167–78.
Stefanescu A, DeFaria Yeh D, Dudzinski DM. Heart failure in adult congenital heart disease. Curr Treat Options Cardiovasc Med. 2014;16:337.
Diller GP, Gatzoulis MA. Pulmonary vascular disease in adults with congenital heart disease. Circulation. 2007;115:1039–50.
Merchant FM, Kella D, Book WM, Langberg JJ, Lloyd MS. Cardiac resynchronization therapy in adult patients with repaired tetralogy of Fallot and left ventricular systolic dysfunction. Pacing Clin Electrophysiol. 2014;37:321–8.
Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:e81–e192.
Suradi HS, Hijazi ZM. Adult congenital interventions in heart failure. Interv Cardiol Clin. 2017;6:427–43.
Kenny D, Rhodes JF, Fleming GA, et al. 3-year outcomes of the Edwards SAPIEN transcatheter heart valve for conduit failure in the pulmonary position from the COMPASSION multicenter clinical trial. JACC Cardiovasc Interv. 2018;11:1920–9.
Silversides CK, Kiess M, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: outflow tract obstruction, coarctation of the aorta, tetralogy of Fallot, Ebstein anomaly and Marfan’s syndrome. Can J Cardiol. 2010;26:e80–97.
Stout KK, Broberg CS, Book WM, et al. Chronic heart failure in congenital heart disease: a scientific statement from the American Heart Association. Circulation. 2016;133:770–801.
Van De Bruaene A, Meier L, Droogne W, et al. Management of acute heart failure in adult patients with congenital heart disease. Heart Fail Rev. 2018;23:1–14.
Hermsen JL, Stout KK, Stempien-Otero A, Verrier ED, Mokadam NA. Long-term right ventricular assist device therapy in an adult with pulmonary atresia/intact ventricular septum. ASAIO J. 2018;64:e72–4.
Cedars A, Vanderpluym C, Koehl D, Cantor R, Kutty S, Kirklin JK. An Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) analysis of hospitalization, functional status, and mortality after mechanical circulatory support in adults with congenital heart disease. J Heart Lung Transplant. 2018;37:619–30.
VanderPluym CJ, Cedars A, Eghtesady P, et al. Outcomes following implantation of mechanical circulatory support in adults with congenital heart disease: an analysis of the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS). J Heart Lung Transplant. 2018;37:89–99.
Schweiger M, Lorts A, Conway J. Mechanical circulatory support challenges in pediatric and (adult) congenital heart disease. Curr Opin Organ Transplant. 2018;23:301–7.
Alshawabkeh LI, Hu N, Carter KD, et al. Wait-list outcomes for adults with congenital heart disease listed for heart transplantation in the U.S. J Am Coll Cardiol. 2016;68:908–17.
Ross HJ, Law Y, Book WM, et al. Transplantation and mechanical circulatory support in congenital heart disease: a scientific statement from the American Heart Association. Circulation. 2016;133:802–20.
Khan AM, Paridon SM, Kim YY. Cardiopulmonary exercise testing in adults with congenital heart disease. Expert Rev Cardiovasc Ther. 2014;12:863–72.
Dallaire F, Wald RM, Marelli A. The role of cardiopulmonary exercise testing for decision making in patients with repaired tetralogy of Fallot. Pediatr Cardiol. 2017;38:1097–105.
Stefanescu A, Macklin EA, Lin E, et al. Usefulness of the Seattle Heart Failure Model to identify adults with congenital heart disease at high risk of poor outcome. Am J Cardiol. 2014;113:865–70.
Baggen VJ, van den Bosch AE, Eindhoven JA, et al. Prognostic value of N-terminal pro-B-type natriuretic peptide, troponin-T, and growth-differentiation factor 15 in adult congenital heart disease. Circulation. 2017;135:264–79.
Heng EL, Bolger AP, Kempny A, et al. Neurohormonal activation and its relation to outcomes late after repair of tetralogy of Fallot. Heart. 2015;101:447–54.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Carazo, M.R., Landzberg, M.J., Jokhadar, M. (2020). Born with a Failing Right Heart. In: Tsao, L., Afari, M. (eds) Clinical Cases in Right Heart Failure. Clinical Cases in Cardiology. Springer, Cham. https://doi.org/10.1007/978-3-030-38662-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-38662-7_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-38661-0
Online ISBN: 978-3-030-38662-7
eBook Packages: MedicineMedicine (R0)